Abstract
Background
As the importance of meniscus in joint function becomes more apparent, there is a growing interest in meniscus repair techniques. Notably, biological augmentation methods have shown promising results for meniscus healing, despite their challenges in practical implementation. The purpose of this study was to evaluate meniscus healing and clinical outcomes of meniscus repair with bone marrow aspirate for horizontal or radial tears.
Methods
This study retrospectively reviewed patients who underwent arthroscopic meniscal repair with bone marrow aspirate from the iliac crest. A total of 30 patients with horizontal or radial meniscus tears confirmed by magnetic resonance imaging (MRI) were included, excluding those with insufficient data or concurrent surgeries. Patient demographic characteristics, operative data, and clinical outcomes including pain numeric rating scale, International Knee Documentation Committee score, Lysholm score, and Tegner activity scale were evaluated. For radiographic evaluation, knee x-rays, preoperative MRIs, and postoperative 3-month MRIs were evaluated.
Results
Thirty patients (15 women and 15 men) with a mean age of 46.8 ± 15.2 years were followed up for a mean of 25.1 ± 3.4 months. Of these patients, 22 (73%) had horizontal meniscal tears, while 8 (27%) had radial tears. Clinical outcomes were significantly improved over the time from the initial to 2 years after surgery. Meniscus healing was 60% on MRI at 3 months after surgery. There was no correlation between changes in clinical scores and healing rate. Furthermore, there was no statistically significant difference in the healing rate or changes in clinical scores according to tear patterns. Retears were observed in 2 patients, who were non-compliant with rehabilitation and were managed conservatively.
Conclusions
Augmentation with bone marrow aspirate harvested from the iliac crest for meniscal repair of horizontal or radial tears yields favorable healing rates in MRI and clinical outcomes, highlighting its potential for addressing challenging meniscal repair.
Keywords: Bone marrow cell, Bone marrow aspirate, Meniscus, Arthroscopy
As the role of the meniscus in joint lubrication, stability, and chondroprotection becomes increasingly recognized, interest in meniscus repair continues to grow.1,2,3) Indications for meniscal repair are determined by factors such as tear pattern, location, vascularity, and concomitant injuries. In particular, the tear pattern plays a crucial role. Although short-term clinical outcomes for longitudinal tears tend to be favorable, especially for peripheral tears with good vascularity, outcomes for horizontal or radial tears have been inferior.4) To preserve the function of the meniscus, indications for meniscal repair are broadening. In particular, for horizontal or radial tears that involve the avascular zone of the meniscus, biological augmentation is necessary and implemented to enhance the capacity of healing. Contemporary approaches to meniscal healing include synovial trephination,5) fibrin clot,6,7,8) platelet-rich plasma (PRP),9,10,11,12) and bone marrow stimulating procedures.13,14,15,16)
Recently, several attempts have been made to promote healing by intra-articular release of growth factors and mesenchymal stem cells from the bone marrow of the intercondylar notch.13,14,16) Despite the limitations of biological agents in bone marrow venting procedures assisting meniscus healing, promising results have been reported in both clinical usefulness and in vivo application through the application of bone marrow aspirate concentrate (BMAC).17,18) However, the practical implementation of BMAC presents certain challenges due to the requirement of additional equipment and financial resources. To date, no studies have demonstrated the use of simple bone marrow aspirate, an alternative that can eliminate the need for extra equipment and cost in the context of meniscus healing.
The purpose of this study was to evaluate clinical outcomes and meniscus healing after arthroscopic repair for horizontal/radial meniscus tears with bone marrow aspirates from the ilium. The hypothesis of this study was that even simple bone marrow aspirate could positively influence meniscus healing and clinical outcomes.
METHODS
This study was approved by the Institutional Review Board of Seoul National University College of Medicine/Seoul National University Hospital (IRB No. H-2305-110-1432). All investigations were conducted in conformity with ethical principles of research. As this study is a retrospective study, informed consent was exempted by the board.
Participants
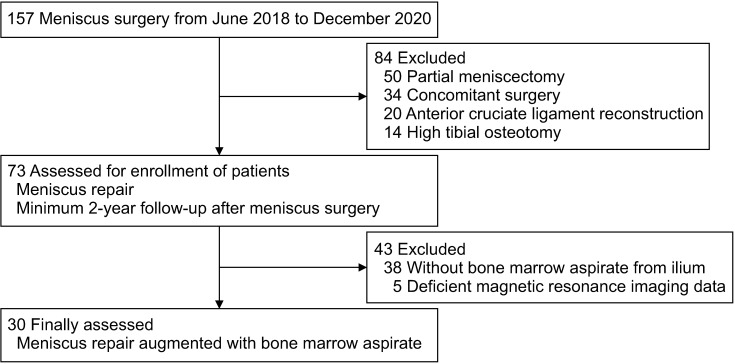
Data of patients who underwent arthroscopic meniscal repair with bone marrow aspirate from the iliac crest between June 2018 and December 2020 were retrospectively reviewed. During the same period, 157 patients underwent meniscus surgery. Excluding 50 patients who received partial meniscectomy and 34 patients who had concomitant surgeries, a total of 73 patients received meniscus repair. A total of 30 patients were finally assessed, excluding those who underwent meniscus repair without augmentation with bone marrow aspirate and those without available magnetic resonance imaging (MRI) data (Fig. 1). All patients exhibited mechanical symptoms, including giving way or buckling. They also demonstrated positive results in the McMurray test and joint line tenderness. Patients with horizontal tears were initially treated conservatively using weight control, activity modification, and daily administration of prescribed anti-inflammatory or analgesic medication. Surgical intervention was considered if conservative treatments were unsuccessful or if patients exhibited mechanical symptoms. In contrast, immediate surgical intervention was performed for patients with complete radial tears. The choice between partial meniscectomy and meniscus repair was primarily guided by the etiology of the tear and the associated Kellgren-Lawrence (K-L) grade. Specifically, repair was more frequently conducted when the tear was traumatic, and the K-L grade was between 0 to 2.
Fig. 1. Flow diagram showing the selection of study participants.
Surgical Techniques
All surgical procedures were performed by a single experienced surgeon (HSH). A routine arthroscopic examination was performed to assess meniscus tears, cartilage, and ligament injuries. Unstable meniscal fragments were removed using basket forceps or a motorized shaver. Trephination was performed at the meniscocapsular junction to enhance vascular supply to the meniscus tear location.
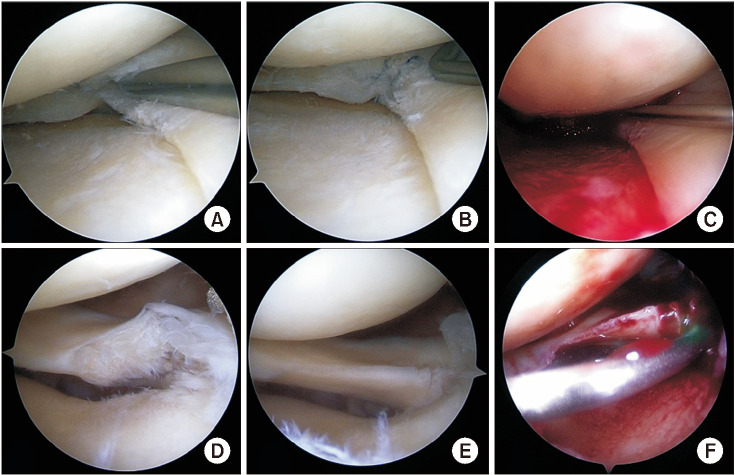
For meniscus repair, the inside-out technique was used for tears located in the middle, while the all-inside technique using a FAST-Fix device (Smith and Nephew) was employed for tears extending from the body to the posterior horn. Meniscus repair techniques were applied differently depending on the patterns of the meniscus tear. For horizontal meniscus tears, both leaflets were preserved by using circumferential compression stitches. In the case of radial meniscus tears, tension was generated at the periphery of the meniscus, and horizontal mattress sutures were applied at the radial tear site. To augment meniscal healing, bone marrow aspirate was harvested from the anterior iliac crest. A 1-cm stab incision was created on the ipsilateral anterior iliac crest, and a Jamshidi needle was advanced from the midpoint of the crest. Subsequently, 5–10 mL of bone marrow was extracted. A saline pump was stopped and suction was applied. Air was then injected into the knee joint to create a dry arthroscopic environment. Under arthroscopic visualization, the bone marrow aspirate was then inserted into the repair site (Fig. 2).
Fig. 2. A 49-year-old female patient who underwent meniscus repair surgery due to a right medial meniscus horizontal tear (A-C) and a 54-year-old male patient who underwent meniscus repair due to a right lateral meniscus posterior radial tear (D-F). (A) Arthroscopic findings revealing a concurrent medial meniscus horizontal tear. (D) Arthroscopic findings for lateral meniscus radial tear. (B, E) Meniscus repair utilizing the all-inside technique. (C, F) Insertion of bone marrow aspirate obtained from the iliac crest at the repair site.
Postoperative rehabilitation protocol was individualized according to the pattern of meniscal tear. For horizontal tears, knee flexion was limited to avoid shear force, while permitting partial weight-bearing to ensure only compressive forces were applied. In the case of radial tears, non-weight-bearing was implemented for 4 weeks to prevent distraction forces due to weight-bearing. If the tear location was in the mid or posterior horn, flexion was also restricted to less than 90° for 4 weeks. In all cases, range of motion exercises were conducted without restrictions 1 month after surgery. Bicycle use was permitted from the sixth postoperative week. Light jogging was allowed after 3 months.
Data Collection
Patients’ demographic characteristics and operative data were retrospectively collected from electronic health records and the institutional database. Patient-reported outcomes, such as pain numeric rating scale (NRS), International Knee Documentation Committee (IKDC) subjective knee form,19) Lysholm score, and Tegner activity scale, were collected preoperatively and at 3 months, 1 year, and 2 years postoperatively.
For preoperative radiographic evaluation, knee radiographs and weight-bearing teleradiogram were obtained to evaluate hip-knee-ankle angle (HKAA), mechanical lateral distal femoral angle (mLDFA), medial proximal tibia angle (MPTA), joint line convergence angle (JLCA), joint line orientation angel, and K-L grade. Radiographic variables such as HKAA, mLDFA, MPTA, JLCA, and K-L grade were measured using an automated program developed with a deep learning model.20)
Pre- and postoperative 3-month MRIs were evaluated using a classification system for meniscal tears described by Ogawa et al.13) Grade 0 was defined as a normal meniscus. Grade 1 was defined as central globular intrameniscal alteration. Grade 2 was defined as horizontal, triangular, or band-like signal intensity within the meniscus. Grade 3 was defined as a linear alteration continuous with the meniscus surface. In this study, healing was classified as grades 0 to 2 and non-healing was designated as grade 3. Two independent observers (BSC and JW) measured the MRI healing grades. Interobserver and intraobserver reliability was assessed, and a second set of measurements was obtained 1 month after the first measurement.
Statistical Analysis
Parametric data were analyzed using an independent t-test or Mann-Whitney U-test according to normal distribution. Categorical data were analyzed using the Fisher exact test or chi-square test to compare meniscal healing with previously reported data. A repeated measures analysis of variance was employed to compare clinical scores at different time points. Additionally, to determine the relationship between clinical scores and healing, statistical differences in changes in clinical scores between healing and non-healing groups were examined. A post-hoc power analysis was performed to calculate the power of the present study (1-β probability). To evaluate the intra- and interobserver reliability, the intraclass correlation coefficients (ICCs) were calculated, accompanied by a 95% CI and the standard error of the measurement. Statistical significance was set at 0.05. IBM SPSS version 25.0 (IBM Corp.) was used for all statistical analyses.
RESULTS
Thirty patients (15 women and 15 men) with a mean age of 46.8 ± 15.2 years (range, 21–72 years) underwent meniscal repair with bone marrow aspirate. They were followed for a mean of 25.1 ± 3.4 months (range, 24–41 months) after surgery. Demographic, operative, and radiographic data were collected preoperatively (Table 1). Of these patients, 22 (73%) had horizontal meniscal tears and 8 (27%) had radial tears. Among those with horizontal meniscal tears, the all-inside technique was utilized in 17 patients (77%). For patients with radial tears, the all-inside method was applied in 5 patients (63%). There was no statistically significant difference between the 2 tear patterns (p = 0.461). The remaining patients were treated using the inside-out technique.
Table 1. Preoperative Demographic Characteristics, Lesion Features, and Radiographic Data.
| Variable | Value | ||
|---|---|---|---|
| Number of patients | 30 | ||
| Demographic data | |||
| Age (yr) | 46.8 ± 15.2 (21 to 72) | ||
| Female sex | 15 (50) | ||
| Involved side of knee (right) | 21 (70) | ||
| Body mass index (kg/m2) | 24.5 ± 2.8 (18.6 to 30.3) | ||
| Follow-up period (mo) | 25.1 ± 3.4 (24 to 41) | ||
| Side of tear | |||
| Medial meniscus | 19 (63) | ||
| Lateral meniscus | 11 (37) | ||
| Pattern of tear | |||
| Horizontal tear | 22 (73) | ||
| Radial tear | 8 (27) | ||
| Technique of repair | |||
| All-inside repair | 22 (73) | ||
| Inside-out repair | 8 (27) | ||
| Preoperative radiographic data | |||
| HKAA (°) | 178.5 ± 3.0 (173.9 to 184.8) | ||
| mLDFA (°) | 86.7 ± 3.1 (81.7 to 95.8) | ||
| MPTA (°) | 86.9 ± 2.4 (81.6 to 93.4) | ||
| JLCA | 1.6 ± 1.9 (–4.1 to 4.6) | ||
| JLOA (°) | 2.5 ± 2.8 (–5.0 to 6.8) | ||
| K-L grade | |||
| 0 | 18 (60) | ||
| 1 | 5 (17) | ||
| 2 | 7 (23) | ||
Values are presented as mean ± standard deviation (range) or number (%).
HKAA: hip-knee-ankle angle, mLDFA: mechanical lateral distal femur angle, MPTA: medial proximal tibia angle, JLCA: joint line convergence angle, JLOA: joint line orientation angle, K-L: Kellgren-Lawrence.
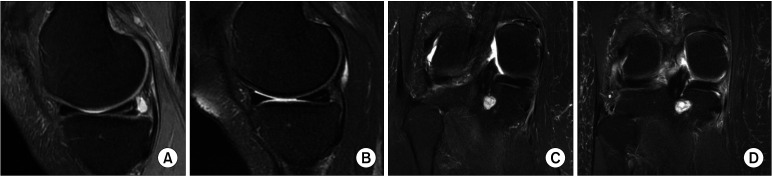
Clinical outcomes, including pain NRS, IKDC subjective score, and Tegner activity scale, all demonstrated statistically significant improvements (Table 2). Preoperatively, all patients had a meniscal tear classification of grade 3. At 3 months after surgery, MRI revealed healing in 18 patients (60%) (3 patients with grade 1, Fig. 3A and B; and 15 patients with grade 2, Fig. 3C and D) and non-healing in 12 patients (40%). Post-hoc power analysis was calculated to be 75.6% using 2 independent proportions (the proportion of healing in the present study and historical study were 60% and 29.6%, respectively). Measurements of MRI healing grade were reproducible, with intraand interobserver ICCs of > 0.80. Changes in clinical scores and the healing rate showed no correlations. Furthermore, there was no statistically significant difference in the healing rate or the change in clinical score according to tear pattern (Table 3).
Table 2. Demographic and Clinical Data in Patients with Medial Meniscus Posterior Root Tears.
| Variable | Preoperative | Postoperative 3 mo | Postoperative 1 yr | Postoperative 2 yr | p-value* |
|---|---|---|---|---|---|
| Pain NRS | 4.8 ± 1.3 | 2.9 ± 1.5 | 1.4 ± 1.0 | 1.2 ± 1.5 | < 0.001† |
| IKDC subjective score | 42.0 ± 10.8 | 48.7 ± 10.6 | 63.2 ± 12.0 | 74.5 ± 13.1 | < 0.001† |
| Lysholm score | 64.1 ± 12.1 | 74.0 ± 11.1 | 85.5 ± 8.3 | 84.9 ± 19.0 | < 0.001† |
| Tegner activity scale | 2.8 ± 1.2 | 2.5 ± 1.0 | 2.5 ± 0.8 | 3.2 ± 1.7 | < 0.001† |
Values are presented as mean ± standard deviation.
NRS: numeric rating scale, IKDC: International Knee Documentation Committee.
*A repeated measured analysis of variance to compare clinical scores at 4 time points. †Statistically significant.
Fig. 3. A 49-year-old female patient who underwent meniscus repair surgery due to a right medial meniscus horizontal tear. (A) Preoperative magnetic resonance imaging (MRI) showing the presence of a meniscus horizontal tear. (B) Three-month postoperative MRI confirming grade 1 healing. A 54-year-old male patient who underwent meniscus repair due to a right lateral meniscus posterior radial tear. (C) Preoperative MRI showing the presence of a radial tear. (D) Three-month postoperative MRI confirming grade II healing.
Table 3. Comparison of Healing Rate and Changes of Clinical Scores According to Tear Pattern.
| Variable | Horizontal tear (n = 22) | Radial tear (n = 8) | p-value |
|---|---|---|---|
| Meniscus healing | 12 (55) | 6 (75) | 0.312 |
| Mean change of pain NRS | –3.8 ± 1.9 | –3.5 ± 2.1 | 0.800 |
| Mean change of IKDC subjective score | 21.7 ± 16.6 | 27.9 ± 17.5 | 0.522 |
| Mean change of Lysholm score | 18.7 ± 14.4 | 13.0 ± 25.7 | 0.564 |
| Mean change of Tegner | 0 ± 1.6 | 0.3 ± 1.3 | 0.781 |
Values are presented as number (%) or mean ± standard deviation.
NRS: numeric rating scale, IKDC: International Knee Documentation Committee.
In 2 patients (a 45-year-old man with a medial meniscus radial tear and a 22-year-old man with a lateral meniscus horizontal tear), retear findings were observed in postoperative 3 months MRI. In these patients, compliance with the rehabilitation protocol was insufficient. Despite experiencing mild knee joint pain, conservative treatment with medications was applied to these patients. No other adverse effects were observed.
DISCUSSION
The most significant findings in this study are as follows: (1) when bone marrow aspirate obtained from the iliac crest was used for repair of horizontal or radial meniscal tears, a favorable healing rate of 60% was observed on MRIs performed at 3 months after surgery, and (2) clinical scores after surgery showed significant improvements compared to preoperative values.
While augmentation methods for meniscal repair, such as synovial trephination,5) fibrin clot,6,7,8) PRP,9,10,11,12) and bone marrow venting procedure,13,14,15,16) have been studied, no studies to date have reported direct injection of bone marrow aspirate into the repair site. Previous studies have revealed the contribution of bone marrow elements to repair healing, showing higher healing rates and better clinical outcomes when meniscal repair is performed simultaneously with anterior cruciate ligament (ACL) reconstruction.6,14,16) Ahn et al.16) have reported a healing rate of 73% for horizontal meniscal tear repairs augmented with marrow stimulation technique using a 5-mm reamer in the intercondylar notch of the femur. The usage of a 5-mm reamer could be considered an invasive procedure with an isolated meniscus tear. Dean et al.15) have found comparable failure rates for meniscal repair between a bone marrow venting procedure and concomitant ACL reconstruction. Previous studies on biological augmentation were less for more challenging horizontal or radial tears, with fewer instances of postoperative MRI evaluations to assess healing rates. Regarding comparison with prior studies (Table 4),6,10,11,13,14,16) the current study demonstrated a statistically significantly higher healing rate than that of the study of Ogawa et al.,13) which specifically investigated horizontal tears with an MRI follow-up (60% vs. 30%, p = 0.022).
Table 4. Comparison of Biological Augmentation Techniques between Current and Previous Studies.
| Study | Augmentation method | Study design | Number of subjects | Age (yr) | Female sex (%) | Follow-up (mo) | Type of tear (%) | Healing rate (%) | Evaluation of healing: method (time, mo) | Clinical score |
|---|---|---|---|---|---|---|---|---|---|---|
| Hashimoto et al.6) | Fibrin clot | Case series | 30 | Mean, 23.2 | 33 | Mean, 25.9 | Horizontal, 30; radial, 10; complex, 20 | 63 | NA (final) | Lysholm, improved Tegner, worsened |
| Griffin et al.10) | PRP | Case control | 15 vs.20 | Mean, 31 | 20 | Mean, 48 | Horizontal, 20 vs. 15; radial, 7 vs. 15; longitudinal, 73 vs. 70 | NA | NA | IKDC, NS Lysholm, NS |
| Kaminski et al.11) | PRP | Case control | 19 vs.18 | Median, 30 vs. 26 | 21 vs. 17 | Median, 54 | Longitudinal | 85 vs. 47 | AS & MR (mean, 4.5) | Pain, NS IKDC PRP, improved |
| Ogawa et al.13) | BM venting | Case series | 52 | Mean, 40.6 | 38 | Mean, 37.5 | Horizontal, 52; longitudinal, 48 | 30 | MR (final) | Lysholm, improved |
| Kaminski et al.14) | BM venting | RCT (vs. ACLR) | 23 vs.21 | Median, 29 vs. 28 | 35 vs. 20 | Median, 44 | Longitudinal | 100 vs. 76 | AS (mean, 35) | Pain, NS IKDC, NS |
| Ahn et al.16) | BM venting | Case series | 32 | Mean, 42.1 | 28 | Mean, 45.6 | Horizontal | 91 | AS (mean, 17.4) | Pain, improved Lysholm, improved Tegner, improved |
| This study | Iliac bone marrow aspirate | Case series | 30 | Mean, 46.8 | 50 | Mean, 25.1 | Horizontal, 73; radial, 27 | 60 | MR (mean, 3) | Pain, improved IKDC, improved Lysholm, improved Tegner, improved |
NA: not applicable, PRP: platelet-rich plasma, IKDC: International Knee Documentation Committee, NS: no significant difference, RCT: randomized controlled trial, AS: arthroscopy, MR: magnetic resonance, BM: bone marrow, ACLR: anterior cruciate ligament reconstruction.
The quantity of bone marrow elements that can be obtained through a bone marrow venting procedure was limited. In addition, information regarding these elements remained unclear. Bone marrow elements contain cells including platelets, progenitor cells, and mesenchymal stem cells. Bone marrow elements also contain enriched growth factors (such as platelet-derived growth factor, vascular endothelial growth factor, transforming growth factor, and bone morphogenic protein-2) and cytokines.21) These cells and growth factors can influence cell behavior and promote mesenchymal stromal cell differentiation to facilitate meniscal healing.22) In our study, bone marrow aspirate was not obtained from the intercondylar notch but rather from the iliac crest. It gave a better yield of bone marrow mesenchymal stem cells. The number of stem cells present in bone marrow aspirates and their clonogenic capacity were higher from the iliac crest than those from the proximal tibia or distal femur.23,24) The aspirate from the iliac crest, rich in progenitor cells and possessing higher efficacy, is assumed to yield superior healing when it is directly injected into the repair site. Additionally, in the present study, BMAC known to require additional equipment and extra cost was not used. This highlights the advantage of using bone marrow aspirate as it can be easily applied to the repair site.
In the present study, all measured clinical scores were improved and maintained for 2 years after surgery. Maheshwer et al.25) have shown that the minimal clinically important difference (MCID) and the patient-acceptable symptomatic state (PASS) for meniscus repair of IKDC scores are 10.9 and 69.0, respectively. Current results revealed an increase of 32.5 in the IKDC subjective score from baseline, reaching 74.5 at 2 years after surgery, surpassing both MCID and PASS thresholds. However, the degree of MRI healing showed no correlation with clinical scores, supporting the study of Miao et al.26) showing that there might be a lack of correlation between radiological results and clinical scores. Nonetheless, further long-term follow-up studies are necessary to determine whether meniscal healing could impact osteoarthritis (OA) progression and long-term clinical outcomes.
Although previous studies have shown that factors such as meniscus tear location,27) age,28) body mass index,29) and limb alignment30) might influence meniscal healing, the current study did not find a correlation with these variables. As the purpose of the current study was not to identify factors influencing the healing rate, further evaluation with a larger number of patients and long-term outcomes is needed.
The present study has certain limitations. First, the retrospective nature of this study was a limitation as it inhibited comprehensive evaluation of control groups. In the surgical database, there were few cases of simple repair without biological augmentation in patients known to have difficult-to-repair horizontal or radial tears. Additionally, the use of fibrin clots, PRP, or bone marrow venting was infrequent. However, a significant strength of this study is that it was the first study to use bone marrow aspirates for meniscus repair augmentation. Secondly, due to the evaluation of MRI scans at only 3 months after surgery, the complete status of meniscal healing might not have been accurately detected. Third, the results of this study might not be applicable to the general population for analysis of OA progression due to the limited number of patients and a short follow-up period. Fourth, there could be a selection bias, as only patients with repairable conditions might have been included. Fifth, the inclusion of both horizontal and radial tears might have acted as a confounding factor. Therefore, further studies are needed to compare based on tear patterns or repair methods in a larger patient population. Nevertheless, the significance of this study lies in the demonstration of a promising healing rate when using bone marrow aspiration as an augmentation in tear patterns traditionally considered difficult to repair.
In conclusion, the use of bone marrow aspirate harvested from the iliac crest can yield favorable healing rates and clinical outcomes for horizontal or radial tears. Our results showed better meniscal healing on MRI compared to previous reports using bone marrow venting procedures.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Becker R, Kopf S, Seil R, Hirschmann MT, Beaufils P, Karlsson J. From meniscal resection to meniscal repair: a journey of the last decade. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3401–3404. doi: 10.1007/s00167-020-06316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung KS, Ha JK, Kim YS, et al. National trends of meniscectomy and meniscus repair in Korea. J Korean Med Sci. 2019;34(32):e206. doi: 10.3346/jkms.2019.34.e206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hong SY, Han W, Jang J, et al. Prognostic factors of midto long-term clinical outcomes after arthroscopic partial meniscectomy for medial meniscal tears. Clin Orthop Surg. 2022;14(2):227–235. doi: 10.4055/cios20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gan JZ, Lie DT, Lee WQ. Clinical outcomes of meniscus repair and partial meniscectomy: does tear configuration matter? J Orthop Surg (Hong Kong) 2020;28(1):2309499019887653. doi: 10.1177/2309499019887653. [DOI] [PubMed] [Google Scholar]
- 5.Shelbourne KD, Benner RW, Nixon RA, Gray T. Evaluation of peripheral vertical nondegenerative medial meniscus tears treated with trephination alone at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2015;31(12):2411–2416. doi: 10.1016/j.arthro.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 6.Hashimoto Y, Nishino K, Orita K, et al. Biochemical characteristics and clinical result of bone marrow-derived fibrin clot for repair of isolated meniscal injury in the avascular zone. Arthroscopy. 2022;38(2):441–449. doi: 10.1016/j.arthro.2021.05.026. [DOI] [PubMed] [Google Scholar]
- 7.Kale S, Deore S, Gunjotikar A, Singh S, Ghodke R, Agrawal P. Arthroscopic meniscus repair and augmentation with autologous fibrin clot in Indian population: a 2-year prospective study. J Clin Orthop Trauma. 2022;32:101969. doi: 10.1016/j.jcot.2022.101969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chahla J, Kennedy NI, Geeslin AG, et al. Meniscal repair with fibrin clot augmentation. Arthrosc Tech. 2017;6(6):e2065–e2069. doi: 10.1016/j.eats.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Everhart JS, Cavendish PA, Eikenberry A, Magnussen RA, Kaeding CC, Flanigan DC. Platelet-rich plasma reduces failure risk for isolated meniscal repairs but provides no benefit for meniscal repairs with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(8):1789–1796. doi: 10.1177/0363546519852616. [DOI] [PubMed] [Google Scholar]
- 10.Griffin JW, Hadeed MM, Werner BC, Diduch DR, Carson EW, Miller MD. Platelet-rich plasma in meniscal repair: does augmentation improve surgical outcomes? Clin Orthop Relat Res. 2015;473(5):1665–1672. doi: 10.1007/s11999-015-4170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaminski R, Kulinski K, Kozar-Kaminska K, et al. A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. Biomed Res Int. 2018;2018:9315815. doi: 10.1155/2018/9315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie Y, Xing Q, Wang S, Yang Z, Hu A, Wu Q. Can platelet-rich plasma enhance the effect of meniscus repair? A meta-analysis of randomized controlled trials Platelet-rich plasma and meniscus repair. J Orthop Surg (Hong Kong) 2022;30(3):10225536221131483. doi: 10.1177/10225536221131483. [DOI] [PubMed] [Google Scholar]
- 13.Ogawa H, Matsumoto K, Sengoku M, Yoshioka H, Akiyama H. Arthroscopic repair of horizontal cleavage meniscus tears provides good clinical outcomes in spite of poor meniscus healing. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3474–3480. doi: 10.1007/s00167-019-05782-y. [DOI] [PubMed] [Google Scholar]
- 14.Kaminski R, Kulinski K, Kozar-Kaminska K, Wasko MK, Langner M, Pomianowski S. Repair augmentation of unstable, complete vertical meniscal tears with bone marrow venting procedure: a prospective, randomized, double-blind, parallel-group, placebo-controlled study. Arthroscopy. 2019;35(5):1500–1508. doi: 10.1016/j.arthro.2018.11.056. [DOI] [PubMed] [Google Scholar]
- 15.Dean CS, Chahla J, Matheny LM, Mitchell JJ, LaPrade RF. Outcomes after biologically augmented isolated meniscal repair with marrow venting are comparable with those after meniscal repair with concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(6):1341–1348. doi: 10.1177/0363546516686968. [DOI] [PubMed] [Google Scholar]
- 16.Ahn JH, Kwon OJ, Nam TS. Arthroscopic repair of horizontal meniscal cleavage tears with marrow-stimulating technique. Arthroscopy. 2015;31(1):92–98. doi: 10.1016/j.arthro.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 17.Koch M, Hammer S, Fuellerer J, et al. Bone marrow aspirate concentrate for the treatment of avascular meniscus tears in a one-step procedure-evaluation of an in vivo model. Int J Mol Sci. 2019;20(5):1120. doi: 10.3390/ijms20051120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bakowski P, Mieloch AA, Porzucek F, et al. Meniscus repair via collagen matrix wrapping and bone marrow injection: clinical and biomolecular study. Int Orthop. 2023;47(10):2409–2417. doi: 10.1007/s00264-023-05711-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 20.Jo C, Hwang D, Ko S, et al. Deep learning-based landmark recognition and angle measurement of full-leg plain radiographs can be adopted to assess lower extremity alignment. Knee Surg Sports Traumatol Arthrosc. 2023;31(4):1388–1397. doi: 10.1007/s00167-022-07124-x. [DOI] [PubMed] [Google Scholar]
- 21.Schafer R, DeBaun MR, Fleck E, et al. Quantitation of progenitor cell populations and growth factors after bone marrow aspirate concentration. J Transl Med. 2019;17(1):115. doi: 10.1186/s12967-019-1866-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blough CL, Bobba CM, DiBartola AC, et al. Biologic augmentation during meniscal repair. J Knee Surg. 2023;36(5):498–506. doi: 10.1055/s-0041-1739198. [DOI] [PubMed] [Google Scholar]
- 23.Cavallo C, Boffa A, de Girolamo L, et al. Bone marrow aspirate concentrate quality is affected by age and harvest site. Knee Surg Sports Traumatol Arthrosc. 2023;31(6):2140–2151. doi: 10.1007/s00167-022-07153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vasiliadis AV, Galanis N. Human bone marrow-derived mesenchymal stem cells from different bone sources: a panorama. Stem Cell Investig. 2020;7:15. doi: 10.21037/sci-2020-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maheshwer B, Wong SE, Polce EM, et al. Establishing the minimal clinically important difference and patient-acceptable symptomatic state after arthroscopic meniscal repair and associated variables for achievement. Arthroscopy. 2021;37(12):3479–3486. doi: 10.1016/j.arthro.2021.04.058. [DOI] [PubMed] [Google Scholar]
- 26.Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011;39(4):735–742. doi: 10.1177/0363546510388930. [DOI] [PubMed] [Google Scholar]
- 27.Borque KA, Laughlin MS, Webster E, Jones M, Pinheiro VH, Williams A. A comparison of all-inside and inside-out meniscal repair in elite athletes. Am J Sports Med. 2023;51(3):579–584. doi: 10.1177/03635465221147058. [DOI] [PubMed] [Google Scholar]
- 28.Rohde MS, Shea KG, Dawson T, et al. Age, sex, and BMI differences related to repairable meniscal tears in pediatric and adolescent patients. Am J Sports Med. 2023;51(2):389–397. doi: 10.1177/03635465221145939. [DOI] [PubMed] [Google Scholar]
- 29.Sommerfeldt MF, Magnussen RA, Randall KL, et al. The relationship between body mass index and risk of failure following meniscus repair. J Knee Surg. 2016;29(8):645–648. doi: 10.1055/s-0035-1569480. [DOI] [PubMed] [Google Scholar]
- 30.Yeo DY, Suhaimi F, Parker DA. Factors predicting failure rates and patient-reported outcome measures after arthroscopic meniscal repair. Arthroscopy. 2019;35(11):3146–3164. doi: 10.1016/j.arthro.2019.06.016. [DOI] [PubMed] [Google Scholar]