Abstract
Background
Transverse or short oblique periprosthetic femoral fractures around total hip arthroplasty (THA) stems are typically classified as B1 fractures (stem well-fixed) and usually managed with fixation. These fractures have high non-union rates. This study aimed to identify reoperation rates in patients with operatively managed transverse or short oblique fractures around a cemented polished taper-slip stem and determine any associations with treatment failure.
Methods
This retrospective cohort study included 31 patients with Arbeitsgemeinschaft für Osteosynthesefragen transverse or short oblique Vancouver B1 periprosthetic femoral fractures around THA with a cemented taper slip stem: 12 males (39%); mean age 74 ± 11.9 years (range 44-91); mean BMI 28.5 ± 1.4 (range 16-48); median American Society of Anesthesiologists score 3. Patient journeys were assessed and re-interventions recorded. The primary outcome was reoperation.
Results
The mean time from primary THA to fracture was 11.3 ± 7.8 years (0.5-26 years). Surgical management involved fixation in 27/31 cases and revision-THA (r-THA) in 4/31. Ten patients (32%) required reoperation (8 following ORIF and 2 following r-THA, P = .584), most commonly within 2 years of injury (9/10) due to non-union (6/10). No significant associations with reoperation requirement were identified. Kaplan-Meier survival free from reoperation was 67.4% (95% CI 49.8-85.0) at 2 years, unaffected by initial management with fixation or revision (Log rank 0.898). Of those reoperated, 60% (6/10) required multiple reoperations to achieve bony union or a stable revision construct.
Conclusions
These fractures are challenging to manage with either fixation or revision. Patients should be counseled about a one in 3 risk of reoperation and a one in 5 risk of requiring multiple reoperations.
Keywords: Periprosthetic femoral fractures, Transverse, Short oblique, Non-union, Failure
Introduction
Periprosthetic femoral fractures (PFFs) around total hip arthroplasties (THAs) are increasing in incidence at a rate of 13% per year [[1], [2], [3]]. Their management is challenging and is associated with significant patient morbidity and mortality [4,5]. The surgical management of PFFs is guided by the Unified Classification System (UCS) [6], an expansion of the Vancouver classification, and typically involves fracture fixation when stems are well fixed (B1), and revision arthroplasty where the fracture has rendered the femoral stem loose (B2/B3) [7,8].
The most commonly implanted stem in the United Kingdom is the Exeter V40 (Stryker, Mahwah, NJ). Despite excellent all-cause survival [9,10], polished tapered slip (PTS) stem designs have a higher risk of PFFs than composite beam stem designs [[11], [12], [13], [14]]. The most common fracture type around PTS stems are B2 fractures of a long spiral pattern [15], and recent evidence has suggested that provided these fractures can be anatomically reduced, fixation is associated with lower morbidity and reoperations rates than revision surgery [16]. Long-term follow-up of type B fractures around PTS stems treated with fixation has demonstrated that compared to B2 fractures treated with fixation, fixation failure requiring reoperation is highest among B1 fractures [17]. This may reflect that B1 fractures include fracture patterns associated with longer union times and risk of non-union, such as transverse or short oblique fractures (clinical radiographs of these fracture patterns presented in Figure 1, Figure 2) where there is potentially less surface area for bone healing [17,18].
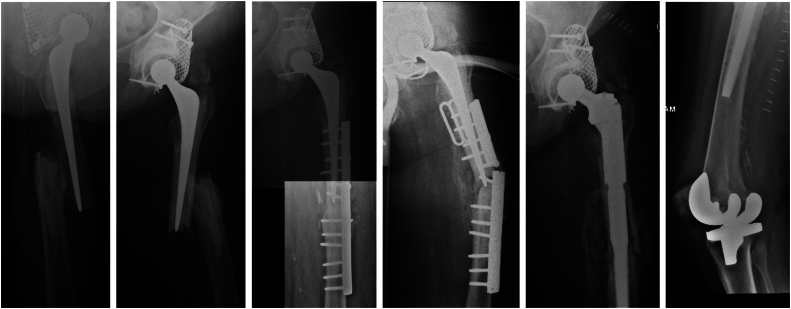
Figure 1.
Transverse B1 fracture, treated with a single plate go on to non-union and conversion to uncemented fluted tapered stem (a Link MP).
Figure 2.
(a) Clinical radiographs of B1 transverse fracture treated with ORIF cables plate and strut graft. (b) Clinical radiographs of B1 spiral fracture.
The aim of this study was to report the outcomes of transverse and short oblique periprosthetic fractures involving a cemented PTS stem. The primary outcome measure was reoperation. Secondary outcomes included residential status, complications, and mortality.
Material and methods
Ethical approval was obtained for this retrospective cohort study (Scotland (A) Research Ethics Committee 20/SS/0125). Between 2007 and 2022, 396 consecutive unilateral PFFs around a polished tapered Exeter stem were identified from a prospectively collected trauma database. Patients with operatively managed B1 fractures of an Arbeitsgemeinschaft für Osteosynthesefragen (AO) transverse or short oblique pattern were included in this study. Patients with hemiarthroplasties, with stems other than cemented PTS stems, UCS (Vancouver) A, B2, B3, C, D, and E fractures, spiral fractures, and those who underwent non-operative management were excluded from the study. This gave a study population of 31 patients with operatively managed transverse or short oblique fractures (AO classification) involving THAs with well-fixed cemented Exeter stems.
Electronic patient records were examined, and the following data recorded: demographic data, BMI, American Society of Anesthesiologists score (ASA), date of primary prosthesis, date of injury, details of operative management, and complications. Mortality was calculated at 1 year. Modes of surgical management failure were determined, and revision surgery or other reoperations were recorded.
Radiographic review was performed by 2 orthopedic surgeons (CEHS, MPB), using picture archiving and communication system (Kodak Carestream, Rochester, NY). Fractures were classified according to the UCS [6], and fracture pattern was recorded according to the AO classification. Additional notes were also recorded if the fracture had atypical features (lateral beaking and cortical or cystic changes). All subsequent radiographs were reviewed using the national (Scotland) picture archiving and communication system archive to identify any subsequent revision surgery which may have occurred out with the study institution.
Statistical analysis
Data were analyzed using SPSS version 27.0. Univariate analysis was performed using non-parametric (Mann-Whitney U-test) tests as appropriate to assess variables for significant differences between operative successes and failures. Survival analysis was undertaken with Kaplan–Meier analysis using the endpoints reoperation for any reason; failure of fixation; and revision of ≥1 component. Log rank statistic was used to compare treatment strategies. A P value of ≤.05 was considered statistically significant.
Results
Of the 31 patients, 12 were male (39%), with mean age 74 ± 11.9 (range 44-91) and mean BMI 28.5 ± 1.4 (range 16-48). The median ASA was 3. Time from primary THA to fracture was 11.3 ± 7.8 years (0.5-26 yrs).
Primary surgical management was fixation with non-locked dynamic compression plates in 27/31 and rTHA in 4/31. Where open reduction and internal fixation (ORIF) was performed, intraoperative image intensifier was used for 9/27 cases; bone grafts in 3/27; dual plates in 3/27; and cables in 21/27. Revision THA was primarily performed for 3/31 patients due to poor quality of the cement mantle, and signs of radiographic aseptic loosening around the THA.
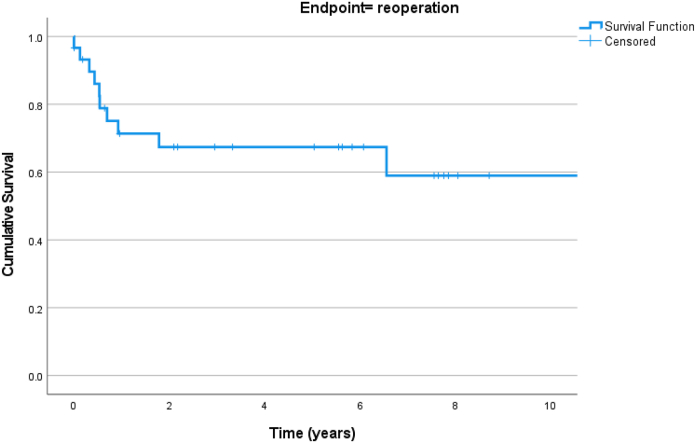
Ten of 31 (32%) patients required reoperation and are detailed in Table 1. Nine of these reoperations were required within 2 years of index PFF: 1 following rTHA and 8 following ORIF. Non-union was the commonest mode of failure and occurred in 6/9 early failures (including one rTHA, patient had ORIF with cement-on-cement revision). Other modes of failure included inadequate fixation and refracture and infection (Table 1). Kaplan–Meier survival free from reoperation was 67.4% (95% CI: 49.8-85.0) at 2 years (Fig. 3).
Table 1.
Summary of the patients who required reoperation after UCS B1 PFF of transverse/short oblique pattern involving a PTS stem.
| Patient | THA for | Fracture features | Primary PFF surgery | Mode of failure | First reop | Number of reops | Ultimate construct |
|---|---|---|---|---|---|---|---|
| 46F | AVN | Transverse atypical | ORIF plate only (no adjuncts) Not anatomically reduced. No II | NU | Revision fixation to dual plates | 5 | Chronically infected PFR |
| 66F | OA | Transverse atypical | ORIF plate and cable (no adjuncts) Anatomic reduction Intraop II used | NU | 1 component revision: PFR | 3 | PFR plus captive cup after dislocation x2 |
| 88F | Fracture | Transverse atypical | ORIF plate only (no adjuncts) Anatomic reduction No II | Refracture | Revision fixation to long distal locking plate | 3 | Revision fixation for further NU |
| 81F | OA | Transverse atypical | ORIF plate only (no adjuncts) Anatomic reduction No II | NU | 1 component revision: uncemented fluted tapered stem | 2 | rTHA with uncemented fluted taper plus one DAIR |
| 82F | OA | Short oblique | ORIF plate and cable (no adjuncts) Anatomic reduction No II | NU | 2 component revision: PFR with captive cup | 2 | PFR and further acetabular revision for dislocation |
| 84F | OA | Short oblique | ORIF plate and cable (no adjuncts) Anatomic reduction No II | Inadequate fixation | Revision fixation with bone graft | 1 | |
| 72M | OA | Short oblique | ORIF plate and cable (no adjuncts) Anatomic reduction No II | Infection | Excision arthroplasty | 1 | |
| 75M | OA | Short oblique | ORIF plate and cable (no adjuncts) Anatomic reduction No II | NU | 1 component revision: uncemented fluted tapered stem plus strut graft | 1 | |
| 44F | OA | Transverse atypical | 2 component revision: uncemented fluted taper stem plus cemented cup | Infection | DAIR at 6 years | 2 | Acetabular revision for loosening at 11 years |
| 83M | OA | Short oblique | 1 component revision: C-in-C stem revision plus fixation with plate and cables | NU | 2 component revision: PFR with captive cup | 1 |
AVN, avascular necrosis; NU, nonunion; OA, osteoarthritis; PFR, proximal femoral replacement: no adjuncts; no additional plate or strut graft were utilized in the procedure.
Those in italics were primarily treated with revision THA.
Figure 3.
Kaplan–Meier survivorship of surgically managed transverse/oblique periprosthetic fractures for the endpoint reoperation.
There was no difference in survival free from reoperation between patients managed initially with ORIF or rTHA (Log rank 0.898). Details of the patients who underwent a revision (r) THA as initial management for their PFF are detailed in Table 2.
Table 2.
Summary of the patients who underwent rTHA stem revisions for PFF treatment.
| Patient case | THA for | PFF | Surgical intervention |
|---|---|---|---|
| 44F | OA | Transverse | 2 component revision: |
| Uncemented fluted tapered stem plus cemented cup | |||
| 83M | OA | Short oblique | 1 component revision: |
| C-in-C femur with cable and plate to fracture | |||
| 75F | rTHA | Short oblique | 1 component revision: |
| Uncemented fluted tapered stem plus cables. | |||
| 88F | OA | Transverse | 2 components revision: |
| PFR plus Constrained cup |
Multiple reoperations were required in 6/10 patients. Of the 8 failures of fixation, 3 underwent refixation of whom 2 went on to unite (though one refractured). The relative risk of requiring multiple reoperations following initial ORIF was 1.2 (95% CI 0.17 -8.5) compared to those who had undergone rTHA. Five of 27 (19%) patients initially managed with fixation ended up requiring rTHA all for non-union and fixation failure. Figure 2 displays clinical radiographs of a patient included in the study cohort, who sustained non-union and required an rTHA. Ultimately, 4 of the cohort (13%) required proximal formal replacement, 3 required uncemented fluted tapered stems (10%), and 3 had femoral strut grafts (10%).
Patients who did and did not require reoperation had comparable age, BMI, sex, ASA, preoperative mobility, time from arthroplasty to fracture, and surgical management, and no significant associations with reoperation requirement were identified (Table 3). There were 2 patients (one from each group) that had a change in residential status after injury (Table 3). The relative risk of 1 year mortality was 1.6 (95% CI: 0.25-10.1) among patients who required reoperation compared to those who did not.
Table 3.
Comparison of the 2 groups, reoperation vs no reoperation.
| Variable | Successful primary management (n = 21) | Reoperation (n = 10) | P value |
|---|---|---|---|
| Age | 76 | 75 | .880b |
| BMI | 28.2 (1.58) | 30.0 (3.5) | .535a |
| Female sex | 12 [57] | 6 [60] | 1.00 |
| ASA | |||
| 2 | 10 [48] | 2 [20] | .105 |
| 3 | 8 [38] | 8 [80] | |
| 4 | 2 [10] | 0 [0] | |
| Preop mobility | |||
| Unaided | 6 [29] | 4 [10] | .434 |
| 1 stick | 5 [24] | 4 [40] | |
| 2 sticks | 4 [19] | 0 [0] | |
| Frame | 3 [14] | 2 [2] | |
| Chair/bedbound | 2 [10] | 0 [0] | |
| Time from THA to PFF | 10.3 | 14.4 | .629b |
| Management | |||
| ORIF | 18 [86] | 8 [80] | .584 |
| Revision | 2 [10] | 2 [20] | |
| Bone graft | 1 [5] | 1 [10] | 1.00 |
| Cables | 14 [67] | 6 [60] | .690 |
| Intra-op II | 5 [24] | 4 [40] | .431 |
| Change in residential status. | 1 [5] | 1 [10] | 1.00 |
| Mortality | |||
| 1 year | 4 [21] | 1 [10] | .640 |
Data are given as mean (SD) or number [%].
T-Test.
Mann–Whitney U.
Discussion
This study has identified a unique, challenging but rare subset of PFF. The data though limited by the patient numbers and the retrospective nature of the study design have produced some striking results that will impact patient care.
Among patients with transverse or short oblique UCS B1 periprosthetic fractures at the level of well-fixed cemented PTS stems, 30% required reoperation after the primary management of their PFF. The risk of reoperation did not differ between patients who had initially underwent fixation vs those treated initially with revision. When reoperation was required, 60% of patients required multiple reoperations to obtain either bony union or a stable revision construct, with 13% of the cohort ultimately requiring proximal femoral endoprostheses. These are difficult fractures to manage, which are associated with a high mortality risk. Patients should be counseled as to the risks of repeated surgery at presentation.
On reflection of the 2 groups: non-reoperation vs reoperation, there were no differences in the age, sex, BMI, overall health (ASA), and clinical frailty score. Therefore, one can assume the “bone health” would be comparable for the 2 groups. This is further supported by reflection of our greater PFF data base, of over 500 patients. PFF patients in general are elderly, frail female, ASA 3, with a high clinical frailty score, but the rate of non-union is significantly lower in the UCS B2 [17]. As a result, we can conclude that no patient or fracture features were identified as being associated with the risk of reoperation. Further supporting the morphology of the fracture that precipitates the high risk of non-union and failure.
The significance of the subtype of B1 fracture around the PTS stem has only recently become apparent [[15], [16], [17], [18]]. Chakrabarti et al. in 2019 published work indicating the clinical significance of the transverse B1 PFF in a group of 22 patients [18]. Jain et al. in 2021 published a large multi-centered study of 584 PFF with 247 B1 fractures. There was no information regarding the fracture pattern in this group. Despite this, the study revealed a large number of primary revisions for the B1 fractures indicating concerns over primary fixation failure [15]. Powell-Bowns et al. in 2021 reviewed 152 B fractures, 74 being B1. This study showed those patients had 12% risk of re-operation [16]. The same group looked at the outcomes of PFF treatment at 5 years, and this article highlighted B1 fractures and how the morphology could influence the outcome [17].
Transverse and short oblique long-bone fractures offer limited surface area for union and are susceptible to non-union [17,18]. These fractures frequently occur at the stem tip at the distal cement mantle making them difficult to compress. Although cerclage cables can be used in some oblique fractures, for transverse fractures, compression is achieved by dynamic compression plating or the use of a dynamic compression device. Due to the prolonged healing time of transverse fractures [15], unilateral plate fixation may be insufficient, and dual plating, or strut grafts, (Fig. 2) may be considered for primary fixation. In addition, this group of transverse and short oblique fractures can also include periprosthetic atypical femoral fractures that have an independent increased risk of non-union as they occur through biologically abnormal bone [19]. It has yet to be determined whether teriparatide is beneficial to bone union in atypical femoral fractures. If a role is confirmed in these biologically challenging fractures, then such medical augmentation may be useful in these biomechanically challenging transverse periprosthetic fractures.
Augmentation of plate fixation with cortical strut grafting or dual plating can be used to stiffen the fixation construct and help facilitate bony union prior to fatigue failure of a unilateral plate [[20], [21], [22]]. Neither of these strategies are “new” concepts, and both have been used in PFF treatment in previous decades in both the proximal and distal femur [20,21]. Vancouver C and supracondylar PFF have established evidence to support dual plating [23]. There is however limited evidence with regards to dual plating in B1 proximal fractures [21]. Performing dual plating at the primary procedure requires greater exposure and soft-tissue stripping than unilateral plating, and therefore may contribute to non-union risk. The use of strut allografts in contrast has resulted in union rate of up to 98% in B1 fractures with well-fixed implants [21]. However, specific fracture patterns are not discussed or reported. At our own center, transverse fractures account for 6%-8% of the PFFs managed, and therefore, obtaining robust data on optimum treatment strategies is difficult without multicenter studies. When revision arthroplasty is performed, the fracture still has to heal to avoid cantilever bending and ultimately failure of the stem [14]. Revision arthroplasty therefore does not avoid non-union as a complication.
Conclusions
Transverse and short oblique periprosthetic fractures at the tip of the stem are difficult fractures to manage. Despite well-fixed stems and UCS-B1 status, these fractures are associated with very high reoperation rates of one in 3. This should be anticipated, the patient warned, and measures taken, such as strut grafting or dual plating, to improve the chance of union and potentially avoid multiple reoperations with ever-increasing risks. The role for medical management of bone health in these biomechanically challenging fractures remains unclear and is an avenue for further research. Surgeons must not underestimate these fractures, often considered the most straight forward of periprosthetic fracture if they are to “get it right first time.”
Conflicts of interest
NDC is a member of the editorial board for the bone and joint journal and bone and joint research. CEHS is a paid consultant for Stryker, Smith and Nephew, and Osstec and is in the Editorial Board of the Bone and Joint Journal. MM is in the speakers’ bureau of/gave paid presentations for Stryker. All the other authors have no conflicts to disclose.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2024.101551.
CRediT authorship contribution statement
Matilda F.R. Powell-Bowns: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Damien Martin: Writing – original draft, Data curation. Abbey Bowley: Data curation. Matthew Moran: Writing – original draft. Nick D. Clement: Writing – review & editing, Writing – original draft. Chloe E.H. Scott: Writing – review & editing, Writing – original draft, Methodology, Investigation, Data curation, Conceptualization.
Appendix A. Supplementary data
References
- 1.Patsiogiannis N., Kanakaris N., Giannoudis P.R. Periprosthetic hip fractures: an update into their management and clinical outcomes. EFFORT Open Rev. 2021;6:75–92. doi: 10.1302/2058-5241.6.200050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Scottish arthroplasty Project. https://www.arthro.scot.nhs.uk/Reports/Main.html
- 3.Brittain R., Howard P., Lawrence S., Stonadge J., Wilkinson M., Wilton T., et al. NJR statistical analysis, support and associated services. National Joint Registry | 19th Annual Report. reports.njrcentre.org.uk/Portals/13/PDFdownloads/NJR 19th Annual Report 2022.pdf
- 4.Bhattacharyya T., Chang D., Meigs J.B., Estok D.M., Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007;89-A:2658–2662. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 5.Griffiths E.J., Cash D.J.W., Kalra S., Hopgood P.J. Time to surgery and 30-day morbidity and mortality of periprosthetic hip fractures. Injury. 2013;44:1949–1952. doi: 10.1016/j.injury.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Duncan C.P., Haddad F.S. The Unified Classification System (UCS): Improving our understanding of periprosthetic fractures. Bone Joint J. 2014;96 B:713–716. doi: 10.1302/0301-620X.96B6.34040. [DOI] [PubMed] [Google Scholar]
- 7.Rayan F., Dodd M., Haddad F.S. European validation of the Vancouver classification of peri-prosthetic proximal femoral fractures. J Bone Joint Surg Br. 2008;90:1576–1579. doi: 10.1302/0301-620X.90B12.20681. [DOI] [PubMed] [Google Scholar]
- 8.Jain S., Farook M.Z., Aslam-Pervez N., Amer M., Martin D.H., Unnithan A., et al. A multicentre comparative analysis of fixation versus revision surgery for periprosthetic femoral fractures following total hip arthroplasty with a cemented polished taper-slip femoral component. Bone Joint J. 2023;105-B:124–134. doi: 10.1302/0301-620X.105B2.BJJ-2022-0685.R1. [DOI] [PubMed] [Google Scholar]
- 9.Petheram T.G., Whitehouse S.L., Kazi H.A., Hubble M.J.W., Timperley A.J., Wilson M.J., et al. The Exeter Universal cemented femoral stem at 20 to 25 years a report of 382 hips. Bone Joint J. 2016;98-B:1441–1449. doi: 10.1302/0301-620X.98B11.37668. [DOI] [PubMed] [Google Scholar]
- 10.Purbach B., Kay P.R., Siney P.D., Fleming P.A., Wroblewski B.M. The C-stem in clinical practice: Fifteen-year follow-up of a triple tapered polished cemented stem. J Arthroplasty. 2013;28:1367–1371. doi: 10.1016/j.arth.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 11.Carli A.V., Negus J.J., Haddad F.S. Periprosthetic femoral fractures and trying to avoid them: what is the contribution of femoral component design to the increased risk of periprosthetic femoral fracture? Bone Joint J. 2017;99-B(1 Supple A):50–59. doi: 10.1302/0301-620X.99B1.BJJ-2016-0220.R1. [DOI] [PubMed] [Google Scholar]
- 12.Meek R.M.D., Norwood T., Smith R., Brenkel I.J., Howie C.R. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011;93:96–101. doi: 10.1302/0301-620X.93B1.25087. [DOI] [PubMed] [Google Scholar]
- 13.Lamb J.N., Van Duren B.H., Redmond A., Pandit H.G., Baetz J., Messer-Hannemann P., et al. A calcar collar is protective against early periprosthetic femoral fracture around cementless femoral components in primary total hip arthroplasty: a registry study with biomechanical validation. Bone Joint J. 2019;101-B:779–786. doi: 10.1302/0301-620X.101B7.BJJ-2018-1422.R1. [DOI] [PubMed] [Google Scholar]
- 14.Palan J., Smith M.C., Gregg P., Mellon S., Kulkarni A., Tucker K., et al. The influence of cemented femoral stem choice on the incidence of revision for periprosthetic fracture after primary total hip arthroplasty: an analysis of national joint registry data. Bone Joint J. 2016;98-B:1347–1354. doi: 10.1302/0301-620X.98B10.36534. [DOI] [PubMed] [Google Scholar]
- 15.Jain S., Lamb J., Townsend O., Scott C.E.H., Kendrick B., Middleton r, et al. Risk factors influencing fracture characteristics in postoperative periprosthetic femoral fractures around cemented stems in total hip arthroplasty. A multicentre observation cohort study of 384 fractures. Bone Jt Open. 2021;2:466–475. doi: 10.1302/2633-1462.27.BJO-2021-0027.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell-Bowns M.F.R., Oag E., Ng N., Pandit H., Moran M., Patton J.T., et al. Vancouver B periprosthetic fractures involving the Exeter cemented stem Reducible fractures with intact bone-cement interfaces can be fixed. Bone Joint J. 2021;103 B:309–320. doi: 10.1302/0301-620X.103B2.BJJ-2020-0695.R1. [DOI] [PubMed] [Google Scholar]
- 17.Powell-Bowns M.F., Oag E., Martin D.H., Clement N.D., Moran M., Scott C.E. Factors associated with failure of fixation of Vancouver B fractures around a cemented polished tapered stem: a 5 to 14 year follow up study. Injury. 2023;54:763–769. doi: 10.1016/j.injury.2023.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Chakrabarti D., Thokur N., Ajnin S. Cable plate fixation for Vancouver Type-B1 periprosthetic femoral fractures-our experience and identification of a subset at risk of non-union. Injury. 2019;50:2301–2305. doi: 10.1016/j.injury.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 19.MacKenzie S.A., Ng R.T., Snowden G., Powell-Bowns M.F.R., Duckworth A.D., Scott C.E.H. Periprosthetic atypical femoral fractures exist and are associated with duration of bisphosphonate therapy. Bone Joint J. 2019;101-B:1285–1291. doi: 10.1302/0301-620X.101B10.BJJ-2019-0599.R2. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y.H., Mansukhani S.A., Kim J.S., Park J.W. Use of locking plate and strut onlay allografts for periprosthetic fracture around well-fixed femoral components. J Arthroplasty. 2017;32:166–170. doi: 10.1016/j.arth.2016.05.064. [DOI] [PubMed] [Google Scholar]
- 21.Kubik J.F., Bornes T.D., Gausden E.B., Klinger C.E., David W.S., Helfet D.L. Surgical outcomes of dual-plate fixation for periprosthetic femur fractures around a stable hip arthroplasty stem. Arch Orthop Trauma Surg. 2022;142:3605–3611. doi: 10.1007/s00402-021-03950-9. [DOI] [PubMed] [Google Scholar]
- 22.Haddad F.S., Duncan C.P., Daniel B., Lewallen D.G., Gross A., Chandler H.P. Periprosthetic femoral fractures around well fixed implants: use of cortical onlay allografts with or with out a plate. J Bone Joint Surg. 2002;84:945–950. [PubMed] [Google Scholar]
- 23.Kriechling P., Bowley A.L.W., Ross L.A., Moran M., Scott C.E.H. Double plating for periprosthetic distal femur fracture is a suitable option compared to distal femur replacement: analysis of 111 cases. Bone Jt Open. 2024;5:489–498. doi: 10.1302/2633-1462.56.BJO-2023-0145.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.