Abstract
Purpose:
Here, we describe cardiac magnetic resonance imaging (CMR) findings in patients with proven COVID-19 infection and presenting with cardiac problems both at presentation and in convalescence from a tertiary care center, in North India. A pertinent review of the literature is also discussed.
Materials and Methods:
Retrospective analysis of patients with real-time reverse transcriptase-polymerase chain reaction proven COVID-19 infection either at presentation or convalescence referred for CMR at our facility from January 2021 to December 2023 was done. CMR was performed on a 3T system (Ingenia, Philips Healthcare, Best, The Netherlands) and examinations were customized according to the clinical indications.
Results:
Retrospective analysis yielded 14 patients (4 at presentation; 10 in convalescence). Patients at presentation 4/14 had clinically presented with chest pain with raised troponins and electrographic abnormalities, while 10/14 patients had presented with clinical features of heart failure with two-dimensional transthoracic echocardiography demonstrating systolic dysfunction with reduced left ventricular ejection fraction. Out of 14, 4 patients at presentation, CMR showed features of acute myocarditis in three patients, while one had inferior wall myocardial infarction (MI) (this patient on catheter angiogram had aneurysmally dilated coronary arteries with thrombus and stenosis in the mid right coronary artery which was successfully stented). Out of 14, 10 patients on CMR had features of dilated cardiomyopathy (DCMP).
Conclusion:
Cardiac involvement in COVID-19 can have vivid clinicoradiological presentations with features of myocarditis and MI at presentation or DCMP in convalescence. CMR in such cases is a problem-solving tool where myocarditis is candidly differentiated from MI. Moreover, follow-up CMR demonstrates temporal changes in COVID-19-associated myocarditis and evaluation of cardiac structure and function in patients presenting with DCMP.
Keywords: Acute coronary syndrome, cardiovascular complications of COVID-19, cardiac magnetic resonance imaging, coronary artery aneurysm, myocarditis, myocardial infarction
INTRODUCTION
COVID-19 infection usually begins with a respiratory tract infection, however can have multisystemic involvement, including the cardiovascular system. COVID-19 patients with pre-existing cardiac comorbidities have an increased risk of developing acute myocardial damage.[1,2] Myocardial injury, stress-induced cardiomyopathy, pericardial inflammation, and acute coronary syndrome are the major cardiovascular complications of COVID-19.[1,2,3,4] Various imaging modalities including, transthoracic echocardiography (TTE), computed tomography coronary angiography (CTCA), cardiac magnetic resonance imaging (CMR), and conventional catheter coronary angiography (CCA) help in the diagnosis and management of these complications with TTE being the initial imaging modality of choice. CMR provides improved tissue characterization and serves as an indispensable imaging modality for the evaluation of myocardial inflammatory changes in these patients.[1,4] In this study, we report multimodality cardiac imaging findings in COVID-19 patients from our institution with a spectrum of imaging findings on CMR.
MATERIALS AND METHODS
CMR cases of proven COVID-19 infection with real-time reverse transcriptase-polymerase chain reaction either at presentation or in convalescence referred for CMR at our facility from January 2021 to December 2023 were retrieved from our system and analyzed.
All CMR examinations were performed on a 3T system (Ingenia, Philips Healthcare, Best, The Netherlands) and examinations were customized according to the clinical indications. For suspected myocarditis short-tau-inversion-recovery (STIR) sequences were performed in three planes (horizontal and vertical long axis-single slice and short axis-three slices-base, mid cavity, and apex) in addition to cine and late gadolinium enhancement (LGE) imaging.
Ethical approval was obtained from the institute ethics committee and department publication review board.
RESULTS
The retrospective analysis yielded 14 patients who underwent CMR examination during the study period with a mean age of presentation (36 ± 18 years). Four patients were scanned at presentation while 10 were in convalescence (mean duration 18 ± 3 months). Patients at presentation 4/14 had clinically presented with chest pain with raised troponins and electrographic abnormalities. 10/14 patients in convalescence had presented with clinical features of heart failure (progressive shortness of breath, weakness or swelling of feet, and/or rhythm abnormalities with two-dimensional transthoracic echocardiography demonstrating systolic dysfunction with reduced left ventricular ejection fraction. 4/14 patients [Table 1] at presentation: on CMR, three had features of acute myocarditis (raised signal intensity on STIR sequences with areas of typical subepicardial predominant LGE) [Figure 1] while one had inferior wall myocardial infarction (MI) (this patient on catheter angiogram had aneurysmally dilated coronary arteries with thrombus in the proximal segment and stenosis in mid-segment of the right coronary artery which was successfully treated with angioplasty and placement of stent) [Figures 2 and 3]. Out of 14, 10 patients in convalescence: on CMR had features of dilated cardiomyopathy (DCMP) (compromised left ventricular ejection fraction with global hypokinesia and thinned out LV walls, No LGE).
Table 1.
Details of cardiac magnetic resonance imaging finding in patients at presentation
| Age/sex | STIR abnormalities | Wall motion abnormalities and function (EF) | LGE |
|---|---|---|---|
| 18/male | Confluent hyperintensities in lateral wall, apex, and infero-septum | Mild hypokinesis in lateral wall, infero-septum, and apex EF - 51% | Patches of mid-myocardial enhancement co-localizing to areas of STIR hyperintensities (thick arrows) and papillary muscle |
| 22/male | Patchy hyperintense signal in lateral wall (base and mid-cavity) | Global hypokinesis; more pronounced in lateral walls EF - 39% | Epicardial in anterolateral and inferolateral segments in base and mid cavity |
| 32/male | Foci of hyperintense signal in lateral wall (base and mid-cavity) | Regional wall motion abnormalities (hypokinesis) along lateral walls EF - 62% | Epicardial and mid myocardial in anterolateral and inferolateral segments in base and mid cavity |
| 43/male | Normal signal | Regional wall motion abnormalities (hypokinesis) in inferior walls (base to apex) (45) | Transmural LGE in inferior segments (4, 9, 15). Sub-endocardial infarction in basal antero-septum |
EF: Ejection fraction, STIR: Short-tau-inverse-recovery, LGE: Late gadolinium enhancement
Figure 1.
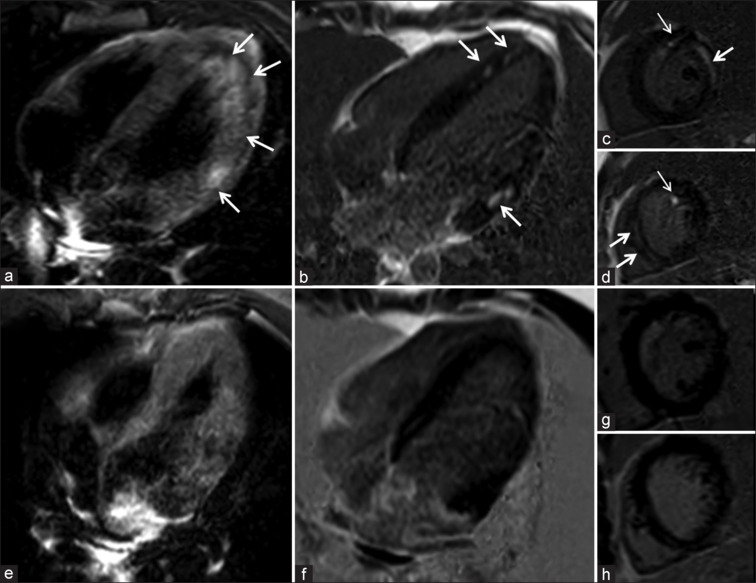
P1-A 14-year-old male patient with COVID-19 presented with sudden onset chest pain warranting admission to the emergency department. Electrographic-suggested inferior wall myocardial infarction requiring emergent catheter coronary angiography (CAA). CAA was unremarkable. Troponin levels were 4500 ng/L) a). Cardiac magnetic resonance imaging (CMR)-short-tau-inversion-recovery (STIR) horizontal long axis image shows confluent hyperintensities in LV lateral wall, apex, inferoseptum (arrows), (b-d) late gadolinium enhancement (LGE) horizontal long axis and short axis mid cavity and apex shows patches of mid myocardial enhancement co-localizing to areas of STIR hyperintensities (thick arrows). Note LGE in papillary muscle (thin arrows). Follow-up CMR images (e) STIR and LGE images (f-h) show complete resolution of abnormalities
Figure 2.
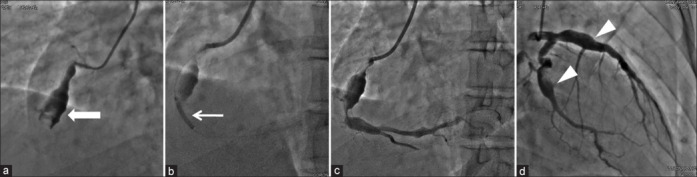
P4-45-year-old COVID-19-positive male patient presented with acute chest pain with STEMI-like presentation to the emergency department. ECG-was suggestive of inferior wall myocardial infarction requiring urgent catheter coronary angiography (CAA). CAA images show fusiform aneurysms of coronary arteries (a-d). Mid right coronary artery shows thrombotic occlusion with stenotic lesion distally (a). Percutaneous angioplasty with stenting was done (b and c)
Figure 3.
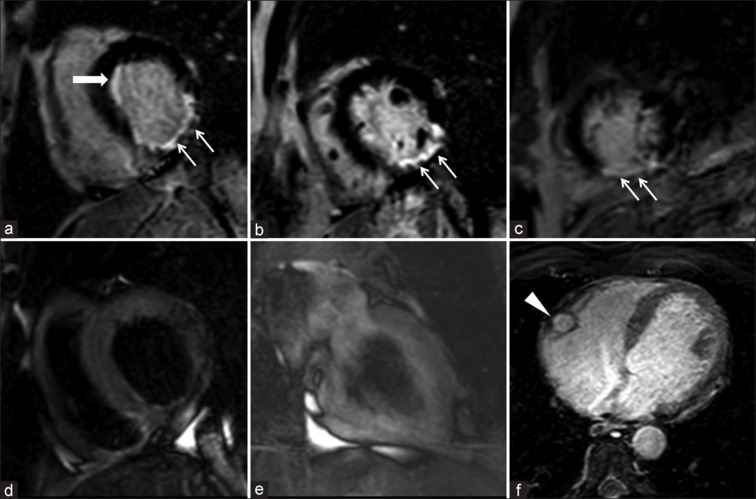
P4: Cardiac magnetic resonance imaging late gadolinium enhancement (LGE) images (a-c-short axis base to apex) show transmural LGE in segments 4, 9, 15 (thin arrows). Note sub-endocardial infarction in basal antero-septum (a-thick arrow) short-tau-inversion-recovery images (d and e) show normal signal. Note dilated mid right coronary artery on SFFP image (f)
DISCUSSION
Cardiovascular complications of COVID-19 generally include myocarditis, pericarditis, stress-induced cardiomyopathy, heart failure, acute coronary syndrome, arrhythmia, and thromboembolism.[1,4] Virus-induced cytotoxicity, endothelial injury, dysregulation of renin-angiotensin-system (RAS), and increased thrombo-inflammatory response are the pathological processes triggering cardiovascular manifestations in COVID-19.[1,5] Clinical presentation is varied and can be nonspecific. Complaints such as atypical chest pain, palpitations, worsening of dyspnea, and/or new onset of arrhythmias in acute COVID-19 patients give important clues of cardiac involvement.[1,4] In addition, elevated blood troponin levels act as an indicator of myocardial injury.[1,2,4]
Imaging plays an important role in the diagnostic workup of these patients. TTE, cardiac CT including CTCA and CT angiography thorax, CMR, and CCA are the imaging tools for evaluation of cardiac complications.[1,4,6,7,8] TTE serves as an initial work-up tool for the assessment of cardiac structure and function. CMR has the added advantage of being noninvasive, and radiation free with improved tissue characterization properties for the evaluation of myocardial injury as well as differentiating myocarditis from MI.[1,7] Findings on TTE include wall motion abnormalities, ventricular dysfunction, valve regurgitation, intracardiac thrombus, cardiac chamber dilatation, and pericardial effusion.[1,6,8] CMR in COVID-19-induced acute myocarditis may show diffuse myocardial edema on STIR sequences, the characteristic noninfarct pattern of enhancement on LGE sequences, reduced biventricular function, and increased values on T1 and T2 mapping sequences.[1,4,6,9]
CMR in cases of MI may show regional wall motion abnormalities along the affected coronary territory, myocardial edema (in cases of acute MI), myocardial thinning (in cases of chronic MI), perfusion deficits, and characteristic subendocardial or transmural LGE along affected vascular territorial distribution. Moreover, CMR also provides important information regarding various prognostic indicators for risk stratification including scar burden, peri-infarct ischemia, microvascular obstruction, and hemorrhage. CTCA and CCA also guide in evaluating the specific coronary involvement and its extent with endovascular management using CCA.[1,6,7,10] Likewise, global hypokinesia and dilated cardiac chambers with markedly compromised ventricular function with or without intracardiac thrombus are seen in patients with DCMP on TTE and CMR. Pericardial inflammation is seen as pericardial thickening with enhancement and pericardial effusion on CMR.[1,4,9] In COVID-19 patients with arrhythmia, CMR can be used in evaluating for any structural abnormalities such as myocardial edema, ischemia, or fibrosis.[1,3,6] A prospective multicenter CMR study in COVID-19-recovered patients showed normalized LV function in 89%, myocarditis-like scar in 26%, infarction and/or ischemia in 22%, and dual pathology in 6% of the study subjects.[11]
In addition to myocarditis, a literature search showed very few cases reporting the presence of coronary artery dilatation in patients who recovered from COVID-19 or who had COVID-19 antibodies.[12,13] Further, coronary aneurysms can lead to thrombosis secondary to stasis and endothelial injury and contribute to acute coronary syndrome. Acute coronary syndrome in COVID-19 occurs secondary to plaque rupture or coronary thrombosis.[1,4,10] While plaque rupture is due to an incited systemic inflammatory response and catecholamine surge, coronary thrombosis occurs due to the hypercoagulable state of COVID-19.[4,10,12] Literature also provides some insights into MI with nonobstructive coronary arteries in COVID-19 patients which may occur due to dysregulated RAS and cytokine storm leading to an imbalance between oxygen supply and demand. There have been few case reports of DCMP in COVID-19.[8,14] The persistent immune activation by the virus increases the risk of developing DCMP in such patients.[15]
Thus, there can be varied presentations of cardiovascular complications in COVID-19. Imaging modalities have a definite role in evaluating these complications with CMR acting as a problem-solving tool. Moreover, follow-up imaging using CMR provides important information regarding temporal changes in COVID-19-associated myocarditis and evaluation of cardiac structure and function in patients presenting with DCMP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nakou E, De Garate E, Liang K, Williams M, Pennell DJ, Bucciarelli-Ducci C. Imaging findings of COVID-19-related cardiovascular complications. Card Electrophysiol Clin. 2022;14:79–93. doi: 10.1016/j.ccep.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5:751–3. doi: 10.1001/jamacardio.2020.1105. [DOI] [PubMed] [Google Scholar]
- 3.Luetkens JA, Isaak A, Öztürk C, Mesropyan N, Monin M, Schlabe S, et al. Cardiac MRI in suspected acute COVID-19 myocarditis. Radiol Cardiothorac Imaging. 2021;3:e200628. doi: 10.1148/ryct.2021200628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basu-Ray I, Almaddah NK, Adeboye A, Vaqar S, Soos MP. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. Cardiac Manifestations of Coronavirus (COVID-19) [PubMed] [Google Scholar]
- 5.Domingo P, Mur I, Pomar V, Corominas H, Casademont J, de Benito N. The four horsemen of a viral apocalypse: The pathogenesis of SARS-CoV-2 infection (COVID-19) EBioMedicine. 2020;58:102887. doi: 10.1016/j.ebiom.2020.102887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catapano F, Marchitelli L, Cundari G, Cilia F, Mancuso G, Pambianchi G, et al. Role of advanced imaging in COVID-19 cardiovascular complications. Insights Imaging. 2021;12:28. doi: 10.1186/s13244-021-00973-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76:2043–55. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Omidi F, Hajikhani B, Kazemi SN, Tajbakhsh A, Riazi S, Mirsaeidi M, et al. COVID-19 and cardiomyopathy: A systematic review. Front Cardiovasc Med. 2021;8:695206. doi: 10.3389/fcvm.2021.695206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demirkiran A, Everaars H, Amier RP, Beijnink C, Bom MJ, Götte MJ, et al. Cardiovascular magnetic resonance techniques for tissue characterization after acute myocardial injury. Eur Heart J Cardiovasc Imaging. 2019;20:723–34. doi: 10.1093/ehjci/jez094. [DOI] [PubMed] [Google Scholar]
- 10.Bermejo-Martin JF, Almansa R, Torres A, González-Rivera M, Kelvin DJ. COVID-19 as a cardiovascular disease: The potential role of chronic endothelial dysfunction. Cardiovasc Res. 2020;116:e132–3. doi: 10.1093/cvr/cvaa140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866–78. doi: 10.1093/eurheartj/ehab075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khalid A, Patel N, Yusuf Ally Z, Ehsan S. Incidental finding of coronary artery dilatation in children with history of COVID-19 having minimal or no symptoms: Raising red flag. Cureus. 2022;14:e24348. doi: 10.7759/cureus.24348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerber N, Flynn PA, Holzer RJ. Coronary artery dilation in an asymptomatic pediatric patient with COVID19 antibodies. Pediatr Cardiol. 2021;42:460–2. doi: 10.1007/s00246-021-02566-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kishore R, Choudekar A, Xess AB, Dar L, Anand RK, Saxena A, et al. Dilated cardiomyopathy in a child with COVID-19. Indian J Pediatr. 2021;88:278–9. doi: 10.1007/s12098-020-03524-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komiyama M, Hasegawa K, Matsumori A. Dilated cardiomyopathy risk in patients with coronavirus disease 2019: How to identify and characterise it early? Eur Cardiol. 2020;15:e49. doi: 10.15420/ecr.2020.17. [DOI] [PMC free article] [PubMed] [Google Scholar]


