Abstract
Oblique lateral interbody fusion (OLIF) is a minimally invasive surgery for the treatment of lumbar degenerative diseases (LDD). Under normal bone mass(NB), supplemental with lateral plate (LP) fixation has been proven to provide stability and reduce complications. However, it is unclear whether OLIF combined with LP fixation can achieve satisfactory fixation effects in cases of osteoporosis(OP) or osteopenia (OS)? In this study, Eighteen L3-5 spinal specimens from 3 to 6 months old fresh calves were equally divided into 3 groups: group A (NB), group B (OS) and group C (OP). A load control scheme was adopted and evaluated using multidirectional nondestructive moments (± 7.5 N·m). An electronic universal tester and a tensile/torsion tester were simulated to generate 6 degrees of freedom of motion, and a VIC-3D three-dimensional optical full-field strain measurement system dynamically tracked the surgical segmental displacement. Each spine was evaluated under the following conditions at the L4-5 level: intact (INT); OLIF stand-alone (SA); cage supplemented with LP, cage supplemented with unilateral pedicle screws (UPS), and cage supplemented with bilateral pedicle screws (BPS). The current data show that With NB and OS models, LP fixation significantly reduced ROM in the LB and AR directions, with slightly less stability than BPS fixation and comparable to UPS. In the case of OP, LP fixation may increase the risk of internal fixation failure, and it is more preferable to choose BPS fixation with stronger stability.
Keywords: Osteoporosis, Fixation, Biomechanics, Lateral plate
Subject terms: Diseases, Medical research
Introduction
OLIF is an effective minimally invasive procedure for the treatment of LDD1–3. It establishes a surgical channel from the natural gap between the left psoas major muscle and the abdominal aorta, avoids damage to the small joints of the lumbar posterior column and the muscle-ligament complex, and has the advantages of minimally invasive indirect decompression, effective intervertebral fusion, and rapid postoperative recovery2,4. Compared with the traditional lumbar interbody fusion, the characteristics of the OLIF surgical approach allow the implantation of a larger cage and across the bilateral vertebral epiphyseal ring, thereby significantly improving the stability of the fusion segment interface4–6. Therefore, for patients with good bone density7, single-segment fusion and no endplate injury during surgery, simple OLIF can achieve satisfactory clinical results8,9. However, LDD mostly occurs in elderly patients with different degrees of bone loss. Bone loss reduces the elastic modulus and tensile strength of the vertebral body, which may increase the relative displacement of the vertebral body and Cage in the same radial direction, resulting in loosening or fracture of the internal fixation device5,10,11. In addition, in the absence of additional fixation, the stress is completely concentrated on the surface of the Cage and the end plate, increasing the risk of cage subsidence12,13. Therefore, when considering OLIF surgery, supplementary internal fixation can be used to avoid symptomatic cage subsidence. The construction of posterior BPS conforms to the three-column theory of spinal stability and can provide multi-plane stability14–16. However, BPS fixation requires additional posterior surgery and two anterior and posterior incisions, which increases surgical trauma and time. In addition, patients need to be transferred from lateral position to prone position during operation, which increases the risk of cage displacement17,18, which reduces the minimally invasive advantages of OLIF.
The lateral plate (LP) can complete the interface fixation through the same approach, it avoids the change of surgical position19,20. It has been shown to provide fixed stability19–21. Our previous study has confirmed that under normal bone conditions, LP can meet the stability requirements of the fixed segment22. However, the proportion of osteoporosis in patients with LDD is gradually increasing, and it is on the rise in the young age group. Osteoporosis seriously affects the bonding strength between the screw and the bone interface, and is prone to screw loosening, displacement or withdrawal23, which increases the risk of internal fixation failure24. So can LP fixation effectively improve stability and reduce cage subsidence when OLIF surgery is performed in patients with OS or OP? No related reports report. Therefore, the purpose of this study is to evaluate the effect of supplemental LP fixation on strengthening stability under different bone conditions from a biomechanical perspective, and to provide a reference for the application of LP in OLIF.
Materials and methods
The study was performed in compliance with the Chinese laws on animal experimentation and was approved by the Ethical Committee of General Hospital of Ningxia Medical University (No. KYLL-2022-1137). As agreed with the ethical committee, all methods were performed in accordance with the relevant guidelines and regulations and in accordance with ARRIVE guidelines.
Specimen preparation
Eighteen fresh L3-5 spinal specimens of 3–6 months old calves were selected. These specimens underwent X-ray examination to exclude fractures, lumbar deformity and any metastatic disease. After that, all specimens were carefully removed muscle and adipose tissue to avoid damage to spinal ligaments, intervertebral discs, and joint capsules. To form a functional spinal cord unit for testing. The specimens were divided into group A (NB group), group B (OS group) and group C (OP group), with 6 specimens in each group. The mean BMD was (1.49 ± 0.03) g/cm2, (1.48 ± 0.16) g/cm2, and (1.50 ± 0.08) g/cm2 in groups A, B, and C, respectively. The difference between the three groups was not statistically significant (P = 0.76). Group A did not do any treatment, and groups B and C were decalcified. All specimens were immersed in 10% formaldehyde solution for 24 h, and then rinsed with PBS liquid for 3 times, 30 min each time. After that, the group A specimens were sealed in a plastic bag and stored in a freezer at -20 °C. Groups B and C specimens were immersed in a configured 18.3% ethylene diamine tetraacetic acid (EDTA) solution for decalcification. The soaking solution was changed every day to keep the concentration of EDTA constant. X-ray and dual-energy X-ray absorptiometry (DEXA) scanner (syngo Osteo CT; siemens) and Micro CT (SkyScan 1176; belgium) to detect changes in bone mineral density (BMD). The mean BMD of the lumbar spine decreased to 75% –87% of the mean, which was defined as osteopenia. BMD below 75% of the mean was defined as osteoporosis, and severe osteoporosis was defined as BMD below 63% of the mean25. After the BMD reaches the expected level, the same, it is sealed and stored in a freezer at -20 ℃.
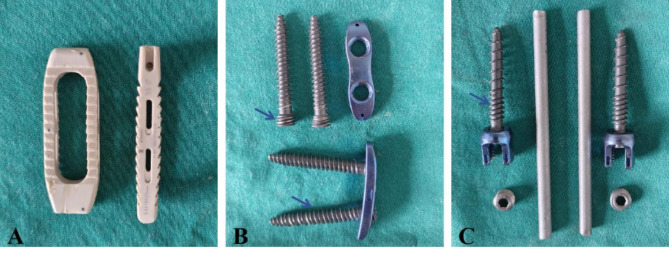
The device used was the “Minimally invasive small-incision lateral lumbar anterior interbody fusion system” (Wego Medical Devices Co., Ltd., Shandong, China), which consisted of a cage structure (8.5*18*85 mm, 55 mm, 0° anterior convexity, PEEK material) (Fig. 1A), pedicle screw (6.5*40 mm), and a connecting rod (5.5*40 mm) (Fig. 1C).The LP was 3D printed using medical titanium alloy material (Ti6A14 V), including a pair of bicortical bone screws (nut diameter 7.5 mm; screw length 50 mm) and lateral plate (length 45 mm, narrowest part 4 mm in the middle, screw hole diameter 10 mm, screw hole spacing 10 mm). The bottom of the lateral plate was designed with a light arc (Fig. 1B).
Fig. 1.
Experimental surgical model implants. (A) Large-sized Cage fusion applied in OLIF. (B) The LP fixation system: it consists of 1 lateral plate and 2 bicortical bone screws with a locking connection (arrow) at the end of the screw to the lateral plate and a denser thread than the pedicle screws. (C) Pedicle screw fixation system applied in UPS and BPS.
Surgical constructs
The surgical model of each specimen included four types of SA, LP, UPS and BPS fixation. The three groups of specimens were first tested in the INT with FE, LB and AR to obtain the baseline ROM values. Afterwards, the annulus fibrosus, nucleus pulposus and cartilaginous endplates were progressively removed using a 5-mm osteotome, spatula and nucleus pulposus forceps. Four consecutive fixations were performed after completion of the discectomy, including; SA; LP, UPS and BPS.
SA: The endplates were machined into rectangular holes using a high-speed oscillating saw cutter, and the appropriate Cage was selected according to the morphology of the calf vertebrae and inserted into the intervertebral space from the posterolateral direction to make close contact with the upper and lower endplates.
LP: After implantation of the fusion Cage, the LP were installed at the upper and lower edges of the L4-L5 vertebral bodies on the lateral side, and 2 cortical bone screws were screwed through the LP across the epiphyseal rings bilaterally to complete the interfacial fusion fixation.
UPS and BPS: The bilateral intervertebral plate space and articular surface of the synchondrosis were exposed, the Weinstein method was used to locate the bilateral pedicle entry points, pedicle screws were implanted unilaterally or bilaterally, the pre-curved rods were installed, and the screws were screwed into the nuts for fixation.
Biomechanical testing
The specimens were thawed for 48 h at room temperature until a full range of flexion and extension was possible. The upper end of L3 vertebral body and the lower end of L5 vertebral body were embedded and fixed with denture base resin (denture base resin type II), after which they were fixed with a cylindrical metal fixation device and attached to the base of the test device for pure moment loading application. An electronic universal tester (SUNS, Shenzhen, China; resolution 0.1 N) produced FE and LB of the specimen. The specific operation is as follows: by applying an axial load to the upper tooling center, the experimental bone is installed on the side of the tooling center, and an offset force arm is formed between the upper tooling center and the experimental bone axis. The torque load is formed by the axial load and the offset force arm. The mechanical testing machine applies a vertical upward or downward load. Because the adjustment mechanism can control the distance between the fixture and the center of the test device, an eccentric torque can be generated. After the spinal model is subjected to the torque, the upper fixture can realize the flexion and extension of the spinal model after the adjustment of the degree of freedom, and the lower fixture can realize the left bending and right bending of the spinal model after the adjustment of the degree of freedom. Tensile/torsion tester (DYNA-MESS, Germany; resolution 0.01 N·m) produced AR of the specimen. The specific operation is as follows: The fixed connection between the experimental instrument and the experimental bone is realized by the tooling, so as to ensure that the torque axis of the torsion testing machine coincides with the central axis of the experimental bone. The torsion torque is applied by the testing machine to ensure the torsion test of pure torque. When the spine torsion test is carried out, the mechanical testing machine applies a torsion load, and the axis of the fixture is adjusted to coincide with the axis of the testing machine by adjusting the mechanism. The other four degrees of freedom of the test device are eliminated by the pad block, and the left rotation and right rotation motion can be realized.
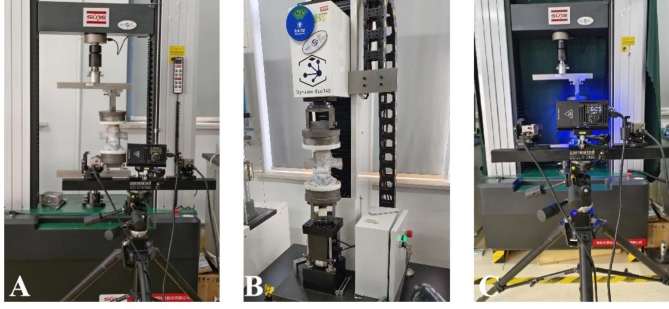
Both spine simulators could be made to produce a 6-degree-of-freedom direction of motion (Fig. 2A and B). Surgical segmental displacements were dynamically tracked using a VIC-3D three-dimensional optical full-field strain measurement system (ACQTEC instrucments technologies, Coltd, Shanghai, China; camera resolution 4096·3000pixels; camera frame rate 30FPS; in-plane displacement resolution 0.000005·field of view; the out-of-plane displacement resolution is 0.00001·field of view ; strain resolution 20µstrain.) (Fig. 2C).
Fig. 2.
Testing of all experimental devices. (A) Electronic universal tester generating FE and LB of the specimen. (B)Tensile/torsion tester generating AR of the specimen. (C)VIC-3D system dynamically tracking the surgical segment displacement.
After the upper and lower ends of the vertebrae were securely fixed, pure torque was applied to the L3 vertebrae via a servomotor. The direction of the load was adjusted to induce FE, LB, and AR. The test sequence was (1) SA, (2) LP, (3) UPS, (4) BPS. Two preconditioning cycles were performed on the specimens to avoid the viscoelastic effect of the spine before recording the motion data for each loading scenario. To minimize the effect of different surgical methods on specimen flexibility, an unloading and recovery time of 10 - minute was set between each surgical method. No compressive preload was applied to the specimen26. A load control protocol was used to apply a pure moment at the tail at a rate of 1 (°)/s, applied quasi-statically in increments of 1.5 Nm, with each incremental load held for 45s, with a maximum value of 7.5 Nm. The ROM was expressed in the form of Euler angles (°) in the x-, y-, and z-axes. The samples were kept moist by spraying 0.9% saline throughout the test. All tests were conducted at room temperature of 25 °C.
Statistical analysis
Statistical analysis was performed using SPSS 24.0 (IBM Corp., Armonk, NY, USA) statistical software. For all models ROM values were recorded and expressed as mean standard deviation (SD). The degree of decrease or increase in ROM was expressed as a percentage (%), namely: (ROM surgical model -ROMINT)/ROMINT*100. A larger value of ROM indicates a greater instability of the fixed segments. Comparison of ROM data was performed by one-way repeated measures ANOVA, and between-group differences were analyzed using a Tukey post hoc test was used for two-by-two comparisons between groups. p < 0.05 was considered a statistically significant difference.
Results
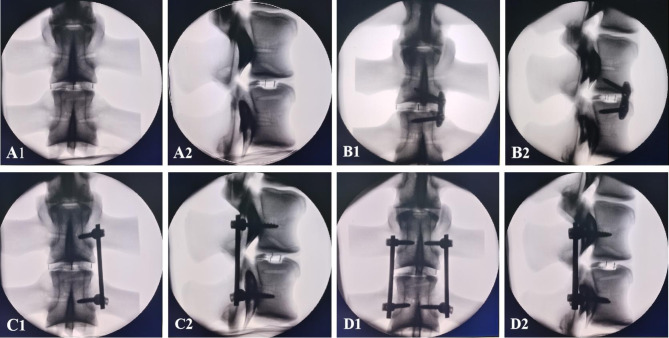
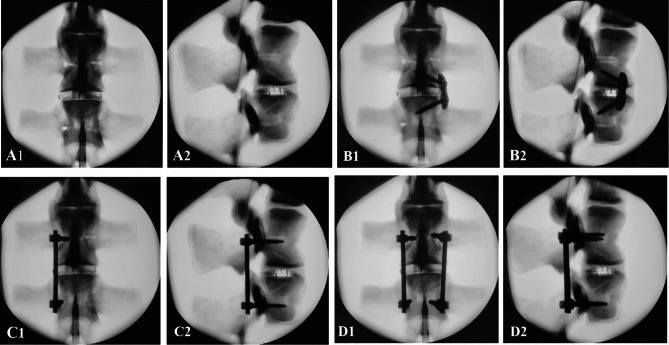
X-ray film outcomes
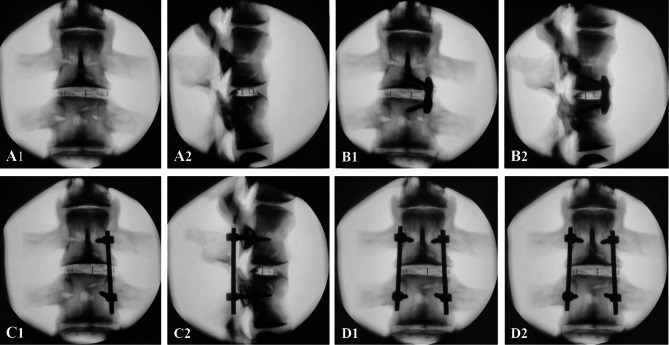
X-rays showed no vertebral fractures were observed and the fusion was fixed in place and well positioned. There were no signs of vertebral fracture, screw or LP loosening or breakage in any of the tested scenarios (Figs. 3, 4 and 5). Table 1 provides the complete ROM for all loading modes, and the mean normalized instrumentation level ROM datas are shown in Fig. 6A-C for visual comparisons across all fixation configurations and all test orientations.
Fig. 3.
Under NB, X-ray showed that the implants were well positioned, and no screw breakage or entry into the spinal canal was observed. (A) SA surgical model; (B) LP surgical model; (C) UPS surgical model; (D) BPS surgical model.
Fig. 4.
Under BM, X-ray showed that the implants were well positioned, and no screw breakage or entry into the spinal canal was observed. (A) SA surgical model; (B) LP surgical model; (C) UPS surgical model; (D) BPS surgical model.
Fig. 5.
Under OP, X-ray showed that the implants were well positioned, and no screw breakage or entry into the spinal canal was observed. (A) SA surgical model; (B) LP surgical model; (C) UPS surgical model; (D) BPS surgical model.
Table 1.
The average ROM of L4/5 level under different Surgical models (°).
| Working state | INT | SA | LP | UPS | BPS | |
|---|---|---|---|---|---|---|
| NB | FE | 4.27 ± 0.07 | 2.21 ± 0.04* | 1.11 ± 0.12*† | 0.66 ± 0.01*†$ | 0.62 ± 0.01*†$ |
| LB | 5.19 ± 0.02 | 2.49 ± 0.08* | 0.93 ± 0.09*† | 0.95 ± 0.16*†‡ | 0.87 ± 0.14*†‡ | |
| AR | 1.94 ± 0.03 | 1.14 ± 0.11* | 0.81 ± 0.10*† | 0.76 ± 0.08*†‡ | 0.59 ± 0.06*†$# | |
| OS | FE | 4.49 ± 0.02 | 2.44 ± 0.06* | 1.32 ± 0.11*† | 0.89 ± 0.03*† | 0.86 ± 0.03*†$ |
| LB | 5.51 ± 0.1 | 2.88 ± 0.1* | 1.10 ± 0.09*† | 1.11 ± 0.06*†‡ | 1.02 ± 0.4*†‡ | |
| AR | 2.22 ± 0.05 | 1.37 ± 0.11* | 0.95 ± 0.11*† | 0.91 ± 0.10*†‡ | 0.78 ± 0.17*†$# | |
| OP | FE | 5.02 ± 0.05 | 2.85 ± 0.09* | 1.83 ± 0.23*† | 1.09 ± 0.01*† | 1.04 ± 0.01*†$# |
| LB | 6.40 ± 0.42 | 3.28 ± 0.02* | 1.61 ± 0.07*† | 1.64 ± 0.15*†‡ | 1.43 ± 0.12*†‡# | |
| AR | 2.48 ± 0.11 | 1.60 ± 0.11* | 1.17 ± 0.06*† | 1.15 ± 0.07*†‡ | 0.92 ± 0.17*†$# |
Values are presented as mean ± SD.
*Significant difference from INT (P < 0.05).
†Significant difference from SA (P < 0.05).
‡Significant difference from LP (P > 0.05).
$Significant difference from LP (P < 0.05).
#Significant difference from UPS (P < 0.05).
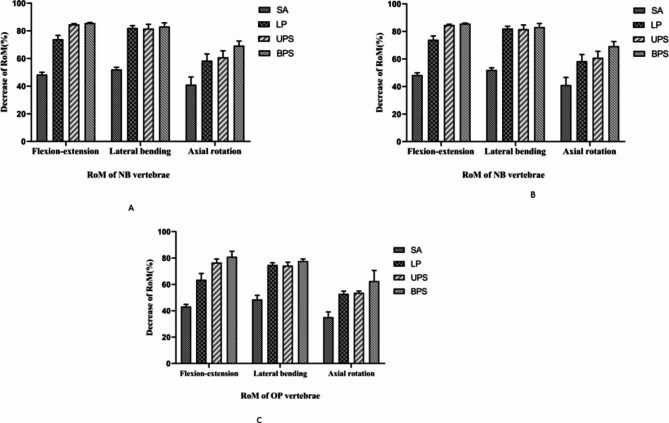
Fig. 6.
Percentage normalization of different fixation modalities using ROM of INT as a baseline. (A) ROM of each surgical model under NB conditions; (B) ROM of each surgical model under OS conditions; (C) ROM of each surgical model under OP conditions.
Changes of vertebral BMD
Group B had a BMD of (1.16 ± 0.04) g /cm2 at 4 weeks of decalcification, which meets the criterion for bone loss, and the vertebral body BMD was reduced by 24.32% compared with that before decalcification, which met the criteria of bone loss, stopped decalcification, and was placed in the refrigerator at -20℃ for freezing and preservation. BMD (0.90 ± 0.65) g /cm2 at 6 weeks of decalcification in group C. At this time, vertebral BMD was reduced by 39.36% compared with that before decalcification, which met the criteria of osteoporosis, and decalcification was stopped, and was sealed and kept in freezing and preservation for spare use.
Flexion and extension
Regardless of bone condition, ROM in each loading FE direction was significantly reduced relative to INT in SA, LP, UPS, and BPS fixation (P < 0.001). Group A had a reduction of 48.48%, 74%, 84.78%, and 85.71%, respectively. Group B had a reduction of 45.87%, 70.82%, 80.18%, and 81.84%, respectively. Group C decreased by 43.22%, 63.55%, 78.49% and 81.28%, respectively. Compared with SA, supplemental UPS or BPS fixation significantly reduced the ROM of FE (P < 0.001) and provided better control of anterior flexion and posterior extension motions, with a change of 70.45%, 63.37%, and 60.10% for UPS; and a change of 72.27%, 65.8%, and 64.82% for BPS, respectively. The reduction was not significant with supplemental LP fixation, with changes of 49.55%, 46.09%, and 35.79%, respectively, and the ROM was higher in FE working conditions for both SA and LP in different bone conditions. With the increase of the degree of osteoporosis, the improvement of ROM fixed by various structures gradually decreased. There was no significant difference between the two fixation methods of UPS and BPS in NB and OS (P > 0.05). Under OP, BPS fixation provided the strongest fixation and significantly reduced the ROM of FE (P < 0.05).
Lateral bending
Under different bone conditions, compared with INT, the ROM of SA, LP, UPS and BPS decreased significantly (P < 0.05), and the decrease rates in group A were 52.02%, 82.08%, 81.70% and 83.24%, respectively. The decrease rates of group B were 47.73%, 80.04%, 79.85% and 81.49%, respectively. The decrease rates of group C were 48.67%, 74.8%, 74.33% and 77.78%, respectively. Similarly, as the degree of osteoporosis increases, the stability of various structural fixations gradually decreases. In the LB condition, additional internal fixation further reduced ROM compared with SA (P < 0.05). Adding LP structures reduced the ROM of SA structures 62.65%, 61.81% and 50.91% (P < 0.01). Supplemental UPS and BPS internal fixation reduced the ROM of the SA structure 61.85%, 61.45%, 50% and 65.06%, 64.58%, 56.71% (P < 0.001), and all three internal fixation modalities provided better control of LB motion. The BPS structure showed greater overall ROM reduction than the UPS and LP structures, but there were no significant differences (P > 0.05).
Axial rotation
In the direction of AR movement, a similar trend to LB was observed. The ROM of SA, LP, UPS, and BPS were significantly lower than that of INT (P < 0.05), with rates of decrease of 40.93%, 58.55%, 60.62%, and 69.43% in group (A) The rates of decrease in group B were 38.28%, 57.21%, 59.01%, and 64.86% in group (B) Group C The decline rates were 35.22%, 52.63%, 53.44%, and 62.75%, respectively. The reduction in ROM for each fixation in group C was lower than that in groups A and B with the same fixation method. The LP and UPS structures reduced ROM equivalently (P = 0.579). The BPS fixation provided the most rigid structure and was significantly more stable than the LP and UPS structures, with a reduction in ROM of 26.25%, 17.89%, and 21.36% compared to that in the LP structure, and 22.37%, 14.29%, and 20% compared to the UPS structure (P < 0.05).
Discussion
OLIF has been widely used in minimally invasive treatment of LDD1,2,27. Compared with cages placed through anterior and posterior approaches, the OLIF lateral approach allows the placement of a wider cage that is larger and spans the epiphyseal ring. It not only increases the contact area between the cage and the endplate, but also effectively restores the physiological lordosis of the lumbar spine2,5, and provides the axial and coronal rigidity of the anterior column. Preservation of the posterior muscle-ligament complex limits the flexion-extension motion of the fused segments and provides greater segmental stability. Given this benefit of lateral lumbar fusion, it has been suggested that OLIF may not require extensive or invasive posterior fixation3,13. Therefore, alternative and less invasive fixation methods are considered to achieve stability in lateral fixation. In the current biomechanical study, the authors describe a new single-level fusion fixation technique that eliminates the risk of posterior column articular synchondrosis damage28. LP placement using the same surgical approach without extending the intraoperative incision footprint, avoiding changes in patient position and damage to posterior lumbar structures, which may reduce blood loss, operative time, and risk of infection19,20,22. Several studies have demonstrated that supplemental LP can biomechanically improve the stability of intervertebral fusion structures19,22,28–30, reduce Cage subsidence, and increase fusion rates31. However, the results of the above studies were based on normal bone quality, and to our knowledge, whether OLIF combined with LP fixation in the presence of bone loss or osteoporosis can satisfy the need for intervertebral stability has not been studied. In this study, we not only evaluated the biomechanics of the LP under different bone conditions, but also compared it with OLIF combined with other fixation modalities.
The results show that compared with INT, the ROM of all fixed modes is significantly reduced. The results of the study are similar to Song et al.19 and Mcmains et al.32 among all the fixed models, the observed trend is that the ROM decreases sequentially according to BPS, UPS, LP, SA in FE; BPS, LP, UPS, SA in LB, and BFS, UPS, LP, SA in AR. The SA ROM exceeds the rest of the fixed models, especially in FE and AR, and it is considered that this phenomenon is related to the unequal height of front and rear sidewalls of this Cage. However, compared with the SA of Fogel et al.15 (FE-31.6%, LB-32.5%, AR-69.4%) and Den Haese et al.33 (FE-36%, LB-42%, AR-56%) lateral approach, the stability of SA model in this study was improved (FE-45.87%, LB-52.02%, AR-40.93%), which can be attributed to the wider cage used in OLIF. Since the OLIF procedure minimizes the interference with the normal anatomical structure of the human body, SA reduces the need for additional screw fixation34, which is consistent with our clinical observations. After supplemented with LP fixation, the primary stability of SA in all directions was significantly enhanced, especially in LB and AR. It has been reported that the LP has little effect on the lumbar FE motion limitation14,21, this study confirmed this point again. In FE, the ROM of the LP structure was 14.8% lower than that of the SA fixation, and the flexion and extension stability were weak. The reason for this result may be that during the FE movement, the LP was fixed on the outside of the vertebral body. Although the special placement angle of the screw increased the depth of the screw, the longitudinal axis of the screw used intersected with the lumbar rotation axis at a small angle, and the force arm on the sagittal plane and cross section was lower than that of the BPS screw, so the limitation of ROM was very small. Therefore, in clinical practice, we usually recommend that patients wear a lumbar brace after surgery to avoid excessive flexion and extension of the lumbar spine. After the posterior pedicle screw fixation was added, the stability of each motion state was further improved compared with the normal model, especially the stability enhancement was more obvious in FE, which was related to the pedicle screw passing through the locking facet joint and reducing the flexion and extension movement of the facet joint35. In terms of LB, LP fixation significantly reduced intervertebral ROM, indicating the inherent benefits of direct anterior column fixation. The ROM of LP in FE, LB and AR decreased by 74%, 82.08% and 58.55% respectively under NB, and decreased by 70.82%, 80.04% and 57.21% respectively under OS. The stability of LP in the NB and OS models were similar to that of the integrated LP designed by Basra et al.36 (FE-73%, LB-79%, AR-57%), which was higher than that of the double-hole side plate structure reported by Nayak et al.37 (FE-52.3%, LB-71%, AR-45.3%). This may be related to the integrated structure of the LP device. That is, the self-locking formation of the screws with the side plates through threads and the blocking double-locking integrated design between the tail of the screws and the side plates, to some extent, form a solid frame structure between the screws and the steel plates and transfer the pressure to the vertebral body for fixation38, allowing it to achieve stability in lateral fixation as an integrated design. Compared to the UPS, the LP has comparable stability in the LB and AR, and the overall ROM is comparable between the LB direction and the BPS structure. Results were similar to those of Bozkus et al.39 using 4 cortical screws for LP fixation (FE -77.5%, LB -89%, AR -50%). Except for a small change in the FE state, the stability of the surgical segment in the OLIF-LP fixation model increased significantly, which was consistent with previous biomechanical studies5,6,15,19,20,22,28. By providing AR and LB comparable to BPS rigidity, LP significantly reduced the need for posterior fixation in these respective planes. Clinically, Dakwar et al.31 reported a strategy of LP combined with multilevel interbody fusion for the treatment of degenerative scoliosis in adults, and the results showed that minimally invasive assisted fixation methods including UPS and LP could be used for multilevel LLIF. Therefore, various fixation methods, including LP fixation, are expected to further explore the potential marginal differences in intraoperative fixation needs. Combining the literature and our study, we believe that single-level LP fixation can satisfy the intervertebral stabilization needs for both NB and OS.
Although many previous biomechanical and clinical studies15,19,20,22,28,30,31,35 have evaluated the optimal supplementation device for LLIF. However, few biomechanical studies have evaluated the stability of LP in OP. Liu et al.35 analyzed the effect of osteoporosis on the biomechanics of various supplemental fixations by building a finite element model of L3-S1 and analyzing the effect of osteoporosis on the biomechanics of various supplemental fixations. The results showed that the ROM of a single segment in the OP model had greater maximum stresses on the fusion apparatus, endplate, and fixation instruments than in the normal model, which may increase the risk of fracture and internal fixation failure. Song et al.19 concluded that LP fixation in the OP condition does not provide adequate strength and may increase the risk of fusion displacement and subsidence. In the present study, under OP, the LP fixation model was less stable than the above mentioned literature reports15,36,39 (FE -63.55%, LB -74.8%, and AR -58.55%) in all movement states. The ROM was greater in the OP model in all movement patterns under the same fixation regimen compared to the NB and OS models in the same group. This discrepancy may be explained by the fact that the modulus of elasticity of the OP model is less than that of the normal model, the implant-bone interface strength may be insufficient, and the internal fixation is less resistant to pullout when external forces are present. Therefore, the ROM restriction is not as good as that of the normal model, which may be the reason why fusion subluxation is more likely to occur in a more spine than in a normal spine. Compared to the NB and OS models, the OP condition showed a downregulation in the FE, LB and AR motion state fixation model stability, with a less pronounced decrease in BPS, which decreased by 4.43%, 0.56%; 5.46%, 3.71% and 6.68%, 2.11%, respectively. In contrast, LP and UPS decreased more than BPS fixation in the osteoporotic condition, especially in FE and AR exercise, the reason for which may be related to the stress redistribution due to the imbalance inherent in the lumbar fixation segments of UPS and LP fixation. Under OP, the ROM reduction of each fixation method was significantly lower than that of the normal bone mass group and the bone mass reduction group, but there was no significant difference in the ROM reduction of BPS fixation. BPS fixation provides the most rigid structure, and its stability is significantly higher than that of LP structure and UPS structure. Compared with LP structure, the ROM of BPS is reduced by 26.25%, 17.89% and 21.36%, respectively. Compared with UPS structure, the ROM of BPS is reduced by 22.37%, 14.29% and 20%, respectively. As BPS fixation further increases the stiffness of the surgical segment, it reduces the coupled motion effects40 that may be caused by UPS and LP fixation and provides a stable mechanical environment for early implant fusion5,6. Also, the likelihood of fatigue rupture in the long term of the pedicle nail bar will be reduced with the reduced stress on the nail bar19,20. Therefore, in osteoporosis, BPS fixation can provide better implant-bone interface strength due to multiple fixation points and better load distribution, which may be more desirable.
Limitations
There are several limitations to this study. Firstly, the results of in vitro biomechanical testing reflect only immediate postoperative stability and do not take into account the long-term effects of the biological healing process on the fixation interface. Second, the small sample size of the study group limited its statistical power. Multiple fixation regimens were tested on the same specimen, and repeated implantation and extraction of screws may lead to bone microstructural damage in the nail tracts, affecting the extraction strength and structural stiffness of later fixation modalities in the sequence. Finally, the constructed in vitro animal model specimens cannot well represent the actual clinical situation, such as the exclusion of muscle effects. Therefore, further clinical studies are needed to compare the effects of various fixation methods.
Conclusions
LP fixation stability was significantly better than SA, especially in the LB and AR directions, and the overall stability was weaker than that of BPS fixation and comparable to that of UPS. Under OP, LP fixation may increase the risk of failure of internal fixation. It may be more desirable to choose BPS fixation.
Acknowledgements
This study was supported by Ningxia Provincial Key Research and Development Planed Projects (No.2023BEG02017); General Hospital of Ningxia Medical University Medical Engineering Special Project (No. NYZYYG-005).
Author contributions
Z.G. designed experiments. Z.W., and W.Y. performed experiments. X.L., S.L., Z.C., and J.Z. analysed data. Z.W. wrote the manuscript. All authors revised the manuscript.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhiqiang Wang and Wanzhong Yang contributed equally to this work.
References
- 1.Abe, K. et al. Perioperative complications in 155 patients who underwent oblique lateral Interbody Fusion surgery: perspectives and indications from a Retrospective, Multicenter Survey. SPINE42, 55–62 (2017). [DOI] [PubMed] [Google Scholar]
- 2.Woods, K. R., Billys, J. B. & Hynes, R. A. Technical description of oblique lateral Interbody Fusion at L1-L5 (Olif25) and at L5-S1 (Olif51) and evaluation of Complication and Fusion Rates. SPINE J.17, 545–553 (2017). [DOI] [PubMed] [Google Scholar]
- 3.Ziino, C. et al. Single position Versus lateral-then-prone positioning for lateral Interbody Fusion and Pedicle Screw fixation. J. Spine Surg.4, 717–724 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wen, J. et al. Unilateral versus bilateral percutaneous pedicle screw fixation in oblique lumbar Interbody Fusion. WORLD NEUROSURG.134, e920–e927 (2020). [DOI] [PubMed] [Google Scholar]
- 5.Fan, K. et al. Biomechanical Analysis of Double-Level Oblique Lumbar Fusion with different types of fixation: a Finite element-based study. ORTHOP. SURG.15, 1357–1365 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang, S. et al. Oblique lateral Interbody Fusion combined with different internal fixations for the treatment of degenerative lumbar spine disease: a finite element analysis. BMC MUSCULOSKEL DIS.23, 206 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xue, S. & Wu, T. Biomechanical performances of an oblique lateral Interbody Fusion Cage in models with different bone densities: a finite element analysis. Indian J. Orthop.57, 86–95 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He, W. et al. Standalone oblique lateral Interbody Fusion Vs. Combined with Percutaneous Pedicle Screw in Spondylolisthesis. BMC MUSCULOSKEL DIS.21, 184 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu, J. et al. Modic Changes (mcs) Associated with Endplate Sclerosis can prevent cage subsidence in oblique lumbar Interbody Fusion (Olif) stand-alone. WORLD NEUROSURG.138, e160–e168 (2020). [DOI] [PubMed] [Google Scholar]
- 10.Ehresman, J. et al. Vertebral bone quality score and postoperative lumbar Lordosis Associated with need for reoperation after lumbar Fusion. World Neurosurg.140, e247–e252 (2020). [DOI] [PubMed] [Google Scholar]
- 11.Tempel, Z. J., Gandhoke, G. S., Okonkwo, D. O. & Kanter, A. S. Impaired bone Mineral Density as a predictor of Graft Subsidence following minimally invasive transpsoas lateral lumbar Interbody Fusion. Eur. Spine J.24 (Suppl 3), 414–419 (2015). [DOI] [PubMed] [Google Scholar]
- 12.Soriano-Baron, H. et al. Biomechanical effects of an oblique lumbar peek cage and posterior augmentation. World Neurosurg.126, e975–e981 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Zeng, Z. Y. et al. Complications and Prevention strategies of oblique lateral Interbody Fusion technique. Orthop. Surg.10, 98–106 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cappuccino, A. et al. Biomechanical Analysis and review of lateral lumbar Fusion constructs. SPINE35, S361–S367 (2010). [DOI] [PubMed] [Google Scholar]
- 15.Fogel, G. R., Parikh, R. D., Ryu, S. I. & Turner, A. W. Biomechanics of lateral lumbar Interbody Fusion constructs with lateral and posterior plate fixation: Laboratory Investigation. J. Neurosurg-Spine. 20, 291–297 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Kornblum, M. B., Turner, A. W., Cornwall, G. B., Zatushevsky, M. A. & Phillips, F. M. Biomechanical evaluation of stand-alone lumbar polyether-ether-ketone interbody cage with Integrated screws. Spine J.13, 77–84 (2013). [DOI] [PubMed] [Google Scholar]
- 17.Amato, V., Giannachi, L., Irace, C. & Corona, C. Accuracy of Pedicle Screw Placement in the Lumbosacral spine using conventional technique: computed Tomography Postoperative Assessment in 102 consecutive patients. J. Neurosurg-Spine. 12, 306–313 (2010). [DOI] [PubMed] [Google Scholar]
- 18.Xue, H., Tu, Y. & Cai, M. Comparison of Unilateral Versus bilateral instrumented transforaminal lumbar Interbody Fusion in degenerative lumbar diseases. Spine J.12, 209–215 (2012). [DOI] [PubMed] [Google Scholar]
- 19.Song, C. et al. Biomechanical Evaluation of Oblique Lumbar Interbody Fusion with various fixation options: a finite element analysis. Orthop. Surg.13, 517–529 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang, Z., Fogel, G. R., Liao, Z., Sun, Y. & Liu, W. Biomechanical analysis of lateral lumbar Interbody Fusion constructs with various fixation options: based on a validated finite element Model. World Neurosurg.114, e1120–e1129 (2018). [DOI] [PubMed] [Google Scholar]
- 21.Laws, C. J., Coughlin, D. G., Lotz, J. C., Serhan, H. A. & Hu, S. S. Direct lateral Approach to lumbar Fusion is a Biomechanically Equivalent Alternative to the Anterior Approach: an in Vitro Study. Spine37, 819–825 (2012). [DOI] [PubMed] [Google Scholar]
- 22.Cai, Z. et al. Evaluation of the Stability of a novel lateral plate internal fixation: an in Vitro Biomechanical Study. World Neurosurg.158, e237–e244 (2022). [DOI] [PubMed] [Google Scholar]
- 23.Di Silvestre, M., Parisini, P., Lolli, F. & Bakaloudis, G. Complications of thoracic pedicle screws in Scoliosis Treatment. Spine32, 1655–1661 (2007). [DOI] [PubMed] [Google Scholar]
- 24.Hou, Y. & Yuan, W. Influences of Disc Degeneration and Bone Mineral density on the Structural Properties of Lumbar End Plates. Spine J.12, 249–256 (2012). [DOI] [PubMed] [Google Scholar]
- 25.Egermann, M., Goldhahn, J. & Schneider, E. Animal models for fracture treatment in osteoporosis. Osteoporos. Int.16 (Suppl 2), S129–S138 (2005). [DOI] [PubMed] [Google Scholar]
- 26.Wilke, H. J., Wenger, K. & Claes, L. Testing criteria for spinal implants: recommendations for the standardization of in Vitro Stability Testing of spinal implants. Eur. Spine J.7, 148–154 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu, H. F. et al. Comparison of oblique lateral Interbody Fusion (Olif) and minimally invasive transforaminal lumbar Interbody Fusion (Mi-Tlif) for treatment of lumbar degeneration disease: a prospective cohort study. Spine47, E233–E242 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le Huec, J. C., Liu, M., Skalli, W. & Josse, L. Lumbar lateral interbody cage with plate augmentation: in Vitro Biomechanical Analysis. Eur. Spine J.11, 130–136 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reis, M. T. et al. Biomechanical evaluation of lateral lumbar Interbody Fusion with secondary augmentation. J. Neurosurg-Spine. 25, 720–726 (2016). [DOI] [PubMed] [Google Scholar]
- 30.Wang, Y. et al. Biomechanical evaluation of an oblique lateral locking plate system for oblique lumbar Interbody Fusion: a finite element analysis. World Neurosurg.160, e126–e141 (2022). [DOI] [PubMed] [Google Scholar]
- 31.Dakwar, E., Cardona, R. F., Smith, D. A. & Uribe, J. S. Early outcomes and Safety of the minimally invasive, lateral retroperitoneal Transpsoas Approach for Adult degenerative scoliosis. NEUROSURG. FOCUS. 28, E8 (2010). [DOI] [PubMed] [Google Scholar]
- 32.McMains, M. C. et al. A biomechanical analysis of lateral interbody construct and supplemental fixation in adjacent-segment disease of the lumbar spine. World Neurosurg.128, e694–e699 (2019). [DOI] [PubMed] [Google Scholar]
- 33.DenHaese, R., Gandhi, A., Ferry, C., Farmer, S. & Porter, R. An in Vitro Biomechanical evaluation of a lateral lumbar Interbody Fusion device with Integrated lateral modular plate fixation. Glob Spine J.11, 351–358 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shasti, M. et al. Biomechanical evaluation of lumbar lateral Interbody Fusion for the treatment of adjacent segment disease. Spine J.19, 545–551 (2019). [DOI] [PubMed] [Google Scholar]
- 35.Liu, Z. X. et al. Effects of osteoporosis on the Biomechanics of various supplemental fixations co-applied with oblique lumbar Interbody Fusion (Olif): a finite element analysis. BMC Musculoskel Dis.23, 794 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Basra, S., Bucklen, B., Muzumdar, A., Khalil, S. & Gudipally, M. A. Novel lateral lumbar Integrated plate-spacer Interbody Implant: in Vitro Biomechanical Analysis. Spine j.15, 322–328 (2015). [DOI] [PubMed] [Google Scholar]
- 37.Nayak, A. N., Gutierrez, S., Billys, J. B., Santoni, B. G. & Castellvi, A. E. Biomechanics of lateral plate and pedicle screw constructs in lumbar spines instrumented at two levels with laterally placed interbody cages. Spine J.13, 1331–1338 (2013). [DOI] [PubMed] [Google Scholar]
- 38.Zhang, Y. et al. Finite element analysis of different locking plate fixation methods for the treatment of Ulnar Head Fracture. J. Orthop. Surg. Res.16, 191 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bozkus, H., Chamberlain, R. H., Perez, G. L., Crawford, N. R. & Dickman, C. A. Biomechanical Comparison of Anterolateral Plate, lateral plate, and pedicle screws-rods for enhancing anterolateral lumbar Interbody Cage stabilization. Spine29, 635–641 (2004). [DOI] [PubMed] [Google Scholar]
- 40.Goel, V. K. et al. Effects of Rigidity of an internal fixation device. A Comprehensive Biomechanical Investigation. Spine16, S155–S161 (1991). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.