Abstract
Objective:
China has been undergoing a rapid nutrition transition in the past few decades. This review aims to characterise commonly reported dietary patterns in Chinese populations and their associations with health outcomes.
Design:
We searched PubMed, Embase and CNKI from inception to June 2020 to identify observational studies reporting dietary patterns or the associations between dietary patterns and health outcomes. Information regarding dietary patterns, their association with health outcomes and other related items was collected.
Setting:
Chinese population and Chinese immigrants.
Participants:
Not applicable.
Results:
Results from 130 studies with over 900 000 participants were included. Six dietary patterns were identified: traditional whole-grain diet (Traditional WG), traditional non-whole-grain diet (Traditional NWG), plant-based diet (Plant-based), animal food diet (Animal-food), Western energy-dense diet (Western) and other unclassified diets (Unclassified). The Plant-based diet was associated with a reduced risk of CVD and cancer from prospective studies, reduced risk of diabetes, hypertension, cognitive impairment and depressive symptoms from all study designs. The Traditional WG diet was associated with a reduced risk of diabetes and hypertension. Animal-food diet is associated with a range of metabolic diseases, and Western diet was associated with increased risks of obesity and depressive symptoms.
Conclusion:
Multiple dietary patterns identified reflect the diversity and transitioning of the Chinese diet. A healthy Chinese diet, comprising both the Traditional WG and Plant-based diets, was associated with reduced risks of specific undesirable health outcomes. Promoting this healthy diet will improve public health among the Chinese populations.
Keywords: Chinese diets, Dietary pattern, CVD, Cancer, Metabolic syndrome, Systematic review and meta-analysis
The Chinese diet has evolved over thousands of years, influenced by the country’s vast geography, numerous ethnic groups and rich cultural history. The traditional Chinese diet comprises cereals and vegetables with few animal foods and is considered to be healthful when adequate intake levels are achieved(1,2). Since the 1950s, China has been undergoing a nutrition transition towards a more westernised diet in parallel with rapid socio-economic and demographic changes(3–5). This transition has helped overcome food scarcity and improve the nutritional status of the Chinese population over the past few decades(5,6), but it has also led to unhealthy outcomes(7,8). Evidence from the Cornell China Study, one of the most comprehensive nutrition studies conducted in the 1980s(9), shows that counties in China with higher animal-based food consumption were more likely to have had higher death rates from Western diseases than those with higher plant-based food consumption(1). The burden of chronic diseases has been increasing rapidly in China. From 1990 to 2010, the age-standardised mortality of diabetes mellitus and ischaemic heart disease increased by 52·3 % and 31·6 %, respectively(7,10). It was estimated that dietary risk factors (mainly diets low in fruits, vegetables, whole grains, and nuts and high in Na) accounted for 16·3 % of this increase(7,10). Thus, an update on the characterisation of the Chinese diet to define beneficial and detrimental components is necessary for policymakers and public health professionals to provide up-to-date dietary advice to revert undesirable dietary transitions in developing countries similar to that in China(11–14).
In nutritional epidemiology, it is often preferable to estimate adherence to a certain dietary pattern (e.g. the Mediterranean diet) than to analyse the individual dietary components in relation to the population’s health status(15). This is because people do not consume isolated nutrients or single foods, and different nutrients and foods interact with each other(15). Therefore, dietary pattern analysis can provide more integrated dietary information to explore the associations with health outcomes.
China has a population of 1·4 billion as of 2018(16), and it is estimated that over 45 million people of Chinese ethnicity live in Southeast Asia, North America, Europe, Australia, Japan, South Korea and other countries(17). Chinese cuisine is highly diverse and is strongly related to geographic differences in agricultural practices and food availability, as well as ethnic and other cultural and socio-economic factors(18–23). Therefore, identifying an ‘overall’ or ‘unique’ dietary pattern for the Chinese population is neither feasible nor of particular interest. Instead, identifying common dietary patterns and summarising their key features would better characterise the Chinese diet. Many studies have reported on Chinese dietary patterns and their relationship with health outcomes in the last two decades. However, a systematic review and appraisal of published Chinese dietary pattern studies is lacking.
In this study, we performed a systematic review of the literature to characterise the dietary patterns among Chinese populations. In addition, we assessed the associations between the identified Chinese dietary patterns and health outcomes to characterise healthy Chinese dietary patterns.
Methods
Searches
We used three databases, Ovid Medline (https://ovidsp.ovid.com/), Embase (https://www.embase.com/home) and China National Knowledge Infrastructure (CNKI, https://cnki.net/), to find all published studies that used modelling techniques to identify dietary patterns in the Chinese population. Search terms included combinations of ‘diet*’ AND ‘pattern*’ AND (‘China’ OR ‘Chinese’) with specific terms including ‘food’, ‘intake’, ‘principal component*’, ‘PCA’, ‘factor*’, ‘FA’ and ‘cluster*’ for Medline and Embase. Similar terms in Chinese were used for CNKI. The databases were searched from inception until June 2020, and no language restrictions were set. The reference lists of identified studies and other literature sources, including Cochrane Database of Systematic Reviews, Google Scholar, were also searched.
Study inclusion and exclusion criteria
Studies that fulfilled the following a priori eligibility criteria were included: (a) original study, (b) used a FFQ or 24-h dietary recall, (c) Chinese population and (d) published in English or Chinese. The exclusion criteria were (a) non-original report, (b) study of individual foods or nutrients, (c) no dietary pattern reported and (d) study only of infant feeding. If more than one paper was published from the same study with identical dietary patterns and health outcomes, only the most recent paper was included.
Study selection
The initial literature search yielded 3047 records, of which 1839 duplicates were excluded. Of the remaining 1208 records, 1079 were excluded for the following reasons: unrelated reports or reviews; no dietary pattern reported; no healthy participants included; study of diets in non-human species; and no access to the full text. A total of 130 studies were included in the systematic review to summarise the major dietary patterns in the Chinese population(24–153). Another fifty-nine studies were excluded based on the following exclusion criteria: no health outcome reported (n 11); subset or duplicate of another study (n 2); health outcome without sufficient data (fewer than three studies for each outcome) (n 40); and non-cohort study for cancer and cardiovascular health outcomes (n 6). Ultimately, seventy-one studies were included in the meta-analysis to investigate the associations between identified dietary patterns and health outcomes (Fig. 1).
Fig. 1.
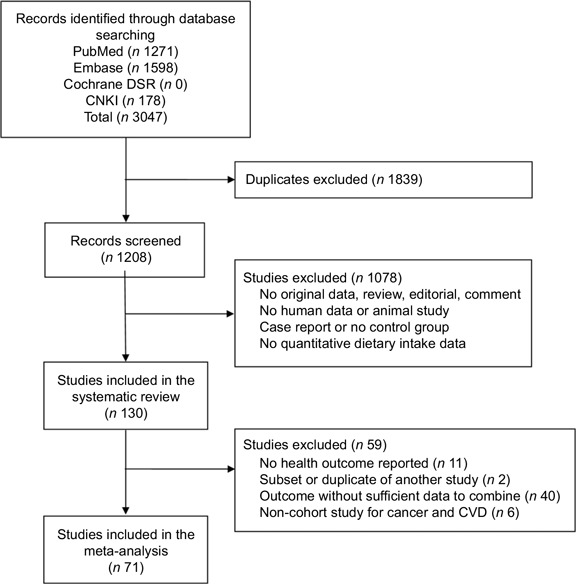
Flow chart describing the study selection process
Data extraction
X.F.H. conducted the search using the databases listed above. The data were initially extracted by R.Z. and were 100 % validated independently by another two team members (Y.Y.L. and C.Y.C.). Two databases were compiled separately for the review. One database contained the relevant characteristics of the included studies: authors, publication year, journal title, geographical area, years data were collected, study name and design if available, specific populations studied, sample size, dietary intake assessment methods, statistical methods, food groups or items used, reported dietary pattern names, percentage of the total variance of original food items explained by the dietary patterns (for studies using factor analysis or principal component analysis), statistical adjustments made in the analysis and any other relevant information about the study. The other database consisted of effect size measures between identified dietary patterns and health outcomes (OR, hazard ratio, relative risk (RR) or prevalence ratio) and their standard errors from the published data. Continuous outcomes (e.g. systolic blood pressure) were not included in the data extraction and synthesis.
Quality assessment of included studies
For studies reporting the association between dietary patterns and health outcomes, we assessed their quality with a modified nine-point version of the Newcastle–Ottawa scale (see online supplementary material, Supplemental Material 2), focusing on dietary assessment, dietary pattern identification and confounding control(154). Study quality was categorised as high (score ≥ 7), medium (score 5–6) or low (score ≤ 4).
Definition of dietary pattern categories
The classification of dietary patterns varied among the studies. Common methods included classification based on typical food groups (e.g. vegetables/fruits, meat, etc.)(29,34,83), time period or dietary transition (e.g. traditional, Western or modern)(53,110,121,133), associations with health (e.g. healthy)(89,93) or other characteristics (e.g. balanced, prudent, high protein, macho, condiment or beverage)(47,56,71,96). To better summarise the identified dietary patterns, we grouped them into the following six categories: traditional whole-grain diet (Traditional WG, with wheat and other cereals as staple foods), traditional non-whole-grain diet (Traditional NWG, with rice as the staple food), plant-based diet (Plant-based), animal food diet (Animal-food), Western energy-dense diet (Western) and unclassified diets (Unclassified, including all other diets). The re-classification of dietary patterns was kept minimal and only when deemed essential to facilitate the comparison and interpretation of results from different studies. The main re-classification divided the ‘traditional’ dietary pattern into either whole-grain or non-whole-grain, depending on whether relevant food items/groups (e.g. whole grains, coarse grains and other cereals) were reported as high factor-loading items for that dietary pattern. No dietary pattern was re-classified to either traditional pattern if the term was not used in the original study. A similar principle was applied to other dietary patterns. An additional ‘fruit-rich diet’ was named for one cohort study(29), which reported two plant-based dietary patterns (fruit-rich v. vegetable-rich) showing opposite associations with multiple health outcomes. The re-classification was performed independently by three team members (R.Z., Y.Y.L. and C.Y.C.), and any discrepancies were resolved by consensus or consulting with senior members (X.F.H. or H.M.C.). Dietary patterns were re-classified before the meta-analysis to avoid potential bias in analysing the associations between dietary patterns and health outcomes. The names of the original dietary patterns and the re-classified patterns for each study are presented in online supplementary material, Supplemental Material 1.
Data analysis
The association between a given dietary pattern and health outcome was analysed using an inverse-variance weighted random-effects model. Most of the included studies (61 out of 71) used factor analysis, principal component analysis or reduced rank regression to identify dietary patterns and reported their results in tertiles, quartiles or quintiles of dietary pattern scores (with intermediate categories omitted in some studies). These studies estimated the effect size by comparing the group with the highest dietary pattern scores (Q3, Q4 or Q5) to the group with the lowest dietary pattern scores (Q1). The remaining ten studies identified dietary patterns using cluster analysis, comparing the group with a dietary pattern of interest (e.g. Western) to the group with another dietary pattern (e.g. Traditional). Results from both types of studies were pooled together. Heterogeneity was quantified with the I 2 statistic(155). The relative influence of each study on the pooled estimates was determined by omitting one study at a time. Four sets of sensitivity analyses were conducted to investigate factors that may bias the associations between identified dietary patterns and health outcomes: (1) the dietary pattern identification method (studies using factor analysis or principle component analysis v. all studies), (2) study design (cohort studies v. cross-sectional studies), (3) participants’ age of included studies (studies with adult participants only v. all studies) and (4) combining the Plant-based diet and Traditional WG diet into a Chinese healthy diet (only Plant-based diet was included if both dietary patterns were reported in the same study).
The following health outcomes were summarised: CVD from cohort studies, including fatal and non-fatal stroke, acute myocardial infarction, and CHD; cancer from cohort studies, including fatal and non-fatal events; metabolic outcomes from all study designs, including type 2 diabetes, hypertension, general obesity (defined using BMI), abdominal obesity (defined using waist circumstance), cognitive impairment and depressive symptoms. Lipid disorders and gestational diabetes were reported as well. However, no synthesis was done due to an insufficient number of studies. Additional information about the Population, Intervention, Comparison, Outcomes and Study design criteria is available in Table S1 (see online supplementary material, Supplemental material 2).
The review protocol was registered in the Prospero database under the registration number: CRD42022321001. This review was conducted as per PRISMA 2020 guidelines (http://www.prisma-statement.org/PRISMAStatement).
Results
Study characteristics
The 130 studies included in the systematic review collected data from the Chinese population living in mainland China (n 19 for national or multiregional studies, n 83 for studies conducted in a single province or city), Hong Kong Special Administrative Region (SAR) (n 13), Macao SAR (n 1), Taiwan (n 4) and Singapore (n 7), as well as Chinese immigrants living in the USA and Malaysia (n 3) (Table 1, Fig. S1). Nine studies reported dietary data collected before 2000, sixty-three studies reported data collected between 2001 and 2010, and the remaining fifty-eight studies collected dietary data after 2011. One-third (n 43) of the included studies used a cohort design, 58 % (n 76) were cross-sectional studies and the rest were case–control studies (n 11). About 85 % of the studies (n 110) used an FFQ to assess dietary intake. Factor analysis or principal component analysis (n 108) were the most common methods used to derive dietary patterns. The longitudinal associations between dietary patterns and CVD were examined in six studies, and those with cancer were examined in another five. The most commonly investigated health outcomes were metabolic conditions, that is, diabetes (n 15), abdominal obesity (n 14), hypertension (n 14) and general obesity (n 9). An increasing number of studies reported cognitive and mental health outcomes after 2010 and gestational outcomes after 2015. Dietary patterns were identified using food groups in sixty-three studies and food items in the remaining studies (see online supplementary material, Supplemental Material 1). Researchers included 11–55 food groups and 33–280 food items. Ten studies focused on children (< 18 years old), seventeen studies reported on the elderly only (≥ 60 years old or average age over 60 years), and the remaining studies were conducted in adults. The sample size of included studies ranged from 130 to 481 242, and the total number of subjects in the included studies was 902 620. Results of the participants were included in multiple analyses of associations with health outcomes, with a total number of 2 076 893.
Table 1.
Characteristics of the studies included in the systematic review
| Characteristic | Study count |
|---|---|
| Region | |
| National and multiregional | 19 |
| Hong Kong SAR | 13 |
| Macao SAR | 1 |
| Taiwan | 4 |
| Single province in mainland China | 83 |
| Singapore | 7 |
| Chinese immigrants living in other countries | 3 |
| Study design | |
| Cohort | 43 |
| Cross-sectional | 76 |
| Case–control | 11 |
| Publication language | |
| English | 114 |
| Chinese | 16 |
| Dietary intake assessment method | |
| FFQ | 110 |
| 24-h recall * | 20 |
| Dietary pattern derivation method | |
| Factor analysis (principal component analysis) | 108 |
| Cluster analysis † | 14 |
| Reduced-rank regression | 7 |
| Structure equation | 1 |
| Dietary data collection period ‡ | |
| Before 2000 | 9 |
| 2001–2010 | 63 |
| After 2011 | 58 |
| Average dietary pattern identified | 3 |
| Health outcome included in meta-analysis § | |
| CVD | 6 |
| Cancer | 5 |
| Diabetes | 15 |
| Hypertension | 14 |
| General obesity | 9 |
| Abdominal obesity | 14 |
| Depressive symptoms | 5 |
| Cognitive impairment | 6 |
SAR, Special Administrative Region.
Four studies reported both FFQ and 24-h recall.
Ten studies used factor analysis and cluster analysis together.
Time of completion for multi-wave cohort studies.
Some studies reported multiple health outcomes.
Most studies provided adequate information on the selection of the study population, the methods used to assess dietary intake and derive dietary patterns, the ascertainment of health outcomes, and the statistical methods used to analyse the associations between dietary patterns and health outcomes. In total, 117 studies were assessed for quality, as thirteen studies only reported dietary patterns and did not investigate their relationship with health outcomes. Overall, 81·2 % of all studies assessed (95 out of 117) and 86·1 % of the studies included in the meta-analysis (62 out of 71) were rated as high quality. Papers published in Chinese were generally more concise, with fewer tables and supplementary materials. However, the methods used to assess dietary intake, derive dietary patterns and adjust for covariates were similar to those of the studies published in English.
Summary of dietary patterns
Of the seventy-nine studies reporting traditional Chinese dietary patterns, forty-six reported Traditional WG (featuring whole grains, wheat, fresh vegetables and fruits, legumes, soyabean and products), fifty-four reported Traditional NWG (featuring rice, fresh vegetables and pork) and twenty reported both (Tables 2 and 3). In addition, seventy-seven studies reported Plant-based (featuring fresh vegetables and fruits, legumes, soyabean and products, and mushrooms and fungi), eighty-three reported Animal-food (featuring red meat and processed meat) and eighty-eight reported Western (featuring soft drinks and snacks) diets. Finally, forty-six reported Unclassified diets, among which high-salt condiments and alcohol were the two most commonly reported groups.
Table 2.
Classified dietary patterns and most frequently reported food groups or items
| Dietary pattern | No. of studies | Food groups or items most frequently reported |
|---|---|---|
| Traditional whole-grain | 46 | Whole grains, coarse grains, wheat, other cereals, fresh vegetables, fresh fruits, legumes, soyabean and products, fish and seafood, tubers, nuts, tea |
| Traditional non-whole-grain | 54 | Rice, fresh vegetables, pork, poultry, fish |
| Plant-based | 77 | Fresh vegetables (dark green and leafy), fruits, legumes, soyabean and products, mushrooms and fungi, whole grains, coarse cereals, nuts, fish and seafood |
| Animal-food | 83 | Red meat (pork, beef and lamb), processed meat, poultry, organ meat, fish and seafood, egg, fat/oil |
| Western | 88 | Soft drink, juice, fast food, French fries/chips, milk and dairy products, cakes, snacks, desserts, processed products, alcohol |
| Unclassified * | 46 | Condiments, alcohol, and combinations of food groups or items that do not fit into the other defined patterns |
High-salt pattern (i.e. condiment pattern) and beverage pattern were the two main unclassified patterns.
Table 3.
Number of studies reporting the classified dietary patterns
| Traditional whole-grain | Traditional non-whole-grain | Plant-based | Animal-food | Western | Unclassified | |
|---|---|---|---|---|---|---|
| Traditional whole-grain | 20 | 13 | 20 | 35 | 20 | |
| Traditional non-whole-grain | 23 | 25 | 38 | 23 | ||
| Plant-based | 62 | 47 | 13 | |||
| Animal-food | 30 | 20 | ||||
| Western | 35 | |||||
| Unclassified |
One to six dietary patterns were reported per study, with an average of three. Plant-based and Animal-food diets were the most frequently reported in the same study (n 62), followed by Plant-based and Western (n 47). Traditional WG and Plant-based diets had similar lists of high factor-loading food groups or items and were the least likely to be identified in the same study (n 13). Among regions, studies conducted in Hong Kong SAR, Singapore and coastal regions like Shanghai and Tianjin were more likely to report Plant-based and Animal-food diets. In national and multiregional studies, traditional Chinese dietary patterns were often further categorised into traditional northern (wheat-based) and traditional southern (rice-based) diets. No clear temporal trend was observed in the reported dietary patterns. However, studies before 2015 were more likely to focus on diseases such as cancer, CVD and metabolic conditions. Recently, studies started to focus on mental health conditions and certain sub-populations, for example pregnant women.
Dietary patterns and health outcomes
Figure 2 shows the associations between dietary patterns, CVD, cancer and diabetes in cohort studies. The RR associated with the Plant-based diet was 0·85 (95 % CI 0·74, 0·97) for cancer and 0·78 (95 % CI 0·67, 0·92) for CVD. The Animal-food diet was associated with an increased risk of CVD (RR 1·16, 95 % CI 1·04, 1·31) and diabetes (RR 1·26, 95 % CI 1·12, 1·42). The Traditional NWG diet was associated with a decreased risk of diabetes with RR 0·76 (95 % CI 0·64, 0·91).
Fig. 2.
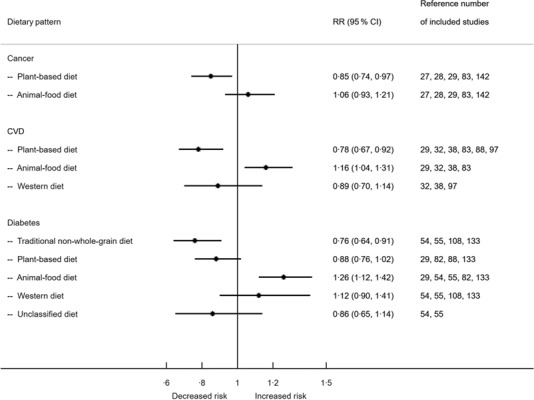
Associations between dietary patterns in Chinese population and CVD, cancer and diabetes from cohort studies. RR, relative risk.
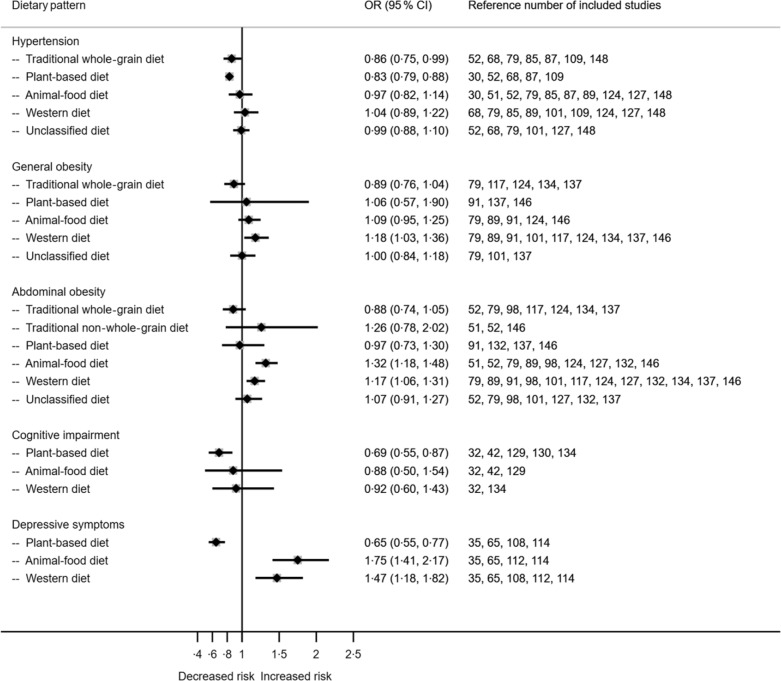
Figure 3 shows the associations between dietary patterns, selected metabolic and other health conditions from studies with both cohort and cross-sectional designs. Greater adherence to the Traditional WG diet resulted in decreased risk of hypertension (OR 0·86, 95 % CI 0·75, 0·99). Animal-food diet was associated with an increased risk of abdominal obesity (1·32, 95 % CI 1·18, 1·48). Meanwhile, the Western diet was associated with an increased risk of general obesity (OR 1·18, 95 % CI 1·03, 1·36) and abdominal obesity (OR 1·17, 95 % CI 1·06, 1·31). Adherence to the Plant-based diet was associated with a reduced risk of cognitive impairment (OR 0·69, 95 % CI 0·55, 0·87) and depressive symptoms (OR 0·65, 95 % CI 0·55, 0·77). Animal-food and Western diets were associated with increased risks of depressive symptoms (OR 1·75, 95 % CI 1·41, 2·17 and OR 1·47, 95 % CI 1·18, 1·82, respectively). Forest plots with more details for each outcome are provided in online supplementary material, Supplemental Fig. 6–13.
Fig. 3.
Associations between dietary patterns in the Chinese population and hypertension, general obesity, abdominal obesity, cognitive impairment and depressive symptoms.
Sensitivity analysis showed that the pooled estimates between dietary patterns and health outcomes were similar with or without studies using cluster analysis (see online supplementary material, Supplemental Fig. 2), with or without cross-sectional studies (see online supplementary material, Supplemental Fig. S3, for diabetes only), with or without participants aged 18 years or less (see online supplementary material, Supplemental Fig. 4), and with and without Plant-based diet and Traditional WG diet combined into one (see online supplementary material, Supplemental Fig. 5).
Discussion
This is the first systematic review and meta-analysis of Chinese dietary pattern studies, covering data collected from more than 900 000 participants living in mainland China, Hong Kong SAR, Macao SAR, Taiwan and Singapore, as well as Chinese immigrants living in the USA and Malaysia. The results of the systematic review have identified six commonly reported dietary patterns, including: (1) the Traditional WG diet (with wheat and other cereals as staple foods), (2) Traditional NWG diet (with rice as the staple food), (3) plant-based diet (Plant-based), (4) animal food diet (Animal-food), (5) Western energy-dense diet (Western) and (6) unclassified diets (Unclassified, including all other diets). Among these, a ‘healthy Chinese diet’ characterised by traditional style, whole grain and plant-based components was consistently associated with decreased risk of various health outcomes. In the rest of the discussion, we would like to focus on the following two perspectives: the diversity of Chinese diets and their explanation, the features of a healthy Chinese diet and how it compares to other healthy diets.
China has experienced a rapid diet transition over the last few decades(6,156). The diet transition occurred in two ways. In one way, the diet transition in China towards a westernised diet is unfavourable. From 1952 to 1992, cereal consumption increased from 540 g/d to 645 g/d, while the percentage of coarse grains decreased from 70 % to 16 %(6). Data from the CHNS showed that the average daily intake of whole grains further decreased by approximately 10 % from 1997 to 2011(157). Meanwhile, the consumption of animal-sourced foods, half of which were pork and pork products, tripled from 30 g/d to 103 g/d(6). While the total energy intake decreased, the percentage of energy intake from fat tripled from 7·6 % to 22·5 % and further increased to 27·3 % in 1997 and 35·6 % in 2015(24,79,110,158). Our results also reflect this diet transition. Two-thirds of the included studies reported either the Animal-food or the Western diet, and fifty-three reported both. Recent data have shown that the transition toward the Animal-food and Western diets is ongoing. For example, the average daily total meat consumption in China increased from 75 g to 90 g (normalised to a 2000 kcal diet) between 2002 and 2012(159–161). Statistics from the FAO’s Food Balance sheet also suggested that the increase in meat consumption continued after 2012(8). In the present review, Animal-food diet was found to be associated with increased risk of CVD and diabetes from cohort studies. The Western diet and Animal-food diet were found to be associated with increasing risk of obesity and depression. These are in agreement with the literature(162,163). The other associations, for example, between Animal-food diet and cancer and between Western diet and diabetes, are also positive; however, they are insignificant. If the transition from a plant-based diet to animal food and the Western diet in China cannot be controlled or reverted, the burden of chronic diseases in China, especially those attributed to poor diet quality, will continually increase. The other way of transitioning towards a more balanced and diverse diet is hard to capture in the current review as many of the studies included are cross-sectional. Fresh fruit and vegetables are becoming more available and affordable for certain geographical and rural areas in China due to improved supply chains, etc(22,164). Evidence suggests that vegetable consumption declined consistently until 1992, stabilised and then increased thereafter(3,157). As positive changes in the Chinese diet, fruit consumption has been increasing over time(4). In contrast, the average Na intake has been decreasing, although it remains above the WHO’s recommendation(165).
As expected, various dietary patterns were reported in the included studies. This could be explained mainly by three factors: (1) geographic variations in agriculture practices and food availability, (2) heterogeneity in social and economic status, cultural background of included participants, dietary pattern naming conversion between research groups and (3) diet transition among Chinese population for the last few decades. China is a large and diverse country, both geographically and culturally(166). For example, wheat and other cereals are staple foods in northern China, whereas rice is a staple food in southern China(23). Moreover, residents of coastal regions and southeastern China have greater access to fish and seafood than those of interior regions(52,53). In addition, certain vegetables are frequently consumed in some regions but rarely in others. More than half of the included studies were conducted in a single province or sub-administrative region. The food lists used to assess dietary intake and the identified dietary patterns varied across these studies. Differences in socio-economic development level (e.g. western v. eastern China; rural v. urban) are another important factor determining the variability and affordability of nutritious food(22). Such differences were more likely to be captured by studies using the two national nutrition surveys, the Chinese National Nutrition and Health Survey (CNNHS) and the Chinese Health and Nutrition Survey (CHNS)(167–169). Cultural tradition, ethnic background, dietary habits, food preparation and cooking methods play influential roles in people’s dietary choices(18–20,23). Besides the above-mentioned factors, the naming and reporting of dietary patterns could be arbitrary. The same dietary pattern could be named ‘healthy’ based on its relationship with health outcomes, ‘vegetable-rich’ based on food groups or ‘traditional’ due to cultural preference.
Despite rapid dietary changes, traditional diets remained prominent. Two-thirds of the included studies reported at least one traditional dietary pattern. In this review, we re-classified them into either Traditional WG or Traditional NWG, depending on whether food groups or items related to whole grains are a high-loading factor during the dietary pattern identification process. Given the sharp decline in whole grain consumption in the Chinese population, it is reasonable to assume that participants who adhere to the Traditional WG diet consume more whole-grain foods than those adopting other diets. However, this does not necessarily mean they consume a ‘whole-grain diet’. Besides the difference in whole grains, wheat is more likely to be a high factor-loading item (staple food) in the Traditional WG diet and rice in the Traditional NWG identified in this review. The traditional WG diet is more likely to be associated with a lower risk of metabolic risk factors (see online supplementary material, Supplemental Fig. 8–11). However, it is out of the scope of this review to compare the health impact of wheat-based diet and rice-based diet among the Chinese population, given many factors may bias such comparison. There has been concern about rice consumption and the risk of diabetes among the Chinese population(170). The present review found inconclusive evidence of this relationship. Traditional NWG diet, more likely with rice as a staple food, showed a negative association with diabetes (Fig. 2, see online supplementary material, Supplemental Fig. 8). Many of the studies reporting the Traditional NWG diet were conducted in wealthy coastal provinces in southern China, where dietary quality, social development and healthcare system are different from the other regions. Second, evidence suggests that rice cultured in southern China has higher amylose contents and a lower glycemic index(171). It may not be feasible to define a standard ‘traditional Chinese diet’. However, healthy Chinese diets may share common features.
The Traditional WG diet shared more similarities with the Plant-based diet than the Traditional NWG diet in terms of high factor-loading food groups and their associations with health outcomes. Moreover, few studies (13 out of 130) reported both Traditional WG and Plant-based diets (Table 3). The shared food groups/items between the two diets are: whole grains (coarse cereals), fresh fruits and vegetables, soyabeans and products, mushrooms and fungi, nuts, and fish and seafood. Moreover, the sensitivity analysis revealed that the associations of these combined diets and many health outcomes, especially metabolic conditions, followed the same trends with similar magnitudes as those for each of the patterns individually (e.g. effect size 0·86 v. 0·83 for hypertension, 0·78 v. 0·79 for diabetes; see online supplementary material, Supplemental Fig. 5). Therefore, these two diets appear to be essentially the same dietary pattern reported under different names in the literature. This combined ‘healthy Chinese diet’ can be broadly characterised by an abundance of plant foods, a preference for whole grains over refined grains, the inclusion of soyabeans and products, mushrooms, and fungi as integral components of the daily diet, and a balanced diet (e.g. not a vegetarian diet) with a high proportion of fish and seafood.
The identified healthy Chinese diet shares features similar to other well-known healthy diets, such as the Mediterranean(172,173) and Japanese diets(174). The common food groups or items in the healthy Chinese diet are also key elements in established dietary indexes, such as the Mediterranean Diet Score(175), Healthy Eating Index(176), Diet Quality Index(177) and DASH score(178). The associations between this healthy Chinese diet and health outcomes were comparable to other dietary patterns. For example, adherence to the healthy Chinese diet was associated with a 22 % decrease in CVD incidence or mortality, within the range of 12 % to 31 % from other reviews(179–182). This dietary pattern was also associated with a 15 % decrease in cancer incidence and mortality (mainly from colorectal cancer and breast cancer), in agreement with the latest evidence on diet and cancer(182,183). The evidence for the negative associations between the healthy Chinese diet and risk of CVD, cancer and diabetes is strong as they are based on results from cohort studies. Moreover, the association between the healthy Chinese diet or its components and metabolic syndrome was in accordance with reviews on other healthy diets(179,184–187). Finally, even the evidence for the negative associations between the healthy Chinese diet and depressive symptoms and cognitive impairment is only moderate as they were only based on mixed cohort studies and cross-sectional studies; the negative association is similar to that reported for the Mediterranean diet(188).
This study holds scientific, clinical and public health implications. First, the findings of the present review shed light on additional exploration into the health-promoting components of the typical traditional Chinese diet. Second, the clinical efficacy of dietary interventions characterised by a healthy Chinese dietary style merits further investigation. Third, these findings provide scientific evidence informing public health nutrition policies to address the escalating burden of chronic diseases in China and elsewhere where Chinese diets are common.
Our study has several limitations. Some are related to the scope of the review and dietary assessment in general. The review included dietary pattern studies only. Studies focus on the beneficial effects of a single food item or group, key nutrients, or certain types of meals that were not within the scope. Thus, certain healthy components of the Chinese diet, such as green tea, mushrooms and tofu, might have been overlooked. Furthermore, the standard dietary assessment method may not capture certain diet features. For example, food preparation and cooking methods, timing of meals, and the use of certain herbs and spices. This may have little impact on summarising the existing Chinese dietary patterns; however, it may compromise our effort to characterise a healthy Chinese diet and its components. Some are related to the heterogeneity of included studies. For example, (1) diets were assessed using different tools (e.g. FFQ v. 24-h recall) to different degrees of detail (e.g. number of food groups or items analysed), (2) dietary patterns were retained with different eigenvalue and factor-loading cut-offs, and named with different conventions, (3) study design, health outcome definition, statistical analyses and covariate adjustments varied among studies as well. We conducted various sensitivity analyses, showing that the associations observed between dietary patterns and health outcomes are robust regardless of the above-mentioned factors. Some are related to our data synthesis. The renaming of dietary patterns, including cross-sectional studies and case–control studies for certain health outcomes, and summarising studies from different geographic levels, regions and social development statuses may also introduce additional heterogeneity to the meta-analysis. The heterogeneity resulted in the relatively modest effect size observed in the associations between dietary patterns and health outcomes. Nonetheless, it is clear that the Traditional WG and Plant-based diets are ‘healthier’ than the Animal-food and Western diets.
Further work needs to be done to understand Chinese dietary patterns and healthy Chinese diets. First, it is worth exploring if any unique healthy food item or group is being ignored by current dietary pattern analysis. Second, although healthy dietary patterns share similar characteristics, one pattern may not work for all the Chinese population. It may be worth exploring the optimal components for populations with different staple foods by region, economic development status or by food transition progress. Third, temporal trend analysis of dietary patterns at the regional and national level may help public health policymakers estimate potential healthcare needs and plan for proper public health interventions.
Conclusion
We identified multiple dietary patterns that reflect the diverse dietary patterns among different Chinese populations and the transition of the Chinese diet from a traditional plant-based diet to a westernised and animal food diet. Despite the heterogeneity of the results and the relatively small effects size observed, our results still clearly showed that a ‘healthy Chinese diet’ characterised by whole grains, fresh vegetables, soyabean and products, fish and seafood, mushrooms and fungi, and nuts was associated with better cardiovascular health and reduced risks of metabolism conditions, cognitive impairment and depressive symptoms. Animal-food diet was associated with a higher risk of CVD, diabetes, abdominal obesity and depressive symptoms. Western diet were associated with an increased risk of both general and abdominal obesity and depressive symptoms. The present review provides moderate to high-quality evidence on the associations between identified dietary patterns among the Chinese population and specific health outcomes. Findings on cancer, CVD and diabetes were based on cohort studies. Therefore, the evidence for the negative associations between the healthy Chinese diet, that is, the combination of the traditional WG diet and the Plant-based diet with cancer, CVD and diabetes is strong compared with the moderate evidence of the other health outcomes, including hypertension, cognitive impairment, abdominal obesity and depressive symptoms, which were based on mixed cohort studies and cross-sectional studies. The results of this systematic review and meta-analysis can help inform nutrition and public health policymakers to revert the nutrition transition and reduce disease burdens among Chinese populations.
Future studies with more standardised dietary assessment tools and reporting guidelines – such as a comprehensive summary of daily or annual intake at food group or food item level – would greatly facilitate the comparison and classification of dietary patterns between studies. Additionally, longitudinal studies are needed to strengthen our understanding of the association between Chinese dietary patterns and specific health outcomes, such as particular types of cancer and CVD, and between fatal and non-fatal events. These studies would also help confirm whether the observed associations between metabolic conditions and other health outcomes are consistent over time.
Supporting information
Hu et al. supplementary material
Hu et al. supplementary material
Acknowledgements
The authors thank Yuet-Ying Lam (Y.Y.L.) and Chi-Yau Chung (C.Y.C.) for their careful work validating the extracted data and the re-classification of dietary patterns from the original studies.
Financial support
H.M.C. received findings from the Canada Research Chair Program (CRC). CRC has no role in the design, analysis or writing of this article.
Conflicts of interest
None of the authors has a conflict of interest to declare.
Authorship
X.F.H. and H.M.C. conceived the study. X.F.H. performed the literature searches. X.F.H. and R.Z. screened articles for inclusion. R.Z. extracted data for analysis. X.F.H. undertook the meta-analysis and produced forest plots and summary results, under the supervision of H.M.C. X.F.H. and H.M.C. wrote the first draft of the manuscript. All authors revised the manuscript and approved the final version.
Ethics of human subject participation
This study did not require ethical approval, as the data used have been published previously and hence are already in the public domain. Consent is not required when conducting a systematic review.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980024001927
References
- 1. Campbell TC, Parpia B & Chen J (1998) Diet, lifestyle, and the etiology of coronary artery disease: the Cornell China study. Am J Cardiol 82, 18T–21T. [DOI] [PubMed] [Google Scholar]
- 2. Chen JD & Xu H (1996) Historical development of Chinese dietary patterns and nutrition from the ancient to the modern society. World Rev Nutr Diet 79, 133–153. [DOI] [PubMed] [Google Scholar]
- 3. Du S, Lu B, Zhai F et al. (2002) A new stage of the nutrition transition in China. Public Health Nutr 5, 169–174. [DOI] [PubMed] [Google Scholar]
- 4. Popkin B, Keyou G, Fengying Z et al. (1993) The nutrition transition in China: a cross-sectional analysis. Eur J Clin Nutr 47, 333–346. [PubMed] [Google Scholar]
- 5. Popkin BM & Du S (2003) Dynamics of the nutrition transition toward the animal foods sector in China and its implications: a worried perspective. J Nutr 133, 3898S–3906S. [DOI] [PubMed] [Google Scholar]
- 6. Du SF, Wang HJ, Zhang B et al. (2014) China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes Rev 15, 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. He Y, Li Y, Yang X et al. (2019) The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol 7, 540–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Han A, Sun T, Ming J et al. (2020) Are the Chinese moving toward a healthy diet? Evidence from Macro data from 1961 to 2017. Int J Environ Res Public Health, 17, 5294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Campbell TC & Campbell TM (2007) The China Study: the Most Comprehensive Study of Nutrition Ever Conducted and the Startling Implications for Diet, Weight Loss and Long-Term Health. Kent Town, USA: Wakefield Press.
- 10. Yang G, Wang Y, Zeng Y et al. (2013) Rapid health transition in China, 1990–2010: findings from the Global Burden of disease study 2010. Lancet 381, 1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hu F, Liu Y & Willett W (2011) Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev 12, 552–559. [DOI] [PubMed] [Google Scholar]
- 12. Zhai F, Fu D, Du S et al. (2002) What is China doing in policy-making to push back the negative aspects of the nutrition transition? Public Health Nutr 5, 269–273. [DOI] [PubMed] [Google Scholar]
- 13. Yang YX, Wang XL, Leong PM et al. (2018) New Chinese dietary guidelines: healthy eating patterns and food-based dietary recommendations. Asia Pac J Clin Nutr 27, 908–913. [DOI] [PubMed] [Google Scholar]
- 14. Chen CM, Zhao W, Yang Z et al. (2008) The role of dietary factors in chronic disease control in China. Obes Rev 9, 100–103. [DOI] [PubMed] [Google Scholar]
- 15. Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13, 3–9. [DOI] [PubMed] [Google Scholar]
- 16. National Bureau of Statistics (2019) China Statistical Year Book 2019. Beijing: NBS. [Google Scholar]
- 17. Zhuang G (2011) Historical changes in numbers and distribution of overseas Chinese in the world. Shi Jie Li Shi 5, 4–14. [Google Scholar]
- 18. Ge K, Zhai F & Wang Q (1997) Effect of nationality on dietary pattern and meal behavior in China. Am J Clin Nutr 65, 1290S–1294S. [DOI] [PubMed] [Google Scholar]
- 19. Zhai F, He Y, Wang Z et al. (2007) Status and characteristic of dietary intake of 12 minority nationalities in China. J Hyg Res 36, 539–541. [PubMed] [Google Scholar]
- 20. Zhao W, You Y, Zhang X et al. (2002) Study on the food consumption pattern of elderly people in four ‘cuisine’ areas of China. J Hyg Res 31, 34–37. [PubMed] [Google Scholar]
- 21. Huang Y & Tian X (2019) Food accessibility, diversity of agricultural production and dietary pattern in rural China. Food Policy 84, 92–102. [Google Scholar]
- 22. Zhai FY, Du SF, Wang ZH et al. (2014) Dynamics of the Chinese diet and the role of urbanicity, 1991–2011. Obes Rev 15, 16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Song F & Cho MS (2017) Geography of food consumption patterns between south and north China. Foods 6, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Batis C, Sotres-Alvarez D, Gordon-Larsen P et al. (2014) Longitudinal analysis of dietary patterns in Chinese adults from 1991 to 2009. Br J Nutr 111, 1441–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Beasley JM, Yi SS, Ahn J et al. (2019) Dietary patterns in Chinese Americans are associated with cardiovascular disease risk factors, the Chinese American Cardiovascular Health Assessment (CHA CHA). J Immigr Minor Heal 21, 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Butler LM, Koh W-P, Lee H-P et al. (2006) Prospective study of dietary patterns and persistent cough with phlegm among Chinese Singaporeans. Am J Respir Crit Care Med 173, 264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Butler LM, Wang R, Koh W et al. (2008) Prospective study of dietary patterns and colorectal cancer among Singapore Chinese. Br J Cancer 99, 1511–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Butler LM, Wu AH, Wang R et al. (2010) A vegetable-fruit-soy dietary pattern protects against breast cancer among postmenopausal Singapore Chinese women. Am J Clin Nutr 91, 1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cai H, Shu XO, Gao Y-T et al. (2007) A prospective study of dietary patterns and mortality in Chinese women. Epidemiology 18, 393–401. [DOI] [PubMed] [Google Scholar]
- 30. Cai H, Zheng W, Xiang Y-B et al. (2007) Dietary patterns and their correlates among middle-aged and elderly Chinese men: a report from the Shanghai Men’s Health Study. Br J Nutr 98, 1006–1013. [DOI] [PubMed] [Google Scholar]
- 31. Chan RSM, Yu BWM, Leung J et al. (2019) How dietary patterns are related to inflammaging and mortality in community-dwelling older Chinese adults in Hong Kong - a prospective analysis. J Nutr Heal Aging 23, 181–194. [DOI] [PubMed] [Google Scholar]
- 32. Chan R, Chan D & Woo J (2013) A cross sectional study to examine the association between dietary patterns and cognitive impairment in older Chinese people in Hong Kong. J Nutr Health Aging 17, 757–765. [DOI] [PubMed] [Google Scholar]
- 33. Chan R, Chan D, Lau W et al. (2014) A cross-sectional study to examine the association between dietary patterns and risk of overweight and obesity in Hong Kong Chinese adolescents aged 10–12 years. J Am Coll Nutr 33, 450–458. [DOI] [PubMed] [Google Scholar]
- 34. Chan R, Chan D & Woo J (2013) The association of a priori and a posterior dietary patterns with the risk of incident stroke in Chinese older people in Hong Kong. J Nutr Health Aging 17, 866–874. [DOI] [PubMed] [Google Scholar]
- 35. Chan R, Chan D & Woo J (2014) A prospective cohort study to examine the association between dietary patterns and depressive symptoms in older Chinese people in Hong Kong. PLoS One 9, e105760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chan R, Leung J, Tang N et al. (2020) Dietary patterns and telomere length in community-dwelling Chinese older men and women: a cross-sectional analysis. Eur J Nutr 59, 3303–3311. [DOI] [PubMed] [Google Scholar]
- 37. Chan R, Leung J & Woo J (2015) Dietary patterns and risk of frailty in Chinese community-dwelling older people in Hong Kong: a prospective cohort study. Nutrients 7, 7070–7084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chan R, Leung J & Woo J (2016) A prospective cohort study to examine the association between dietary patterns and Sarcopenia in Chinese community-dwelling older people in Hong Kong. J Am Med Dir Assoc 17, 336–342. [DOI] [PubMed]
- 39. Chan R, Yau F, Yu B et al. (2019) The role of dietary patterns in the contribution of cardiorespiratory fitness in community-dwelling older Chinese adults in Hong Kong. J Am Med Dir Assoc 20, 558–563. [DOI] [PubMed]
- 40. Chan R, Yu B, Leung J et al. (2019) Association of dietary patterns with serum high-sensitivity C-reactive protein level in community-dwelling older adults. Clin Nutr ESPEN 31, 38–47. [DOI] [PubMed] [Google Scholar]
- 41. Chen Q, Feng Y, Yang H et al. (2019) A vitamin pattern diet is associated with decreased risk of gestational diabetes mellitus in Chinese women: results from a case control study in Taiyuan, China. J Diabetes Res, 5232308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Chen YC, Jung CC, Chen JH et al. (2017) Association of dietary patterns with global and domain-specific cognitive decline in Chinese elderly. J Am Geriatr Soc 65, 1159–1167. [DOI] [PubMed] [Google Scholar]
- 43. Cui X, Dai Q, Tseng M et al. (2007) Dietary patterns and breast cancer risk in the shanghai breast cancer study. Cancer Epidemiol Biomarkers Prev 16, 1443–1448. [DOI] [PubMed] [Google Scholar]
- 44. Dai X, He P, Zhang Y et al. (2010) Dietary pattern of Shanghai community-based middle and aged women. J Hyg Res 39, 472–477. [PubMed] [Google Scholar]
- 45. Dai Z, Butler LM, van Dam RM et al. (2014) Adherence to a vegetable-fruit-soy dietary pattern or the Alternative Healthy Eating Index is associated with lower hip fracture risk among Singapore Chinese. J Nutr 144, 511–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dang S, Wang Z, Kang Y et al. (2010) Study on the dietary pattern assessed with semi-quantitative food frequency questionnaire among rural Tibetan women with children younger than 2 years in Lhasa city. Chinese J Epidemiol 31, 394–399. [PubMed] [Google Scholar]
- 47. Du HY, Jiang H, Karmin O et al. (2017) Association of dietary pattern during pregnancy and gestational diabetes mellitus: a prospective cohort study in Northern China. Biomed Environ Sci 30, 887–897. [DOI] [PubMed] [Google Scholar]
- 48. Gao X, Yao M, McCrory MA et al. (2003) Dietary pattern is associated with homocysteine and B vitamin status in an urban Chinese population. J Nutr 133, 3636–3642. [DOI] [PubMed] [Google Scholar]
- 49. Guo C (1997) Diet pattern of Chinese people and some risk factors harmful to health. Chinese J Epidemiol 18, 375–376. [PubMed] [Google Scholar]
- 50. He DH, Yang M, Zhang RH et al. (2015) Dietary patterns associated metabolic syndrome in Chinese adults. Biomed Environ Sci 28, 370–373. [DOI] [PubMed] [Google Scholar]
- 51. He J-R, Yuan M-Y, Chen N-N et al. (2015) Maternal dietary patterns and gestational diabetes mellitus: a large prospective cohort study in China. Br J Nutr 113, 1292–1300. [DOI] [PubMed] [Google Scholar]
- 52. He Y, Li Y, Lai J et al. (2013) Dietary patterns as compared with physical activity in relation to metabolic syndrome among Chinese adults. Nutr Metab Cardiovasc Dis 23, 920–928. [DOI] [PubMed] [Google Scholar]
- 53. He Y, Ma G, Zhai F et al. (2009) Dietary patterns and glucose tolerance abnormalities in Chinese adults. Diabetes Care 32, 1972–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hong X, Li J, Wang Z et al. (2013) Dietary patterns and hyperglycemia in a follow-up study in Nanjing city. Chinese J Prev Med 47, 135–141. [PubMed] [Google Scholar]
- 55. Hong X, Xu F, Wang Z et al. (2016) Dietary patterns and the incidence of hyperglyacemia in China. Public Health Nutr 19, 131–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hong X, Ye Q, Wang Z et al. (2016) Reproducibility and validity of dietary patterns identified using factor analysis among Chinese populations. Br J Nutr 116, 842–852. [DOI] [PubMed] [Google Scholar]
- 57. Hsu C-C, Jhang H-R, Chang W-T et al. (2014) Associations between dietary patterns and kidney function indicators in type 2 diabetes. Clin Nutr 33, 98–105. [DOI] [PubMed] [Google Scholar]
- 58. Hu J, Oken E, Aris IM et al. (2019) Dietary patterns during pregnancy are associated with the risk of gestational diabetes mellitus: evidence from a Chinese prospective birth cohort study. Nutrients 11, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Huang Z, Li N & Hu YM (2019) Dietary patterns and their effects on postpartum weight retention of lactating women in south central China. Nutrition 67–68, 110555. [DOI] [PubMed] [Google Scholar]
- 60. Jaacks LM, Crandell J, Mendez MA et al. (2015) Dietary patterns associated with HbA1c and LDL cholesterol among individuals with type 1 diabetes in China. J Diabetes Complications 29, 343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Jia Q, Xia Y, Zhang Q et al. (2015) Dietary patterns are associated with prevalence of fatty liver disease in adults. Eur J Clin Nutr 69, 914–921. [DOI] [PubMed] [Google Scholar]
- 62. Lee S-A, Cai H, Yang G et al. (2010) Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br J Nutr 104, 265–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lee S-CC, Yang Y-HH, Chuang S-YY et al. (2012) Risk of asthma associated with energy-dense but nutrient-poor dietary pattern in Taiwanese children. Asia Pac J Clin Nutr 21, 73–81. [PubMed] [Google Scholar]
- 64. Li X, Yu C, Guo Y et al. (2019) Association between tea consumption and risk of cancer: a prospective cohort study of 0·5 million Chinese adults. Eur J Epidemiol 34, 753–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Li Y, He Y, Lai J et al. (2011) Dietary patterns are associated with stroke in Chinese adults. J Nutr 141, 1834–1839. [DOI] [PubMed] [Google Scholar]
- 66. Liao K, Gu Y, Liu M et al. (2019) Association of dietary patterns with depressive symptoms in Chinese postmenopausal women. Br J Nutr 122, 1168–1174. [DOI] [PubMed] [Google Scholar]
- 67. Lin S, Gao T, Sun C et al. (2019) Association of dietary patterns and endoscopic gastric mucosal atrophy in an adult Chinese population. Sci Rep 9, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Liu D, Zhao LY, Yu DM et al. (2019) Dietary patterns and association with obesity of children aged 6–17 years in medium and small cities in China: findings from the CNHS 2010–2012. Nutrients 11, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Liu J, Yang S, Luo MJ et al. (2020) Association between dietary patterns and fluorosis in Guizhou, China. Front Nutr 6, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Liu R, Dang S, Yan H et al. (2012) Dietary patterns and nutrients intakes in rural residents in Hanzhong of Shaanxi Province. J Hyg Res 41, 997–1003. [PubMed] [Google Scholar]
- 71. Liu R, Dang S, Yan H et al. (2012) Dietary patterns and its relationship with hypertension among rural residents in Hanzhong, Shanxi province. Chinese J Epidemiol 33, 37–41. [PubMed] [Google Scholar]
- 72. Liu X, Peng Y, Chen S et al. (2018) An observational study on the association between major dietary patterns and non-alcoholic fatty liver disease in Chinese adolescents. Medicine (Baltimore) 97, e0576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Liu X, Wang X, Lin S et al. (2015) Reproducibility and validity of a food frequency questionnaire for assessing dietary consumption via the dietary pattern method in a Chinese rural population. PLoS One 10, e0134627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Liu Z, Ho SC, Xie YJ et al. (2015) Whole plant foods intake is associated with fewer menopausal symptoms in Chinese postmenopausal women with prehypertension or untreated hypertension. Menopause 22, 496–504. [DOI] [PubMed] [Google Scholar]
- 75. Lu Q, Tao F, Hou F et al. (2016) Emotion regulation, emotional eating and the energy-rich dietary pattern. A population-based study in Chinese adolescents. Appetite 99, 149–156. [DOI] [PubMed] [Google Scholar]
- 76. Lyu S, Su J, Xiang Q et al. (2014) Association of dietary pattern and physical activity level with triglyceride to high-density lipoprotein cholesterol ratio among adults in Jiangsu, China: a cross-sectional study with sex-specific differences. Nutr Res 34, 674–681. [DOI] [PubMed] [Google Scholar]
- 77. Mak JKL, Pham NM, Lee AH et al. (2018) Dietary patterns during pregnancy and risk of gestational diabetes: a prospective cohort study in Western China 11 Medical and Health Sciences 1111 Nutrition and Dietetics 11 Medical and Health Sciences 1114 Paediatrics and Reproductive Medicine. Nutr J 17, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Meng F, Chen D, Wu Y et al. (2020) Study of relationship between dietary patterns and precocious puberty of school-age girls in Shenzhen. Chinese J Epidemiol 41, 738–742. [DOI] [PubMed] [Google Scholar]
- 79. Mu M, Wang S-F, Sheng J et al. (2014) Dietary patterns are associated with body mass index and bone mineral density in Chinese freshmen. J Am Coll Nutr 33, 120–128. [DOI] [PubMed] [Google Scholar]
- 80. Na L, Han T, Zhang W et al. (2015) A snack dietary pattern increases the risk of hypercholesterolemia in Northern Chinese adults: a prospective cohort study. PLoS One 10, e0134294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Nettleton JA, Steffen LM, Ni H et al. (2008) Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 31, 1777–1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Odegaard AO, Koh W-P, Butler LM et al. (2011) Dietary patterns and incident type 2 diabetes in Chinese men and women the Singapore Chinese Health Study. Diabetes Care 34, 880–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Odegaard AO, Koh W-P, Yuan J-M et al. (2014) Dietary patterns and mortality in a Chinese population. Am J Clin Nutr 100, 877–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Qin B, Adair LS, Plassman BL et al. (2015) Dietary patterns and cognitive decline among Chinese older adults. Epidemiology 26, 758–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Qin Y, Melse-Boonstra A, Pan X et al. (2014) Association of dietary pattern and body weight with blood pressure in Jiangsu Province, China. BMC Public Health 14, 948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Qin Y, Melse-Boonstra A, Yuan B et al. (2012) Zinc biofortification of rice in China: a simulation of zinc intake with different dietary patterns. Nutrients 4, 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Ruan Y, Huang Y, Zhang Q et al. (2018) Association between dietary patterns and hypertension among Han and multi-ethnic population in southwest China. BMC Public Health 18, 1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Seah JYH, Ong CN, Koh WP et al. (2019) A dietary pattern derived from reduced rank regression and fatty acid biomarkers is associated with lower risk of type 2 diabetes and coronary artery disease in Chinese adults. J Nutr 149, 2001–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Shang X, Li Y, Liu A et al. (2012) Dietary pattern and its association with the prevalence of obesity and related cardiometabolic risk factors among Chinese children. PLoS One 7, e43183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Shi Z, Hu X, Yuan B et al. (2008) Vegetable-rich food pattern is related to obesity in China. Int J Obes 32, 975–984. [DOI] [PubMed] [Google Scholar]
- 91. Shi Z, El-Obeid T, Li M et al. (2019) Iron-related dietary pattern increases the risk of poor cognition. Nutr J 18, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Shi Z & Ganji V (2020) Dietary patterns and CVD risk among Chinese adults: a prospective cohort study. Eur J Clin Nutr 74, 1725–1735. [DOI] [PubMed] [Google Scholar]
- 93. Shi Z, Hu X, Yuan B et al. (2006) Association between dietary patterns and anaemia in adults from Jiangsu Province in Eastern China. Br J Nutr 96, 906–912. [DOI] [PubMed] [Google Scholar]
- 94. Shi Z, Taylor AW, Riley M et al. (2018) Association between dietary patterns, cadmium intake and chronic kidney disease among adults. Clin Nutr 37, 276–284. [DOI] [PubMed] [Google Scholar]
- 95. Shi Z, Yuan B, Hu G et al. (2011) Dietary pattern and weight change in a 5-year follow-up among Chinese adults: results from the Jiangsu Nutrition Study. Br J Nutr 105, 1047–1054. [DOI] [PubMed] [Google Scholar]
- 96. Shi Z, Yuan B, Wittert GA et al. (2012) Monosodium glutamate intake, dietary patterns and asthma in Chinese adults. PLoS One 7, e51567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Shi Z, Zhen S, Zimmet PZ et al. (2016) Association of impaired fasting glucose, diabetes and dietary patterns with mortality: a 10-year follow-up cohort in Eastern China. Acta Diabetol 53, 799–806. [DOI] [PubMed] [Google Scholar]
- 98. Shu L, Shen XM, Li C et al. (2017) Dietary patterns are associated with type 2 diabetes mellitus among middle-Aged adults in Zhejiang Province, China. Nutr J 16, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Shu L, Zheng PF, Zhang XY et al. (2019) Dietary patterns and Helicobacter pylori infection in a group of Chinese adults ages between 45 and 59 years old: an observational study. Medicine (Baltimore) 98, e14113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Shu L, Zheng P-F, Zhang X-Y et al. (2015) Association between dietary patterns and the indicators of obesity among Chinese: a cross-sectional study. Nutrients 7, 7995–8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Sun J, Buys NJ & Hills AP (2014) Dietary pattern and its association with the prevalence of obesity, hypertension and other cardiovascular risk factors among Chinese older adults. Int J Environ Res Public Health 11, 3956–3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Sun Q, Ma JS, Wang H et al. (2019) Associations between dietary patterns and 10-year cardiovascular disease risk score levels among Chinese coal miners - - a cross-sectional study. BMC Public Health 19, 1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Sun Q, Wang H, Qiao N et al. (2020) Association of dietary patterns and diabetes risk level among adult residents in Datong city of Shanxi Province. Chinese J Prev Med 54, 278–282. [DOI] [PubMed] [Google Scholar]
- 104. Tao X, Shao Y, Xu D et al. (2022). Dietary patterns and nutrient intake in university students of Macao: A cross-sectional study. Nutrients, 14(17), 3642. doi: 10.3390/nu14173642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Tian HM, Wu YX, Lin YQ et al. (2019) Dietary patterns affect maternal macronutrient intake levels and the fatty acid profile of breast milk in lactating Chinese mothers. Nutrition 58, 83–88. [DOI] [PubMed] [Google Scholar]
- 106. Tian Y, Min J, Liu P et al. (2011) Clustering analysis on the dietary patterns of residents in Jiangsu Province. J Hyg Res 40, 771–775. [PubMed] [Google Scholar]
- 107. Tsai Y-T, Liu J-P, Tu Y-K et al. (2012) Relationship between dietary patterns and serum uric acid concentrations among ethnic Chinese adults in Taiwan. Asia Pac J Clin Nutr 21, 263–270. [PubMed] [Google Scholar]
- 108. Villegas R, Yang G, Gao Y-T et al. (2010) Dietary patterns are associated with lower incidence of type 2 diabetes in middle-aged women: the Shanghai Women’s Health Study. Int J Epidemiol 39, 889–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Wang CJ, Yang TF, Wang GS et al. (2018) Association between dietary patterns and depressive symptoms among middle-aged adults in China in 2016–2017. Psychiatry Res 260, 123–129. [DOI] [PubMed] [Google Scholar]
- 110. Wang D, He Y, Li Y et al. (2011) Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health 11, 925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Wang S, Mu M, Ruan L et al. (2012) Influence of different dietary patterns on bone mineral density and body mass index of college freshmen in urban and rural areas of China. Chinese J Epidemiol 33, 572–575. [PubMed] [Google Scholar]
- 112. Wei X, He JR, Lin Y et al. (2019) The influence of maternal dietary patterns on gestational weight gain: a large prospective cohort study in China. Nutrition 59, 90–95. [DOI] [PubMed] [Google Scholar]
- 113. Weng T-T, Hao J-H, Qian Q-W et al. (2012) Is there any relationship between dietary patterns and depression and anxiety in Chinese adolescents? Public Health Nutr 15, 673–682. [DOI] [PubMed] [Google Scholar]
- 114. Woo J, Yu BWM, Chan RSM et al. (2018) Influence of dietary patterns and inflammatory markers on atherosclerosis using ankle brachial index as a surrogate. J Nutr Heal Aging 22, 619–626. [DOI] [PubMed] [Google Scholar]
- 115. Xia Y, Wang N, Yu B et al. (2017) Dietary patterns are associated with depressive symptoms among Chinese adults: a case–control study with propensity score matching. Eur J Nutr 56, 2577–2587. [DOI] [PubMed] [Google Scholar]
- 116. Xia Y, Xiang Q, Gu Y et al. (2018) A dietary pattern rich in animal organ, seafood and processed meat products is associated with newly diagnosed hyperuricaemia in Chinese adults: a propensity score-matched case-control study. Br J Nutr 119, 1177–1184. [DOI] [PubMed] [Google Scholar]
- 117. Xu F, Chong B-Q, Cai T et al. (2020) Associations between major dietary patterns and anxiety in middle-aged adults in eastern China. Public Health Nutr 24(7), 1716–1724. doi: 10.1017/S1368980020000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Xu SS, Hua J, Huang YQ et al. (2020) Association between dietary patterns and chronic kidney disease in a middle-aged Chinese population. Public Health Nutr 23, 1058–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Xu S-H, Qiao N, Huang J-J et al. (2016) Gender differences in dietary patterns and their association with the prevalence of metabolic syndrome among Chinese: a cross-sectional study. Nutrients 8, 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Xu T, Wang X, Huang J et al. (2019) The relationship between dietary pattern and serum C-reactive protein concentration. Chinese J Prev Med 53, 408–410. [DOI] [PubMed] [Google Scholar]
- 121. Xu X, Hall J, Byles J et al. (2015) Dietary pattern is associated with obesity in older people in China: data from China Health and Nutrition Survey (CHNS). Nutrients 7, 8170–8188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Yan S, Cao H, Gu C et al. (2018) Dietary patterns are associated with attention-deficit/hyperactivity disorder (ADHD) symptoms among preschoolers in mainland China. Eur J Clin Nutr 72, 1517–1523. [DOI] [PubMed] [Google Scholar]
- 123. Yang C-Q, Shu L, Wang S et al. (2015) Dietary patterns modulate the risk of non-alcoholic fatty liver disease in Chinese adults. Nutrients 7, 4778–4791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Yang J, Dang S, Cheng Y et al. (2017) Dietary intakes and dietary patterns among pregnant women in Northwest China. Public Health Nutr 20, 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Yang Y, Hu X-M, Chen T-J et al. (2016) Rural-urban differences of dietary patterns, overweight, and bone mineral status in Chinese students. Nutrients 8, 537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Yap RWK, Shidoji Y, Hon WM et al. (2012) Association and interaction between dietary pattern and VEGF receptor-2 (VEGFR2) gene polymorphisms on blood lipids in Chinese Malaysian and Japanese adults. Asia Pac J Clin Nutr 21, 302–311. [PubMed] [Google Scholar]
- 127. Ye J, Lv Y, Li Z et al. (2019) Associations of dietary patterns with hypertension among adults in Jilin Province, China: a structural equation modelling approach. Public Health Nutr 22, 1048–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Ye Q, Hong X, Wang Z et al. (2018) Joint associations of dietary pattern and television viewing with CVD risk factors among urban men and women in China: a cross-sectional study. Br J Nutr 119, 74–82. [DOI] [PubMed] [Google Scholar]
- 129. Yin X, Chen Y, Lu W et al. (2020) Association of dietary patterns with the newly diagnosed diabetes mellitus and central obesity: a community based cross-sectional study. Nutr Diabetes 10, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Yin Z, Chen J, Zhang J et al. (2018) Dietary patterns associated with cognitive function among the older people in underdeveloped regions: finding from the NCDFaC study. Nutrients 10, 464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Yin Z, Ren Z, Jing G et al. (2019) A cohort study on the association between dietary patterns which benefit for normal kidney function and the cognitive performance in the Chinese elderly. Chinese J Epidemiol 40, 427–432. [DOI] [PubMed] [Google Scholar]
- 132. Yin Z, Ren Z, Xu X et al. (2018) Association between blood pressure related dietary patterns and identified cognitive performance in the elderly Chinese – a study by reduced rank regression method. Chinese J Epidemiol 39, 781–785. [DOI] [PubMed] [Google Scholar]
- 133. Yu C, Shi Z, Lv J et al. (2015) Major dietary patterns in relation to general and central obesity among Chinese adults. Nutrients 7, 5834–5849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Yu C, Shi Z, Lv J et al. (2017) Dietary patterns and insomnia symptoms in Chinese adults: the China Kadoorie Biobank. Nutrients 9, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Yu FN, Hu NQ, Huang XL et al. (2018) Dietary patterns derived by factor analysis are associated with cognitive function among a middle-aged and elder Chinese population. Psychiatry Res 269, 640–645. [DOI] [PubMed] [Google Scholar]
- 136. Yu R, Woo J, Chan R et al. (2011) Relationship between dietary intake and the development of type 2 diabetes in a Chinese population: the Hong Kong Dietary Survey. Public Health Nutr 14, 1133–1141. [DOI] [PubMed] [Google Scholar]
- 137. Yuan Y-QQ, Li F, Meng P et al. (2016) Gender difference on the association between dietary patterns and obesity in Chinese middle-aged and elderly populations. Nutrients 8, 448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Zeng F, Wu B, Fan F et al. (2013) Dietary patterns and the risk of hip fractures in elderly Chinese: a matched case-control study. J Clin Endocrinol Metab 98, 2347–2355. [DOI] [PubMed] [Google Scholar]
- 139. Zhang C-X, Ho SC, Fu J-H et al. (2011) Dietary patterns and breast cancer risk among Chinese women. Cancer Causes Control 22, 115–124. [DOI] [PubMed] [Google Scholar]
- 140. Zhang JG, Wang ZH, Wang HJ et al. (2015) Dietary patterns and their associations with general obesity and abdominal obesity among young Chinese women. Eur J Clin Nutr 69, 1009–1014. [DOI] [PubMed] [Google Scholar]
- 141. Zhang J, Wang H, Wang Y et al. (2015) Dietary patterns and their associations with childhood obesity in China. Br J Nutr 113, 1978–1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Zhang J, Zhang B, Wang H et al. (2013) Dietary patterns of Chinese adults in nine provinces. Chinese J Epidemiol 34, 37–40. [PubMed] [Google Scholar]
- 143. Zhang M, Chang H, Gao Y et al. (2012) Major dietary patterns and risk of asymptomatic hyperuricemia in Chinese adults. J Nutr Sci Vitaminol (Tokyo) 58, 339–345. [DOI] [PubMed] [Google Scholar]
- 144. Zhang M, Zhu Y, Li P et al. (2015) Associations between dietary patterns and impaired fasting glucose in Chinese men: a cross-sectional study. Nutrients 7, 8072–8089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Zhang W, Xiang Y-B, Li H-L et al. (2013) Vegetable-based dietary pattern and liver cancer risk: results from the Shanghai women’s and men’s health studies. Cancer Sci 104, 1353–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Zhang Y, Tan H, Dai X et al. (2012) Dietary patterns are associated with weight gain in newlyweds: findings from a cross-sectional study in Shanghai, China. Public Health Nutr 15, 876–884. [DOI] [PubMed] [Google Scholar]
- 147. Zhen S, Ma Y, Zhao Z et al. (2018) Dietary pattern is associated with obesity in Chinese children and adolescents: data from China Health and Nutrition Survey (CHNS). Nutr J 17, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Zheng P-F, Shu L, Zhang X-Y et al. (2016) Association between dietary patterns and the risk of hypertension among Chinese: a cross-sectional study. Nutrients 8, 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Zhou J, Sheng J, Fan Y et al. (2019) Dietary patterns, dietary intakes and the risk of type 2 diabetes: results from the Hefei Nutrition and Health Study. Int J Food Sci Nutr 70, 412–420. [DOI] [PubMed] [Google Scholar]
- 150. Zhou X, Chen R, Zhong C et al. (2018) Maternal dietary pattern characterised by high protein and low carbohydrate intake in pregnancy is associated with a higher risk of gestational diabetes mellitus in Chinese women: a prospective cohort study. Br J Nutr 120, 1045–1055. [DOI] [PubMed] [Google Scholar]
- 151. Zhu W, Guan Y, Xu C et al. (2020) Influence of dietary patterns on type 2 diabetes mellitus in local residents aged 40 years and above in Songjiang district, Shanghai. Chinese J Epidemiol 41, 508–513. [DOI] [PubMed] [Google Scholar]
- 152. Zuo H, Shi Z, Dai Y et al. (2014) Serum leptin concentrations in relation to dietary patterns in Chinese men and women. Public Health Nutr 17, 1524–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Zuo H, Shi Z, Yuan B et al. (2013) Dietary patterns are associated with insulin resistance in Chinese adults without known diabetes. Br J Nutr 109, 1662–1669. [DOI] [PubMed] [Google Scholar]
- 154. Wells G, Shea B, O’ Connell D et al. (2009) The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta- Analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed August 2020).
- 155. Higgins JPT & Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21, 1539–1558. [DOI] [PubMed] [Google Scholar]
- 156. Piazza AL (1986) Food Consumption and Nutritional Status in the PRC. New York: Routledge. [Google Scholar]
- 157. Li Y, Wang DD, Ley SH et al. (2016) Potential impact of time trend of life-style factors on cardiovascular disease burden in China. J Am Coll Cardiol 68, 818–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Wang L, Wang H, Zhang B et al. (2020) Elevated fat intake increases body weight and the risk of overweight and obesity among Chinese adults: 1991–2015 trends. Nutrients 12, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. He Y, Yang X, Xia J et al. (2016) Consumption of meat and dairy products in China: a review. Proc Nutr Soc 75, 385–391. [DOI] [PubMed]
- 160. Daniel CR, Cross AJ, Koebnick C et al. (2011) Trends in meat consumption in the USA. Public Health Nutr 14, 575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Wang ZH, Zhai FY, Wang HJ et al. (2015) Secular trends in meat and seafood consumption patterns among Chinese adults, 1991–2011. Eur J Clin Nutr 69, 227–233. [DOI] [PubMed] [Google Scholar]
- 162. Clemente-Suárez VJ, Beltrán-Velasco AI, Redondo-Flórez L et al. (2023) Global impacts of Western diet and its effects on metabolism and health: a narrative review. Nutrients 15, 2749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Cordain L, Eaton SB, Sebastian A et al. (2005) Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr 81, 341–354. [DOI] [PubMed] [Google Scholar]
- 164. Chang X, DeFries RS, Liu L et al. (2018) Understanding dietary and staple food transitions in China from multiple scales. PLoS One 13, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Du S, Batis C, Wang H et al. (2014) Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr 99, 334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Zhu YX, Huang J, Zhang ZK et al. (2013) Geography and similarity of regional cuisines in China. PLoS One 8, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Popkin BM, Du S, Zhai F et al. (2010) Cohort profile: the China Health and Nutrition Survey-monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol 39, 1435–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Li L, Rao K, Kong L et al. (2005) A description on the Chinese national nutrition and health survey in 2002. Chinese J Epidemiol 26, 478–484. [PubMed] [Google Scholar]
- 169. Zhao L, Ma G, Piao J et al. (2016) Scheme of the 2010–2012 Chinese nutrition and health surveillance. Chinese J Prev Med 50, 204–207. [DOI] [PubMed] [Google Scholar]
- 170. Hu EA, Pan A, Malik V et al. (2012) White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review. BMJ 344, e1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Calingacion M, Laborte A, Nelson A et al. (2014) Diversity of global rice markets and the science required for consumer-targeted rice breeding. PLoS One 9, e85106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Willett WC, Sacks F, Trichopoulou A et al. (1995) Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 61, 1402s–1406s. [DOI] [PubMed] [Google Scholar]
- 173. Sofi F, Macchi C, Abbate R et al. (2013) Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17, 2769–2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Sasaki S (2020) What is the scientific definition of the Japanese diet from the viewpoint of nutrition and health? Nutr Rev 78, 18–26. [DOI] [PubMed] [Google Scholar]
- 175. Bach A, Serra-Majem L, Carrasco JL et al. (2006) The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: a review. Public Health Nutr 9, 132–146. [DOI] [PubMed] [Google Scholar]
- 176. Kennedy ET, Ohls J, Carlson S et al. (1995) The Healthy Eating Index: design and applications. J Am Diet Assoc 95, 1103–1108. [DOI] [PubMed] [Google Scholar]
- 177. Patterson RE, Haines PS & Popkin BM (1994) Diet quality index: capturing a multidimensional behavior. J Am Diet Assoc 94, 57–64. [DOI] [PubMed] [Google Scholar]
- 178. Vogt TM, Appel LJ, Obarzanek E et al. (1999) Dietary approaches to stop hypertension: rationale, design, and methods. DASH Collaborative Research Group. J Am Diet Assoc 99, S12–8. [DOI] [PubMed] [Google Scholar]
- 179. Chiavaroli L, Viguiliouk E, Nishi SK et al. (2019) DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients 11, 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Zampelas A & Magriplis E (2020) Dietary patterns and risk of cardiovascular diseases: a review of the evidence. Proc Nutr Soc 79, 68–75. [DOI] [PubMed]
- 181. Rodríguez-Monforte M, Flores-Mateo G & Sánchez E (2013) Dietary patterns and CVD: a systematic review and meta-analysis of observational studies. Br J Nutr 114, 1341–1359. [DOI] [PubMed] [Google Scholar]
- 182. Sofi F, Cesari F, Abbate R et al. (2008) Adherence to Mediterranean diet and health status: meta-analysis. BMJ 337, a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Grosso G, Bella F, Godos J et al. (2017) Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev 75, 405–419. [DOI] [PubMed] [Google Scholar]
- 184. Schwingshackl L, Missbach B, König J et al. (2015) Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr 18, 1292–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Franquesa M, Pujol-Busquets G, García-Fernández E et al. (2019) Mediterranean diet and cardiodiabesity: a systematic review through evidence-based answers to key clinical questions. Nutrients 11, 655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Siervo M, Lara J, Chowdhury S et al. (2015) Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr 113, 1–15. 2014/11/28. [DOI] [PubMed] [Google Scholar]
- 187. Kastorini CM, Milionis HJ, Esposito K et al. (2011) The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534 906 individuals. J Am Coll Cardiol 57, 1299–1313. [DOI] [PubMed] [Google Scholar]
- 188. Psaltopoulou T, Sergentanis TN, Panagiotakos DB et al. (2013) Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol 74, 580–591. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hu et al. supplementary material
Hu et al. supplementary material