Abstract
Background
Different pulmonary pathologies may require a partial or total lung lobectomy as treatment. This study compared two techniques for performing a caudal pulmonary lobectomy: a traditional lateral thoracotomy (LT) and a novel transdiaphragmatic (TD) approach.
Methods
TD and LT approaches were performed on each of 18 canine cadavers. The operator and order of intervention were randomised at the beginning of the study. To compare both techniques, surgical time, percentage of area of lobe removed, incision length and iatrogenic damage were recorded.
Results
The mean length of surgery for the TD approach (1155 ± 232.8 seconds) was non‐inferior to the LT approach (1126.8 ± 180.6 seconds) (p = 0.6131). The mean percentage of the area of caudal lobe that was successfully removed during the TD approach was 25.83 ± 8.95% (range 10.55‒40.72%) of the lobe surface, while 100% of the caudal lobe was removed during the LT approach. There was no statistical difference in iatrogenic damage between the procedures.
Limitations
This is a non‐inferiority ex vivo study carried out by three different surgeons, and no leak test was performed after lobectomies.
Conclusion
Partial caudal lung lobectomy can be performed in dogs by the TD approach without greater iatrogenic damage or longer surgical duration than the traditional LT approach.
Keywords: canine, lung, surgery, transdiaphragmatic lung lobectomy
INTRODUCTION
Pulmonary lobectomy is a surgical technique that consists of removing a pulmonary lobe (complete pulmonary lobectomy) or part of it (partial pulmonary lobectomy) as a surgical treatment for pathologies of this organ. In veterinary medicine, different intrathoracic approaches to perform a pulmonary lobectomy have been described. 1 , 2
Intercostal thoracotomy is a widely used surgical technique for the thoracic cavity. 3 It allows the approach to the cavity in the hemithorax where the intervention is performed, as well as access to the mediastinum. 4 However, this technique has been reported to be significantly associated with postoperative pain, 5 largely due to the possible compression of the intercostal nerves by the use of circumcostal sutures to close the thoracic cavity. 6
Median sternotomy has also been described as a thoracic approach. 7 This technique allows bilateral visualisation of the thoracic cavity through a single approach. 4 However, it is less commonly used due to the higher rate of complications (between 17% and 78%) compared to the intercostal approach. 7
In human medicine, minimally invasive techniques such as thoracoscopy or video‐assisted thoracoscopy surgery (VATS) have been used to reduce surgical pain and improve postsurgical recovery. 8 These advantages can also be observed in veterinary medicine. 9 , 10 , 11
Compared with conventional techniques, the transdiaphragmatic (TD) approach, first described by Fingeroth and Birchard, 12 is associated with decreased morbidity and better exposure of the caudal thorax. 13 This approach has been described for performing cardiopulmonary resuscitation in canine cadavers, 14 pacemaker implantation in small animals, 12 , 15 , 16 pericardectomy, 13 porto‐azygous shunt attenuation, 17 thoracic duct ligation 18 and removal of foreign bodies migrating from the stomach and duodenum. 19 Additionally, the ventral midline approach may be less demanding given its greater use and understanding among clinicians. 14
The objective of this study was to describe and evaluate the feasibility of the TD approach through a celiotomy for performing pulmonary lobectomies as an alternative to the traditional intercostal approach in a canine cadaveric model. It was hypothesised that this approach would allow the performance of caudal partial pulmonary lobectomies, with a surgery time no longer than that of lateral thoracotomy (LT) and producing a similar amount of trauma in the surrounding structures.
MATERIALS AND METHODS
Eighteen fresh canine cadavers weighing between 15.3 and 39.2 kg were used in the study. All dogs were euthanased for reasons unrelated to this study.
Three veterinarians participated in this study: one board‐certified surgeon and two surgical residents. Each surgeon was randomly assigned to each dog to perform both approaches. Random assignment was also used to determine which approach would have to be carried out first and on which caudal lobe each procedure would be performed for each patient. For this randomisation, the website https://www.random.org/ was used. Each surgeon performed a total of 12 procedures (six TD and six LT).
In order to quantify the percentage of lobes removed through the TD approach, a total pulmonary lobectomy of the caudal lobe of the TD approach was performed at the end of the procedure by an intercostal approach. All lobectomies, both partial and total, were performed with a thoracoabdominal model linear surgical stapler (Linear Stapler LS6035, Aesculap) with a blue staple cartridge of staples measuring 60 mm in length and 3.5 mm in height (Linear Staple Cartridge LSC6035). In order to record timing and incision length, a stopwatch and a metric ruler were used. A cross‐stitch plastic paper was used to measure the areas of pulmonary lobes removed. Three time intervals were recorded: T1 was the time interval between the start of skin incision and completion of pulmonary lobectomy, T2 was the time interval between the placement of the first suture and complete skin closure and Tt was the sum of T1 and T2.
In order to make the study similar to a procedure with live animals, especially during the approaches and lobectomies, all dogs were intubated through a tracheostomy. In this way, it was possible to inflate their lungs with a manual pump and maintain a mean pulmonary pressure between 10 and 20 cm of H2O with a digital sphygmomanometer (TL100 Digital Manometer Handheld, SEAFRONT) (Figure 1). 14
FIGURE 1.

Manual pump device for maintenance of pulmonary pressure
Description of TD surgical technique
As described previously by Jack et al., 14 all dogs were positioned in dorsal recumbency. A ventral midline incision was made starting 2 cm cranial to the xiphoid and extending at least halfway down the midline by using a number 23 scalpel blade. After the xiphoid and linea alba were exposed, the cranial linea alba was tented, and a reversed scalpel blade was used to enter the abdomen as in a midline celiotomy. The incision in the abdominal wall was extended caudally to the level of the skin incision with Mayo scissors. At the cranial aspect, the abdominal incision was extended along the right lateral aspect of the xiphoid to the caudoventral aspect of the right ninth rib. The falciform ligament was resected. A Balfour retractor was placed in the cranial portion of the abdominal incision for better exposure of the cavity. The incision on the diaphragm was made with a scalpel (number 11 blade) adjacent to the sternum to minimise inadvertent trauma to the lungs or heart through the pars sternalis muscle and extended circumcostally with scissors to the corresponding side of the lobectomy. Gentle manual retraction by an assistant was used to expose the caudal lung lobe, and partial lobectomy of the maximum possible portion of the lung lobe was carried out with the stapling device (Figure 2). Closure of the diaphragm was accomplished with a simple continuous suture pattern. The abdominal incision was closed routinely in three layers.
FIGURE 2.
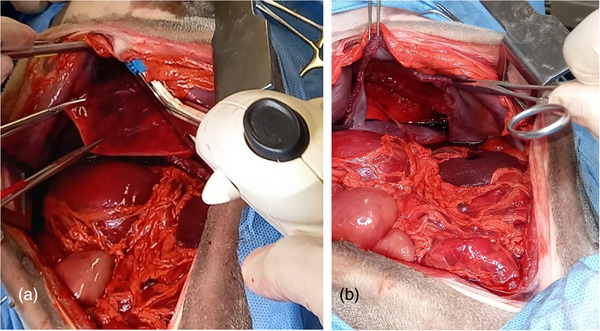
(a) Thoracoabdominal linear surgical stapler prior to partial lung lobectomy through the transdiaphragmatic approach. (b) The remaining left caudal lobe after the lobectomy
Description of LT surgical technique
All dogs were positioned in lateral recumbency prior to a routine LT, as described by Caywood and Lipowitz. 1 The sixth intercostal space was standardised as the TL approach space. 20 This was identified cranially by palpation from the 12th intercostal space. An incision was made with a number 23 scalpel blade through the skin and subcutaneous tissue over the targeted rib space. The incision was continued through the latissimus dorsi and serratus ventralis muscles with Metzembaum scissors. The intercostal muscles (external and internal of the sixth space) and pleura were then incised with the Metzembaum scissors. To widen the intercostal space, a manual Farabeuf retractor (proximal retraction) and a Finochietto retractor (cranial and caudal retraction) were used. To mobilise the caudal lobe, it was necessary to section its pulmonary ligament located on the medial edge of the lobe from the hilum to the mediastinal pleura. Total caudal pulmonary lobectomy was then performed using a stapler according to the technique described by Monnet 4 (Figure 3). Closure of the thoracic cavity was performed with circumcostal sutures, followed by simple continuous closure of the regional muscle, subcutaneous tissue and skin.
FIGURE 3.
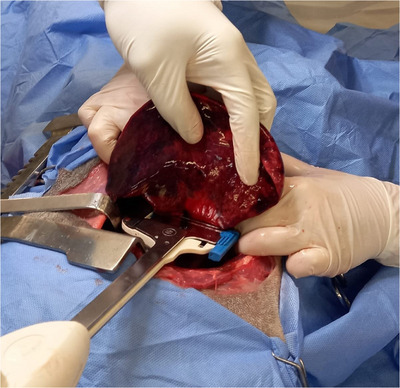
Total caudal left lung lobectomy through lateral thoracotomy
Research assistants monitored each participant during the procedures and recorded the following data for each technique: the time interval between skin incision and completion of pulmonary lobectomy, the time interval between the placement of the first suture and complete skin closure, the total time spent, the incision length, the percentage of lobe removed with each technique (Figures 4 and 5) and any iatrogenic damage that occurred during the procedure. In this last aspect, although lung leakage tests were not performed, visual assessment of lacerations on the surface of the lungs and liver, damage to large blood vessels and other potential tissue damage caused by the surgical procedure was performed.
FIGURE 4.

Comparison of the total lung lobe area obtained through a lateral thoracotomy (left) or transdiaphragmatic approach (right) in a canine cadaver
FIGURE 5.

Surface area of the lung lobe obtained through the transdiaphragmatic approach (right) and rest of the lobe (left).
Statistical analysis
To test the non‐inferiority in mean procedure time of TD compared with LT, a non‐inferiority margin of 60 seconds was defined based on Jack et al. 14 A non‐inferiority power analysis was performed for the first six procedures (two for each surgeon) with the predefined 60‐second non‐inferiority margin, with an alpha set at 0.05 with 80% power. The analysis indicated that a minimum of 17 cadavers would be required to show statistical non‐inferiority.
All data are presented as the mean, standard deviation (SD) and range of values obtained during the performance of the TD and LT approaches for caudal pulmonary lobectomy in canine cadavers.
Comparisons between the three surgeons were carried out using ANOVA and the Duncan test. The surgical duration data were first tested for normality using the Shapiro‐Wilk test, and either the Student's t‐test or the assigned rank test was used to compare the two techniques.
Descriptive analysis was carried out to compare the surgical time, incision length and percentage of the lobe removed for the two approaches. The difference in the percentage of the lobe removed was also analysed according to whether a right or left TD was performed.
Descriptive statistics were performed in Microsoft Excel 2016 (Office 16, Microsoft), and all other analyses were performed in SAS 9.4 (SAS Institute).
RESULTS
Eighteen fresh cadavers with a mean weight of 25.13 kg (SD 5.29, range 15.3–39.2) were used in this study. TD and LT were performed on each cadaver. None was discarded during or after the study.
With a confidence level of 95%, it was shown that there were no significant differences in any of the measured time intervals among the three surgeons. Overall, there were no significant differences in the time taken to complete the two surgical techniques (TD: 1155.0 seconds, SD 232.8, range 817.8–1755.0; LT: 1126.8 seconds, SD 180.6, range 753.6–1627.8) (p = 0.6131). The upper limit of the 95% confidence interval (CI) for the difference in the means between the TD and LT groups was 47 seconds. This was below the predefined non‐inferiority margin of 60 seconds; therefore, we could conclude that the TD approach was non‐inferior to the LT approach (Table 1).
TABLE 1.
Comparison of variables for both of the pulmonary lobectomy techniques
| Variable | TD | LT | p‐Value | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | ||
| T1 | 390.0 | 92.4 | 259.8‒567.0 | 465.6 | 129.0 | 303.0‒820.0 | 0.0432 |
| T2 | 765.0 | 168.6 | 459.0‒1188.0 | 660.6 | 162.6 | 456.0‒1203.0 | 0.0243 |
| Tt | 1155.0 | 232.8 | 817.8‒1755.0 | 1126.8 | 180.6 | 756.3‒1627.8 | 0.6131 |
| Incision length | 20.99 | 2.1 | 17.5‒25.5 | 19.73 | 1.84 | 16.5‒23.9 | 0.0170 |
Abbreviations: LT, lateral thoracotomy; SD, standard deviation; TD, transdiaphragmatic; Tt, total time spent; T1, time interval between skin incision and completion of pulmonary lobectomy; T2, time interval between the placement of the first suture and complete skin closure.
The time interval between skin incision and completion of pulmonary lobectomy (T1) was significantly longer for LT (465.6 seconds, SD 129.0, range 303.0‒820.0) than for TD (390 seconds, SD 92.4, range 259.8‒567.0) (p = 0.0432) (Table 1). The time interval between the placement of the first suture and complete skin closure (T2) also varied significantly between techniques, being longer for TD (765.0 seconds, SD 168.6, range 459.0–1188.0) than for LT (660.6 seconds, SD 162.6, range 456.0–1203.0) (p = 0.0243) (Table 1).
The mean cutaneous surgical incision was significantly longer for TD (20.99 cm, SD 2.1, range 17.5–25.5) than for LT (19.73 cm, SD 1.84, range 16.5–23.9) (p = 0.0170) (Table 1).
A mean of 25.83% of the surface of the lobe (SD 8.95, range 10.55‒40.72) was removed during the TD approach, while 100% of the lung lobe was always removed during the LT approach. For TD, there were no significant differences in the percentage of the caudal lung lobe removed depending on which hemithorax was approached through the diaphragm (p = 0.7900).
Finally, diaphragmatic laceration was identified in two of the 18 cadavers (11.11%) during TD. In both cases, the lacerations were secondary to the use of scissors to enlarge the approach, and both were sutured without incident. No iatrogenic damage was observed during LT.
DISCUSSION
To the best of the authors' knowledge, this is the first published report of a study in which two techniques to approach the thoracic cavity for lung lobectomies have been compared.
Although the power analysis showed that significant results could have been obtained with 17 cadavers, we decided to add one more cadaver so that each surgeon would have six cadavers in total and could perform each of the approaches six times.
Although we observed statistical differences between the two surgical approaches when evaluating T1 and T2, there were no differences in the total time spent between the two techniques. During the study, a non‐inferiority test was established to demonstrate that the TD approach for lung lobectomies was not significantly worse than the LT approach. A non‐inferiority margin of 60 seconds was defined based on the study by Jack et al. 14 In that study, the authors used a predefined margin of 30 seconds to compare LT and TD for open‐chest cardiopulmonary resuscitation. We considered it appropriate to double that time to 1 minute because we hypothesised that our interventions would not only be longer but would also lack urgency in a living patient. In our study, the upper limit of the 95% CI for the mean difference between the two approaches was 47 seconds, thus concluding the non‐inferiority of the TD approach.
The difference observed in T1 (TD 390 ± 92.4 seconds vs. LT 465 ± 129 seconds) may be due to the more complex dissection and approach of the thoracic cavity through an intercostal approach. In turn, the abdominal approach may be a more commonly used approach for surgeons, which could explain the shorter time required for this approach, even with a diaphragmatic opening. Performing a complete pulmonary lobectomy through LT could imply the use of more time compared to a partial lobectomy performed through TD. The closure of the diaphragmatic incision could contribute to the longer time observed for the TD approach at T2 (TD 765 ± 168.6 seconds vs. LT 660.6 ± 162.6 seconds).
The TD approach allows an average of 25.83% of the caudal pulmonary lobe to be removed. This approach therefore has a great limitation when compared to the LT approach, through which both partial and total lobectomy of the caudal lobe can be performed. The TD approach would be limited not only to the apical location of the lesion but also to the type of lesions that may benefit from a partial lobectomy, such as lung perforation, inhaled plant foreign bodies lodged at this level, or bullae. Therefore, it is of paramount importance to know the exact location of the lesion preoperatively in order to be able to consider the use of the TD approach.
The proximity of the lungs to the chest wall appears to be one of the reasons previously reported to justify the occurrence of iatrogenic damage to this organ with the LT approach. 14 In our study, there was no damage with this approach. This contrasts with other studies in both human and veterinary medicine, with reported incidences of iatrogenic lung injuries in between 28.6% and 36% of cases. 14 , 21
Other potential complications that would require evaluation during the TD approach are iatrogenic damage to other structures and organs in both the abdominal and thoracic cavities. In this regard, in our study, only two small diaphragmatic lacerations were caused in two of the cadavers when performing the TD approach. These injuries originated from the cranial and paraxiphoid enlargement of the abdominal incision and were sutured without incident. No iatrogenic lung injury occurred with the TD approach, similar to what was described by Jack et al. 14 However, in that study, liver damage was found in 21.4% of patients with the TD approach, contrary to our study, where no damage was caused to this organ in any of the procedures.
LT has been associated with numerous complications, mainly postoperative pain, lameness, rib fractures and pulmonary trauma. 3 , 14 , 22 The preservation of muscular structures has been shown to reduce postsurgical pain in LT. 5 , 22 Moreover, postoperative pain seems to be largely associated with potential nerve entrapment caused by the circumcostal sutures used to close the thoracic cavity. 6 In our study, we decided not to preserve the latissimus dorsi during the intercostal approach because the analysis of postsurgical pain was not the objective of the study and because we believed that it would not influence the results obtained.
Thoracoscopy and VATS have been developed as alternative techniques to traditional methods of pulmonary lobectomy with the aim of reducing surgical pain and improving postsurgical recovery. 11 , 23 , 24 , 25 , 26 However, they have the disadvantage of being technically more difficult procedures and economically more expensive. 9 , 10 , 11
TD approaches have previously been used in both veterinary and human medicine to target intrathoracic structures. In veterinary medicine, the TD approach has been shown to be feasible to perform cardiopulmonary resuscitation, 14 for the placement of cardiac pacemakers 12 , 15 , 16 or as an approach to perform pericardiectomies in dogs. 13 Similarly, this approach has also been used for lung biopsies in rabbits, 27 porto‐azygous shunt attenuation, 17 ablation of the chyle cisterna 28 and thoracic duct ligation in dogs. 18 In addition, Calvo et al. 29 used this approach in combination with caudal sternotomy for the removal of a foreign body that had migrated from the stomach into the heart.
Along with these examples, it is important to highlight that, according to Sériot et al. 30 and Baudin Tréhiou et al., 31 82.5% and 90.9%, respectively, of grass awn foreign bodies migrate into the respiratory system by perforating the caudal lobes. The TD approach could facilitate resolution of the problem in these cases where the foreign body is positioned in the apical area of the lobe due to the greater ease of performing a ventral celiotomy instead of an intercostal approach. In addition, when dealing with grass awn foreign bodies, it is not uncommon to observe the abdominal location of the grass awn with a lesion at some point in the migratory tract, especially at the thoracic level in case of inhaled foreign bodies. 30 , 32 , 33 In these cases, this technique allows exposure of the caudal thorax and the abdomen through a single incision. In this way, the morbidity and possible complications of wounds, recovery times and hospital stays, costs and postoperative pain can be reduced compared to a double approach to the thorax and abdomen at the same time. 20 , 34
Potential disadvantages of the TD approach include insufficient access to the required portion of the caudal lung lobe and potential cross‐contamination between the thoracic and abdominal cavities, with surgical site infection of both at the same time. 14 To date, none of these complications has been described in clinical cases.
There are limitations in this study that are inherently associated with ex vivo studies. A leak test after pulmonary lobectomy was not performed. It was decided not to perform the leak test since our study was not intended to evaluate the pulmonary lobectomy technique using surgical stapling but rather to demonstrate that the TD approach is a valid alternative surgical technique to more traditional techniques for performing caudal partial pulmonary lobectomy in canine patients. Another limitation could be the non‐section of the pulmonary ligament in the TD approach. In a lateral approach, this ligament must be transected in order to mobilise externally the caudal lobe for removal. 4 In the absence of a previous description of the TD approach for pulmonary lobectomy, we decided not to section it because we believed that it would not influence the caudal traction of the lobe. Future studies would be required to verify whether it influences the total volume of lung lobe that can be removed. Despite these limitations, the TD approach was completed satisfactorily by all three surgeons, who did not encounter major difficulties in performing it despite not having performed it previously.
To the best of our knowledge, no previous study has directly compared the TD approach with a lateral intercostal approach to address caudal lung lobe pathology. Our study supports the hypothesis of non‐inferiority of TD compared to LT by comparing the time necessary to complete the surgeries. We also report the amount of caudal lung lobe able to be removed via a TD approach in cadavers that weigh between 15.3 and 39.2 kg. Iatrogenic damage, which could cause an intraoperative complication in a living patient, is rare.
In summary, the TD approach could be considered as a surgical technique to perform a right or left partial caudal pulmonary lobectomy in canine cadavers, but more research is required prior to its use in live patients.
AUTHOR CONTRIBUTIONS
Conceptualisation: Jose Luis Fontalba‐Navas. Design of the study: Jose Luis Fontalba‐Navas and Jesus Rodriguez‐Quiros. Acquisition of data: Samuel Rico‐Hidalgo, Jose Luis Fontalba‐Navas and Marta Fabregas‐Mena. Analysis and interpretation of data: Samuel Rico‐Hidalgo, Jose Luis Fontalba‐Navas, Marta Fabregas‐Mena and Jesus Rodriguez‐Quiros. Drafting of the article: Samuel Rico‐Hidalgo and Marta Fabregas‐Mena. Revision: Samuel Rico‐Hidalgo, Jose Luis Fontalba‐Navas, Luis Matres‐Lorenzo, Ignacio Calvo and Jesus Rodriguez‐Quiros. Final approval: Jose Luis Fontalba‐Navas, Luis Matres‐Lorenzo, Ignacio Calvo and Jesus Rodriguez‐Quiros.
CONFLICT OF INTEREST STATEMENT
The authors declare they have no conflicts of interest.
FUNDING INFORMATION
The authors received no specific funding for this work.
ETHICS STATEMENT
This study is approved by the Ethics and Animal Experimentation Committee of the Hospital Clinico Veterinario Complutense (Madrid, Spain; approval number: 08‐2022).
ACKNOWLEDGEMENTS
We thank the Veterinary Anatomy and Embryology Department of the Faculty of Veterinary Medicine at Complutense University of Madrid for their technical support and knowledge. In addition, we are sincerely thankful to Ricardo Garcia Mata for his technical assistance with the statistical analysis.
Rico‐Holgado S, Fontalba‐Navas J, Fabregas‐Mena M, Matres‐Lorenzo L, Calvo I, Rodriguez‐Quiros J. Feasibility of lung lobectomy through a transdiaphragmatic approach in dogs. Vet Rec. 2024;e4394. 10.1002/vetr.4394
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Caywood DD, Lipowitz AJ. Surgical approaches and techniques for managing pulmonary disease. Vet Clin North Am Small Anim Pract. 1987;17(2):449–467. [DOI] [PubMed] [Google Scholar]
- 2. Mayhew PD, Hunt GB, Steffey MA, Culp WTN, Mayhew KN, Fuller M, et al. Evaluation of short‐term outcome after lung lobectomy for resection of primary lung tumors via video‐assisted thoracoscopic surgery or open thoracotomy in medium‐ to large‐breed dogs. J Am Vet Med Assoc. 2013;243(5):681–688. [DOI] [PubMed] [Google Scholar]
- 3. Moores AL, Halfacree ZJ, Baines SJ, Lipscomb VJ. Indications, outcomes and complications following lateral thoracotomy in dogs and cats. J Small Anim Pract. 2007;48(12):695–698. [DOI] [PubMed] [Google Scholar]
- 4. Monnet EL. Lungs. In: Johnston SA, Tobias KM, editors. Veterinary surgery: small animal. 2nd ed. St. Louis, MI: Elsevier; 2018. p. 1983–1999. [Google Scholar]
- 5. Yoon HY, Lee S, Jeong SW. Intercostal thoracotomy in 20 dogs: muscle‐sparing versus traditional techniques. J Vet Sci. 2015;16(1):93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rooney MB, Mehl M, Monnet E. Intercostal thoracotomy closure: transcostal sutures as a less painful alternative to circumcostal suture placement. Vet Surg. 2004;33(3):209–213. [DOI] [PubMed] [Google Scholar]
- 7. Bleakley S, Phipps K, Petrovsky B, Monnet E. Median sternotomy versus intercostal thoracotomy for lung lobectomy: a comparison of short‐term outcome in 134 dogs. Vet Surg. 2018;47(1):104–113. [DOI] [PubMed] [Google Scholar]
- 8. Landreneau RJ, Hazelrigg SR, Mack MJ, Dowling RD, Burke D, Gavlick J, et al. Postoperative pain‐related morbidity: video‐assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 1993;56(6):1285–1289. [DOI] [PubMed] [Google Scholar]
- 9. Peláez MJ, Jolliffe C. Thoracoscopic foreign body removal and right middle lung lobectomy to treat pyothorax in a dog. J Small Anim Pract. 2012;53(4):240–244. [DOI] [PubMed] [Google Scholar]
- 10. Walton RS. Video‐assisted thoracoscopy. Vet Clin North Am Small Anim Pract. 2001;31(4):729–759. [DOI] [PubMed] [Google Scholar]
- 11. Case JB. Advances in video‐assisted thoracic surgery, thoracoscopy. Vet Clin North Am Small Anim Pract. 2016;46(1):147–169. [DOI] [PubMed] [Google Scholar]
- 12. Fingeroth JM, Birchard SJ. Transdiaphragmatic approach for permanent cardiac pacemaker implantation in dogs. Vet Surg. 1986;15(4):329–333. [Google Scholar]
- 13. De Ridder M, Kitshoff A, Devriendt N, Or M, Rubio‐Guzman A, de Rooster H. Transdiaphragmatic pericardiectomy in dogs. Vet Rec. 2017;180(4):95. [DOI] [PubMed] [Google Scholar]
- 14. Jack MW, Wierenga JR, Bridges JP, Baltzer WI, Crosse KR. Feasibility of open‐chest cardiopulmonary resuscitation through a transdiaphragmatic approach in dogs. Vet Surg. 2019;48(6):1042–1049. [DOI] [PubMed] [Google Scholar]
- 15. Fox PR, Mattiesen DT, Purse D, Brown NO. Ventral abdominal, transdiapragmatic approach for implantation of cardiac pacemakers in the dog. J Am Vet Med Assoc. 1986;189(10):1303–1308. [PubMed] [Google Scholar]
- 16. Visser LC, Keene BW, Mathews KG, Browne WJ, Chanoit G. Outcomes and complications associated with epicardial pacemakers in 28 dogs and 5 cats. Vet Surg. 2013;42(5):544–550. [DOI] [PubMed] [Google Scholar]
- 17. Or M, Kitshoff A, Devriendt N, De Ridder M, Quist‐Rybachuk G, de Rooster H. Transdiaphragmatic approach to attenuate porto‐azygos shunts inserting in the thorax. Vet Surg. 2016;45(8):1013–1018. [DOI] [PubMed] [Google Scholar]
- 18. Staiger BA, Vet M, Stanley BJ, Acvs D. Single paracostal approach to thoracic duct and cisterna chyli: experimental study and case series. Vet Surg. 2011;40:786–794. [DOI] [PubMed] [Google Scholar]
- 19. Garcia‐Pertierra S, Das S, Burton C, Barnes D, Murgia D, Anderson D, et al. Surgical management of intrathoracic wooden skewers migrating from the stomach and duodenum in dogs: 11 cases (2014–2020). J Small Anim Pract. 2022;63(5):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tillson DM. Thoracic surgery: important considerations and practical steps. Vet Clin North Am Small Anim Pract. 2015;45(3):489–506. [DOI] [PubMed] [Google Scholar]
- 21. Puchwein P, Sommerauer F, Clement HG, Matzi V, Tesch NP, Hallmann B, et al. Clamshell thoracotomy and open heart massage—a potentially life‐saving procedure can be taught to emergency physicians: an educational cadaveric pilot study. Injury. 2015;46(9):1738–1742. [DOI] [PubMed] [Google Scholar]
- 22. Nutt AE, Knowles TG, Nutt NG, Murrell JC, Carwardine D, Meakin LB, et al. Influence of muscle‐sparing lateral thoracotomy on postoperative pain and lameness: a randomized clinical trial. Vet Surg. 2021;50(6):1227–1236. [DOI] [PubMed] [Google Scholar]
- 23. Walsh PJ, Remedios AM, Ferguson JF, Walker DD, Cantwell S, Duke T. Thoracoscopic versus open partial pericardectomy in dogs: comparison of postoperative pain and morbidity. Vet Surg. 1999;28(6):472–479. [DOI] [PubMed] [Google Scholar]
- 24. Nagahiro I, Andou A, Aoe M, Sano Y, Date H, Shimizu N. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg. 2001;72(2):362–365. [DOI] [PubMed] [Google Scholar]
- 25. Gonzalez‐Zamora JF, Perez‐Guille B, Soriano‐Rosales RE, Jimenez‐Bravo‐Luna MA, Gutierrez‐Castrellon P, Ridaura‐Sanz C. Video‐assisted thoracoscopy for diaphragmatic plication: experimental study in canine model. J Laparoendosc Adv Surg Tech. 2005;15(6):661–666. [DOI] [PubMed] [Google Scholar]
- 26. Laksito MA, Chambers BA, Yates GD. Thoracoscopic‐assisted lung lobectomy in the dog: report of two cases. Aust Vet J. 2010;88(7):263–267. [DOI] [PubMed] [Google Scholar]
- 27. Wittmaack MCN, da Câmara Barros FFP, do Espírito Santo Silva P, Matsui A, Sembenelli G, Mariano RSG, et al. The feasibility and effectiveness of thoracoscopic transdiaphragmatic approach for lung biopsy in rabbits. A randomized study. Acta Cir Bras. 2020;35(5):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sakals S, Schmiedt CW, Radlinsky MG. Comparison and description of transdiaphragmatic and abdominal minimally invasive cisterna chyli ablation in dogs. Vet Surg. 2011;40(7):795–801. [DOI] [PubMed] [Google Scholar]
- 29. Calvo I, Weilland L, Pratschke K. Traumatic myocardial laceration as a result of suspected cranial migration of a sewing needle from the stomach of a dog. Aust Vet J. 2011;89(11):444–446. [DOI] [PubMed] [Google Scholar]
- 30. Sériot P, Dunié‐Mérigot A, Tréhiou CB, Blond L, Bernardin F, Poujol L, et al. Treatment and outcome of spontaneous pneumothorax secondary to suspected migrating vegetal foreign body in 37 dogs. Vet Rec. 2021;189(4):e22. [DOI] [PubMed] [Google Scholar]
- 31. Baudin Tréhiou C, Gibert S, Sériot P, Dunié‐Mérigot A, Blond L. CT is helpful for the detection and presurgical planning of lung perforation in dogs with spontaneous pneumothorax induced by grass awn migration: 22 cases. Vet Radiol Ultrasound. 2020;61(2):157–166. [DOI] [PubMed] [Google Scholar]
- 32. Hopper BJ, Lester N V., Irwin PJ, Eger CE, Richardson JL. Imaging diagnosis: pneumothorax and focal peritonitis in a dog due to migration of an inhaled grass awn. Vet Radiol Ultrasound. 2004;45(2):136–138. [DOI] [PubMed] [Google Scholar]
- 33. Hennessey E, Cassel N, Nuth E, Biller D. CT can identify characteristic features of hypaxial muscle abscesses in dogs due to presumed migrating vegetal foreign material as well as additional changes along the migratory tract in other anatomic regions. Vet Radiol Ultrasound. 2022;63(6):691–698. [DOI] [PubMed] [Google Scholar]
- 34. Dhaliwal RS, Kalkat MS. One‐stage surgical procedure for bilateral lung and liver hydatid cysts. Ann Thorac Surg. 1997;64(2):338–341. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


