Abstract
Background and objectives
Idiopathic condylar resorption (ICR) can be described as a dysfunctional remodeling of the temporomandibular joint (TMJ). It is clinically characterized by morphological changes in TMJ including reduced ramus height, accelerated mandibular retrusion and reduced growth in juveniles. With a strong predilection towards females (90 %) within an age group of 10 to 40 years, diagnosis and management of ICR is a critical clinical challenge. The aim of this study is to present a comprehensive review of diagnosis and management strategies for ICR.
Materials and Methods
Literature search based on keywords relating to ICR was conducted on PubMed (Medline) database. Studies fulfilling the inclusion criteria (reports based on clinical diagnosis and management of ICR) were selected for comprehensive review.
Results
253 articles were identified through literature search. After abstract screening and full-text review, 54 studies were selected for qualitative synthesis. Diagnosis of ICR is established by combination of clinical and radiographic findings, patient history, and exclusion of all known local/systemic factors contributing to condylar resorption. Management of ICR depends on condylar activity and surgeon’s ability to preserve the articular disc and mandibular condyle, and could either be surgical or non-surgical. Surgical treatment can be either by orthognathic surgery alone or through a combination of orthognathic and TMJ surgeries.
Conclusion
Based on the present review, it may be concluded that diagnosis and management of ICR requires adequate clinical understanding of the condition. Identifying the stage of ICR is important in deciding optimum treatment plan. While early-stage ICR could be managed non-surgically by orthodontic and splint therapies, advanced stage disease require simultaneous TMJ Surgery with orthognathic correction for skeletal stability. Future research should focus on elucidating underlying mechanisms of ICR, refining diagnostic criteria, and optimizing treatment protocols to enhance patient outcomes.
Keywords: Idiopathic Condylar Resorption, Progressive condylar resorption, Temporomandibular Joint Replacement, Temporomandibular Joint Reconstruction, Orthognathic Surgery
1. Introduction
Idiopathic condylar resorption (ICR) is a rare clinical condition affecting the mandibular condyle, leading to progressive resorption of the articulating surface of condyle, leading to reduction in vertical height over a period of time (Arnett et al., 1996a, Arnett et al., 1996b). Although reported in both genders, it has a greater female predilection (9:1 female to male ratio) and is often reported among adolescent girls, so much so that the condition has also been referred to as ‘Cheerleaders Syndrome’, indicating a preponderance towards female teenagers actively engaged in sporting activities (Wolford and Cardenas, 1999, Wolford, 2001). ICR is also reported in the literature with other names such as idiopathic condylosis, progressive condylar resorption and condylar atrophy, and may be associated with traumatic injuries that exacerbate the condition (Wolford and Cardenas, 1999, Wolford, 2001, Handelman and Greene, 2013, Hatcher, 2013, Chamberland, 2019, Alali et al., 2024). Condylar resorption may occur secondary to temporomandibular joint (TMJ) dysfunction, trauma, surgery, rheumatoid arthritis, autoimmune conditions like systemic lupus and scleroderma, and steroid therapy (Mercuri 2008). Nevertheless, ICR has no relatable underlying cause and could be termed as ‘primary condylar resorption’, and is rarely reported in patients over the age of 20 years (Mehra et al., 2016, Peacock et al., 2019, Ha et al., 2020).
The anatomy of the TMJ is such that the articular disc is interposed between the articulating surfaces of the mandibular condyle and glenoid fossa of the temporal bone, ensuring smooth movements of the TMJ during function (Hatcher, 2013, Ji et al., 2020, Shen et al., 2022). When the condylar height is reduced as a result of ICR, the mandible is retracted posteriorly leading to retrognathia, malocclusion and open bite (Park et al., 2019, Lee et al., 2024b, Lee et al., 2024a). Therefore, patients with ICR often report symptoms including pain in the jaws and TMJ, reduced range of TMJ function, headaches and clicking or popping noises owing to disc displacement without reduction (Hatcher, 2013, Chamberland, 2019). This is in part because ICR is characterized by dysfunctional remodeling associated with morphological changes in the TMJ (Arnett et al., 1996a, Arnett et al., 1996b). Patients with ICR typically demonstrate specific facial morphologic characteristics that correlate with class II skeletal or dental malocclusion, high mandibular plane angle and progressive mandibular retrusion, and may present at times with anterior open bite (Wolford and Cardenas, 1999, Park et al., 2019, Wang et al., 2021). Based on an analysis of young orthodontic patients, approximately 0.36 % of all patients were diagnosed with ICR and the incidence rose significantly after orthognathic surgery for 1.2 % to 5.8 % (Handelman and Greene, 2013, Kristensen et al., 2017, Tanaka, 2023). Interestingly, the incidence of ICR was the highest, ranging from 19 % to 31 %, among orthodontic and orthognathic surgery patients who presented with class II mandibular relationship and a high mandibular plane angle (Handelman and Greene, 2013, Kajii et al., 2019, Park et al., 2019). Among such patients, the rate of condylar erosion owing to ICR was reportedly around 0.12 mm/month or 1.5 mm/year, as assessed by panoramic radiography (Wolford and Cardenas 1999).
Diagnosis of ICR is usually established by a combination of clinical and radiographic findings, patient history, and exclusion of all known local and systemic factors that may contribute to condylar resorption (Mitsimponas et al., 2018, Zarour et al., 2020, Tanaka, 2023). With the advancement of radiographic and non-radiographic imaging modalities including computed tomography (CT), magnetic resonance imaging (MRI), radionuclide scanning and soft-tissue imaging, establishing a diagnosis of ICR has gained credibility (Young, 2017, Zhou et al., 2021, Lee et al., 2024b, Lee et al., 2024a). There are at least three theories reported to explain the etiopathology of ICR and these include hormonal mediation, avascular or hypovascular necrosis and dysfunctional remodeling of the condyle (Mitsimponas et al., 2018). The hormonal mediation theory is based on the premise that ICR is more commonly reported among young females in the teen to adolescent age groups, when metabolic activity due to hormones is predominant (Yuan et al., 2021). Estrogen more than progesterone is capable of influencing cartilage metabolism and higher concentration of estrogen receptors have also been reported in the TMJ articular disc cartilage of female patients with temporomandibular dysfunction (TMD) (Abubaker et al., 1993). It is further hypothesized that an exaggerated hormone mediated metabolic response to normal TMJ function leads to synovial hyperplasia and damage to supporting ligaments causing anterior disc displacement, all of which are capable of precipitating ICR (Papadaki et al., 2007). On the other hand, according to the theory of avascular/hypovascular necrosis abnormal compression in the retrodiscal area of TMJ leads to capillary constriction, which sets in a vicious cycle of events leading to ICR (Chuong and Piper 1993). Finally, the dysfunctional remodeling theory suggests the inability of host tissues to remodel and adapt in response to mechanical stresses, as the reason for ICR (Mercuri 2008). Irrespective of the aforementioned theories, inflammation and receptor medicated osteoclastic bone resorption remain the keystone in etiopathogenesis of ICR (Mitsimponas et al., 2018, Nobrega et al., 2024).
Although several treatment options have been suggested for the treatment of ICR, none of them have been proved superior over the other. Some of these include orthodontic treatment with or without splint therapy, orthognathic correction, surgical repositioning of TMJ disc and stabilization, condylar repair procedures such as condylotomy with or without costal cartilage grafting, and total alloplastic TMJ reconstruction as a last resort (Mitsimponas et al., 2018). Despite the advancements in diagnosis and treatment of ICR, there is still paucity in terms of understanding the pathophysiology of the condition leading to sub-optimal treatment outcomes (Pedersen and Stoustrup 2021). Moreover, the response to different treatment modalities for ICR are also not reported in detail. Therefore, the aim of this study is to present a comprehensive review of diagnosis and management strategies for ICR, from what has been reported in contemporary scientific literature.
2. Materials and methods
The present study was designed as a comprehensive review of literature to address the focused question, ‘What are the different diagnostic and treatment methods for idiopathic condylar resorption (ICR)’? Accordingly, the present review was conducted based on the ‘PCC (Population/Concept/Context) framework for scoping literature reviews’.
Population – Reports based on patients with ICR.
Concept – Enhancing current understanding about the pathophysiology of ICR.
Context – Clinical diagnosis and management of ICR.
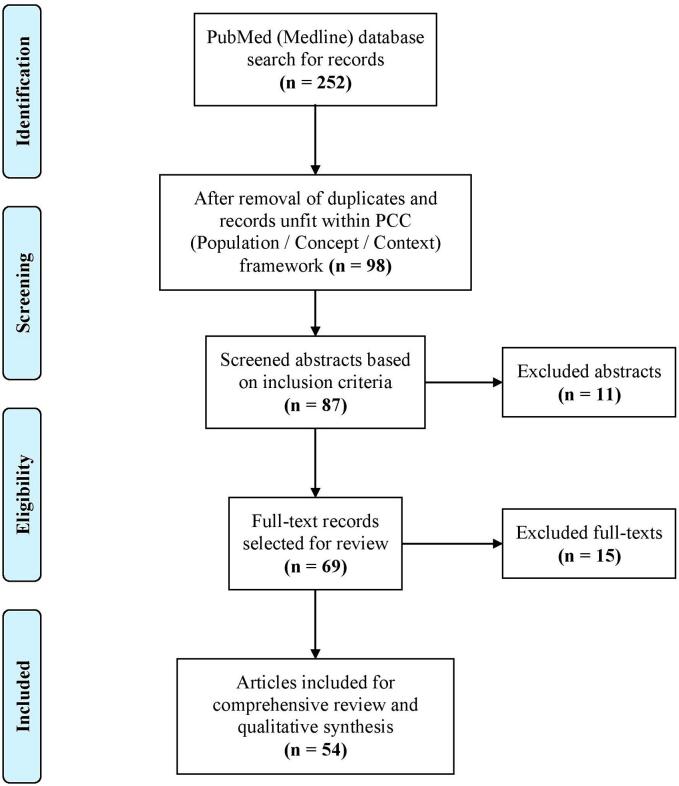
Based on the aforementioned criteria, a literature search of published studies was conducted in the PubMed (Medline) database (NCBI-NLM, National Institute of Health, Bethesda, MD, USA) using the key words, “idiopathic condylar resorption”, “condylar resorption”, “condylosis”, “condylar atrophy” and “progressive condylar resorption”. Boolean operators (AND, OR and NOT) were used to optimize, expand or restrict search, required. Study selection was based on agreement among all authors, and any disagreement was resolved through discussion. The process of study selection is elucidated as a flowchart in Fig. 1. The final selected studies were subjected reading and group discussion among authors to synthesize the narrative review.
Fig. 1.
Flowchart describing the study selection process for review of literature, based on PRISMA (Preferred reporting items for systematic reviews and meta-analyses) statement (Moher et al., 2009).
3. Results
Initial search through PubMed (Medline) database yielded 252 records, which were title screened for removal of duplicates and inclusion based on PCC criteria. Following initial screening 98 records were selected for abstract screening out of which 11 abstracts were excluded as they were not pertaining to diagnosis and management of ICR. Based on abstract screening of the selected 87 records, 69 full texts were retrieved and discussed among the authors for final selection of studies for review. After exclusion of 15 full texts, which were either case reports with inadequate data or review articles non-relevant to the present study objectives, 54 full text were selected for final literature review (Fig. 1). Detailed discussion about the qualitative data retrieved from the selected studies is presented below.
4. Discussion
4.1. History
Obtaining a meticulous history is imperative for optimum diagnosis and management of ICR. History of previous orthodontic or orthognathic surgery treatment, orthopedic devices, steroid use, local or systemic connective tissue and autoimmune diseases that may cause mandibular condylar resorption should be elicited by the clinician (Papadaki et al., 2007, Chung et al., 2011, Chung et al., 2012, Ji et al., 2020, Iwasa and Tanaka, 2022). Pertinent surgical risk factors should also be considered in patients who undergo or are planned for orthognathic surgery, for skeletal class II malocclusion, as they might accentuate an already existing pathological process of ICR (Merkx and Van Damme, 1994, Chigurupati and Mehra, 2018, Lee et al., 2019). These include medial or lateral condylar torqueing due to rigid fixation of the mandibular segments during surgery, prolonged periods of maxillo-mandibular fixation after bimaxillary surgery, large mandibular advancements and anti-clockwise rotation of the distal and proximal segments especially in patients with steep mandibular plane angle (Kau and Bejemir, 2015, Mehra et al., 2016, Chigurupati and Mehra, 2018). In addition, local factors such as osteoarthritis, reactive arthritis, infection, and traumatic injuries can predispose to ICR or exacerbate a pre-existing condition (Posnick and Fantuzzo, 2007, Mercuri, 2008, Young, 2017). Since ICR rarely affects joints other than TMJ, it is important to obtain laboratory tests when other joints are involved as this helps to evaluate for any systemic causes affecting multiple synovial joints throughout the body (Troulis et al., 2008, Alsabban et al., 2018). These conditions could include connective tissue and autoimmune diseases, such as rheumatoid arthritis, scleroderma, systemic lupus erythematosus, and Sjögren's syndrome (Wolford and Cardenas, 1999, Troulis et al., 2008, Alsabban et al., 2018). In light of the above reports from the literature, it is pertinent to record a detailed history for establishing a diagnosis of ICR and planning management on a case-by-case basis.
4.2. Etiology
The term ‘idiopathic’ in ICR clearly suffices that the condition has no identifiable cause, which leads to progressive mandibular condylar resorption (Sansare et al., 2015, Mercuri and Handelman, 2020). Although several theories emerged to explain the etiology behind it, none of them are able to point out specifically the etiology behind ICR (Papadaki et al., 2007, Mitsimponas et al., 2018). Prominent among them is the hormonally mediated theory, according to which, the greater female predilection associated with certain pathologic states affecting the TMJ could be influenced by estrogenic effects (Milam et al., 1987, Yuan et al., 2021). In addition to the presence of estrogen and progesterone receptors in TMJ disc tissue, which is indicative of them being a target site for metabolic activity, sex hormones are also capable of eliciting biochemical and molecular changes leading to synovial inflammation, hyperplasia and osteoclastic bone resorption (Arnett and Tamborello, 1990, Abubaker et al., 1993, Wolford and Cardenas, 1999). The aforementioned changes in the TMJ result in production of destructive substrates and cytokines leading to anterior displacement of the disc and increasing exposure of the condylar head to the resorptive phenomena (You et al., 2011, He et al., 2019, Pedersen and Stoustrup, 2021). The next credible explanation for ICR is based on theory of avascular necrosis that suggests compression of blood vessels in the retrodiscal tissues due to morphological changes, mechanical stress and trauma, as the reason behind etiopathogenesis of ICR (Schellhas et al., 1989, Mitsimponas et al., 2018). According to this theory, which more popularly explains avascular necrosis of femoral condyles, cortical and medullary infarction of the mandibular condyle leads to structural weakening and joint collapse (Schellhas et al., 1989). This theory is further able to lend credence to the clinical signs and symptoms associated with ICR such as severe pain, bone fragility, articular surface collapse, and degenerative joint changes during late stages (Chuong and Piper 1993). Lastly, the theory of dysfunctional remodeling proposes the inability of TMJ and condylar tissues to adapt and remodel in response to functional demands (Mercuri 2008). This theory could possibly explain the higher prevalence of ICR among patients with morphological abnormalities including skeletal and dental malocclusion, and parafunctional habits (You et al., 2011, Yang and Hwang, 2015, Young, 2017). In the absence of clear explanation towards the etiology, it is alluring to assume that the etiopathogenesis of ICR could be the result of interplay between all the aforementioned hypotheses.
4.3. Signs and symptoms
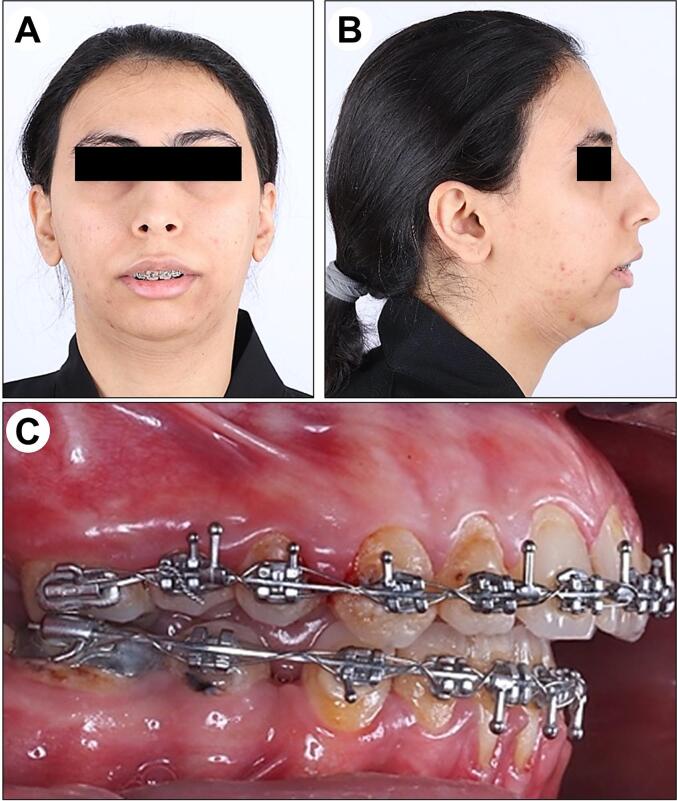
It is important for oral and maxillofacial surgeons, orthodontists and dental practitioner to recognize the signs and symptoms of ICR, for early diagnosis and timely management (Alexander, 2012, Rahman et al., 2019). As mentioned earlier, ICR is predominantly seen among young (teen and adolescent) females, with class II skeletal tendencies (Iwasa and Tanaka 2022). Clinical signs of ICR include progressive open bite, increasing overjet or class II malocclusion, mandibular retrognathia, and a retruded chin presenting as disappearing chin phenomenon (Arnett et al., 1996a, Arnett et al., 1996b, Papadaki et al., 2007). In terms of clinical presentation, the mandible appears to rotate clockwise, which creates a bird-face deformity (Mitsimponas et al., 2018, Mao et al., 2023), as shown in Fig. 2. Although patients with ICR present with a wide array of clinical symptoms, they may be found in only 25 % of them (Wolford and Cardenas 1999). These symptoms include malocclusion in general, followed by open bite, TMJ pain, myofascial pain, headaches, decreased mouth opening, and TMJ clicking, with an average frequency of about 98 %, 64 %, 60 %, 55 %, 44 %, 37 %, and 30 %, respectively reported by Alsabban et al., (2018). Considering the variable nature of signs of symptoms associated with ICE, understanding them is important for clinicians involved in the diagnosis and management of this condition.
Fig. 2.
Representative clinical images of a patient with idiopathic condylar resorption: (A) Frontal view, (B) Lateral profile view, and (C) Intraoral occlusion.
4.4. Radiographic presentation
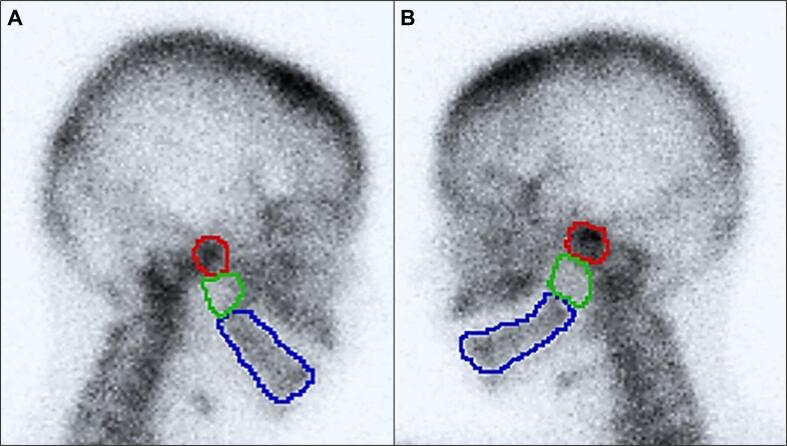
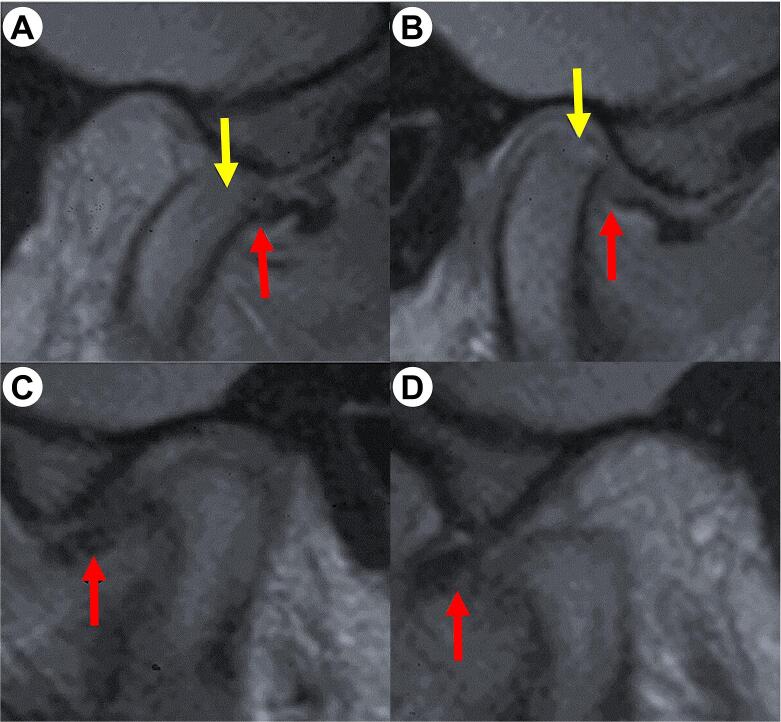
ICR can be identified and described by a combination of one or more radiographic imaging modalities such as panoramic radiograph (OPG), lateral cephalogram, cone beam computed tomography (CBCT) scans, Technetium-99 m bone scans, and magnetic resonance imaging (MRI) (Sansare et al., 2015). Findings based on panoramic radiographs include diminished volume of condyle, and alteration of condylar contour as shown in Fig. 3A. Similarly, lateral cephalometric radiographs can provide information pertaining to anterior open bite, high mandibular plane angle, decreased ramus height, increased overjet, class II skeletal relationship, and decreased ‘sella–nasion–B-point’ (SNB) angle, as shown in Fig. 3B. Since ICR is a condition characterized by progressive resorption, radionuclide bone scans using Technetium-99m as a radioisotope helps assess the degree of metabolic activity in the condylar region, in comparison to other parts of the mandible (Troulis et al., 2008). This helps to make a distinction between disease progression and arrested phases, as shown in Fig. 4. With respect to structural abnormalities in the TMJ arising as a result of ICR, the best radiodiagnostic modality is using MRI scanning (Zarour et al., 2020). In addition to identifying disc position relative to the condyle and glenoid fossa, MRI also provides information about decreased condylar volume, disc displacements either with or without reduction, thinning or erosion of the condylar cortex, and presence of any amorphous appearing soft tissue in the TMJ synovial cavity (Fig. 5). The advent of CBCT has enabled ease of efficiency and portability in terms of imaging the TMJ. Although it is not the imaging modality of choice for cartilage and soft tissue, CBCT scans provide information about excessive joint space due to hyperplastic synovial tissues, decrease in condylar size, loss of integrity of condylar cortex, reduction in ramus height and bony changes within the articulating surfaces of TMJ (Sansare et al., 2015, He et al., 2019).
Fig. 3.
Representative radiographic images of a patient with idiopathic condylar resorption: (A) Panoramic radiograph and (B) Lateral cephalometric radiograph.
Fig. 4.
Image showing the outcomes of Technetium-99m bone scan in a patient with idiopathic condylar resorption and color coded to indicate ratio of radioisotope uptake: (A) Right side – Condyle (5.4), Ramus (2.4), Body (2.3); and (B) Left side − Condyle (4.8), Ramus (2.2), Body (2.4).
Fig. 5.
Magnetic resonance imaging (T1-weigted) showing sagittal sections through the temporomandibular joint (TMJ) in a patient with idiopathic condylar resorption (ICR): (A) Right TMJ in open mouth position, and (B) closed mouth position showing an anteriorly displaced disc, which doesn’t reduce back to position (red arrow). The antero-superior surface of the condyle presenting a missing low-signal rim (yellow arrow), which is indicative of active erosion of the surface of the condyle. (C) Left TMJ of the same patient in closed mouth position and (D) open mouth position showing a disc displaced anteriorly without reduction (red arrow), along with a reduction in its anteroposterior dimension while maintaining biconcave shape. The condylar surface is flattened with reduced height and shows a low-signal rim indicative of stable stage of ICR.
4.5. Stages of idiopathic condylar resorption
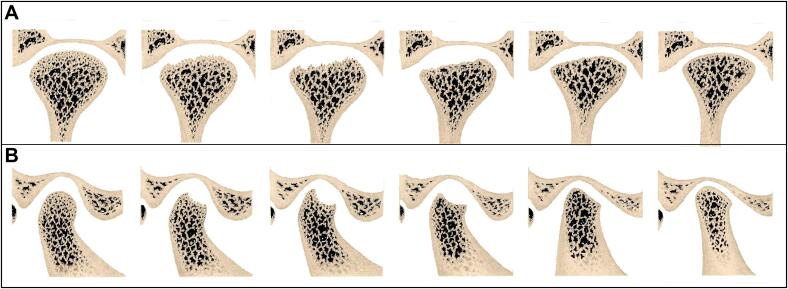
Based on radiographic findings, ICR can be classified into three different phases, namely soft tissue phase, active/destructive phase, and stable/reparative phase (He et al., 2019). The soft tissue phase of disease progression occurs prior to condylar resorption and is characterized by a non-reducing, anterior disc displacement accompanied by limited mouth opening (less than 30 mm) and TMJ pain (Shen et al., 2022). This phase precipitates condylar resorption as a result of continued osteodegenerative processes and when it persists, it leads to the development of the active/destructive phase of ICR (Hatcher 2013). In the active/destructive phase, loss of cortex occurs along the antero-superior surface of the condyles, and a cavitation defect extends into the subchondral bone, resulting in loss of condylar volume (Lee et al., 2024b). This is followed by a stable/reparative phase wherein condylar cortex undergoes flattening and decortication (Yang and Hwang, 2015, Lee et al., 2024b, Lee et al., 2024a). The stable/reparative phase usually occurs after the causative factors have been controlled, thereby allowing the condyle to adapt and distribute functional loads over a larger stress-bearing area. This leads to restoration of condylar motion and reduction in severity of pain and associated symptoms (Hatcher 2013). Although the aforementioned phases are identified only based on radiographic imaging and have no comparable clinical correlation, determining the phase or stage of disease progression in ICR helps plan appropriate treatment. Fig. 6 shows representative images of the different stages of ICR.
Fig. 6.
Anatomic images drawn based on radiographic presentation of idiopathic condylar resorption (ICR), showing the sequence of disease progression – (from left to right) normal condyle, beginning stage of active condylar destruction, stage of continuing condylar destruction, beginning of condylar repair stage, advanced condylar repair stage, stable stage of ICR after progressive condylar resorption: (A) Coronal section and (b) Sagittal section through the temporomandibular joint.
4.6. Treatment options
Based on the present review of literature, several treatment modalities, both surgical and non-surgical, have been proposed to manage ICR, based on the stage of disease progression. In general, non-surgical management such as orthodontic treatment, either with or without occlusal splint therapy, is suggested when ICR is not active and is considered as a means of preventing further disease progression (Lee et al., 2019, Ha et al., 2020, Zhou et al., 2021, Lee et al., 2024a). This is especially beneficial when disfigurement of facial soft tissue is mild and acceptable to the patient, and acts by relieving the stress on condyles due to occlusal loading (Nitzan and Palla, 2017, Noh and Park, 2021, Lee et al., 2024b, Lee et al., 2024a). Arthrocentesis and arthroscopy are other conservative treatment options that are available for mainly controlling the clinical signs and symptoms of ICR (Mercuri 2008). Nevertheless, these procedures cannot help in removal of hyperplastic synovial tissue and also do not enable repositioning of the displaced articular disc into a position where it can resume normal functions. Therefore, these procedures are predictably unsuccessful in treating ICR, particularly if correction of the jaw deformity is attempted (Wolford and Cardenas 1999).
When dentofacial deformity is present, management of ICR depends on condylar activity and the surgeon’s ability to preserve the relationship between the articular disc and the mandibular condyle, in line with a stable occlusal relationship (Warburton and Mercuri 2022). Consequently, surgical treatment can be in the form of orthognathic surgery alone or a combination of orthognathic surgery with TMJ surgery. Within TMJ surgery, it could either be through disc preservation and stabilization, or by means of a total TMJ replacement, which could be autogenous or alloplastic (Alkindi et al., 2018, Alkindi et al., 2019). If orthognathic surgery alone is performed, the clinician must confirm the absence of condylar activity for a period at least one-year, and preferably up to two-years (Mercuri, 2000, Rahman et al., 2019). Moreover, certain criteria such as stable posterior facial height to anterior facial height ratio, no change in ramus length, chin position, malocclusion, and overjet at two-time points for at least one-year apart should be present (Wolford and Cardenas, 1999, Rahman et al., 2019). It is important to remember here that, whenever possible, correction of the malocclusion should be done with maxillary orthognathic surgery alone, in an effort to decrease loading of the TMJ, minimize pain and dysfunction, and to not re-induce ICR (Mehra et al., 2016, Chigurupati and Mehra, 2018). However, in this way the esthetic outcomes of dentofacial deformity correction are considered less favorable, as this does not address the main issue of mandibular retrognathism (Chigurupati and Mehra, 2018, Mitsimponas et al., 2018). Furthermore, orthognathic surgery alone was reported to have a high relapse rate ranging from 83.33-100 % (Merkx and Van Damme, 1994, Sansare et al., 2015). Based on a study conducted on 16 patients with ICR, Ha et al., (2020) reported an 18.75 % skeletal relapse rate after undergoing orthodontic treatment followed by orthognathic surgery and functional splint therapy. They therefore, advocated splint therapy to be begun prior to mandibular advancement surgery, as an adjunct to achieve post-operative skeletal stability (Ha et al., 2020).
Wolford and Cardenas (1999) proposed a protocol for simultaneous TMJ surgery along with orthognathic surgical correction of the skeletal malocclusion. According to their protocol, an open joint surgery is performed to remove hyperplastic synovial tissue, reposition the disc back to its position and stabilize the condyle. In their technique, condylar stabilization was achieved by fixing a “MITEK” mini anchor plate on the posterior condylar head and held in place by sutures acting as artificial ligaments (Wolford and Cardenas 1999). Based on a follow-up study of patients with ICR treated using the aforementioned protocol, Wolford (2001) reported long-term skeletal stability without any relapse. Although simultaneous TMJ and orthognathic surgery helps resolve jaw and occlusal discrepancies at the same time, this protocol would be applicable only for patients with early stages of ICR, wherein the disc and condyle are salvageable (Wolford and Cardenas, 1999, Wolford, 2001). Alternatively, when the condyle and articular disc are either irreversibly damage or are unsalvageable, condylotomy or condylectomy with costochondral graft (CCG) is a viable TMJ surgical treatment option (Saeed and Kent, 2003, Troulis et al., 2008, Peacock et al., 2019). This technique involves reconstructing the TMJ using a costal graft with a cartilage cap (costochondral graft) harvested from the 5th and 6th ribs, and could also be used simultaneously alongside orthognathic surgery for dentofacial deformity correction (Troulis et al., 2008). Considering its inherent growth potential, use of CCG for TMJ reconstruction is an ideal choice for young patients in the growing age (Saeed and Kent 2003). Based on a long-term study on 15 patients with ICR who underwent condylectomy and CCG for TMJ reconstruction, Troulis et al., (2008) reported stable outcomes with a change from skeletal class II to class I mandibular relationship, post-treatment. Interestingly, all the patients in that study were treated during the active resorption stage of ICR and reported post-operative reduction in anterior open bite, reproducible occlusal relationship, normal mouth opening and complete range of TMJ function (Troulis et al., 2008). Similar findings were also reported by Peacock et al., (2019), albeit the surgical procedures in this study, namely condylectomy and CCG reconstruction of TMJ, were performed through endoscopy. While the use of CCG after condylectomy seems to be a viable option among young patients with ICR, even during the active stage of disease, the technique is not free from complications such as uncontrolled growth post-grafting leading to mandibular asymmetry, ankyloses and donor site morbidity (Saeed and Kent, 2003, Papadaki et al., 2007).
In the last two decades, the most preferred surgical option for management of ICR especially in patients with advanced stage condylar resorption has been total TMJ replacement or reconstruction (Warburton and Mercuri 2022). This procedure involves reconstruction of the entire TMJ articular complex (condylar and glenoid fossa components) using alloplastic prosthesis, after condylectomy and coronoidectomy (Mercuri, 2000, Mercuri and Handelman, 2020). One of the greatest advantages of this procedure, in comparison to previously reported surgical interventions for ICR, is the ability to combine it with simultaneous bimaxillary orthognathic surgery for correction of severe dentofacial deformities (Mehra et al., 2016, Chigurupati and Mehra, 2018, Warburton and Mercuri, 2022, Alali et al., 2024). In comparison to the surgical protocol suggested by (Wolford and Cardenas 1999), alloplastic TMJ reconstruction not only enables treatment of ICR patients in whom the condyle and articular disc are not salvageable, but also allows simultaneous maxillary orthognathic surgery for stable recovery of dentofacial form and function (Warburton and Mercuri, 2022, Alali et al., 2024). Similarly, alloplastic TMJ reconstruction overcomes the challenges associated with condylectomy and CCG, such as ability to treat advanced stage ICR patients, no donor site morbidity and negligible risk of post-operative asymmetry, relapse or remodeling (Mehra et al., 2016, Chigurupati and Mehra, 2018). With advances in technology, the longevity and biocompatibility of alloplastic prosthesis used for TMJ reconstruction has improved tremendously. Moreover, the advent of three-dimensional modeling based on radiographic imaging, rapid prototyping, virtual surgical planning and newer biomaterials have made patient specific alloplastic TMJ prosthesis the norm rather than an exception (Alkindi et al., 2018, Alkindi et al., 2019). Nevertheless, the cost of alloplastic biomaterials used for TMJ reconstruction and its fabrication, and their unsuitability for use in young growing children with ICR are certain challenges to be overcome through future research. Fig. 7 shows the surgical and radiographic images of patient treated with total alloplastic TMJ reconstruction.
Fig. 7.
Surgical management of idiopathic condylar resorption with total alloplastic temporomandibular joint (TMJ) reconstruction: (A) Intra-operative image showing fixation of the alloplastic glenoid fossa prosthesis, (B) Intra-operative image showing fixation of the ramus and condyle component of the alloplastic TMJ prosthesis, and (C) Lateral cephalometric radiograph taken one year post-operatively showing stable TMJ position and occlusion.
Based on the reviewed literature, for advanced stage ICR patients who have completed their growth phase and in whom condyle and articular disc are diseased beyond repair, alloplastic TMJ reconstruction combined with bimaxillary orthognathic surgery and adjunct orthodontic treatment would be the preferred treatment option (Wang et al., 2019). However, distraction osteogenesis is one surgical option which despite being reported for the clinical treatment of even severe cases of ICR, is still not popular as evidenced by the paucity of reports in the literature and could be an area for future research consideration (Schendel et al., 2007, Zhang et al., 2020).
5. Conclusion
Diagnosis of ICR relies on patient history, clinical and radiographic assessment. With various imaging modalities available to identify the stages of ICR, clinicians should make a guided decision towards formulating a proper treatment plan. Treatment strategies for ICR must be determined based on severity of the condylar resorption activity, ability to structurally and functionally preserve the articular disc and mandibular condyle, and the presence of dentofacial deformities. Conservative treatment approach, such as occlusal splint therapy with or without orthodontic treatment, is considered effective in early stages. Whereas surgical interventions, including orthognathic surgery and TMJ reconstruction, will be necessary in advanced cases.
The protocol of simultaneous orthognathic surgery for dentofacial deformity correction and TMJ surgery for ICR, as an early-stage management, has shown remarkable promise when the disc and condyle can be salvaged. Conversely, alloplastic TMJ replacement with simultaneous orthognathic surgery, offers a viable option for end-stage management, demonstrating long-term skeletal stability and functional improvement. Future research should focus on elucidating the underlying mechanisms of ICR, refining diagnostic criteria, and optimizing treatment protocols to enhance patient outcomes. Given the complex nature of ICR, a multidisciplinary approach involving orthodontists, oral and maxillofacial surgeons, and other specialists such as physical therapists, is essential for effective management and to reduce and prevent the risk of recurrence or complications.
Ethical Statement
This study was reviewed and approved by the Institutional Review Board, King Saud University (Approval No. E-24-8433).
Acknowledgment
The authors acknowledge College of Dentistry Research Center, King Saud University and Deanship of Scientific Research, King Saud University for their support.
Footnotes
Peer review under responsibility of King Saud University. Production and hosting by Elsevier
Contributor Information
Yasser S. Alali, Email: yalali@ksu.edu.sa.
Khaled M. Al Habeeb, Email: kmh-100@hotmail.com.
Khaled A. Al Malhook, Email: khalidmhq7@gmail.com.
Sami Alshehri, Email: smalshehri@iau.edu.sa.
References
- Abubaker, A. O., W. F. Raslan and G. C. Sotereanos, 1993. Estrogen and progesterone receptors in temporomandibular joint discs of symptomatic and asymptomatic persons: a preliminary study. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 51, 1096-1100. https://doi.org/10.1016/s0278-2391(10)80448-3. [DOI] [PubMed]
- Alali Y.S., Habeeb K.M.A., Malhook K.A.A. Bilateral alloplastic temporomandibular joint reconstruction with orthognathic surgery: a case report of idiopathic condylar resorption. International Journal of Community Medicine and Public Health. 2024;11:2912–2920. 10.18203/2394-6040.ijcmph20241857 [Google Scholar]
- Alexander R. Idiopathic condylar resorption. Report of a case. N. Y. State Dent. J. 2012;78:22–25. [PubMed] [Google Scholar]
- Alkindi M., Ramalingam S., Badwelan M., et al. In-Vivo Biocompatibility and functional efficacy of customized electron beam-melted titanium mandibular reconstruction plates. Journal of Biomaterials and Tissue Engineering. 2018;8:1642–1651. doi: 10.1166/jbt.2018.1919. [DOI] [Google Scholar]
- Alkindi M., Ramalingam S., Moiduddin K., et al. In Vitro Biomechanical simulation testing of custom fabricated temporomandibular joint parts made of electron beam melted Titanium, zirconia, and poly-methyl methacrylate. Appl. Sci. 2019;9:5455. [Google Scholar]
- Alsabban, L., F. J. Amarista, L. G. Mercuri, et al., 2018. Idiopathic Condylar Resorption: A Survey and Review of the Literature. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 76, 2316 e2311-2316 e2313. https://doi.org/10.1016/j.joms.2018.07.008. [DOI] [PubMed]
- Arnett G.W., Milam S.B., Gottesman L. Progressive mandibular retrusion–idiopathic condylar resorption. Part I. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- Arnett G.W., Milam S.B., Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 1996;110:117–127. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- Arnett G.W., Tamborello J.A. Progressive Class II development: female idiopathic condylar resorption. Oral Maxillofac. Surg. Clin. North Am. 1990;2:699–716. 10.1016/S1042-3699(20)30456-8 [Google Scholar]
- Chamberland S. Progressive idiopathic condylar resorption: three case reports. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2019;156:531–544. doi: 10.1016/j.ajodo.2018.05.023. [DOI] [PubMed] [Google Scholar]
- Chigurupati R., Mehra P. Surgical Management of Idiopathic condylar resorption: orthognathic surgery versus temporomandibular total joint replacement. Oral Maxillofac. Surg. Clin. North Am. 2018;30:355–367. doi: 10.1016/j.coms.2018.05.004. [DOI] [PubMed] [Google Scholar]
- Chung C.J., Choi Y.J., Kim I.S., et al. Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2011;140:404–417. doi: 10.1016/j.ajodo.2009.12.037. [DOI] [PubMed] [Google Scholar]
- Chung C.J., Choi Y.J., Kim I.S., et al. Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption. L' Orthodontie Francaise. 2012;83:225–238. doi: 10.1051/orthodfr/2012022. [DOI] [PubMed] [Google Scholar]
- Chuong R., Piper M.A. Avascular necrosis of the mandibular condyle-pathogenesis and concepts of management. Oral Surg. Oral Med. Oral Pathol. 1993;75:428–432. doi: 10.1016/0030-4220(93)90164-y. [DOI] [PubMed] [Google Scholar]
- Ha N., Hong Y., Qu L., et al. Evaluation of post-surgical stability in skeletal class II patients with idiopathic condylar resorption treated with functional splint therapy. Journal of Cranio-Maxillo-Facial Surgery : Official Publication of the European Association for Cranio-Maxillo-Facial Surgery. 2020;48:203–210. doi: 10.1016/j.jcms.2020.01.004. [DOI] [PubMed] [Google Scholar]
- Handelman C.S., Greene C.S. Progressive/Idiopathic condylar resorption: an orthodontic perspective. Semin. Orthod. 2013;19:55–70. 10.1053/j.sodo.2012.11.004 [Google Scholar]
- Hatcher D.C. Progressive condylar resorption: pathologic processes and imaging considerations. Semin. Orthod. 2013;19:97–105. 10.1053/j.sodo.2012.11.005 [Google Scholar]
- He Y., Lin H., Lin Q., et al. Morphologic changes in idiopathic condylar resorption with different degrees of bone loss. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:332–340. doi: 10.1016/j.oooo.2019.05.013. [DOI] [PubMed] [Google Scholar]
- Iwasa A., Tanaka E. Signs, Symptoms, and Morphological Features of Idiopathic Condylar Resorption in Orthodontic Patients: A Survey-Based Study. J. Clin. Med. 2022;11 doi: 10.3390/jcm11061552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Y.D., Resnick C.M., Peacock Z.S. Idiopathic condylar resorption: a systematic review of etiology and management. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130:632–639. doi: 10.1016/j.oooo.2020.07.008. [DOI] [PubMed] [Google Scholar]
- Kajii T.S., Fujita T., Sakaguchi Y., et al. Osseous changes of the mandibular condyle affect backward-rotation of the mandibular ramus in Angle Class II orthodontic patients with idiopathic condylar resorption of the temporomandibular joint. Cranio : the Journal of Craniomandibular Practice. 2019;37:264–271. doi: 10.1080/08869634.2017.1421446. [DOI] [PubMed] [Google Scholar]
- Kau C.H., Bejemir M.P. Application of virtual three-dimensional surgery planning in management of open bite with idiopathic condylar resorption. Annals of Maxillofacial Surgery. 2015;5:249–254. doi: 10.4103/2231-0746.175760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen K.D., Schmidt B., Stoustrup P., et al. Idiopathic condylar resorptions: 3-dimensional condylar bony deformation, signs and symptoms. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2017;152:214–223. doi: 10.1016/j.ajodo.2016.12.020. [DOI] [PubMed] [Google Scholar]
- Lee W.E., Chen Y.J., Yu S.J., et al. Evaluation of body composition and bone mineral density in patients with and without idiopathic condylar resorption of temporomandibular disorders by dual energy X-ray absorptiometry. Journal of Dental Sciences. 2024;19:1469–1476. doi: 10.1016/j.jds.2024.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee G.H., Park J.H., Lee S.M., et al. Orthodontic Treatment protocols for patients with idiopathic condylar resorption. J. Clin. Pediatr. Dent. 2019;43:292–303. doi: 10.17796/1053-4625-43.4.12. 10.17796/1053-4625-43.4.12 [DOI] [PubMed] [Google Scholar]
- Lee G.H., Park J.H., Park Y.G., et al. Orthodontic treatment of an open bite after splint therapy for a patient with idiopathic condylar resorption. Journal of the World Federation of Orthodontists. 2024;13:38–47. doi: 10.1016/j.ejwf.2023.12.001. [DOI] [PubMed] [Google Scholar]
- Mao B., Tian Y., Li J., et al. A quantitative analysis of facial changes after orthodontic treatment with vertical control in patients with idiopathic condylar resorption. Orthod. Craniofac. Res. 2023;26:402–414. doi: 10.1111/ocr.12623. [DOI] [PubMed] [Google Scholar]
- Mehra P., Nadershah M., Chigurupati R. Is Alloplastic Temporomandibular Joint reconstruction a viable option in the surgical management of adult patients with idiopathic Condylar Resorption? Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2016;74:2044–2054. doi: 10.1016/j.joms.2016.04.012. [DOI] [PubMed] [Google Scholar]
- Mercuri L.G. The use of alloplastic prostheses for temporomandibular joint reconstruction. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2000;58:70–75. doi: 10.1016/s0278-2391(00)80020-8. [DOI] [PubMed] [Google Scholar]
- Mercuri L.G. Osteoarthritis, osteoarthrosis, and idiopathic condylar resorption. Oral Maxillofac. Surg. Clin. North Am. 2008;20(169–183):v–vi. doi: 10.1016/j.coms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Mercuri L.G., Handelman C.S. Idiopathic Condylar resorption: what should We Do? Oral Maxillofac. Surg. Clin. North Am. 2020;32:105–116. doi: 10.1016/j.coms.2019.09.001. [DOI] [PubMed] [Google Scholar]
- Merkx M.A., Van Damme P.A. Condylar resorption after orthognathic surgery. Evaluation of treatment in 8 patients. Journal of Cranio-Maxillo-Facial Surgery : Official Publication of the European Association for Cranio-Maxillo-Facial Surgery. 1994;22:53–58. doi: 10.1016/s1010-5182(05)80297-5. [DOI] [PubMed] [Google Scholar]
- Milam S.B., Aufdemorte T.B., Sheridan P.J., et al. Sexual dimorphism in the distribution of estrogen receptors in the temporomandibular joint complex of the baboon. Oral Surg. Oral Med. Oral Pathol. 1987;64:527–532. doi: 10.1016/0030-4220(87)90025-9. [DOI] [PubMed] [Google Scholar]
- Mitsimponas K., Mehmet S., Kennedy R., et al. Idiopathic condylar resorption. Br. J. Oral Maxillofac. Surg. 2018;56:249–255. doi: 10.1016/j.bjoms.2018.02.016. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitzan, D. W. and S. Palla, 2017. “Closed Reduction” Principles Can Manage Diverse Conditions of Temporomandibular Joint Vertical Height Loss: From Displaced Condylar Fractures to Idiopathic Condylar Resorption. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 75, 1163 e1161-1163 e1120. https://doi.org/10.1016/j.joms.2017.01.037. [DOI] [PubMed]
- Nobrega M.T.C., Almeida F.T., Friesen R., et al. Idiopathic condylar resorption in adolescents: a scoping review. J. Oral Rehabil. 2024;51:1610–1620. doi: 10.1111/joor.13704. [DOI] [PubMed] [Google Scholar]
- Noh H.K., Park H.S. Considerations for vertical control with microimplants in a idiopathic condylar resorption patient: A case report. J. Orthod. 2021;48:172–182. doi: 10.1177/14653125211002211. [DOI] [PubMed] [Google Scholar]
- Papadaki M.E., Tayebaty F., Kaban L.B., et al. Condylar Resorption. Oral Maxillofac. Surg. Clin. North Am. 2007;19:223–234. doi: 10.1016/j.coms.2007.01.002. 10.1016/j.coms.2007.01.002 [DOI] [PubMed] [Google Scholar]
- Park J.H., Park J.J., Papademetriou M., et al. Anterior open bite due to idiopathic condylar resorption during orthodontic retention of a Class II Division 1 malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2019;156:555–565. doi: 10.1016/j.ajodo.2019.05.010. [DOI] [PubMed] [Google Scholar]
- Peacock Z.S., Lee C.C.Y., Troulis M.J., et al. Long-Term Stability of Condylectomy and Costochondral Graft Reconstruction for Treatment of Idiopathic Condylar Resorption. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2019;77:792–802. doi: 10.1016/j.joms.2018.10.007. [DOI] [PubMed] [Google Scholar]
- Pedersen T.K., Stoustrup P. How to diagnose idiopathic condylar resorptions in the absence of consensus-based criteria? Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2021;79:1810–1811. doi: 10.1016/j.joms.2021.04.026. [DOI] [PubMed] [Google Scholar]
- Posnick J.C., Fantuzzo J.J. Idiopathic condylar resorption: current clinical perspectives. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2007;65:1617–1623. doi: 10.1016/j.joms.2007.03.026. [DOI] [PubMed] [Google Scholar]
- Rahman F., Celebi A.A., Louis P.J., et al. A comprehensive treatment approach for idiopathic condylar resorption and anterior open bite with 3D virtual surgical planning and self-ligated customized lingual appliance. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2019;155:560–571. doi: 10.1016/j.ajodo.2017.08.032. [DOI] [PubMed] [Google Scholar]
- Saeed N.R., Kent J.N. A retrospective study of the costochondral graft in TMJ reconstruction. Int. J. Oral Maxillofac. Surg. 2003;32:606–609. doi: 10.1054/ijom.2003.0418. [DOI] [PubMed] [Google Scholar]
- Sansare K., Raghav M., Mallya S.M., et al. Management-related outcomes and radiographic findings of idiopathic condylar resorption: a systematic review. Int. J. Oral Maxillofac. Surg. 2015;44:209–216. doi: 10.1016/j.ijom.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Schellhas K.P., Wilkes C.H., Fritts H.M., et al. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am. J. Roentgenol. 1989;152:551–560. doi: 10.2214/ajr.152.3.551. [DOI] [PubMed] [Google Scholar]
- Schendel S.A., Tulasne J.F., Linck D.W., 3rd Idiopathic condylar resorption and micrognathia: the case for distraction osteogenesis. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2007;65:1610–1616. doi: 10.1016/j.joms.2007.05.001. [DOI] [PubMed] [Google Scholar]
- Shen P., Zhang D., Luo Y., et al. Characteristics of patients with temporomandibular joint idiopathic condylar resorption. Cranio : the Journal of Craniomandibular Practice. 2022;1–7 doi: 10.1080/08869634.2022.2100973. [DOI] [PubMed] [Google Scholar]
- Tanaka E. Etiology and Diagnosis for Idiopathic Condylar Resorption in Growing Adolescents. J. Clin. Med. 2023;12 doi: 10.3390/jcm12206607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troulis M.J., Tayebaty F.T., Papadaki M., et al. Condylectomy and costochondral graft reconstruction for treatment of active idiopathic condylar resorption. Journal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons. 2008;66:65–72. doi: 10.1016/j.joms.2007.08.030. [DOI] [PubMed] [Google Scholar]
- Wang J., Veiszenbacher E., Waite P.D., et al. Comprehensive treatment approach for bilateral idiopathic condylar resorption and anterior open bite with customized lingual braces and total joint prostheses. American Journal of Orthodontics and Dentofacial Orthopedics : Official Publication of the American Association of Orthodontists, Its Constituent Societies, and the American Board of Orthodontics. 2019;156:125–136. doi: 10.1016/j.ajodo.2018.02.017. [DOI] [PubMed] [Google Scholar]
- Wang H., Xue C., Luo E., et al. Three-dimensional surgical guide approach to correcting skeletal Class II malocclusion with idiopathic condylar resorption. Angle Orthod. 2021;91:399–415. doi: 10.2319/050320-383.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warburton G., Mercuri L.G. Alloplastic reconstruction of the temporomandibular joint in patients with dentofacial deformities. Atlas Oral Maxillofac. Surg. Clin. North Am. 2022;30:223–233. doi: 10.1016/j.cxom.2022.06.004. [DOI] [PubMed] [Google Scholar]
- Wolford, L. M. and L. Cardenas, 1999. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 116, 667-677. https://doi.org/10.1016/s0889-5406(99)70203-9. [DOI] [PubMed]
- Wolford, L. M., 2001. Idiopathic condylar resorption of the temporomandibular joint in teenage girls (cheerleaders syndrome). Proceedings (Baylor University. Medical Center). 14, 246-252. https://doi.org/10.1080/08998280.2001.11927772. [DOI] [PMC free article] [PubMed]
- Yang H.J., Hwang S.J. Bone mineral density and mandibular advancement as contributing factors for postoperative relapse after orthognathic surgery in patients with preoperative idiopathic condylar resorption: a prospective study with preliminary 1-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:112–118. doi: 10.1016/j.oooo.2015.03.004. [DOI] [PubMed] [Google Scholar]
- You, M. S., H. J. Yang and S. J. Hwang, 2011. Postoperative functional remodeling of preoperative idiopathic condylar resorption: a case report. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 69, 1056-1063. https://doi.org/10.1016/j.joms.2010.01.012. [DOI] [PubMed]
- Young A. Idiopathic condylar resorption: the current understanding in diagnosis and treatment. Journal of Indian Prosthodontic Society. 2017;17:128–135. doi: 10.4103/jips.jips_60_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan M., Xie Q., Shen P., et al. Do sex hormone imbalances contribute to idiopathic condylar resorption? Int. J. Oral Maxillofac. Surg. 2021;50:1244–1248. doi: 10.1016/j.ijom.2021.01.017. [DOI] [PubMed] [Google Scholar]
- Zarour C.C., Robinson C., Mian A., et al. Idiopathic Mandibular Condyle Resorption. Cureus. 2020;12:e11365. doi: 10.7759/cureus.11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Z., Y. Lu, L. Lu, et al., 2020. Distraction osteogenesis for patients with severe idiopathic condylar resorption. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 157, 439. https://doi.org/10.1016/j.ajodo.2020.01.007. [DOI] [PubMed]
- Zhou J., Fu Y., Yu L., et al. A novel three-dimensional morphological analysis of idiopathic condylar resorption following stabilisation splint treatment. J. Oral Rehabil. 2021;48:560–567. doi: 10.1111/joor.13154. [DOI] [PubMed] [Google Scholar]