Abstract
Objective
To understand the hospitalization expenditures and the composition of hospitalized patients with chronic obstructive pulmonary disease (COPD) in Yunnan Province from 2016 to 2022 and to identify the factors that influence them. The study aims to provide evidence-based information to health administration, hospitals, health insurance offices, and other related departments to help them formulate relevant policies.
Methods
This study analyzed data from 728,980 COPD patients in Yunnan Province between 2016 and 2022. This study described trends in hospitalization expenditures and their components over a 7-year period. Path analysis was used to investigate the factors that affect hospitalization expenditures.
Results
The average hospitalization expenditures for 2016–2022 were 7828 CNY. The total hospitalization expenditures were continuously increasing, from 828 million CNY to 967 million CNY, which is a 16.84% increase. However, the average expenditure per hospitalization decreased from 9185 CNY to 7261 CNY, which is a decrease of 20.95%. The main components of hospitalization expenditures were diagnostic fees, medication fees, and comprehensive medical service fees. The proportion of medication fees is decreasing, while the proportion of diagnostic fees and comprehensive medical services fees are increasing. The results of the path analysis indicate that age, gender, ethnicity, hospital level, admission route, medical payment method, COPD with acute lower respiratory tract infection, non-acute exacerbation of COPD, rehabilitation treatment experience, and comorbidity have both direct and indirect effects on hospitalization expenditures through length of stay (LOS). Additionally, marital status indirectly affects hospitalization expenditures through LOS.
Conclusion
Shortening the average LOS is crucial for hospitals to improve efficiency and reduce unnecessary expenses for patients. To achieve this, it is necessary to actively implement clinical pathway management and establish a standardized diagnosis and treatment system.
Keywords: COPD, Hospitalization expenditures, Influencing factors, Path analysis, China
Background
Chronic obstructive pulmonary disease (COPD) is a heterogeneous lung condition characterized by chronic respiratory symptoms such as dyspnea, cough, and sputum. It is associated with an abnormal inflammatory response of the lungs to harmful particles and gases [1]. COPD is a chronic disease that seriously impacts human health, with a high prevalence rate and a large population. Between 2012 and 2015, the China Pulmonary Health Study found that the prevalence rate of COPD among people aged 40 years and older was 13.7% and that there were close to 100 million COPD patients in China [2]. Similarly, from 2014 to 2016, the prevalence rate of COPD among residents of Yunnan Province aged 40 years and older was 11.3% [3].
Due to its high prevalence, long duration, and progressive nature, COPD imposes a heavy economic burden on families and society. In 2004, data from the United States estimated the total economic burden of COPD to be $23.9 billion per year, and it was expected that patients with COPD would have to pay about $1500 annually [4]. A study conducted in Singapore between 2005 and 2009 found that COPD patients had an average total annual medical cost of nearly US$9.9 million, of which hospitalization expenditures were as much as US$7.2 million [5]. In 2006, a study of 24 hospitals in China revealed that the direct medical expenditure per COPD patient was 11,744 CNY, with an additional per-patient indirect medical expenditure of 1,570 CNY. The total cost per patient with COPD accounted for 40% of the total household income [6]. Similarly, a cross-sectional study conducted in Beijing, Shanghai, Guangzhou, and Chengdu found that the average annual direct medical expenditure of patients was 11,968 CNY, with hospitalization expenditure being the primary source of direct costs, accounting for 65.9% [7]. These studies collectively suggest that COPD imposes a significant economic burden, with hospitalization expenses being the primary contributor.
COPD is associated with many comorbidities, including diabetes, cardiovascular disease, pulmonary artery disease, and malnutrition. However, COPD and its comorbidities combine to exacerbate the hospitalization expenditure for patients. The hospitalization expenditure for patients with comorbidities were 4.7 times higher than for patients without comorbidities [8]. As the disease progresses, the frequency of acute exacerbations rises. The occurrence of an acute exacerbation of COPD not only has a significant impact on the quality of life of the patient, but also increases the financial burden on the patient. Patients who experience three or more acute exacerbations have direct medical costs that are two times higher than patients who have never had an acute exacerbation [9]. The main factors affecting the hospitalization expenditure for COPD include disease severity, acute exacerbations and frequency, LOS, comorbidities, hospital grade, age, etc [10, 11].
Many of the existing studies on the influencing factors of hospitalization expenditures rely on regression analysis [12–16]. However, several studies have shown that LOS does not only directly affect hospitalization costs, but other factors can also indirectly affect hospitalization expenditures through LOS [17–19]. Regression models only show the direct effect of the independent variable on the dependent variable and do not reveal information about possible indirect effects. Path analysis can overcome this limitation. Therefore, in our study, researchable influencing factors were extracted based on the information on the first page of the hospitalization case, and using path analysis to investigate the direct and indirect factors affecting hospitalization expenditures and to reflect the interrelationships among independent, intermediate, and dependent variables by calculating the direct, indirect, and total effects of the independent variables on the dependent variable. In order to provide essential information and evidence-based support for the health administration, hospitals, health insurance, and other related departments to formulate relevant policies and make scientific decisions.
Methods
Data source and exclusion criteria
According to the diagnostic criteria for COPD in the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). The first page of the hospitalization cases of patients hospitalized with a primary diagnosis disease code of J44 in Yunnan Province from 2016 to 2022 was collected, totaling 843,688 cases. And according to the exclusion criteria: (1) exclude ICD-10 major diagnosis codes of J44.801-J44.807; (2) exclude patients with missing basic information; (3) exclude patients with missing information on hospitalization expenditures; (4) exclude hospitalization time less than 24 h; and (5) exclude patients with an age < 20 years(thresholds for age are based on a study of the prevalence of patients with COPD in China) [2]. A total of 728,980 cases were included in the study. For cases that experienced two or more hospitalizations, each hospitalization was studied as a separate case.
Measurement
The data for this study was mainly obtained from the first page of the hospitalization cases. The contents of the first page of the hospitalization cases were filled out in accordance with the norms issued by the National Health Commission of the People’s Republic of China ([2011] No.84) [20]. The first page of the hospitalization case includes information about the patient’s demographic characteristics, clinical characteristics, and hospitalization expenditures. Patient’s demographic and clinical characteristics information includes age, gender, ethnicity, marital status, hospital level, admission route, LOS, medical payment method, primary diagnosis, rehabilitation treatment experience, and comorbidity. Hospitalization expenditures include total expenditures and 6 categories of component expenditures. Operational definitions of hospitalizations expenditures are shown in Table 1.
Table 1.
Operational definitions of hospitalizations expenditures
| Variables | definition |
|---|---|
| Total hospitalization expenditures | Sum of all component expenditures |
| Comprehensive medical service fee | 1.General medical service fee: consultation fees, bed charges, consultation fees and nutritional counselling. |
| 2.General treatment operation fee: the costs of injections, debridement, dressing changes, catheterization, oxygen, resuscitation and intensive care. | |
| 3.Nursing care fee: costs of hierarchical care and specialized care during the patient’s hospital stay. | |
| 4.Other fee: the costs of ward heating, ward air-conditioning, ambulance use, etc. | |
| Diagnostic fee | 1.Pathological diagnosis fee: pathology-related examination programme costs. |
| 2.Laboratory diagnosis fee: laboratory testing costs. | |
| 3.Imaging diagnosis fee: fees for imaging tests such as fluoroscopy, angiography, CT, MRI, ultrasound, nuclear scanning, PET, etc. | |
| 4.Clinical diagnosis item fee: the costs of various other tests carried out by clinical departments for diagnostic purposes. | |
| Treatment fee | 1.Treatment fee: costs incurred for items treated clinically using non-invasive and invasive means. |
| 2.Traditional Chinese medical treatment fee: the costs arising from treatment using Chinese medicine. | |
| Rehabilitation fee | Costs incurred for the rehabilitation of patients, including rehabilitation assessment and treatment. |
| Medication fee | 1.Chinese medication fee: the costs of proprietary Chinese medicines and herbal medicines. |
| 2.Western medicines fee: the costs of organic chemical drugs, inorganic chemical drugs and biological products. | |
| Other fee | 1.Blood and blood products fee: costs incurred for clinical use of blood. |
| 2.Consumables fee: consumables that are allowed to be charged separately by the local health and price management authorities. | |
| 3.Other fee: sum of costs not attributable to the above categories during the patient’s stay in the hospital. |
Statistical methods
For quantitative data, information conforming to normal distribution was expressed as  , and the number of non-normally distributed data was expressed as M(P25,P75); for categorical variables, we described them using the percentages (%). The Mann-Whitney U test and the Kruskal-Wallis H test were used for the analysis of variance. Path diagrams were constructed based on multiple linear regression equations. The statistically significant variables in the multiple linear regression analysis were used as independent variables, and the total cost of hospitalization and LOS were used as dependent variables. And the direct effect, indirect effect, and total effect of the independent variables on the dependent variables were calculated. A probability value of P < 0.05 was considered statistically significant in multiple linear regression. We did all data analyses with SPSS (version 26.0; International Business Machines Corporation, USA) and AMOS (version 24.0 International Business Machines Corporation, USA).
, and the number of non-normally distributed data was expressed as M(P25,P75); for categorical variables, we described them using the percentages (%). The Mann-Whitney U test and the Kruskal-Wallis H test were used for the analysis of variance. Path diagrams were constructed based on multiple linear regression equations. The statistically significant variables in the multiple linear regression analysis were used as independent variables, and the total cost of hospitalization and LOS were used as dependent variables. And the direct effect, indirect effect, and total effect of the independent variables on the dependent variables were calculated. A probability value of P < 0.05 was considered statistically significant in multiple linear regression. We did all data analyses with SPSS (version 26.0; International Business Machines Corporation, USA) and AMOS (version 24.0 International Business Machines Corporation, USA).
Results
Demographic and clinical characteristics of COPD cases
A total of 728,980 cases were included in the study. There were 531,924 cases (72.97%) of males and 197,056 cases (27.03%) of females; the average age of the patients was 72.18 ± 10.93 years old, and there were 450,171 cases (61.75%) of patients ≥ 70 years old; there were 617,672 cases (84.73%) of Han nationality, and there were 111,308 cases (15.27%) of other ethnic minorities; there were 639,156 cases (87.68%) of patients who were in marriage, and there were 89,824 cases (12.32%) who were not in marriage; the main diagnosis of COPD with acute exacerbation was 392,337 cases (53.82%), and COPD with acute lower respiratory tract infection (ARTI) was 269,039 cases (36.91%), and non-acute exacerbation of COPD was 67,604 cases (9.27%); and the number of patients who admitted to a tertiary hospital was 232,308 cases (31.90%), 496,672 cases (68.10%) in secondary hospitals; 118,422 cases (16.24%) of patients were admitted as emergencies, and 610,558 cases (83.76%) were admitted as non-emergencies; 76.64% of the patients’ LOS ranged from 6 to 14 days; there were 639,985 cases (87.79%) paid by medical insurance and 88,995 cases (12.21%) paid by non-medical insurance; 664,174 cases (91.11%) did not undergo rehabilitation treatment, and 64,806 cases (8.89%) did undergo rehabilitation treatment; 97.41% of the patients had comorbidity (Table 3).
Table 3.
Univariate analysis of hospitalization expenditures, 2016–2022
| Factors | N | % | hospitalization expenditures | P-Value | |
|---|---|---|---|---|---|
| M | (P25,P75) | ||||
| Gender | <0.001 | ||||
| Male | 531,924 | 72.97 | 6494 | (4506, 9975) | |
| Female | 197,056 | 27.03 | 5817 | (4131, 8612) | |
| Age | <0.001 | ||||
| 20–39 | 2877 | 0.39 | 5072 | (3379, 7854) | |
| 40–49 | 17,516 | 2.40 | 5230 | (3624, 7875) | |
| 50–59 | 74,935 | 10.28 | 5511 | (3893, 8179) | |
| 60–69 | 183,481 | 25.17 | 5835 | (4149, 8647) | |
| ≥ 70 | 450,171 | 61.75 | 6710 | (4662, 10368) | |
| Ethnicity | <0.001 | ||||
| Han nationality | 617,672 | 84.73 | 6371 | (4411, 9814) | |
| Other ethnic minorities | 111,308 | 15.27 | 5947 | (4306, 8546) | |
| Marital status | <0.001 | ||||
| Married | 639,156 | 87.68 | 6225 | (4356, 9445) | |
| Unmarried* | 89,824 | 12.32 | 6887 | (4706, 10767) | |
| Hospital level | <0.001 | ||||
| Tertiary hospital | 232,308 | 31.90 | 10,301 | (7473, 14495) | |
| Secondary Hospital | 496,672 | 68.10 | 4999 | (3669, 6764) | |
| Admission route | <0.001 | ||||
| Emergency | 118,422 | 16.24 | 7293 | (4820, 11554) | |
| Non-emergency* | 610,558 | 83.76 | 6135 | (4321, 9219.) | |
| Length of stay | <0.001 | ||||
| ≤ 5 | 80,934 | 11.1 | 3494 | (2578, 4838) | |
| 6–14 | 558,705 | 76.64 | 6160 | (4523, 8767) | |
| 15–23 | 74,123 | 10.17 | 12,752 | (8947, 18128) | |
| ≥ 24 | 15,218 | 2.09 | 21,260 | (14080, 32362) | |
| Medical payment method | <0.001 | ||||
| Medical insurance* | 639,985 | 87.79 | 6305 | (4417, 9586) | |
| Non-medical insurance* | 88,995 | 12.21 | 6235 | (4197, 9655) | |
| Primary diagnosis | <0.001 | ||||
| COPD with acute lower respiratory tract infection | 269,039 | 36.91 | 6927 | (4837, 10502) | |
| COPD with acute exacerbation | 392,337 | 53.82 | 5973 | (4188, 9110) | |
| non-acute exacerbation of COPD * | 67,604 | 9.27 | 5642 | (3967, 8456) | |
| Rehabilitation treatment experience | <0.001 | ||||
| Yes | 664,174 | 91.11 | 6229 | (4371, 9425) | |
| No | 64,806 | 8.89 | 7126 | (4655, 11215) | |
| Comorbidity | <0.001 | ||||
| Yes | 710,128 | 97.41 | 6172 | (4286, 9394) | |
| No | 18,852 | 2.59 | 3218 | (2186, 4653) | |
*Ps: “Unmarried” includes: Unmarried, Widowed, Divorced, Other; “Non-emergency” includes: Outpatient, Transferred from other medical institutions, Other; “Medical insurance” includes: urban workers’ basic medical insurance, urban residents’ basic medical insurance, new rural cooperative medical insurance, commercial medical insurance, full public payment, and other social insurance; “Non-medical insurance” includes: indigent assistance, full out-of-pocket payment, and other payment; “non-acute exacerbation of COPD” includes: J44.800, J44.900, J44.900 × 002, J44.900 × 003, J44.900 × 004, and J44.900 × 005
Hospitalization expenditures of COPD cases
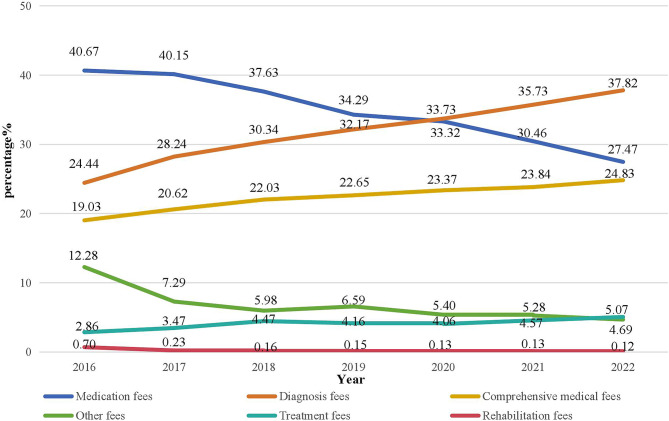
As shown in Table 2, the number of patients continued to rise from 2016 to 2022, with the highest hospitalization expenditure reaching 427,103 CNY, while the lowest hospitalization expenditures were 50 CNY. The average patient hospitalization expenditure was 7,828 CNY, with a median of 6,086 (4,203, 9,282) CNY. The total hospitalization expenditures were continuously increasing, from 828 million CNY to 967 million CNY, which is a 16.84% increase. However, the average expenditure per hospitalization decreased from 9,185CNY to 7,261CNY, which is a decrease of 20.95%. The main components of hospitalization expenditures were diagnostic fees, medication fees, and comprehensive medical service fees. The proportion of diagnostic fees increased from 24.44 to 37.82%; the proportion of medication fees decreased from 40.67 to 27.47%; the proportion of comprehensive medical service fees increased from 19.03 to 24.83%; the proportion of treatment fees increased from 2.86 to 5.07%; the proportion of other fees decreased from 12.28 to 4.69%; and the proportion of rehabilitation fees decreased from 0.70 to 0.12% (Fig. 1). The test for trend was performed with a polynominal contrast procedure, revealing statistically significant differences between years in diagnostic fees, medication fees, comprehensive medical service fees, treatment fees, rehabilitation fees, other fees (p < 0.001).
Table 2.
Growth rate of hospitalization expenditures for patients with COPD, 2016–2022
| Year | N | Total hospitalization expenditure (million) | Growth rate of a fixed base(%) | Chain growth rate(%) | the average per hospitalization expenditure | Growth rate of a fixed base(%) | Chain growth rate(%) |
|---|---|---|---|---|---|---|---|
| 2016 | 90,129 | 828 | - | - | 9185 | - | - |
| 2017 | 89,471 | 799 | -3.54 | -3.54 | 8924 | -2.84 | -2.84 |
| 2018 | 83,748 | 769 | -7.1 | -3.68 | 9183 | -0.02 | 2.9 |
| 2019 | 106,082 | 867 | 4.74 | 12.74 | 8174 | -11.01 | -10.99 |
| 2020 | 106,221 | 839 | 1.31 | -3.28 | 7895 | -14.04 | -3.41 |
| 2021 | 120,122 | 922 | 11.42 | 9.98 | 7678 | -16.4 | -2.75 |
| 2022 | 133,207 | 967 | 16.84 | 4.86 | 7261 | -20.95 | -5.44 |
Hospitalization expenditures were calculated using 2022 as the base year after discounting using the consumer price index of Yunnan Province. The Table 1 shows the costs after discounting
Fig. 1.
Hospitalization expenditures components and trends for COPD, 2016–2022
Univariate analysis
The Mann-Whitney U test and Kruskal-Wallis test show that age, gender, ethnicity, marital status, hospital level, admission route, LOS, medical payment method, primary diagnosis, rehabilitation treatment experience, and comorbidity were statistically associated with hospitalization expenditures (P < 0.001). Furthermore, differences were statistically significant in both two-by-two comparisons of age and primary diagnosis groups (P < 0.001), as shown in Table 3. From the results of the univariate analysis alone, hospitalization expenditures were higher for patients who were male, Han nationality, unmarried, admitted to a tertiary hospital, admitted in an emergency, paid by medical insurance, had rehabilitation experience, and had comorbidities. In addition with age, LOS, and severity of disease, patients’ hospitalization expenditures increased.
Path analysis
Model construction and fitting
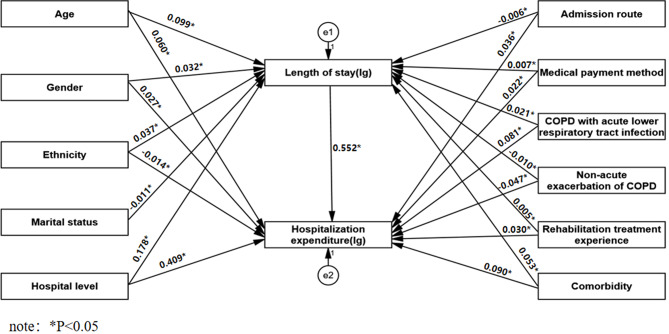
The data on LOS and hospitalization expenditures exhibit a skewed distribution. To address this, we log-transformed the dependent variables, Y1 = lg(LOS), Y2 = lg (hospitalization expenditure). Age (X1), gender(X2), ethnicity(X3), marital status(X4), hospital level(X5), admission route(X6), medical payment method(X7), COPD with acute lower respiratory tract infection(X8), non-acute exacerbation of COPD(X9), rehabilitation treatment experience(X10), and comorbidity(X11) as 11 independent variables. The results of the multiple linear regression analysis model for Y1 showed F = 4059.887, R2 = 0.058, p < 0.001, and the results of the multiple linear regression model for Y2 showed F = 117182.017, R2 = 0.639, p < 0.001.
The path analysis model consisted of the following two regression equations:
 |
The pathway model was constructed. The single arrow in Fig. 2 represents a single effect, or causality. And the parameter estimation of the model was carried out by maximum likelihood method to obtain the path coefficients between the variables.
Fig. 2.
Path diagram of factors affecting hospitalization expenditures
The results showed that = 0.044, P = 0.835 > 0.05, which indicated that the S matrix of the sample data and the matrix of the hypothetical model can be fit. The proposed causal model for hospitalization expenditures of COPD was supported by the survey data. Model fitting showed that the influences of age, gender, ethnicity, hospital level, admission route, medical payment method, COPD with acute lower respiratory tract infection, non-acute exacerbation of COPD, rehabilitation treatment experience, and comorbidity not only had direct effects but also indirectly affected hospitalization expenditures through LOS, while marital status indirectly affected hospitalization expenditures through LOS. The total effects on hospitalization expenditures for patients with COPD, in descending order, were: LOS, hospital level, comorbidity, age, COPD with acute lower respiratory tract infection, gender, rehabilitation treatment experience, admission route, medical payment method, ethnicity, marital status, and non-acute exacerbation of COPD, as shown in Table 4.
Table 4.
Direct effect, indirect effect and total effect of influencing factors
| Variable | direct effect | indirect effect | total effect | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| →HP | →LOS→HP | →HP+ ( →LOS→HP ) | |||||||||
| path coefficient | 95% CI | % | path coefficient | 95% CI | % | path coefficient | 95% CI | ||||
| LOS | 0.552 | 0.550 | 0.553 | 100.00 | - | - | - | 0.552 | 0.550 | 0.553 | |
|
Hospital level (Ref: secondary hospitals) |
0.409 | 0.408 | 0.410 | 80.67 | 0.098 | 0.097 | 0.100 | 19.33 | 0.507 | 0.506 | 0.509 |
|
Comorbidity (Ref: no) |
0.090 | 0.089 | 0.092 | 75.63 | 0.029 | 0.028 | 0.030 | 24.37 | 0.119 | 0.117 | 0.121 |
| Age | 0.060 | 0.059 | 0.062 | 52.17 | 0.055 | 0.054 | 0.056 | 47.83 | 0.115 | 0.113 | 0.117 |
| COPD with acute lower respiratory tract infection | 0.081 | 0.080 | 0.082 | 87.10 | 0.012 | 0.011 | 0.013 | 12.90 | 0.093 | 0.091 | 0.095 |
|
Gender (Ref: female) |
0.027 | 0.026 | 0.028 | 60.00 | 0.018 | 0.016 | 0.019 | 40.00 | 0.045 | 0.043 | 0.046 |
|
Rehabilitation treatment experience (Ref: no) |
0.030 | 0.029 | 0.031 | 90.91 | 0.003 | 0.001 | 0.004 | 9.09 | 0.033 | 0.031 | 0.035 |
|
Admission route (Ref: Non-emergency) |
0.036 | 0.034 | 0.037 | 109.09 | -0.003 | -0.005 | -0.002 | -9.09 | 0.033 | 0.031 | 0.034 |
|
Medical payment method (Ref: Non-medical insurance) |
0.022 | 0.020 | 0.023 | 84.62 | 0.004 | 0.003 | 0.005 | 15.38 | 0.026 | 0.024 | 0.028 |
|
Ethnicity (Ref: other ethnic minorities) |
-0.014 | -0.016 | -0.013 | -233.33 | 0.020 | 0.019 | 0.021 | 333.33 | 0.006 | 0.004 | 0.008 |
|
Marital status (Ref: Unmarried) |
- | - | - | -0.006 | -0.008 | -0.005 | 100.00 | -0.006 | -0.008 | -0.005 | |
| Non-acute exacerbation of COPD | -0.047 | -0.049 | -0.045 | 88.68 | -0.006 | -0.007 | -0.004 | 11.32 | -0.053 | -0.055 | -0.050 |
HP hospitalization expenditure, LOS length of stay, CI confidence interval
Model evaluations
After the model is fitted, the goodness of fit of the model is demonstrated through metrics that reflect the effectiveness of the fit. The CMIN/DF = 0.044, RMR = 0.000, RMSEA = 0.000, GFI = 1.000, CFI = 1.000, AGFI = 1, IFI = 1, NFI = 1, and TLI = 1 metrics of this model show that the model fits well, and all of them are in line with the values of the reference standard.
Discussion
In this study, we assessed COPD hospitalization expenditures and their components in Yunnan province, China, and examined the factors associated with COPD hospitalization expenditures. The results of our study showed an average expenditure per hospitalization of 7,828 CNY with a decreasing trend. The main finding of the study was LOS. The influencing factors of age, gender, ethnicity, hospital level, admission route, medical payment method, COPD with acute lower respiratory tract infection, non-acute exacerbation of COPD, rehabilitation treatment experience, and comorbidity not only had direct effects but also indirectly affected hospitalization expenditures through LOS. Marital status had an indirect effect on hospitalization expenditures through LOS. The findings of our research can be used as a point of comparison with the results of similar studies conducted in other countries and regions of China.
In this study, the total hospitalization expenditures were continuously increasing, from 828 million CNY to 967 million CNY, which is a 16.84% increase, as well as the number of patients increased from 90,129 to 133,207, an increase of 47.80%. However, the average expenditure per hospitalization decreased from 9,185CNY to 7,261CNY, which is a decrease of 20.95%. When the number of patient cases increases, healthcare organizations can better use resources and more fully utilize shared infrastructure such as operating rooms, testing rooms, and equipment. The cost of the facilities required per patient can be spread over more patients, thus lowering the average expenditure per hospitalization.
In terms of the composition of hospitalization expenditures, the study found that medication fees, diagnosis fees, and comprehensive medical service fees were the main components of hospitalization expenditures, and these three types of fees accounted for more than 80% of the total expenditures of patients with COPD, which is consistent with the results of other study [21]. The trend of medication fees is decreasing. In 2019, with the issuance of the Pilot Program for Centralized Purchasing of Medicines by State Organizations, centralized purchasing of medicines has been upgraded to a national strategy, the core purpose of which is to reduce the price of medicines by means of centralized procurement, to reduce intermediate links, and to improve the efficiency and quality of the supply of medicines, so as to alleviate the financial burden on patients [22]. The fees for diagnostic and comprehensive medical services have increased, possibly due to the nationwide implementation of the zero-plus-fee policy for medication. This policy is an important measure to separate medical treatment from medication, and lowering the fees for medication will make it possible to adjust other costs [23, 24]. Currently, it is emphasized to increase the value of medical workers’ labor. By giving reasonable compensation to medical staff, it can reduce the unnecessary medical behaviors they take to increase their income, thus reducing the medical costs of patients [25].
The key to rationally controlling hospitalization expenditures is to identify the factors affecting hospitalization expenditures. We used path analysis to found that LOS is both an independent variable and an intermediate variable affecting hospitalization expenditures, which is consistent with the results of other studies [26–28]. The LOS is an important indicator that can directly reflect the efficiency of hospital management, diagnostic and treatment techniques, and the effectiveness of medical service work [29]. The average LOS for patients with COPD was 7–9 days in Asia, 3–5 days in the USA and European [30], and LOS in our study was mainly concentrated on 6–14 days. The results of the path analysis showed that the total effect of LOS (0.522) ranked first among all factors. LOS was the main factor affecting hospitalization expenditures. Some studies have confirmed that there was a positive correlation between hospitalization expenditures and LOS in patients with COPD. As the LOS increased, the hospitalization expenditure also increased, which is consistent with the results of other studies [31, 32]. The path analysis found that other factors affect hospitalization expenditures directly and also indirectly through LOS.
The first is the patient’s demographic sociological factors, including: age, gender, ethnicity and marital status. In this study, it was found that age had a direct effect of 0.060 (52.17%) and an indirect effect of 0.055 (47.83%). Although this an uncontrollable factor, it is one of the important factors that affect hospitalization expenditures. As patients age, their physical and immune system functions decline, which may exacerbate symptoms. The likelihood of repeat admissions is relatively high [33, 34]. Therefore, the treatment time for elderly patients is prolonged, leading to an increase in hospitalization expenditures. A study in Henan Province, China also suggests that special attention should be paid to the elderly population with COPD [35]. Gender and ethnicity were small influencing factors on hospitalization expenditures, with total effects of 0.045 and 0.006, respectively. Among them, male patients’ hospitalization expenditures were significantly higher than those of females, and the hospitalization expenditures of Han nationality patients were higher than those of other ethnic minorities, which is consistent with the results of other studies [16, 36]. In other scholars’ studies [37], marital status was excluded from the regression equation fitting process. However, this study found that although marital status has no direct effect on hospitalization expenditures, there is still an indirect effect(-0.006). Married patients have lower hospitalization expenditures than unmarried patients. Married patients often have access to support from their spouses, family members, and close friends. This support can improve the effectiveness of treatment, provide better care and supervision, and facilitate the timely detection of changes in the patient’s symptoms, resulting in shorter hospital stays and reduced hospitalization expenditures [38].
Having analyzed the impact of demographic and sociological factors on hospitalization expenditures, we further explored how patient healthcare characteristics and behaviors influence hospitalization expenditures. Factors reflecting patients’ healthcare characteristics and behaviors, including hospital level, acute exacerbations, comorbidities, rehabilitation experience, admission route, and medical payment method. The results of the path analysis showed that the total effect of hospital level was 0.507, the direct effect was 0.409(80.67%), and the indirect effect was 0.098(19.33%). The direct effect of hospital level on hospitalization expenditure was found to be more significant. There are notable discrepancies in the level of medical services provided by hospitals of varying grades, and hospitalization expenditures may also vary. Hospitals of a higher grade typically possess more sophisticated medical technology and a more specialized medical workforce, enabling them to offer a greater range of complex and specialized medical services. These factors may contribute to higher costs. As a result, hospitalization expenditures are higher in the tertiary hospitals than in the secondary hospitals. In addition, patients in higher level hospitals usually have more severe and complex conditions that require more advanced treatment, resulting in a longer LOS and higher hospitalization expenses, which is consistent with the results of other study [39]. Clinical pathway is an advanced medical quality management model. It has obvious effects on reducing the average LOS, increasing the number of bed turnovers, reducing the average hospitalization expenditures, standardizing diagnostic and therapeutic behaviors, and improving the economic and social benefits of hospitals [40, 41]. Hospitals should implement clinical pathway management to improve the efficiency of healthcare services and reduce unnecessary LOS.
Acute exacerbation of COPD and comorbidities are also important factors affecting hospitalization expenditures. Patients with both of these conditions had relatively high hospitalization expenditures. They require additional treatment and care, such as medications, oxygen therapy, and physical therapy. The longer the duration of these treatment measures, the related expenditure will increase [42]. Some studies have shown that increasing the frequency of acute exacerbations from 1 per year to 2 or more per year will triple the cost of medication for the patient [43]. COPD and its comorbidities combine to exacerbate the hospitalization expenditure for patients. An Italian study noted a significant association between comorbidities and hospitalization days and hospitalization expenditures, particularly among patients with cardiovascular disease or diabetes, who had the longest LOS and highest hospitalization expenditures [44]. In the management of comorbidities in patients with COPD, early detection of comorbidities in patients with COPD is achieved through regular health screening and assessment. Regular monitoring and follow-up are also used to make timely adjustments to the treatment regimen to control the disease and reduce the risk of acute exacerbations. Hospital level, acute exacerbation and comorbidities are the main factors affecting hospitalization expenditures. In addition to this, rehabilitation experience, admission route, and healthcare payment method also affect hospitalization expenditures, but the total effect is small, which is consistent with the results of other studies [27, 45].
This study has the following limitation. Firstly, the first page of the hospitalization case is an important carrier of medical information reflecting the patient’s hospitalization, medical services, and related expenditures. However, this data does not contain information on individual characteristics and lifestyles, and exploration of the factors affecting hospitalization expenditures is limited. Secondly, in accordance with the principles of ethical review, personal information such as patients’ names, ID cards, home addresses and telephone numbers could not be obtained for this study. Consequently, it was not possible to identify repeat admissions. For cases undergoing two or more hospitalizations, each hospitalization was studied as a separate case, which may have led to an underestimation. Thirdly, Although this study collected data from 2016 to 2022, the study is still essentially a cross-sectional study, and the results can only explain the factors influencing costs, not the underlying reasons for the observed cost increases.
Conclusion
COPD continues to carry a heavy disease burden in Yunnan Province. In order to effectively reduce patients’ disease burden, we need to have a deep understanding and pay attention to the factors that lead to an increase in hospitalization expenditures. Admission to tertiary hospitals, acute exacerbations, and comorbidities were the main influences on hospitalization expenditures. In addition, we should focus on specific groups, such as men, older patients, Han nationality, and unmarried groups. The most meaningful finding of this study is LOS, as a key intermediate variable, plays a dual role in influencing hospitalization expenditures. Therefore, shortening the average LOS remains an important goal for hospitals to improve efficiency and reduce unnecessary expenditures for patients.
Acknowledgements
We would like to thank all participants of the Strategic Research and Consulting Project of” Comprehensive Prevention and Control of Chronic Obstructive Pulmonary Disease in Yunnan Province based on Population Medical Model” of Chinese Academy of Engineering and thank for their efforts in collecting data on the first page of the hospitalization cases of patients with COPD from 2016 to 2022.
Authors’ contributions
All authors critically reviewed and contributed to the intellectual content of the manuscript. SYT and YHZ conceived and designed the study. GYW, WLC, AHW, JLM and GHL collected and cleaned up the data. AHW, JLM and GHL analyzed the data and wrote the manuscript. SYT and YHZ revised the manuscript. The first three authors AHW, JLM and GHL contributed equally to this paper and should be regarded as co-first authors. All authors read and approved this manuscript before submission to this journal.
Funding
This study was funded by the Strategic Research and Consulting Project of” Comprehensive Prevention and Control of Chronic Obstructive Pulmonary Disease in Yunnan Province based on Population Medical Model” of Chinese Academy of Engineering(NO.2022-DFZD-30) and Union Specific Project Foundation of Yunnan Provincial Science and Technology Department and Kunming Medical University (202301AY070001-073).
Data availability
Data generated and/or analyzed during the study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was initiated and led by the First People’s Hospital of Yunnan Province and was approved by the Ethics Committee of the First People’s Hospital of Yunnan Province (KHLL2022-KY141-C-1). Written informed consent has been obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aihan Wen, Jinliang Meng and Guohong Luo contributed equally as joint first authors.
Contributor Information
Songyuan Tang, Email: tsythailand@hotmail.com.
Yunhui Zhang, Email: yunhuizhang3188@126.com.
References
- 1.Àlvar Agustí BartoloméR, Celli GJ, Criner, et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Am J Respir Crit Care Med. 2023;207(7):819–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–17. [DOI] [PubMed] [Google Scholar]
- 3.Shan Y, Yang Y, Qin M, et al. Analysis of the prevalence and influencing factors of chronic obstructive pulmonary disease among residents aged 40 years and above in Yunnan Province. Mod Prev Med. 2018;45(20):3654–8. [Google Scholar]
- 4.Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004;364(9434):613–20. [DOI] [PubMed] [Google Scholar]
- 5.Teo WS, Tan WS, Chong WF, et al. Economic burden of chronic obstructive pulmonary disease. Respirology. 2012;17(1):120–6. [DOI] [PubMed] [Google Scholar]
- 6.He Q, Zhou X, Xie C, et al. Impact of chronic obstructive pulmonary disease on the quality of life and economic burden of patients in selected Chinese cities. Chin J Tuberculosis Respiratory Med. 2009;32(4):253–7. [PubMed] [Google Scholar]
- 7.Chen X, Wang N, Chen Y, et al. Costs of chronic obstructive pulmonary disease in urban areas of China: a cross-sectional study in four cities. Int J Chronic Obstr Pulm Dis. 2016;11:2625–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mapel DW, Hurley JS, Frost FJ, et al. Health care utilization in chronic obstructive pulmonary disease. A case-control study in a health maintenance organization. Arch Intern Med. 2000;160(17):2653–8. [DOI] [PubMed] [Google Scholar]
- 9.Amol D, Dhamane C, Moretz Y, Zhou, et al. COPD exacerbation frequency and its association with health care resource utilization and costs. Int J Chronic Obstr Pulm Dis. 2015;0(0):2609–2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li M, Wang F, Chen R, et al. Factors contributing to hospitalization costs for patients with COPD in China: a retrospective analysis of medical record data. Int J Chronic Obstr Pulm Dis. 2018;13(0):3349–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petra Menn J, Heinrich RM, Huber, et al. Direct medical costs of COPD – an excess cost approach based on two population-based studies. Respir Med. 2012;106(4):540–8. [DOI] [PubMed] [Google Scholar]
- 12.Zafari Z, Li S, Eakin MN, et al. Projecting Long-Term Health and Economic Burden of COPD in the United States. Chest. 2021;159(4):1400–10. [DOI] [PubMed] [Google Scholar]
- 13.Koul PA, Nowshehr AA, Khan UH, Jan RA, Shah SU. Cost of severe chronic obstructive pulmonary disease exacerbations in a high Burden Region in North India. Ann Glob Health. 2019;85(1):13. 10.5334/aogh.2423. [DOI] [PMC free article] [PubMed]
- 14.Agboado G, Peters J, Donkin L. Factors influencing the length of hospital stay among patients resident in Blackpool admitted with COPD: a cross-sectional study. Bmj Open. 2012;2(5):231–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang J. Analysis of factors affecting the direct economic burden of patients hospitalized with chronic obstructive pulmonary disease in a tertiary hospital in Beijing. Med Soc. 2015;28(07):19–22. [Google Scholar]
- 16.Hua G, Fang H, Ming Q. Analysis of factors affecting hospitalization expenditures of 257134 patients with chronic obstructive pulmonary disease in Yunnan Province in 2019[J]. Appl Prev Med. 2021;27(06):514–6. [Google Scholar]
- 17.Rosarin Sruamsiri H, Kubo Jörg. Hospitalization costs and length of stay of Japanese children with respiratory syncytial virus. Medicine. 2018;97(29):e11491-11491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ting W, Li Y, Qian L, et al. Analysis of factors affecting hospitalization costs for lung cancer surgery patients based on structural equation modeling. Chin Health Econ. 2019;38(06):61–3. [Google Scholar]
- 19.Xiao Y, Yuan D, Yue L, et al. Analysis of factors influencing hospitalization costs of cirrhotic patients based on structural equation modeling. Chin Med Records. 2023;24(06):87–90. [Google Scholar]
- 20.Notice of the Ministry of Health on the revision of the first page of the hospitalization cases. National Health Commission of the People’s Republic of China. 2011. http://www.nhc.gov.cn/wjw/gfxwj/201304/47b4226ff93c4800bab61c045ddb6642.shtml. Accessed 16 Sep 2024.
- 21.Yin PWJ, Wang L, et al. The Burden of COPD in China and its provinces: findings from the global burden of Disease Study 2019. Front Public Health. 2022;10:859499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin J. Analysis of patients’ sub-average hospitalization costs in tertiary public hospitals based on the degree of structural change. China Hosp Stat. 2023;30(01):55–8. [Google Scholar]
- 23.Huang X, Li Y, Yang Y. Study on the evaluation of cost control effect of relevant Medical Reform policies–based on Zero Markup on drugs, Zero Markup on Consumables, and Value-based payment for medical cases. Health Econ Res. 2023;40(02):69–73. [Google Scholar]
- 24.Liu W, Hsu CH, Liu T, et al. Systematic review of the Effect of a zero-markup policy for essential drugs on Healthcare costs and utilization in China, 2015–2021. Front Med (Lausanne). 2021;8–618046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liang J. Study on the influencing factors of medical costs of patients hospitalized with chronic obstructive pulmonary disease in a tertiary hospital in Guizhou Province. Guizhou University; 2023. [Google Scholar]
- 26.Ren M. Research on the analysis of influencing factors of hospitalization cost of participating farmers based on recursive system model and structural equation model. Guangxi Medical University; 2012. [Google Scholar]
- 27.Shan H, Yu J, Han X, et al. Analysis of recursive system and structural equation modeling of factors influencing hospitalization costs for patients with chronic obstructive pulmonary disease[J]. J Community Med. 2018;16(14):1138–45. [Google Scholar]
- 28.Wang T, Yu L, Lang Q, et al. Analysis of factors affecting hospitalization costs of lung cancer surgery patients based on structural equation modeling. China Health Econ. 2019;38(06):61–3. [Google Scholar]
- 29.Scott D, Ramsey, Richard Hobbs. Chronic obstructive Pulmonary Disease, Risk factors, and outcome trials: comparisons with Cardiovascular Disease. Annals Am Thorac Soc. 2006;3(7):635–40. [DOI] [PubMed] [Google Scholar]
- 30.Rehman AU, Hassali MA, Muhammad SA, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in the USA, Europe, and Asia: results from a systematic review of the literature. Expert Rev PharmacoEcon Outcomes Res. 2019;20(6):661–72. [DOI] [PubMed] [Google Scholar]
- 31.Ruparel M, López-Campos JL, Castro-Acosta A, Hartl S, Pozo-Rodriguez F, Roberts CM. Understanding variation in length of hospital stay for COPD exacerbation: European COPD audit. ERJ Open Res. 2016;2(1):00034-2015. [DOI] [PMC free article] [PubMed]
- 32.Rehman AU, Hassali MAA, Muhammad SA, et al. The economic burden of chronic obstructive pulmonary disease (COPD) in Europe: results from a systematic review of the literature. Eur J Health Econ. 2020;21(2):181–94. [DOI] [PubMed] [Google Scholar]
- 33.Stefan MS, Pekow PS, Priya A, et al. Association between Initiation of Pulmonary Rehabilitation and Rehospitalizations in patients hospitalized with chronic obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2021;204(9):1015–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164. [DOI] [PubMed]
- 35.Yu C, Xia Q, Li Q, et al. Hospitalization costs of COPD cases and its associated factors: an observational study at two large public tertiary hospitals in Henan Province, China. BMC Geriatr. 2023;23(1):457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao H, Bai Y, Li M, et al. Hospitalization status and direct economic burden of chronic obstructive pulmonary disease in the elderly. Chin J Gerontol. 2016;36(05):1196–8. [Google Scholar]
- 37.Jianping R, Hua L, Zhengzhong M, Zhengmin Y, Zhicheng D, Yurun Z, et al. Study on the economic burden of chronic obstructive pulmonary disease and its influencing factors. Health Econ Res. 2002(10):16–7. 10.14055/j.cnki.33-1056/f.2002.10.005.
- 38.Wang H, Zeng Y, Lian G, et al. Survey on the Impact of Family Support on Quality of Life and Medical Assistance for the Elderly. J Nanjing Med Univ (Social Sci Edition). 2020;20(06):559–63. [Google Scholar]
- 39.Feng Q, Yan C. Analysis of factors affecting hospitalization costs of patients with chronic obstructive pulmonary disease in Hunan Province. J Hunan Univ Traditional Chin Med. 2023;43(04):740–6. [Google Scholar]
- 40.Agus Kosasih. Implementation of clinical pathway for management of Copd Exacerbation. Respiratory Sci. 2021;1(3):166–73. [Google Scholar]
- 41.Bán A, Aniza Ismail R, Harun, et al. Impact of clinical pathway on clinical outcomes in the management of COPD exacerbation. BMC Pulm Med. 2012;12(1):0–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu Y, Liu W, Jiang HL, et al. Pneumonia is Associated with increased mortality in hospitalized COPD patients: a systematic review and Meta-analysis. Respiration. 2021;100(1):64–76. [DOI] [PubMed] [Google Scholar]
- 43.Anand A, Dalal L, Christensen F, Liu, et al. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chronic Obstr Pulm Dis. 2010;0(0):341–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Terzano C, Colamesta V, Unim B, Romani S, Meneghini A, Volpe G, et al. Chronic obstructive pulmonary disease (COPD) exacerbation: impact of comorbidities on length and costs during hospitalization. Eur Rev Med Pharmacol Sci. 2017;21(16):3680–9. [PubMed]
- 45.Jia L, Gui L, Juan H, et al. Passage analysis of factors affecting hospitalization expenditures in patients with chronic obstructive pulmonary disease. Mod Prev Med. 2022;49(04):605–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data generated and/or analyzed during the study are available from the corresponding author on reasonable request.