Abstract
Objective
The effects of exercise on the health of people with Crohn’s disease (CD) remain unclear. This study aimed to explore the perspective of Chinese CD patients on exercise and the quantitative relationship between exercise and patient-reported outcomes.
Methods
This study used a mixed methods design consisting of three components. (1) Big data were mined from social media, and latent Dirichlet allocation (LDA) was used to perform cluster analysis on topics related to physical exercise. (2) A seven-step Colaizzi process was used to conduct semistructured interviews to obtain in-depth information about exercise. (3) A cross-sectional study was performed to examine this relationship using the Global Physical Activity Questionnaire (GPAQ) and Patient-reported Outcome Measurement Information System (PROMIS).
Results
LDA yielded a total of 1536 exercise-related posts; eight topics concerning CD patients were obtained through clustering (peer support, exercise therapy, diet, fatigue, exercise type, intestinal symptoms, body constitution and mental health), and 11 patients were interviewed to validate the results of LDA and explore the insight of Chinese CD. We identified two themes: the effects of exercise on people with CD and factors that promote and hinder exercise. A total of 119 patients with CD were surveyed. Considering confounding factors such as disease activity and medication, moderate-intensity recreational PA increased patients’ physical function and improved anxiety, depression, fatigue, pain intensity, and pain impact (all p < 0.05). In contrast, high-intensity work may lead to anxiety, depression, fatigue, pain, and pain effects (all p < 0.001). In addition, sedentary behaviour may lead to depression (p = 0.006).
Conclusion
Patients with CD tend to seek guidance on exercise through social media, and they generally believe that exercise is beneficial, especially for their psychological and spiritual health, despite difficulties in exercising. Physical activity may be an important factor affecting patients’ psychological health.
Lay summary
Crohn’s disease has a profound impact on mental and emotional health, reducing patients’ quality of life. Exercise is a good habit that can enhance mental, emotional and social health, but there is currently no standard exercise program for patients with Crohn’s disease. The exercise experience of Chinese patients with Crohn’s disease can be helpful in formulating exercise plans.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12876-024-03533-z.
Keywords: Physical activity, Exercise, Crohn’s disease, Patient-reported outcomes, Global physical activity questionnaire
Key Messages
What is already known?
• Studies on Western Crohn’s disease populations have shown that exercise can significantly improve physical fitness and quality of life
• Chinese patients’ attitudes and experiences with exercise are currently unclear.
What is new here?
• Chinese patients with Crohn’s disease actively exchange exercise-related experiences on social media and can obtain support.
• Exercise has a positive impact on patients, but there are still several factors that restrict Chinese patients with Crohn’s disease from exercising.
• Moderate exercise and reducing sedentary behaviour can reduce depression and fatigue and improve physical function.
How can this study help patient care?
• Understanding the exercise attitudes and behaviours of Chinese patients with Crohn’s disease patients can provide personalized support for patients with Crohn’s disease in the Chinese environment.
• This study provides evidence for the development of standardized exercise intervention programs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12876-024-03533-z.
Introduction
Crohn’s disease (CD) is a type of inflammatory bowel disease (IBD) in which uncontrolled inflammation can lead to long-term complications, including fibrosis, intestinal fistulas, and intestinal tumours [1]. Developed countries such as North America and Western Europe have high incidences of CD. The annual incidence rate can reach 29.3/100,000 people [2]. However, in the past 20 years, the incidence of CD in Western countries has remained relatively stable or even decreased, whereas the incidence in Eastern Europe and Asia has shown a continuous increasing trend [3]. More specifically, the incidence of CD has increased drastically in East Asian countries such as China [4], South Korea, and Japan.
The course of CD is characterized by alternating active and remission phases, protracted recovery, and the need for lifelong treatment, all of which seriously affect patients’ quality of life [5]. The aetiology and pathogenesis of this disease remain unclear but are generally believed to be closely related to genetics, immunity, microbiology and the environment [6]. Although drug treatment is currently the most important treatment method, there are still problems with this approach (e.g., low response rates and adverse reactions) [7]. Therefore, an increasing amount of research has been devoted to exploring the potential benefits of lifestyle interventions [8, 9], such as exercise [10], in patients with IBD. Physical exercise (PE) is a planned, organized, repeatable physical activity aimed at improving health or physical fitness [11]. Physical activity (PA) refers to any physical activity generated by the contraction of skeletal muscle activity that increases energy expenditure above the basal metabolic level [12]. PA can be divided into four categories: occupation, transportation, household chores, and leisure [13]. Although the concepts of PA and exercise are different and PE is a type of PA, the two are often used interchangeably in studies. In this article, owing to different purposes and plans, we use both terms.
Currently, there is limited research suggesting that PA may be a protective factor against IBD. Specifically, PA may be especially beneficial for people with CD. Sonnenberg evaluated the occupational distribution of 12,014 IBD patients on the basis of German social security statistics and reported that working in open air and work that involves high levels of PA were protective factors against the onset of IBD, whereas working in air-conditioned environments or working long irregular shifts were risk factors for developing IBD [14]. A prospective cohort study of women in the U.S. also revealed that PA was inversely associated with the risk of CD but not with the risk of UC [15]. A prospective cohort study in the United States compared the correlation between PA levels and disease activity six months later in patients with IBD and revealed that people with CD in remission who had higher PA levels had worse disease activity six months later (OR 0.72, 95% CI 0.55–0.94; p = 0.02) [16]. A cross-sectional survey in the Netherlands revealed a negative correlation between PA levels and disease activity in CD patients (n = 176), but no correlation between PA levels and disease activity was observed in UC patients (n = 162) [17]. Robinson et al. [18] conducted a one-year low-impact exercise program for CD patients for the first time and reported a correlation between the number of exercises and improvement in bone density. Multiple studies have subsequently conducted exercise interventions for CD patients, including resistance exercises [19, 20], endurance exercises (such as walking, running, cycling, etc.) [21–23], and high-intensity interval training, among others. These studies examined the beneficial changes in subjective parameters (psychological, disease acceptance, and quality of life) and objective parameters (body composition, disease activity) associated with exercise in CD patients. Interestingly, most of these results revealed that exercise is beneficial for patients’ psychological problems and emotions, but the improvement in disease activity is weak. This may be due to the dual effects of the proinflammatory and anti-inflammatory effects of exercise [24], and thus far, there is still limited evidence on the mechanism of action of exercise on the gastrointestinal tract. Notably, previous studies have shown that patients who fully comply have better ‘training outcomes‘ [18]. The nature of relapse and remission in patients with Crohn’s disease can be explained by poor adherence, but environmental, cognitive, and social variables also play important roles in exercise behaviour [25]. The current research subjects of exercise programs are mostly Western populations, and there is currently no research on exercise interventions for the Chinese CD population. Therefore, understanding the exercise views of Chinese CD patients is a prerequisite for developing exercise prescriptions tailored to Chinese CD patients to improve exercise intake and maintenance. However, there is currently no standardized exercise protocol for CD patients.
The WHO points out that regular exercise is beneficial for everyone, regardless of age, sex or physical condition [26]. Currently, exercise research focuses mostly on Western populations. Owing to the different cultures, lifestyle habits, and environments of Eastern and Western patients, patients’ exercise preferences may also differ. Currently, no high-quality exercise intervention has been performed among Chinese patients; thus, it is impossible to provide patients with practical exercise recommendations. Some evidence from the Chinese population shows that the implementation of an exercise intervention can reduce the risk of various chronic diseases, including cancer [27] and cardiovascular disease [28]. Furthermore, exercise interventions can improve patient outcomes [29]. However, the impact of physical activity levels on CD patients in China remains unclear.
The internet has improved the convenience and breadth of patients’ access to health information [30]. Social media plays a particularly important role for many people, including adolescents [31], women [32], and college students [33], and has also changed the health information-seeking behaviour of IBD patients [34]. Previous research on social media text data has typically used natural language processing techniques [35]. Although mature technologies ensure the accuracy of data analysis methods, machine analysis lacks linguistic and contextual insight [36]. In addition, identifying the user identities of internet data is difficult, which leads to the inability to identify data from patients and healthy people. Therefore, the accuracy of the content is further questioned. Although interview research provides human language understanding and exploration of text depth, it is often limited by sample size, manpower, and time. Our previous study [37] explored the experiences and perspectives of Chinese CD patients and reported that exercise is one of the topics of concern for Chinese CD patients. However, these conclusions still lack real-world validation. Therefore, in this study, our aim is to further mine text data related to exercise on social media, validate the results on the basis of real-world interviews, and quantify the relationship between exercise habits and patient-reported outcomes.
Methods
Study design and setting
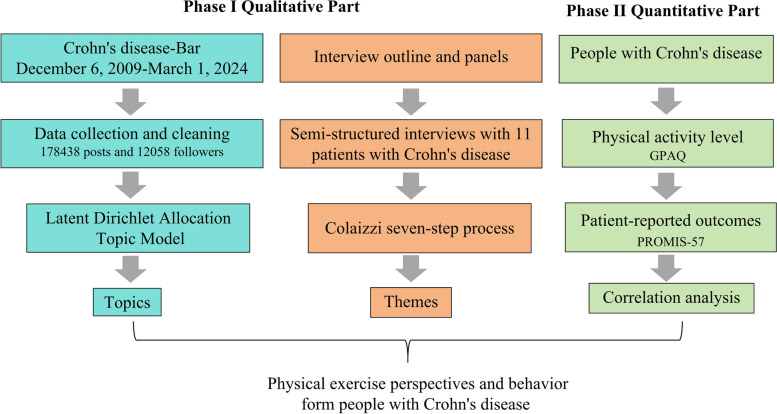
This study was approved by the Ethics Review Board of the First School of Clinical Medicine, Zhejiang Chinese Medical University (No. 2024-KL-261-01). The study was conducted in two phases by using a mixed methods design. In phase I, big data were mined from social media to understand CD patients’ perspectives on exercise, and LDA was used to perform cluster analysis on topics; additionally, semistructured interviews were conducted to perform an in-depth analysis of the research issues from the patient perspective. In phase II, a cross-sectional study was performed to examine the relationship between PA levels and patient-reported outcomes. Although the concepts of “exercise” and PA are different, we use exercise terminology that patients are more familiar with in qualitative research. In cross-sectional surveys, the term PA is used. Phases I and II were performed in accordance with the Standards for Reporting Qualitative Research (SRQR) and the Strengthening the Reporting of the Observational Studies in Epidemiology (STROBE) statement, respectively. The study flow chart is shown in Fig. 1.
Fig. 1.
Flow chart of the study
Phase I – Qualitative Study: CD patients’ perspectives on exercise on social media and the real world
Latent Dirichlet Allocation (LDA)
Baidu Tieba is the largest Chinese online community, consisting of a variety of subcommunities addressing topics. Crohn’s disease-Bar is a subbar of Baidu Tieba and forms a community for CD patients to communicate and discuss [37]. Users can browse posts and express their opinions by registering an account. As of March 1, 2024, the Crohn’s disease-Bar has 178,438 posts and 12,058 followers (Fig. 1). Following our previously described approach [36], we used the Python-based “request” and “selenium” packages [38] to conduct web crawling (a method that extracts target data from web pages) [39]. We collected all text data (including topic posts, user comments and replies) on the Crohn’s disease-Bar. A total of 6,982 topic posts and 178,438 text records (comments and replies) were downloaded. To ensure the quality of the data, we cleaned the data to eliminate blank lines, repeated text, special symbols, numbers and letters. Text with a string length less than 10 was also deleted, and only Chinese strings were retained. We located all exercise-related posts on the basis of several Chinese keywords (“运动”, “锻炼”, “健身”, and “体力活动”), browsed and reviewed all textual data, and retained exercise-related textual data.
LDA is a probability-based topic model algorithm [40, 41]. It assumes that documents are generated on the basis of a certain number of topics and that a given number of topics can be extracted from a corpus containing a certain number of documents [42, 43]. In this study, we used 1536 posts as files for further analysis. Each post is considered a document. In this study, the Python toolkit “Jieba” was first used to segment Chinese sentences into separate words, and second, stop words whose meanings could not be identified in the word segmentation were removed. Finally, we incorporated synonyms and phrases. In short, LDA can perform unsupervised clustering analysis on predefined text data by segmenting sentences and clustering words with similar meanings. Clustering refers to the process of dividing a set of data into several categories on the basis of a certain similarity measure. We went through representative clusters of terms and examined the most representative posts to define the topics.
In LDA, it is important to find the optimal number of topics, as this facilitates the extraction of clear, meaningful, high-quality topics [44]. The selection of the number of topics for LDA is usually based on topic perplexity scores or research area experience. Generally, the lower the level of confusion is, the better the clustering effect; however, this may lead to overfitting of the model. Therefore, work experience and retrospective analysis of the final results are necessary. In this study, we calculate the model perplexity score from 1 to 20 topic numbers to obtain the topic number score and examine the intertopic distance map. Investigator triangulation is applied in this process, where an external researcher analysed the results of different K values and selects the optimal number of topics. In addition, we considered previous experience and peer research results [36]. The three together determine the optimal number of topics. Finally, Gensim [41] was used to implement the LDA model, and “pyLDAvis” was used for visualization.
Qualitative interviews
The interview subjects were CD patients admitted to the Gastroenterology Department of Zhejiang Provincial Hospital of Traditional Chinese Medicine; these patients were selected through convenience and purposive sampling. were selected by convenience and purpose sampling. The inclusion criteria were as follows: diagnosed with CD and able to communicate fluently in Chinese. The sample size was determined by thematic saturation [45]; that is, the recruitment of participants ceased when no new information was obtained. In this study, after the 9th participant was interviewed, the topic reached saturation. After two additional participants were interviewed, no new themes were generated. Thus, we concluded the interviews. Each participant was asked to sign an informed consent form before participating in the study. Participation was voluntary, and all the data were kept confidential. In addition, the participants were assured that they could withdraw from the study at any time.
On the basis of the literature review and group discussion, we designed the first draft of the interview outline. In addition, we integrated the subtopics of LDA model clustering into the outline to validate the results of LDA in the real world. After two preinterviews were conducted, the outline was refined and finalized. The research team (SS, MZ, JC, XY and MiZ) conducted one-on-one semistructured interviews with each participant. The interviews were conducted in a quiet room at the hospital, and each interview was audio-recorded in its entirety. The interview durations ranged from 30 to 56 min, and all interviews were conducted by a researcher trained in qualitative research (SS). MiZ is a female qualitative research expert who oversees the quality and integrity of the research process.
Prior to the formal interview, the interviewer (SS) established a rapport with the interviewee, explained the topic and purpose of the interview, and obtained consent for recording. Throughout the interview process, the interviewer listened to the opinions of the participants, conducted detailed inquiries, promptly questioned and clarified any deviations from the participants, and avoided asking leading questions. Additionally, the interviewer observed participants’ nonverbal messages (such as facial expressions and body language). The interviews ended when the participants indicated that they had nothing more to add. Recordings were converted to text within 24 h, and participants were given transcripts for review and feedback.
Colaizzi’s phenomenological approach was applied for data analysis [46]. Briefly, two coders (MZ and JC) independently and repeatedly read the interview transcripts, identified meaningful statements and completed text coding and clustering themes, etc. The term ‘theme’ refers to the focus on identifying, encoding, and reporting recurring patterns and central concepts from textual data. Second, MZ and JC repeatedly compared and identified their results. Specifically, the research team reviewed coded data regularly to identify relationships between themes, deliberate on the implications of new data, and identify final themes. Saturation was considered reached when new data no longer yielded additional themes. Data analysis was completed using NVivo12 Plus software [47].
LDA has improved the efficiency of social media big data analysis, and real-world interviews can further validate the results of LDA and conduct deep mining. In this study, two researchers (SS, JC) trained in qualitative techniques to analyse, compare, contrast, and combine LDA themes and interview results and confirm similarities and differences. These results were confirmed by a gastroenterologist (YF).
Phase II – Quantitative Study: A survey on the PA levels and self-reported outcomes of CD patients
Participant
Patients with CD who visited the Department of Gastroenterology, Zhejiang Provincial Hospital of Traditional Chinese Medicine, between January and March 2024 were invited to participate in this study. The inclusion criteria were as follows: diagnosed with CD; aged 18–80 years; and volunteered to participate in the study. Those who were unable to complete the questionnaire due to language, cognitive, or mental problems were excluded. We explained the purpose of this study to eligible patients and obtained their consent. The participants were asked to complete an electronic questionnaire containing general demographic information as well as a questionnaire on PA levels and patient-reported outcomes.
Covariate assessment
We included covariates on the basis of the literature and prior clinical knowledge. The participant demographic factors (age, sex, body mass index, smoking status, alcohol status, marital status and residence), disease activity levels and current medication were considered and collected as covariate assessments. The participants’ disease activity levels were scored using the Harvey Bradshaw Index (HBI) [48]. The remission period is 0–4, the mild active period is 5–7, the moderate active period is 8–16 points, and the severe active period is ≥ 16. The participants’ current medication treatment plans were retrieved from the electronic medical records system, and their medication usage patterns were categorized into five categories: mesalazine, traditional immunosuppressants, biologics, immunosuppressants combined with biologics and others.
Global Physical Activity Questionnaire (GPAQ)
The Chinese version of the GPAQ (version 2) was used in this study (https://www.who.int/zh/publications/m/item/global-physical-activity-questionnaire). The GPAQ consists of 16 questions (including an item on sedentary time) assessing participants’ “usual” 1-week level of physical activity (work, travel, leisure activities) and is quantified by metabolic equivalent tasks (METs) [49]. Moderate and vigorous intensity during work and leisure activities were scored as 4 and 8 METs, respectively; travel activities were scored as 4 METs. The total moderate to vigorous physical activity (MVPA) was evaluated [50]. The PA levels of each participant were quantified into five subcategories: work physical activity (vigorous), work physical activity (moderate), recreation physical activity (vigorous), recreation physical activity (moderate), and travel physical activity (walking or bicycling). We further calculated the total work MVPA, total leisure MVPA, and total MVPA. In short, in our study, physical activity was quantified through eight subcategories. In addition, sedentary time was classified into a separate subcategory. We divided participants into low- and high-level PA groups on the basis of their level of total MVPA. The population with high levels of physical activity is defined as the highest 50% of the cohort with nonzero physical activity [51].
Patient-reported Outcome Measurement Information System (PROMIS-57)
The PROMIS–57 is a 57-item multidimensional questionnaire designed to assess respondents’ symptoms, including physical functioning, anxiety, depression, fatigue, sleep disturbance, pain interference, pain intensity, and ability to participate in social roles [52]. Pain intensity was assessed using one item with 11 response options (ranging from 0 to 10); the remaining domains were assessed using eight items that were scored using a five-point Likert scale. Therefore, the scores for each domain ranged from 840 [53]. The raw scores were converted to T scores (mean = 50, standard deviation (SD) = 10). A higher T score indicates better functioning or greater symptom severity. The Cronbach’s α coefficient for this sample was satisfactory (0.96). The Chinese version of the PROMIS-57 was translated by the PROMIS National Center (PNC)-China (https://pnc-china.fudan.edu.cn), and we obtained permission to use the PROMIS instrument from PNC-China.
Data analysis
In Phase I, LDA for model analysis and visualization was performed using Python. The coding process was completed using NVivo12 Plus software. In Phase II, categorical and continuous variables are described using frequencies (percentages) and means (standard deviations) or medians (Q1:Q3), respectively. A t test was used for continuous variables that followed a normal distribution; otherwise, the Wilcoxon rank sum test was used. Chi-square tests were used to compare categorical variables. Multiple linear regression analysis was used to explore the correlation between PA and patient-reported outcomes and to exclude potential confounding factors. Statistical analysis was performed using R language (version 4.3.1).
Results
Phase I – qualitative study
LDA Topic model analysis
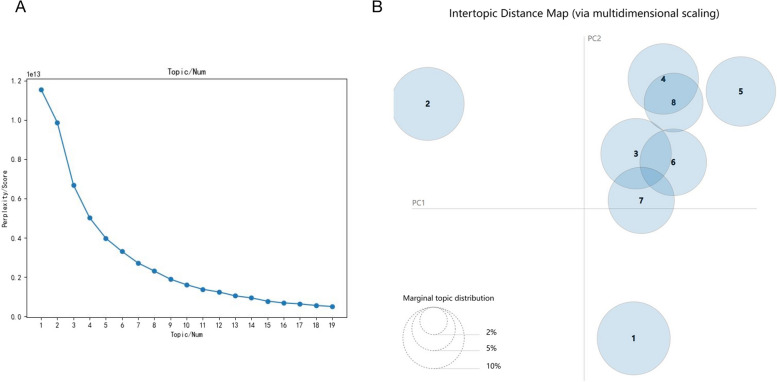
A total of 1536 posts were used for the LDA analysis. We calculated perplexity scores for 1–20 topics (Fig. 2A) and examined the intertopic distance map. By comparing the results of different numbers of topics (i.e., whether the topic words under each cluster can be well defined), we ultimately determined the optimal number of topics (k = 8). The intertopic distance map showed good clustering (Fig. 2B). On the basis of the results of LDA, we backtracked the original posts under each cluster and defined 8 categories of exercise topics in which CD patients participate in discussions on social media. Table 1 shows the representative term cluster with each term’s prevalence and assigned topic.
Fig. 2.
LDA topic model analysis. A Perplexity scores for different numbers of topics. B Intertopic distance map
Table 1.
Representative term clusters with prevalence and assigned topic
| Cluster Number | Representative term cluster | Prevalence (%) | Topic |
|---|---|---|---|
| 1 | come on, it’s okay, normal people, colleagues, mentality, control, suggestions, victory, bravery | 14.1 | Peer Support |
| 2 | exercise therapy, medicine, western medicine, rehabilitation, conditioning, treatment, mesalazine, Traditional Chinese medicine | 14.1 | Exercise Therapy |
| 3 | diet, food, less oil, breakfast, combination, spicy, honey, eating, nutrition, light | 13.2 | Diet |
| 4 | tired, fatigue, intensity, sleep, moderate, intense, time, symptoms | 13.2 | Fatigue |
| 5 | running, working out, squats, levator exercises, walking, fitness, vigorous, aerobic exercise | 12.8 | Exercise Type |
| 6 | constipation, attacks, abdominal pain, life, lighten, useless, danger | 11.8 | Intestinal Symptoms |
| 7 | body, resistance, immunity, constitution, strong, maintenance, poor, weak, bone | 11.6 | Body Constitution |
| 8 | mentality, body, exercise, control, mood, cheer, try, emotion, brave, relax | 9.2 | Mental |
The two most common topics of the posts focused on peer support and therapy (mean share within posts = 14.1%, respectively), which reflects that patients can gain peer support and communicate information about exercise therapy through social media. By tracking the original posts, we found that they encourage peers to exercise consistently and communicate exercise methods, which may improve patients’ exercise compliance. A total of 13.2% discussed diet issues related to exercise (e.g., they do not know if they need to supplement relevant nutrients after exercise), and the fatigue caused by exercise was also a focus of attention for patients (13.2%). In addition, the discussion of exercise type was also one of the topics in which patients were interested (12.8%), and patients could not determine which type of exercise was most beneficial for themselves. We also found that patients discussed the impact of exercise on disease symptoms (11.8%) and individual body constitution (11.6%). They are more concerned about whether exercise can alleviate symptoms and improve their physical condition. The impact of exercise on mental health has also been widely discussed (9.2%), and most people agree that exercise can improve their mood. There was no considerable difference in the proportion of patient discussions among all these topics (from 9.2 to 14.1%). These results reflect the attention of CD patients to exercise, and LDA excellently summarizes subtopics related to exercise.
Qualitative interviews
Although LDA has advantages in terms of data breadth, the depth of its results is limited. Therefore, we conducted structured interviews in the real world to validate the results of LDA and further explore the exercise perspectives of CD patients. The interview study included 11 participants, 45% of whom were female, all of whom were between 18 and 57 years old, and 3 were in the active disease stage (Table S1).
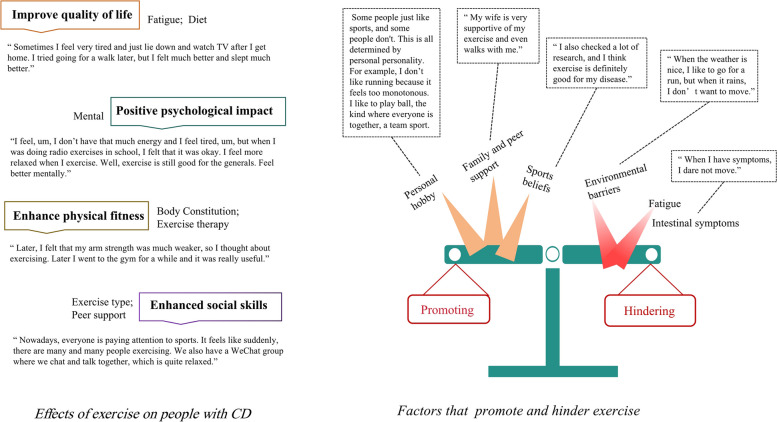
Two themes emerged from the content analysis of the interviews: the effects of exercise on people with CD and the factors that promote and hinder exercise.
The impact of exercise on CD patients is mainly composed of four subthemes: (i) positive psychological impact (e.g., exercise is good… feel better mentally) and (ii) improving quality of life (e.g., sometimes I feel very tired and just lie down and watch TV after I get home. I tried going for a walk later, but I felt much better and slept much better), (iii) enhancing physical fitness (I felt that my arm strength was much weaker, so I thought about exercising. Later, I went to the gym for a while and it was really useful) and (iv) increasing social skills (e.g., we also have a WeChat group where we chat and talk together, which is quite relaxed). These results indicate that exercise has beneficial effects on CD patients, with more beneficial effects reflected in subjective parameters such as psychological state and social and quality of life, in addition to enhancing physical fitness.
Personal interests (e.g., I don’t like running because it feels too monotonous. I like to play ball), family support (e.g., my wife is very supportive of my exercise and even walks with me) and beliefs about sports (e.g., I think exercise is definitely good for my disease) were the main facilitators for patients to exercise. Instead, intestinal symptoms and environmental barriers (such as weather, sports and facilities) prevent patients from exercising. These subthemes provide an overview of the factors promoting and barriers to exercise in Chinese CD patients.
Interestingly, by comparing the results of LDA and interviews, the topics clustered by LDA were mostly mentioned by patients in the interviews, but the theme of “sports beliefs” was newly discovered in the interviews. These results further validate the credibility of the LDA model and confirm the importance of interviews in the real world. The results of both the LDA and the interviews are summarized together (Fig. 3).
Fig. 3.
Schematic diagram of the qualitative interviews
Phase II quantitative study
The results of social media and interviews draw attention to the potential benefits of exercise for patients’ mental health outcomes. Therefore, we conducted a cross-sectional study to explore the correlation between physical activity and patient-reported outcomes.
Demographic characteristics of the patients surveyed
We collected a total of 127 questionnaires, 8 of which were excluded because of incomplete questionnaires; ultimately, 119 were included in the final analysis. The mean age was 30.6 ± 8.8 years, the average BMI was 21.63 ± 3.2 kg/m2, and the male-to-female ratio was 2.5 (85/34). Two participants (1.7%) smoked, and 7 participants (5.8%) drank alcohol. According to the HBI scoring results, the majority of participants were in the remission phase (n = 92, 77.3%), 24 were in the mild activity phase (20.2%), only 3 were in the moderate activity phase (2.5%), and no severe activity phase patients were found. According to the current medication regimens of the participants, 79.8% of them (n = 95) were treated with biologics alone, whereas 13.4% (n = 16) were treated with traditional immunosuppressive agents in combination with biologics. Three (2.5%) and two (1.7%) individuals were treated with mesalazine alone and traditional immunosuppressive agents, respectively. The remaining three individuals were classified as other because of the use of different Chinese herbal medicines. Table 2 summarizes the characteristics of the cross-sectional study subjects. More detailed results can be found in Supplementary File S2.
Table 2.
Characteristics of the study subjects
| Variable | N = 119 |
|---|---|
| Age | 30.6 ± 8.8 |
| BMI [kg/m2] | 21.63 ± 3.2 |
| Sex male [%] | 85 (71.4%) |
| Smoking | 2 (1.7%) |
| Alcohol | 7 (5.8%) |
| Residence City [%] | 87 (73.1%) |
| Disease activity level | |
| Remission | 92 (77.3%) |
| Mild active | 24 (20.2%) |
| Moderate active | 3 (2.5%) |
| Severe active | 0 (0%) |
| Current medications | |
| Mesalazine | 3 (2.5%) |
| Immunosuppressives | 2 (1.7%) |
| Biologicals | 95 (79.8%) |
| Immunosuppressives + biologicals | 16 (13.4%) |
| Others | 3 (2.5%) |
| GPAQ (MET-mins/wk) | Median (Q1; Q3) |
| Work | |
| Vigorous | 0 (0; 0) |
| Moderate | 0 (0; 0) |
| Total Work MVPA | 0 (0; 488) |
| Travel | |
| Moderate | 120 (0; 480) |
| Recreation | |
| Vigorous | 0 (0; 120) |
| Moderate | 120 (0; 480) |
| Total Recreation MVPA | 240 (0; 720) |
| GPAQ Total MVPA | 944 (240; 1920) |
| Sedentary mins/day | 360 (210; 450) |
| PROMIS-57 T Score | Mean (SD) |
| Physical functioning | 50.49 ± 8.95 |
| Anxiety | 49.23 ± 9.33 |
| Depression | 49.28 ± 9.58 |
| Fatigue | 49.36 ± 9.60 |
| Sleep disturbance | 49.92 ± 9.49 |
| Ability to participate in social roles | 49.29 ± 9.65 |
| Pain interference | 1.03 ± 1.52 |
| Pain intensity | 49.31 ± 8.73 |
The results are expressed as numbers (%), medians (Q1:Q3) and means (SDs). BMI: body mass index, MVPA: moderate and vigorous physical activity
The correlation between physical activity and patient-reported outcomes
We conducted correlation analysis between the subcategories of the GPAQ and the eight outcome T scores of the PROMIS-57. The results of multiple linear regression analysis revealed that residence, disease activity, current medication, PA and sedentary time had varying degrees of impact on the reported outcomes of patients, whereas age, sex, BMI, smoking, and alcohol consumption had no effect. Specifically, compared with participants living in cities, those living in the countryside have poorer physical function (p = 0.019) and social skills (p < 0.001). Moderate disease activity may lead to poorer physical function (p = 0.026), whereas disease activity, whether mild or moderate, affects the reported outcomes of the remaining patients (p < 0.05). Not taking medication regularly was significantly associated with anxiety (p = 0.032), depression (p = 0.008), and fatigue (p = 0.003). Table 3 lists the factors that affect patient-reported outcomes. The positive or negative sign of the coefficient represents a positive/negative impact on the outcome score, and the numerical value represents the ability to influence. More detailed results of the multiple linear regression analysis can be found in Supplementary File S3.
Table 3.
Significant variables in the multiple linear regression results
| Patients reported outcomes | Related variables | Estimated Coefficients | p value |
|---|---|---|---|
| Physical Function | Residence (countryside) | −4.748 | 0.019 |
| Activity (moderate) | −12.23 | 0.026 | |
| Recreation (moderate) | 0.002 | 0.035 | |
| Anxiety | Activity (mild) | 6.035 | 0.005 |
| Activity (moderate) | 17.44 | 0.001 | |
| Medication (others) | −16.37 | 0.032 | |
| Work (vigorous) | 0.003 | < 0.001 | |
| Recreation (moderate) | −0.003 | 0.009 | |
| Depression | Activity (mild) | 6.835 | < 0.001 |
| Activity (moderate) | 18.18 | < 0.001 | |
| Medication (others) | −18.8 | 0.008 | |
| Work (vigorous) | 0.003 | < 0.001 | |
| Recreation_(moderate) | −0.003 | 0.002 | |
| Sedentary time | 0.014 | 0.006 | |
| Fatigue | Activity (mild) | 7.903 | < 0.001 |
| Activity (moderate) | 16.96 | 0.003 | |
| Medication (others) | −16.59 | 0.033 | |
| Work(vigorous) | 0.002 | 0.008 | |
| Recreation (moderate) | −0.002 | 0.027 | |
| Social ability | Residence (countryside) | −7.646 | < 0.001 |
| Activity (mild) | −2.648 | 0.236 | |
| Activity (moderate) | −17.55 | 0.003 | |
| Pain interference | Activity (mild) | 6.462 | 0.002 |
| Activity (moderate) | 20.31 | < 0.001 | |
| Work_(vigorous) | 0.002 | 0.004 | |
| Recreation_(moderate) | −0.002 | 0.016 | |
| Pain | Activity (mild) | 1.071 | 0.003 |
| Activity (moderate) | 3.063 | < 0.001 | |
| Work_(vigorous) | 0.0003 | 0.012 | |
| Recreation_(moderate) | −0.0004 | 0.024 |
In this study, the impact of PA on patient-reported outcomes was the focus of our attention. After confounding factors such as disease activity and medication were considered, moderate-intensity recreational PA increased patients’ physical function and improved anxiety, depression, fatigue, pain intensity, and pain impact (all p < 0.05). In contrast, high-intensity work may lead to anxiety, depression, fatigue, pain, and pain effects (all p < 0.001). In addition, sedentary behaviour may lead to depression (p = 0.006). Moderate-intensity work, travel PA and vigorous recreational activities did not affect the scores of patients’ reported outcomes.
The participants were classified into the low- (n = 67) or high- (n = 52) MVPA group according to the overall MVPA level (cut-off value of 1120 MET-mins/wk). Compared with the low-MVPA group, the high-MVPA group had no significant difference in the scores of the eight types of outcomes (all p < 0.05).
Discussion
Exercise is an auxiliary treatment that is used by an increasing number of CD patients. There is no consensus regarding the health benefits of exercise for IBD patients or the optimal intensity and type of exercise for treating CD. Research on the Western CD population has provided some knowledge; however, the attitudes and experiences of Chinese patients towards exercise are currently unclear. In addition, the shared decision-making (SDM) model is becoming the mainstream approach for IBD medical decision-making [54]. In China, there is a significant difference between ideal decision-making and actual decision-making among IBD patients [55]. Therefore, understanding the exercise needs and dilemmas of patients is necessary for healthcare professionals to develop “exercise prescriptions”.
Previous studies [56–58] have utilized LDA for social media data analysis; although grounded theory has been used for relevant validation [56], it can guarantee the accuracy of data analysis and lacks further validation from real-world data and a deep understanding of the problem. Our study analysed patient needs and behaviours by mining social media data and using interview methods. LDA enables us to analyse large amounts of data comprehensively and solve workload limitations, whereas traditional interview research enables us to verify the themes of LDA and analyse the data in more depth and detail. The results of the LDA analysis suggested that patients communicate approximately 8 exercise-related topics through social media. Through social media, patients mainly provide peer support, encourage patients to exercise more, and exchange treatment experiences. The choice of exercise type and related nutritional issues are also the focus of patient discussions. A series of effects of exercise on the body, including fatigue, symptoms, and physical and psychological effects, are the focus of discussion among patients. In the interview results, the themes clustered by the LDA model were also mentioned by patients. We summarized the interview results into two aspects: the effects of exercise on people with CD and the factors that promote and hinder exercise. Exercise has a positive psychological impact on patients in terms of improving quality of life, enhancing physical fitness, and enhancing social skills. Some factors, including personal interests, family support, and health beliefs, encourage patients to engage in physical exercise. The fatigue and environmental obstacles caused by diseases (such as weather and sports facilities) hinder patients from exercising. Recently, a study [59] in the UK investigated movement disorders in patients with inflammatory bowel disease and reported that their increased fear of toilet emergencies was the reason for their lack of exercise participation. Another qualitative study [60] on moderately to severely active IBD suggested that disease activity, symptom management, lack of exercise knowledge, and uncertainty in exercise value are the main factors affecting patient exercise. Our results are consistent with these findings; therefore, we recommend considering exercising at locations where individuals with CD are comfortable with the location and use of restrooms, for example, home workouts or a familiar gym.
The results of social media and patient interviews further provide directional information for the quantitative part of the study. The qualitative findings confirmed that exercise can enhance the mental health and social skills of CD patients, and this interesting result prompted us to further quantify this relationship. Patient-reported outcomes are direct measures of patient experience and help clinicians obtain information about patients’ symptom burden, psychological status, physical function, quality of life, and satisfaction [61, 62]. Research has shown that mental health has a profound effect on the body’s inflammatory response. This is particularly evident in people with CD, where psychological stress is associated with heightened episodes of the disease [63]. In this study, we quantified the relationships between physical activity and patients’ physical and mental health using the GPAQ and PROMIS-57 questionnaires. The results of multiple linear regression analysis revealed that moderate-intensity recreational PA can enhance patients’ physical function and improve anxiety, depression, fatigue, pain intensity, and pain interference, whereas vigorous PA is associated with increased anxiety, depression, fatigue, pain, and pain effects. Moderate-intensity work, travel PA (walking or bicycling) and vigorous recreational activities did not affect the scores of patients’ reported outcomes. A series of national surveys [64–66] based on the Chinese population revealed that excessive occupational, traffic and housework physical activities increase new-onset hypertension. This evidence highlights the harmful effects of vigorous PA. Similarly, our research also demonstrated the adverse effects of vigorous PA and the protective role of moderate recreational PA. Notably, our grouped analysis of total MVPA revealed that high and low levels of total MVPA had no effect on patient-reported outcomes, which may be due to the combined effects of work, travel, and recreational PA. This result is reasonable because, in this study, work PA was considered a risk factor, whereas recreational PA was a protective factor. In the future, it is necessary to explore the impact of different exercise patterns (such as the proportions of different PA types) on patients.
Increased leisure sedentary behaviours, such as television and computer viewing time, are associated with numerous adverse health outcomes [67]. A study based on two population datasets in Canada suggested that sedentary occupations were twice as likely to be associated with IBD [68]. Our study indicated that CD patients who are accustomed to prolonged sitting have higher depression scores. Physical activity may play an important role in the treatment of mild to moderate mental health disorders, particularly depression and anxiety disorders [69]. Our research confirms this finding. Moderate physical activity, as well as reduced sitting time, is beneficial for the mental health and physical function of people with CD.
This study has several limitations that deserve discussion. In qualitative research, although the interview sample size is based on saturation, the interviewees were randomly selected and did not undergo stratified sampling on the basis of age, disease activity, and place of residence, which may lead to selection bias. In addition, the participants in the qualitative interviews were recruited from only one hospital, which may reduce the generalizability of the conclusions. Future studies involving multiple centres can increase the reliability of this study. In quantitative research, owing to the cross-sectional approach used here, this quantitative study cannot establish a causal relationship between variables. Therefore, future longitudinal studies are necessary. Second, the measurement of physical activity was conducted in the form of a questionnaire, which may lead to recall bias. An accelerometer based on wearable devices can more accurately measure physical activity. Third, we conducted this study at only one tertiary hospital in Hangzhou, China. This region may differ from western, eastern, and northern China in terms of lifestyle and social structure, so further multicentre studies are needed. In the future, interviews with CD patients from different regions, environments, cultures, and ages are still needed to understand the exercise needs of different subgroups of the population and to assist in developing personalized exercise plans.
Conclusion
Patients with CD tend to seek exercise guidance and experience through social media and generally believe that exercise is beneficial, especially for their psychological health. Quantitative correlation analysis confirmed this finding, and the results revealed that engaging in moderate recreational PA, reducing vigorous PA and sedentary behaviour are beneficial for the physical and psychological health of patients.
Supplementary Information
Acknowledgements
The authors of this study would like to thank the participants. We also thank to Baidu Tieba for providing the data and the developers of the Python software and R language software. We also thank PNC China Center for authorizing the use of PRMIS-57. ©2008-2022 PROMIS Health Organization (PHO). This material can be reproduced without permission by clinicians for use with their own patients. Any other use, including electronic use, requires written permission of the PHO.
Authors’ contributions
SS, JC and MZ: conceived the study design and wrote the manuscript. MiZ and XY: made data analysis and prepared the figures. YS, YH and KN: distributed and collected questionnaires. YF and BL: superivised the scientific work and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This publication was funded by the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (No. 2024KY1214) and the 2024 General Scientific Research Project of Zhejiang Provincial Department of Education -Special Project for Reform of Professional Degree Graduate Training Mode (No. Y202456174).
Data availability
All data is provided in the original text and supplementary documents.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First School of Clinical Medicine, Zhejiang Chinese Medical University (no. 2024-KL-261-01). Informed consent was obtained from all individual participants (Interviews and cross-sectional studies) for study participation. The text data used for LDA come from the public website Baidu Tieba, a publicly available website. According to the statement of Baidu Tieba (browsing and copying data are for the purpose of obtaining information and cannot be used for commercial purposes), ethical approval was not required for the secondary analysis of publicly available data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Plevris N, Lees CW. Disease monitoring in inflammatory bowel disease: evolving principles and possibilities. Gastroenterology. 2022;162(5):1456-e14751. [DOI] [PubMed] [Google Scholar]
- 2.Ng SC, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–78. [DOI] [PubMed] [Google Scholar]
- 3.Park J, Cheon JH. Incidence and prevalence of inflammatory bowel disease across Asia. Yonsei Med J. 2021;62(2):99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng SC, et al. Epidemiology of inflammatory bowel disease from 1981 to 2014: results from a territory-wide Population-based registry in Hong Kong. Inflamm Bowel Dis. 2016;22(8):1954–60. [DOI] [PubMed] [Google Scholar]
- 5.Roda G, et al. Crohn’s disease. Nat Rev Dis Primers. 2020;6(1):22. [DOI] [PubMed] [Google Scholar]
- 6.Dolinger M, Torres J, Vermeire S. Crohn’s disease. Lancet. 2024;403(10432):1177–91. [DOI] [PubMed] [Google Scholar]
- 7.Gold SL, Steinlauf AF. Efficacy and safety of dual biologic therapy in patients with inflammatory bowel disease: a review of the literature. Gastroenterol Hepatol (N Y). 2021;17(9):406–14. [PMC free article] [PubMed] [Google Scholar]
- 8.Lopes EW et al. Lifestyle factors for the prevention of inflammatory bowel disease. Gut, 2022. [DOI] [PMC free article] [PubMed]
- 9.Bauer N, et al. Evaluation of a multimodal stress management and comprehensive lifestyle modification program on quality of life and gastrointestinal symptoms in patients with Crohn’s disease: a randomized controlled pilot trial with 9-month follow-up. Digestion. 2024;105(3):201–12. [DOI] [PubMed] [Google Scholar]
- 10.Scheffers LE, et al. Physical training and healthy diet improved bowel symptoms, quality of life, and fatigue in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2023;77(2):214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Izquierdo M, et al. International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. 2021;25(7):824–53. [DOI] [PubMed] [Google Scholar]
- 12.Ekelund U, et al. Dose-response associations, physical activity intensity and mortality risk: a narrative review. J Sport Health Sci. 2024;13(1):24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paudel S, et al. Do associations of physical activity and sedentary behaviour with cardiovascular disease and mortality differ across socioeconomic groups? A prospective analysis of device-measured and self-reported UK Biobank data. Br J Sports Med. 2023;57(14):921–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sonnenberg A. Occupational distribution of inflammatory bowel disease among German employees. Gut. 1990;31(9):1037–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khalili H, et al. Physical activity and risk of inflammatory bowel disease: prospective study from the nurses’ Health Study cohorts. BMJ. 2013;347:f6633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones PD, et al. Exercise decreases risk of future active disease in patients with inflammatory bowel disease in remission. Inflamm Bowel Dis. 2015;21(5):1063–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lamers CR, et al. Patient experiences with the role of physical activity in inflammatory bowel disease: results from a survey and interviews. BMC Gastroenterol. 2021;21(1):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson RJ, et al. Effect of a low-impact exercise program on bone mineral density in Crohn’s disease: a randomized controlled trial. Gastroenterology. 1998;115(1):36–41. [DOI] [PubMed] [Google Scholar]
- 19.Cronin O, et al. Moderate-intensity aerobic and resistance exercise is safe and favorably influences body composition in patients with quiescent inflammatory bowel disease: a randomized controlled cross-over trial. BMC Gastroenterol. 2019;19(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Souza Tajiri GJ, de Castro CL, Zaltman C. Progressive resistance training improves muscle strength in women with inflammatory bowel disease and quadriceps weakness. J Crohns Colitis. 2014;8(12):1749–50. [DOI] [PubMed] [Google Scholar]
- 21.Lamers CR, et al. Repeated prolonged moderate-intensity walking exercise does not appear to have harmful effects on inflammatory markers in patients with inflammatory bowel disease. Scand J Gastroenterol. 2021;56(1):30–7. [DOI] [PubMed] [Google Scholar]
- 22.Ng V, et al. Low-intensity exercise improves quality of life in patients with Crohn’s disease. Clin J Sport Med. 2007;17(5):384–8. [DOI] [PubMed] [Google Scholar]
- 23.Klare P, et al. The impact of a ten-week physical exercise program on health-related quality of life in patients with inflammatory bowel disease: a prospective randomized controlled trial. Digestion. 2015;91(3):239–47. [DOI] [PubMed] [Google Scholar]
- 24.Peters HP, et al. Potential benefits and hazards of physical activity and exercise on the gastrointestinal tract. Gut. 2001;48(3):435–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watters C, et al. Positive and negative wellbeing as predictors of exercise uptake in Crohn’s disease: An exploratory study. Psychol Health Med. 2001;6(3):293–9. [Google Scholar]
- 26.Bull FC, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Su J, et al. Association between physical activity and cancer risk among Chinese adults: a 10-year prospective study. Int J Behav Nutr Phys Act. 2022;19(1):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett DA, et al. Association of physical activity with risk of major cardiovascular diseases in Chinese men and women. JAMA Cardiol. 2017;2(12):1349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hidalgo JL, Sotos JR. Effectiveness of Physical exercise in older adults with mild to moderate depression. Ann Fam Med. 2021;19(4):302–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang X, Shi J, Kong H. Online Health Information seeking: a review and meta-analysis. Health Commun. 2021;36(10):1163–75. [DOI] [PubMed] [Google Scholar]
- 31.O’Reilly M, et al. Is social media bad for mental health and wellbeing? Exploring the perspectives of adolescents. Clin Child Psychol Psychiatry. 2018;23(4):601–13. [DOI] [PubMed] [Google Scholar]
- 32.Chan KL, Chen M. Effects of social media and mobile health Apps on pregnancy care: meta-analysis. JMIR Mhealth Uhealth. 2019;7(1):e11836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li M, et al. Psychological impact of health risk communication and social media on college students during the COVID-19 Pandemic: cross-sectional study. J Med Internet Res. 2020;22(11):e20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ni Z, et al. Characteristics and associated factors of health information-seeking behaviour among patients with inflammatory bowel disease in the digital era: a scoping review. BMC Public Health. 2024;24(1):307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voskergian D, Jayousi R, Yousef M. Topic selection for text classification using ensemble topic modeling with grouping, scoring, and modeling approach. Sci Rep. 2024;14(1):23516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sun S, et al. Patients’ perspectives on irritable bowel syndrome: a qualitative analysis based on social media in China. Qual Life Res. 2023;32(9):2561–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun S, et al. Patients’ perspectives on, experience with and concerns about Crohn’s disease: insights from Chinese social media. BMC Gastroenterol. 2023;23(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang Z. A survey of modern crawler methods. In: Proceedings of the 6th International Conference on Control Engineering and Artificial Intelligence. 2022.
- 39.Demšar J, et al. Orange: data mining toolbox in python. J Mach Learn Res. 2013;14(1):2349–53. [Google Scholar]
- 40.Blei DM, Ng A, Jordan MI. Latent dirichlet allocation. J Machine Learn Res. 2003;3(Jan):993–102. [Google Scholar]
- 41.Ehek R, Sojka P. Software Framework for Topic Modelling with Large Corpora. In: Proceedings of the LREC 2010 Workshop on New Challenges for NLP Frameworks. 2004.
- 42.Xie T, Qin P, Zhu L. Study on the topic mining and dynamic visualization in view of LDA model. Mod Appl Sci. 2018;13(1):204. [Google Scholar]
- 43.Sarkar D. Text analytics with Python: A Practical Real-World Approach to Gaining Actionable Insights from your Data. Apress; 2016.
- 44.Zhang Y, Jin R, Zhou ZH. Understanding bag-of-words model: a statistical framework. Int J Mach Learn Cybernetics. 2010;1(1–4):43–52. [Google Scholar]
- 45.Perdikogianni GM. A comparative method for themes saturation (CoMeTS) in qualitative interviews. JPC Bull Iron Steel. 2017;17(5):571-88. [Google Scholar]
- 46.Edward KL, Welch T. The extension of Colaizzi’s method of phenomenological enquiry. Contemp Nurse. 2011;39(2):163–71. [DOI] [PubMed] [Google Scholar]
- 47.Gibbs GR. Qualitative data analysis: explorations with NVivo. Open Univ. 2002;26(93):105–38. [Google Scholar]
- 48.Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1(8167):514. [DOI] [PubMed] [Google Scholar]
- 49.Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6(6):790–804. [DOI] [PubMed] [Google Scholar]
- 50.Cleland CL, et al. Validity of the Global Physical Activity Questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14:1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lo CH, et al. Healthy lifestyle is associated with reduced mortality in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2021;19(1):87-e954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cella D, et al. PROMIS(®) Adult Health profiles: efficient short-form measures of seven health domains. Value Health. 2019;22(5):537–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cella D, et al. The patient-reported outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Song K, Wu D. Shared decision-making in the management of patients with inflammatory bowel disease. World J Gastroenterol. 2022;28(26):3092–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang L, et al. Treatment decision-making in Chinese inflammatory bowel disease patients. Inflamm Bowel Dis. 2022;28(Suppl 2):S76-84. [DOI] [PubMed] [Google Scholar]
- 56.Gonzalez G, et al. Social media analytics of overactive bladder posts: what do patients know and want to know? Int Urogynecol J. 2021;32(10):2729–36. [DOI] [PubMed] [Google Scholar]
- 57.Yang Y, et al. Spatial evolution patterns of public panic on Chinese social networks amidst the COVID-19 pandemic. Int J Disaster Risk Reduct. 2022;70:102762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dzubur E, et al. Patient concerns and perceptions regarding Biologic therapies in Ankylosing spondylitis: insights from a large-scale survey of social media platforms. Arthritis Care Res (Hoboken). 2019;71(2):323–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sinclair J, Brooks-Warburton J, Bottoms L. Perceptions, behaviours and barriers towards exercise practices in inflammatory bowel disease. PLoS ONE. 2024;19(4):e0299228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang J, et al. Attitude and influencing factors on exercise in patients with moderately to severely active inflammatory bowel disease: a qualitative study. BMJ Open. 2023;13(12):e080084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.LeBlanc TW, et al. Patient-reported outcomes in cancer care - hearing the patient voice at greater volume. Nat Rev Clin Oncol. 2017;14:763–72. [DOI] [PubMed] [Google Scholar]
- 62.Sloan JA, et al. The Mayo Clinic manuscript series relative to the discussion, dissemination, and operationalization of the Food and Drug Administration guidance on patient-reported outcomes. Value Health. 2010;10(s2):S59-63. [DOI] [PubMed] [Google Scholar]
- 63.Schneider KM, et al. The enteric nervous system relays psychological stress to intestinal inflammation. Cell. 2023;186(13):2823-e283820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li R, et al. Transportation physical activity and new-onset hypertension: a nationwide cohort study in China. Hypertens Res. 2022;45(9):1430–40. [DOI] [PubMed] [Google Scholar]
- 65.Li Q, et al. Occupational physical activity and new-onset hypertension: a nationwide cohort study in China. Hypertension. 2021;78(1):220–9. [DOI] [PubMed] [Google Scholar]
- 66.Li R, et al. Domestic physical activity and new-onset hypertension: a nationwide cohort study in China. Am J Med. 2022;135(11):1362-e13706. [DOI] [PubMed] [Google Scholar]
- 67.Foster HME, et al. Understanding how much TV is too much: a nonlinear analysis of the association between television viewing time and adverse health outcomes. Mayo Clin Proc. 2020;95(11):2429–41. [DOI] [PubMed] [Google Scholar]
- 68.Bernstein CN, et al. The relationship between inflammatory bowel disease and socioeconomic variables. Am J Gastroenterol. 2001;96(7):2117–25. [DOI] [PubMed] [Google Scholar]
- 69.Paluska SA, Schwenk TL. Physical activity and mental health: current concepts. Sports Med. 2000;29(3):167–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data is provided in the original text and supplementary documents.