Abstract
Background
Musculoskeletal (MSK) conditions are the leading cause of disability worldwide. In MSK care, access to physical therapy is a major issue. The effectiveness of telerehabilitation phone assessment in improving access to care for MSK conditions has not yet been established in Saudi Arabia.
Purpose
To compare the effect of using a telerehabilitation phone with face-to-face care initial assessment on access to care, number of sessions and goals achievement at discharge.
Methods
This is a retrospective unmatched case-control analysis of a total of 724 Epic ® Electronic Medical Records guided by the Evidence standards framework for digital health technologies. Closed referrals from January 1st, 2022, to August 4th, 2022, for adults referred to Physical Therapy for MSK conditions were included. Participants who received a phone assessment were compared to those who received face-to-face care. The t-test was used to compare the means of the lead time, days to second appointment and number of treatment sessions. Univariate logistic regression was conducted to obtain the odds ratio of the outcome factors in the phone group. Statistical significance was set at p ≤ .05. Additionally,we compared the percentage of goal achievement at discharge.
Results
The lead time in days was significantly lower for the phone group (3.82 ± 5.36) compared to the face-to-face group (15.65 ± 17.71) p < 0.0001. Longer lead times from referral to first appointment were less likely to be a phone appointment and more likely to be a face-to-face appointment p < 0.001. However, the time from the first to the second appointment was significantly longer for the phone group p<0.0001. There was no significant difference in the number of appointments between both groups. The majority of the patients in both groups achieved all therapy goals (over 80% for phone and over 75% for face-to-face).
Conclusion
Initial telerehabilitation phone assessments compared to face-to-face care were associated with improved access to care, and there was no difference in the number of therapy sessions associated with achieving treatment goals. Future research is needed to determine the clinical effectiveness of phone initial assessments in the management of musculoskeletal conditions.
Keywords: Telerehabilitation, physical therapy, telehealth , access to care, phone assessment
Introduction
Musculoskeletal (MSK) conditions are defined as conditions which affect the locomotor system, including muscles, bones, joints, tendons, and ligaments. 1 MSK conditions were ranked as the second leading cause of disability in all Gulf Cooperation Council countries as measured by years of life lived with disability in 2019. In Saudi Arabia, the prevalence of MSK conditions was seventh among all diseases in 2019 2 and the third reason for hospital visits. 3 Telerehabilitation is one of the models of healthcare provision in Saudi Arabia, and it is defined as the delivery of rehabilitation services to patients at a distance using information and communication technologies to improve accessibility, for example, using phone or videoconferencing. 4 The COVID-19 pandemic has forced the speedy adoption of telerehabilitation in Saudi Arabia, 5 and it continues to be used in alignment with the Health Sector Transformation Program and Vision 2030 launched by the Saudi Government. 6 In 2021, telerehabilitation guidelines were developed to facilitate the rehabilitation clinician's role in Saudi Arabia in providing consultation, follow-up, education, assessment, monitoring, or therapy remotely using communication technologies. Moreover, these guidelines have included ethical considerations relevant to Saudi culture and the health care system. 5
The COVID-19 pandemic has forced the speedy adoption of telerehabilitation worldwide, including Saudi Arabia, due to restricted traditional in-person visits during the pandemic to reduce the spread of infection. 5 The purpose of telerehabilitation is to increase accessibility and improve continuity of care in vulnerable, geographically remote populations with disabilities, with the potential for saving time and resources in healthcare. 4 In a recent study in Saudi Arabia, participants showed significant improvements in disability and a high level of satisfaction with the telerehabilitation intervention. 7
In April 2020, due to the rapid increase in COVID-19 cases and lockdown, Johns Hopkins Aramco Healthcare (JHAH) launched telehealth services, 8 including the Rehabilitation Services Division, specifically the Physical Therapy Department by starting phone visits for all cases, including new and follow-up patients. The sessions included evaluation, re-evaluation, and education of the patients and/ or their families. In addition to home instructions and advice, which may consist of exercise photographs/videos/ educational handouts sent via the PhysioTools ® 9 website and/ or MyChart to patients’ registered e-mails in their electronic records PhysioTools ® 9 is a web-based application used by physical therapists to provide a tailored exercise program sent via email. MyChart 10 is an online health portal and mobile application used at JHAH that gives patients easy access to appointment booking, test results and educational material which can be shared by health providers. This telerehabilitation model continued at JHAH rehabilitation services beyond the COVID-19 pandemic.
Physical therapy phone assessment and advice services reduce usual waiting list-based care and provide faster access to treatment. In addition, telerehabilitation can provide an increase in patients’ access to health specialties that are not provided in person in their cities. 11 Providing an initial phone physiotherapy service for patients with musculoskeletal conditions reduced waiting time, required fewer appointments, and was as effective as providing usual care physical therapy, but was associated with slightly lower patient satisfaction. 12
In 2013, Salisbury et al. 13 showed that physical therapy initial assessment by phone was convenient for patients to access advice or treatment (or both) and provided a triage function since patients who had the most to gain from early in-person treatment can be identified and prioritized. This model could be particularly appropriate for the assessment and treatment of musculoskeletal conditions. 13 Additionally, for some conditions such as osteoarthritis, the main recommended treatment is advice about maintaining physical activities and provision of a structured exercise program rather than hands-on therapy. Moreover, best practice guideline recommendations for musculoskeletal rehabilitation include education and exercise,14,15 both can be implemented through telerehabilitation using videoconferencing, handouts and videos sent via web or phone applications. Therefore, waiting lists might be congested with patients who could benefit from assessment and advice from a physical therapist but could have little more to gain from face-to-face appointments or are unlikely to gain benefit from physiotherapy and could be discharged. Services that have implemented this model show that half of all patients can be managed by phone alone, reducing delays for initial treatment advice and non-attendance rates at subsequent face-to-face appointments. 13 Although using physiotherapy phone assessments reduced delays in care, they were not associated with increased patient satisfaction with access to care, and overall satisfaction of patients was slightly lower than usual care. 13 However, in a recent systematic review by Amin et al., 16 the authors reported patients were satisfied with both telerehabilitation and face-to-face interventions. Overall, there was evidence that patients and rehabilitation professionals were satisfied with telerehabilitation compared to face-to-face consultations. 16
A 2024 study by Moore and Lewis 17 in the UK found that self-referral to MSK physical therapy through an in-person compared to a phone initial assessment led to fewer inappropriate sessions, reduced missed appointments, and an increase in one-off assessments. This method also resulted in higher patient satisfaction and greater physical therapist satisfaction, along with cost and time savings when compared to an equivalent number of telephone assessments.
Although physical therapy phone assessment and advice for MSK conditions have been investigated in the UK, the effectiveness of these practices has not yet been established in Saudi Arabia. This study will answer the following question: Does providing a phone initial assessment, compared to a face-to-face initial assessment for adults with musculoskeletal conditions, improve access to care, and reduce the number of sessions needed to achieve therapy goals? We hypothesized that the phone compared to the face-to-face initial assessment group, would have a shorter lead time, fewer number of sessions, a higher number of same-day closing referrals, a lower rate of no-show and cancellations, and a similar percentage of goal achievement at discharge.
The overarching aim of this project was to investigate the impact of using phone initial assessment compared to usual care face-to-face initial assessment on the following outcomes: 1) lead time to initial and second appointment; 2) number of sessions per episode of care; 3) number of referrals closed at the first appointment; 4) Percentage of no show and patient cancellation; 5) goals achievement at discharge.
Methods
Framework, study design and data source
The Evidence standards framework (ESF) for digital health technologies was used to guide the design of our study.18,19 Our study is a retrospective unmatched case-control 20 analysis of a total of 724 Epic ® Electronic Medical Records (EMR). This design is unmatched, with the comparison group selected for all cases using certain criteria as opposed to the matched design, where controls are selected on a case-by-case basis. 21 This design is suitable for the evaluation of telehealth products using retrospective data. The use of the unmatched control groups allows for control of confounding variables.21,22 Based on previous research, the matching factors were age, gender, and socio-economic status.21,23 We have obtained ethical approval for our study from the JHAH Institutional Review Board (IRB).
Study population
Individuals with closed referrals from January 1st, 2022, to August 4th, 2022, for adults aged >18 years who were referred to the Physical Therapy Department (Dhahran and Ras Tanura Clinics) at JHAH, Saudi Arabia, for musculoskeletal conditions were included. A closed physical therapy referral occurs when it is no longer authorized for scheduling appointments. This means that the patient cannot book any further sessions under that referral, typically due to the completion of treatment. Musculoskeletal physical therapy referrals can be for conditions affecting the upper limb, lower limb or spine, such as shoulder tendinitis, knee osteoarthritis or lower back pain. Referrals to the physical therapy department are received from primary care and specialty care physicians, including orthopedic surgeons, rheumatologists, neurologists, neurosurgeons, and pain specialists. Primary care physicians have the option to refer some patients to the primary care physical therapist, who can see them on the same day. All other referrals from primary and specialty clinics are received by the physical therapy department and are triaged by a physical therapist who could request scheduling a phone or face-to-face initial assessment based on clinical judgement. Participants who received a phone initial assessment were compared to the face-to-face initial assessment group, controlling for age, gender, and educational level.21,23
Referrals were selected if they matched the following criteria: Inclusion criteria: 1) closed musculoskeletal referrals from January 1st, 2022, to August 4th, 2022; 2) adults aged >18 years; 3) referred to the Physical Therapy Department at JHAH Dhahran and Ras Tanura sites. Exclusion criteria: 1) open musculoskeletal referrals authorized for scheduling appointments; 2) age < 18 years old, 3) duplicate referrals; 4) referrals seen by primary care physical therapy 30 min initial assessment; 5) neurological referrals; 6) postoperative referrals; 7) pediatric referrals; 8) women's health referrals (involving pelvic floor, e.g., bowel & balder incontinence or post-breast cancer lymphedema); 9) referral to other JHAH sites in AlAhsa, Abqaiq, and Udalliya.
Variables
Our study will compare two groups: First, the phone group, which included patients who received an initial 30-minute phone assessment by a physical therapist, which included history of present illness, past medical history, pain assessment, functional limitations, goals for treatment and outcome measures. Based on the assessment, the patients were provided with advice and sent educational materials/exercises through the PhysioTools ® 9 and/ or MyChart 10 application as needed. If necessary, they were offered an in-person 60-minute session (described below) followed by in-person follow-up sessions of 40 minutes (described below) each as needed. Second, the face-to-face group included patients who received the usual care 60-minute assessment in person by a physical therapist, which included the history of present illness, past medical history, pain assessment, functional limitations, range of motion, muscle strength, special tests, goals for treatment and outcome measures. This can be followed by in-person follow-up sessions of 40 minutes each, as needed. The in-person sessions may include exercise, education, manual therapy or other physical therapy modalities, as per the physical therapist's clinical judgement. In addition, printed or emailed educational materials/home exercises through the PhysioTools ® 9 and/ or MyChart 10 applications were provided..
The following are the definitions of our study outcomes: Primary: 1) lead time to initial appointment: the average number of days between the date of creation of the physical therapy referral and the date of the first patient appointment; Secondary: 1) lead time to the second appointment: the average number of days between the first and second appointment; 2) number of sessions per episode of care: the average total number of sessions per referral; 3) number of referrals closed on the first appointment: number of referrals closed at the first encounter; 4) rate of no-show and patient cancellations: percentage of no-show or cancellations of appointments; 5) goals achievement at discharge: the percentage of patient's goal achievement as the reason for discharge, whether patients achieved all or some therapy goals or achieved rehabilitation to the maximum potential or other reasons.
Potential confounding variables in telehealth include age, gender, and socioeconomic status.18,21–23
Data extraction
The JHAH Health Informatics Team extracted and anonymized data from consecutive patients from January 1st, 2022, to August 4th, 2022. A total of 1198 medical records matched our inclusion and exclusion criteria in the Epic® EMR. Patients who received consultations over the phone were matched with patients who received face-to-face treatment in a 1:1 ratio based on age, gender, and educational level. After records were excluded due to missing data, a total of 724 records were identified and included in the analysis.
Data analysis
IBM Statistical Package for Social Sciences ® (SPSS) software version 29 was used to carry out the analysis. Descriptive statistics using frequency and percentage were used to summarize the groups’ characteristics: age, gender, educational level, type of pain (acute, chronic, or other), pain score at the initial visit, and referral type (spine, upper limb, and lower limb). The t-test was used to compare the means of the groups (initial phone visit, initial face-to-face assessment) for lead time, number of treatment sessions, closing of referrals on the first session, and the rate of no-show or cancellation. Univariate logistic regression was conducted to obtain the odds ratios between the two groups with respect to the outcome variable. A p -value < 0.05 was considered to be significant for the analysis. In addition, we compared the percentage of the reasons for discharge in each group: achieved all therapy goals, achieved some therapy goals, rehabilitated to maximum potential, poor compliance, or other. We conducted a complete case analysis, and records with missing data were excluded.
Sample size justification
A case-control study design was used to investigate the efficacy of phone initial assessment in reducing the waiting time. Based on available information, approximately 40% of patients had not received phone appointments. To detect a significant difference in the waiting time between cases and controls, with 90% confidence that the estimate of the odds ratio (OR) will not underestimate the true OR by more than 25% of its true value, which is assumed to be within 2, a sample size of 270 subjects was required in each of the case and control groups. Assuming 20% missing data, at least 648 records needed to be extracted.
Results
Tables 1 and 2 provide the characteristics of the two groups: the phone and face-to-face initial assessment. The analysis was matched based on age, gender, and education level. The mean pain score was 6.28 ± 1.83 for the phone and 6.59 ± 2.07 for the face-to-face groups. There was no significant difference in the average pain score between the two groups. The average number of appointments was 6.91 ± 4.50 in the first group and 6.85 ± 4.57 in the second group, with no significant difference between them. A total of 4.75% of referrals were closed on the first appointment in the phone group, compared to 6.79% in the face-to-face group with no significant difference. There was a statistically significant difference in the primary study outcome, the lead time, which was significantly shorter for the phone group, 3.82 ± 5.36, compared to the face-to-face group, 15.65 ± 17.71, with a p-value of <0.0001. Similarly, the time from the first appointment to the second appointment was significantly longer for the phone group, 17.41 ± 14.48 compared to the face-to-face group, 12.21 ± 15.78, with a p-value of <0.0001 (Table 3).
Table 1.
Demographics of both phone and face-to-face groups n = 724
| Variables | |
| Age, mean (SD) | 51.33 (12.55) |
| Gender, n (%) | |
| Female | 261 (72.1) |
| Male | 101 (27.9) |
| Education level, n (%) | |
| Primary School | 12 (3.79) |
| High School | 10 (3.15) |
| College | 91 (28.71) |
| Other | 204 (64.35) |
Table 2.
Comparison of the characteristics between phone and face-to-face groups
| Phone | Face-to-face | P-value | |||
|---|---|---|---|---|---|
| 362 | 362 | ||||
| mean | SD | mean | SD | ||
| Average Pain score | 6.28 | 1.83 | 6.59 | 2.07 | 0.107 |
| N | % | N | % | ||
| Referred To Department | <.0001 | ||||
| DHH Physical Therapy | 339 | 93.65% | 289 | 79.83% | |
| RT Physical Therapy | 23 | 6.35% | 73 | 20.17% | |
| Referral Type | 0.6702 | ||||
| Upper Extremity | 96 | 26.52% | 109 | 30.11% | |
| Lower Extremity | 89 | 24.59% | 91 | 25.14% | |
| Spinal | 177 | 48.90% | 162 | 44.75% | |
| Pain type | 0.4900 | ||||
| Acute pain | 94 | 29.75% | 63 | 25.61% | |
| Chronic pain | 221 | 69.94% | 181 | 73.58% | |
| Other | 1 | 0.32% | 2 | 0.82% | |
Table 3.
Average lead time in days and number of appointments for phone and face-to-face phone groups
| Group | |||||
|---|---|---|---|---|---|
| Phone | Face-to-face | ||||
| 362 | 362 | ||||
| mean | SD | mean | SD | P-value | |
| Average lead time in days for first appointment | 3.82 | 5.36 | 15.65 | 17.71 | <.0001 |
| Average Number of Appointments per episodes | 6.91 | 4.50 | 6.85 | 4.57 | 0.869 |
| Average lead time in days for second appointment | 17.41 | 14.48 | 12.21 | 15.78 | <.0001 |
| N | % | N | % | ||
| Number of referral closed on 1st appointment | 21 | 4.75 | 30 | 6.79 | 0.1942 |
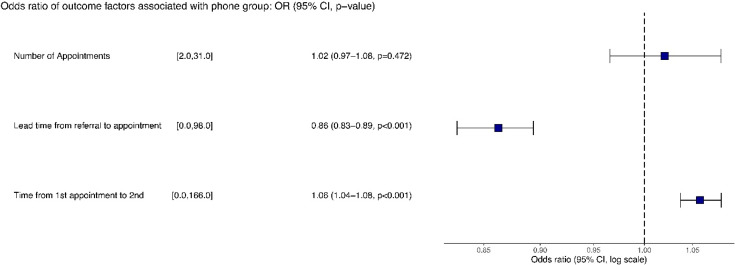
Figure 1 shows the OR with 95% confidence interval (CI). Comparing the phone group to the face-to-face group, three explanatory variables were considered: number of appointments, lead time from referral to first appointment, and time from first to second appointment. The results showed that the number of appointments was not significantly associated with the odds of being in the phone group. However, longer lead times from referral to appointment were less likely being a phone appointment and more likely to a face-to-face appointment, while longer time intervals between first and second appointment were more likely to be a phone appointment (p -value < 0.001 for both variables).
Figure 1.
Odds ratio of outcome factors associated with phone group.
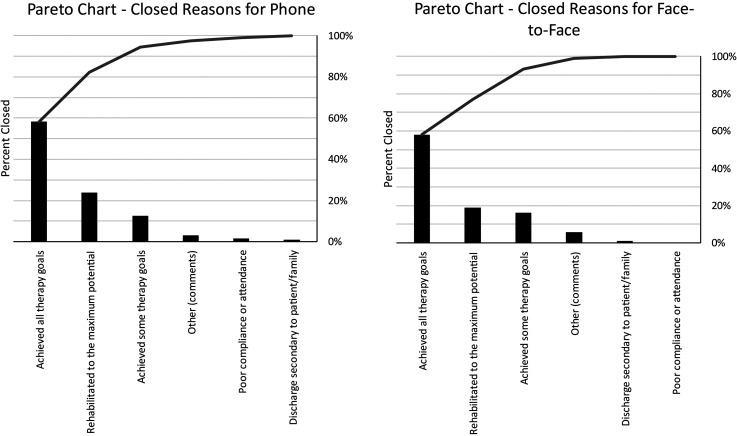
The Pareto chart in Figure 2 shows that the top two reasons for closure in both groups were achieving all therapy goals and rehabilitating to the maximum potential. Together, these reasons accounted for most closures (over 75% for face-to-face and over 80% for phone). The third most common reason for closure was achieving some therapy goals, which accounted for around 12% of phone and 16% of face-to-face closures. Other reasons for closure, such as poor compliance or attendance and discharge due to patient/family reasons, accounted for less than 2% of closures each.
Figure 2.
Pareto chart showing reason for discharge and closing referral for the two groups
A binomial analysis was conducted on the closed status for both groups. As shown in Table 4, the canceled status for phone appointments accounted for 20.4% (511) and for face-to-face appointments accounted for 22.6% (560) of the total appointments. For the completed status, the phone appointments represented 73.4% (1834) and the face-to-face appointments represented 72.1% (1789) of the total appoitments. The no-show status consisted of 6.2% (154) phone appointments and 5.1% (127) face-to-face appointments. However, the binomial analysis did not reveal statistically significant results.
Table 4.
Frequency and percentage of cancelled, completed, no-show and scheduled appointments for phone compared to face-to-face groups
|
Frequency Percentage |
Groups | ||
|---|---|---|---|
| Phone N % |
Face-to-face N % |
||
| Closed status | Canceled | 511 20.4% |
560 22.6% |
| Completed | 1834 73.4% |
1789 72.1% |
|
| No Show | 154 6.2% |
127 5.1% |
|
| No Show Error | 0 0.0% |
1 0.0% |
|
| Scheduled | 1 0.0% |
3 0.1% |
|
| Total Appointments | 2500 | 2480 | |
| Total Cases | 362 | 362 | |
| Total Cases Responding | 362 | 362 | |
Discussion
Our study aimed to explore the impact of initial phone telerehabilitation physiotherapy assessment for patients with musculoskeletal conditions at JHAH in Saudi Arabia beyond the COVID-19 pandemic. The results showed that there was no significant difference (p-value < 0.05) in the average number of appointments between both groups. However, there was a statistically significant difference in the primary study outcome, the lead time, which was significantly shorter for the phone group compared to the face-to-face group. This can be attributed to a recent practice at JHAH, in addition to regular scheduled phone visits, they were used to utilize in-person late cancellation slots (< 24 h), which has contributed to improving access to care as well as enhancing the schedule utilization. The time from the first appointment to the second appointment was significantly longer for the phone group compared to the face-to-face group. This could be explained by the fact that they were scheduled face-to-face assessment slots, with limited availability and underlined the importance of making more of these slots available to improve access and continuity of care. The top two reasons for discharging patients and closing referrals in both groups were achieving all therapy goals and rehabilitating to the maximum potential. . We found no significant difference (p-value < 0.05) between both groups for closing referrals at the first appointment.
The results of this study are consistent with previous studies that have shown that telerehabilitation phone assessments improve access to care. 13 Although our study did not have a clinical outcome measure as a variable, we looked at the reason for discharge, and the top reason in both groups was the achievement of all therapy goals. A recent study in Saudi Arabia have shown that telerehabilitation for patients with muscloskeletal conditions using videoconferencing as an alternative to in-person care, had a positive impact on improving patient outcomes and was an acceptable method of rehabilitation. 7
Our study adds to the existing literature by reinforcing evidence of using phone initial assessment in reducing lead time and improving access to care for patients with musculoskeletal conditions. Contrary to our findings of no difference between both groups in closing referrals at the first encounter, a recent study has reported that face-to-face initial assessment was more effective than phone initial assessment at closing referrals at the first appointment with a statistically significant difference (p < 0.05). 17
This study has several strengths and limitations. Our major strength is that we were able to help estimate the effects of phone physical therapy assessment using existing data in the EPIC EMR by using a case-control design, which is suitable for retrospective analysis of existing data. 20 Another strength of this design is that it included the unmatched control group based on confounding variables identified from the literature, which may affect the outcome of telerehabilitation, including age, gender and educational level.19,20 Including this control group eliminated several biases of single group study design threatening the validity of the study, such as regression towards the mean and confounding variables. Our limitations are related to biases of retrospective design, including selection bias. 20 Another limitation of this design is that certain variables that have the potential to impact the outcome may not have been included as part of the EMR. 24 In our case we were unable to control for other confounders, such as socioeconomic status, due to the lack of this data in the EMR. Another source of bias in the retrospective design was the incompleteness of the EMR data, 24 which led to the exclusion of these records due to missing data. Therefore, the results of our study should be interpreted with caution, and the cause-and-effect relationship between our variables cannot be determined.
Conclusion
Our study has provided evidence that telerehabilitation phone visit initial assessment was associated with improved access to care and physical therapy goal achievement at discharge for patients with musculoskeletal conditions in Saudi Arabia. More studies are needed to determine the clinical effectiveness, patient and provider satisfaction, and economic impact of telerehabilitation phone compared to face-to-face assessments with long-term follow-up to inform the development of telerehabilitation programs for patients with musculoskeletal conditions.
Acknowledgements
This study has been undertaken as part of the Epic Scholar Program, a collaboration between the JHAH's Research Office and Johns Hopkins Medicine. We would like to acknowledge the support of Mrs. Lamia Alazayer, Senior Director of Specialized Therapy and Clinical Services, Dr. Hayat Almushcab, Manager of the Research Department, and our Biostatistician, Anwar Alotaibi. We would also like to acknowledge the funds provided by JHAH to publish our work.
Footnotes
| Author | Contribution |
| Lina Elsabbagh | Conceptualization, methodology, data curation, formal analysis & writing |
| Hanan AlQahtani | Conceptualization, methodology, data curation, formal analysis & writing |
| Alanood Adil Alsultan | Conceptualization, methodology, data curation, formal analysis & writing |
| Haya Jassem AlDossary | Conceptualization, methodology, data curation, formal analysis & writing |
| Husain Alresheidi | Conceptualization, methodology & writing |
| Akram Abdelhamid | Conceptualization, methodology & writing |
| Dina W Buraik | Conceptualization, Methodology, Data Curation & Writing |
The funding for the open-access publication fees was provided by JHAH. In addition, the authors received an authorship incentive.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by JHAH.
Ethical considerations: This study received ethical approval from the JHAH IRB(approval #22-20) on January 23, 2023. This is an IRB-approved retrospective study, all patient information was de-identified and patient consent was not required.
Guarantor: L.E
ORCID iD: Lina Elsabbagh https://orcid.org/0000-0002-4523-9563
References
- 1. Musculoskeletal conditions . World Health Organization - Technical Report Series . 2021.
- 2.Alzahrani H, Alshehri MA, Alotaibi M, et al. Burden of musculoskeletal disorders in the gulf cooperation council countries, 1990–2019: findings from the global burden of disease study 2019. Front Med (Lausanne) 2022; 9: 855414. 20221004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alrwaily M, Alanazi F. Prevalence and determinants of knowledge of musculoskeletal disorders among healthcare providers and students in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc 2022; 15: 1789–1797. 20220825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seron P, Oliveros MJ, Gutierrez-Arias R, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther 2021; 101: pzab053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qureshi AZ, Ullah S, Aldajani AA, et al. Telerehabilitation guidelines in Saudi Arabia. Telemed J E Health 2021; 27: 1087–1098. 20210127. [DOI] [PubMed] [Google Scholar]
- 6.Saudi Government V. Health Sector Transformation Program. 2023.
- 7.Alsobayel H, Alodaibi F, Albarrati A, et al. Does telerehabilitation help in reducing disability among people with musculoskeletal conditions? A preliminary study. Int J Environ Res Public Health 2022; 19: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johns Hopkins Aramco Healthcare. JHAH Appointments and Referrals, https://www.jhah.com/en/patient-information/appointments-and-referrals (2023).
- 9.PhysioTools ® https://gateway.physiotools.com/PTMaintenance/login.
- 10.MyChart, https://www.jhah.com/en/about-mychart#:∼:text=Your%20online%20health%20portal%20MyChart,just%20a%20few%20simple%20steps.
- 11.Baroni MP, Jacob MFA, Rios WR, et al. The state of the art in telerehabilitation for musculoskeletal conditions. Archives of Physiotherapy 2023; 13: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iles R. A physiotherapy telephone assessment and advice service for patients with musculoskeletal problems can improve the process of care while maintaining clinical effectiveness. J Physiother 2013; 59: 130. [DOI] [PubMed] [Google Scholar]
- 13.Salisbury C, Montgomery AA, Hollinghurst S, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ (Online) 2013; 346: f43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nice. Overview | Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain | Guidance | NICE. 2021.
- 15.Korownyk CS, Montgomery L, Young J, et al. PEER Simplified chronic pain guideline: management of chronic low back, osteoarthritic, and neuropathic pain in primary care. Can Fam Physician 2022; 68: 179–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amin J, Ahmad B, Amin S, et al. Rehabilitation professional and patient satisfaction with telerehabilitation of musculoskeletal disorders: a systematic review. Biomed Res Int 2022; 2022: 7366063. 20220802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore L, Lewis A. Self-referral to musculoskeletal physiotherapy in the national health service (NHS): a mixed methods, four-domain analysis of 1,000 adult new patients initially assessed via telephone versus face-to-face. Eur J Physiother 2024: 1–12.39555220 [Google Scholar]
- 18.Unsworth H, Dillon B, Collinson L, et al. The NICE evidence standards framework for digital health and care technologies - developing and maintaining an innovative evidence framework with global impact. Digit Health 2021; 7: 20552076211018617. 20210624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Institute for Health and Care Excellence. Evidence standards framework for digital health technologies, www.nice.org.uk/corporate/ecd7 (2018).
- 20.Mann CJ. Observational research methods. Research design II : cohort. cross sectional, and case-control studies. Emerg Med J 2003; 20: 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Office for Health Improvement Disparities. Case-control study: comparative studies, https://www.gov.uk/guidance/case-control-study-comparative-studies (2021).
- 22.Office for Health Improvement Disparities. Evaluating digital health products, https://www.gov.uk/government/collections/evaluating-digital-health-products.
- 23.Alanezi F. Factors affecting the adoption of e-health system in the kingdom of Saudi Arabia. Int Health 2021; 13: 456–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Talari K, Goyal M. Retrospective studies - utility and caveats. J R Coll Physicians Edinb 2020; 50: 398–402. [DOI] [PubMed] [Google Scholar]