Abstract
Introduction
Sickle cell disease (SCD) is one of the most common genetic diseases in the world, annually affecting approximately 310 000 births and causing >100 000 deaths. Vaso-occlusive crisis (VOC) is the most frequent complication of SCD, leading to bone pain, thoracic pain (acute chest syndrome) and/or abdominal spasms. It is the main cause of mortality in patients with SCD, reducing life expectancy. Hyperbaric oxygen therapy (HBOT) is a safe and well-established method of increasing tissue oxygen delivery immediately by up to 10-fold to 20-fold. In the context of VOC, HBOT has the potential to limit sickling. A previous pilot study of nine patients showed the safety and potential benefits of HBOT on VOC-induced pain. Our study aimed to assess the clinical safety and effectiveness of HBOT for treating VOC, its biological mechanisms of actions and its cost-effectiveness.
Methods and analysis
This is a multicentric, triple-blinded, randomised controlled trial. Patients aged 8 years or above with a diagnosed major form of SCD, presenting at one of the participating centres’ emergency departments (EDs) with a VOC requiring level 3 analgesia (according to WHO definition), will be eligible. Exclusion criteria are pregnancy, mechanical ventilation, previous history of stroke or prior transcranial Doppler ultrasound anomaly, contraindication to HBOT and the need for above 2 L/min of oxygen. All patients will receive the usual care for VOCs, including hydration, analgesics, normobaric oxygen therapy and when medically indicated, antibiotic therapy and/or transfusions. Within 24 hours of their arrival in the ED (or longer in specific cases), and after obtaining informed consent, patients will be randomised into the HBOT intervention group (2.0 atmosphere absolute (ATA), 90 min, FIO2=1) or the sham group (1.3 ATA, 90 min, FIO2=0.21). After their first HBOT session, patients will return to their acute-care ward. Patients in both arms will undergo a second and third session within 24–36 hours of the first, unless their Visual Analogue Scale (VAS)-pain is ≤2 without use of level 3 analgesics. The difference in the pain-VAS before and after HBOT and other outcomes will be compared between the intervention and sham groups. Our composite primary outcome will be (1) the change in global VAS-pain 6 hours after initiation of HBOT; (2) the number of patients with a VAS-pain score >4 and/or a morphine dosage >1 mg/hour intravenous after the HBOT/sham session. Other outcomes to be reported are morphine usage, length of stay, biological parameters, satisfaction, complications and cost.
Ethics and dissemination
Ethical approval CER Geneva 2019-01707 (last submission V.5.1, 06.15.2023). The results of the studies will be disseminated by several media, including publications in peer-reviewed international medical journals, and presentations at national and/or international conferences.
Trial registration number
Keywords: Emergency Service, Hospital; Anaemia; INTERNAL MEDICINE
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Direct comparison of hyperbaric oxygen therapy to a control in sickle cell disease vaso-occlusive crisis in a randomised trial.
Use of a validated sham treatment.
Triple blinding to avoid any bias.
Multidisciplinary involvement in the study.
Logistically complex study to operationalise.
Introduction
Sickle cell disease (SCD) is the most frequent autosomal recessive disease, resulting in the production of sickle haemoglobin (HbS). Severe forms of SCD include haemoglobin SS resulting from the inheritance of HbS, Sβ0-thalassaemias due to co-inheritance of HbS with the β0-thalassemia mutation or other forms of co-inheritance of HbS with other β-globin gene mutation such as haemoglobin C (SC form) or β+-thalassaemias (Sβ+). Vaso-occlusive crisis (VOC) is the most common complication of SCD with an annual incidence of approximately 60% in adult sufferers. VOC usually causes bone, chest and/or abdominal pain and is a leading cause of death in patients with SCD.1 Acute chest syndrome (ACS) is a specific clinical presentation of VOC that is caused by pulmonary capillary occlusion and is defined by a triad of symptoms (chest pain, fever and radiological infiltration).2 It remains a major cause of hospitalisation and SCD-related mortality. Due to accompanying acute complications (such as VOC and ACS), with or without infections and chronic complications (such as stroke, pulmonary hypertension, chronic lung disease or nephropathy), SCD is associated with a reduced life expectancy and a median age of death of 43 years (IQR 31.5–55 years).3
Physiopathology of SCD
Hypoxia, acidosis, infection, dehydration or exposure to cold can trigger VOC/ACS by facilitating falciformation, due to HbS polymerisation. This leads to acute vaso-occlusion and haemolysis-mediated endothelial dysfunction,2 4 inflammation and, ultimately, to vascular damage and tissue hypoxia with multiorgan injury.5 6 Other cellular mechanisms involved in VOC/ACS are adherence of sickle cells to the vascular endothelium, involving intercellular adhesion molecules such as ICAM-1, VCAM-1, PAF and CD 367,10; erythrocyte-leucocyte-platelet endothelium interactions11 with leucocytes12 and platelet activation13; an increase in the number of circulating leucocytes14 and formation of reactive oxygen forms (reactive oxygen species) which cause major endothelial dysfunction.15 Intravascular haemolysis and cell adhesion promote both vasculopathy and vaso-occlusion,16,18 as well as inflammation.19 Mitochondrial dysfunction is an additional element of this vicious cycle, promoting platelet activation and the release of inflammation activators.20
Usual care
Home-based management of a VOC is usually based on WHO classification level 1 and 2 analgesics (1: non-steroidal anti-inflammatory drugs or acetaminophen; 2: codeine, tramadol). When VOC management is impossible with these analgesics, WHO classified level 3 analgesics are introduced (3: morphine or its derivatives, eg, fentanyl, oxycodone, buprenorphine or hydromorphone). Other VOC management is symptom appropriate and includes adapted hydration, local warming, oxygen therapy, folate administration and antibiotic therapy. When these management strategies prove insufficient, or, in the presence of severe ACS,21 22 ischaemic stroke, recurrent severe infection or side effects that limit the use of morphine, erythrapheresis and transfusions can be used. Alloimmunisation remains an extremely frequent consequence of the use of erythrocyte transfusion which, consequently, excludes the possibility of further transfusions or exchange transfusions as a therapeutic option in certain patients. Some patients become impossible to transfuse and HBOT is then an ultimate treatment offered in case of VOC. The recent availability of L-glutamine, crizanlizumab and voxelotor provides an alternative or additional alternative to hydroxyurea, which remains the first choice for disease-modifying therapy.3
Overall survival rates remain high for individuals with SCD who have undergone allogeneic hematopoietic stem cell transplantation using matched sibling donors. Newer approaches to graft-versus-host (GVHD) prophylaxis and the incorporation of post-transplant cyclophosphamide have improved engraftment rates, reduced GVHD and have allowed for alternative donors for individuals in the absence of a HLA-matched sibling. Despite progress in this field, the increase in world SCD prevalence means management of VOCs remains a real and persistent problem, requiring the identification of alternative treatments outside of opioid and transfusion therapy.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy (HBOT) is a long-established technique with several recognised indications, including carbon monoxide poisoning and anaerobic soft tissue infection.23 HBOT consists of intermittent periods of breathing 100% oxygen at a pressure above that of sea level. The increase in pressure produced in the compression chamber significantly increases the partial pressure of the inspired gases in the blood and peripheral tissues,24 reducing ischaemia, and as a consequence, reducing/reversing sickling. HBOT allows the enhanced oxygenation of tissues where blood circulation is deficient, meaning oxygen no longer needs the support of erythrocytes to circulate and to be diffused.
In practice, the pressure increase is achieved by introducing compressed air into the hyperbaric chamber. Changes in ambient pressure modify the volume that the gas occupies, including in the body (eg, ear cavities, sinuses). In the hyperbaric chamber, when at the targeted pressure (outside of compression, decompression phases and during air breaks), patients breathe 100% oxygen through a specifically adapted mask or hood (if mask cannot be adjusted to patient morphology). A member of the HMU (Hyperbaric Medicine Unit) team monitors patients at all times during HBOT sessions. In a preliminary consultation prior to the first session, the treatment process and manoeuvres necessary to equalise pressure across tympanic membranes are explained. At the Geneva hospital, a multiplace hyperbaric chamber (HAUX, Germany) will be used. During sessions, the airlock system allows entry into or exit from the main chambers without any pressure change. A second airlock allows the passage of any small pieces of equipment required in the event of an emergency. When breathing 100% oxygen, there is no accumulation of nitrogen in the tissues, thus excluding the risk of decompression sickness.
To best simulate HBOT in the sham arm, our group has previously validated a procedure that will be employed in this study.25 Using the method described later, the study identified a pressure of 1.3 ATA, FIO2=0.21 as being most realistic in creating the illusion of HBOT in healthy volunteers. Its advantages are of being extremely low risk (equivalent of a pressure at 3 m of depth in water) and having an FIO2 equivalent of 0.27.25 With this approach, even if there is a slight positive effect from the minimal pressurisation, equivalent to breathing air with a FIO2 of 0.27 in the sham group, it is considered as not affecting overall results. When breathing air at 1.3 ATA, there is no accumulation of nitrogen in the tissues, thus excluding the risk of decompression sickness.
Adverse events of HBOT are extremely infrequent.26 27 In 99.3% of all HBOT sessions, no adverse events were recorded. The most frequently occurring event was ear/sinus barotrauma (0.37%), followed by claustrophobia (0.16%) and symptomatic hypoglycaemia (0.08%). More serious events, such as seizure (0.02%) or lung toxicity (0.01%), occurred very rarely. Only one instance of confirmed pulmonary barotrauma was identified out of 1.5 million treatments.27 To minimise the risk of middle ear/sinus barotrauma caused by difficulty with ear equalisation, resulting in a feeling of pressure, ear pain or discomfort, an ear examination will be carried out before the HBOT session. Patients will systematically be accompanied and ‘educated’ by HMU staff during their first compression (the initial phase of HBOT). The recognised presentation of central nervous system (CNS) oxygen toxicity during clinical hyperbaric oxygen treatment is an oxygen toxicity seizure (Paul Bert effect). Prodromal symptoms (twitching, staring gaze, auditory hallucinations, visual changes, nausea, vertigo, anxiety and irritability) have been reported, although they appear in <50% of cases of oxygen toxicity. Tonic–clonic seizure activity rapidly follows these signs. Other potential side effects include progressive myopia, headache, nausea, numbness or pulmonary dyspnoea.
Rationale for the study
In the early stages of VOC, the falciformation process is reversible if conditions, especially oxygenation, improve. HBOT is effective in increasing tissue oxygenation by increasing dissolved O2 in the blood and limiting local hypoxaemia, a promoter of falciformation. This is often sufficient to break the vicious cycle of VOC and ACS. HBOT demonstrated an improvement in microcirculatory vascular flow, a decrease in leucocyte adhesion and an increase in tissue ATP in a rodent liver model.28 HBOT may influence the NO synthetase and NO secretion, particularly in the CNS, leading to increase regional brain blood flow by vasodilation.29 It also downregulates cell adhesion proteins such as ICAM-1, VCAM-1, PAF and CD36.1830,32 Thus, HBOT could counterbalance the effects of VOC which induces an overexpression of adhesion phenomena and leads to NO deficiency.33 Several cases of complications related to SCD treated with HBOT have already been documented since 1966 in clinical cases or retrospective series with favourable outcomes reported for a number of patients.33,42 In hyperbaric medicine guidelines, SCD is a recognised indication for HBOT,19 with a low level of evidence (type C recommendations).23 The North American guidelines, however, did not include SCD as an indication.43 Our group published a pilot non-comparative study on nine patients with SCD, hospitalised for severe and resistant VOC, treated with HBOT (2.5 atmosphere absolute (ATA), 90 min, FIO2=1). We observed a significant decrease in mean Visual Analogue Scale (VAS) score after one HBOT session compared with the VAS evaluated before the session. For two patients, the HBOT session was interrupted due to minor ear barotrauma (otalgia) during compression, but no problems relating to tolerance were reported in the seven other patients.44
This study aimed to investigate the effect of HBOT in SCD-VOC in terms of efficacy on clinical outcomes (such as pain severity, analgesic consumption, duration of hospitalisation) and its safety.
Methods and analysis
Setting
The study will be conducted in three or more academic hospitals in Switzerland and France: The Geneva University Hospitals (Switzerland) have recruited 15 patients, as a pilot feasibility phase, between 30 September 2022 and 30 April 2024. We are currently identifying two other hospitals in France.
Study design
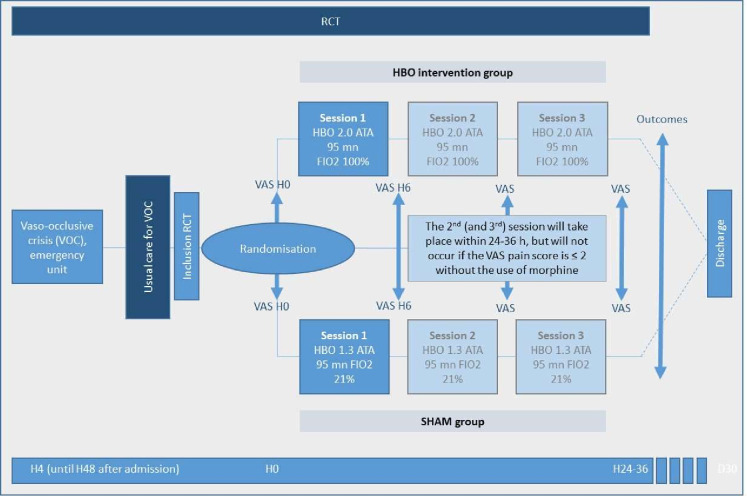
This is a superiority, triple-blinded (patient, clinician and research team), multicentric randomised controlled trial (RCT) comparing HBOT (intervention) superiority to a sham in the treatment of VOC in SCD (figure 1).
Figure 1. Schematic diagram of the randomised controlled trial (RCT). ATA, atmosphere absolute; VAS, Visual Analogue Scale; VOC, vaso-occlusive crisis.
All patients with VOC presenting at the ED will receive the current standard treatment according to the adult or paediatric protocols: hydration, normobaric oxygen therapy to maintain SpO2≥94%, analgesics (preferably intravenous morphine or derivatives via PCA pump (patient controlled analgesia)) and antibiotic therapy (when indicated). The baseline pain VAS will be evaluated by the patient on arrival and if the all the inclusion criteria are met without exclusion criteria, a hyperbaric physician will verify the absence of contraindications to HBOT. The screening will ideally take place in the ED, aiming at patient inclusion in the study within the first 4 hours of arrival where possible (or up to 24 hours or possibly more in specific cases).
After informed consent, a pain VAS and a Categorical Pain Score (CPS) will be evaluated by the patients immediately prior to their transfer to the HMU. There, the randomisation between the intervention arm (2.0 ATA, 90-minute session, FIO2 100%) and the sham arm (1.3 ATA, 90-minute session, FIO2 21%) will be carried out. Solely the HMU team will know in which study arm the patient has been randomised. The patient, treating physician and research team will be blinded to group allocation. All patients will receive the established standard of care, including PCA (if already in progress) during the HBOT sessions as per protocol. A HBOT session can be interrupted at any time in case of complications, and this would be documented in the source document and CRF.
Patient satisfaction and their impression of receiving the treatment or sham will be documented after the first session, using a questionnaire.
An additional Biobank will be collected from patients recruited at the Geneva University Hospitals only. For adult participants who consent to this substudy, venous blood samples will be taken immediately before and after the first HBOT session. A third blood sample will be taken at 24–36 hours post start time of the first HBOT session (depending on time 24-hour point falls). If the patient is discharged from hospital before H24, the third blood sample will be taken just before discharge.
A VAS pain score will be evaluated 4 hours after the end of the initial HBOT session by blinded staff in the ED/ward. As HMU staff know the allocated arm, they will not assess any of the patient outcomes to avoid bias. A second and third HBOT session will systematically be scheduled within 24–36 hours after the first session. Subsequent sessions will be consistent with the randomisation arm (sham or treatment). VAS pain scores will be evaluated immediately prior to and after the second and third sessions and again at 4 hours post session. These sessions will be cancelled if the patient’s VAS score ≤2 without morphine treatment. In this case, we can consider that the VOC is finished. The second/third session will be cancelled in both arms of the study if a patient’s condition deteriorates, meaning that they need >2 L/min O2 to maintain their SpO2>92%. Although the protocol will be interrupted for these patients, they will be integrated into the analysis in ‘intention to treat’.
If a transfusion or exchange transfusion is administered after the first or second session, the specific effect of the HBOT treatment cannot be evaluated and thus, subsequent sessions will be cancelled. The VAS scores considered for analysis will be those collected before the transfusion/exchange. In certain strictly defined circumstances and only for patients needing more than 2 L/min of oxygen, patients will not be recruited in the RCT but could receive HBOT off protocol, as per usual practice in the institution. After inclusion, patients will be followed up for 1 year (by telephone or medical file).
Sample size
We estimated the sample size calculation based on our primary, patient-focused, outcome: the difference in reduction in VAS score between H0 and H6 between study arms. The minimum difference in VAS score between H0 and H6 considered as clinically relevant is 1.3 points (on a scale of 0 to 10), particularly for the treatment of VOC in ER.45 46 In the sham group, the decreased VAS score between H0 and H6 is expected to be less marked than in the intervention group (difference of more than 1.3). The expected SD of the VAS score difference between H0 and H6 is based on a preliminary study of nine patients. In this study, the SD of the VAS score after HBOT was 2.0 and the SD of the difference between H0 and H6 was 1, which corresponds to a strong correlation (0.88) between the VAS score at H0 and H6. With a more conservative assumption that the correlation between H0 and H6 is 0.50, the SD of the VAS score difference between H0 and H6 is 2 in the HBOT group. Assuming that the SD of the difference is the same in the sham group and a bilateral risk alpha of 0.05, the sample size to obtain a 90% power is 50 patients per study arm (100 patients in total).
Study phase
This is a phase III study. An RCT remains the only appropriate design to answer the question of effectiveness of HBOT on VOC. This study follows the pilot study published by our group in 2012. As SCD is a rare disease, the considered sample size is sufficient to meet the phase III criteria.
Patient population
Any patient, 8 years of age or older with a VOC, admitted to the ED and requiring level 3 analgesia (according to WHO definition) may be screened and included in this study unless they have exclusion criteria.
Inclusion and exclusion criteria
Inclusion and exclusion criteria are listed in detail in box 1.
Box 1. Eligibility criteria.
Inclusion criteria:
Patients aged 8 or older.
Diagnosed with a major SCD disorder (SS, SC, Sβ0 and Sβ+-thalassemias, other).
A presentation of a VOC (with or without ACS) unresponsive to level 2 analgesics (WHO classification) which fulfils the criteria necessary for consultation at an ED.
The ability to carry out the Valsalva manoeuvre.
The ability to give informed consent and sign a written informed consent form (consent and signature of legal guardian is required for minor patients or those under guardianship).
Exclusion criteria:
Pregnancy.
Indication for mechanical ventilation (non-invasive ventilation/oro-tracheal intubation).
Contraindication for HBOT established by a physician responsible for hyperbaric medicine.
An anomaly in the results of prior transcranial Doppler (TCD) ultrasound (>200 cm/s) or a previous history of stroke (but TCD will not be performed for the study).
Patients requiring more than 2 L/min (28%) of normobaric oxygen to maintain an SpO2 ≥92% (the placebo group would receive equivalent of only 27% O2).
HBOT, hyperbaric oxygen therapy; SCD, sickle cell disease; VOC, vaso-occlusive crisis.
The contraindication for HBOT established by a physician responsible for hyperbaric medicine was as per ECHM/UHMS guidelines (European Committee for Hyperbaric Medicine/Undersea & Hyperbaric Medical Society), for example, untreated pneumothorax, Eustachian tube dysfunction, claustrophobia or other usual contraindications.47
Due to the particular sensitivity of patients with SCD, the study’s HBOT protocol limits pressure to 2.0 ATA with 100% oxygen in order to decrease the risk of seizure. In children, transcranial Dopplers are carried out regularly and abnormalities (>200 cm/s) are an exclusion criterion to limit the possible risk of seizures.
Recruitment
To optimise recruitment, this study has been presented to and discussed with the Swiss Sickle Cell Association. Patient awareness of this protocol will be raised by the haematologist responsible for outpatient follow-up of patients with SCD. The study has been presented to the ED team on several occasions and some of the ED team have been included as investigators to optimise inclusion directly from the ER. Alerts to beeps and emails have been set up on the electronic files of patients with SCD to notify the research and HMU teams of the arrival of a patient with VOC to the ED. Treatment by HBOT outside of the protocol for VOC will not be possible unless contraindications exist for inclusion in the sham arm.
Potential patients will be identified on their arrival by the triage nurse or treating physician who will inform the hyperbaric physician of their arrival. The hyperbaric physician and/or research nurse will then verify the patient’s inclusion and exclusion criteria. The hyperbaric physician is responsible for giving information concerning the study and obtaining the patient’s/legal representative’s informed consent. The patient will then be transferred to the HMU, next to the ED. There, the HMU team will carry out the randomisation and be responsible for giving the treatment/sham according to randomised arm. Data will be collected by research personnel from their respective participating centres. The data will be entered into the eCRF (REDCap software) with confidentiality storage.
Randomisation
Randomisation will be carried out by the HBOT team using REDCap. It will be stratified by site but also by the average hourly dose of morphine received since arrival in the ED until the time of randomisation (high vs low, high=morphine intravenous equivalent, ≥5 mg/hour intravenous, low=<5 mg/hour intravenous in adult patients). Randomisation will be carried out between the intervention strategy (HBOT session at 2 ATA; 90 min; FIO2=1) and the sham (HBOT session at 1.3 ATA; 90 min; FIO2=0.21). Patients will be treated using the same strategy for all sessions. Randomisation will be triple blinded: the patient, treating physician and research team will not be aware of the randomisation arm, only the HMU team.
To preserve the blinding, the randomisation blocks are completely random and the randomisation list created by a researcher completely external to the protocol. The size of randomised group is 1:1 (same numbers of subjects in the two groups).
A questionnaire will be given to the patient to evaluate their experience and impressions. To avoid influencing patients, the HMU team will be excluded from involvement in the questionnaire and more importantly from the evaluation of the VAS. The statistician will equally be blinded to the intervention/sham group allocation.
Intervention and sham
Conventional treatment (standard of care) will already have been initiated regardless of patients’ group. A specific hyperbaric compatible device allows morphine to be administered via a PCA pump while the hyperbaric chamber is pressurised. Vital signs will be measured before and after the HBOT to identify the improvement or worsening of a patient’s condition.
Intervention group
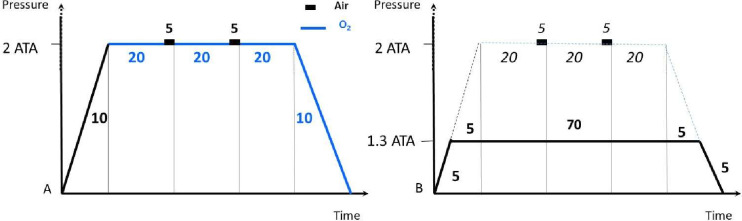
During pressurisation, patients in the intervention group will breathe an FiO2 of 1 (pure oxygen) via a specifically adapted mask. Both compression and decompression phases will take 10 min each (1 m per minute). Compression will be performed on air and decompression in oxygen. Each session will last 90 min (10 min of compression to 2.0 ATA, followed by 3 cycles of 20 min of oxygen at pressure with 5 min on air between cycles, followed by 10 min of decompression) (figure 2). Surveillance by a member of the HMU team is assured throughout the entirety of each session.
Figure 2. Representation of procedures for intervention (A) and sham (B). Intervention (A): 10 min of compression to 2.0 ATA, followed by 3 cycles of 20 min of oxygen at pressure with 5 min on air between cycles, followed by 10 min of decompression (total of 90 min). Sham (B): 5 min of compression period followed by 80 min at 1.3 ATA with air, then a decompression period of 5 min (total of 90 mn). ATA, atmosphere absolute.
Sham group
A previously validated sham25 will be used using the same chamber as in the intervention arm, but with the pressure limited to 1.3 ATA and an FIO2 at 0.21 (via the same model of mask as the intervention arm). As described, additional measures will be taken to simulate the intervention session such as faster compression with ventilation during the fictitious compression time, heating at compression and cooling at decompression. The sham session will be identical in duration to the intervention group (total duration of 90 min with 5 min compression period followed by 80 min at 1.3 ATA with air, then a decompression period of 5 min) (figure 2). The sham group (control group) will avoid only mild potential adverse effects of pressurisation such as minimal ear barotrauma.
Unblinding emergency procedure
If side effects are experienced, the sessions (HBOT/sham) will be interrupted. An unblinding procedure may be proposed in the event of a serious adverse event (SAE), for example, as barotrauma or seizure. This procedure will be initiated by the HMU team, with the agreement of the coordinating investigator. Unblinding will allow the treating clinician to investigate and treat the cause of the SAE. An identical unblinding procedure will also be implemented for the second and/or third session.
Standard of care given to all patients in both randomised groups
The usual protocols for VOC/ACS should be implemented as soon as possible after the patient’s arrival at the hospital.
All patients should benefit from a treatment that will include:
Normobaric oxygen therapy administered by nasal cannula to maintain a SpO2≥94%.
Intravenous hydration: NaCl 1500 mL/24 hours (adapted in the case of paediatric inclusion).
Analgesics: Paracetamol and intravenous morphine (±PCA) according to defined adult or paediatric guidelines. (A PCA protocol will be established for unified management. This will involve, eg, morphine boluses of 0.025–0.05 mg/kg without background infusion initially in adult patients, with hydromorphone or fentanyl often being used for paediatric patients.)
Antibiotic therapy for ACS, documented infectious syndrome or suspected infection (Co-Amoxycillin+macrolide or Levofloxacin in case of allergy).
Transfusion therapy (transfusion or exchange transfusion) may be indicated according to the usual recommendations.
Criteria for discontinuing or modifying interventions
Adverse events may result in the interruption of HBOT/sham sessions. In the event of a failure to equalise ears, a myringotomy (tympanic perforation) will be proposed. A separate consent from the patient will be sought before performing this. In the case of refusal, patients will no longer continue to benefit from the chamber but will be analysed in their randomised arm. Panic attacks, other manifestations of anxiety or claustrophobia related to confinement in the chamber is prevented by the presence of a healthcare personnel who accompany patients during their first HBOT compression and who remain nearby afterwards.
Seizures due to the oxygen toxicity can be resolved, with no residual neurological damage, by decreasing the inspired partial pressure of oxygen (PO2), resulting in a reduced cerebral PO2. If necessary, benzodiazepines are used. However, combining benzodiazepines with morphine should be considered with much caution due to the increased risk of respiratory depression (both drugs depress the brainstem areas responsible for regulating breathing in any hypoxic patients).
Other adverse events usually recede after treatment ceases. In the case of a serious adverse reaction during the first or the second session, additional sessions will be foregone. If the patient does not wish to undergo the second or third session, it will be cancelled. Since the main outcome is evaluated after the first session, any patients leaving the protocol will not be replaced.
If transfusion therapy (simple or exchange transfusion) is administered because of the VOC or ACS, this will be considered as a treatment failure and the protocol will be interrupted. If the indication for transfusion therapy is not related to VOC and/or ACS, it should be administered, where possible, after the end of the third HBOT session, after the last assessment with the VAS score, that is, 4 hours after the last session. If the indication is urgent, it may be administered without delay. Exchange transfusion may be indicated for the treatment of acute priapism (lasting more than 3 hours with little or no effect from intracavernous etilnephrine injections), ischaemic stroke and recurrent severe infection. It could also be indicated prior to surgery.
Data Safety Monitoring Board
The appointed Data Safety Monitoring Board (DSMB) will be unblinded and will undertake an interim safety analysis to ensure that no serious adverse events occur significantly more frequently in the intervention group than in the sham group. A comparative analysis will be carried out by Fisher’s test. The DSMB will benefit from regular reports on safety outcomes (after 6, 12, then 50 patients) and, if necessary, will have the option of requesting the discontinuation of the study for safety reasons. Furthermore, an internal independent audit from the HUG also validated the continuation of the study to the extent that it would be funded, by proposing substantial improvements.
Objectives
Primary objective
The primary objective of this study was to measure the effectiveness of HBOT in the treatment of SCD-VOC, as measured by a decrease in the pain level 6 hours after the initiation of HBOT.
Secondary objectives
The secondary objective of this study was to analyse safety and other clinical, biological and cost outcomes of this HBOT procedure on patients with SCD and to observe the effects of HBOT on relevant biological markers (CRP [C-reactive protein], LDH [Lactate DesHydrogenase]) during a sickle-cell crisis, duration of VOC, transfusion therapy indications, morphine doses, length of stay (LOS) and the occurrence of adverse events. In addition, we wish to analyse the long-term impact of HBOT by observing the frequency of VOC recurrence during the following year as well as analysing cost implications of the implementation of HBOT.
An ancillary study will analyse the effect of HBOT on the evolution of biological markers of interest during a VOC in both the intervention and sham groups. As described earlier, blood samples will be taken from adult patients included at the Geneva centre only, who consent to this additional study (‘Biobank study’).
Outcomes
All outcomes are detailed in table 1.
Table 1. Outcomes parameters and measurement.
| First primary outcome | |
| Difference in the global VAS (VAS 0 to 10) | Difference between the global VAS score—H0 (immediately before first HBOT session) and the global VAS score—H6 (4 hours after first HBOT session). Pain network: Réseau douleur à Genève aux HUG - HUG. |
| Second primary outcome | |
| Composite outcome: Number of patients with a VAS >4 and/or a morphine dose within 4 hours after the HBOT session >1 mg/hour IV morphine equivalent in addition to the usual outpatient dose. | This evaluation will be made 4 hours after each HBOT session. The dose will be calculated based on PCA morphine usage data. All additional forms of morphine administered will be included in this calculation. An equivalent of this morphine will be calculated according to the recommendations of the Pain Network. |
| Secondary outcomes | |
| Length of stay | In the different acute wards (in days), starting from admission to the ED until discharge or transfer to a rehabilitation facility |
| CPS ranges from 0 to 3 points in 7 body sites (the 4 limbs, ribs and sternum, head, and spine and pelvis). | Difference between the global CPS score—H0 (immediately before first HBOT session) and the global CPS score—H6 (4 hours after first HBOT session). Same measurements for second and third sessions. |
| Number of patients relieved at H6 and H24 | Defined by a reduction of VAS score >30% with doses of level 3 painkillers inferior or equal to compared with H049 |
| Frequency of patients with VOC terminated at each visit | VOC is terminated when VAS <2, in the absence of level 3 painkillers |
| Duration of VOC since inclusion (in hours) | A VOC is considered terminated when at least 3 of the following four criteria are met: absence of fever for 8 hours; absence of pain progression and requirement of intravenous infusion of opioid analgesics for the last 8 hours; pain-free mobilisation; or absence of spontaneous pain with a CPS of 1 or less. The success rate will be defined as the percentage of VOC terminated without recourse to transfusion and or the occurrence of complications.50 |
| Indications and use of transfusions or transfusion exchanges | |
| The occurrence of complications during hospitalisation | |
| Vital signs | Heart rate, blood pressure and percutaneous oxygen saturation will be measured before and after each HBOT session |
| Relevant biological markers of sickle cell crisis | CRP (C-reactive protein), LDH (Lactate DesHydrogenase), haemoglobin and reticulocytes levels, leucocytes, when carried out at inclusion and again at H24 |
| Patient satisfaction and impression questionnaire | Questions about :
|
| The Patient Global Impression of Change scale (PGIC) | Assessed as recommended by IMMPACT for use in chronic pain clinical trials as a core outcome measure of global improvement with treatment49 |
| Evaluation of VOC recurrences requiring hospitalisation | A new episode of VOC will be defined by the recurrence of painful spell after a free interval >24 hours pain-free or with usual pain level |
| A medico-economic analysis | Based on the actual expenditure in the intervention and control groups |
| Ancillary study ‘Biobank’ | Blood samples to measure these biomarkers will be taken immediately before and after the first HBOT session, with a third sample being taken at 24 to 36 hours after the beginning of the HBOT session or just before discharge if less than 24 hours. Consequences of oxidative stress on lipids: Dosage of plasma malondialdehyde, measurement of lipid peroxidation, dosage of Thiols Barbituric Acid Reactive SpeciesOxidative stress on proteins (Oxyblot): Measurement of advanced glycation products, nitrosation products and protein glutathione formationSerum markers of inflammation: Dosage of pro and anti-inflammatory cytokines (IL2-IL6, IL10, IL1-β, TNFα, IL12)Adhesion proteins: ICAM-1, VCAM-1, glycocalixTissue ischaemia: ischaemia modified albumin |
| Safety outcomes | Any side effects will be systematically documented both during and/or following each HBOT session by the HMU or ward team. Details will include date, precise time, duration and a detailed account of the event as well as the action and effect of the action taken. The probability of the HBOT session being accountable for the side effect and severity will be rated according to the usual grading: mild (tolerable), moderate (interferes with daily activity) or severe (daily activities impossible). Any serious adverse event must be reported to the principal investigator within 24 hours. |
CPSCategorical Pain ScoreCRPC-reactive proteinEDemergency departmentHBOThyperbaric oxygen therapyHMUHyperbaric Medicine UnitIVintravenousLDHLactate DesHydrogenasePCAPatient Controlled AnalgesiaVASVisual Analogue ScaleVOCvaso-occlusive crisis
First primary outcome
The difference in the global VAS pain score was evaluated immediately before (H0) and 4 hours after (H6) the HBOT/sham session.48
Second primary outcome (composite outcome)
The number of patients with a VAS pain score >4 and/or a morphine dosage >1 mg/hour (or 0.02 mg/kg/hour) intravenously after the HBOT/sham session was evaluated.
Secondary outcomes (comparison to be made between the intervention and sham groups)
Differences in VAS pain scores between H0 and H24, difference between H0, H6 and H24 of Categorical Pain Score (CPS) ranges from 0 to 3 points in seven body sites, change in hourly doses of morphine; accumulated dose of parenteral opioid equivalent from baseline until VOC resolution or until discharge; time until discontinuation of intravenous opioids; length of hospital stay; number of patients experiencing relief from pain at both H6 and H24 (with a reduction in VAS pain score >30% compared with H0); change in pain intensity from baseline to every 4 hours during awake time, until VOC resolution; pain location; patient’s ‘global impression of change’ (using a 7-point rating scale with the options ‘very much improved,’ ‘much improved,’ ‘minimally improved,’ ‘no change,’ ‘minimally worse,’ ‘much worse,’ and ‘very much worse’)49; frequency of patients with VOC terminated at each visit (VOC is terminated when VAS<2, in the absence of painkillers of level 3) and time until end of VOC (until 48 hours of follow-up); absence of parenteral opioid use; indications for and implementation of transfusion therapies during hospitalisation; complications (notably ACS, priapism, stroke or other) and values of appropriate biomarkers associated with a sickle cell crisis (LDH, CRP); readiness for discharge as judged by the patient or physician; evaluation of patient satisfaction via a questionnaire; recurrences of VOC during the following year; further hospitalisations during the following year; treatment costs; death during hospitalisation or after discharge; occurrence of adverse events of HBOT/sham.
The different outcomes will be identified in the patient’s electronic charting system by the research team and entered into the eCRF. The specific outcomes (scores, biology, investigations) will be prescribed by the HMU physician/research team and performed and then documented by the clinical team in charge of the patient.
Statistical methods
Analysis of the primary outcome
The primary outcome is the change in global VAS between before (H0) and after (H6) the first HBOT session. The mean change in VAS will be reported in each arm with the two-sided 95% CI. The null hypothesis that the mean change in VAS is the same in both arms will be tested using linear regression model adjusted for the centre and for the hourly dose of morphine prior to inclusion (high vs low, defined by the average hourly dose since admission converted into morphine intravenous equivalent, respectively, >5 mg/hour intravenous or ≤5 mg/hour intravenous). The risk of type I error will be 0.05 two-sided. The intervention’s effect will be assessed by the adjusted mean difference in change of VAS between study arms and will be reported with the two-sided 95% CI. Other adjustments will be considered, for example, depending on the homozygous or heterozygous type, treatment with hydroxycarbamide or a complication with an ACS.
Analysis of the second primary outcome (composite)
The proportion of patients with a VAS pain score >4 and/or a morphine dosage >1 mg/hour intravenous (or equivalent in mcg/kg for the paediatric protocol) after the HBO session will be reported with the Clopper-Pearson exact 95% CI in each study arm. The null hypothesis that the risk to have this outcome is the same in both study arms will be tested using binomial generalised linear regression models adjusted for the centre and the hourly dose of morphine prior to inclusion. The risk of type I error will be 0.05 two-sided. The adjusted difference of risk (from a binomial regression model) and the adjusted risk ratio (from a log-binomial model) will be reported with the two-sided 95% CI.
Analysis of the secondary outcomes
The difference in VAS pain scores between H0 and H24, the difference in hourly doses of morphine between before and after HBOT and the difference in biomarkers (LDH, CRP) between before and after HBOT will be reported in each arm using the same two-sided 95% CI used for the primary outcome.
The length of hospital stay will be described by median and quartiles and compared between study arms with non-parametric test since the distribution of the LOS is expected to deviate considerably from the normal. The van Elteren test (a stratified version of the Mann-Whitney’s test) will be used with stratification on centres and hourly dose of morphine prior to inclusion.
The frequency of patients with a reduction in VAS pain score of 30% or more from H6 to H24 and the frequency of patients with VAS <2 (in the absence of painkillers of level 3) at each visit will be reported with the Clopper-Pearson exact 95% CI in each study arm as for the second primary outcome.
Recurrences of VOC and further hospitalisations during the following year will be described. Survival analyses (Kaplan-Meier survival estimates and log-rank test stratified on centres and hourly dose of morphine prior to inclusion) will be conducted to compare the risk of the first recurrence and the first hospitalisations between intervention and sham. A Cox regression model will be used to assess the HR adjusted for the centre and the hourly dose of morphine prior to inclusion. If needed, survival models with competing risk will be used.
A comparative description can be provided of other outcomes (accumulated dose of parenteral opioid, absence of opioid use, time to discontinuation of intravenous opioids, pain location, transfusions, complications, patient’s satisfaction, readiness for discharge, costs).
The patient’s ‘global impression of change’ will be described and compared between study arms using van Elteren’s test.
The significance level will be two-sided α=0.05 for all analyses. Analyses will be conducted with R (R Development Core Team (2008), R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria).
Any deviation from the original statistical plan will be described and justified in the final trial report.
Analysis population and missing data
Dataset to be analysed
The analysis will be carried out in intention to treat. A sensitivity analysis will be performed in per-protocol analysis (excluding patients who did not have the HBO/sham session). No method of managing missing data is envisaged. The main outcome should be available in all situations.
Interim analysis
No interim effectiveness analysis will be performed. Only an interim safety analysis is envisaged.
Patient and public involvement
The protocol was presented to, discussed with and approved by the patients’ association ‘Suisse-Drépano’ (Swiss Association of Sickle Cell Patients). Information will be disseminated to all its members, and an information session will be proposed by the principal investigator.
Ethics and dissemination
HBOT-SCD study will be carried out in accordance with the research plan and the Declaration of Helsinki, the Swiss Law and Swiss regulatory authority’s requirements as applicable. The application has been approved by the lead committee, that is, the Ethic Committee of Geneva (CER 2019-01707). All protocol modification will be approved by the Ethic Committee. Specific insurance has been taken out to cover possible complications of the protocol for patients.
The results of the studies will be disseminated by several media, including publications in peer-reviewed international medical journals, and presentations at national and/or international conferences. The results can also be incorporated into international recommendations. The authorship will follow the GCP rules.
Data will be shared according to FAIR principles.
Discussion and implications
A feasibility and safety phase was initiated at the Geneva University Hospitals in 2022 (first inclusion the 30.09.2022). Fifteen patients were included with DSMB analyses after the inclusion of 6 and 12 patients recommending the continuation of the study in its current state.
The results of the HBOT-Sickle cell disease study could have an important impact on the effective and rapid management of VOCs in SCD. Often extremely painful and leading to long hospitalisations, these crises have potentially serious consequences and require significant use of both morphine and blood products. A positive study would have a major impact on patients with SCD, improving the quality of life for patients not only in Europe but also worldwide. This is an opportunity to test the effectiveness of the HBOT in VOC-SCD management with a well-designed RCT and a validated sham.
The use of morphine and the need for iterative transfusions to manage the patients during VOCs and ACSs are associated with potentially serious health consequences such as opioid dependence and transfusion risks, as well as the use of scarce resources. Expected benefits of HBOT are the reduction of the level and duration of pain severity, crisis duration, hospital length of stay, number of transfusions required, cumulative quantity of opioids and frequency of ACS and VOCs. Indeed, breaking of the vicious cycle of the crisis early should decrease the frequency/severity of further VOCs and their consequences.
This RCT will increase the level of evidence concerning the efficacy of HBOT in SCD-VOC, and if the results are positive, could broaden its indications. If positive, HBOT could be proposed as an alternative to conventional treatments, creating a place for it among current therapeutic options. This could be of particular value in low-income countries, where the disease is frequent, and use of transfusions remains problematic. The introduction of mobile and easy installed hyperbaric chambers could then be considered in these countries.
The medico-economic interest will of course have to be analysed, but the possible reduction of LOS and the use of blood transfusions will potentially lead to major savings when compared with the cost of this technique. This study will use a hyperbaric chamber that is already marketed, licensed and used in other pathologies.
In conclusion, we are anticipating that this study will clarify the strength of evidence, either supporting or refuting indication for the use of HBOT in the treatment of VOC-SCD.
Acknowledgements
We would like to thank all SCD-patients, all members of HBOT-SCD study group, the HMU team, the adult and paediatric ER teams, medical ward staff and pain teams, the research nurses, the coordinators and monitors, and the Clinical Research Centre of Hôpitaux Universitaires de Genève (HUG).
Footnotes
Funding: This study is partially funded by the Research funding of Geneva University Hospitals and the French Society of Physiology and Subaquatic and Hyperbaric Medicine (MedSubHyp).
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-084825).
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: HBOT-SCD study group: Jérôme Stirnemann, Jacques Serratrice, Tamara Mann, Pierre Louge, Christophe Combescure, Kaveh Samii, Rodrigue Pignel, Thomas Agoritsas, Marc Ansari, Giovanna Cannas, Yves Chalandon, Laurent Cimasoni, Pierre Cougoul, Benoit Desgraz, Alain Gervaix, Olivier Grosgurin, Thierry Joffre, Claude Lae, Pierre Louge, Marie-Anne Magnan, Etienne Menager, Annie Momo Bona, Marc Alain Panchard, Michel Pellegrini, Solène Poutrel, Jean-Luc Reny, Beatrice Riu, Cyril Sahyoun and Sylvain Boet.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting or dissemination plans of this research. Refer to the Methods and analysis section for further details.
Contributor Information
Jerome Stirnemann, Email: Jerome.stirnemann@hcuge.ch.
Jacques Serratrice, Email: jacques.serratrice@hcuge.ch.
Tamara Mann, Email: tamara.mann@hcuge.ch.
Pierre Louge, Email: pierre.louge@hcuge.ch.
Combescure Christophe, Email: christophe.combescure@hcuge.ch.
Kaveh Samii, Email: kaveh.samii@hcuge.ch.
Rodrigue Pignel, Email: rodrigue.pignel@hcuge.ch.
Thomas Agoritsas, Email: thomas.agoritsas@hcuge.ch.
Marc Ansari, Email: marc.ansari@hcuge.ch.
Giovanna Cannas, Email: giovanna.cannas@chu-lyon.fr.
Yves Chalandon, Email: Yves.Chalandon@hug.ch.
Laurent Cimasoni, Email: laurent.cimasoni@hcuge.ch.
Pierre Cougoul, Email: cougoul.pierre@iuct-oncopole.fr.
Benoit Desgraz, Email: benoit.desgraz@hcuge.ch.
Alain Gervaix, Email: alain.gervaix@hcuge.ch.
Olivier Grosgurin, Email: olivier.grosgurin@hcuge.ch.
Thierry Joffre, Email: thierry.joffre@chu-lyon.fr.
Claude Lae, Email: claude.lae@hug.ch.
Marie-Anne Magnan, Email: marieanne.magnan@free.fr.
Etienne Menager, Email: etienne.menager@hcuge.ch.
Annie Momo Bona, Email: momobona.a@chu-toulouse.fr.
Marc-Alain Panchard, Email: marc-alain.panchard@hcuge.ch.
Michel Pellegrini, Email: michel.pellegrini@hcuge.ch.
Jean-Luc Reny, Email: jean-luc.reny@hug.ch.
Beatrice Riu, Email: riu.b@chu-toulouse.fr.
Cyril Sahyoun, Email: cyril.sahyoun@hcuge.ch.
Sylvain Boet, Email: sylvain.boet@hcuge.ch.
References
- 1.Arnal C, Godeau B. Stratégie de La Prise En Charge Des Crises Vaso-Occlusives Non Compliquées de l’adulte Drépanocytaire. La drépanocytose. Paris: Girot, R; 2003. pp. 77–83. [Google Scholar]
- 2.Vichinsky EP, Neumayr LD, Earles AN, et al. Causes and Outcomes of the Acute Chest Syndrome in Sickle Cell Disease. N Engl J Med . 2000;342:1855–65. doi: 10.1056/NEJM200006223422502. [DOI] [PubMed] [Google Scholar]
- 3.Brandow AM, Liem RI. Advances in the diagnosis and treatment of sickle cell disease. J Hematol Oncol. 2022;15:20. doi: 10.1186/s13045-022-01237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sundd P, Gladwin MT, Novelli EM. Pathophysiology of Sickle Cell Disease. Annu Rev Pathol. 2019;14:263–92. doi: 10.1146/annurev-pathmechdis-012418-012838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Setty BNY, Stuart MJ, Dampier C, et al. Hypoxaemia in sickle cell disease: biomarker modulation and relevance to pathophysiology. Lancet. 2003;362:1450–5. doi: 10.1016/S0140-6736(03)14689-2. [DOI] [PubMed] [Google Scholar]
- 6.Kaul DK, Hebbel RP. Hypoxia/reoxygenation causes inflammatory response in transgenic sickle mice but not in normal mice. J Clin Invest. 2000;106:411–20. doi: 10.1172/JCI9225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joneckis CC, Ackley RL, Orringer EP, et al. Integrin alpha 4 beta 1 and glycoprotein IV (CD36) are expressed on circulating reticulocytes in sickle cell anemia. Blood. 1993;82:3548–55. [PubMed] [Google Scholar]
- 8.Gupta K, Gupta P, Solovey A, et al. Mechanism of interaction of thrombospondin with human endothelium and inhibition of sickle erythrocyte adhesion to human endothelial cells by heparin. Biochim Biophys Acta. 1999;1453:63–73. doi: 10.1016/s0925-4439(98)00085-4. [DOI] [PubMed] [Google Scholar]
- 9.Udani M, Zen Q, Cottman M, et al. Basal cell adhesion molecule/lutheran protein. The receptor critical for sickle cell adhesion to laminin. J Clin Invest. 1998;101:2550–8. doi: 10.1172/JCI1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ducrocq R, Pascaud O, Bévier A, et al. Strategy linking several analytical methods of neonatal screening for sickle cell disease. J Med Screen. 2001;8:8–14. doi: 10.1136/jms.8.1.8. [DOI] [PubMed] [Google Scholar]
- 11.Matsui NM, Borsig L, Rosen SD, et al. P-selectin mediates the adhesion of sickle erythrocytes to the endothelium. Blood. 2001;98:1955–62. doi: 10.1182/blood.v98.6.1955. [DOI] [PubMed] [Google Scholar]
- 12.Fadlon E, Vordermeier S, Pearson TC, et al. Blood polymorphonuclear leukocytes from the majority of sickle cell patients in the crisis phase of the disease show enhanced adhesion to vascular endothelium and increased expression of CD64. Blood. 1998;91:266–74. [PubMed] [Google Scholar]
- 13.Wun T, Paglieroni T, Tablin F, et al. Platelet activation and platelet-erythrocyte aggregates in patients with sickle cell anemia. J Lab Clin Med. 1997;129:507–16. doi: 10.1016/s0022-2143(97)90005-6. [DOI] [PubMed] [Google Scholar]
- 14.Castro O, Brambilla DJ, Thorington B, et al. The acute chest syndrome in sickle cell disease: incidence and risk factors. The Cooperative Study of Sickle Cell Disease. Blood. 1994;84:643–9. [PubMed] [Google Scholar]
- 15.Kato GJ, Steinberg MH, Gladwin MT. Intravascular hemolysis and the pathophysiology of sickle cell disease. J Clin Invest. 2017;127:750–60.:89741. doi: 10.1172/JCI89741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perelman N, Selvaraj SK, Batra S, et al. Placenta growth factor activates monocytes and correlates with sickle cell disease severity. Blood. 2003;102:1506–14. doi: 10.1182/blood-2002-11-3422. [DOI] [PubMed] [Google Scholar]
- 17.Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330:1639–44. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 18.Solovey A, Lin Y, Browne P, et al. Circulating activated endothelial cells in sickle cell anemia. N Engl J Med. 1997;337:1584–90. doi: 10.1056/NEJM199711273372203. [DOI] [PubMed] [Google Scholar]
- 19.Gladwin MT, Kanias T, Kim-Shapiro DB. Hemolysis and cell-free hemoglobin drive an intrinsic mechanism for human disease. J Clin Invest. 2012;122:1205–8.:62972. doi: 10.1172/JCI62972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cardenes N, Corey C, Geary L, et al. Platelet bioenergetic screen in sickle cell patients reveals mitochondrial complex V inhibition, which contributes to platelet activation. Blood. 2014;123:2864–72. doi: 10.1182/blood-2013-09-529420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brandow AM, Carroll CP, Creary S, et al. American Society of Hematology 2020 guidelines for sickle cell disease: management of acute and chronic pain. Blood Adv. 2020;4:2656–701. doi: 10.1182/bloodadvances.2020001851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simon E, Long B, Koyfman A. Emergency Medicine Management of Sickle Cell Disease Complications: An Evidence-Based Update. J Emerg Med. 2016;51:370–81. doi: 10.1016/j.jemermed.2016.05.042. [DOI] [PubMed] [Google Scholar]
- 23.Mathieu D, Marroni A, Kot J. Tenth European Consensus Conference on Hyperbaric Medicine: preliminary report. Diving Hyperb Med. 2016;46:122–3. [PubMed] [Google Scholar]
- 24.Camporesi EM, Bosco G. Mechanisms of action of hyperbaric oxygen therapy. Undersea Hyperb Med. 2014;41:247–52. [PubMed] [Google Scholar]
- 25.Louge P, Pignel R, Serratrice J, et al. Validation of sham treatment in hyperbaric medicine: a randomised trial. Diving Hyperb Med. 2023;53:51–4. doi: 10.28920/dhm53.1.51-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Camporesi EM. Side effects of hyperbaric oxygen therapy. Undersea Hyperb Med. 2014;41:253–7. [PubMed] [Google Scholar]
- 27.Jokinen-Gordon H, Barry RC, Watson B, et al. A Retrospective Analysis of Adverse Events in Hyperbaric Oxygen Therapy (2012-2015): Lessons Learned From 1.5 Million Treatments. Adv Skin Wound Care. 2017;30:125–9. doi: 10.1097/01.ASW.0000508712.86959.c9. [DOI] [PubMed] [Google Scholar]
- 28.Chen MF, Chen HM, Ueng SW, et al. Hyperbaric oxygen pretreatment attenuates hepatic reperfusion injury. Liver. 1998;18:110–6. doi: 10.1111/j.1600-0676.1998.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 29.Kaul DK, Liu XD, Fabry ME, et al. Impaired nitric oxide-mediated vasodilation in transgenic sickle mouse. Am J Physiol Heart Circ Physiol. 2000;278:H1799–806. doi: 10.1152/ajpheart.2000.278.6.H1799. [DOI] [PubMed] [Google Scholar]
- 30.Solovey A, Gui L, Key NS, et al. Tissue factor expression by endothelial cells in sickle cell anemia. J Clin Invest. 1998;101:1899–904. doi: 10.1172/JCI1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buras JA, Stahl GL, Svoboda KK, et al. Hyperbaric oxygen downregulates ICAM-1 expression induced by hypoxia and hypoglycemia: the role of NOS. Am J Physiol Cell Physiol . 2000;278:C292–302. doi: 10.1152/ajpcell.2000.278.2.C292. [DOI] [PubMed] [Google Scholar]
- 32.Kaul DK, Liu X, Zhang X, et al. Inhibition of sickle red cell adhesion and vasoocclusion in the microcirculation by antioxidants. Am J Physiol Heart Circ Physiol. 2006;291:H167–75. doi: 10.1152/ajpheart.01096.2005. [DOI] [PubMed] [Google Scholar]
- 33.Mehdaoui H, Drepanocytose DJH. Traité de Médecine Hyperbarre. Ellipses; 2022. pp. 416–23. [Google Scholar]
- 34.Desforges JF, Wang MY. Sickle cell anemia. Med Clin North Am. 1966;50:1519–32. doi: 10.1016/s0025-7125(16)33102-9. [DOI] [PubMed] [Google Scholar]
- 35.Laszlo J, Obenour W, Saltzman HA. Effects of hyperbaric oxygenation on sickle syndromes. S Med J. 1969;62:453–6. doi: 10.1097/00007611-196904000-00018. [DOI] [PubMed] [Google Scholar]
- 36.Reynolds JD. Painful sickle cell crisis. Successful treatment with hyperbaric oxygen therapy. JAMA. 1971;216:1977–8. [PubMed] [Google Scholar]
- 37.Freilich DB, Seelenfreund MH. Hyperbaric oxygen, retinal detachment, and sickle cell anemia. Arch Ophthalmol. 1973;90:90–3. doi: 10.1001/archopht.1973.01000050092002. [DOI] [PubMed] [Google Scholar]
- 38.Coeur P, Bertrand JL, Woehrle R, et al. Oxygénothérapie hyperbare des crises douloureuses osseuses rebelles de la drépanocytose homozygote. Nouv Presse Med. 1975;4:1655. [PubMed] [Google Scholar]
- 39.Freilich DB, Seelenfreund MH. Long-term follow-up of scleral buckling procedures with sickle cell disease and retinal detachment treated with the use of hyperbaric oxygen. Mod Probl Ophthalmol. 1977;18:368–72. [PubMed] [Google Scholar]
- 40.Perrimond H. Médecine Hyperbare. La Drépanocytose; 1992. pp. 131–6. [Google Scholar]
- 41.Mehdaoui H, Letellier E. Université de Lille: mémoire de DIU; 1994. L’oxygénothérapie hyperbare pour les drépanocytaires. [Google Scholar]
- 42.Dubois B. Drépanocytose et Hyperbarie. Université de Lilles; 2001. [Google Scholar]
- 43.Huang E. Hyperbaric Oxygen Therapy Indications. 15th Edition. Undersea and Hyperbaric Medical Society; 2023. [Google Scholar]
- 44.Stirnemann J, Letellier E, Aras N, et al. Hyperbaric oxygen therapy for vaso-occlusive crises in nine patients with sickle-cell disease. Diving Hyperb Med. 2012;42:82–4. [PubMed] [Google Scholar]
- 45.Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38:633–8. doi: 10.1067/mem.2001.118863. [DOI] [PubMed] [Google Scholar]
- 46.Lopez BL, Flenders P, Davis-Moon L, et al. Clinically significant differences in the visual analog pain scale in acute vasoocclusive sickle cell crisis. Hemoglobin. 2007;31:427–32. doi: 10.1080/03630260701587810. [DOI] [PubMed] [Google Scholar]
- 47.Gawdi R, Cooper J. Hyperbaric Contraindications. Treasure Island (FL) ineligible companies: StatPearls; 2024. Jeffrey cooper declares no relevant financial relationships with ineligible companies. [Google Scholar]
- 48.Dampier CD, Smith WR, Wager CG, et al. IMPROVE trial: a randomized controlled trial of patient-controlled analgesia for sickle cell painful episodes: rationale, design challenges, initial experience, and recommendations for future studies. Clin Trials. 2013;10:319–31. doi: 10.1177/1740774513475850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the Clinical Importance of Treatment Outcomes in Chronic Pain Clinical Trials: IMMPACT Recommendations. J Pain. 2008;9:105–21. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 50.Bartolucci P, El Murr T, Roudot-Thoraval F, et al. A randomized, controlled clinical trial of ketoprofen for sickle-cell disease vaso-occlusive crises in adults. Blood. 2009;114:3742–7. doi: 10.1182/blood-2009-06-227330. [DOI] [PubMed] [Google Scholar]