Corresponding Author

Key Words: cardiac surgical procedures, cardiac tumors, cardiovascular surgical procedures, heart neoplasms, myxoma
Surgical resection is the mainstay of treatment for cardiac tumors, but the strategy to be adopted varies according to the site, size, and relationship with cardiac structures. When it comes to extensive left atrial tumors (Figure 1) in which it is not possible to peel the tumor from the adherent left atrial surfaces without compromising oncologic clearance, the procedure of choice proposed by some centers1 is cardiac autotransplantation: a procedure encompassing cardiac explantation, ex vivo tumor resection, and reconstruction of the heart with its subsequent reimplantation in its owner.
Figure 1.
Cardiac Tumors in the Left Atrium
In this issue of JACC: Case Reports, Lim et al2 reported a case of a giant left atrial ancient schwannoma (a tumor with advanced degenerative changes and diffuse hypocellular areas in its core) treated with extensive biatrial and interatrial septal resection followed by reconstruction of the heart anatomy. An important distinguishing feature of this case is that the surgical procedure was performed without autotransplantation via a modified superior transseptal approach and resection including the tumor en bloc with the entire left atrial roof, most of the posterior left atrial wall, the entire interatrial septum, and part of the right pulmonary vein antrum close to the right superior pulmonary vein. In comparison with autotransplantation, the modified superior transseptal approach does not include anastomoses in the aorta, pulmonary artery trunk, and inferior vena cava, which leads to maintenance of cardiac alignment and significant reduction in aortic cross-clamp times. The downside of this strategy is the worse exposure for the left pulmonary vein antrum and left atrial appendage.
Some important pieces of information about left atrial tumors to keep in mind:
-
1.
Benign myxomas are the most common tumors arising in the left atrium (approximately 80%) and are managed with prompt surgical resection because of the risk of embolization.3, 4, 5
-
2.
Tumors arising in the left atrium tend to grow into the atrial lumen and cause symptoms by obstructing blood flow or creating mitral regurgitation.3, 4, 5
-
3.
Left atrial tumors may simulate mitral valve disease and produce symptoms of heart failure and/or pulmonary hypertension.3, 4, 5
-
4.
The classic tumor plop is found in only 15% of cases.3, 4, 5
-
5.
Notwithstanding the higher frequency of myxomas in women, men are more likely to have events of embolization.6
-
6.
With myxomas, the incidence of embolization is associated with smaller size (≤4.5 cm) and softer tumors.7
-
7.
Being a malignant tumor and arising more often in the left atrium, leiomyosarcomas have a high rate of local recurrence and systemic spread.8
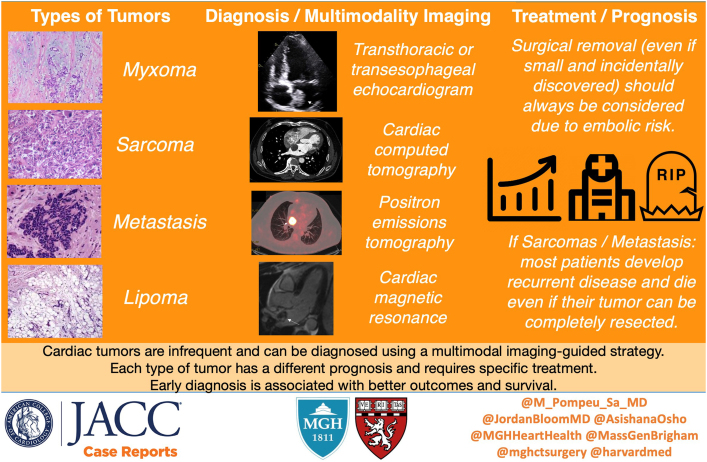
Although percutaneous and/or open surgical biopsy are the gold standard to establish the diagnosis, there is a role to be played by multimodality imaging in establishing the diagnosis and preoperative planning.9 Once a cardiac tumor is suspected (oftentimes after transthoracic or transesophageal echocardiogram), patients may be referred for cardiac magnetic resonance for further investigation. Cardiac magnetic resonance provides a complete multiplanar and noninvasive evaluation of the tumor and its potential involvement with the cardiac chambers and pericardium. Furthermore, information about the extracardiac structures often proves useful in preoperative planning. However, cardiac computed tomography (CT) has become increasingly commonplace in the assessment of cardiac tumors.10 Electrocardiogram-gated cardiac CT facilitates a more precise delineation of the tumor margins and relationship to tissue planes, which is particularly valuable for preoperative planning. Moreover, cardiac CT is optimal for the exclusion of obstructive coronary artery disease, which is also helpful in preoperative planning.10 Additionally, positron emission tomography (PET) facilitates a precise assessment of the metabolic activity of tumors using fluorodeoxyglucose (FDG).10,11 FDG-PET is useful for staging malignancies while also unveiling any myocardial and pericardial involvement. It is also helpful in the appraisal of initial responses to chemotherapy and radiotherapy. The amount of FDG uptake by tumors is used to differentiate between benign and malignant tumors.10,11
Besides the diagnosis, the multimodality imaging can be helpful with the surgical planning for resection of the tumor, being even more useful in the scenario in which surgeons decide to apply the surgical technique described by Lim et al.2 In the setting of resection of a cardiac tumor in the left atrium without removing the entire heart from the mediastinum, the preoperative recognition of anatomic structures and planes of dissection plays a major role because it helps with the recognition of presence/absence of normal anatomic landmarks that may be lost due to the presence of the tumor. This could define, for instance, if the surgeon will access the tumor via the right atrium and interatrial septum, via the left atrium directly, or via the left atrium roof, and so forth, or if the surgeon will have no choice but to remove the heart completely from the mediastinum to have access to all the structures and resect the tumor appropriately (as in situations such as primary cardiac sarcoma extending to the origin of the left pulmonary veins or involving the anterior left atrium1).
Be that as it may, the choice between superior transseptal, partial, and complete autotransplant relies on surgical expertise and needs to be individualized. Similarly to the world of structural heart in which well-established imaging protocols help in the decision-making process, surgeons should become more skilled in the art of preoperative imaging to make better decisions in terms of surgical strategies to be adopted in this scenario.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Al Abri Q., El Nihum L.I., Ali A., et al. Outcomes of full and partial cardiac autotransplantation for complex left-sided heart tumors. Ann Thorac Surg Short Reports. 2023;1(1):164–167. [Google Scholar]
- 2.Lim K., Ho J.Y.K., Chow S.C.Y., Fujikawa T., Wong R.H.L. Radical bi-atrial resection via a modified superior transseptal approach for a giant left atrial tumor. JACC Case Rep. 2024;29 [Google Scholar]
- 3.Pinede L., Duhaut P., Loire R. Clinical presentation of left atrial cardiac myxoma. A series of 112 consecutive cases. Medicine (Baltimore) 2001;80:159. doi: 10.1097/00005792-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Jelic J., Milicić D., Alfirević I., et al. Cardiac myxoma: diagnostic approach, surgical treatment, and follow-up. A twenty-year experience. J Cardiovasc Surg (Torino) 1996;37:113. [PubMed] [Google Scholar]
- 5.Pucci A., Gagliardotto P., Zanini C., et al. Histopathologic and clinical characterization of cardiac myxoma: review of 53 cases from a single institution. Am Heart J. 2000;140:134. doi: 10.1067/mhj.2000.107176. [DOI] [PubMed] [Google Scholar]
- 6.Elbardissi A.W., Dearani J.A., Daly R.C., et al. Embolic potential of cardiac tumors and outcome after resection: a case-control study. Stroke. 2009;40:156. doi: 10.1161/STROKEAHA.108.525709. [DOI] [PubMed] [Google Scholar]
- 7.Wang Z., Chen S., Zhu M., et al. Risk prediction for emboli and recurrence of primary cardiac myxomas after resection. J Cardiothorac Surg. 2016;11:22. doi: 10.1186/s13019-016-0420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pins M.R., Ferrell M.A., Madsen J.C., et al. Epithelioid and spindle-celled leiomyosarcoma of the heart. Report of 2 cases and review of the literature. Arch Pathol Lab Med. 1999;123:782. doi: 10.5858/1999-123-0782-EASCLO. [DOI] [PubMed] [Google Scholar]
- 9.Bruce C.J. Cardiac tumours: diagnosis and management. Heart. 2011;97:151–160. doi: 10.1136/hrt.2009.186320. [DOI] [PubMed] [Google Scholar]
- 10.Tyebally S., Chen D., Bhattacharyya S., et al. Cardiac tumors: JACC CardioOncology state-of-the-art review. JACC CardioOncol. 2020;2(2):293–311. doi: 10.1016/j.jaccao.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahbar K., Seifarth H., Schäfers M., et al. Differentiation of malignant and benign cardiac tumors using 18F-FDG PET/CT. J Nucl Med. 2012;53:856–863. doi: 10.2967/jnumed.111.095364. [DOI] [PubMed] [Google Scholar]