Abstract
BACKGROUND:
Self-management is important for asthma control, yet it is unclear whether asthmatic patients have sufficient knowledge to optimally manage their disease. We examined the associations between the knowledge of self-management in adult patients attending a polyclinic in Singapore, sociodemographic factors, and asthma control.
MATERIALS AND METHODS:
A cross-sectional survey was conducted among adult asthmatic patients in a public primary care clinic (polyclinic) using convenience sampling. A a structured and validated self-administered questionnaire solicited the responses of study participants. Questionnaire comprised three sections: (1) Sociodemographic and asthma-related variables, (2) Modified Asthma Self-Management Questionnaire (ASMQ), and (3) The GINA assessment of asthma control. Participants completed the questionnaire in the clinic waiting area and returned them into a sealed box in the same area. Data were analyzed using SPSS version 29.0. Summary statistics were used to describe the study sample; t-test or analysis of variance (ANOVA), as appropriate, tested the differences in self-management knowledge by sociodemographic characteristics. Logistic regression was used to determine the association between asthma control and self-management knowledge controlling for sociodemographic characteristics.
RESULTS:
The sample comprised 141 asthma patients; Out of a total of 100 points, the mean ASMQ score was 46.8 (standard deviation 21.7). The scores for the knowledge of self-management of Asthma differed by age, level of education, and having been taught about asthma on bivariate analyses (P < 0.05). Linear regression showed a significant association of asthma self-management knowledge with educational level only. No association was observed between ASMQ scores and asthma control.
CONCLUSION:
There were gaps in patients’ knowledge about asthma self-management, although they were generally knowledgeable about the inhaler technique. Higher education levels were associated with higher levels of knowledge beyond the effect of age and having been instructed about asthma, suggest that it is crucial that educational programs on asthma are made accessible to patients with lower levels of education. Further research needs to determine whether asthma educational programs targeting the knowledge gaps found in this study can improve knowledge of self-management and asthma control.
Keywords: Asthma, knowledge, primary care, self-management, Singapore
Introduction
Asthma is a common chronic respiratory condition seen in primary care[1] with 10.5% of Singapore residents aged 18–69 years having a diagnosis of lifetime asthma.[2] This respiratory condition has evolved from a low-prevalence, low-impact disease to a high prevalence problem of significant magnitude.[3] Despite the availability of asthma medications, asthma mortality in Singapore is 3 times that of other developed nations such as the United States and New Zealand.[3]
Self-management refers to the day-to-day management of a chronic disease.[4] Self-management of asthma refers to what patients do to monitor and control their symptoms and prevent exacerbation.[5] This includes effective inhaler use, self-monitoring of symptoms, use of a written asthma action plan (WAAP), and adherence to medications and appointments.[6] Knowledge of self-management of asthma empowers patients to self-manage their asthma. Both local and international guidelines have emphasized the importance of self-management.[6,7] Education on self-management is a cost-effective way of treating asthma sufferers[8] and has been shown to reduce emergency visits and hospital admissions in Singapore.[9] Self-management is particularly important in asthma because it is a variable disease and can be exacerbated even if a patient’s asthma is well-controlled.
In a study of 2467 patients in 8 Asian countries including Singapore in 2014, patients consistently overestimated their level of asthma control contrary to what their symptoms suggested: 81.6% of study participants with Global Initiative for Asthma (GINA)-defined uncontrolled asthma perceived that their asthma was under control.[10] In another study of 332 patients in a hospital intensive care unit in Singapore, 64.0% of the 127 patients with severe asthma neither had regular reviews nor received controller medications.[11] This suggests a poor self-perception of asthma control and a lack of knowledge of self-management.
While there were local studies that examined physicians’ drug prescribing patterns and use of the WAAP in primary care,[12,13,14] few studies have been done to assess patients’ knowledge and understanding of asthma management. The existing local studies in primary care were done before the introduction of international clinical practice guidelines on the management of asthma.[15,16] Thus, little is known about the current level of the knowledge of self-management and its sociodemographic determinants in asthmatic patients in Singapore primary care.
The aim of this study was to measure self-management knowledge of asthmatic adult patients attending a primary care clinic (polyclinic) in the Western region of Singapore, as well as the relationship between levels of the knowledge of self-management and demographic factors. A secondary aim was to examine the relationship between levels of the knowledge of self-management and asthma control. The hypotheses are as follows: (a) asthmatic patients with certain demographic factors, such as the level of knowledge of self-management of younger asthmatics or those with higher education may be higher and (b) a higher level of knowledge of asthma self-management will in turn result in higher odds of having well-controlled asthma.
Materials and Methods
This was a descriptive, cross-sectional study using a self-administered questionnaire. The study was conducted in a polyclinic in the Western part of Singapore. Ethical approval was obtained from the Domain Specific Review Board (DSRB) vide Letter No. 2020/01443 dated 09/02/2021. Consent was implied if the participant was willing to complete and submit the questionnaire. The study participants were adult outpatients at the polyclinic from May 2021 to January 2022. The inclusion criteria were patients above 21 years old, with a diagnosis of bronchial asthma in the electronic health records, with no cognitive impairment, able to read and understand English, and able to give informed consent to participate in the study. Exclusion criteria included having chronic obstructive pulmonary disease or other chronic respiratory diseases.
Knowing that 735 unique adult asthma patients were seen in this polyclinic from September 2019 to August 2020, and given an estimated population variance of 2.56 for raw Asthma Self-Management Questionnaire (ASMQ) scores reported in a previous study,[17] the required sample size was estimated at 130 for this study considering a margin of error of 0.25 and a 95% confidence level.
Between May 2021 and January 2022, 141 eligible asthmatic patients were identified and enrolled using convenience sampling. No financial incentives were given to participants. Eligible patients with a diagnosis of asthma in their medical records were identified by care providers (doctors and nurses). Patients were then informed of the study by the care providers and were given the questionnaire and a cover letter detailing the intent of the study. Participants were informed that their participation was voluntary and their decision to participate would not jeopardize their healthcare in any way. They were also assured of their anonymity. Participants completed the self-administered questionnaire in the clinic waiting area and returned them into a sealed box in the same area. Each participant was then given a unique participant ID by the research assistant after the questionnaire forms were returned. Completion and return of the questionnaire implied consent to participate.
The study questionnaire comprised three sections: (1) Sociodemographic and asthma-related variables: These included information on age, sex, ethnicity, highest education level, smoking status, family history of asthma, age of asthma diagnosis, having a WAAP, and having been taught about asthma by a healthcare provider. (2) Modified ASMQ, a validated 16-item questionnaire that assesses knowledge of self-management of asthma in English,[18] that measures knowledge of preventive strategies, inhaler use, medications, and use of peak flow meters. The original ASMQ underwent content validation by 3 senior family physicians and 2 respiratory physicians with a range of 7–24 years of practice. Following content validation, questions 5 and 11 on peak flow were deemed less relevant as they were not routinely used in Singapore owing to concerns about infection control. Permission was then obtained from the creators of the ASMQ to remove these two questions from the questionnaire. A correct answer was awarded 1 point, and a wrong or “don’t know” answer had no points. The final score of the modified ASMQ was scored out of 14 instead of 16. The raw score was then transformed to range from 0 to 100 as follows: (raw score/14) × 100. Higher modified scores indicated more knowledge of asthma self-management. Participants were considered to have poor knowledge if their scores were below 50, adequate knowledge if their scores were between 50 and 75, and good knowledge if their scores were above 75. (3) The GINA assessment of asthma control,[6] is an internationally recognized set of 4 questions for rating asthma control. Asthma is considered well-controlled if responses to all questions below were “no,” partially controlled if one or two responses were “yes” and uncontrolled if three to four responses were “yes.” The 4 questions are: In the last 4 weeks have you had (1) Daytime asthma symptoms more than twice/week? (2) Any night waking due to asthma? (3) To use a reliever inhaler more than twice/week? (4) Any activity limitation because of asthma?
Data were analyzed using the Statistical Package for the Social Sciences software version 29.0 (IBM SPSS Statistics for Windows, Version 29.0. Armonk, NY, USA: IBM Corp.). Descriptive statistics were used to characterize the sample. Next, independent samples t-test (for binary variables) and one-way analysis of variance (for categorical variables with more than two categories, followed by the post hoc test, Tukey’s honestly significant difference) were used to test differences in self-management knowledge by sociodemographic characteristics. Findings from the bivariate analyses were then confirmed by multiple regression. Linear regression was used to test associations between self-management knowledge as the dependent variable and sociodemographic characteristics as independent variables (asthma control was excluded from this analysis). Binomial logistic regression was used to test the association of levels of asthma control as the dependent variable, which was dichotomized into “well-controlled asthma” versus “partly controlled and uncontrolled asthma”, and self-management knowledge while adjusting for sociodemographic characteristics. A P < 0.05 was considered statistically significant. Missing data were handled with list-wise deletion (i.e., complete case analysis was performed).
Results
All 141 completed questionnaires were included in the data analyses. Seven of the participants (5.0% of the total sample) did not include their age in the questionnaire. There was no other missing data. Table 1 shows the demographic characteristics of participants who completed the questionnaire. The 14-question modified ASMQ scores were treated as normally distributed in the analysis with a mean score of 46.8. As summarized in Figure 1, the question with the highest percentage of correct responses (81.6%) was question 8 (“After you have used your inhaler, you should hold your breath for several seconds”). The question with the lowest percentage of correct responses (13.5%) was question 1 (“A main method of preventing asthma flare-ups is to get a flu vaccine”). The question with the highest proportion of incorrect responses (66.0%) was question 9 (“if you are having symptoms and don’t know why, the first thing you should do is change your immediate environment”). A tabulation of all incorrect responses is included in Table 2.
Table 1.
Characteristics of asthma patients in a polyclinic at Western part of Singapore, 2022 (n=141)
| Characteristics | N (%) |
|---|---|
| Age (years)*, mean±SD | 46.2±14.4 |
| Age group (years)* | |
| 21–35 | 34 (25.3) |
| 36–60 | 79 (59.0) |
| >60 | 21 (15.7) |
| Sex | |
| Male | 58 (41.1) |
| Female | 83 (58.9) |
| Ethnicity | |
| Chinese | 45 (31.9) |
| Malay | 60 (42.6) |
| Indian | 31 (22.0) |
| Others | 5 (3.5) |
| Level of education | |
| Primary education and below | 16 (11.3) |
| Secondary education | 45 (31.9) |
| Tertiary education | 80 (56.7) |
| Smoking status | |
| Smoker | 34 (24.1) |
| Nonsmoker | 107 (75.9) |
| Family history of asthma | |
| Yes | 79 (56.0) |
| No | 62 (44.0) |
| Has WAAP | |
| Yes | 44 (31.2) |
| No | 71 (50.4) |
| Unsure | 26 (18.4) |
| Taught about asthma | |
| Yes | 116 (82.3) |
| No | 25 (17.7) |
| Knowledge on asthma self-management | |
| Poor (<50) | 70 (49.6) |
| Adequate (50–75) | 58 (41.1) |
| Good (>75) | 13 (9.2) |
| Level of asthma control based on GINA | |
| Well controlled | 68 (48.2) |
| Partly controlled | 46 (32.6) |
| Uncontrolled | 27 (19.1) |
| Raw ASMQ score, mean±SD | 6.55±3.03 |
| Transformed ASMQ score, mean±SD | 46.8±21.7 |
*As 7 participants did not indicate their age, the analysis for age was based on n=134. ASMQ=Asthma Self-Management Questionnaire, GINA=Global Initiative for Asthma, SD=Standard deviation, WAAP=Written Asthma action plan
Figure 1.
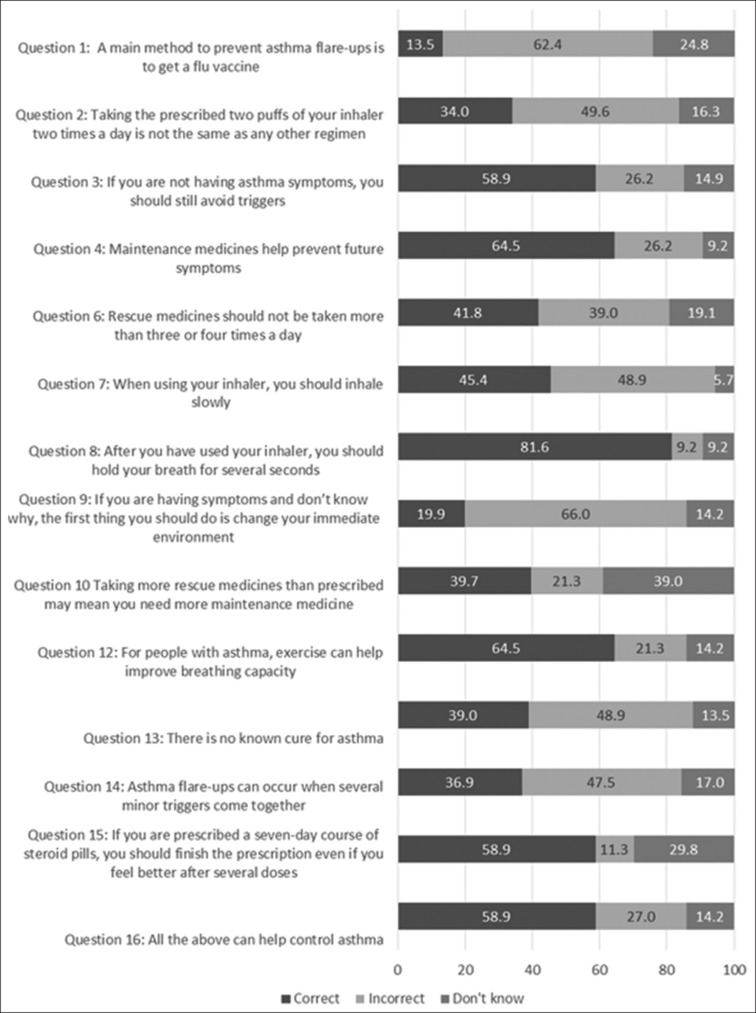
Frequency distribution of responses to the 14 items of the Asthma Self-Management Questionnaire by asthma patients attending a polyclinic in Western part of Singapore, 2022 (n=141)
Table 2.
Frequency distribution of incorrect responses to 14 items in the Asthma Self-Management Questionnaire by asthma patients attending a polyclinic in Western part of Singapore, 2022 (n=141)
| ASMQ items | Incorrect responses | N (%) |
|---|---|---|
| A main method to prevent asthma flare-ups is to | Take medicines before meals | 43 (30.5) |
| Take steroids in pill form | 22 (15.6) | |
| Go to the emergency room at the first sign of symptoms | 23 (16.3) | |
| Taking the prescribed two puffs of your inhaler two times a day | Is the same as taking one puff four times a day | 17 (12.1) |
| Is the same as taking four puffs once a day | 21 (14.9) | |
| Can be arranged in any way as long as you take a total of four puffs a day | 32 (22.7) | |
| If you are not having asthma symptoms | Your lungs are not sensitive to irritants | 11 (7.8) |
| It is ok to skip some doses of medicine | 20 (14.2) | |
| You are probably cured of asthma | 6 (4.3) | |
| Maintenance medicines | Don’t need to be taken every day | 6 (4.3) |
| Make you breathe better right after you take them | 31 (22.0) | |
| Can only be taken in pill form | 0 | |
| Rescue medicines | Help prevent future flare-ups | 43 (30.5) |
| Have no side effects | 5 (3.5) | |
| Do not cause you to become tolerant to medicine | 7 (5.0) | |
| When using your inhaler, you should | Take shallow breaths | 28 (19.9) |
| Inhale quickly | 40 (28.4) | |
| Press your inhaler several times while you are inhaling | 1 (0.7) | |
| After you have used your inhaler, you should | Take the second puff as soon as possible after the first puff | 8 (5.7) |
| Keep taking puffs until you feel better | 0 | |
| Wash the inhaler in a tub of water | 5 (3.5) | |
| If you are having symptoms and don’t know why, the first thing you should do is | Take some doses of steroid medicines | 54 (38.3) |
| Call your doctor | 32 (22.7) | |
| Count how fast you are breathing | 7 (5.0) | |
| Taking more rescue medicines than prescribed | Is really not harmful | 8 (5.7) |
| Is a good way to manage symptoms caused by exercise | 18 (12.8) | |
| May mean you can take less maintenance medicine | 4 (2.8) | |
| For people with asthma, exercise | Is something that should not be done regularly | 4 (2.8) |
| Is only good if done for at least 30 min at a time | 13 (9.2) | |
| Can trigger symptoms because the lungs are not taking in enough oxygen | 13 (9.2) | |
| Asthma can be cured by | Taking daily medicine | 34 (24.1) |
| Avoiding triggers, such as dust and cigarette smoke | 33 (23.4) | |
| Using a peak flow meter | 2 (1.4) | |
| Asthma flare-ups | Usually occur suddenly without warning | 41 (29.1) |
| Cannot be triggered by strong emotions | 5 (3.5) | |
| Always cause wheezing | 21 (14.9) | |
| If you are prescribed a 7-days course of steroid pills | You don’t have to avoid triggers while you are taking the pills | 5 (3.5) |
| Your symptoms can’t get worse while you are taking the pills | 10 (7.1) | |
| You don’t need to use your peak flow meter while you are taking the pills | 1 (0.7) | |
| Which of the following can help control asthma? | Reducing stress levels | 16 (11.3) |
| Drinking plenty of water to stay hydrated | 12 (8.5) | |
| Avoiding foods with sulfites, such as dried fruits and wine | 10 (7.1) |
In bivariate analyses, the scores on the knowledge of asthma self-management significantly differed among subgroups based on age, education level, and having been given instructions on asthma. The subgroup with a WAAP had a higher asthma self-management knowledge score than the subgroup without, but this difference did not reach significance [Table 3].
Table 3.
Comparison of Asthma Self-Management Questionnaire scores by sociodemographic characteristics and asthma related characteristics of asthma patients attending a polyclinic in Western part of Singapore, 2022 (n=141)
| Variables | N (%) | Transformed ASMQ score Mean±SD | P-value* |
|---|---|---|---|
| Age group (n=134) | |||
| 21–35 | 34 (25.4) | 54.8±191 | 0.003 |
| 36–60 | 79 (59.0) | 47.3±22.5 | |
| >60 | 21 (15.7) | 34.4±18.3 | |
| Sex | |||
| Male | 58 (41.1) | 48.8±19.9 | 0.372 |
| Female | 83 (58.9) | 45.4±22.9 | |
| Ethnicity | |||
| Chinese | 45 (31.9) | 49.8±21.4 | 0.689 |
| Malay | 60 (42.6) | 45.8±21.2 | |
| Indian | 31 (22.0) | 45.1±23.4 | |
| Others | 5 (3.5) | 41.4±22.8 | |
| Level of education | |||
| Primary education and below | 16 (11.3) | 29.0±18.3 | <0.001 |
| Secondary education | 45 (31.9) | 39.5±18.2 | |
| Tertiary education | 80 (56.7) | 54.5±20.6 | |
| Smoking history | |||
| Smoker | 34 (24.1) | 40.8±20.6 | 0.062 |
| Nonsmoker | 107 (75.9) | 48.7±21.8 | |
| Family history of asthma | |||
| Yes | 79 (56.0) | 47.9±21.7 | 0.494 |
| No | 62 (44.0) | 45.4±21.7 | |
| Having a WAAP | |||
| Yes | 44 (31.2) | 51.9±20.8 | 0.058 |
| No or unsure | 97 (68.8) | 44.5±21.8 | |
| Being taught about asthma | |||
| Yes | 116 (82.3) | 48.9±21.5 | 0.013 |
| No | 25 (17.7) | 37.1±20.4 | |
| Level of asthma control based on GINA | |||
| Well-controlled | 68 (48.2) | 47.4±22.3 | 0.518 |
| Partly-controlled | 46 (32.6) | 48.4±19.2 | |
| Uncontrolled | 27 (19.1) | 42.6±24.1 | |
ASMQ=Asthma Self-Management Questionnaire; GINA=Global Initiative for Asthma, WAAP=Written asthma action plan, SD=Standard deviation
In linear regression [Table 4], sociodemographic characteristics accounted for 25% of the variance of asthma self-management knowledge (R2 = 0.26, P < 0.001). Among the independent variables, only educational level remained significantly associated with asthma self-management knowledge, to the extent that participants with a tertiary education had higher knowledge scores than participants with primary education or no education (Standardized β = 20.82, β = 0.47, P < 0.001).
Table 4.
Multiple linear regression model: Predictors of asthma self-management knowledge score among asthma patients at a polyclinic in Western part of Singapore, 2022 (n=134)
| Characteristics | Unstandardized β | Standardized β | SE of β | t | P-value* |
|---|---|---|---|---|---|
| Age (reference 21–35) | |||||
| 36–60 | −5.28 | −0.12 | 4.40 | −1.20 | 0.233 |
| Above 60 | −11.42 | −0.19 | 6.58 | −1.74 | 0.085 |
| Sex (reference male) | −1.29 | −0.03 | 3.86 | −0.33 | 0.739 |
| Ethnicity (reference Chinese) | |||||
| Malay | −2.44 | −0.06 | 4.24 | −0.58 | 0.566 |
| Indian | −3.95 | −0.08 | 4.79 | −0.82 | 0.412 |
| Others | −7.68 | −0.07 | 9.47 | −0.81 | 0.419 |
| Level of education (reference primary education or below) | |||||
| Secondary education | 10.35 | 0.22 | 6.03 | 1.72 | 0.088 |
| Tertiary education | 20.82 | 0.47 | 6.04 | 3.45 | 0.001 |
| Smoking history | −8.98 | −0.18 | 4.25 | −2.12 | 0.037 |
| Family history of asthma | −0.48 | −0.01 | 3.75 | −0.13 | 0.899 |
| Having a WAAP | −3.00 | −0.07 | 4.02 | −0.75 | 0.457 |
| Being taught about asthma | 6.79 | 0.12 | 4.95 | 1.37 | 0.173 |
Model statistics: R2=0.26, adjusted R2=0.19, F (12,121)=3.58, P<0.001. ASMQ=Asthma Self-Management Questionnaire, WAAP=Written asthma action plan, SE=Standard error, *Statistically significant at P<0.05
The level of self-management knowledge (ASMQ) scores did not vary with GINA-defined levels of asthma control, neither in bivariate analysis [Table 3] nor in multivariate analysis [Table 5]. Binomial logistic regression further highlighted that none of the sociodemographic characteristics were associated with higher odds of good asthma control [Table 5].
Table 5.
Logistic regression analysis: Factors associated with well control of asthma among asthma patients at a polyclinic in Western part of Singapore, 2022 (n=134)
| Characteristics | OR | 95% CI for OR | P-value* |
|---|---|---|---|
| Modified ASMQ score | 1.01 | 0.99–1.03 | 0.433 |
| Age (reference 21–35) | |||
| 36–60 | 1.01 | 0.41–2.50 | 0.979 |
| Above 60 | 1.02 | 0.26–3.97 | 0.983 |
| Sex (reference male) | 1.12 | 0.51–2.46 | 0.788 |
| Ethnicity (reference Chinese) | |||
| Malay | 0.83 | 0.35–1.95 | 0.662 |
| Indian | 1.02 | 0.39–2.68 | 0.973 |
| Others | 5.17 | 0.50–53.13 | 0.167 |
| Level of education (reference primary education or below) | |||
| Secondary education | 0.78 | 0.23–2.69 | 0.696 |
| Tertiary education | 0.71 | 0.20–2.56 | 0.598 |
| Smoking history | 0.78 | 0.32–1.88 | 0.576 |
| Family history of asthma | 1.03 | 0.48–2.21 | 0.937 |
| Having a WAAP | 1.40 | 0.62–3.20 | 0.420 |
| Being taught about asthma | 1.26 | 0.45–3.50 | 0.657 |
ASMQ=Asthma Self-Management Questionnaire, OR=Odds ratio, CI=Confidence interval, WAAP=Written asthma action plan, *Statistically significant at P<0.05
Discussion
This study showed that asthmatic patients in Singapore had good knowledge in some aspects of inhaler technique but had poor knowledge about the flu vaccine and the assessment of environmental triggers. From the tested demographic factors, participants with higher education had higher level of the knowledge of asthma self-management beyond the effect of age, having been taught about asthma, and other sociodemographic characteristics. By contrast, the positive effect of age and being taught about asthma on knowledge about asthma was better accounted for by education levels.
The mean ASMQ score of this study is 46.8/100, higher than a similarly conducted Vietnamese study[19] (mean score of 30/100) and a Saudi Arabian study[17] (mean raw score 3.5/14, or a transformed score of 25/100). Both these studies also used the 14-question modified ASMQ without the questions on the peak flow meter. The difference in mean score could be explained by the higher educational level of our study population. Only 11.9% of our study participants had “below secondary education” as compared with 27.0% with “below secondary education” in the Vietnamese study and 40.2% with “below intermediate education” (equivalent to below secondary education) in Saudi Arabia.
Although there is currently no gold standard for measuring patient knowledge of asthma,[20] similar studies done previously have shown low knowledge of self-management in asthmatic patients in Singapore. In a study conducted in five polyclinics in 1992,[16] the mean score of an interviewer-administered questionnaire of knowledge of asthma mechanism and its medications was 1.4 (median 1) out of a total score of 6.
Only 28 (19.9%) participants knew that they should first change their immediate environment if they experience symptoms without knowing why. In contrast, 54 (38.3%) participants chose the incorrect answer “If you are having symptoms and don’t know why, the first thing you should do is take some doses of steroid medicines.” A study in a local tertiary hospital of 94 subjects showed that only 43.6% of that study’s participants were aware of the role of oral prednisolone.[21] Consistently, poor knowledge of the use of oral corticosteroids might have led participants to select the incorrect answer for question 9.
Patients with lower levels of education had lower asthma knowledge scores. A similar relationship was also previously found in local studies involving asthma patients in five polyclinics in 1992[16] and a tertiary care hospital,[21] and overseas studies.[19,22,23] While inadequate health literacy can be a barrier to good asthma knowledge, tailored education in the form of a one-on-one session on asthma education before discharge from the hospital has been shown to improve inhaler technique and knowledge on inhaler use of patients with lower literacy.[24] In the polyclinics, asthma education is also done one-on-one with patients by either the doctor or the nurse, usually with the help of patient education materials. However, patients with lower literacy or poor reading skills may not be able to understand medical instructions in standard patient education materials.[25] A review done on asthma-related patient education materials in 2020 showed that only 2 of the 30 leaflets (6.7%) used in Singapore primary care met the recommended reading level of below secondary education.[26] This could also explain why being taught about asthma and self-management of asthma did not retain significance after covarying for education. It is, therefore, important for healthcare providers to assess the comprehension of patients with lower literacy especially when using patient education materials.
In our study, there was no significant difference in ASMQ scores in participants with a WAAP and those without. The WAAP is recommended by both global[6] and local guidelines[7] and has been adopted in all polyclinics under the recommendation of the Singapore National Asthma Programme.[27] The WAAP educates patients on the early recognition and treatment of deteriorating asthma[28] and includes specific instructions for the patient about increasing the doses of reliever and control medicines, the use of oral corticosteroids, when and how to access medical care when there is exacerbation.[6] In contrast to our study, prior research has associated having a written asthma plan with good asthma self-management knowledge in Sweden.[29] The results in our study could suggest that just having a WAAP is insufficient in Singapore, as patients might still not know about trigger avoidance or the need to change their environment if they experience symptoms. These aspects of asthma self-management are not included in the local WAAP document, and it is unclear if they are included in the Swedish setting. It is also unclear if the Swedish study examined these specific aspects of self-management knowledge in their questionnaire study.
Patients taught about asthma had higher ASMQ scores; however, this difference was not significant after co-varying for education levels. Out of the 141 participants, 116 (82.3%) reported being ever taught about asthma. Forty-five (31.0%) participants reported being taught about inhaler technique and 33 (23.4%) participants left the open-ended question “what were you taught about?” blank. The small difference in ASMQ scores in these subgroups could be because this question was not able to measure or quantify how much patients were taught about asthma. Nevertheless, it is encouraging that questions relating to inhaler technique had a higher rate of correct responses: Question 7 (“when using your inhaler you should inhale slowly”) had 45.4% correct responses and question 8 (“after you have used your inhaler you should hold your breath for several seconds”) had 81.6% correct responses.
This study did not demonstrate a significant difference in levels of knowledge of asthma self-management and subgroups of patients with different levels of asthma control. ASMQ scores in previous studies have been associated with better asthma outcomes – higher ASMQ scores have been associated with better scores on the Asthma Quality of Life Questionnaire,[18] the Asthma Control Test, and GINA-defined assessment of asthma control.[19] A possible reason for this could be that there was an unexpectedly high number of patients (48.2%) with well-controlled asthma, possibly due to convenience sampling.
This study demonstrates notable strengths, including minimal missing data and successful attainment of the desired sample size, despite fewer clinic visits for both chronic disease management[30] and acute respiratory tract infections[31] during the COVID-19 pandemic in 2021. It was also the first study in Singapore to use the ASMQ. While the ASMQ measured levels of knowledge without subthemes, responses to individual questions showed gaps in the knowledge of asthmatic patients in Singapore, which were not previously known. These findings can help guide future improvements in asthma education programs.
This study’s limitations stem from its research methodology: the self-administered questionnaire did not allow for data capture of the nonresponders, and convenience sampling might have resulted in over-representation of participants with good asthma control. Secondly, as this study was done in one polyclinic, the results may not be generalizable to other primary care institutions. Furthermore, only English-speaking participants were enrolled in this study, omitting information on the knowledge of self-management of asthma patients who might be more proficient in other languages. Finally, as this was a questionnaire-based cross-sectional study, causal relationships could not be established based on the findings and recall bias could not be excluded.
Conclusion
This study has revealed gaps in the knowledge of patients’ self-management of asthma, although patients were generally more knowledgeable about inhaler technique. It has also shown that the knowledge of the self-management of asthma of patients with higher educational levels is better. Levels of knowledge of asthma self-management did not differ among patients with different levels of asthma control in this study, possibly because of the over-representation of well-controlled asthmatic patients.
Nevertheless, our study prompts further research to identify sociodemographic and behavioral determinants of asthma control, beyond levels of self-management knowledge. Interventions designed for patients with lower levels of education as well as interventional studies that examine the effect of asthma education on improvement in identified knowledge gaps in this study should be considered.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Health Information Division, Ministry of Health, Singapore Primary Care Health Survey Report. 2014 Available from: https://www.moh.gov.sg/resources- statistics/reports/primary-care-survey-2014-report . [Last accessed on 2022 Feb 24] [Google Scholar]
- 2.Epidemiology and Disease Control Division, Ministry of Health, Singapore National Health Survey. 2010 Available from: https://www.moh.gov.sg/resources-statistics/reports/national-health-survey-2010 . [Last accessed on 2022 Feb 24] [Google Scholar]
- 3.Koh MS, Yii AC, Ong YY. Asthma in Singapore: Past, present and future. Ann Acad Med Singap. 2017;46:81–3. [PubMed] [Google Scholar]
- 4.Lorig KR, Holman H. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 5.Mancuso CA, Sayles W, Allegrante JP. Knowledge, attitude, and self-efficacy in asthma self-management and quality of life. J Asthma. 2010;47:883–8. doi: 10.3109/02770903.2010.492540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global Initiative for Asthma Global Strategy for Asthma Management and Prevention. 2020 Available from: https://www.ginasthma.org . [Last accessed on 2024 Sep 29] [Google Scholar]
- 7.ACE Clinical Guidance (ACG), Ministry of Health, Singapore Asthma – Optimising Long-Term Management with Inhaled Corticosteroid. 2020 Available from: https://go.gov.sg/acg-asthma-optimising-long-term-management-with-inhaled-corticosteroid . [Last accessed on 2024 Sep 29] [Google Scholar]
- 8.Hsu J, Wilhelm N, Lewis L, Herman E. Economic evidence for US asthma self-management education and home-based interventions. J Allergy Clin Immunol Pract. 2016;4:1123–34.e27. doi: 10.1016/j.jaip.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prabhakaran L, Lim G, Abisheganaden J, Chee CB, Choo YM. Impact of an asthma education programme on patients’ knowledge, inhaler technique and compliance to treatment. Singapore Med J. 2006;47:225–31. [PubMed] [Google Scholar]
- 10.Price D, David-Wang A, Cho SH, Ho JC, Jeong JW, Liam CK, et al. Time for a new language for asthma control: Results from REALISE Asia. J Asthma Allergy. 2015;8:93–103. doi: 10.2147/JAA.S82633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim T, Prabakaran L, Abisheganaden J, Chua G, Heng B, Sun Y. The WHO classification of severe asthma in intensive care patients. Eur Respir J. 2011;38:880. [Google Scholar]
- 12.Tan NC, Tay IH, Ngoh A, Tan M. Factors influencing family physicians’ drug prescribing behaviour in asthma management in primary care. Singapore Med J. 2009;50:312–9. [PubMed] [Google Scholar]
- 13.Tan NC, Tay IH, Ngoh A, Tan M. A qualitative study of factors influencing family physicians’ prescription of the written asthma action plan in primary care in Singapore. Singapore Med J. 2009;50:160–4. [PubMed] [Google Scholar]
- 14.Tan NC, Chow MH, Goh P, Goh LG, Lim TK. Primary care doctors’ practice in the management of adult asthma patients. Singapore Med J. 2002;43:061–066. [PubMed] [Google Scholar]
- 15.Lee KA, Lim YW, Ng TP. Asthma self care efficacy and morbidity in polyclinic outpatients. Ann Acad Med Singap. 1995;24:846–50. [PubMed] [Google Scholar]
- 16.Wong ML, Ng TP, Hong CY, Koh KT, Goh LG, Ling SL. Understanding asthma: Patient survey. Ann Acad Med Singap. 1994;23:861–5. [PubMed] [Google Scholar]
- 17.AI E, Alharthi B, Alharthi S. Self-management and control of asthma among adult patients in King Faisal medical complex Taif, KSA. Int J Res Pharm Sci. 2017;7:24–9. [Google Scholar]
- 18.Mancuso CA, Sayles W, Allegrante JP. Development and testing of the asthma self-management questionnaire. Ann Allergy Asthma Immunol. 2009;102:294–302. doi: 10.1016/S1081-1206(10)60334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen VN, Huynh TT, Chavannes NH. Knowledge on self-management and levels of asthma control among adult patients in Ho Chi Minh City, Vietnam. Int J Gen Med. 2018;11:81–9. doi: 10.2147/IJGM.S157050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pink J, Pink K, Elwyn G. Measuring patient knowledge of asthma: A systematic review of outcome measures. J Asthma. 2009;46:980–7. doi: 10.3109/02770900903338486. [DOI] [PubMed] [Google Scholar]
- 21.Chai SM, Tan KL, Wong JL, Eng P. Asthma knowledge among adult asthmatic outpatients in a tertiary care hospital. Asian Pac J Allergy Immunol. 2004;22:81–9. [PubMed] [Google Scholar]
- 22.Sharifi L, Pourpak Z, Heidarnazhad H, Bokaie S, Moin M. Asthma knowledge, attitude, and self-efficacy in Iranian asthmatic patients. Arch Iran Med. 2011;14:315–20. [PubMed] [Google Scholar]
- 23.Madhushani H, Subasinghe H. Knowledge attitudes and practices of asthma; Does it associate with demographic factors of adult patients. Asian Pac J Health Sci. 2016;3:94–9. [Google Scholar]
- 24.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 26.Phua CY, Zheng L, Tan NC, Tang WE, Elizabeth Smith H. Review of the quality of printed patient education materials on asthma available in primary care in Singapore. J Asthma. 2020;57:787–98. doi: 10.1080/02770903.2019.1602876. [DOI] [PubMed] [Google Scholar]
- 27.Chong PN, Tan NC, Lim TK. Impact of the Singapore National Asthma Program (SNAP) on preventor-reliever prescription ratio in polyclinics. Ann Acad Med Singap. 2008;37:114–7. [PubMed] [Google Scholar]
- 28.Holt S, Masoli M, Beasley R. The use of the self-management plan system of care in adult asthma. Prim Care Respir J. 2004;13:19–27. doi: 10.1016/j.pcrj.2003.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wireklint P, Hasselgren M, Montgomery S, Lisspers K, Ställberg B, Janson C, et al. Factors associated with knowledge of self-management of worsening asthma in primary care patients: A cross-sectional study. J Asthma. 2021;58:1087–93. doi: 10.1080/02770903.2020.1753209. [DOI] [PubMed] [Google Scholar]
- 30.Liow Y, Keong Loh VW, Young D. 100 days on: The primary care response to COVID-19 in Singapore. Singapore Med J. 2022;63:545–7. doi: 10.11622/smedj.2020162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Average Daily Polyclinic Attendances for Selected Diseases. Available from: https://data.gov.sg/dataset/average-daily-po lyclinic-attendances-selected-diseases?view_id%3Db99e6960-2279-4a6b-92fb-93607d 21fcdc%26resource_id%3Ddd4dcaac-aa8d -49de-a96a-b809f8d3ae0d . [Last accessed on 2022 Apr 18] [Google Scholar]


