Abstract
Background
Corneal subepithelial infiltrates (SEIs) are characteristic clinical findings of adenoviral keratoconjunctivitis (AKC). In eyes with SEIs, both corneal opacity and irregular astigmatism may interfere with vision. However, irregular astigmatism is often overlooked in patients with AKC. Here, we report a case of decreased vision due to irregular corneal surfaces detected by Placido ring mires in eyes with corneal SEIs after AKC.
Case presentation
: An 8-year-old girl with decreased vision was referred to our clinic. She had been diagnosed with AKC two years prior by a different physician. Thereafter, she experienced recurring episodes of decreased vision, epiphora, and photophobia in both eyes. The symptoms persisted despite resolution of the corneal opacity with steroid eye drops. Despite mild corneal opacity, both eyes exhibited distorted Placido ring patterns on corneal topography. The decreased vision in both eyes was due to the irregular corneal surface caused by SEIs, rather than corneal opacity. Topical 0.1% tacrolimus eye drops were effective in treating corneal opacity and irregular corneal surfaces.
Conclusions
Our findings highlight that vision loss due to SEIs after AKC may stem from an irregular corneal surface regardless of corneal opacity severity, and the usefulness of a conventional and simple topography using Placido rings during treatment with 0.1% tacrolimus eye drops for SEIs in AKC.
Keywords: Placido ring mires, Irregular astigmatism, Subepithelial corneal infiltrates, Adenoviral keratoconjunctivitis
Background
Corneal subepithelial infiltrates (SEIs) are characteristic clinical findings of adenoviral keratoconjunctivitis (AKC). SEIs cause photophobia and decreased vision [1, 2]. In eyes with SEIs, both corneal opacity and irregular astigmatism may interfere with vision [3, 4]. However, irregular astigmatism is often overlooked in AKC regardless of corneal opacity severity, because physicians frequently assume that visual impairment is solely due to corneal opacity resulting from SEIs. Anterior segment optical coherence tomography (AS-OCT), which is used to detect irregular astigmatism, is available at only a limited number of facilities. Therefore, a simple method for detecting irregular astigmatism caused by SEIs in AKC is required, especially in children.
Steroid eye drops are effective in the short-term for the treatment of SEIs. However, steroids often lead to the recurrence of SEIs after treatment discontinuation [2, 5, 6]. In addition, steroids are also associated with adverse effects such as cataracts and glaucoma, particularly in children [7, 8]. In recent years, immunosuppressive agents have been used as an alternative to steroids for the treatment of SEIs in an increasing number of cases [2, 6, 9–12].
Here, we describe the case of an 8-year-old girl with persistent vision loss due to irregular astigmatism, despite improved corneal opacity due to SEIs. We successfully detected irregular astigmatism using a Placido disc topography. In addition, the patient experienced improved vision following treatment with 0.1% tacrolimus eye drops. We also documented improvements in corneal surface irregularities due to SEIs using a simple and conventional topography with Placido ring mires. We present some considerations for diagnosing irregular astigmatism due to SEIs and suggest treatments with immunosuppressive agents.
Case presentation
An 8-year-old girl with decreased vision was referred to our clinic. She had been diagnosed with AKC two years prior by a different physician. Since the onset of AKC, she had complained of decreased vision, epiphora, and photophobia in both eyes. She had previously received treatment with corticosteroids, antiallergic agents, and sodium hyaluronate eye drops before presenting at our clinic. Although her symptoms subsided temporarily after treatment, the symptoms such as photophobia and blurred vision frequently recurred. During the initial referral examination at our clinic, the Snellen best-corrected visual acuity (BCVA) was 20/200 in the right eye and 20/50 in the left eye. Symptoms of epiphora and photophobia were remarkable in the right eye. Cycloplegic retinoscopy revealed no significant differences compared to non-cycloplegic retinoscopy results of mild hyperopic astigmatism. Corneal opacity due to SEIs spared the visual axis in both eyes (Fig. 1). The tear meniscus volume was within the normal range and there were no signs of fluorescein staining or chronic papillary conjunctivitis. However, distorted Placido ring mires on corneal topography (PR 8000; San Contact Lens, Inc., Kyoto, Japan) were observed in both eyes (Fig. 2A-a, e, B-a and e), although the patient was instructed to blink immediately before the measurements. Fundoscopy and a B-scan with optical coherence tomography of the retina revealed no abnormal findings (Fig. 3). Therefore, we concluded that the decreased vision in both eyes was caused by an irregular corneal surface due to the SEIs.
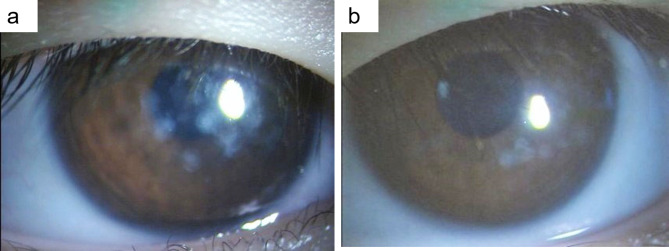
Fig. 1.
Slit-lamp photographs of the right (a) and left (b) eyes at the initial visit to our clinic. Corneal opacity due to subepithelial infiltrates was observed in both eyes; however, it spared the visual axis. The Snellen BCVA was 20/200 in the right eye and 20/50 in the left eye. BCVA, best-corrected visual acuity
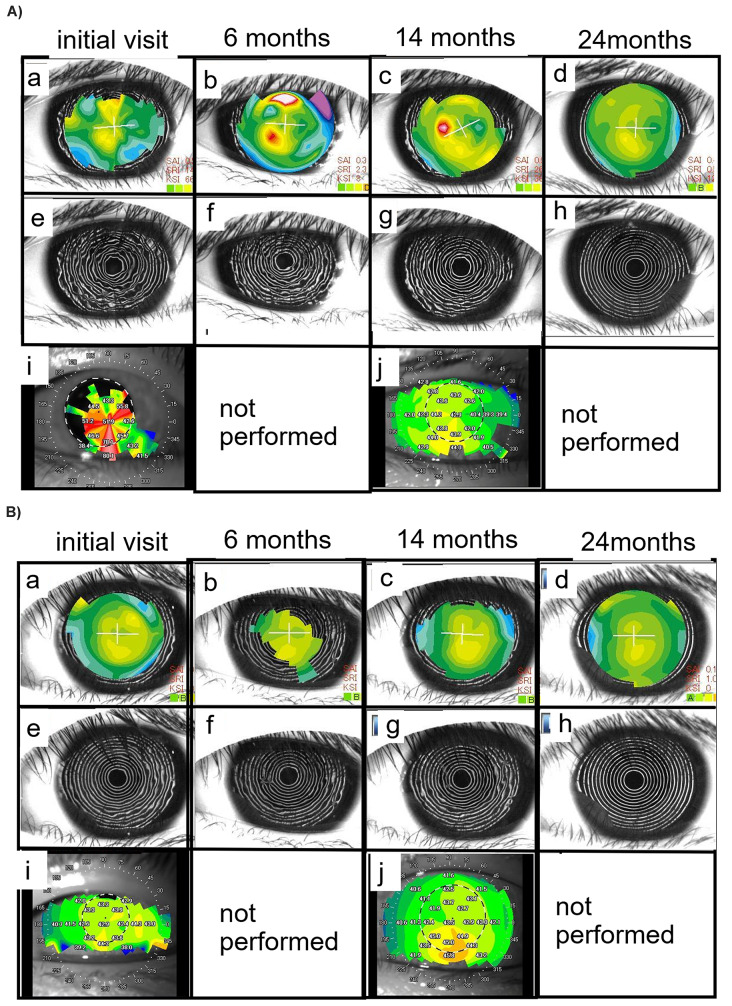
Fig. 2.
Chronological changes in the color-coded axial map (upper row; a,b,c,d) and Placido rings (middle row; e,f, g,h) on Placido disc-based corneal topography (PR 8000; San Contact Lens, Inc., Kyoto, Japan) of the right (A) and left (B) eyes The distorted Placido ring mires effectively illustrated the progression of resolution throughout the treatment course, especially in the right eye. The Snellen BCVA was 20/200 in the right eye, and 20/50 in the left eyes at the initial visit (a, e), 20/63 in the right eye, and 20/20 in the left eye at 6 months (b, f), 20/50 in the right eye, 20/25 in the left eye at 14 months (c, g), and 20/20 in both eyes at 24 months (d, h). Lower row: Color-coded axial map produced by a swept-source corneal optical tomography device (CASIA 2; Tomey, Nagoya, Japan). Topographic maps at the initial visit (i) and 14-month follow-up visit (j). BCVA, best-corrected visual acuity
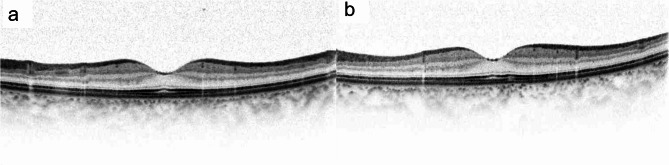
Fig. 3.
Vertical B-scan with optical coherence tomography images of macula in the right (a) and the left (b) eyes taken at the initial visit showed no abnormalities
Although the corneal opacity due to SEIs resolved in both eyes and the visual acuity of the left eye improved after starting 0.1% fluorometholone three times per day, the visual acuity and the irregularity of corneal topography in the right eye showed no improvement. Therefore, treatment with topical 0.1% tacrolimus eye drops twice daily was initiated in both eyes at the 2-month follow-up visit. Consequently, the mire ring disorder gradually improved and the corneal surface became smooth (Fig. 2A and B, corresponding panels a-d, e-h). Placido ring mires (Fig. 2A and B, corresponding panels e-h) more effectively revealed changes in corneal surface irregularities during the course of treatment rather than the color-coded map display by the PR-8000 (Fig. 2A and B, corresponding panels a-d).
Since the irregularity of the corneal surface in the left eye was mild, the improvement in the distorted mire rings was more remarkable in the right eye (Fig. 2A, corresponding panels e-h).
In addition, the color-coded map of swept-source (SS)-AS-OCT (CASIA2; Tomey, Nagoya, Japan) failed to provide useful data (Fig. 2A and B, corresponding panels i and j). Fourteen months after starting the topical tacrolimus treatment, the Snellen BCVA improved to 20/40 (the Snellen BCVA of 20/20 using a hard contact lens) in the right eye, reaching 20/20 at 24 months.
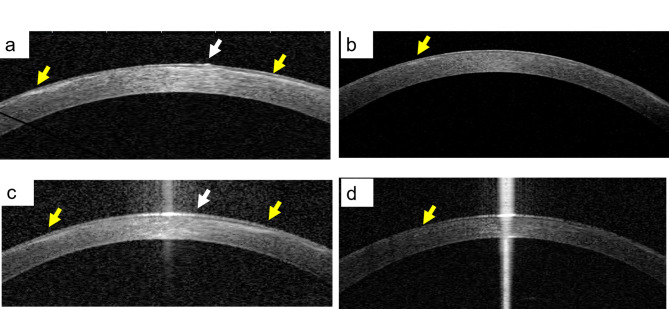
Cross-sectional views of SS-AS-OCT (the CASIA 2; Tomey, Nagoya, Japan) of both eyes revealed irregularities of the corneal surface and hyperreflective lesions in the corneal subepithelial region (white and yellow arrows in Fig. 4a and b) at 9 months after starting 0.1% tacrolimus eye drops, which contributed to the irregularity of Placido ring mires. These ocular surface irregularities and hyperreflective lesions gradually resolved at 18 months after starting 0.1% tacrolimus eye drops (Fig. 4c and d). No adverse effects were observed during the treatment with 0.1% tacrolimus eye drops.
Fig. 4.
Cross-sectional views of swept-source anterior segment optical coherence tomography (SS-OCT) at 9 months after starting 0.1% tacrolimus eye drops in the right (a) and left (b) eyes, irregularities in the corneal epithelial surface (white arrow) and hyperreflective lesions in the corneal subepithelial region (yellow arrow) were observed. Both issues were resolved at 18 months after starting 0.1% tacrolimus eye drops in the right (c) and left (d) eyes
Discussion
Here we described a case of post-AKC SEIs that resulted in decreased visual acuity due to the corneal surface irregularity. Although no significant corneal opacity was observed in the visual axis, irregularities in the corneal epithelial surface resulted in irregular astigmatism, leading to blurred vision. Even minor distortions in the corneal surface can reduce the quality of retinal images. Typically, in cases of SEIs after AKC, physicians focus only on the severity of opacity; however, irregularities of the corneal surface must also be noted. Unfortunately, a direct examination of the corneal surface using slit-lamp microscopy did not provide sufficient information to detect vision-reducing irregular astigmatism in the present case.
Recent advances in corneal imaging systems, such as SS-AS-OCT topography, have enabled a more precise understanding of the corneal surface [13]. However, it can be particularly challenging to keep children still for long periods. In fact, the color-coded map of SS-AS-OCT yielded complicated and unreliable results despite its applicability (Fig. 2A and B, panels i and j). In contrast, a Placido disc paired with an autorefractometer featuring a keratometer is widely accessible and can be rapidly performed, yielding results that are easy to interpret visually. The Placido rings are marked in black and white, enabling an easy display of irregularities. Although we used corneal topography (PR 8000) to detect the Placido ring patterns, similar observations could be obtained using a Placido disc paired with an autorefractometer featuring a keratometer. Thus, employing a simple topography with Placido ring mires facilitates the easy detection of abnormal corneal surfaces.
Pathologically, SEIs are immune responses to adenovirus antigens rather than viral multiplication [14]. Therefore, topical steroids are usually effective and offer a significant advantage in suppressing the subsequent progression to SEIs [15]. Nevertheless, SEIs flare up upon the tapering of steroids, resulting in persistent white opacities that can lead to vision loss [2, 5, 6]. In addition, the topical administration of corticosteroids can prolong viral shedding and infection [16, 17]. Alternatively, topical immunosuppressive agents, including cyclosporine A and tacrolimus, have been proposed as treatments for SEIs [2, 6, 9–12]. In our case, the irregularities of the corneal surface and distorted Placido ring mires on the corneal topography resolved after administration of 0.1% tacrolimus eye drops. We speculate that the 0.1% tacrolimus eye drops effectively suppressed the overactive immune response to residual dead viral particles, causing the irregular corneal surface. Similarly, recent studies have demonstrated a significant improvement in visual acuity in patients treated with topical tacrolimus [10, 11]. Despite potential adverse effects, including burning, tearing, irritation, photophobia, and redness [10], topical tacrolimus has the advantage of preventing intraocular pressure elevation, resulting in fewer SEI recurrences than topical steroid treatment [9, 12]. However, topical immunosuppressive agents also promote viral replication and prolong viral shedding [18]. Notably, combined povidone-iodine (polyvinylpyrrolidone-iodine; PVP-I) therapy with corticosteroids or immunosuppressant is proposed to accelerate clinical resolution and promote rapid eradication of adenovirus virions in patients with AKC [19, 20]. This warrants further prospective investigation.
In conclusion, this report highlights that vision loss due to SEIs after AKC may stem from an irregular ocular surface regardless of corneal opacity severity and the efficacy of topical tacrolimus in treating this condition. Moreover, it demonstrates the importance of observing Placido ring mires, a conventional and simple method that provides the most realistic projection of the corneal surface.
Acknowledgements
The authors thank Aki Yanagisawa, an optometrist from the Nagata Eye Clinic for performing visual acuity test, corneal topography, and anterior segment optical coherence tomography.
Abbreviations
- AKC
Adenoviral keratoconjunctivitis
- SEI
Subepithelial infiltrates
- AS-OCT
Anterior segment optical coherence tomography
- BCVA
Best-corrected visual acuity
Author contributions
KAS designed the observation and performed the treatment of this patient. NT collected and analyzed the data and results of this patient. KAS and NT organized the data and drafted the manuscript. HK and SK supervised the treatment and case report of this patient. All authors have read and approved the final version of the manuscript.
Funding
No funding was received.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This case report and the use of tacrolimus eye drops to treat SEIs after AKC were approved by the Institutional Review Board of Nagata Eye Clinic (#2018-004).
Consent for publication
Written informed consent was obtained from the patient’s parents for the publication of this case. The patient’s anonymity was ensured.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dawson CR, Hanna L, Togni B. Adenovirus type 8 infections in the United States. IV. Observations on the pathogenesis of lesions in severe eye disease. Arch Ophthalmol. 1972;87:258–68. [DOI] [PubMed] [Google Scholar]
- 2.Levinger E, Slomovic A, Sansanayudh W, et al. Topical treatment with 1% cyclosporine for subepithelial infiltrates secondary to adenoviral keratoconjunctivitis. Cornea. 2010;29:638–40. [DOI] [PubMed] [Google Scholar]
- 3.Kurna SA, Altun A, Oflaz A, et al. Evaluation of the impact of persistent subepithelial corneal infiltrations on the visual performance and corneal optical quality after epidemic keratoconjunctivitis. Acta Ophthalmol. 2015;93:377–82. [DOI] [PubMed] [Google Scholar]
- 4.Yildiz BK, Urvasizoglu S, Yildirim Y, et al. Changes in higher-order aberrations after phototherapeutic keratectomy for subepithelial corneal infiltrates after epidemic keratoconjunctivitis. Cornea. 2017;36:1233–6. [DOI] [PubMed] [Google Scholar]
- 5.Laibson PR, Dhiri S, Oconer J, et al. Corneal infiltrates in epidemic keratoconjunctivitis. Response to double-blind corticosteroid therapy. Arch Ophthalmol. 1970;84:36–40. [DOI] [PubMed] [Google Scholar]
- 6.Jeng BH, Holsclaw DS. Cyclosporine A 1% eye drops for the treatment of subepithelial infiltrates after adenoviral keratoconjunctivitis. Cornea. 2011;30:958–61. [DOI] [PubMed] [Google Scholar]
- 7.Ohji M, Kinoshita S, Ohmi E, et al. Marked intraocular pressure response to instillation of corticosteroids in children. Am J Ophthalmol. 1991;112:450–4. [DOI] [PubMed] [Google Scholar]
- 8.Oiwa M, Suzuki Y, Tomita T, et al. Effect of ophthalmic steroids (topical steroids) on intraocular pressure after strabismus surgery in children. Nippon Ganka Gakkai Zasshi. 2022;126:1039–45. [Google Scholar]
- 9.Gouider D, Khallouli A, Maalej A, et al. Corticosteroids versus cyclosporine for subepithelial infiltrates secondary to epidemic keratoconjunctivitis: a prospective randomized double-blind study. Cornea. 2021;40:726–32. [DOI] [PubMed] [Google Scholar]
- 10.Ghanem RC, Vargas JFC, Ghanem VC. Tacrolimus for the treatment of subepithelial infiltrates resistant to topical steroids after adenoviral keratoconjunctivitis. Cornea. 2014;33:1210–3. [DOI] [PubMed] [Google Scholar]
- 11.Berisa Prado S, Riestra Ayora AC, Lisa Fernández C, et al. Topical tacrolimus for corneal subepithelial infiltrates secondary to adenoviral keratoconjunctivitis. Cornea. 2017;36:1102–5. [DOI] [PubMed] [Google Scholar]
- 12.Bhargava R, Kumar P. Comparison of the safety and efficacy of topical tacrolimus (0.03%) versus dexamethasone (0.05%) for subepithelial infiltrates after adenoviral conjunctivitis. Indian J Ophthalmol. 2019;67:594–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanclerz K, Khoramnia R, Wang X. Current developments in corneal topography and tomography. Diagnostics (Basel). 2021;11:1466. 10.3390/diagnostics11081466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lund OE, Stefani FH. Corneal histology after epidemic keratoconjunctivitis. Arch Ophthalmol. 1978;96:2085–8. [DOI] [PubMed] [Google Scholar]
- 15.Holland EJ, Fingeret M, Mah FS. Use of topical steroids in conjunctivitis: a review of the evidence. Cornea. 2019;38:1062–7. [DOI] [PubMed] [Google Scholar]
- 16.Romanowski EG, Roba LA, Wiley L, et al. The effects of corticosteroids of adenoviral replication. Arch. Ophthalmol. 1996;114:581–5. [DOI] [PubMed] [Google Scholar]
- 17.Romanowski EG, Yates KA, Gordon YJ. Topical corticosteroids of limited potency promote adenovirus replication in the Ad5/NZW rabbit ocular model. Cornea. 2002;21:289–91. [DOI] [PubMed] [Google Scholar]
- 18.Romanowski EG, Pless P, Yates KA, et al. Topical cyclosporine a inhibits subepithelial immune infiltrates but also promotes viral shedding in experimental adenovirus models. Cornea. 2005;24:86–91. [DOI] [PubMed] [Google Scholar]
- 19.Kulkarni C, Ballal K. A treatment protocol for minimizing duration and complications of adenoviral epidemic keratoconjunctivitis. Taiwan J Ophthalmol. 2020;10:269–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuura K, Terasaka Y, Miyazaki D, et al. Comparative study of topical regimen for adenoviral kearoconjunctivitis by 0.1% fluorometholone with and without polyvinyl alcohol iodine. Jpn J Ophthalmol. 2021;65:107–14. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.