Abstract
Infective endocarditis is rare but carries significant morbidity, including risk of systemic embolization. A 67-year-old woman presented with endocarditis. Evaluation revealed a mobile mitral valve vegetation and a right atrial mass. Owing to prohibitive surgical risk, percutaneous aspiration thrombectomy was pursued. Immediate preprocedural transesophageal echocardiography revealed that the mitral mass had embolized in the interval, and it was incidentally found in the common left femoral artery on ultrasound. The patient underwent aspiration thrombectomy of the right atrial mass and open surgical extraction of the mitral valve vegetation from the femoral artery in the same index procedure. This case highlights the high embolization potential of these types of valvular vegetations and the need for rapid intervention.
Key Words: echocardiography, endocarditis, mitral valve, thrombus, ultrasound
Graphical Abstract
History of Presentation
A 67-year-old woman presented to an outside institution with lower back and hip pain, fevers, and chills lasting the preceding week. She was found to be in septic shock and was started on vasopressors and antibiotics. Initial laboratory testing revealed leukocytosis and lactic acidosis, and blood cultures were positive for Staphylococcus aureus. A transthoracic echocardiogram (TTE) followed by transesophageal echocardiogram (TEE) confirmed a large, mobile, mitral valve vegetation and right atrial mass. Magnetic resonance imaging (MRI) of the lumbar spine showed L2-L3 and L4-L5 discitis or osteomyelitis with right sacroiliac joint effusion. MRI also showed right psoas fluid collection or abscess. She was referred to our institution for cardiothoracic surgical evaluation of endocarditis with multiple systemic emboli.
Take-Home Messages
-
•
Left-side endocarditis carries with it significant morbidity and early intervention is crucial including for poor surgical candidates.
-
•
Ultrasound may be helpful in identifying the embolic site in cases where a large cardiac vegetation embolizes to the peripheral vasculature.
On physical examination, the patient was oriented to self only but following commands. Cardiac auscultation revealed a systolic murmur heard best at the apex. There was no jugular venous distention. The lungs were clear to auscultation bilaterally. The abdomen was soft, nontender, and nondistended. There was no peripheral edema.
Past Medical History
Her past medical history included end-stage renal disease on hemodialysis, hypertension, heart failure with preserved ejection fraction, hyperlipidemia, paroxysmal atrial fibrillation, and type 2 diabetes mellitus.
Differential diagnosis
At the time of her presentation to our institution, the diagnosis of septic shock due to infective endocarditis had been established. The source of her initial bacteremia was thought to be from her permanent hemodialysis line which had subsequently been exchanged. Vertebral osteomyelitis, right psoas abscess, and mitral valve infective endocarditis were thought to be sequelae of this initial central line–associated bloodstream infection.
Investigations
MRI of the brain demonstrated multiple punctate foci of ischemia in the bilateral cerebral hemispheres, which were concerning for septic emboli. TEE showed a large (2 cm × 1 cm), irregular, mobile pedunculated mass adherent to the posterior mitral valve leaflet (likely P1/P2) with associated mild to moderate mitral regurgitation (Videos 1 and 2). It also showed a large (3 cm × 2.4 cm), irregular mass with a broad-based neck adherent to the right atrial free wall extending to the interatrial septum at the level of the superior vena cava–right atrium junction (Video 3). This mass was predominantly fixed but had mobile components.
Management
Cardiothoracic surgery determined that she was at high to prohibitive risk for open heart surgery, given her multiple infected sites, comorbid conditions, recent strokes, and poor rehabilitation potential after surgery. Therefore, a catheter-based aspiration of the mitral valve vegetation and right atrial mass was planned. In the operating room, a preprocedural TEE was performed, which showed that the bulk of the mitral vegetation had embolized, with small residual fragments adherent to the mitral valve (Videos 4 and 5). The decision was made to proceed with aspiration and sample collection of the right atrial mass. Once aspiration was complete, whole-body CT angiography was planned to search for the embolized mitral valve vegetation.
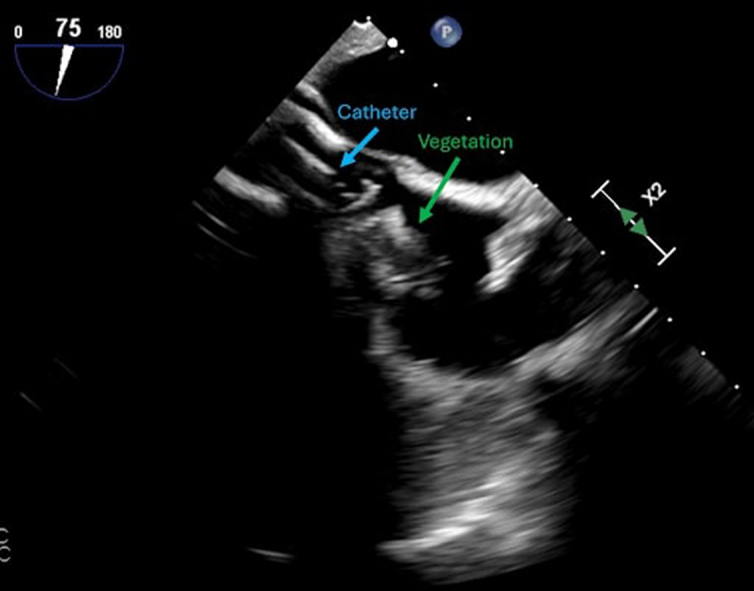
During preparation for femoral vein access, ultrasound of the left femoral site revealed a filling defect of the left femoral artery, which was suspicious for the embolized mitral valve vegetation. Right femoral artery access was obtained and a Rösch inferior mesenteric catheter was advanced over a wire into the left common iliac artery. An iliofemoral angiogram was performed, revealing a filling defect in the left common femoral artery involving the superficial femoral artery and profunda, consistent with what was likely the embolized mitral valve vegetation (Video 6). Next, percutaneous aspiration of the right atrial mass was performed with a 26-F Angiovac aspiration cannula using venous-venous bypass circuit and TEE guidance, yielding thrombus material (Video 7, Figures 1 and 2), however not all of the mass was removed owing to part of it being adherent to the atrial wall. Percutaneous aspiration of the femoral mass was contemplated, but owing to the delicate location of the mass at the femoral-profunda bifurcation, vascular surgery specialists were consulted in the laboratory and performed a left femoral cut-down, endarterectomy, and vegetation removal followed by surgical repair of the artery (Figure 3).
Figure 1.
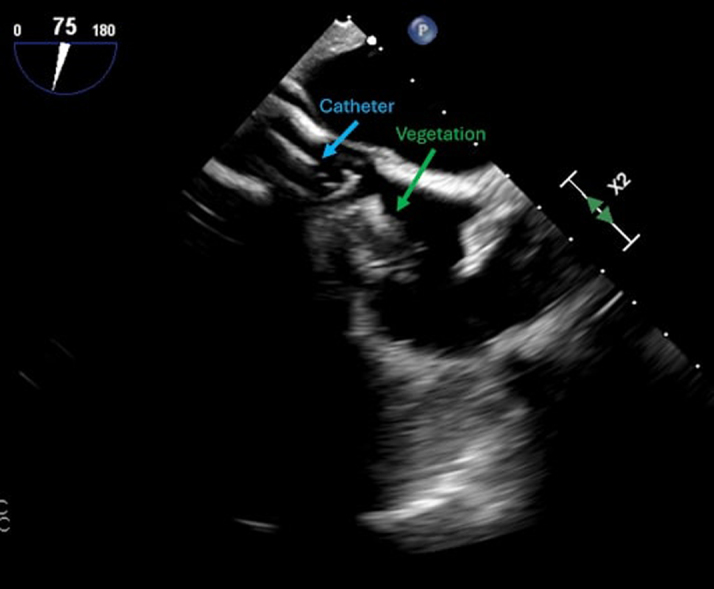
Intraprocedural Transesophageal Echocardiographic Midesophageal Bicaval View, Demonstrating 26-F Angiovac Aspiration Cannula Making Contact With Right Atrial Mass
Figure 2.
Fragments of Right Atrial Mass Removed by Means of Aspiration Thrombectomy
Figure 3.
Mitral Mass Removed by Means of Left Femoral Endarterectomy
Pathology revealed that both the right atrial and the femoral masses consisted of organizing blood clot, acute inflammatory exudate, bacterial colonies, and abundant calcifications, consistent with an organizing thromboembolism.
Outcome and Follow-Up
The patient was placed on a heparin drip and later changed to apixaban for anticoagulation. MRI of the lumbar spine was done, showing a persistent right psoas abscess and discitis. The right psoas abscess was drained by interventional radiology. Intravenous antibiotics were continued for 6 weeks.
Discussion
Infective endocarditis is a rare condition, with an annual incidence of approximately 2 to 12 cases per 100,000 people.1 It occurs as a result of damage to valvular endothelium or endocardium which exposes surfaces to which platelets and fibrin adhere and form a sterile vegetation.2 Bacteria in the bloodstream can then colonize this vegetation. Although it is rare, it carries significant morbidity and mortality in the form of heart failure, uncontrolled infection, and systemic embolization.2 In a large study, 21.1% of patients with left-side infective endocarditis had a new embolic event or died in 30 days.3 To prevent systemic embolism, the American Heart Association recommends considering valve surgery when the vegetation size is >10 mm.4 This recommendation is backed by multiple analyses showing that patients with this vegetation size have significantly increased odds of both embolism and mortality.3,4 In a small randomized control study, patients with left-side endocarditis, severe valve disease, and large vegetations who were randomized to early surgery had significantly reduced risk of death from any cause and embolic events compared with those who were randomized to conventional treatment.5 In the present case, the patient was not a surgical candidate, owing to acute and chronic medical conditions and acute strokes making bypass risky, so expedient definitive surgical intervention was not pursued. In cases of poor surgical candidates with large vegetations, it remains critical to pursue percutaneous vegetation aspiration as soon as possible. This is especially true in the case of Staphylococcus aureus infection, which has been identified as an independent predictor of poor outcomes in infective endocarditis.6 Transseptal catheter-based aspiration for a left-side mass may be a suitable alternative to traditional surgical management and would have been used in this case had the vegetation not migrated. These procedures are currently routinely used for right-sided masses.7, 8, 9 Examples of successful retrieval of left-side masses using this transseptal technique may be found in other papers in JACC: Case Reports.10
The presence of a large mitral mass on initial TEE that was not seen on subsequent preprocedural TEE 3 days later was a unique finding that highlighted the potential for rapid embolization and the need for early intervention to avoid devastating complications. The vegetation was fortunately found on ultrasound imaging while we were obtaining vascular access and resulted in quick surgical intervention and limited limb ischemia. This case highlights the high embolic potential of large mitral valve vegetations and the need for prompt early intervention. Furthermore, successful retrieval of left-side mitral valve vegetations via aspiration thrombectomy has been outlined in other papers in JACC: Case Reports and may remain a viable option for those who are at high surgical risk.10
Conclusions
We present a case of a large mitral valve vegetation that was complicated by septic emboli to the brain and the common femoral artery bifurcation before percutaneous aspiration could be performed. This demonstrates the significant risk associated with large left-side vegetations and the importance of early intervention when feasible. In cases where surgical options do not exist, aspiration thrombectomy may be a viable option for both right- and left-side masses.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The author attests they are in compliance with human studies committees and animal welfare regulations of the author’s institution and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
| Day 0 | Arrived at outside hospital; Started on vasopressors and antibiotics |
|---|---|
| Day 9 | Underwent TEE and was found to have mitral valve vegetation. |
| Day 11 | Transferred to our institution. |
| Day 15 | Underwent repeated TEE, showing a large mitral mass as well as a right atrial mass. |
| Day 18 | Went to the OR for catheter-based aspiration of the mitral valve vegetation and right atrial mass. The mitral valve vegetation was found to have migrated to the left femoral artery. Suction embolectomy of the right atrial mass and endarterectomy of the left femoral artery mass were performed. |
| Day 29 | Right psoas abscess drained by means of interventional radiology. |
| Day 71 | Completed 6 weeks of IV antibiotics. |
Appendix
Index transesophageal echocardiographic mid-esophageal 4-chamber view, demonstrating mobile pedunculated mass adherent to the posterior mitral valve leaflet (A2 scallop).
Index transesophageal echocardiographic mid-esophageal 2-chamber view, demonstrating mobile pedunculated mass adherent to the posterior mitral valve leaflet.
Index transesophageal echocardiographic midesophageal bicaval view, demonstrating irregular mass with a broad-based neck adherent to the right atrial free wall with extension to the interatrial septum at the level of superior vena cava–right atrium junction. The mass is predominantly fixed, but is associated with mobile fragments.
Intraoperative transesophageal echocardiographic midesophageal 4-chamber view, demonstrating echobright mass on the posterior leaflet of the mitral valve. There is no longer a pedunculated mass adherent to the posterior mitral valve leaflet.
Intraoperative transesophageal echocardiographic midesophageal 2-chamber view, demonstrating echobright mass on the posterior leaflet of the mitral valve adjacent to the mitral annulus with small, mobile echodensities, likely consistent with calcification and residual vegetation (P1 and A1 scallops).
Left iliofemoral angiogram, showing a filling defect in the left common femoral artery involving the superficial femoral artery and profunda.
Intraprocedural transesophageal echocardiographic midesophageal bicaval view, demonstrating 26-F Angiovac aspiration in the right atrium making contact with right atrial mass.
References
- 1.Bin Abdulhak A.A., Baddour L.M., Erwin P.J., et al. Global and regional burden of infective endocarditis, 1990-2010: a systematic review of the literature. Glob Heart. 2014;9(1):131–143. doi: 10.1016/j.gheart.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Chambers H.F., Bayer A.S. Native-valve infective endocarditis. N Engl J Med. 2020;383(6):567–576. doi: 10.1056/nejmcp2000400. [DOI] [PubMed] [Google Scholar]
- 3.Sambola A., Lozano-Torres J., Boersma E., et al. Predictors of embolism and death in left-sided infective endocarditis: the European Society of Cardiology EURObservational Research Programme European Infective Endocarditis Registry. Eur Heart J. 2023;44(43):4566–4575. doi: 10.1093/eurheartj/ehad507. [DOI] [PubMed] [Google Scholar]
- 4.Mohananey D., Mohadjer A., Pettersson G., et al. Association of vegetation size with embolic risk in patients with infective endocarditis: a systematic review and meta-analysis. JAMA Intern Med. 2018;178(4):502–510. doi: 10.1001/jamainternmed.2017.8653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang D., Kim Y., Kim S., et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366(26):2466–2473. doi: 10.1056/nejmoa1112843. [DOI] [PubMed] [Google Scholar]
- 6.Diab M., Guenther A., Sponholz C., et al. Pre-operative stroke and neurological disability do not independently affect short- and long-term mortality in infective endocarditis patients. Clin Res Cardiol. 2016;105(10):847–857. doi: 10.1007/s00392-016-0993-x. [DOI] [PubMed] [Google Scholar]
- 7.Zern E.K., Ramirez P.R., Rubin J., et al. Severe tricuspid valve endocarditis: a tale of 2 circuits. JACC Case Rep. 2021;3(11):1343–1349. doi: 10.1016/j.jaccas.2021.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer M.L., Parikshak M., Kiell C., Chugh A.R. Using aspiration-based tricuspid valve endocarditis debridement: highlighting imaging-based modification in a high-risk clinical scenario. JACC Case Rep. 2019;1(5):742–745. doi: 10.1016/j.jaccas.2019.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almanfi A., Nabous I. Percutaneous aspiration of vegetation in tricuspid valve infective endocarditis: a possible novel treatment option. JACC Case Rep. 2022;4(18):1151–1155. doi: 10.1016/j.jaccas.2022.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akhtar Y.N., Barry Iv N., Foster M.T., et al. Case series of percutaneous mechanical aspiration of mitral valve endocarditis. JACC Case Rep. 2022;4(9):523–528. doi: 10.1016/j.jaccas.2022.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Index transesophageal echocardiographic mid-esophageal 4-chamber view, demonstrating mobile pedunculated mass adherent to the posterior mitral valve leaflet (A2 scallop).
Index transesophageal echocardiographic mid-esophageal 2-chamber view, demonstrating mobile pedunculated mass adherent to the posterior mitral valve leaflet.
Index transesophageal echocardiographic midesophageal bicaval view, demonstrating irregular mass with a broad-based neck adherent to the right atrial free wall with extension to the interatrial septum at the level of superior vena cava–right atrium junction. The mass is predominantly fixed, but is associated with mobile fragments.
Intraoperative transesophageal echocardiographic midesophageal 4-chamber view, demonstrating echobright mass on the posterior leaflet of the mitral valve. There is no longer a pedunculated mass adherent to the posterior mitral valve leaflet.
Intraoperative transesophageal echocardiographic midesophageal 2-chamber view, demonstrating echobright mass on the posterior leaflet of the mitral valve adjacent to the mitral annulus with small, mobile echodensities, likely consistent with calcification and residual vegetation (P1 and A1 scallops).
Left iliofemoral angiogram, showing a filling defect in the left common femoral artery involving the superficial femoral artery and profunda.
Intraprocedural transesophageal echocardiographic midesophageal bicaval view, demonstrating 26-F Angiovac aspiration in the right atrium making contact with right atrial mass.




