Abstract
This study examined various factors, including social support as a mediating one, influencing subjective unmet needs (SUN) in Vietnamese older people during the COVID-19 pandemic. Using logistic regression models with a national survey on older persons, we identified determinants of SUN, and then further explored how social support moderated the association between experiencing SUN and chronic diseases. We found that about 25% of Vietnamese older persons experienced SUN during the pandemic, in which more advanced age, living alone, lack of healthcare insurance and having chronic diseases were risk factors, while higher education, better wealth, and stronger social support played as protective factors. Particularly, social support was found a significantly moderated factor between SUN and chronic diseases. Based on these findings, we argued that it would be imperative to strengthen healthcare system at the grassroot level so as to improve accessible and adequate care for older persons, especially those with chronic diseases. Also, enhancing social support via solidary family and community members, particularly in times of crisis, was recommended to address older persons’ healthcare needs.
Keywords: social support, COVID-19, Vietnam, older people, subjective unmet need, chronic diseases
What do we already know about this topic?
Due to the COVID-19 pandemic, patients with chronic diseases, particularly older persons, faced considerable barriers to access healthcare services, such as service disruptions, closures, appointment cancellations, as well as fear of infection, travel restrictions, and income losses. These factors might result in their subjective unmet needs (SUN) of healthcare.
How does your research contribute to the field?
Older persons’ SUN and its determinants have not been explored widely in middle-income countries. Also, no studies investigated the mediating role of social support on the association between older persons’ SUN and their health during the COVID-19 pandemic. Our study is the first to explore these issues with the case of Vietnamese older people.
What are your research’s implications toward theory, practice, or policy?
Our study supported the buffering and main-effect mechanisms in explaining how social support could mitigate experiencing SUN. In addition, with the determinants of SUN, we provided policy implications for Vietnam and other middle-income countries in dealing with SUN among older persons.
Introduction
The COVID-19 pandemic posed unprecedented challenges worldwide. Beyond causing millions of deaths, it has severely strained healthcare systems. 1 To curb the rapid spread of the COVID-19 within and across countries, governments imposed nationwide knockdown or curfews and called for reduction in hospital admissions except for urgent cases in the provision of health. These measures resulted in restricted access to both inpatient and outpatient services for people with regular healthcare needs.1,2 The pandemic presented a considerable barrier for diagnosis, follow-up, and treatment of chronic diseases among non-COVID-19 cases due to service disruptions, closures, and appointment cancellations in all healthcare providers.3,4 Moreover, factors such as fear of infection, travel restrictions, and income losses further limited individuals’ ability to seek healthcare.5,6 These restrictions likely increased subjective unmet needs (SUN), which potentially resulted in poorer health outcomes, economic losses, and increased health inequality.7,8 Sustainable healthcare access is vital for health and well-being of older people, particularly in a crisis like the COVID-19, because they need greater healthcare demands than other groups due to higher prevalence of chronic conditions, disabilities, and mental problems that may exacerbate their vulnerability to the pandemic.9,10 and these health conditions might increase risk of mortality if older persons were infected.11,12 Similarly, older persons might potentially lack of social support and experience misinformation due to measures such as social distancing. 13
Access to healthcare is considered as one of the most important achievements of health systems. SUN, defined as individuals’ subjective assessments of whether they could receive necessary care, is an important measure of barriers to healthcare access. 14 Understanding the factors influencing SUN during the COVID-19 pandemic is crucial for future policy planning, given the significantly negative impacts of unmet healthcare needs on health outcomes. The existing studies on the determinants of SUN during the COVID-19 had 2 key research gaps. First, a limited number of studies specifically addressed older population, with much of the existing research conducted in high-income settings.15 -19 This highlights a lack of knowledge regarding the relationship between experiencing SUN and its determinants in low- and middle-income countries. Secondly, despite the vital role of social support in improving health and well-being among older persons20 -22 and decreasing unmet healthcare needs, 23 to the best of our knowledge, there have been no studies investigating the mediating effect of social support on the association between experiencing SUN and health in older persons during the pandemic.
As a middle-income country, a rapidly aging population has posed significant healthcare challenges for Vietnam. 24 The proportion of older population (those aged 60 and over) is projected to reach about 25% of the total population by 2050. 25 This demographic shift signals an increased demand for healthcare services because chronic disease risks and disability prevalence tend to rise along with age-related health deterioration. The national survey on Vietnamese older people in 2019 highlighted this concern: 52.6% reported poor or very poor health status. 24 Moreover, the prevalence of multiple diagnosed chronic diseases was high, peaking at 53.4% for the middle-old (those aged 70-79) and 42.1% for the oldest old (those aged 80 and over). 24 Heart disease, cancers, and chronic obstructive pulmonary diseases (COPD) were among the most common, collectively accounting for approximately 89% of lost disability-adjusted life years among the Vietnamese older people. 24
Recognizing the challenges of an aging population, the Government of Vietnam (GOV) has implemented a series of healthcare and social protection policies specifically designed for its older citizens. The Law on the Elderly outlines the rights of older persons to access healthcare and prioritizes healthcare for the oldest old. 26 Moreover, GOV provides financial support for vulnerable groups, offering free health insurance to low-income individuals and social assistance programs for those living alone or in poor households without family support.27,28
Vietnam was significantly impacted by the COVID-19 pandemic, in which older persons were particularly affected. The first COVID-19 case was reported on January 23rd, 2020. During the early phases of the COVID-19 pandemic, GOV implemented preventive measures, including social distancing, lockdown, and curfews. These measures were gradually lifted in 2022, 29 and over 11 million cases of infection and 43 000 deaths were reported by early 2024. 30 Notably, on average, 50.4% of fatalities occurred among those aged 65 and older, which was substantially higher than 13.8% of those aged 18 to 49. 31 Despite the government’s proactive efforts to safeguard older people, challenges in meeting their healthcare needs persisted from both demand side (such as fears of infection and reluctance to receive vaccinations) and supply side (such as lower capacity in meeting demand for check-ups, medications, assistive devices, and rehabilitation services). 32
To date, however, there have been no studies to examine the factors influencing unmet healthcare needs in Vietnamese older people during the pandemic. Our study therefore aimed to provide the first empirical evidence on these factors and whether social support could mitigate the relationship between SUN and chronic diseases among Vietnamese older people. More specifically, using the most recent national survey on Vietnamese older people and a standard measure of SUN, we pioneered the examination of various factors affecting SUN and investigated the extent to which social support mediated the relationship between chronic diseases and experiencing SUN.
Literature Review on Social Support and SUN
Social support is a multifaceted concept that can be defined as the perceived availability of assistance from family, friends, and loved ones. Social support plays a crucial role in accessing resources because individuals’ interpretations of life stressors and their perceived availability of coping resources influence the protective benefits of social support. 20 Social support can be categorized into three forms among others, 33 as follows: (i) emotional support (providing a sense of belonging and connection through close relationships and feelings of being cared for); (ii) tangible/instrumental support (offering practical assistance in the form of financial aid, help with daily tasks, and support during crises); and (iii) informational support (providing access to valuable information, such as healthcare recommendations, through advice and discussions).
Social support could affect SUN through buffering and main-effect pathways. 20 For the former, social support acted as a buffer against the negative effects of stress by enhancing self-esteem, promoting healthy coping mechanisms, reducing feelings of loneliness and helplessness,34,35 and reducing loneliness and enhancing physical and mental health for older persons. 36 Stronger social support networks resulted in positive health behaviors (eg, medication adherence, regular exercise, and a healthy diet), and thus increasing confidence and lowering anxiety. 37 For the latter, social support improved access to social resources, particularly tangible/instrumental and informational support, which in turn provided protection to individuals via healthcare services and resources. Strong connections with family, friends, and relatives could offer various support forms, which helped not only to alleviate the burdens associated with stressful situations but also fulfill the psychological need of feeling valued by others.38,39 Significant and positive association between stronger social support and better healthcare access was found.23,40,41 Given these two pathways, we hypothesized in this study that social support, particularly family and community support, mediated the association between experiencing SUN and chronic diseases in Vietnamese older persons.
Data and Analytical Methods
Data
We used the most recent nationally representative survey on the Vietnamese older people (those aged 60 and over), namely the Vietnam Aging Survey (VNAS) in 2022, which was reviewed and approved by the Institute of Social and Medical Studies (ISMS)’s Institutional Review Board in Biomedical Research under the Decision 04/HDDD-ISMS dated July 18th, 2022. The survey aimed to provide timely information on the impact of COVID-19 on Vietnamese older persons’ socioeconomic status, access and utilization of healthcare services and social participation. Face-to-face interviews using structured questionnaires were used to collect data. The survey employed a multiple-stage sampling and population proportionate to size (PPS) methods were used to select provinces, districts, and communes. More specifically, 12 provinces were selected across 6 economic regions in Vietnam. Out of these provinces, 3 districts were chosen in each province and then 4 communes were drawn per 1 selected district. At cluster (village) and individual levels, a systematic random sampling method was used to select 3 villages per commune and 10 people per village. In total, 3168 older people were successfully interviewed.
Since we were interested in unmet needs for healthcare access during the COVID-19, we excluded those who responded that they did not have needs for healthcare services during this time. Finally, the analytic sample consisted of 2140 observations with non-missing values on variables of interest.
Measures
Dependent variable
Subjective unmet needs (SUN) was the outcome of interest, which was measured using the following 3 yes/no questions since the COVID-19 pandemic:
Question 1 measured the forgone healthcare services due to COVID-19 infection: “Have you ever forgone a medical treatment because you were afraid to become infected by the COVID-19?”
Question 2 measured the postponed health treatment: “Have you ever delayed/postponed a medical treatment because you were afraid to be infected by the COVID-19?”
Question 3 measured the unavailable healthcare services: “Did you have a scheduled medical appointment that the doctor or medical facility decided to postpone due to the COVID-19?”
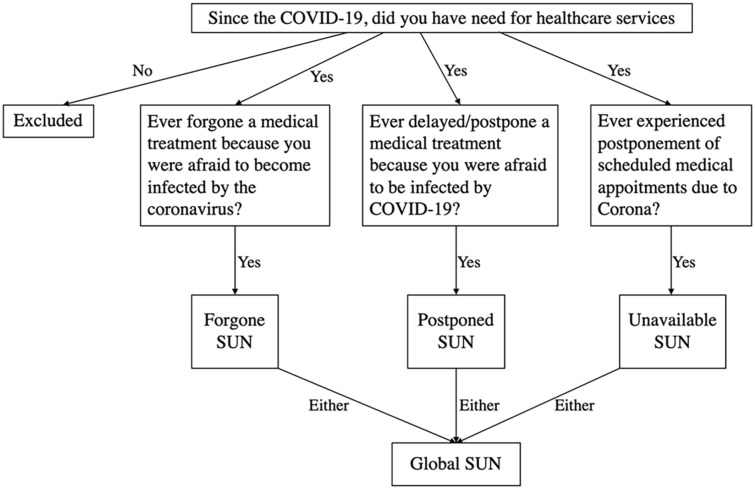
These questions have been used widely to measure SUN across developed and developing countries during the COVID-19 pandemic.18,24 In order to examine different aspects of limits in healthcare access during the COVID-19, we created 3 binary outcomes: (i) forgone SUN if the respondent answered “yes” to the first question; (ii) postponed SUN if the respondent answered “yes” to the second question; and (iii) global SUN if the respondent answered “yes” to each of the 3 questions. The measures of each type of SUN were depicted in Figure 1. Due to the small proportion of the third question (2.4%), it was not feasible to run a regression with this.
Figure 1.
Determination of each type of subjective unmet need (SUN).
Source. Own illustration.
Independent variables
We followed previous studies to select 4 main groups of independent variables.18,24 The first group included demographic variables: age groups (60-64 as reference group; 65-69; 70-74; 75-79; and 80+), gender (1 if females; 0 otherwise), marital status (1 if currently married; 0 otherwise), ethnicity (1 if Kinh [majority] people; 0 otherwise), place of residence (1 if residing in rural areas; 0 if urban areas), and living arrangements (1 if living alone; 0 otherwise).
The second group, presenting socioeconomic status (SES), consisted of the highest educational attainment (no schooling or incomplete primary school [hereafter no schooling] as reference group; primary school; secondary school; and high school and above). Household wealth scores were derived using principal component analysis (PCA) based on a set of durable household assets.42,43 This method has been used in previous studies in Vietnam. 44 The wealth scores were then divided into 5 quintiles, among which the first quintile denoted the poorest (reference group) and the fifth indicated the wealthiest. Health insurance status took on the value of 1 if an older person had a health insurance card, and 0 otherwise.
The third group refers to heath conditions of the respondents. Activities of daily living (ADLs) measured levels of difficulty in 5 activities (eg, eating, getting dressed and undressed, bathing, getting up when lying down, and toileting). Each activity was given 4 responses: no difficulty; mild difficulty; severe difficulty; and could not do at all. Summation of these responses across the 5 activities resulted in 15 points, which were then divided in 4 categories: no ADL difficulty (as reference group); 1-2 ADLs; 3-4 ADLs; and 5+ ADLs. Chronic diseases (such as arthritis and blood pressure problem) consisted of a list of 17 yes/no questions on diagnosed diseases by doctors. If a respondent responded “yes” to a specific disease, he/she was subsequently asked whether he/she received treatment or took medications for that disease in the last 12 months. To align with the above definitions of SUN and following previous literature, we measured the presence of a chronic disease as those who had a chronic disease and were under treatment or took medications for that disease. 24 We measured chronic diseases in categories: no disease (reference group); 1 disease; 2 diseases; 3-4 diseases; and 5+ diseases.
Finally, we controlled for social support variables, which have found to be important determinants of unmet needs for healthcare utilization. 45 The first variable was children’s support, which was measured by whether the respondents received either cash or in-kinds from their children in the last 12 months. The second variable was community support, which was derived from the following question: “Since the COVID-19 pandemic, what types of support that you received from community and individuals (except supports receiving when you/your family gets COVID-19)?” This binary variable took a value of 1 if the respondents received any of the following support (medical supplies such as oxygen or monitor machine; health counseling; health checks; medicines; medicated sanitizers; foods; or money), and 0 otherwise.
Analytical Strategy
We first provided descriptive statistics of independent variables disaggregated by SUN outcomes. Chi-squared tests were used to assess differences in proportion between the dependent and independent variables.
The existing literature has demonstrated the importance of model specification to avoid biased and misleading estimates.46,47 Since our dependent variables were measured as binary, we employed logistic regressions to examine the factors associated with the likelihood of experiencing each type of SUN, controlling for all above-mentioned independents. Following previous literature, we employed Pregibon’s link test to assess the specification form of independent variables. 47 The link test results indicate that the squared predicted values had no explanatory power (ie, P-value > .1) when we regressed our dependent variables on the predicted values and its square, suggesting that all independent variables controlled in our models were well specified. Similarly, to examine the presence of multicollinearity issue, we performed variance inflation factor (VIF) tests, and the results show that the VIF value of each dependent variable was smaller than 2, implying there was no evidence of perfect multicollinearity. 48
In order to further examine whether social support mediated the association between chronic diseases and SUN, we added an interaction term between social support and chronic diseases to logistic regression for each type of SUN. Results were presented by odds ratios (ORs).
All statistical analyses were weighted using the survey weights and clustered at the cluster level (villages) to account for the multistage sample design. Also, statistical significance level was set to P < .05.
Results
Descriptive Statistics
Table 1 presents descriptive statistics of the respondents’ characteristics by types of SUN. In general, 25.1% of respondents experienced SUN due to either forgone, postponed, or unavailable services during the COVID-19. Among them, 21.2% were forwent medical treatments; 11.8% were postponed with their pre-scheduled services, and 2.4% were denied healthcare. Analysis of global SUN revealed significant differences in proportions of those experiencing SUN across age groups, ethnicity, living arrangements, place of residence, the highest educational level, health insurance status, ADL categories, chronic disease categories, and community support. Similar results were found for forgone and postponed SUN, with the following exceptions: living arrangements and health insurance status were statistically insignificant, while gender showed statistical significance.
Table 1.
Descriptive Statistics by Types of Subjective Unmet Need (SUN).
| Characteristics | Global SUN | P-value | Forgone SUN | P-value | Postponed SUN | P-value |
|---|---|---|---|---|---|---|
| Age groups | ||||||
| 60-64 | 19.6 | <.001 | 19.6 | <.05 | 17.9 | <.001 |
| 65-69 | 20.7 | 20.2 | 21.0 | |||
| 70-74 | 24.2 | 23.6 | 29.8 | |||
| 75-79 | 16.9 | 17.0 | 17.9 | |||
| 80+ | 18.6 | 19.6 | 13.4 | |||
| Gender | ||||||
| Male | 40.0 | 39.9 | 34.5 | <.05 | ||
| Female | 60.0 | 60.1 | 65.5 | |||
| Marital status | ||||||
| Married | 61.8 | 59.7 | 61.1 | |||
| Other | 38.2 | 40.3 | 38.9 | |||
| Ethnicity | ||||||
| Kinh | 94.6 | <.001 | 94.3 | <.001 | 94.8 | <.001 |
| Other | 5.4 | 5.7 | 5.2 | |||
| Living arrangements | ||||||
| Living alone | 6.3 | <.05 | 7.0 | 8.7 | ||
| Other | 93.7 | 93.0 | 91.3 | |||
| Place of residence | ||||||
| Urban | 76.9 | <.001 | 24.9 | <.001 | 18.7 | |
| Rural | 23.1 | 75.1 | 81.3 | |||
| Education | ||||||
| No school | 46.0 | <.05 | 48.2 | <.01 | 42.9 | |
| Primary | 18.2 | 18.9 | 19.4 | |||
| Secondary | 21.8 | 18.4 | 27.4 | |||
| High school+ | 14.0 | 14.5 | 10.3 | |||
| Household wealth | ||||||
| First quintile | 22.5 | 24.0 | 25.0 | |||
| Second quintile | 18.6 | 19.2 | 15.1 | |||
| Third quintile | 19.4 | 19.6 | 17.1 | |||
| Fourth quintile | 18.3 | 17.2 | 19.4 | |||
| Fifth quintile | 21.2 | 20.0 | 23.4 | |||
| Health insurance | ||||||
| No | 99.1 | <.05 | 98.9 | 100 | <.05 | |
| Yes | 0.9 | 1.1 | 0.0 | |||
| ADLs | ||||||
| No ADL | 17.9 | <.05 | 18.9 | <.01 | 11.5 | <.001 |
| 1-2 ADLs | 20.5 | 18.1 | 24.6 | |||
| 3-4 ADLs | 22.1 | 23.6 | 21.4 | |||
| 5+ ADLs | 39.5 | 39.4 | 42.5 | |||
| Chronic diseases | ||||||
| No disease | 5.6 | <.001 | 5.1 | <.001 | 5.6 | <.001 |
| 1 disease | 14.3 | 14.3 | 14.7 | |||
| 2 diseases | 20.1 | 19.6 | 19.8 | |||
| 3-4 diseases | 34.1 | 33.7 | 32.1 | |||
| 5+ diseases | 25.9 | 27.3 | 27.8 | |||
| Community support | ||||||
| No | 38 | <.001 | 39.6 | <.001 | 35.3 | <.05 |
| Yes | 62 | 60.4 | 64.7 | |||
| Children support | ||||||
| No | 11.9 | 12.6 | 9.9 | |||
| Yes | 88.1 | 87.4 | 90.1 | |||
Source. Own calculations, using data from VNAS 2022.
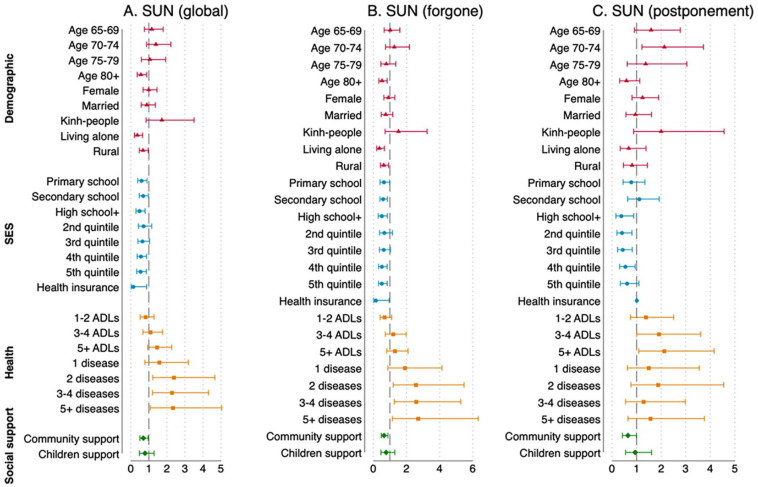
Multiple Regression Results
Figure 2 presents odds ratios (ORs) with 95% confidence intervals for the 3 types of SUN, highlighting factors associated with the likelihood of experiencing each type of SUN. The detailed numerical estimates are provided in Appendix Table A1.
Figure 2.
Determinants of experiencing subjective unmet need (SUN), presented as odds ratios and associated 95% confidence intervals (CI).
Source. Own calculations, using data from VNAS 2022.
Note. 95% CI are represented by 2 vertical bars and ORs are represented as rectangular, circle, square, and diamond markers within these bars.
In order to facilitate interpretation, results are reported by groups of independent variables. Among demographic characteristics, the oldest old had significantly lower odds of experiencing global and forgone SUN (54% and 52% reduction, respectively) compared to the youngest old (those aged 60-64 years), while those aged 70 to 74 were 2.1 times more likely to experience postponed SUN, ceteris paribus. Individuals living alone or residing in rural areas had lower odds of experiencing global and forgone SUN (63% and 32% reduction, respectively) compared to their counterparts.
Regarding socioeconomic status (SES), a consistent pattern emerged: having higher educational attainment, living in wealthier households, and having health insurance were associated with lower probabilities of experiencing all types of SUN.
In terms of health conditions, individuals with 1-2, 3-4, or 5+ chronic diseases had 2.3 to 2.7 times higher odds of experiencing global and forgone SUN compared to those without chronic diseases, ceteris paribus. Interestingly, ADLs were only significantly associated with postponed SUN: individuals with 3 or more ADLs had 1.9 to 2.1 times higher odds compared to those with no ADLs.
Finally, social support played a significantly protective role, that is, receiving community support was associated with a 30% decrease in the odds of experiencing any type of SUN.
Mediating Role of Social Support on the Association Between Experiencing SUN and Chronic Diseases
Given that only community support was consistently associated with all types of SUN, we explored whether it moderated the relationship between SUN and chronic disease categories. We introduced an interaction term between community support and chronic disease categories into the multiple logistic regression models. As the focus was on the interaction effect, and since the magnitudes and significance of other variables remained relatively stable compared to models without interaction, only the interaction term results are reported in Table 2.
Table 2.
Mediating Effects of Community Support, Reported as Odds Ratios and 95% Confidence Intervals (CI).
| Global SUN | Forgone SUN | Postponed SUN | |
|---|---|---|---|
| Variables | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Community support* 1 disease | 0.145* [0.023, 0.905] | 0.167 [0.023, 1.224] | 0.138 [0.015, 1.251] |
| Community support* 2 diseases | 0.118* [0.020, 0.683] | 0.141* [0.022, 0.909] | 0.137 [0.015, 1.278] |
| Community support* 3-4 diseases | 0.279 [0.054, 1.436] | 0.345 [0.059, 2.137] | 0.850 [0.113, 2.393] |
| Community support* 5+ diseases | 0.241 [0.043, 1.347] | 0.429 [0.068, 2.713] | 0.307 [0.040, 2.346] |
| Observations | 2.140 | 2.140 | 2.094 a |
Source. Own calculations, using data from VNAS 2022.
Note. 95% confidence intervals are reported in square brackets.
Forty-six observations were dropped due to zero observation in having health insurance.
indicates P < .05.
In general, the results indicate that community support was consistently associated with lower odds of experiencing any type of SUN across chronic disease categories. However, a significant interaction effect was only observed for those with 1 or 2 chronic diseases experiencing global SUN, and for those with 2 chronic diseases experiencing forgone SUN. More specifically, among those with 1 chronic disease, the community support receivers had 0.145 lower odds of experiencing global SUN than the non-receivers. Regarding individuals with 2 diseases, the community support receivers had 0.118 and 0.141 lower odds of reporting global SUN and forgone SUN than the non-receivers, respectively.
Discussion
Utilizing the latest nationally representative survey on older people, we contributed to the limited empirical evidence on factors influencing SUN during the COVID-19 in Vietnam as a middle-income country. We further highlighted the vital role of social support in mediating the relationship between experiencing SUN and chronic diseases in older persons. This topic has been largely unexplored in the literature. Our findings indicated that about one-fourth of Vietnamese older persons experienced SUN during the COVID-19. More particularly, 21.2% were forwent medical treatments, 11.8% experienced postponed services, and 2.4% were denied care. These figures were slightly lower than those reported in Bangladesh and some European countries.17,18,24
Concerning demographic determinants, we found that higher age was significantly associated with the likelihood of experiencing SUN, although this result was found only for the oldest old. The association between age and SUN during the COVID-19 was not consensus, for example, studies in Canada and Europe found that higher age had a protective effect against SUN,16,18,19 while null effect of such a relationship was found in Korea. 49 Older people living alone were associated with a higher likelihood of SUN than their counterparts living with others, and this finding could be explained by the following 3 combined factors: (i) living alone at old age presents socioeconomic disadvantages and increases risks for physical and mental health across countries,50 -52 and the case of Vietnam showed older people living alone had a higher probability of experiencing chronic diseases, loneliness, and depression53,54; (ii) living alone is significantly associated with increased healthcare utilization15,55,56; and (iii) living alone during the COVID-19 could be exacerbated older persons’ situations since governments applied various preventive measures such as social distancing, knockdown, or curfews.
Regarding SES determinants of SUN, higher educated and wealthier older persons were found to be less likely to experience SUN. This finding was consistent with studies in other countries,57 -59 and Vietnam as well.44,60 Individuals with higher education tend to have better knowledge, resources, and ability in accessing and processing information, which in turn might lower the likelihood of experiencing SUN during COVID-19. The results on these relationships in developed countries were inconsistent, possibly due to variation in study designs in terms of sampling selections and social contexts (ie, education systems and policies during COVID-19).18,19,49
Financial protection for healthcare is generally an important scheme to achieving universal health coverage, especially for older people whose healthcare demand is high. Vietnam is no exception. GOV has made significant efforts in establishing several health insurance schemes to improve financial protection for its older citizens. 28 A national survey on the Vietnamese older persons in 2019 showed that approximately 94% of older people having health insurance cards. 24 During a stressful time like COVID-19, having a health insurance card might provide a sense of security and reduce anxiety related to potential medical expenses, which is in line with the buffering pathway in mitigating SUN as discussed above. Another possible explanation is that medical expenses have been a major reason for delayed medical care among older people whose income tends to decrease at older ages, and as such Vietnamese older persons with health insurance might be less likely to postpone seeking treatments because health insurance could protect them against unanticipated and out-of-pocket expenses. To support this, previous studies showed a significant relationship between health insurance and healthcare utilization and emphasized the role of health insurance in mitigating financial burden among Vietnamese older people.61,62
Since presence of diseases are strongly associated with healthcare utilization among Vietnamese older people,63,64 it was not surprising in this study that chronic diseases were significant predictors of SUN. This result was similar to those found in several studies on European countries.18,19
Finally, we found that social support, particularly community support, significantly mediated the relationship between chronic diseases and experiencing SUN among older persons. Social support is known to be a crucial protective factor for healthy lifestyle, health and wellbeing among older people.22,65,66 This in turn benefits older people with chronic diseases.67 -70 Previous studies found that older people with better social support were less likely to experience chronic diseases and have less challenges in managing their chronic conditions.66,71,72 This evidence supports the buffering and main-effect mechanisms explaining how social support mitigates experiencing SUN.
Based on the above findings, we would suggest the following policies to mitigate unmet healthcare needs among older persons in Vietnam.
First, as more vulnerable older persons (such as those at more advanced age, with lower educational level, living alone, living in less wealthy households, and lack of healthcare insurance) were more likely to experience any type of SUN, they should be prioritized in any healthcare policies and programs so as to be accessible to affordable and adequate healthcare services.
Second, development of grassroot-level healthcare facilities, particularly at commune health centers (CHCs), along with a responsive family doctor system would help provide timely services to local people in general, and older persons in particular. This would help to reduce heavily overloaded services at higher technical level facilities (such as provincial and central hospitals). Various studies have shown that out-of-pocket (OOP) payments, particularly those for transportation, accommodation, and potential income losses for providing care assistance, would have been significantly reduced for those who get treatments at CHCs where some chronic diseases (such as diabetes and hypertension) can be managed.73,74 This would be also important to mitigate forgone, delayed or denied healthcare services for older persons in COVID-19-like situations.
Third, as community support played an important role in reducing unmet healthcare needs of older persons, further promoting socio-political organizations (such as Vietnam Association of the Elderly—VAE; Vietnam’s Women Union—VWU) at community level and encouraging older persons to actively participate in their social activities would be beneficial to older persons to understand their rights to healthcare. Also, community-based activities can supplement or complement family support systems to address the healthcare needs of older Vietnamese, especially during possible crises like COVID-19. A well-known community-based care model in Vietnam, namely Intergenerational Self-Help Club (ISHC), is an example of multi-tasking community support to boost older persons’ health and well-being. 75 These clubs across provinces played important roles in helping older persons in needs for healthcare, social care and income security during the COVID-19. 76
Last, but not least, along with a rapidly aging population, raising awareness and implementing educational programs on chronic diseases (such as changing bad health-related behaviors and practicing good lifestyles) for younger generations would bring a long-term benefit to Vietnam with a healthier population in the coming decades.
Conclusion
This study could provide novel evidence on the mechanisms through which social support potentially mitigated the relationship between experiencing SUN and chronic diseases during COVID-19. We found that the risk factors of SUN included more advanced age, living alone, lack of healthcare insurance, and chronic diseases, while the protective factors included higher education, better wealth, and stronger social support. We also found that social support, particularly from the community, significantly moderated the link between SUN and chronic diseases.
We acknowledge some limitations of this study. Firstly, as the study’s design focused on identifying determinants of SUN and the mediating role of social support, it could not establish causal relationships. Secondly, the cross-sectional nature of the study limits our ability to control for macro-level factors that could have influenced SUN during the COVID-19 pandemic, such as the number of hospitals with geriatric departments, the availability of physicians, public healthcare spending, specific preventive measures, and mortality rates. Future research would benefit from incorporating these macro variables, as existing literature suggests their potential impact on SUN.18,19 Finally, we acknowledge the possibility of reporting bias during the pandemic.
Acknowledgments
We would like to thank the Asian Development Bank (ADB) and the Institute of Social and Medical Studies (ISMS) for permitting us to use the data. The authors also would like to thank Dr. Sakiko Tanaka and Dr. Aiko Kikkawa (ADB) for their insighful and useful comments and suggestions on various drafts of this study.
Appendix
Table A1.
Determinants of Experiencing Subjective Unmet Need (SUN), Reported as Odds Ratios and 95% Confidence Intervals (CI).
| Global SUN | Forgone SUN | Postponed SUN | |
|---|---|---|---|
| Variables | OR [95% CI] | OR [95% CI] | OR [95% CI] |
| Age 65-69 | 1.162 [0.751, 1.796] | 1.019 [0.651, 1.597] | 1.589 [0.909, 2.779] |
| Age 70-74 | 1.394 [0.874, 2.223] | 1.266 [0.737, 2.176] | 2.129** [1.217, 3.722] |
| Age 75-79 | 1.061 [0.584, 1.929] | 0.782 [0.452, 1.354] | 1.369 [0.616, 3.046] |
| Age 80+ | 0.560* [0.355, 0.883] | 0.525** [0.331, 0.832] | 0.589 [0.308, 1.128] |
| Female | 0.994 [0.680, 1.454] | 0.908 [0.633, 1.302] | 1.241 [0.814, 1.894] |
| Married | 0.888 [0.579, 1.363] | 0.745 [0.472, 1.176] | 0.952 [0.564, 1.606] |
| Kinh-people | 1.722 [0.846, 3.507] | 1.516 [0.708, 3.244] | 1.999 [0.876, 4.564] |
| Living alone | 0.362*** [0.202, 0.649] | 0.366** [0.201, 0.666] | 0.678 [0.332, 1.385] |
| Rural areas | 0.674* [0.470, 0.966] | 0.628* [0.430, 0.918] | 0.815 [0.462, 1.438] |
| Primary school | 0.586* [0.380, 0.902] | 0.629* [0.401, 0.986] | 0.774 [0.449, 1.337] |
| Secondary school | 0.678* [0.468, 0.983] | 0.581** [0.397, 0.851] | 1.103 [0.633, 1.921] |
| High school+ | 0.476** [0.285, 0.793] | 0.501* [0.294, 0.852] | 0.370* [0.155, 0.881] |
| Second quintile | 0.699 [0.421, 1.159] | 0.655 [0.373, 1.149] | 0.398* [0.196, 0.809] |
| Third quintile | 0.637 [0.389, 1.042] | 0.616 [0.368, 1.032] | 0.429* [0.224, 0.823] |
| Fourth quintile | 0.554* [0.350, 0.876] | 0.504** [0.305, 0.833] | 0.537* [0.308, 0.938] |
| Fifth quintile | 0.531* [0.326, 0.863] | 0.503** [0.302, 0.838] | 0.605 [0.336, 1.091] |
| Health insurance | 0.134* [0.020, 0.882] | 0.146* [0.022, 0.962] | - a |
| 1-2 ADLs | 0.817 [0.517, 1.289] | 0.668 [0.403, 1.106] | 1.373 [0.751, 2.510] |
| 3-4 ADLs | 1.084 [0.667, 1.761] | 1.195 [0.721, 1.980] | 1.902* [1.001, 3.612] |
| 5+ ADLs | 1.448 [0.927, 2.260] | 1.297 [0.803, 2.093] | 2.122* [1.083, 4.157] |
| 1 disease | 1.577 [0.780, 3.188] | 1.897 [0.870, 4.136] | 1.490 [0.625, 3.552] |
| 2 diseases | 2.384* [1.220, 4.656] | 2.562* [1.199, 5.473] | 1.871 [0.769, 4.551] |
| 3-4 diseases | 2.274* [1.200, 4.310] | 2.585** [1.266, 5.276] | 1.279 [0.549, 2.981] |
| 5+ diseases | 2.330* [1.079, 5.034] | 2.694* [1.147, 6.328] | 1.559 [0.646, 3.764] |
| Community support | 0.695* [0.503, 0.961] | 0.646** [0.043, 0.882] | 0.647* [0.421, 0.995] |
| Children support | 0.787 [0.479, 1.292] | 0.771 [0.458, 1.298] | 0.941 [0.550, 1.609] |
Source. Own calculations, using data from VNAS 2022.
Note. 95% confidence intervals are reported in square brackets.
Unable to estimate due to zero observation in having health insurance.
, **, and *** indicate P < .05, P < .01, P < .001.
Footnotes
Author Contribution Statement: The study’s concept and design were performed by Long Thanh Giang and Thu Dai Bui. Material preparations, data processes and analyses were performed by Dung Duc Le, Van Thi Truong and Anh Lan To, and verified by Long Thanh Giang. The first draft was written by Long Thanh Giang and Dung Duc Le, and commented by Thu Dai Bui, Van Thi Truong, and Anh Lan To. Drafts were revised by Long Thanh Giang. The final manuscript was read and approved by all authors before submission. The revised manuscript along with comments from the referees were done by Long Thanh Giang and Dung Duc Le, and all authors agreed to resubmit the revised version.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Asian Development Bank (ADB) through the TA 6767-REG “Supporting Enhanced COVID-19 Vaccination and Post-COVID-19 Health Security Response in Southeast Asia.”
Ethical/consent Statement: Our study did not require an ethical board approval because we used the secondary data, which was ethically approved.
ORCID iD: Long Thanh Giang  https://orcid.org/0000-0002-6296-0563
https://orcid.org/0000-0002-6296-0563
References
- 1. Ginneken E, Siciliani L, Reed S, Eriksen A, Tille F, Zapata T. Addressing backlogs and managing waiting lists during and beyond the COVID-19 pandemic. Eurohealth. 2022;28(1):35-40. [PubMed] [Google Scholar]
- 2. Mafham MM, Spata E, Goldacre R, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fekadu G, Bekele F, Tolossa T, et al. Impact of COVID-19 pandemic on chronic diseases care follow-up and current perspectives in low resource settings: a narrative review. Int J Physiol Pathophysiol Pharmacol. 2021;13(3):86. [PMC free article] [PubMed] [Google Scholar]
- 4. Schmidt AE, Rodrigues R, Simmons C, Steiber N. A crisis like no other? Unmet needs in healthcare during the first wave of the COVID-19 crisis in Austria. Eur J Public Health. 2022;32(6):969-975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022;20(3):1537-1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Allain-Dupré D, Chatry I, Michalun V, Moisio A. The territorial impact of COVID-19: managing the crisis across levels of government. OECD Policy Responses Coronavirus (COVID-19). 2020;10:1620846020-909698535. [Google Scholar]
- 7. Gibson G, Grignon M, Hurley J, Wang L. Here comes the SUN: self-assessed unmet need, worsening health outcomes, and health care inequity. Health Econ. 2019;28(6):727-735. [DOI] [PubMed] [Google Scholar]
- 8. Quesnel-Vallée A, Willson A, Reiter-Campeau S. Health inequalities among older adults in developed countries: reconciling theories and policy approaches. In: George L, Ferraro K, eds. Handbook of Aging and the Social Sciences. Elsevier; 2016:483-502. [Google Scholar]
- 9. Brown E, Gray R, Monaco SL, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. 2020;222:79-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhao Q, Meng M, Kumar R, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J Med Virol. 2020;92(10):1915-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Porcheddu R, Serra C, Kelvin D, Kelvin N, Rubino S. Similarity in case fatality rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020;14(2):125-128. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization (WHO). Older people & COVID-19. 2024. Accessed March 23, 2024. https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/covid-19
- 13. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70(3):465-472. [DOI] [PubMed] [Google Scholar]
- 15. González-Touya M, Stoyanova A, Urbanos-Garrido RM. COVID-19 and unmet healthcare needs of older people: did inequity arise in Europe? Int J Environ Res Public Health. 2021;18(17):9177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khattar J, Griffith LE, Jones A, et al. Symptoms of depression and anxiety, and unmet healthcare needs in adults during the COVID-19 pandemic: a cross-sectional study from the Canadian Longitudinal Study on Aging. BMC Public Health. 2022;22(1):2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Quintal C, Moura Ramos L, Antunes M, Lourenço Ó. Unmet healthcare needs among the population aged 50+ and their association with health outcomes during the COVID-19 pandemic. Eur J Ageing. 2023;20(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smolić Š, Čipin I, Međimurec P. Access to healthcare for people aged 50+ in Europe during the COVID-19 outbreak. Eur J Ageing. 2022;19(4):793-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tavares AI. Older Europeans’ experience of unmet health care during the COVID-19 pandemic (first wave). BMC Health Serv Res. 2022;22(1):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310. [PubMed] [Google Scholar]
- 21. Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):P25-P32. [DOI] [PubMed] [Google Scholar]
- 22. Newsom JT, Schulz R. Social support as a mediator in the relation between functional status and quality of life in older adults. Psychol Aging. 1996;11(1):34. [DOI] [PubMed] [Google Scholar]
- 23. Baiden P, Den Dunnen W, Fallon B. Examining the independent effect of social support on unmet mental healthcare needs among Canadians: findings from a population-based study. Soc Indic Res. 2017;130:1229-1246. [Google Scholar]
- 24. Ministry of Health VM, Asian Development Bank (ADB), Japan Fund for Poverty Reduction (JFPR), and Institute of Social and Medical Studies (ISMS). Survey on Older Person and Social Health Insurance 2019: Key findings. 2021. Ministry of Health: Hanoi: (unpublished). [Google Scholar]
- 25. General Statistics Office, Vietnam (GSO). The Population and Housing Census 2019: Key Findings. Statistical Publishing House; 2020. [Google Scholar]
- 26. Vietnam National Assembly. The Law on the Elderly (in Vietnamese). 2009. Accessed March 23, 2024. https://vanban.chinhphu.vn/default.aspx?pageid=27160&docid=92321 [Google Scholar]
- 27. UNFPA. Income security for older persons in Viet Nam: Social Pensions. 2014. Accessed March 23, 2024. https://vietnam.unfpa.org/en/publications/income-security-older-persons-viet-nam-social-pensions [Google Scholar]
- 28. Ministry of Health, Vietnam & Health Partnership Group. Joint Annual Health Review 2016: Towards Healthy Aging in Vietnam. Medical Publishing House; 2018. [Google Scholar]
- 29. Hoang VM. The COVID-19 pandemic in Vietnam–success, crisis, and endemic: key thresholds and lessons. J Glob Health. 2022;12:03065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Worldometer. Coronavirus in Vietnam. 2024. Accessed March 23, 2024. https://www.worldometers.info/coronavirus/country/viet-nam/#google_vignette
- 31. Ministry of Health. Bộ Y tế: Số mắc, tử vong do COVID-19 liên tục giảm tại TP HCM và nhiều tỉnh (in Vietnamese). 2021. Accessed March 23, 2024. https://moh.gov.vn/tin-noi-bat/-/asset_publisher/3Yst7YhbkA5j/content/bo-y-te-so-mac-tu-vong-do-covid-19-lien-tuc-giam-tai-tp-hcm-va-nhieu-tinh
- 32. UNDP VietNam. Rapid Assessment of the Socio-Economic Impact of COVID-19 on Persons with Disabilities in Vietnam. United Nations Development Programme; 2020. [Google Scholar]
- 33. Kahn RL. Conboys over the life course: attachment roles and social support. Life Span Dev Behav. 1980;3:253-286. [Google Scholar]
- 34. Andrews G, Tennant C, Hewson DM, Vaillant GE. Life event stress, social support, coping style, and risk of psychological impairment. J Nerv Ment Dis. 1978;166(5):307-316. [DOI] [PubMed] [Google Scholar]
- 35. Maan Diong S, Bishop GD, Enkelmann HC, et al. Anger, stress, coping, social support and health: modelling the relationships. Psychol Health. 2005;20(4):467-495. [Google Scholar]
- 36. Bai Y, Bian F, Zhang L, Cao Y. The impact of social support on the health of the rural elderly in China. Int J Environ Res Public Health. 2020;17(6):2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kendler KS, Myers J, Prescott CA. Sex differences in the relationship between social support and risk for major depression: a longitudinal study of opposite-sex twin pairs. Am J Psychiatry. 2005;162(2):250-256. [DOI] [PubMed] [Google Scholar]
- 38. Thanakwang K, Soonthorndhada K. Mechanisms by which social support networks influence healthy aging among Thai community-dwelling elderly. J Aging Health. 2011;23(8):1352-1378. [DOI] [PubMed] [Google Scholar]
- 39. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145-161. [DOI] [PubMed] [Google Scholar]
- 40. Distelberg B, Taylor S. The roles of social support and family resilience in accessing healthcare and employment resources among families living in traditional public housing communities. Child Fam Soc Work. 2015;20(4):494-506. [Google Scholar]
- 41. Lin C, Li L, Ji G, Jie W. Emotional social support and access to care among older people living with HIV in rural China. Int J Geriatr Psychiatry. 2015;30(10):1041-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21(6):459-468. [DOI] [PubMed] [Google Scholar]
- 43. Wagstaff A, O’Donnell O, Van Doorslaer E, Lindelow M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation. World Bank Publications; 2007. [Google Scholar]
- 44. Le DD, Leon-Gonzalez R, Giang LT. Decomposing gender inequality in functional disability among older people in Vietnam. Arch Gerontol Geriatr. 2020;87:103989. doi: 10.1016/j.archger.2019.103989 [DOI] [PubMed] [Google Scholar]
- 45. Quashie NT, Pothisiri W. Rural-urban gaps in health care utilization among older Thais: the role of family support. Arch Gerontol Geriatr. 2019;81:201-208. [DOI] [PubMed] [Google Scholar]
- 46. Deb P, Norton EC, Manning WG. Health Econometrics Using Stata. Vol. 3. Stata Press; 2017. [Google Scholar]
- 47. Pregibon D. Goodness of link tests for generalized linear models. J R Stat Soc Ser C Appl Stat. 1980;29(1):15-24. [Google Scholar]
- 48. O’brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007;41(5):673-690. doi: 10.1007/s11135-006-9018-6 [DOI] [Google Scholar]
- 49. Kim S, Hwang J. What are the factors affecting older adults’ experience of unmet healthcare needs amid the COVID-19 pandemic in Korea? BMC Geriatr. 2023;23(1):517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kharicha K, Iliffe S, Harari D, Swift C, Gillmann G, Stuck AE. Health risk appraisal in older people 1: are older people living alone an ‘at-risk’ group? Br J Gen Pract. 2007;57(537):271-276. [PMC free article] [PubMed] [Google Scholar]
- 51. Moncatar TR, Nakamura K, Rahman M, Seino K. Health status and health facility utilization of community-dwelling elderly living alone in the Philippines: a nationwide cross-sectional study. Health. 2019;11(11):1554. [Google Scholar]
- 52. Ng KM, Lee TM, Chi I. Relationship between living arrangements and the psychological well-being of older people in Hong Kong. Australas J Ageing. 2004;23(4):167-171. [Google Scholar]
- 53. Giang L, Nguyen TT, Thi Tran N. Factors associated with depression among older people in Vietnam. J Popul Soc Stud. 2019; 27(2): 181-194. [Google Scholar]
- 54. Vo MTH, Nakamura K, Seino K, Vo TV. Greater risk of negative health outcomes of older adults living alone in Vietnam: a community survey. Int J Environ Res Public Health. 2021;18(21):11115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mu C, Kecmanovic M, Hall J. Does living alone confer a higher risk of hospitalisation? Econ Rec. 2015;91:124-138. [Google Scholar]
- 56. Turner AJ, Nikolova S, Sutton M. The effect of living alone on the costs and benefits of surgery amongst older people. Soc Sci Med. 2016;150:95-103. [DOI] [PubMed] [Google Scholar]
- 57. Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(suppl 2):19-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Semyonov M, Lewin-Epstein N, Maskileyson D. Where wealth matters more for health: the wealth–health gradient in 16 countries. Soc Sci Med. 2013;81:10-17. [DOI] [PubMed] [Google Scholar]
- 59. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39(1):273-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Giang LT, Van Duong D, Kim YJ. Factors associated with perceived health status of the Vietnamese older people. Popul Ageing. 2019;12(1):95-108. [Google Scholar]
- 61. Giang LT, Pham THT, Phi PM, Nguyen NT. Healthcare services utilisation and financial burden among Vietnamese older people and their households. Int J Environ Res Public Health. 2023;20(12):6097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Le DD, Leon-Gonzalez R, Giang TL, Nguyen AT. Socio-economic-related health inequality in non-communicable diseases among older people in Viet Nam. Ageing Soc. 2021;41(6):1421-1448. [Google Scholar]
- 63. Nguyen TA, Giang LT. Factors influencing the Vietnamese older persons in choosing healthcare facilities. Health Serv Insights. 2021;14:11786329211017426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Van Minh H, Oh J, Giang KB, et al. Health service utilization among people with noncommunicable diseases in rural Vietnam. J Public Health Manag Pract. 2018;24:S60-S66. [DOI] [PubMed] [Google Scholar]
- 65. Ashida S, Heaney CA. Differential associations of social support and social connectedness with structural features of social networks and the health status of older adults. J Aging Health. 2008;20(7):872-893. [DOI] [PubMed] [Google Scholar]
- 66. Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29:377-387. [DOI] [PubMed] [Google Scholar]
- 67. Feller S, Teucher B, Kaaks R, Boeing H, Vigl M. Life satisfaction and risk of chronic diseases in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS One. 2013;8(8):e73462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Le D, Giang T. Gender differences in prevalence and associated factors of multi-morbidity among older persons in Vietnam. Int J Ageing Dev Ctries. 2016;1(2):113-132. [Google Scholar]
- 69. Le DD, Quashie NT, Prachuabmoh V. How does self-rated health differ among older Vietnamese men and women? Popul Ageing. 2019;12(1):69-93. [Google Scholar]
- 70. Somrongthong R, Hongthong D, Wongchalee S, Wongtongkam N. The influence of chronic illness and lifestyle behaviors on quality of life among older Thais. Biomed Res Int. 2016;2016(1):2525941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143(6):427-438. [DOI] [PubMed] [Google Scholar]
- 72. Clark NM, Becker MH, Janz NK, Lorig K, Rakowski W, Anderson L. Self-management of chronic disease by older adults: a review and questions for research. J Aging Health. 1991;3(1):3-27. [Google Scholar]
- 73. Giang TL, Bui DT. Health insurance reform and support to the poor in HEMA provinces (unpublished project evaluation report). ‘Health Care Support to the Poor of the Northern Uplands and Central Highlands’ (HEMA); 2013.
- 74. Giang TL, Bui DT, Truong TV, To LA. Impact evaluation of free access on Social Health Insurance (SHI) health services at District level (unpublished project evaluation report). Social Health Insurance Project (SHIP); 2020.
- 75. Giang TL, Chu VN, Tran BT. The roles of local governments in protecting rights of older people: the case of intergenerational self-help clubs in Vietnam. Local Administration J. 2020;13(3):235-248. [Google Scholar]
- 76. United Nations Population Fund (UNFPA) & HelpAge International (HAI). The impact of COVID-19 on older persons: Vietnam analytical brief. 2020. Accessed February 20, 2024. https://ageingasia.org/wp-content/uploads/2020/10/Vietnam-Analytical-Brief-September-2020.pdf [Google Scholar]