Abstract
Backgroud
Different from adults, adolescents with genu varum or valgum can be treated with hemi-epiphysiodesis. We conducted a study to report our recent experience of treating idiopathic genu varum and valgum with clinical relevance to planning of hemi-epiphysiodesis. The aim of this study was to compare the varus and valgus groups focusing on the contribution of the distal femur and proximal tibia to the deformities.
Methods
Among patients who visited the outpatient clinic during the recent 4 years, adolescents with genu varum (the varus group) or valgum (the valgus group) greater than 5° were included. The mechanical lateral distal femoral angle (mLDFA) and medial proximal tibial angle (MPTA) were measured. The contribution to deformity (%) in each of the distal femur and the proximal tibia was calculated.
Results
One hundred twenty patients and their 120 legs (randomly selected in bilateral cases) were included. In the varus group (n = 51), the mean hip-knee-ankle alignment was varus 7.1° (range, 5.1°–12.1°). The contribution to deformity was 74.1% ± 27.6% at the proximal tibia (MPTA, 81.9° ± 2.0°) and 14.9% ± 25.1% at the distal femur (mLDFA, 88.1° ± 1.7°). In the valgus group (n = 69), the mean alignment was valgus 6.6° (range, 5.1°–11.9°). The contribution was 69.8% ± 30.8% at the distal femur (mLDFA, 82.4° ± 2.1°) and 33.1% ± 27.8% at the proximal tibia (MPTA = 89.2° ± 1.9°). In subgroup analyses, the MPTA was significantly lower in the varus ≥ 8.4° group than the varus < 8.4° group. The mLDFA was significantly lower and the frequency of MPTA > 91.5° was significantly higher in the valgus ≥ 7.7° group than the valgus < 7.7° group.
Conclusions
Genu varum was mainly associated with deformity of the proximal tibia, whereas genu valgum was related to deformities of the distal femur and proximal tibia. Considering the predominant deformity of the proximal tibia, performing hemi-epiphysiodesis only at the proximal tibia is ideal in most adolescents with genu varum.
Keywords: Coronal plane alignment, Genu varum, Tibia vara, Genu valgum, Hemiepiphysiodesis
Coronal angular deformities around the knee, genu varum and genu valgum, are not rare in adolescent patients and often managed by pediatric orthopedic surgeons.1,2) The alignment abnormalities of the lower extremities may be asymptomatic during adolescence.3) However, the asymmetric load distribution on the knee joint can increase the risk of development and progression of its degenerative changes.4)
Different from adults with the malalignment that can be corrected by surgery including some types of osteotomies, adolescents with genu varum or genu valgum can be treated with hemi-epiphysiodesis, a simpler surgical procedure.5,6,7,8) In order to obtain anatomical correction of angular deformity, it is necessary to accurately determine what anatomical structures caused the deformity. Regarding correction of genu varum or valgum by performing hemi-epiphysiodesis, the distal femoral and proximal tibial physes are good targets as they are close to the knee joint, the center of the deformities, and account for most of the growth of the lower extremity.9) If there is only 1 deformed segment between the 2 (distal femur or proximal tibia), only correcting the deformed segment should be ideal. The expected degree of correction after hemi-epiphysiodesis until the end of growth maturation is correlated with the amount of growth remaining in the same growing patient. If the surgery is performed at both segments, faster correction of the same degree can be obtained compared to the surgery performed at only 1 segment. In other words, genu varum or valgum combined with 1 normal segment and another deformed segment should be operated at an earlier age. Many previous studies on hemi-epiphysiodesis to correct coronal angular deformities in growing patients have reported their favorable results.5,6,7,8,10,11) However, studies dealing with each contribution of the distal femur and proximal tibia to the deformities are rare.6)
On this background, we conducted a study to report our recent experience of treating idiopathic genu varum and valgum with clinical relevance to planning of hemie-piphysiodesis. The aim of this study was to compare the varus and valgus groups focusing on the contribution of the distal femur and proximal tibia to the deformities. It was hypothesized that the distal femoral physis and the proximal tibial physis contribute in different ways in the varus and valgus groups as varus and valgus deformities around the knee are dissimilar in many respects including bone morphology and soft-tissue laxity.12,13,14)
METHODS
The Institutional Review Board of the Samsung Medical Center approved the study protocol (IRB No. 2024-04-018). The informed consent was waived.
Selection of the Study Participants
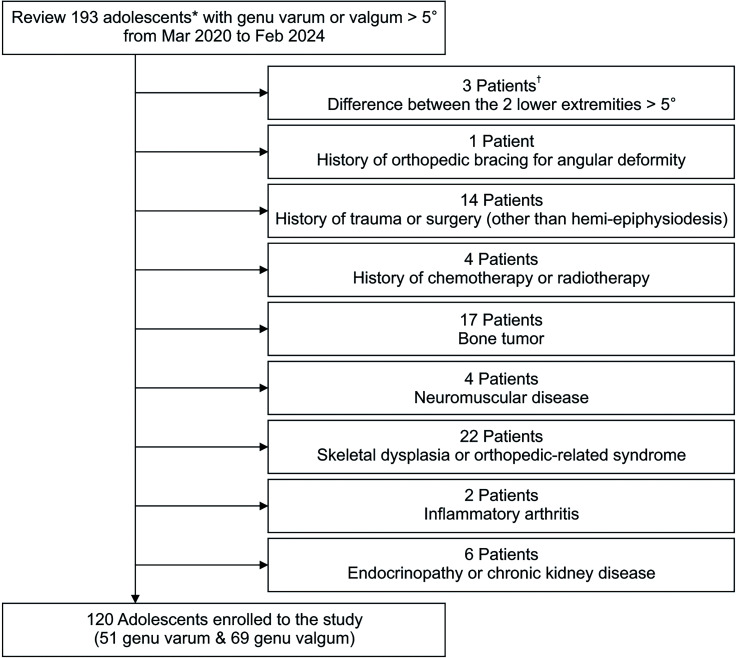
Among patients who visited the outpatient clinic of the corresponding author from March 2020 to February 2024, the study participants were selected. Inclusion criteria were as follows: (1) genu varum (the varus group) or valgum (the valgus group) greater than 5° based on the hip-knee-ankle (HKA) alignment at least 1 of the 2 lower extremities; (2) chronological age < 18 years and bone age ≥ 12.5 years in boys (≥ 10.5 years in girls) based on the time point of the deformity. Among several time points in the same patient, 1 time just before hemi-epiphysiodesis (if performed) or that nearest from the end of growth maturation (if not) was used. Exclusion criteria were as follows: (1) side-to-side difference (STSD) of the HKA alignment between the 2 lower extremities > 5°; (2) history of orthopedic bracing for angular deformity; (3) history of trauma or surgery (other than hemi-epiphysiodesis) in the leg; (4) history of chemotherapy or radiotherapy; (5) bone tumor; (6) neuromuscular disease; (7) skeletal dysplasia (diagnosed or suspected); (8) orthopedic-related syndrome; (9) inflammatory arthritis; and (10) endocrinopathy or chronic kidney disease. After being assessed for eligibility, 120 patients were enrolled to the study (Fig. 1). There were 76 boys and 44 girls, and there were no foreigners. The mean age of the 120 patients was 13.0 ± 1.6 years. Considering the principle of statistical independence,15) 1 side was randomly selected, if both lower extremities met the above criteria, using a program that was freely available (http://www.randomizer.org). Finally, a total of 51 and 69 knees were enrolled to the varus and valgus groups, respectively.
Fig. 1. Flowchart describing the enrollment process. *Patients with the chronological age < 18 years and bone age ≥ 12.5 years in boys (≥ 10.5 years in girls). †If the patients were already excluded due to the prior criterion, they were not repeatably counted.
Radiographic Measurement
Study participants were considered a candidate for hemi-epiphysiodesis. Thus, a radiograph of the hand and wrist was obtained to estimate the bone age and to determine the timing for surgery. The remaining period of growth was calculated using a radiological atlas16) based on the bone age with the assumption that growth around the knee ends at 16 years in boys and 14 years in girls.17) If the finding did not fit both adjacent standards, the mean value of the 2 standards was used.5) The HKA alignment was defined as an alignment between the mechanical axis of the femur and that of the tibia and measured from a standing full-length anteroposterior radiograph of the lower extremities. To minimize measurement errors, the radiograph was taken with the both knees fully extended and the both patellae facing forwards. The mechanical lateral distal femoral angle (mLDFA) and medial proximal tibial angle (MPTA) were measured to describe each alignment of the distal femur and the proximal tibia.18) The neutral alignment was defined as a range of ± 1.5° from the reference value (87° for mLDFA and MPTA), and the alignment was further divided with ranges of 3°.13,14,19)
The contribution of the segment was calculated as follows:
If the MPTA was 81° and the HKA alignment was varus 8°, the contribution of the proximal tibia was
If deformity of the segment and the HKA alignment were reverse (varus and valgus), the contribution was presented as negative (−). The joint line convergence angle (JLCA) was measured as the angle between the line connecting the articular surface of the distal femur and that of the proximal tibia. A medial apex was presented as positive (+), while a lateral apex as negative (−). In addition to radiographic measurement, the body mass index (BMI) at the same time with the radiograph was used as demographic data. All radiographic indicators were measured using the PACS system (Picture Archiving and Communication System; GE Healthcare). All indicators were measured twice (at intervals of minimum 2 weeks) by 2 observers (JWS and KRK), and the calculated mean values were used. The intra- and interobserver differences in measuring the radiographic indicators were assess by calculating intraclass correlation coefficients (ICCs). The reliabilities for the bone age, HKA alignment, mLDFA, MPTA, and JLCA were excellent to good.20) Details of the ICCs are presented in Table 1.
Table 1. Intraclass Correlation Coefficients of Intra- and Interobserver Differences in Measuring Radiographic Indicators.
| Variable | Observer 1* | Observer 2* | Interobserver† |
|---|---|---|---|
| Bone age (yr) | 0.86 | 0.88 | 0.86 |
| HKA alignment (°) | 0.94 | 0.93 | 0.92 |
| mLDFA (°) | 0.87 | 0.85 | 0.85 |
| MPTA (°) | 0.84 | 0.86 | 0.83 |
| JLCA (°) | 0.90 | 0.91 | 0.88 |
HKA: hip-knee-ankle, mLDFA: mechanical lateral distal femoral angle, MPTA: medial proximal tibial angle, JLCA: joint line convergence angle.
*Calculated using the 2 measured values in each observer. †Calculated using the mean of 2 measurements in the observer 1 and that in the observer 2.
Statistical Analysis
All numerical data are presented as mean ± standard deviation to 1 decimal place. The chi-square test, Fisher’s exact test, independent t-test, and Mann-Whitney U-test were used to compare data between 2 groups. First, the varus and valgus groups were compared. Second, subgroup analyses were performed by dividing both groups based on the 75th percentile of the HKA alignment (8.4° in the varus group and 7.7° in the valgus group, respectively). Correlation analyses were used to analyze the associations of the mLDFA, JLCA, and MPTA with the HKA alignment. The coefficients (r) of ≤ 0.35 (in absolute value) were considered weak correlations, 0.36–0.67 moderate correlations, and ≥ 0.68 strong correlations.21) R ver. 4.2.0 (R Foundation for Statistical Computing) was used with the significance level set at p < 0.05.
RESULTS
In the varus group (n = 51), the HKA alignment was varus 7.1° ± 1.8° (range, 5.1°–12.1°) with the growth remaining of 1.4 ± 1.0 years. The alignment was valgus 6.6° ± 1.5° (range, 5.1°–11.9°) with the growth remaining of 1.9 ± 0.7 years in the valgus group (n = 69). The remaining period of growth was shorter and the BMI was lower (older and thinner) in the varus group. In the varus group, the contribution to deformity was 74.1% ± 27.6% at the proximal tibia (MPTA, 81.9° ± 2.0°) and 14.9 ± 25.1% at the distal femur (mLDFA, 88.1° ± 1.7°). The contribution was 69.8% ± 30.8% at the distal femur (mLDFA, 82.4° ± 2.1°) and 33.1% ± 27.8% at the proximal tibia (MPTA, 89.2° ± 1.9°) in the valgus group. The contribution of the distal femur was significantly higher in the valgus group compared to the varus group, and that of the proximal tibia was significantly higher in the varus group. Details of the 2 groups and their comparisons are presented in Table 2.
Table 2. Comparisons of Demographic Characteristics and Radiographic Measurements between the Varus and Valgus Groups.
| Variable | Varus (n = 51) | Valgus (n = 69) | p-value |
|---|---|---|---|
| Sex (male : female) | 29 (56.9) : 22 (43.1) | 47 (68.1) : 22 (31.9) | 0.283* |
| Bone age (yr) | 13.8 ± 1.5 | 13.5 ± 1.0 | 0.218† |
| Growth remaining (yr) | 1.4 ± 1.0 | 1.9 ± 0.7 | 0.003† |
| Body mass index (kg/m2) | 18.6 ± 2.1 | 24.2 ± 3.6 | <0.001† |
| Side (right : left) | 22 (43.1) : 29 (56.9) | 38 (55.1) : 31 (44.9) | 0.268* |
| HKA alignment (°) | Varus 7.1 ± 1.8 (5.1–12.1) | Valgus 6.6 ± 1.5 (5.1–11.9) | 0.167†,‡ |
| mLDFA (°) | 88.1 ± 1.7 | 82.4 ± 2.1 | < 0.001† |
| Contribution of the distal femur (%) | 14.9 ± 25.1 | 69.8 ± 30.8 | < 0.001† |
| MPTA (°) | 81.9 ± 2.0 | 89.2 ± 1.9 | < 0.001† |
| Contribution of the proximal tibia (%) | 74.1 ± 27.6 | 33.1 ± 27.8 | < 0.001† |
| JLCA (°) | 0.8 ± 0.9 | 0.2 ± 0.8 | < 0.001† |
Values are presented as number (%), mean ± SD, or mean ± SD (range).
HKA: hip-knee-ankle, mLDFA: mechanical lateral distal femoral angle, MPTA: medial proximal tibial angle, JLCA: joint line convergence angle, SD: standard deviation.
*Chi-square test. †Independent t-test. ‡Comparison between the absolute values.
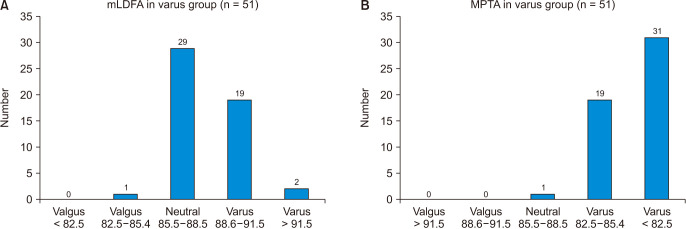
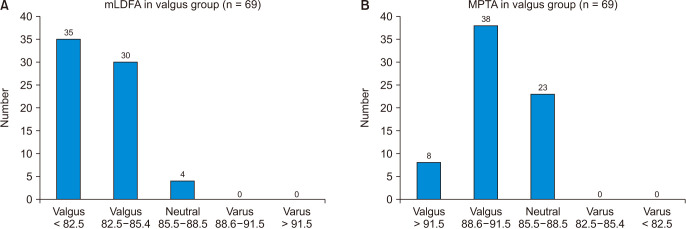
Among the 51 varus limbs, all but 1 (98.0%) showed a varus alignment of the proximal tibia. Specifically, 31 limbs (60.8%) showed a varus alignment with the MPTA < 82.5°. In contrast, 30 limbs (58.8%) had a non-varus alignment of the distal femur. Among the 69 valgus limbs, 65 limbs (94.2%) showed a valgus alignment of the distal femur. Specifically, 35 limbs (50.7%) showed a valgus alignment with the mLDFA < 82.5°. On the other hand, 46 limbs (66.7%) had a valgus alignment, and 23 limbs (33.3%) had a neutral alignment of the proximal tibia. The distribution of the mLDFA and MPTA in the varus and valgus groups are shown in Figs. 2 and 3.
Fig. 2. The distribution of the alignment of the mechanical lateral distal femoral angle (mLDFA; A) and medial proximal tibial angle (MPTA; B) in the varus group (n = 51). The left side of the x-axis indicates a valgus alignment, and the right indicates a varus alignment. It means more severe deformity as it is more peripherally located.
Fig. 3. The distribution of the alignment of the mechanical lateral distal femoral angle (mLDFA; A) and medial proximal tibial angle (MPTA; B) in the valgus group (n = 69). The left side of the horizontal axis indicates a valgus alignment, and the right indicates a varus alignment. It means more severe deformity as it is more peripherally located.
Among the 3 radiographic idicators around the knee (mLDFA, JLCA, and MPTA), only the MPTA showed a moderate correlation (r = −0.469) with the HKA alignment in the varus group. The mLDFA and JLCA had a weak correlation (r = 0.334 and r = 0.241, respectively) with the HKA alignment. In the valgus group, only the mLDFA showed a moderate correlation (r = 0.434) with the HKA alignment. The correlation of the JLCA and MPTA with the HKA alignment was weak (r = 0.026 and r = −0.314, respectively).
Subgroup Analysis
The MPTA was significantly lower and the frequency of MPTA < 82.5° was significantly higher in the varus ≥ 8.4° group compared to the varus < 8.4° group. In contrast, the mLDFA and the frequency of mLDFA > 91.5° were not significantly different between the 2 groups. In other words, severe genu varum was mainly associated with severe deformity of the proximal tibia. The mLDFA was significantly lower and the frequency of MPTA > 91.5° was significantly higher in the valgus ≥ 7.7° group compared to the valgus < 7.7° group. In other words, severe genu valgum was related to severe deformity of the distal femur, as well as that of the proximal tibia. Details of comparisons between the subgroups are presented in Tables 3 and 4.
Table 3. Comparisons between the Varus ≥ 8.4° and Varus < 8.4° Groups.
| Variable | Varus ≥ 8.4° (n = 13) | Varus < 8.4° (n = 38) | p-value |
|---|---|---|---|
| Sex (male : female) | 9 (69.2) : 4 (30.8) | 20 (52.6) : 18 (47.4) | 0.472* |
| Bone age (yr) | 14.5 ± 1.4 | 13.5 ± 1.4 | 0.066† |
| Growth remaining (yr) | 0.9 ± 1.3 | 1.5 ± 0.9 | 0.100† |
| Body mass index (kg/m2) | 19.1 ± 1.8 | 18.4 ± 2.1 | 0.198† |
| Side (right : left) | 4 (30.8) : 9 (69.2) | 18 (47.4) : 20 (52.6) | 0.472* |
| HKA alignment (°) | Varus 9.5 ± 1.1 (8.4–12.1) | Varus 6.2 ± 0.9 (5.1–8.3) | < 0.001† |
| mLDFA (°) | 88.5 ± 2.0 | 88.0 ± 1.6 | 0.417† |
| Frequency of mLDFA > 91.5° | 1 (7.7) | 1 (2.6) | 0.449‡ |
| Contribution of the distal femur (%) | 15.2 ± 20.0 | 14.9 ± 26.9 | 0.991† |
| MPTA (°) | 80.0 ± 2.0 | 82.5 ± 1.6 | < 0.001† |
| Frequency of MPTA < 82.5° | 12 (92.3) | 19 (50.0) | 0.018* |
| Contribution of the proximal tibia (%) | 73.8 ± 20.1 | 74.2 ± 30.0 | 0.804† |
| JLCA (°) | 1.0 ± 1.3 | 0.7 ± 0.8 | 0.127† |
Values are presented as number (%), mean ± SD, or mean ± SD (range).
HKA: hip-knee-ankle, mLDFA: mechanical lateral distal femoral angle, MPTA: medial proximal tibial angle, JLCA: joint line convergence angle, SD: standard deviation.
*Chi-square test. †Mann-Whitney U-test. ‡Fisher’s exact test.
Table 4. Comparisons between the Valgus ≥ 7.7° and Valgus < 7.7° Groups.
| Variable | Valgus ≥ 7.7° (n = 18) | Valgus < 7.7° (n = 51) | p-value |
|---|---|---|---|
| Sex (male : female) | 12 (66.7) : 6 (33.3) | 35 (68.6) : 16 (31.4) | 1.000* |
| Bone age (yr) | 13.2 ± 1.1 | 13.6 ± 1.0 | 0.101† |
| Growth remaining (yr) | 2.1 ± 0.8 | 1.8 ± 0.7 | 0.040† |
| Body mass index (kg/m2) | 24.3 ± 4.1 | 24.2 ± 3.4 | 0.785† |
| Side (right : left) | 11 (61.1) : 7 (38.9) | 27 (52.9) : 24 (47.1) | 0.746* |
| HKA alignment (°) | Valgus 8.8 ± 1.2 (7.7–11.9) | Valgus 5.9 ± 0.7 (5.1–7.5) | < 0.001† |
| mLDFA (°) | 81.2 ± 2.2 | 82.9 ± 1.9 | 0.007† |
| Frequency of mLDFA < 82.5° | 13 (72.2) | 22 (43.1) | 0.065* |
| Contribution of the distal femur (%) | 66.0 ± 19.8 | 71.1 ± 33.9 | 0.243† |
| MPTA (°) | 89.9 ± 2.0 | 89.0 ± 1.8 | 0.073† |
| Frequency of MPTA > 91.5° | 5 (27.8) | 3 (5.9) | 0.024‡ |
| Contribution of the proximal tibia (%) | 34.1 ± 22.6 | 32.8 ± 29.7 | 0.897† |
| JLCA (°) | 0.0 ± 1.0 | 0.2 ± 0.8 | 0.094† |
Values are presented as number (%), mean ± SD, or mean ± SD (range).
HKA: hip-knee-ankle, mLDFA: mechanical lateral distal femoral angle, MPTA: medial proximal tibial angle, JLCA: joint line convergence angle, SD: standard deviation.
*Chi-square test. †Mann-Whitney U-test. ‡Fisher’s exact test.
DISCUSSION
The most important finding of this study is that genu varum was mainly associated with deformity of the proximal tibia and that genu valgum was related to deformities of the distal femur as well as proximal tibia in adolescents. Different from adults who need to undergo an osteotomy to correct coronal deformities around the knee, growing patients can be treated with hemi-epiphysiodesis with minimal morbidity.5,6,7,8,10,11) Our findings have relevance to planning of hemi-epiphysiodesis to correct genu varum or valgum in adolescents. The predominant deformity of the proximal tibia in the varus group suggests the need for hemi-epiphysiodesis only at the proximal tibia for anatomical correction in most adolescents with genu varum. The amount of growth remaining in the distal femur is relatively greater than that in the proximal tibia in growing patients.9) It means that at least twice the remaining period of growth is needed when performing hemi-epiphysiodesis only at the proximal tibia compared to hemi-epiphysiodesis performed at both distal femur and proximal tibia to correct the same degree of deformity. Regarding the valgus group, the distal femur, the main contributor of growth around the knee, showed higher contribution (69.8% ± 30.8%) with the contribution of about one-third at the proximal tibia (33.1% ± 27.8%). In summary, the possibility of needing an earlier surgery should be considered in genu varum than genu valgum with the same degree of deformity.
The predominant tibial deformity of the varus group suggests the possibility that our study participants can be classified as having the adolescent form of tibia vara. There are 3 forms of tibia vara: infantile, juvenile, and adolescent, based on the age at the onset of the deformity.22) This study only included the idiopathic cases that seemed to be developmental variations without definite pathology. To exclude patients with the undiscovered focal lesion around the distal femoral or proximal tibial physes, the STSD > 5° of the HKA alignment was used as exclusion criteria. One of other exclusion criteria was a history of orthopedic bracing for angular deformity. Thus, it is difficult to say that the study participants in the varus group had sequelae or remaining deformities of infantile tibia vara. Nevertheless, mild deformity that occurred in the infantile or juvenile period may have persisted until the adolescent period. The etiology of tibia vara is not clear. But the association with obesity especially in juvenile and adolescent forms has been consistently reported in the West.22,23,24,25) It is noteworthy that the mean BMI was 18.6 ± 2.1 kg/m2 in our 51 adolescents with genu varum, as the finding contrasts to the prior reports in the West. None of the varus group had BMI ≥ 25 kg/m2. It is difficult to determine the etiology of idiopathic genu varum based only on our results. However, we hope readers pay more attention to our clinical experience of treating adolescents with idiopathic genu varum not associated with obesity. Other than obesity, the association between high activity levels and genu varum in adolescents has been repeatedly reported.26,27,28) Not including the degree of sports participation was a limitation of our study. However, the aim of our study was not to identify the etiology of coronal deformities around the knee. Future studies on the topic should cover various factors of weight-bearing including obesity and sports participation.
The remaining period of growth was longer in the valgus group in the comparisons between the varus and valgus groups. Study participants in both groups were idiopathic cases without definite pathology. We believe that their degree of deformity used in the analyses would not have changed significantly over a few years. Therefore, it is difficult to say that the difference of the remaining period has clinical significance. With regard to BMI, it was higher (24.2 ± 3.6 kg/m2) in the valgus group than the varus group (18.6 ± 2.1 kg/m2). On the other hand, severe genu valgum was not related to higher BMI in subgroup analyses between the valgus ≥ 7.7° and valgus < 7.7° groups. Walker et al.1) reported the association of obesity with idiopathic genu valgum. Among their 66 study subjects averagely aged 12.2 years, 47% had BMI ≥ 30 kg/m2 and 71% were categorized as obese. Obviously, the difference between the East and the West should be considered to interpret the findings. This study was limited by its cross-sectional design. Thus, it is difficult to conclude the causal relationship of obesity with the occurrence of genu valgum. Our opinion on the relatively high BMI in the valgus group and the relatively low BMI in the varus group is as follows: It is thought that high BMI and accompanying thick legs in the valgus group would have made the intermalleolar distance (between both ankles) more distant and facilitated the patients to visit the hospital with concern about the appearance compared to thin patients with the similar radiographic alignment of genu valgum. It is also thought that low BMI and accompanying thin legs in the varus group would have made the intercondylar distance (between the both knees) more distant and the fibular heads more prominent and facilitated the patients to visit the doctor compared to patients with thick legs and the similar radiographic alignment of genu varum.
There were several other limitations of this study. First, we could not discuss the actual prevalence rate of genu varum or valgum owing to our study design. Second, the lack of patient-reported outcome measures, associated with pain and limited function, was also a limitation. However, idiopathic coronal deformities around the knee in adolescents were not related to pain or limited function in most patients.3) Last, this study was also limited by the possibility of bias and type II errors because of the small number of study participants. To study the most up-to-date trends, we limited the study period to recent 4 years.
In our cohort of adolescents with idiopathic coronal deformities, genu varum was mainly associated with deformity of the proximal tibia, whereas genu valgum was related to deformities of the distal femur as well as proximal tibia. Considering the predominant contribution of the proximal tibia, performing hemi-epiphysiodesis only at the proximal tibia is ideal to obtain anatomical correction in most adolescents with genu varum. Thus, the possibility of needing an earlier surgery should be considered in idiopathic genu varum than genu valgum with the same degree of deformity.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Walker JL, Hosseinzadeh P, White H, et al. Idiopathic genu valgum and its association with obesity in children and adolescents. J Pediatr Orthop. 2019;39(7):347–352. doi: 10.1097/BPO.0000000000000971. [DOI] [PubMed] [Google Scholar]
- 2.Isin A, Melekoglu T. Genu varum and football participation: does football participation affect lower extremity alignment in adolescents? Knee. 2020;27(6):1801–1810. doi: 10.1016/j.knee.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Carroll KL, Stotts AK, Pearson OC, MacWilliams BA. Patient-reported outcomes of adolescents treated with guided growth to correct idiopathic genu valgum. J Pediatr Orthop. 2023;43(3):162–167. doi: 10.1097/BPO.0000000000002336. [DOI] [PubMed] [Google Scholar]
- 4.Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61(4):459–467. doi: 10.1002/art.24336. [DOI] [PubMed] [Google Scholar]
- 5.Ko KR, Shim JS, Shin TS, Jang MC. Factors affecting rebound phenomenon after temporary hemiepiphysiodesis and implant removal for idiopathic genu valgum in adolescent patients. J Pediatr Orthop. 2022;42(4):e336–e342. doi: 10.1097/BPO.0000000000002090. [DOI] [PubMed] [Google Scholar]
- 6.Lee SW, Lee KJ, Cho CH, et al. Affecting factors and correction ratio in genu valgum or varum treated with percutaneous epiphysiodesis using transphyseal screws. J Clin Med. 2020;9(12):4093. doi: 10.3390/jcm9124093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park BK, Kim HW, Park H, Lee SK, Park KB. Natural behaviours after guided growth for idiopathic genu valgum correction: comparison between percutaneous transphyseal screw and tension-band plate. BMC Musculoskelet Disord. 2022;23(1):1052. doi: 10.1186/s12891-022-05996-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shim JS, Ko KR, Lim KS, Na S. Factors affecting postoperative courses after removal of transphyseal screws inserted for correction of genu valgum. J Pediatr Orthop. 2024;44(5):e411–e418. doi: 10.1097/BPO.0000000000002660. [DOI] [PubMed] [Google Scholar]
- 9.Birch JG, Makarov MA, Jackson TJ, Jo CH. Comparison of Anderson-Green growth-remaining graphs and White-Menelaus predictions of growth remaining in the distal femoral and proximal tibial physes. J Bone Joint Surg Am. 2019;101(11):1016–1022. doi: 10.2106/JBJS.18.01226. [DOI] [PubMed] [Google Scholar]
- 10.Choi KJ, Lee S, Park MS, Sung KH. Rebound phenomenon and its risk factors after hemiepiphysiodesis using tension band plate in children with coronal angular deformity. BMC Musculoskelet Disord. 2022;23(1):339. doi: 10.1186/s12891-022-05310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dai ZZ, Liang ZP, Li H, et al. Temporary hemiepiphysiodesis using an eight-plate implant for coronal angular deformity around the knee in children aged less than 10 years: efficacy, complications, occurrence of rebound and risk factors. BMC Musculoskelet Disord. 2021;22(1):53. doi: 10.1186/s12891-020-03915-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thienpont E, Schwab PE, Cornu O, Bellemans J, Victor J. Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg. 2017;137(3):393–400. doi: 10.1007/s00402-017-2626-x. [DOI] [PubMed] [Google Scholar]
- 13.Mullaji A, Shah R, Bhoskar R, Singh A, Haidermota M, Thakur H. Seven phenotypes of varus osteoarthritic knees can be identified in the coronal plane. Knee Surg Sports Traumatol Arthrosc. 2022;30(8):2793–2805. doi: 10.1007/s00167-021-06676-8. [DOI] [PubMed] [Google Scholar]
- 14.Mullaji A, Bhoskar R, Singh A, Haidermota M. Valgus arthritic knees can be classified into nine phenotypes. Knee Surg Sports Traumatol Arthrosc. 2022;30(9):2895–2904. doi: 10.1007/s00167-021-06796-1. [DOI] [PubMed] [Google Scholar]
- 15.Park MS, Kim SJ, Chung CY, Choi IH, Lee SH, Lee KM. Statistical consideration for bilateral cases in orthopaedic research. J Bone Joint Surg Am. 2010;92(8):1732–1737. doi: 10.2106/JBJS.I.00724. [DOI] [PubMed] [Google Scholar]
- 16.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. Stanford University Press; 1959. [Google Scholar]
- 17.Menelaus MB. Correction of leg length discrepancy by epiphysial arrest. J Bone Joint Surg Br. 1966;48(2):336–339. [PubMed] [Google Scholar]
- 18.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;(280):48–64. [PubMed] [Google Scholar]
- 19.Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S. Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1385–1393. doi: 10.1007/s00167-019-05508-0. [DOI] [PubMed] [Google Scholar]
- 20.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor R. Interpretation of the correlation coefficient: a basic review. J Diagn Med Sonography. 1990;6(1):35–39. [Google Scholar]
- 22.Thompson GH, Carter JR. Late-onset tibia vara (Blount’s disease): current concepts. Clin Orthop Relat Res. 1990;(255):24–35. [PubMed] [Google Scholar]
- 23.Thompson GH, Carter JR, Smith CW. Late-onset tibia vara: a comparative analysis. J Pediatr Orthop. 1984;4(2):185–194. doi: 10.1097/01241398-198403000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Funk SS, Mignemi ME, Schoenecker JG, Lovejoy SA, Mencio GA, Martus JE. Hemiepiphysiodesis implants for late-onset tibia vara: a comparison of cost, surgical success, and implant failure. J Pediatr Orthop. 2016;36(1):29–35. doi: 10.1097/BPO.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 25.Murphy RF, Pacult MA, Barfield WR, Mooney JF. Hemiepiphyseodesis for juvenile and adolescent tibia vara utilizing percutaneous transphyseal screws. J Pediatr Orthop. 2020;40(1):17–22. doi: 10.1097/BPO.0000000000001067. [DOI] [PubMed] [Google Scholar]
- 26.Thijs Y, Bellemans J, Rombaut L, Witvrouw E. Is high-impact sports participation associated with bowlegs in adolescent boys? Med Sci Sports Exerc. 2012;44(6):993–998. doi: 10.1249/MSS.0b013e3182407ca0. [DOI] [PubMed] [Google Scholar]
- 27.De Cock L, Dauwe J, Holzer LA, Bellemans J. Knee alignment in adolescents is correlated with participation in weight-bearing sports. Int Orthop. 2018;42(12):2851–2858. doi: 10.1007/s00264-018-4015-7. [DOI] [PubMed] [Google Scholar]
- 28.Fernquest S, Lloyd T, Pereira C, et al. Coronal-plane leg alignment in adolescence and the effects of activity: a full leg length MRI study. J Orthop Res. 2023;41(5):973–983. doi: 10.1002/jor.25442. [DOI] [PubMed] [Google Scholar]