Abstract
Background
The IMPACT Survey explored the humanistic, clinical, and economic burden of osteogenesis imperfecta (OI) on individuals with OI, their families, caregivers, and wider society. Two previous publications report research methodology, initial insights of the survey, and cost of illness of OI. Here, we present data on the impact of OI on the quality of life (QoL) of adults with OI and explore potential drivers of this impact.
Methods
The IMPACT Survey was an international mixed methods online survey in eight languages (fielded July–September 2021), aimed at adults (aged ≥ 18 years) or adolescents (aged 12–17 years) with OI, caregivers (with or without OI) of individuals with OI, and other close relatives. Survey domains included demographics, socioeconomic factors, clinical characteristics, treatment patterns, QoL, and health economics. We conducted a descriptive analysis of the QoL data, as well as exploratory regression analyses to identify drivers of impact of OI on QoL (independent associations between patient characteristics and the impact on QoL).
Results
1,440 adults with OI participated in the survey. The proportion who reported an impact of OI on their QoL across individual areas in the physical, socioeconomic, and mental well-being domains ranged between 49 and 84%. For instance, 84% of adults reported an impact of OI on the types of leisure activities they could do and 74% on the type of job they could do. More severe self-reported OI and higher fracture frequency were consistently identified as drivers of OI’s impact on QoL. The proportion of adults who reported worrying about different aspects of their lives due to their OI, such as mobility loss, future fractures, and ageing, ranged between 31 and 97%.
Conclusion
IMPACT provides insights into the humanistic burden of OI on adults, revealing that OI has a substantial impact on the QoL of adults. OI severity and fracture frequency were consistently identified as drivers of impact on QoL across all domains. Understanding these drivers may aid in identifying areas for targeted interventions, such as fracture prevention.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-20555-0.
Keywords: Osteogenesis imperfecta, Patient-reported outcomes, Survey, Burden of disease, Fractures, Humanistic burden, Quality of life, Health worries, Pain, Fatigue, Self-reported disease severity
Introduction
Osteogenesis imperfecta (OI) is a rare, heritable condition affecting bone and connective tissue structure and function. Its reported incidence is 1/15,000–20,000, although the actual number may be higher [1–4]. While OI is primarily caused by defects in the Type I collagen genes (COL1A1 and COL1A2), it can also be caused by underlying mutations in other genes linked to collagen synthesis, bone mineralisation, or osteoblast differentiation in rare forms of OI [2]. Symptoms of OI include bone fragility, pain, hypermobility, growth defects, dental abnormalities, cardiovascular and pulmonary issues, and hearing loss [2].
Currently, there are no curative treatments for OI. Care approaches aim to improve mobility and independence by alleviating symptoms and helping individuals to manage them in an optimal way. Due to the varying and potentially complex symptoms [5–10] and the ongoing, multidisciplinary management required, living with OI can affect many aspects of a person’s life.
To date, reports on the humanistic impact of OI have been limited, predominantly focusing on children and specific geographic regions [11]. A substantial proportion of the existing literature on the quality of life (QoL) of adults with OI describes physical functioning, with results suggesting that individuals with OI report impaired physical function and independence compared with the overall population [12–32]. Few publications shed light on mental well-being and social functioning; among those that do, certain knowledge gaps persist. Furthermore, research on the effects of OI on mental health reaches conflicting conclusions, with some authors concluding that OI is correlated with mental health problems and others not [13, 16, 17, 19, 20, 23–25, 33, 34]. Few studies investigate social functioning in adults [19, 24, 33–36], hence the need for further research in this area.
The IMPACT Survey was conducted to better understand the humanistic, economic, and clinical impact of OI on individuals and wider society [37, 38]. Westerheim et al. present the overall findings from the survey, notably that irrespective of age, those with OI experienced a multitude of signs, symptoms, and events that impacted their lives. Here, we present the humanistic burden of OI in adults across physical, socioeconomic, and mental well-being QoL domains, and we identify drivers of impact on QoL.
Methods
Development
The IMPACT Survey was developed by a steering committee consisting of academic researchers, representatives of the Osteogenesis Imperfecta Foundation (OIF, USA), the umbrella association Osteogenesis Imperfecta Federation Europe (OIFE), and representatives of Mereo BioPharma. The survey prioritised topics identified as evidence gaps in a scoping review [11] that were most relevant to individuals with OI and the research community. For more information on the development, design, and fielding of IMPACT, please refer to Westerheim et al. 2024 [37].
Survey domains
The survey included questions on demographics, socioeconomic factors, clinical characteristics, treatment patterns, humanistic impact, and economic outcomes [37]. A list of all survey questions and answer options can be found in Supplementary File 1. To investigate humanistic impact, adults with OI were asked questions about the impact of OI on their lives in the past 12 months (response options included a five-level Likert scale [39]: “not impacted”, “very mildly impacted”, “mildly impacted”, “moderately impacted”, and “severely impacted”) and their worries and concerns about the future (response options included a three-level scale: “do not worry”, “worry a little”, and “worry a lot”). These questions covered many aspects of living, such as careers and finances, social life and relationships, physical well-being and functioning, mental well-being, and healthcare (Table 1).
Table 1.
Domains investigated through questions on quality of life and worries and concerns about the future
| Domain | Impact of OI on quality of life a | Worries and concerns b |
|---|---|---|
| Physical well-being and functioning | Ability to self-care | Getting older |
| Ability to live independently | Ability to care for oneself | |
| Sexual health | Living independently | |
| Losing independence | ||
| Losing mobility | ||
| Ability to have a family | ||
| OI complications | ||
| Future fractures | ||
| Pregnancy | ||
| Menopause | ||
| Careers and finances | Work hours | Losing a job |
| Job type | Future financial situation | |
| Career choices | Financial means to pay for treatment and care | |
| Social life and relationships | Type of leisure activities | Relationship with family and friends |
| Social life | Romantic relationship | |
| Relationships with family and friends | Future of care recipients with OI | |
| Romantic relationships | ||
| Mental well-being | Mental health | |
| Happiness | ||
| Healthcare | Access to doctors | |
| Access to medicines | ||
| Access to care | ||
| Side effects of treatment |
Abbreviations: OI, osteogenesis imperfecta
aQuestions 102 & 106 “In the past 12 months, how would you describe the impact that OI has had on your life?”, where respondents received the following instructions: “This question is about understanding the ‘negative’ impacts or challenges you have faced”; bQuestions 103, 104, 105, 107, 108, & 109 “Do you feel worried or concerned about any of the following things?”
Data processing
As previously reported [37], survey data were translated into English and compiled into a master database using the pandas Python software package. Microsoft Excel was used to clean, code and validate data, as well as to generate descriptive statistics. Data were cleaned to exclude any outliers and nonsensical responses. Free text responses were translated into English, and responses were aligned with previous answer options if applicable or categorised into several recurring themes.
Descriptive analysis
Categorical measures are presented as frequencies (number of respondents, n) and percentages (%) of total survey respondents.
Regression analysis
Multinomial logistic regression analyses were conducted to identify independent associations, henceforth called drivers, of the impact of OI on QoL (“very mildly”, “mildly”, “moderately”, or “severely” impacted) and worries and concerns (“worry a little” or “worry a lot”). Investigated drivers were self-reported OI severity, sex, age, mobility status, employment status, household living arrangement, fracture frequency in the past 12 months, and clinical signs, symptoms, and events experienced in the past 12 months. Due to a broad alignment found between clinical OI type and self-reported OI severity [37], we did not investigate OI type as a driver. A summary of included and excluded variables can be found in Supplementary Material 2. Results of regression analyses are presented as relative risk ratios (RRR), with p-values ≤ 0.05 considered statistically significant. Regression analyses were performed using R version 4.4.0.
Results
Demographics and clinical characteristics
Demographics and clinical characteristics of the adults with OI population (n = 1,440) have been previously reported. Briefly, 70% were female, the median age was 43 years, most adults (66%) reported walking unaided, either indoors or outside, and were in paid employment (58%) [37, 38]. The most common household living situation for adults with OI was living with their partner only (29%). We observed variation in reported living and mobility status between those with differing self-reported OI severities; many adults with severe OI reported living alone (32%) or with their parents (32%), whereas two-thirds of adults with mild OI lived with their partner and children if applicable (67%). Most adults with severe OI used wheelchairs indoors or outdoors (83%), and one-fifth (20%) reported walking unaided, whereas only 6% of those with mild OI used wheelchairs, and 95% reported walking unaided (Please see Supplementary Material 3 for a table of demographics of adults with OI).
Impact of OI on QoL
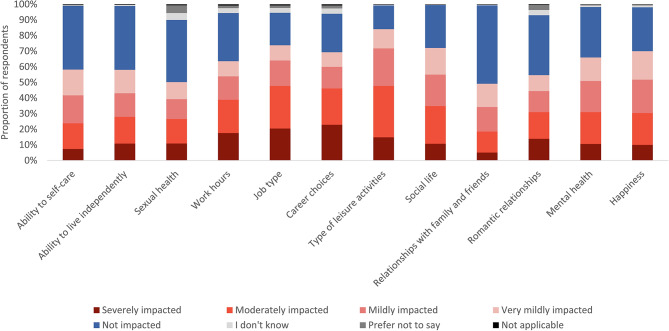
The proportion of adults whose QoL was impacted is reported as a sum of those impacted very mildly, mildly, moderately, and severely. This grouping encompasses all levels of impact. Across all QoL domains, the proportion of adults who were very mildly impacted represents a similar or smaller proportion of those impacted than those mildly or moderately impacted. These proportions are depicted in Fig. 1. A breakdown of each degree of impact, by different patient characteristics, can be found in Supplementary Material 4.
Fig. 1.
The reported degree of impact of OI on the quality of life of adults with OI, displayed as a stacked bar graph of percentages (n = 1,440). Abbreviations: OI, osteogenesis imperfecta. This graph is based on the responses to questions 102 & 106 “In the past 12 months, how would you describe the impact that OI has had on your life?”, where respondents received the following instructions: “This question is about understanding the ‘negative’ impacts or challenges you have faced”
Across all 12 QoL areas queried (Table 1), OI had an impact (ranging from very mild to severe) on the lives of adults. At least 49% of adults with OI were affected in each area. The areas most commonly impacted by OI (reported by over 70% of participants) were job types (74%), social life (72%), and types of leisure activities respondents could do (84%). Areas less commonly impacted were sexual health and relationships with family and friends, yet a substantial proportion of adults were impacted in these areas (50% and 49%, respectively; Table 2; Figs. 1 and 2, Supplementary Material 4).
Table 2.
Impact of OI on quality of life of adults with OI (n = 1,440)
| Impact on quality of life, n (%) a | Severely impacted | Moderately impacted | Mildly impacted | Very mildly impacted | Not impacted | I don’t know | Prefer not to say | Not applicable |
|---|---|---|---|---|---|---|---|---|
| Ability to self-care | 106 (7.4) | 237 (16.5) | 258 (17.9) | 237 (16.5) | 588 (40.8) | 4 (0.3) | 5 (0.3) | 5 (0.3) |
| Ability to live independently | 156 (10.8) | 246 (17.1) | 218 (15.1) | 216 (15.0) | 588 (40.8) | 8 (0.6) | 3 (0.2) | 5 (0.3) |
| Sexual health | 157 (10.9) | 225 (15.6) | 183 (12.7) | 158 (11.0) | 573 (39.8) | 63 (4.4) | 72 (5.0) | 9 (0.6) |
| Work hours | 253 (17.6) | 307 (21.3) | 216 (15.0) | 139 (9.7) | 444 (30.8) | 45 (3.1) | 24 (1.7) | 12 (0.8) |
| Job type | 295 (20.5) | 392 (27.2) | 235 (16.3) | 140 (9.7) | 300 (20.8) | 44 (3.1) | 23 (1.6) | 11 (0.8) |
| Career choices | 329 (22.8) | 335 (23.3) | 199 (13.8) | 135 (9.4) | 355 (24.7) | 49 (3.4) | 27 (1.9) | 11 (0.8) |
| Type of leisure activities | 214 (14.9) | 473 (32.8) | 346 (24.0) | 178 (12.4) | 218 (15.1) | 4 (0.3) | 4 (0.3) | 3 (0.2) |
| Social life | 154 (10.7) | 348 (24.2) | 290 (20.1) | 245 (17.0) | 396 (27.5) | 2 (0.1) | 2 (0.1) | 3 (0.2) |
| Relationships with family and friends | 73 (5.1) | 194 (13.5) | 226 (15.7) | 214 (14.9) | 723 (50.2) | 4 (0.3) | 3 (0.2) | 3 (0.2) |
| Romantic relationships | 200 (13.9) | 246 (17.1) | 194 (13.5) | 147 (10.2) | 552 (38.3) | 48 (3.3) | 46 (3.2) | 7 (0.5) |
| Mental health | 153 (10.6) | 293 (20.3) | 287 (19.9) | 217 (15.1) | 465 (32.3) | 14 (1.0) | 8 (0.6) | 3 (0.2) |
| Happiness | 144 (10.0) | 294 (20.4) | 307 (21.3) | 263 (18.3) | 404 (28.1) | 17 (1.2) | 8 (0.6) | 3 (0.2) |
Abbreviations: OI, osteogenesis imperfecta
aQuestions 102 & 106 “In the past 12 months, how would you describe the impact that OI has had on your life?”, where respondents received the following instructions: “This question is about understanding the ‘negative’ impacts or challenges you have faced”
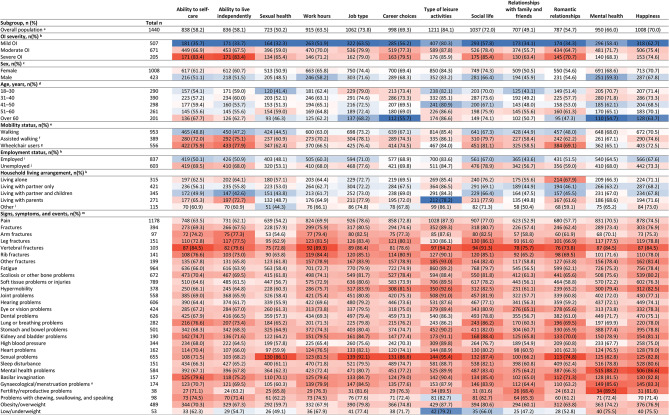
Fig. 2.
Heatmap of impact of OI (ranging from “very mildly” to “severely” impacted) on quality of life of adults with OI (n = 1,440). Proportions in parentheses are based on category totals. Colours indicate differences to the overall population. Subgroups with similar values to the overall population are shown in white, with greater proportions in red and smaller proportions in blue. Abbreviations: OI, osteogenesis imperfecta. aQuestions 102 & 106 “In the past 12 months, how would you describe the impact that OI has had on your life?”, where respondents received the following instructions: “This question is about understanding the ‘negative’ impacts or challenges you have faced”; bQuestion 18 “How would you describe the severity of your OI?”; cQuestion 8 “What is your sex?”; dQuestion 1 “What is your age?”; eQuestion 16 “How do you get around”; f“Assisted walking” includes the use of walking sticks/canes, walking frames, rollators or crutches; g“Wheelchair users” includes the use of manual wheelchairs, powered wheelchairs or mobility scooters; hQuestion 9 “Please indicate which of the following best describe you”; i“Employed” includes respondents who answered “I am in paid employment/self-employed”; j“Unemployed” includes retirees, students, homemakers and volunteers; kQuestions 11 & 12 “Who do you live with?“, multiple answer options possible; l“Other” includes single parents, living with friends or house share, living with caregiver or assistant, and living in supported living accommodation or a care home; mQuestion 113 “Over the past 12 months, have you experienced any of the following signs, symptoms, or events?“; nPopulation potentially affected by gynaecological/menstruation problems include female respondents only
Among those with severe OI, at least 65% of adults were affected in each QoL area investigated. Compared with the overall cohort of adults with OI, a greater proportion of those with severe OI were severely impacted by their OI across QoL areas. OI impacted the romantic relationships of 37% of adults with severe OI, compared to 5% of the overall cohort of adults with OI (Fig. 2, Supplementary Material 5).
Some adults provided free-text responses on the positive impacts of OI on their lives, including developing positive personality traits, such as being more empathetic or resilient and feeling a sense of community.
Drivers of impact of OI on QoL
In each QoL domain (Table 1), several demographics and clinical characteristics were identified as drivers, though not all were common across all domains or levels of impact (graphs showing the results from the regression analysis can be found in Supplementary Material 6, 7, 8 and 9, and relative risk ratios in Supplementary Material 10). However, we observed trends across QoL domains, where certain demographics or clinical characteristics were consistently identified as drivers of impact on QoL.
Drivers of impact on physical well-being and functioning
Various drivers were identified for impact of OI on physical QoL (Supplementary Material 6A–H). Self-reported OI severity, mobility status, and fracture frequency were consistently identified as drivers of OI impact on physical QoL across varying degrees of impact. For example, adults with self-reported moderate or severe OI were more likely to experience a mild to severe impact on their physical health compared with adults with mild OI; those with severe OI were 12.6 times (RRR, P < 0.001) more likely to experience a severe impact on their ability to self-care than those with mild OI (Supplementary Material 6A). Mobility status was also identified as a driver of ability to self-care. Individuals who used mobility aids were 1.5 times (RRR, P < 0.05) more likely to experience a moderate impact on their ability to self-care than those who did not, and those who used wheelchairs were 2.6 times (RRR, P < 0.05) more likely to experience a severe impact on their ability to self-care than those who did not (Supplementary Material 6F). Additionally, those who experienced multiple fractures were more likely to experience a severe impact on their physical health than those who did not fracture. For instance, adults who fractured twice (RRR 3.6, P < 0.05) or more often (RRR 3.9, P < 0.001) in the past 12 months were more likely to experience a severe impact on their sexual health than those who did not fracture (Supplementary Material 6D).
Drivers of impact on social life and relationships
Self-reported OI severity was consistently identified as a driver of impact on social QoL (Supplementary Material 7A). For instance, individuals with severe OI were 16.5 times (RRR, P < 0.001) more likely to experience a severe impact on social life than those with mild OI. Adults over the age of 30 were more likely to report a moderate impact on relationships with family and friends compared with 18- to 30-year-olds, and female respondents were less likely (RRR 0.6, P < 0.05) to experience a severe impact on their romantic relationships than male respondents (Supplementary Material 7B–C). Nonetheless, the impact of age and sex were inconsistent across social QoL areas.
Drivers of impact on careers and finances
Self-reported OI severity and higher fracture frequency were consistently identified as drivers of impact on careers (Supplementary Material 8A and D). For instance, those who experienced three or more fractures were more likely to report any degree of impact on the number of hours they could work than those who did not fracture (Supplementary Material 8D). Furthermore, individuals who experienced pain were 4.1 (RRR, P < 0.001) times more likely to report a severe impact on their work hours than those who did not (Supplementary Material 8E).
Drivers of impact on mental health and well-being
In line with findings across other QoL domains, self-reported OI severity and fracture frequency were consistently identified as drivers of OI impact on mental health and happiness (Supplementary Material 9A and D). For instance, those who experienced three or more fractures were 2.6 times (RRR, P < 0.05) more likely to experience a severe impact on their mental health than those who did not fracture (Supplementary Material 9D). Female respondents were 1.6 times (RRR, P < 0.05) more likely to experience a moderate impact on mental health than male respondents. Other levels of impact (“severely”, “mildly”, and “very mildly” impacted) were comparable between male and female respondents (Supplementary Material 9C).
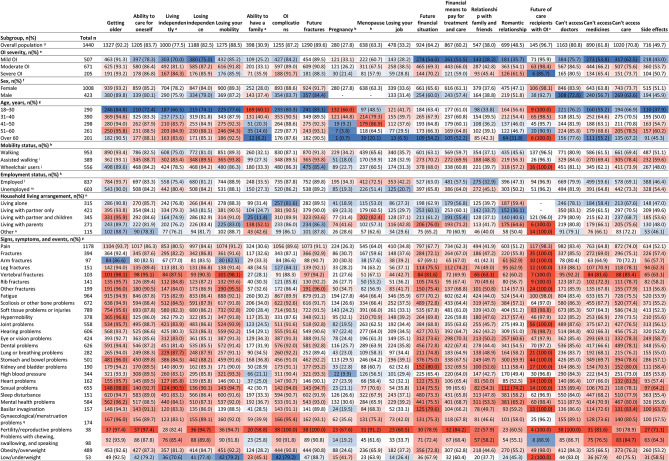
OI-linked worries and concerns
The degree to which adults with OI worried varied depending on the circumstance queried (Table 3). Over half of adults worried a lot about mobility loss (53%), future fractures (48%), and ageing (48%). Areas of lower concern included relationships with family and friends (10%) and job security (14%; Table 3; Figs. 3 and 4, Supplementary Material 11).
Table 3.
Degree of worry about the listed circumstances of adults with OI (n = 1,440)
| Degree of worry, n (%) a | Worry a lot | Worry a little | Don’t worry | Not applicable | I don’t know | Prefer not to say |
|---|---|---|---|---|---|---|
| Getting older | 690 (47.9) | 637 (44.2) | 91 (6.3) | 11 (0.8) | 9 (0.6) | 2 (0.1) |
| Ability to care for oneself | 624 (43.3) | 581 (40.3) | 201 (14.0) | 24 (1.7) | 7 (0.5) | 3 (0.2) |
| Living independently b | 479 (37.1) | 521 (40.4) | 246 (19.1) | 32 (2.5) | 9 (0.7) | 3 (0.2) |
| Losing independence | 679 (47.2) | 509 (35.3) | 206 (14.3) | 30 (2.1) | 11 (0.8) | 5 (0.3) |
| Losing mobility | 768 (53.3) | 507 (35.2) | 140 (9.7) | 16 (1.1) | 7 (0.5) | 2 (0.1) |
| Ability to have a family b | 210 (16.3) | 188 (14.6) | 426 (33.0) | 408 (31.6) | 30 (2.3) | 28 (2.2) |
| OI complications | 604 (41.9) | 651 (45.2) | 150 (10.4) | 15 (1.0) | 17 (1.2) | 3 (0.2) |
| Future fractures | 696 (48.3) | 594 (41.3) | 133 (9.2) | 8 (0.6) | 5 (0.3) | 4 (0.3) |
| Pregnancy c | 182 (18.1) | 98 (9.7) | 220 (21.8) | 472 (46.8) | 17 (1.7) | 19 (1.9) |
| Menopause c | 322 (31.9) | 316 (31.3) | 199 (19.7) | 140 (13.9) | 23 (2.3) | 8 (0.8) |
| Losing a job | 202 (14.0) | 276 (19.2) | 517 (35.9) | 378 (26.3) | 44 (3.1) | 23 (1.6) |
| Future financial situation | 411 (28.5) | 513 (35.6) | 426 (29.6) | 68 (4.7) | 10 (0.7) | 12 (0.8) |
| Financial means to pay for treatment and care | 422 (29.3) | 445 (30.9) | 456 (31.7) | 104 (7.2) | 9 (0.6) | 4 (0.3) |
| Impact on relationships with family and friends | 149 (10.3) | 398 (27.6) | 796 (55.3) | 77 (5.3) | 15 (1.0) | 5 (0.3) |
| Impact on romantic relationships | 276 (19.2) | 423 (29.4) | 568 (39.4) | 119 (8.3) | 26 (1.8) | 28 (1.9) |
| Future of care recipients with OI d | 94 (62.7) | 51 (34.0) | 4 (2.7) | 0 (0.0) | 0 (0.0) | 1 (0.7) |
| Access to doctors | 673 (46.7) | 490 (34.0) | 258 (17.9) | 15 (1.0) | 4 (0.3) | 0 (0.0) |
| Access to medicines | 404 (28.1) | 486 (33.8) | 470 (32.6) | 61 (4.2) | 18 (1.3) | 1 (0.1) |
| Access to care | 495 (34.4) | 525 (36.5) | 373 (25.9) | 34 (2.4) | 7 (0.5) | 6 (0.4) |
| Side effects of treatment | 298 (20.7) | 418 (29.0) | 425 (29.5) | 277 (19.2) | 18 (1.3) | 4 (0.3) |
Abbreviations: OI, osteogenesis imperfecta
aQuestions 103, 104, 105, 107, 108, & 109 “Do you feel worried or concerned about any of the following things?“; bThese answer options were only given to adults with OI who did not have any care recipients with OI (n = 1,290); cPopulation potentially affected by pregnancy and menopause include female respondents only (n = 1,008); dThis answer option was only given to adults with OI who are caregivers for individuals with OI (n = 150)
Fig. 3.
The reported degree of worry about the listed circumstances of adults with OI, displayed as a stacked bar graph of percentages (n = 1,440). Abbreviations: OI, osteogenesis imperfecta. This graph is based on the responses to questions 103, 104, 105, 107, 108, & 109 “Do you feel worried or concerned about any of the following things?”. The answer options “Living independently” and “Ability to have a family” were only given to adults with OI who did not have any care recipients with OI (n = 1,290). Population potentially affected by pregnancy and menopause include female respondents only (n = 1,008). The answer option “Worrying about future of care recipients with OI” was only given to adults with OI who are caregivers for individuals with OI (n = 150)
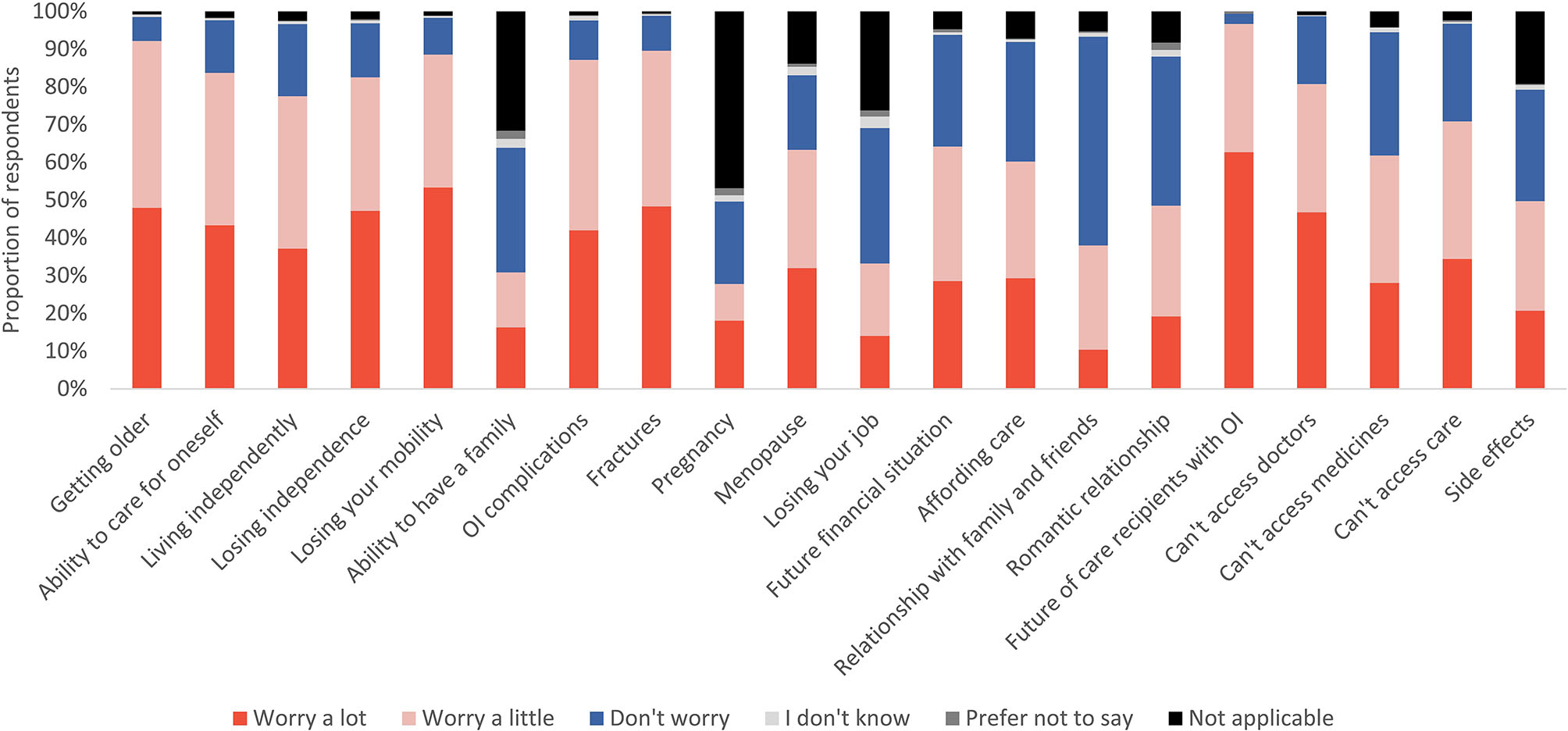
Fig. 4.
Heatmap showing proportion of adults who worry a lot or a little about the listed circumstances (n = 1,440). Proportions in parentheses are based on category totals. Colours indicate differences to the overall population. Subgroups with similar values to the overall population are shown in white, with greater proportions in red and smaller proportions in blue. Abbreviations: OI, osteogenesis imperfecta. aOnly adults without care recipients with OI (n = 1,290) were provided with the answer options “Living independently” and “Ability to have a family”; bPopulation potentially affected by pregnancy and menopause include female respondents only (n = 1,008); cOnly caregivers with OI (n = 150) were provided with the answer option “Worrying about future of care recipients with OI”; dQuestions 103, 104, 105, 107, 108 & 109 “Do you feel worried or concerned about any of the following things?”; eQuestion 18 “How would you describe the severity of your OI?”; fQuestion 8 “What is your sex?”; gQuestion 1 “What is your age?”; hQuestion 16 “How do you get around”; i“Assisted walking” includes the use of walking sticks/canes, walking frames, rollators or crutches; j“Wheelchair users” includes those who use manual wheelchairs, powered wheelchairs or mobility scooters; kQuestion 9 “Please indicate which of the following best describe you”; l“Employed” includes respondents who answered “I am in paid employment/self-employed”; m“Unemployed” includes retirees, students, homemakers and volunteers; nQuestions 11 & 12 “Who do you live with?”, multiple answer options possible; o“Other” includes single parents, living with friends or house share, living with caregiver or assistant, and living in supported living accommodation or a care home; pQuestion 113 “Over the past 12 months, have you experienced any of the following signs, symptoms, or events?”; qPopulation potentially affected by gynaecological/menstruation problems include female respondents only
Similar proportions of those with severe OI worried about various aspects of living compared with the overall cohort of adults with OI. However, smaller proportions of adults with severe OI worried about pregnancy (21% vs. 28% of the overall cohort) or the future of their care recipients with OI (86% of caregivers with severe OI vs. 97% of the overall cohort of caregivers). Greater proportions of adults with severe OI worried about their romantic relationships (61%) compared with the overall cohort of adults with OI (49%; Fig. 4, Supplementary Material 12).
Drivers of worries and concerns
Various drivers were identified for worrying about different areas of respondents’ lives (graphs showing the results of the regression analysis can be found in Supplementary Material 13, 14, 15, and 16 and relative risk ratios in Supplementary Material 17). As was the case for QoL, self-reported OI severity was also identified as a driver of OI-linked worries (“worry a little” or “worry a lot”). Across various areas of their lives, adults with self-reported moderate or severe OI were more likely to report worrying than those with mild OI. For example, those with severe OI were 5.8 (RRR, P < 0.001) times more likely to worry a lot about getting older and 8.6 (RRR, P < 0.001) times more likely to worry a lot about their romantic relationships than those with mild OI (Supplementary Material 13A and 14A). Compared to 18- to 30-year-olds, older respondents were more likely to worry (“a lot” and “a little”) about physical well-being and functioning (Supplementary Material 13B).
Discussion
With data compiled from 1,440 adults, the IMPACT Survey is the most extensive patient-reported dataset on the experience of individuals with OI to date. This report provides insights into the humanistic impact of OI on adults across physical, socioeconomic, and mental well-being QoL domains. Irrespective of demographic and clinical characteristics, most adults experienced an impact on their lives and were worried or concerned about their future.
Impact of OI on QoL across all areas
Sex, mobility status, household living arrangement, employment status, and clinical signs, symptoms, and events were significantly associated with impact on various areas of QoL. However, there was no clear trend: these drivers were not consistently significantly associated across multiple degrees of impact or QoL domains. On the other hand, we found that self-reported OI severity and fracture frequency were consistent drivers of impact on QoL across multiple degrees of impact and QoL domains.
Previous studies identified a correlation between OI severity and QoL impairment, where increased OI severity was correlated with lower QoL [13, 40]. These findings align with the findings of the present study. Additionally, previous studies report that fracture rates are higher in children than in adults with OI [41] but that fracture incidence rates in adults with OI [42] remain higher than in the general population [41, 43]. In adults with OI, fractures impact daily life and emotional well-being [44], with widespread and long-lasting effects on QoL [27, 45]. Fractures can also impair physical function [27], especially in individuals who use mobility aids or those with more severe OI [46]. Our findings suggest that the use of mobility aids and wheelchairs is a driver of impact on ability to self-care. They also suggest that OI severity is a driver of impact on QoL across all areas. Notably, the impact of fractures can extend past physical effects. In previous research, children and adults with OI have reported anxiety about future fractures [47]. This aligns with the results from our study, which found that 90% of adults worried about fractures “a lot” or “a little”.
Impact of OI on the ability to self-care
Over half of the respondents (58%) reported that OI impacted their ability to self-care (ranging from “very mild” to “severe” impact, with 24% reporting a moderate to severe impact). Older individuals in the general population often report a diminished ability to self-care [48, 49]; studies link the ability to self-care to life satisfaction or happiness [50, 51]. In our study, both younger and older adults reported that their ability to self-care was impacted. In addition, similar proportions of younger and older adults worried (either “a lot” or “a little”) about their ability to self-care, highlighting the challenges faced by adults with OI over their lifetimes. Deterioration of an individual’s ability to self-care may happen earlier in life for individuals with OI compared with the general population. These effects may be exacerbated in individuals with OI who use mobility aids, as supported by our findings, which suggest that the use of mobility aids and wheelchairs are drivers of impact on ability to self-care.
Impact of OI on social life and relationships
Around half of adults reported an impact (ranging from “very mild” to “severe” impact) on their relationships with family and friends (49%) and romantic relationships (55%). Furthermore, many adults worried (either “a lot” or “a little”) about their relationships with family and friends (38%) and romantic relationships (49%). Strong interpersonal relationships have been shown to play a crucial role in the overall well-being of the general population [52]. Additionally, social support has been linked to well-being in individuals with chronic illnesses [53]. Chronic illness can strain relationships for various reasons [54] and may affect family dynamics [55]. Individuals with OI may face physical limitations hindering social activities due to health issues linked to OI, such as fractures and hearing loss. Studies have also identified a relationship between disabling barriers and loneliness or social isolation among people with disabilities [56–59]. In addition to the effects of disability, some groups, such as men and older adults, are more likely to experience loneliness [60] and less likely to form intimate friendships [61]. Similarly, our study found that adults with more severe OI, males and older adults (over 60 years) were more likely to experience a severe impact on their relationships. Past research has found worse QoL in older adults with OI [12, 17, 62].
Impact of OI on careers and finances
Over 60% of the adults in our survey reported an impact on their careers and finances. We previously reported that adults with OI missed 1.7 workdays (average) and spend €191 out-of-pocket (average over categories including medicine, physiotherapy, and personal care) over 4 weeks due to their OI [38]. In this report, we identified fractures and pain as drivers of impact on careers. Previous studies have found that chronic pain can negatively impact careers. For example, chronic pain was found to be associated with reduced work performance and negatively correlated with employment retention [63, 64]. Pain is commonly experienced by individuals with OI and can affect QoL [17, 33, 34, 62, 65]. Experiencing fractures can also affect careers among the general population by physically hindering individuals’ ability to work, resulting in lost work hours and, in some cases, preventing a return to work after fracturing [66, 67].
Impact of OI on mental health
In our survey, 66% of adults reported that OI impacts their mental health (ranging from “very mild” to “severe” impact, with 30% reporting a moderate to severe impact). In the IMPACT Survey sample, 40% of participants reported experiencing mental health problems in the past 12 months. Since our survey was fielded in 2021, the COVID-19 pandemic may have resulted in respondents reporting a greater prevalence of mental health problems compared with other years, as was observed in the general population [68].
Despite the impact of the pandemic on mental health, a prevalence of around 40% is in line with the literature on mental health in chronic illness. One review of 29 studies representing 16,000 people with diabetes, obesity, cancer, COPD, or heart disease estimated that the prevalence of anxiety or depression among individuals with chronic illnesses was 36.6% [69]. Furthermore, previous studies have found associations between mental health problems and chronic illness [70]. While OI impacted the mental health of most adults in our survey, some individuals were more impacted than others. Mental health problems were commonly reported by those who experienced any fractures (73%) or vertebral fractures (84%) in the past 12 months.
Impact of OI on attitudes and outlook on life
Our study, like others on chronic illnesses, may not fully reflect the true impact of OI on QoL. Previous reports indicate that symptom underreporting, which may be influenced by factors such as stigma and denial [71, 72], could affect the reported impact of chronic illnesses on QoL. Additionally, studies have found that living with a chronic illness may build resilience and impart a tendency towards stoicism [73]; both are positively associated with better QoL [74, 75]. Resilience was reported in free text responses in our study, demonstrating the adversity that individuals with OI may have to cope with. Some adults also reported an increased sense of empathy and positive impacts on their social life and careers when they found friends, partners, or career opportunities through OI networks. Participation in patient networks was reported to impact QoL positively, through community events and support groups, which highlights the importance of patient groups.
Implications and future research directions
Particular attention needs to be paid to the broader implications of fractures on individuals with OI to improve their QoL. By focusing resources on fracture prevention and pain relief, the careers and productivity of adults with OI may be improved. Furthermore, workplace accommodations, such as the option to work remotely, could help to reduce the negative impact of OI on careers. Working remotely has previously been reported to have a positive impact on well-being for people with disabilities [76]. While OI is associated with a significant impact on various aspects of adults’ lives, there remains a need for more nuanced understanding of the factors driving its impact on QoL. Further studies that collect data on a representative sample from lower-income countries will help address the relationship between poverty and the impact of OI on QoL. Exploring the underlying factors influencing independence and the ability to self-care would provide a more comprehensive understanding of how to address the impact of OI on QoL. Investigating additional potential drivers of impact on QoL, such as economic status, may help identify areas for targeted interventions to improve the lives of adults with OI. This will be aided by a better understanding of the complex relationship between OI and QoL.
Strengths and limitations
Our survey has collated the largest sample of respondents with OI and their caregivers to date [37], and it covers a breadth of topics that have not been previously explored in such detail. To ensure that the survey explored topics of interest to the community, this survey was conducted with input from OI experts and members of the OI community. QoL questions were bespoke to the survey and were reviewed by OI experts and members of the OI community.
The impact of COVID-19 may have led to more negative responses about QoL, worries and concerns. Among the general population, the pandemic and lockdowns affected the social life, leisure activities, careers, and mental health of many individuals [77]. The OI population reported heightened anxiety due to the pandemic [78].
Our survey did not collect data from the general population, which precludes comparison. Direct age-matched controls would improve the reliability of QoL research. Furthermore, our study cohort is not representative of the global OI population. This is due to increased engagement of certain groups, such as females, individuals with more severe OI, and individuals from Europe and the United States. This is typically seen in other surveys. However, despite the rarity of the condition, a large number of respondents engaged with the survey, enabling the collection of a substantial amount of data on underrepresented groups.
This work did not use any validated QoL tools, which may affect the validity of responses. However, since OI is a rare disease, using validated tools may have led to an incomplete understanding of the disease burden by not capturing the unique aspects of the impact of OI on QoL. Recall bias may have also affect our results, as the survey collected self-reported data. However, data on QoL reported by individuals with OI provides unique and specific insights into the experience of those living with OI.
Conclusion
Data from the IMPACT Survey suggest that OI strongly impacts the lives of adults across all investigated QoL domains (physical, socioeconomic, and mental well-being), regardless of demographics and clinical characteristics. Across several areas, more severe self-reported OI and increased fracture frequency were identified as drivers of impact of OI on QoL and OI-linked worries and concerns. Fractures impact the QoL of adults with OI, which highlights the need for improved prevention efforts in adults.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank members of the OIF and OIFE for their participation in the development and dissemination of the IMPACT Survey. We are also grateful for every respondent taking the time to participate and provide information for this research. Authors further thank Michael B Bober, formerly of Alfred I. duPont Hospital, for his significant contributions in planning and reviewing the proposed survey content. Furthermore, the authors would like to thank Maria Rapoport and Alysia Battersby, of Wickenstones, who helped to analyse the data presented here.
Author contributions
IW, TH, TvW, LLW, OS, CR, SP, and FR contributed to the planning of this research. SP drafted and implemented survey questions. IW, TH, TvW, LLW, OS, CR, and FR reviewed the proposed survey content. LD analysed data and drafted the manuscript. IW, TH, TvW, LLW, OS, CR, RD, SP, and FR contributed to the planning of the manuscript, reviewed the work, provided revisions and final approval for the publication of this version of the manuscript. All authors read and approved the final manuscript.
Funding
Funding for this research was provided by Mereo BioPharma Group, London, United Kingdom.
Data availability
Relevant data is provided within the manuscript or supplementary information files. Further data that support the findings of this study are not openly available due to reasons of sensitivity. They are managed by a data management committee and are available upon reasonable request to the authors (impactsurvey@wickenstones.com). Specific data requests can be made on the IMPACT Survey website: https://www.impactsurveyoi.com/.
Declarations
Ethics approval and consent to participate
An ethics approval exemption was granted by Pearl IRB, Indianapolis, IN, USA on 23rd June 2021. The survey protocol is in line with the UK Research Integrity Office’s guidance on good practice in internet-mediated research [79].This online survey was anonymous and did not collect any identifiable data on individuals. Participants were provided with a data privacy statement and consented for their responses to be analysed.
Consent for publication
Not applicable.
Competing interests
LD and RD are employees of Wickenstones Ltd, Oxford, United Kingdom. SP is an employee of Mereo BioPharma Group, London, United Kingdom. At the time of the survey design and development of this report, SP was an employee of Wickenstones Ltd. CR has received payments for their contributions to the present manuscript. TH serves as the Chief Executive Officer of the Osteogenesis Imperfecta Foundation, which has received unrestricted educational grants from Mereo BioPharma Group London, United Kingdom and Ultragenyx Pharmaceuticals Inc, Novato, USA. OS has participated in a national advisory board for Mereo BioPharma Group London, United Kingdom and has received study contracts for clinical studies from Ultragenyx Pharmaceuticals Inc, Novato, USA. FR has received study contracts for experimental preclinical studies with Precithera Inc, Quebec, Canada, Mesentech Inc, Vancouver, Canada and Catabasis Pharmaceuticals Inc, Cambridge, USA. He has participated in advisory boards for Ultragenyx Pharmaceuticals Inc, Novato, USA, Sanofi S.A. Paris, France, Novartis International AG, Basel, Switzerland and Mereo BioPharma Group, London, United Kingdom. FR has received a speaker fee from Ultragenyx Pharmaceuticals Inc, Novato, USA for a lecture and received a donation of experimental drugs for a preclinical study from Acceleron Pharma Inc, Cambridge, USA. CR received an institutional grant from and has been a speaker for BioMarin Pharmaceuticals Inc, Novato, California, has participated in advisory boards for Ultragenyx Pharmaceuticals Inc, Novato, USA. She has received an institutional grant from and is a consultant for Nextcure, Beltville, MD, USA. CR sits on the board of directors of the Osteogenesis Imperfecta Foundation. CR has also participated in an advisory board for Mereo BioPharma Group, London, United Kingdom. TW and IW hold leadership positions in the Osteogenesis Imperfecta Federation Europe, which has received grants from Mereo BioPharma Group, London, United Kingdom (unrestricted), Ultragenyx Pharmaceuticals Inc, Novato, USA (restricted grant for a conference), Quince Therapeutics Inc, San Francisco, CA, USA (donation for a conference), UCB (restricted grant to conference), Angitia Biopharmaceuticals Inc., Woodland Hills, CA, USA (donation to conference), Azafaros BV, Naarden, the Netherlands (donation to conference), Alexion Inc. Boston, MA, USA, (sponsorship of conference); Pega Medical Inc, Laval, Quebec, Canada (donation), PuREC, Shimane, Japan (sponsorship of conference), Takeda, Tokyo, Japan (payment to IW as a panellist; donated to OIFE).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bregou Bourgeois A, Aubry-Rozier B, Bonafe L, Laurent-Applegate L, Pioletti DP, Zambelli PY. Osteogenesis imperfecta: from diagnosis and multidisciplinary treatment to future perspectives. Swiss Med Wkly. 2016;146:w14322. [DOI] [PubMed] [Google Scholar]
- 2.Marini JC, Forlino A, Bachinger HP, Bishop NJ, Byers PH, Paepe A, et al. Osteogenesis imperfecta. Nat Reviews Disease Primers. 2017;3:17052. [DOI] [PubMed] [Google Scholar]
- 3.Folkestad L. Mortality and morbidity in patients with osteogenesis imperfecta in Denmark. Dan Med J. 2018;65(4). [PubMed]
- 4.Bishop N, Osteogenesis Imperfecta. 2021. https://www.orpha.net/consor/cgi-bin/Disease_Search.php?lng=EN%26data_id=654%26Disease_Disease_Search_diseaseGroup=osteogenesis-imperfecta%26Disease_Disease_Search_diseaseType=Pat%26Disease(s)/group%2520of%2520diseases=Osteogenesis-imperfecta%26title=Osteogenesis%2520imperfecta%26search=Disease_Search_Simple. Accessed on: 20 March 2024
- 5.Marr C, Seasman A, Bishop N. Managing the patient with osteogenesis imperfecta: a multidisciplinary approach. J Multidisciplinary Healthc. 2017;10:145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Botor M, Fus-Kujawa A, Uroczynska M, Stepien KL, Galicka A, Gawron K et al. Osteogenesis imperfecta: current and prospective therapies. Biomolecules. 2021;11(10). [DOI] [PMC free article] [PubMed]
- 7.Tauer JT, Robinson ME, Rauch F. Osteogenesis Imperfecta: New perspectives from clinical and translational research. JBMR Plus. 2019;3(8):e10174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dwan K, Phillipi CA, Steiner RD, Basel D. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev. 2016;10(10):CD005088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho TJ, Ko JM, Kim H, Shin HI, Yoo WJ, Shin CH. Management of osteogenesis imperfecta: a multidisciplinary comprehensive approach. Clin Orthop Surg. 2020;12(4):417–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orwoll ES, Shapiro J, Veith S, Wang Y, Lapidus J, Vanek C, et al. Evaluation of teriparatide treatment in adults with osteogenesis imperfecta. J Clin Investig. 2014;124(2):491–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rapoport M, Bober MB, Raggio C, Wekre LL, Rauch F, Westerheim I, et al. The patient clinical journey and socioeconomic impact of osteogenesis imperfecta: a systematic scoping review. Orphanet J Rare Dis. 2023;18(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gooijer K, Harsevoort AGJ, van Dijk FS, Withaar HR, Janus GJM, Franken AAM. A baseline measurement of quality of life in 322 adults with osteogenesis imperfecta. JBMR Plus. 2020;4(12):e10416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hald JD, Folkestad L, Harslof T, Brixen K, Langdahl B. Health-related quality of life in adults with osteogenesis imperfecta. Calcif Tissue Int. 2017;101(5):473–8. [DOI] [PubMed] [Google Scholar]
- 14.Widmann RF, Laplaza FJ, Bitan FD, Brooks CE, Root L. Quality of life in osteogenesis imperfecta. Int Orthop. 2002;26(1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wekre LL, Froslie KF, Haugen L, Falch JA. A population-based study of demographical variables and ability to perform activities of daily living in adults with osteogenesis imperfecta. Disabil Rehabil. 2010;32(7):579–87. [DOI] [PubMed] [Google Scholar]
- 16.Aubry-Rozier B, Richard C, Unger S, Hans D, Campos-Xavier B, Schneider P, et al. Osteogenesis Imperfecta: towards an individualised interdisciplinary care strategy to improve physical activity and quality of life. Swiss Med Wkly. 2020;150:w20285. [DOI] [PubMed] [Google Scholar]
- 17.Forestier-Zhang L, Watts L, Turner A, Teare H, Kaye J, Barrett J, et al. Health-related quality of life and a cost-utility simulation of adults in the UK with osteogenesis imperfecta, X-linked hypophosphatemia and fibrous dysplasia. Orphanet J Rare Dis. 2016;11(1):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKiernan FE. Musculoskeletal manifestations of mild osteogenesis imperfecta in the adult. Osteoporos Int J Estab Result Cooperation Between Eur Foundation Osteoporos Natl Osteoporos Foundation USA. 2005;16(12):1698–702. [DOI] [PubMed]
- 19.Feehan AG, Zacharin MR, Lim AS, Simm PJ. A comparative study of quality of life, functional and bone outcomes in osteogenesis imperfecta with bisphosphonate therapy initiated in childhood or adulthood. Bone. 2018;113:137–43. [DOI] [PubMed] [Google Scholar]
- 20.Yonko EA, Emanuel JS, Carter EM, Sandhaus RA, Raggio CL. Respiratory impairment impacts QOL in Osteogenesis Imperfecta independent of skeletal abnormalities. Archives Osteoporos. 2020;15(1):153. [DOI] [PubMed] [Google Scholar]
- 21.Kruger KM, Caudill A, Rodriguez Celin M, Nagamani SCS, Shapiro JR, Steiner RD, et al. Mobility in osteogenesis imperfecta: a multicenter north American study. Genet Medicine: Official J Am Coll Med Genet. 2019;21(10):2311–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saeves R, Wekre L, Ambjornsen E, Axelsson S, Nordgarden H, Storhaug K. Oral findings in adults with osteogenesis imperfecta. Special care Dentistry: Official Publication Am Association Hosp Dent Acad Dentistry Handicapped Am Soc Geriatric Dentistry. 2009;29(2):102–8. [DOI] [PubMed] [Google Scholar]
- 23.Bendixen KH, Gjorup H, Baad-Hansen L, Dahl Hald J, Harslof T, Schmidt MH, et al. Temporomandibular disorders and psychosocial status in osteogenesis imperfecta - a cross-sectional study. BMC Oral Health. 2018;18(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gjorup H, Beck-Nielsen SS, Hald JD, Haubek D. Oral health-related quality of life in X-linked hypophosphataemia and osteogenesis imperfecta. J Rehabil. 2021;48(2):160–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orlando G, Pinedo-Villanueva R, Reeves ND, Javaid MK, Ireland A. Physical function in UK adults with osteogenesis imperfecta: a cross-sectional analysis of the RUDY study. Osteoporosis Int J Estab Result Cooperation Between Eur Found Osteoporosis National Osteoporosis Foundation USA. 2021;32(1):157–64. [DOI] [PubMed]
- 26.Folkestad L, Hald JD, Hansen S, Gram J, Langdahl B, Abrahamsen B, et al. Bone geometry, density, and microarchitecture in the distal radius and tibia in adults with osteogenesis imperfecta type I assessed by high-resolution pQCT. J Bone Min Res Off J Am Soc Bone Mineral Res. 2012;27(6):1405–12. [DOI] [PubMed] [Google Scholar]
- 27.Matsushita M, Mishima K, Yamashita S, Haga N, Fujiwara S, Ozono K, et al. Impact of fracture characteristics and disease-specific complications on health-related quality of life in osteogenesis imperfecta. J Bone Miner Metab. 2020;38(1):109–16. [DOI] [PubMed] [Google Scholar]
- 28.Bronheim R, Khan S, Carter E, Sandhaus RA, Raggio C. Scoliosis and cardiopulmonary outcomes in osteogenesis imperfecta patients. Spine. 2019;44(15):1057–63. [DOI] [PubMed] [Google Scholar]
- 29.Balkefors V, Mattsson E, Pernow Y, Saaf M. Functioning and quality of life in adults with mild-to-moderate osteogenesis imperfecta. Physiotherapy Res Int J Res Clin Phys Therapy. 2013;18(4):203–11. [DOI] [PubMed] [Google Scholar]
- 30.Khan SI, Yonko EA, Carter EM, Dyer D, Sandhaus RA, Raggio CL. Cardiopulmonary status in adults with Osteogenesis imperfecta: intrinsic lung disease may contribute more than scoliosis. Clin Orthop Relat Res. 2020;478(12):2833–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Widmann RF, Bitan FD, Laplaza FJ, Burke SW, DiMaio MF, Schneider R. Spinal deformity, pulmonary compromise, and quality of life in osteogenesis imperfecta. Spine. 1999;24(16):1673–8. [DOI] [PubMed] [Google Scholar]
- 32.Nicolaou N, Bowe JD, Wilkinson JM, Fernandes JA, Bell MJ. Use of the Sheffield telescopic intramedullary rod system for the management of osteogenesis imperfecta: clinical outcomes at an average follow-up of nineteen years. J Bone Joint Surg Am Vol. 2011;93(21):1994–2000. [DOI] [PubMed] [Google Scholar]
- 33.Tosi LL, Oetgen ME, Floor MK, Huber MB, Kennelly AM, McCarter RJ, et al. Initial report of the osteogenesis imperfecta adult natural history initiative. Orphanet J Rare Dis. 2015;10:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tosi LL, Floor MK, Dollar CM, Gillies AP, Members of the Brittle Bone Disease, Hart C et al. TS,. Assessing disease experience across the life span for individuals with osteogenesis imperfecta: challenges and opportunities for patient-reported outcomes (PROs) measurement: a pilot study. Orphanet J Rare Dis. 2019;14(1):23. [DOI] [PMC free article] [PubMed]
- 35.Moshkovich OB, Macey K, Doll J, Hill HA, Hall CL. Development of the OIQoL-A: a health-related quality of life measure for adults with osteogenisis imperfecta. Value Health. 2017;20(9):A538. [Google Scholar]
- 36.Faleiros de Paiva D. Perceptions of people with osteogenesis imperfecta about the interventions of the occupational therapy and its possibilities of care. Brazilian J Occup Therapy. 2018; 26(2)399–407.
- 37.Westerheim I, Hart T, van Welzenis T, Wekre LL, Semler O, Raggio C, et al. The IMPACT survey: a mixed methods study to understand the experience of children, adolescents and adults with osteogenesis imperfecta and their caregivers. Orphanet J Rare Dis. 2024;19(1):128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hart T, Westerheim I, van Welzenis T, Semler O, Raggio C, Rauch F, et al. The IMPACT survey: the economic impact of osteogenesis imperfecta in adults. Orphanet J Rare Dis. 2024;19(1):222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Likert R. A technique for the measurement of attitudes. Archives Psychol. 1932;140:1–55.
- 40.Song Y, Zhao D, Li L, Lv F, Wang O, Jiang Y, et al. Health-related quality of life in children with osteogenesis imperfecta: a large-sample study. Osteoporos Int J Established Result Cooperation Between Eur Foundation Osteoporos Natl Osteoporos Foundation USA. 2019;30(2):461–8. [DOI] [PubMed] [Google Scholar]
- 41.Folkestad L, Hald JD, Ersboll AK, Gram J, Hermann AP, Langdahl B, et al. Fracture rates and fracture sites in patients with osteogenesis imperfecta: a nationwide register-based cohort study. J Bone Min Res. 2017;32(1):125–34. [DOI] [PubMed] [Google Scholar]
- 42.Goudriaan WA, Harsevoort GJ, van Leeuwen M, Franken AA, Janus GJM. Incidence and treatment of femur fractures in adults with osteogenesis imperfecta: an analysis of an expert clinic of 216 patients. Eur J Trauma Emerg Surg. 2020;46(1):165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Munk SA, Harsevoort GJ, Gooijer K, Edens MA, Franken AA, Janus GJM. Incidence and nonunion rates of tibial fractures in adults with osteogenesis imperfecta: a retrospective cohort study of 402 patients with 42 fractures at an expert clinic. BMC Musculoskelet Disord. 2022;23(1):1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hill M, Hammond J, Sharmin M, Lewis C, Heathfield M, Crowe B, et al. Living with osteogenesis imperfecta: a qualitative study exploring experiences and psychosocial impact from the perspective of patients, parents and professionals. Disabil Health J. 2022;15(1):101168. [DOI] [PubMed] [Google Scholar]
- 45.Gold T, Williams SA, Weiss RJ, Wang Y, Watkins C, Carroll J, et al. Impact of fractures on quality of life in patients with osteoporosis: a US cross-sectional survey. J Drug Assess. 2019;8(1):175–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ibrahim NI, Ahmad MS, Zulfarina MS, Zaris S, Mohamed IN, Mohamed N et al. Activities of Daily Living and determinant factors among older adult subjects with lower body fracture after discharge from hospital: a prospective study. Int J Environ Res Public Health. 2018;15(5). [DOI] [PMC free article] [PubMed]
- 47.Tsimicalis A, Denis-Larocque G, Michalovic A, Lepage C, Williams K, Yao TR, et al. The psychosocial experience of individuals living with osteogenesis imperfecta: a mixed-methods systematic review. Qual Life Res. 2016;25(8):1877–96. [DOI] [PubMed] [Google Scholar]
- 48.Tabrizi JS, Behghadami MA, Saadati M, Soderhamn U. Self-care ability of older people living in urban areas of Northwestern Iran. Iran J Public Health. 2018;47(12):1899–905. [PMC free article] [PubMed] [Google Scholar]
- 49.Haveman-Nies A, De Groot LC, Van Staveren WA. Survey in Europe on N, the Elderly: a concerted action S. Relation of dietary quality, physical activity, and smoking habits to 10-year changes in health status in older europeans in the SENECA study. Am J Public Health. 2003;93(2):318–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Türk R, Akkuş Y, Sönmez T. Relationship between self-care ability and happiness in elderly individuals. Cukurova Med J. 2019;44:366–74. [Google Scholar]
- 51.Borg C, Hallberg IR, Blomqvist K. Life satisfaction among older people (65+) with reduced self-care capacity: the relationship to social, health and financial aspects. J Clin Nurs. 2006;15(5):607–18. [DOI] [PubMed] [Google Scholar]
- 52.Grevenstein D, Bluemke M, Schweitzer J, Aguilar-Raab C. Better family relationships––higher well-being: the connection between relationship quality and health related resources. Mental Health Prev. 2019;14:200160. [Google Scholar]
- 53.Luo Z, Zhong S, Zheng S, Li Y, Guan Y, Xu W, et al. Influence of social support on subjective well-being of patients with chronic diseases in China: chain-mediating effect of self-efficacy and perceived stress. Front Public Health. 2023;11:1184711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moensted ML, Lewis S, Willis K, Dubbin L, Rogers A, Smith L. Friendship, connectedness and (in)authenticity for those with chronic illness: trading in one social gain for another. SSM - Qualitative Res Health. 2023;3:100246. [Google Scholar]
- 55.Vanz AP, Felix TM, da Rocha NS, Schwartz IV. Quality of life in caregivers of children and adolescents with osteogenesis imperfecta. Health Qual Life Outcomes. 2015;13(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olsen J. Socially disabled: the fight disabled people face against loneliness and stress. Disabil Soc. 2018;33(7):1160–4. [Google Scholar]
- 57.Macdonald SJ, Deacon L, Nixon J, Akintola A, Gillingham A, Kent J, et al. The invisible enemy’: disability, loneliness and isolation. Disabil Soc. 2018;33(7):1138–59. [Google Scholar]
- 58.Tough H, Brinkhof MWG, Siegrist J, Fekete C. The impact of loneliness and relationship quality on life satisfaction: a longitudinal dyadic analysis in persons with physical disabilities and their partners. J Psychosom Res. 2018;110:61–7. [DOI] [PubMed] [Google Scholar]
- 59.Gomez-Zuniga B, Pousada M, Armayones M. Loneliness and disability: a systematic review of loneliness conceptualization and intervention strategies. Front Psychol. 2022;13:1040651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ward M, Layte R, Kenny R. Loneliness, social isolation, and their discordance among older adults findings from the Irish longitudinal study. on ageing: TILDA; 2019. [Google Scholar]
- 61.Vigil JM. Asymmetries in the friendship preferences and social styles of men and women. Hum Nat. 2007;18(2):143–61. [DOI] [PubMed] [Google Scholar]
- 62.Arponen H, Waltimo-Siren J, Valta H, Makitie O. Fatigue and disturbances of sleep in patients with osteogenesis imperfecta - a cross-sectional questionnaire study. BMC Musculoskelet Disord. 2018;19(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alleaume C, Bendiane MK, Bouhnik AD, Rey D, Cortaredona S, Seror V, et al. Chronic neuropathic pain negatively associated with employment retention of cancer survivors: evidence from a national French survey. J Cancer Surviv. 2018;12(1):115–26. [DOI] [PubMed] [Google Scholar]
- 64.Kawai K, Kawai AT, Wollan P, Yawn BP. Adverse impacts of chronic pain on health-related quality of life, work productivity, depression and anxiety in a community-based study. Fam Pract. 2017;34(6):656–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Munoz Cortes R, Soriano Pastor JF, Monsalve Dolz V. Chronic pain in adults with osteogenesis imperfecta and its relationship to appraisal, coping, and quality of life: a cross-sectional study. Medicine. 2022;101(40):e30256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Singaram S, Naidoo M. The physical, psychological and social impact of long bone fractures on adults: a review. Afr J Prim Health care Family Med. 2019;11(1):e1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rotondi NK, Beaton DE, Ilieff M, Adhihetty C, Linton D, Bogoch E et al. The impact of fragility fractures on work and characteristics associated with time to return to work. Osteoporosis Int J Established Res Cooperation Between Eur Foundation Osteoporosis Nat Osteoporosis Foundation USA. 2017;28(1):349–58. [DOI] [PubMed]
- 68.Office for National Statistics. Coronavirus and depression in adults, Great Britain: July to August 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsgreatbritain/julytoaugust; 2021. Accessed on: 20 March 2024.
- 69.Dare LO, Bruand PE, Gerard D, Marin B, Lameyre V, Boumediene F, et al. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. 2019;19(1):304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liao B, Xu D, Tan Y, Chen X, Cai S. Association of mental distress with chronic diseases in 1.9 million individuals: a population-based cross-sectional study. J Psychosom Res. 2022;162:111040. [DOI] [PubMed] [Google Scholar]
- 71.Cagle J, Bunting M. Patient reluctance to discuss Pain: understanding stoicism, Stigma, and other contributing factors. J Soc Work End Life Palliat Care. 2017;13(1):27–43. [DOI] [PubMed] [Google Scholar]
- 72.Yong HH. Can attitudes of stoicism and cautiousness explain observed age-related variation in levels of self-rated pain, mood disturbance and functional interference in chronic pain patients? Eur J Pain. 2006;10(5):399–407. [DOI] [PubMed] [Google Scholar]
- 73.Cal SF, Sá LRd, Glustak ME, Santiago MB, Walla P. Resilience in chronic diseases: a systematic review. Cogent Psychol. 2015;2(1):1024928. [Google Scholar]
- 74.Aranguren P. Resilience, pain and quality of life in people with physical disabilities: a systematic review. Eur Psychiatry. 2020;41(S1):S733–S. [Google Scholar]
- 75.Tecson KM, Wilkinson LR, Smith B, Ko JM. Association between psychological resilience and subjective well-being in older adults living with chronic illness. Proc (Bayl Univ Med Cent). 2019;32(4):520–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Allen R, Olsen J, Soorenian A, Verlot M. UK Disability survey research report: Disability Unit; 2021. https://www.gov.uk/government/publications/uk-disability-survey-research-report-june-2021/uk-disability-survey-research-report-june-2021#foreword
- 77.Ferreira LN, Pereira LN, da Fé Brás M, Ilchuk K. Quality of life under the COVID-19 quarantine. Qual Life Res. 2021;30(5):1389–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Smyth D, Hytiris M, Kelday C, McDonnell C, Burren C, Gardner A, et al. Patient-reported experience of clinical care of osteogenesis imperfecta (OI) during the COVID-19 pandemic. Front Public Health. 2022;10:951569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.UK Research Integrity Office. Good practice in research: internet-mediated research; 2016. https://ukrio.org/resources/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Relevant data is provided within the manuscript or supplementary information files. Further data that support the findings of this study are not openly available due to reasons of sensitivity. They are managed by a data management committee and are available upon reasonable request to the authors (impactsurvey@wickenstones.com). Specific data requests can be made on the IMPACT Survey website: https://www.impactsurveyoi.com/.