Abstract
Background and study aims Endoscopic sphincterotomy can be challenging especially in patients with surgically altered anatomy. Although a rotatable sphincterotome (r-sphincterotome) may be useful, its rotational function is often inadequate. We evaluated the feasibility of a newly designed r-sphincterotome equipped with a well-conceived cutting wire.
Methods We measured the movement and dynamics of both the newly designed r-sphincterotome and two existing r-sphincterotomes using in-house equipment. Ideally, the rotational force exerted at the proximal end should transmit directly to the distal end. But it is often challenging, particularly within the constraints of a bent endoscope and working channel. We collected data regarding deviation from the ideal value 10 times for each sphincterotome.
Results The deviation from the ideal value was significantly lower with the newly designed r-sphincterotome than with the conventional r-sphincterotomes (44.9 ± 27.8 vs. 73.7 ± 44.6 and 130.1 ± 71.4 degrees, respectively; P < 0.001). The newly designed r-sphincterotome rotated smoothly and consistently at a constant speed, mirroring the input rotation.
Conclusions We evaluated the feasibility of the newly designed r-sphincterotome using an experimental model. We believe that the findings from these experiments may contribute to easier and more precise sphincterotomies.
Keywords: Pancreatobiliary (ERCP/PTCD), ERC topics, Quality and logistical aspects, Training, Quality management, Performance and complications
Introduction
Endoscopic sphincterotomy is the cornerstone of therapeutic endoscopic retrograde cholangiopancreatography (ERCP), enabling access to the biliary and pancreatic ductal systems. A sphincterotome is generally used for this purpose, and various types are commercially available. The pull type, which facilitates incisions by pushing the cutting wire, is commonly selected 1 . Among the various types of sphincterotomes, one is equipped with a rotational function 2 . However, clear evidence of its effectiveness remains elusive. The primary reason for the limited use of sphincterotomes with rotational function in patients with normal anatomy is that experienced professionals can perform precise curved incisions by manually pulling the cutting wire and manipulating the therapeutic duodenoscope. However, endoscopic sphincterotomy poses difficulties in patients with surgically altered anatomy, such as those who have undergone Billroth II and Roux-en-Y reconstructions. Although ERCP experts can access the papilla in 85% to 95% of these cases 3 4 5 by using balloon-assisted enteroscopy, performing endoscopic sphincterotomy as intended is challenging because the direction of the scope and cutting wire against the papilla is inconsistent.
Because of its difficulty, endoscopic balloon dilation is sometimes chosen by default. In a randomized controlled trial (RCT) by Bergman et al. 6 comparing sphincterotomy and balloon dilation in patients with Billroth II reconstruction, no difference was observed in procedure time or incidence of early adverse events (AEs). However, previous RCTs 7 8 9 10 comparing sphincterotomy and balloon dilation revealed a higher incidence of post-ERCP pancreatitis in balloon dilation and more severe bleeding in sphincterotomy. In a multicenter clinical trial in the United States 10 , post-ERCP pancreatitis occurred in 15.4% of patients who underwent common bile duct (CBD) stone removal with balloon dilation, including two (1.7%) deaths; however, pancreatitis occurred in only 0.8% of those who underwent sphincterotomy ( P < 0.001). Based on these findings, sphincterotomy has become the preferred method for stone extraction in recent years.
If sphincterotomy is considered safe and appropriate even in difficult cases, clinicians will likely choose this procedure. An endoscopic rotatable sphincterotome (r-sphincterotome) may be useful for these patients. To the best of our knowledge, two r-sphincterotomes are currently available. However, their rotational function is inadequate, and they are not widely used, even for patients with surgically altered anatomy. In our experience, these r-sphincterotomes do not adequately rotate under the condition of a bent endoscope. A sphincterotome consists of an operating handle, catheter, and cutting wire. The cutting wire is tapered at its distal end for proper incision. The torque caused by rotating the operating handle (proximal rotational force) may not always be transmitted to the distal side through the catheter.
To address this issue, a novel r-sphincterotome (AIMINGTOME; Asahi Intecc Co., Ltd., Aichi, Japan) with a newly devised cutting wire has been developed. The aim of this study was to compare the feasibility of this novel r-sphincterotome (“N”) with that of the two existing r-sphincterotomes (“A” and “B”) in an experimental model.
Methods
Experimental procedure
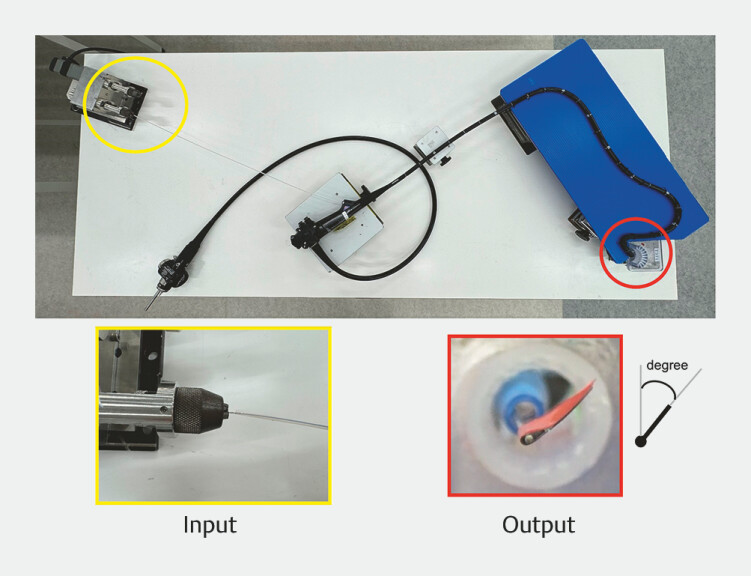
Fig. 1 shows an actual model of the experimental procedure and the input and output degrees of the r-sphincterotomes evaluated in this study. As in clinical treatment, the r-sphincterotome was inserted into a side-viewing duodenoscope (TJF290V; Olympus Medical Systems, Tokyo, Japan). The proximal end of the r-sphincterotome was attached to a servomotor (XU8 K112501; Oriental Motor, Tokyo, Japan), which rotated the sphincterotome at a constant speed. The duodenoscope was manipulated to mimic the curvature of the alimentary tract. With the r-sphincterotome inserted into the duodenoscope, it was rotated at a constant speed (input; 1.5 revolutions per minute) for three complete rotations, while the degree of rotation at the distal end was recorded over time (output; every 2 seconds). Ideal rotation of the sphincterotome was defined as input rotation directly reflecting output in a uniform manner (i.e. rotation in one-to-one correspondence). Deviations from the expected ideal rotation that collected integral value from the base axis were noted. Each measurement was conducted 10 times for each r-sphincterotome.
Fig. 1.
An actual model of the experimental procedure show input and output degrees of the r-sphincterotomes evaluated in this study. The r-sphincterotome was inserted into a side-viewing duodenoscope, that was manipulated to mimic the curvature of the alimentary tract. The proximal end of the r-sphincterotome was attached to a servomotor, which rotated the sphincterotome at a constant speed (input; 1.5 revolution per minute), while the degree of rotation at the distal end was recorded over time (output; every 2 seconds).
Actual endoscopic r-sphincterotomes and cutting wires
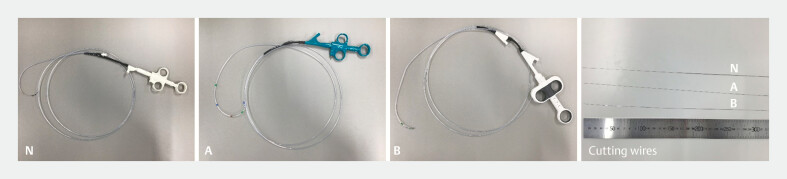
Fig. 2 shows the actual r-sphincterotomes and cutting wires of the r-sphincterotomes. Table 1 summarizes detailed information about the cutting wire and the manufacturers of each sample.
Fig. 2.
The actual r-sphincterotomes and cutting wires of the r-sphincterotomes.
Table 1 Detailed information about the cutting wire for each device.
| Distal diameter, mm | Length of tapered area, mm | Proximal diameter, mm | Manufacturer | |
| All the devices were made of stainless steel. | ||||
| N | 0.21 | 125 | 0.64 | Asahi Intecc |
| A | 0.26 | 270 | 0.45 | Boston Scientific Corporation |
| B | 0.26 | 175 | 0.45 | Micro-Tech |
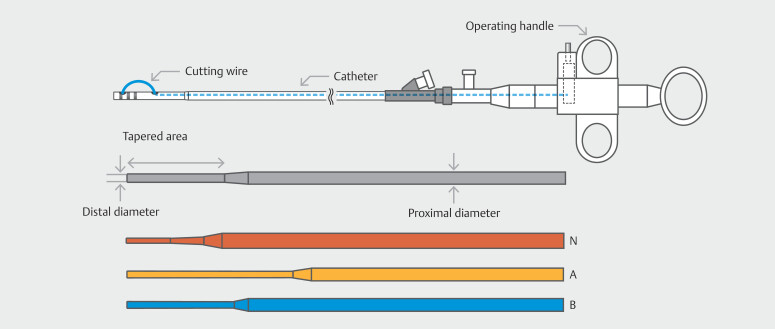
The proximal diameter of the cutting wire for the newly designed r-sphincterotome was thicker than that of the others (N vs. A/B: 0.64 vs. 0.45 mm), whereas the distal end was thinner (0.21 vs. 0.26 mm). The length of the tapered area of the cutting wire was shorter in the newly designed r-sphincterotome ( Table 1 and Fig. 3 ). The material used for each inner structure device was stainless steel.
Fig. 3.
Components of the endoscopic rotatable sphincterotome and comparison of cutting wire configurations. The sphincterotome consists of an operating handle, a catheter, and a cutting wire. The cutting wire is tapered at its distal end to facilitate proper incision. The length of the tapered area and the proximal and distal diameters of the cutting wire are unique to each sphincterotome.
Statistical analysis
Data are expressed as the mean ± 2 × standard error. Differences in quantitative data were compared using the Mann–Whitney U test. All statistical analyses were two-sided, and statistical significance was defined as P < 0.05. All statistical analyses were performed using SPSS software, version 23 (IBM Corp., Armonk, New York, United States).
Results
Measurement of degree of endoscopic r-sphincterotomes
Feasibility of newly designed rotatable sphincterotome for endoscopic sphincterotomy.
Video 1
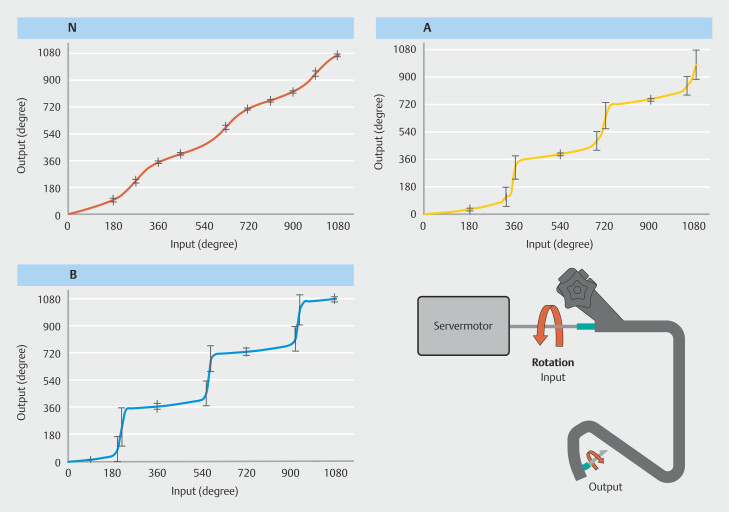
Fig. 4 summarizes the input and output degrees of the r-sphincterotomes during rotation with the servomotor. Deviation from the ideal value was significantly lower in the newly designed r-sphincterotome than in the conventional ones (N vs. A: 44.9 ± 27.8 vs. 73.7 ± 44.6, P < 0.001; N vs. B: 44.9 ± 27.8 vs. 130.1 ± 71.4 degrees, P < 0.001). Video 1 demonstrates the actual movement of each r-sphincterotome. The newly designed r-sphincterotome rotated in the same manner as the input rotation, smoothly and at a constant speed.
Fig. 4.
Schema illustrating the relationship between input and output degrees of the experimental procedure. The endoscopic rotatable sphincterotome was inserted into a side-viewing duodenoscope. The proximal end of the sphincterotome was fastened to a servomotor, which rotated the sphincterotome at a constant speed (input). The duodenoscope was held in a bent position to mimic the alimentary tract. The degree of rotation at the distal end over time was recorded (output).
Discussion
The present experimental study demonstrated that use of the novel r-sphincterotome was feasible and exhibited excellent rotational function. Although the rotational function of a sphincterotome is not always necessary for ERCP experts treating patients with normal anatomy, it might be useful for patients with surgically altered anatomy. This newly designed r-sphincterotome may change the current paradigm and represent a new era in endoscopic sphincterotomy.
Endoscopic sphincterotomy is performed to treat various pancreatobiliary diseases, such as CBD stones, cholangitis, and obstructive jaundice. For biliary sphincterotomy, many experts recommend cutting against the papilla in the 11- to 12-o'clock direction, which provides clean and bloodless opening of the sphincter of Oddi 1 11 12 . However, in some patients with surgically altered anatomy, the papilla cannot be reached using the same therapeutic duodenoscope. Furthermore, even when access to the papilla is possible, the view does not originate from the same direction, resulting in an unfeasible position for precise sphincterotomy. Surgically altered anatomy is broadly classified as Billroth I reconstruction, jejunal interposition, Billroth II reconstruction, and Roux-en-Y reconstruction. In cases of Billroth I reconstruction and jejunal interposition, endoscopic sphincterotomy can be performed in almost the same manner as in patients with normal anatomy using a therapeutic duodenoscope. However, in cases of Billroth II reconstruction and Roux-en-Y reconstruction, the procedure cannot be executed in the same manner. The main reason for this difficulty, as mentioned above, is the altered orientation. Unconventional endoscopic sphincterotomy may cause unexpected AEs such as hemorrhage and/or perforation, even when performed by experts. Furthermore, under technically challenging conditions, hemostasis or stent placement becomes more difficult.
A sphincterotome with rotational function may facilitate an appropriate cutting incision and rescue treatment. However, previously designed r-sphincterotomes could not rotate through a bent endoscope. Whether the cutting wire rotates as intended by the clinician depends on how the rotational force is directly transmitted from the operating handle (proximal side) to the distal end. The cutting wire of the newly designed r-sphincterotome consists of a thick proximal side and a short distal end, which easily transmits the rotational force. This novel r-sphincterotome is equipped with a well-conceived cutting wire that uniformly transmits the rotational force from the proximal to the distal end (as shown in Video 1). If the rotational force is not transmitted uniformly, the force retained in the cutting wire can cause twisted rotation in an unintended direction or wire breakage. Ideally, the rotational force on the proximal side should be transmitted directly to the distal end. However, achieving this ideal condition is challenging, particularly within the constraints of a bent endoscope and working channel. As depicted in Fig. 4, the newly designed r-sphincterotome reflects the input rotation to output with higher accuracy and precision compared with previous r-sphincterotomes ( P < 0.001).
A limitation of this study is that all measurements were performed in vitro using laboratory equipment. In addition, because the study was conducted under strictly defined conditions, the numeric data may not represent absolute values; rather, they serve as useful relative values. A large-scale, multicenter, prospective study under various clinical conditions is necessary to establish the practicality of the r-sphincterotome.
Conclusions
In conclusion, we evaluated the feasibility of the newly designed r-sphincterotome using an experimental model. We believe that the findings from these experiments may contribute to easier and more precise endoscopic sphincterotomy.
Acknowledgement
We are indebted to Toshiaki Wakisaka, Shinichi Tanisaka, Tomoki Kosugi, and Mikio Terauchi for providing technical assistance with the engineering analysis.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Ryozawa S, Itoi T, Katanuma A et al. Japan Gastroenterological Endoscopy Society guidelines for endoscopic sphincterotomy. Dig Endosc. 2018;30:149–173. doi: 10.1111/den.13001. [DOI] [PubMed] [Google Scholar]
- 2.Kurita A, Kudo Y, Yoshimura K et al. Comparison between a rotatable sphincterotome and a conventional sphincterotome for selective bile duct cannulation. Endoscopy. 2019;51:852–857. doi: 10.1055/a-0835-5900. [DOI] [PubMed] [Google Scholar]
- 3.Bedogni G, Bertoni G, Contini S et al. Endoscopic sphincterotomy in patients with Billroth II partial gastrectomy: comparison of three different techniques. Gastrointest Endosc. 1984;30:300–304. doi: 10.1016/s0016-5107(84)72425-4. [DOI] [PubMed] [Google Scholar]
- 4.Shimatani M, Matsushita M, Takaoka M et al. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849–854. doi: 10.1055/s-0029-1215108. [DOI] [PubMed] [Google Scholar]
- 5.Hori Y, Naitoh I, Miyabe K et al. Simultaneous side-by-side bilateral metal stent placement using a colonoscope in a patient with Billroth II reconstruction. Endoscopy. 2018;50:E218–E219. doi: 10.1055/a-0624-1947. [DOI] [PubMed] [Google Scholar]
- 6.Bergman JJ, van Berkel AM, Bruno MJ et al. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19–26. doi: 10.1067/mge.2001.110454. [DOI] [PubMed] [Google Scholar]
- 7.Bergman JJ, Rauws EA, Fockens P et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124–1129. doi: 10.1016/S0140-6736(96)11026-6. [DOI] [PubMed] [Google Scholar]
- 8.Vlavianos P, Chopra K, Mandalia S et al. Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut. 2003;52:1165–1169. doi: 10.1136/gut.52.8.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujita N, Maguchi H, Komatsu Y et al. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151–155. doi: 10.1067/mge.2003.56. [DOI] [PubMed] [Google Scholar]
- 10.Disario JA, Freeman ML, Bjorkman DJ et al. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291–1299. doi: 10.1053/j.gastro.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 11.Maydeo A, Borkar D. Techniques of selective cannulation and sphincterotomy. Endoscopy. 2003;35:S19–S23. doi: 10.1055/s-2003-41532. [DOI] [PubMed] [Google Scholar]
- 12.Mirjalili SA, Stringer MD. The arterial supply of the major duodenal papilla and its relevance to endoscopic sphincterotomy. Endoscopy. 2011;43:307–311. doi: 10.1055/s-0030-1256229. [DOI] [PubMed] [Google Scholar]