Abstract
Background
Traditional dental anatomy education, reliant on cadaver dissections and lectures, faces challenges such as high costs, ethical concerns, and difficulty conveying complex 3D dental structures. Virtual reality (VR) offers a solution by providing immersive, interactive learning environments that can enhance students’ understanding. This study systematically reviews the effectiveness of VR in dental anatomy education compared to traditional methods, focusing on its potential to improve learning outcomes.
Methods
A comprehensive search was conducted across Web of Science (WoS), PubMed, and Scopus databases until May 2024. Data were extracted, summarized, and analyzed for qualitative synthesis. The following keywords and their combinations were used: " dental OR dentistry”, “education OR teaching”, “virtual AND reality OR VR”, and “anatomy OR dental AND anatomy”. Studies were included if they met the following criteria: Investigated the use of VR in anatomy education. Compared VR-based learning to other methods such as lecture-based teaching, 3D printed or natural models, or non-interactive 3D models. Quantitative synthesis was performed using standardized mean differences (SMD) with Hedges’d and 95% confidence intervals (CI).
Results
Out of 178 records screened, seven studies were included in the meta-analysis and eight in the personal evaluation analysis. The analysis indicates a moderately positive effect of VR on dental anatomy education (SMD = 0.74, p = 0.05) compared to lecture-based education using X-ray, CBCT, or 3D models. However, at the same time, VR falls short compared to clinical experience, training with physical teeth, or quality printed models. Studies reported rare cases of discomfort, disorientation, diplopic image, and VR sickness.
Conclusions
The use of VR-based learning moderately positively affects educational outcomes, and enhances knowledge retention, especially before clinical experience. The personal evaluation of students showed a strong interest in VR, with positive feedback on its ease of use, accuracy, and educational value.
Keywords: Dental education, Dentistry, Virtual reality, VR, Systematic review, Meta-analysis
Introduction
For centuries, the cornerstone of anatomy education has been a solemn ritual—the study of cadavers. With its meticulous precision and raw exposure to the human form, dissection has provided an invaluable hands-on experience that has shaped generations of medical professionals [1]. However, this traditional method is not without its limitations. Access to cadavers can be severely restricted by cost, ethical considerations surrounding body donation, and regional variations in availability [2]. Even when available, traditional methods often struggle to effectively convey the body’s intricate three-dimensionality [3]. Static images in textbooks and even physical models fail to capture the dynamic relationships between muscles, organs, and bones. This is where virtual reality (VR) is poised to revolutionize how we learn about the human body [4, 5]. While foundational in imparting theoretical knowledge, traditional lecture-based teaching often falls short in delivering the spatial and interactive understanding necessary for mastery of complex anatomical structures. Lectures rely heavily on static images and diagrams, which can be abstract and difficult for students to translate into a three-dimensional understanding of the human body, and students allowed to experience the VR report positive feedback [6]. Moreover, the passive nature of lectures can limit student engagement and retention of information. This approach contrasts sharply with VR’s immersive, interactive experience, which can transform anatomy education from a passive memorization experience to an active exploration and discovery journey [7, 8]. Similarly, three-dimensional (3D) printed models are beneficial for providing tactile learning aids and improving practical learning outcomes [9, 10]. Although these models offer a tangible representation of anatomical structures, they are static and cannot demonstrate physiological processes or allow for the dynamic manipulation of parts [11]. These models can also be expensive and may not capture the fine details necessary for a comprehensive understanding of complex anatomy. Non-interactive 3D models, whether digital or physical, similarly fail to provide the interactive experience that VR can offer.
In the field of microsurgery, the need for precise anatomical knowledge is paramount. This is true for example in neurosurgery, ophthalmic surgery, or dentistry, as professionals work in a limited workspace and manipulate small, delicate tissues. The understanding of oral and maxillofacial anatomy, including the relationships between teeth, bones, nerves, and blood vessels. Traditional methods of teaching anatomy, which often rely on cadavers, textbooks, and non-interactive models, can be insufficient for conveying the complexities of these structures. VR technology, however, offers a powerful tool to enhance dental education by providing a fully immersive, interactive experience [12]. Dental students can use VR to explore detailed virtual models of the oral cavity, manipulate these models to observe structures from different angles, and even simulate dental procedures, gaining valuable hands-on experience in a risk-free environment [13]. VR technology creates a fully immersive, simulated environment that users can interact with in a seemingly real or physical way [14]. This potential transformation in anatomy education shifts the experience to an active journey of exploration and discovery, as shown in a recent study by Chen et al., where participants scored best post-intervention in VR and cadaver groups [8]. VR technology offers an immersive experience and the potential to enhance anatomy education in several ways [15–17]:
Enhanced Visualization: VR allows students to explore a detailed virtual human body. They can rotate, zoom in, and dissect layers, gaining a superior understanding of spatial relationships between organs, muscles, and bones. This surpasses the limitations of static 2D images and even 3D models, offering a dynamic and interactive learning experience.
Overcoming Cadaver Limitations: VR can alleviate the challenges associated with cadaver dissection. Access to cadavers can be limited due to ethical restrictions, costs, and regional variations. VR offers a readily available and standardized alternative, ensuring all students have equal access to a complete and realistic anatomical model.
Engaging Active Learning: VR transforms anatomy learning from passive observation to active exploration. Students can virtually dissect a body, isolate specific structures, and even visualize physiological processes like blood flow or nerve impulses. This improves knowledge retention and promotes critical thinking skills.
Addressing Ethical Concerns: The use of cadavers raises ethical considerations regarding body donation and respect for the deceased. VR offers an alternative that avoids these concerns while still providing a realistic and comprehensive learning experience.
Benefit for patients: A study by Fahim et al. 2022 reports the potential of VR and AR in overcoming dental phobia especially in pediatric patients [18].
The primary aim of this systematic review and meta-analysis is to evaluate the effectiveness of VR technology in dental anatomy education compared to other teaching methods.
Practical applications of VR for anatomy education
The potential of VR in anatomy education is rapidly transforming classrooms and training labs. VR technology enables students to explore a meticulously detailed virtual human body with unprecedented realism and interactivity [19]. By providing a dynamic and interactive learning environment, VR enhances students’ ability to comprehend complex anatomical structures and physiological processes, especially in times such as the COVID-19 pandemic, when personal interaction needs to be limited [20, 21]. Moreover, VR models can simulate various pathological conditions and surgical procedures, allowing students to practice critical thinking and decision-making in realistic clinical scenarios [8, 22]. In Table 1, specific applications that showcase its versatility, are presented [23–25].
Table 1.
Applications and benefits of VR in dental anatomy education
| Application | Description | Benefits |
|---|---|---|
| Interactive Anatomy | Students explore a detailed 3D human body model |
- Independent learning and exploration - Self-directed manipulation of structures Visualization of spatial relationships |
| Augmented Dissection | VR overlays information onto cadavers during dissection |
- Combines traditional and digital learning - Provides real-time visualizations of physiological processes - Enhances understanding of anatomical structures |
| VR Patient Simulations | Medical professionals practice procedures in realistic virtual environments |
- Safe and realistic training for complex scenarios - Improves decision-making skills and reduces errors - Enhances preparation for real-world patient care |
| Advanced Visualization Techniques | Visualize physiological processes in real time |
- Understand dynamic bodily functions - Gain a holistic view of anatomy and physiology - Enhance comprehension of complex systems |
| Dental Anatomy and Procedures | Explore detailed virtual models of the oral cavity |
- Practice dental techniques in a risk-free setting - Understand relationships between oral structures - Develop practical skills and confidence |
| Collaborative and Remote Education | Shared virtual spaces for collaborative learning |
- Enables remote education - Fosters collaboration and peer support - Enhances learning through interaction |
| Continuous Professional Development | Ongoing training for healthcare professionals |
- Rehearse complex procedures - Stay updated with latest techniques - Improve patient care and outcomes |
By embracing these practical applications, VR technology has the potential to significantly enhance the quality and accessibility of all visually dependent education, not only dental, or anatomy, paving the way for more effective and inclusive training for future healthcare professionals.
Materials and methods
This systematic review and meta-analysis study was registered in OSF Registries, registration DOI: 10.17605/OSF.IO/4HYQC.
Search strategy
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [26]. The Population, Intervention, Comparison, and Outcomes (PICO) framework was used to develop the research eligibility criteria [27]: population (dentistry students, practitioners), intervention (education using virtual reality), comparison (other types of lectures), and outcome (higher educational value). The review question: Is virtual reality enhancing dental anatomy education? Secondary research question: How do participants evaluate the VR experience?
A comprehensive literature search was conducted across multiple databases, including PubMed, Scopus, Web of Science, and Google Scholar to identify relevant studies. The search included articles published up to May 2024. The following keywords and their combinations were used: " dental OR dentistry”, “education OR teaching”, “virtual AND reality OR VR”, and “anatomy OR dental AND anatomy”.
Study inclusion and exclusion criteria
Studies were included if they met the following criteria: Investigated the use of VR in anatomy education. Compared VR-based learning to other methods such as lecture-based teaching, 3D printed or natural models, or non-interactive 3D models. Reported outcomes related to learning effectiveness, knowledge retention, spatial understanding, and student engagement. Published in peer-reviewed journals and available in English.
Studies were excluded if they: Focused solely on augmented reality (AR) without VR. Did not provide comparative data between VR and traditional methods. Were conference abstracts, reviews, or editorials and were not available in full text.
Data extraction
Two independent reviewers (KB and SH) extracted data from the selected studies. Discrepancies were resolved through discussion and consultation with a third reviewer (HEF). The following data were extracted: study characteristics (author, year, country); participant demographics (number, age, gender); intervention details (type of VR system, duration of use); comparator details; outcomes measured (test scores, retention rates, spatial understanding, interest levels), board approval/informed consent, and key findings. For studies that provided qualitative data, thematic analysis was performed to identify common themes and insights related to the use of VR in anatomy education. This included student and instructor feedback on the advantages and challenges of VR technology. The primary and secondary outcomes measures included: Educational value and knowledge retention (pre- and post-intervention test scores). Accuracy, ease of use, and spatial understanding (assessed through practical exams and self-administered questionnaires). Student interest (measured by engagement scales and self-administered questionnaires).
Data synthesis and analysis
All analyses were conducted using SPSS v29 software (IBM SPSS Statistics for Windows, Version 29.0.2.0, Armonk, NY, USA). For studies reporting comparable quantitative test score data, effect sizes were calculated using standardized mean differences (SMD) with Hedges’d and 95% confidence intervals (CI). Forest plots were used to graphically visualize the findings, providing a clear representation of the effect sizes and their corresponding confidence intervals across the included studies. Heterogeneity among the studies was assessed using the I² statistic, which measures the percentage of total variation across studies due to heterogeneity rather than chance. An I² value greater than 50% was interpreted as indicating substantial heterogeneity, suggesting that the variation in effect sizes was likely due to differences between the studies rather than random variation. Due to the low number of available studies, no subgroup analyses were performed.
Publication bias was assessed using a funnel plot and Egger’s test for asymmetry, where p < 0.1 in Egger’s test indicates the presence of publication bias [28, 29]. P-values lower than 0.05 were considered significant. The quality of the included studies was assessed based on the Newcastle-Ottawa Scale (NOS). Each study was evaluated for potential selection, comparability, and reporting biases, where scores 0–3 represent low quality (high risk of bias), 4–6 moderate quality (medium risk), and 7–9 high quality [30].
Results
Study selection and characteristics
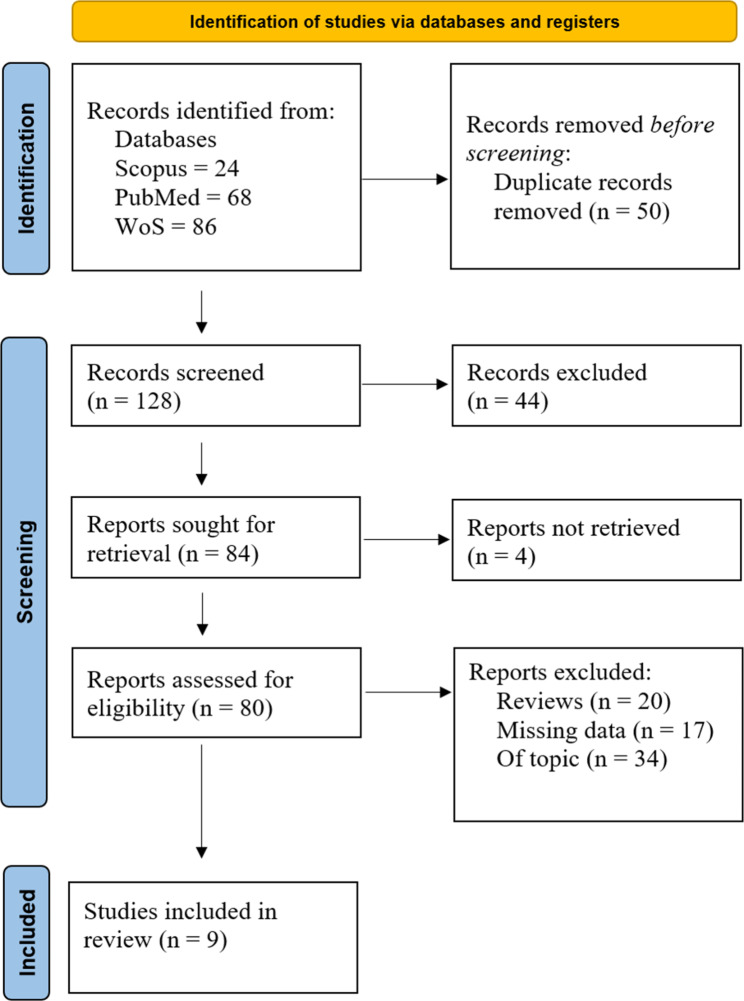
In total, 178 results were retrieved from the initial database search. After removing duplicates, 128 records underwent title, keywords, and abstract screening. This excluded 44 records, leaving 84 for full-text retrieval, of which 4 were not retrieved. 80 full-text articles were assessed for inclusion eligibility which excluded 71 articles. Finally, nine studies were included in the final analysis (Fig. 1). Out of these, seven studies were included in the meta-analysis and eight in the personal evaluation analysis. These were peer-reviewed studies on the effects of VR in the education of dentistry-related applications, published between 2004 and 2024. All of these studies were randomized controlled trials; four used a between-subjects design, four used a within-subjects design, and one was observational. These studies included 563 eligible participants (547 1st -4th year dentistry students and 16 dentists). Student mean age based on reported data was 22.18 ± 2.32. The sex distribution was 53.8% male and 46.2% female. Five studies were conducted in the USA, two in Germany, and one each in Saudi Arabia and Brazil.
Fig. 1.
PRISMA flow diagram
Various VR modalities and software/hardware combinations were used in the study groups. The interventions for control groups included educational methods such as standard lecture-based sessions, visual inputs using either X-Ray or CBCT and non-interactive 3D models. Interactive models used naturally extracted teeth or 3D printed models. The duration of the interventions ranged from 15 to 20 min, through 2 h to three two-week sessions of 2,5 –3 h per day. For all research studies, primary results were determined by evaluation of test scores or multiple-choice questionnaires (MCQ). Eight studies reported student personal evaluations and satisfaction levels with the VR system or the possibility of such an educational option. Study characteristics are presented in Table 2.
Table 2.
Overview of included studies
| Study (country) Study design | Participants (gender) mean age |
Study group / Controls | Modality used | Control modality | Duration | Evaluation | Ref. |
|---|---|---|---|---|---|---|---|
|
Jasinevicius, 2004 (USA) RCT-BS |
28 dentistry students after finishing the first year (23 M:5 F) N/A | 15 / 13 |
virtual reality simulation units: Classic DentSim |
non-computer assisted units: KaVo Simulator |
Three two-week sessions of 2.5–3 h per day | Comparison of tooth preparations from randomly selected envelopes − 3 from each student combined from all three sessions divided into Class I, Class II, and full gold crown. | [39] |
|
von Sternberg, 2007 (Germany) RCT-BS |
41 students with no apicectomy experience (N/A) N/A | 20 / 21 | VOXEL-MAN on a cadaveric porcine jaw | no prior apicectomy training | 3 sessions of VR at basic, advanced and expert training | By grading of evaluated parameters (1 = best − 6 = worst), preservation of vital structures, defect volume, deviation from the intended extent of resection (2 mm) and the time required to complete the procedure | [40] |
|
Kim-Berman, 2019 (USA) RCT-WS |
109 first-year dental students, only 61 eligible (N/A) N/A | 61 / self | Virtual Dental Library using Arthea software and Android device | Real tooth identification tests | Two occasions |
VR real tooth identification tests (1) 25 questions; (2) 50 questions Final 40 MCQ test |
[41] |
|
Zorzal, 2020 (Brazil) OS |
16 dentists (12 M:4 F) 23–64 years |
16 / - | IMMPLANT a virtual reality educational tool | none | 20–30 min |
SUS questionnaire workload analysis using NASA-TL |
[42] |
|
Reymus, 2020 (Germany) RCT-WS |
42 third-year dental students (N/A) N/A | 42 / self | VR software VRED 2018 and head-mounted display |
1. Radiograph 2. CBCT |
2 h | A questionnaire of 31 questions divided into 3 parts: based on a radiograph, CBCT, VR | [43] |
|
Mahrous, 2021 (USA) RCT-WS |
70 first-year dental students after dental anatomy course (30 M:40 F) 23.3 ± 1.9 y | 70 / self | AR/VR HMD and an iPhone |
1. natural human tooth 2. 3D virtual model 3. physical 3D printed model |
During the experiment |
A questionnaire of 17 questions. Educational value was the degree to which the modality contributed to the student’s understanding of dental anatomy |
[44] |
|
Kim-Berman, 2023 (USA) RCT-WS |
90 first-year dental students (40 M:50 F) 22.9 ± 2.74 |
90 / self | Immersive View VR software with Oculus Rift |
3D imaging − 6 min 32 s CBCT − 6 min 26 s |
VR software − 10 min 50 s + 30-min learning session using VR/CBCT |
Three 10-item MCQ tests for each of the three time points, preintervention (T1), immediate postintervention (T2), and 2 weeks postintervention (T3) | [45] |
|
Alsufyani, 2023 (Saudi Arabia) RCT-BS |
69 first-year dental students (42 M:27 F) < 20–35; >20–34 |
34/35 |
Oculus Quest 2 VR software by Black Dune Studio |
conventional educational lecture for 30 min | 15–20 min | Quiz of 20 MCQ questions | [46] |
|
Samuel, 2024 (USA) RCT-BS |
52 s-year students 94 3rd + 4th year students G1 25.6 years; G2 26-27.5 years |
52/94 |
Oculus Rift S + VARIANT-VR haptic enabled iPadOS with Vuforia |
Traditional training methods (lectures, anatomical landmarks) | 30 min per student | Post-training surveys immediately after the session and after the first clinical experiences | [47] |
RCT-BS: randomized controlled trial between subjects; RCT-WS: randomized controlled trial within subjects; OS: observational study
Inter-rater reliability
The inter-investigator reliability (Kappa) was calculated by evaluating the selected titles and abstracts, resulting in a Kappa value of 0.851. This indicates a high level of reliability between the reviewers [31].
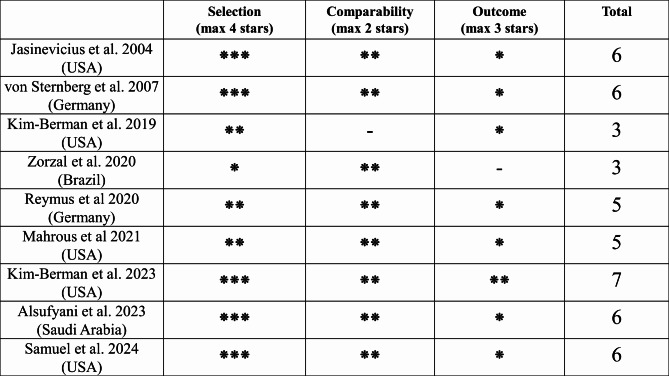
Risk of bias assessment
According to the NOS, one study was assessed as high quality, six as moderate quality, and two as low quality with high reporting bias, as shown in Fig. 2. Due to the nature of the intervention, blinding of students and teachers during the study was not practical. Most studies were found to have a low risk regarding data completeness and selective reporting. The assessment examined whether the studies avoided selective outcome reporting by ensuring that all outcomes were adequately reported in the manuscripts. Additional information to study informed consent/board approval, bias, and personal evaluation is presented in Table 3.
Fig. 2.
Risk of bias assessment according to the Newcastle-Ottawa Scale
Table 3.
Additional information on study quality and personal evaluation
| Author, year (Country) | Board-approved or Informed Consent | The study reported blinding or potential bias | Personal evaluation | Ref |
|---|---|---|---|---|
| Jasinevicius et al. 2004 (USA) | Yes | The trainers were not informed whether the students had received virtual surgery training. | N/A | [39] |
| von Sternberg et al. 2007 (Germany) | No | Authors who were blind to the identity of the grouping visually evaluated the preparations; participants received a monetary stipend at the end of the study, without prior knowledge | Self-assessment by the students | [40] |
| Kim-Berman et al. 2019 (USA) | No | Students were given extra credit in the preclinical dental anatomy continuation course for participating | Post survey questionnaire | [41] |
| Zorzal et al. 2020 (Brazil) | Yes | - |
Post survey questionnaire SUS questionnaire |
[42] |
| Reymus et al. 2020 (Germany) | Yes | - |
Post survey questionnaire Issues with interacting with VR |
[43] |
| Mahrous et al. 2021 (USA) | Yes | - | Post survey questionnaire | [44] |
| Kim-Berman et al. 2023 (USA) | Yes | - | Post survey questionnaire | [45] |
| Alsufyani et al. 2023 (Saudi Arabia) | Yes | - | Post survey questionnaire | [46] |
| Samuel et al. 2024 (USA) | Yes | Participants self-selected into the study, possibly influencing motivation. Different levels of prior clinical experience between study and control groups could influence outcomes. | Self-Reported Confidence Levels | [47] |
Data analysis – virtual reality applications and personal evaluation
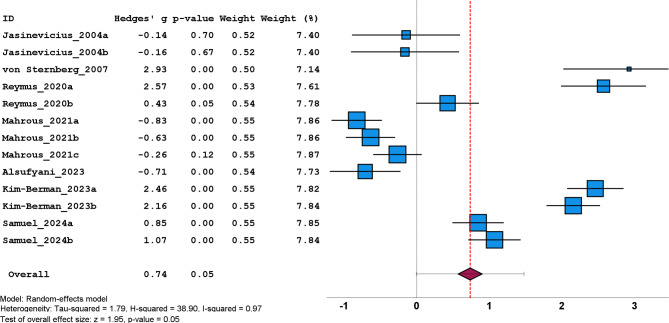
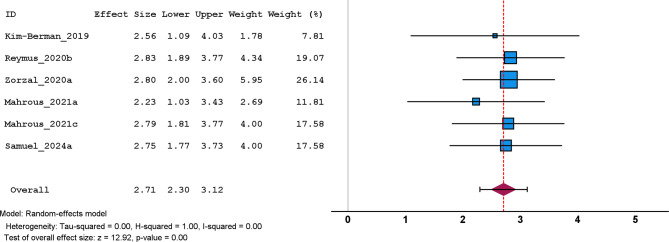
Seven studies with 13 comparable variables provided data from 486 dentistry students concerning the application of VR technology compared to lecture-based education, using X-ray, CBCT, or 3D models. In these studies, the authors used various types of VR software/hardware combinations to evaluate the effects on students’ theoretical or practical (visual) knowledge after the VR intervention. The overall effect size suggests a moderately positive effect of VR technology in dental anatomy education (SMD = 0.74) that is statistically significant with p = 0.05. This means that lectures, X-rays, and CBCTs were less effective in enhancing students’ knowledge compared to VR, however, compared to training with physical teeth, or quality printed models, VR shows slightly lower scores. In the analysis, high heterogeneity was observed (I2 = 0.97). In Fig. 3 we can see a forest plot comparing the effectiveness of VR-based anatomy education to traditional lecture-based teaching methods, indicating a moderately positive effect.
Fig. 3.
Effectiveness of VR vs. other types of lectures
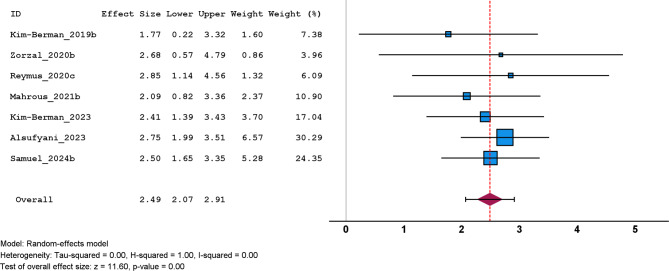
Students’ personal evaluation of the VR experience was analyzed based on two distinguishing factors. First the system’s accuracy, ease of use, and spatial understanding. Second student interest. The analyses were carried out using a pre-calculated effect size based on questionnaires normalized to a scoring system of 1 to 3, where 1 is the worst and 3 represents the best score. The forest plot in Fig. 4 illustrates the comparison between VR-based learning and hands-on clinical experience or training with physical models, such as printed anatomical models and physical teeth. Results show, that while VR is regarded as very accurate and easy to use, it falls short compared to clinical experience and training with physical models (SMD = 2.49, 95% CI = 2.07 to 2.91). The effect sizes in most studies favor physical models and clinical experience, indicating that while VR is beneficial, it does not fully replace the tactile and practical learning obtained through direct interaction with physical objects.
Fig. 4.
Personal evaluation: accuracy, ease of use, and spatial understanding compared to other educational methods
Figure 5 displays a summary of students’ personal evaluations of VR in anatomy education, highlighting their feedback on engagement. The majority of students reported a strong interest in VR technology, with positive feedback on its usability and the immersive experience it provides. Students appreciated the ability to visualize and interact with 3D anatomical structures, which enhanced their understanding and retention of the material. Two studies reported rare cases of discomfort, disorientation, diplopic image, and VR sickness.
Fig. 5.
Personal evaluation: interest and engagement levels
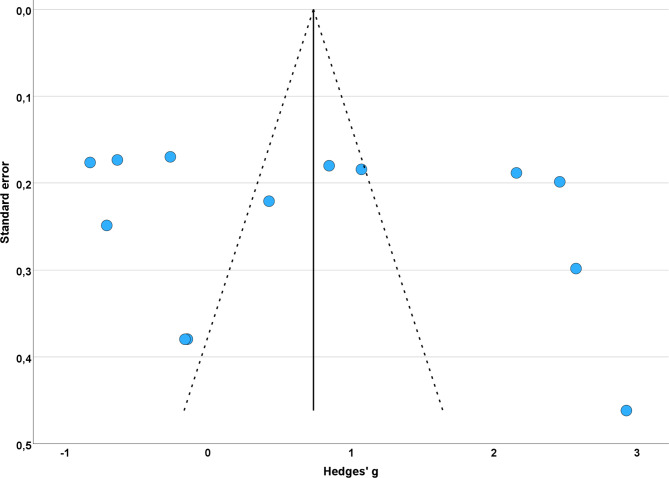
Publication bias and sensitivity analysis
For the primary analyses, funnel plots were created to check for the risk of publication bias (Fig. 6). The shape of the funnel plot appeared reasonably symmetrical, suggesting no major publication bias. Although several studies were located outside the 95% confidence intervals, this can occur due to random variation or differences in study methodologies. Additionally, Egger’s test showed non-significant asymmetry (p = 0.882), further indicating that there was no significant publication bias in this review.
Fig. 6.
Funnel plot of eect sizes for clinical trials included in the meta-analysis
A sensitivity analysis was performed to confirm the reliability of the results, due to significant heterogeneity (> 75%). When any individual study was excluded from the model, the significant effect of VR on examination scores remained consistent, with the pooled SMD staying at 0.74 (95% CI: 0.00–1.52), similar to the original results (SMD = 0.74, 95% CI: 0.00-1.47).
Discussion
The integration of VR in anatomy education offers numerous benefits, including enhanced visualization of spatial relationships, and overcoming the limitations of 2D examination methods [32]. Moreover, VR applications are slowly getting hold in many dental specialties from education to stress elevation using VR animation in child dentistry [33]. Dentistry is a specialized field, with a high emphasis on anatomical knowledge. VR allows dental students to explore detailed virtual models of the oral cavity, simulate dental procedures, and gain an almost hands-on experience in a safe and controlled environment. Our study on VR in dental anatomy education produced similar results to a recent study by Zhao et al. on VR effectiveness in teaching general anatomy, where exposure to VR moderately improved test scores in students [22]. The moderately positive impact of VR leads to an improved understanding of dental anatomy; however, our findings suggest that, when compared to clinical practice exposure, current VR hardware and particularly software are not as highly regarded.
Virtual reality (VR) technology in dental anatomy education, while offering immersive and detailed visualizations, comes with certain limitations. One significant drawback is the high cost of VR equipment, which can be prohibitive for many educational institutions [34]. Additionally, the technology requires substantial technical support and maintenance. Users often experience physical discomforts such as head pain, eye strain, and nausea due to prolonged use of VR headsets, a phenomenon known as “VR sickness [35].” These symptoms can reduce the effectiveness of VR as a learning tool by limiting the duration for which students can comfortably use the technology [36]. Moreover, the initial learning curve associated with mastering VR interfaces can be steep, potentially detracting from the time spent on actual anatomical studies. Despite these challenges, ongoing advancements in VR technology aim to mitigate these issues, making it a more viable option for education in the future.
Future developments may include even more realistic simulations and systems to mimic the tactile experience of dissection. Mannequin simulators with VR and advanced haptic feedback are already used in otorhinolaryngology [37]. It is only a matter of time before VR becomes more affordable, accessible, and accurate. This will push its integration into educational curricula, potentially becoming a standard component of medical and dental training programs [38]. The ideal approach to anatomy education likely lies in a blended learning model that combines the strengths of VR with traditional methods. This hybrid approach allows students to benefit from the hands-on experience of cadaver dissection, the theoretical knowledge from lectures, and the interactive, immersive capabilities of VR. Such a comprehensive educational strategy will foster a deeper and more nuanced understanding of human anatomy, better preparing future generations of medical and dental professionals.
Limitations of this review are mainly low sample size due to lack of more available research. Most studies don’t have a control group that complicates the comparing of scores from given educational methods. Also, most studies mainly reported post-intervention information. Age and gender information in some studies were unable to be obtained. Last, studies should report more on VR sickness and complications of using the headset.
Conclusions
The results of this meta-analysis underscore the potential of VR technology to enhance anatomy education by providing a more interactive and engaging learning experience compared to traditional lecture-based methods. VR has been shown to improve the comprehension of complex anatomical structures and offers a valuable supplement to traditional teaching methods. However, VR does not entirely replace the benefits of hands-on clinical experience and physical models, which provide essential tactile feedback and practical skills. The positive reception from students suggests a promising future for integrating VR into anatomy curricula.
By embracing VR technology, educational institutions can provide a richer, more engaging learning experience that empowers students with a profound understanding of the human body, ultimately improving the quality of healthcare provided by future professionals. Future research should explore ways to combine VR with physical models to leverage the strengths of both approaches and maximize educational outcomes.
Acknowledgements
Not applicable.
Abbreviations
- VR
Virtual reality
- SMD
Standardized mean difference
- CI
Confidence Interval
- CBCT
Cone Beam Computed Tomography
- 3D
Three-dimensional
- 2D
Two-dimensional
- AR
Augmented reality
- COVID-19
Coronavirus disease 2019
- NOS
Newcastle-Ottawa Scale
- MCQ
Multiple-choice questionnaire
- RCT-BS
Randomized controlled trial between subjects
- RCT-WS
Randomized controlled trial within subjects
- OS
Observational study
Author contributions
KB and SH designed the study, collected data, analyzed results, and wrote the first manuscript; HEF and AT contributed to manuscript revisions, third opinion, and methodology. All authors read and approved the final manuscript.
Funding
This article received no external funding.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Estai M, Bunt S. Best teaching practices in anatomy education: a critical review. Ann Anat. 2016;208:151–7. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh SK. The practice of ethics in the context of human dissection: setting standards for future physicians. Ann Anat. 2020;232:151577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Persaud A, Maus A, Strait L, Zhu D. 3D bioprinting with live cells. Eng Regeneration. 2022;3(3):292–309. [Google Scholar]
- 4.Wang CY, Yin T, Ma KH, Shyu JF, Cheng CP, Wang YC, et al. Enhancing anatomy education through cooperative learning: harnessing virtual reality for effective gross anatomy learning. J Microbiol Biol Educ. 2023;24(3):e00100–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Samadbeik M, Yaaghobi D, Bastani P, Abhari S, Rezaee R. The applications of virtual reality technology in Medical groups Teaching. J Adv Med Educ Prof. 2018;6(3):123–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Castro PL, Ginés R, Ramírez JA, Mompeó B, Domínguez L, Rodríguez A, et al. Study on the acceptance of virtual reality as a complement to the study of human anatomy. Educación Médica. 2023;24(4):100820. [Google Scholar]
- 7.Jiang H, Vimalesvaran S, Wang JK, Lim KB, Mogali SR, Car LT. Virtual reality in medical students’ education: scoping review. JMIR Med Educ. 2022;8(1):e34860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Zhu J, Cheng C, Pan Z, Liu L, Du J, et al. Can virtual reality improve traditional anatomy education programmes? A mixed-methods study on the use of a 3D skull model. BMC Med Educ. 2020;20(1):395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobroś K, Hajto-Bryk J, Zarzecka J. Application of 3D-printed teeth models in teaching dentistry students: a scoping review. Eur J Dent Educ. 2023;27(1):126–34. [DOI] [PubMed] [Google Scholar]
- 10.Kasihani NN, Rikawarastuti R, Study of 3D printing model in dental health education preclinic practices: narrative review. JDHT J Dent Hygiene Therapy. 2023;4(1):88–96. [Google Scholar]
- 11.Kolla S, Elgawly M, Gaughan JP, Goldman E. Medical Student Perception of a virtual reality Training Module for anatomy education. Med Sci Educ. 2020;30(3):1201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erdilek D, Gümüştaş B, Güray Efes B. Digitalization era of dental education: a systematic review. Dent Med Probl. 2023;60(3):513–25. [DOI] [PubMed] [Google Scholar]
- 13.Llena C, Folguera S, Forner L, Rodríguez-Lozano FJ. Implementation of augmented reality in operative dentistry learning. Eur J Dent Educ. 2018;22(1):e122–30. [DOI] [PubMed] [Google Scholar]
- 14.Joda T, Gallucci GO, Wismeijer D, Zitzmann NU. Augmented and virtual reality in dental medicine: a systematic review. Comput Biol Med. 2019;108:93–100. [DOI] [PubMed] [Google Scholar]
- 15.Yang J. Technology-enhanced Preclinical Medical Education (anatomy, histology and occasionally, Biochemistry): a practical guide. Adv Exp Med Biol. 2023;1431:65–93. [DOI] [PubMed] [Google Scholar]
- 16.Alharbi Y, Al-Mansour M, Al-Saffar R, Garman A, Alraddadi A. Three-dimensional virtual reality as an innovative teaching and Learning Tool for human anatomy courses in Medical Education: a mixed methods study. Cureus. 2020;12(2):e7085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wickramasinghe N, Thompson BR, Xiao J. The opportunities and challenges of Digital Anatomy for Medical Sciences: Narrative Review. JMIR Med Educ. 2022;8(2):e34687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fahim S, Maqsood A, Das G, Ahmed N, Saquib S, Lal A, et al. Augmented reality and virtual reality in Dentistry: highlights from the current research. Appl Sci. 2022;12(8):3719. [Google Scholar]
- 19.Aasekjær K, Gjesdal B, Rosenberg I, Bovim LP. Virtual Reality (VR) in Anatomy Teaching and Learning in Higher Healthcare Education. In: Akselbo I, Aune I, editors. How Can we Use Simulation to Improve Competencies in Nursing? Cham: Springer International Publishing; 2023 [cited 2024 Jun 4]. pp. 117–29. 10.1007/978-3-031-10399-5_10
- 20.Karbasi Z, Niakan Kalhori SR. Application and evaluation of virtual technologies for anatomy education to medical students: a review. Med J Islam Repub Iran. 2020;34:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinou N, Sinou N, Filippou D. Virtual reality and augmented reality in anatomy education during COVID-19 pandemic. Cureus 15(2):e35170. [DOI] [PMC free article] [PubMed]
- 22.Zhao J, Xu X, Jiang H, Ding Y. The effectiveness of virtual reality-based technology on anatomy teaching: a meta-analysis of randomized controlled studies. BMC Med Educ. 2020;20(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romand M, Dugas D, Gaudet-Blavignac C, Rochat J, Lovis C. Mixed and augmented reality tools in the medical anatomy curriculum. Stud Health Technol Inf. 2020;270:322–6. [DOI] [PubMed] [Google Scholar]
- 24.Gurses ME, Hanalioglu S, Mignucci-Jiménez G, Gökalp E, Gonzalez-Romo NI, Gungor A, et al. Three-Dimensional modeling and extended reality simulations of the cross-sectional anatomy of the Cerebrum, Cerebellum, and Brainstem. Oper Neurosurg (Hagerstown). 2023;25(1):3–10. [DOI] [PubMed] [Google Scholar]
- 25.Lan L, Mao RQ, Qiu RY, Kay J, de Sa D. Immersive virtual reality for patient-specific Preoperative Planning: a systematic review. Surg Innov. 2023;30(1):109–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 27.Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54(10):1046–55. [DOI] [PubMed] [Google Scholar]
- 29.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. Ottawa Hospital Research Institute. [cited 2024 Jun 5]. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 31.Mandrekar JN. Measures of interrater agreement. J Thorac Oncol. 2011;6(1):6–7. [DOI] [PubMed] [Google Scholar]
- 32.García-Robles P, Cortés-Pérez I, Nieto-Escámez FA, García-López H, Obrero-Gaitán E, Osuna-Pérez MC. Immersive virtual reality and augmented reality in anatomy education: a systematic review and meta-analysis. Anat Sci Educ. 2024;17(3):514–28. [DOI] [PubMed] [Google Scholar]
- 33.Farronato M, Maspero C, Lanteri V, Fama A, Ferrati F, Pettenuzzo A, et al. Current state of the art in the use of augmented reality in dentistry: a systematic review of the literature. BMC Oral Health. 2019;19(1):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in Medical Education and Treatment. Oman Med J. 2020;35(3):e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang E, Kim HT, Yoo B. Virtual reality sickness: a review of causes and measurements. Int J Human–Computer Interact. 2020;36(17):1658–82. [Google Scholar]
- 36.Yusof NA, Zamli Z, Wan Salleh WMS, Che Azemin MZ. Virtual reality in anatomy education: advantages and challenges. Malaysian Journal of Medicine and Health Sciences. 2022 Dec 1 [cited 2024 Jun 4];18(Supp 22). https://medic.upm.edu.my/jurnal_kami/volume_18_2022-14249?L=en
- 37.Proctor MD, Campbell-Wynn L. Effectiveness, usability, and acceptability of haptic-enabled virtual reality and mannequin modality simulators for surgical cricothyroidotomy. Mil Med. 2014;179(3):260–4. [DOI] [PubMed] [Google Scholar]
- 38.Abundez Toledo M, Ghanem G, Fine S, Weisman D, Huang YM, Rouhani AA. Exploring the promise of virtual reality in enhancing anatomy education: a focus group study with medical students. Front Virtual Real. 2024 Mar 20 [cited 2024 Jun 4];5. https://www.frontiersin.org/articles/10.3389/frvir.2024.1369794
- 39.Jasinevicius TR, Landers M, Nelson S, Urbankova A. An evaluation of two Dental Simulation systems: virtual reality versus contemporary non-computer-assisted. J Dent Educ. 2004;68(11):1151–62. [PubMed] [Google Scholar]
- 40.von Sternberg N, Bartsch MS, Petersik A, Wiltfang J, Sibbersen W, Grindel T, et al. Learning by doing virtually. Int J Oral Maxillofac Surg. 2007;36(5):386–90. [DOI] [PubMed] [Google Scholar]
- 41.Kim-Berman H, Karl E, Sherbel J, Sytek L, Ramaswamy V. Validity and user experience in an augmented reality virtual tooth identification test. J Dent Educ. 2019;83(11):1345–52. [DOI] [PubMed] [Google Scholar]
- 42.Zorzal ER, Paulo SF, Rodrigues P, Mendes JJ, Lopes DS. An immersive educational tool for dental implant placement: a study on user acceptance. Int J Med Inf. 2021;146:104342. [DOI] [PubMed] [Google Scholar]
- 43.Reymus M, Liebermann A, Diegritz C. Virtual reality: an effective tool for teaching root canal anatomy to undergraduate dental students - a preliminary study. Int Endod J. 2020;53(11):1581–7. [DOI] [PubMed] [Google Scholar]
- 44.Mahrous A, Elgreatly A, Qian F, Schneider GB. A comparison of pre-clinical instructional technologies: natural teeth, 3D models, 3D printing, and augmented reality. J Dent Educ. 2021;85(11):1795–801. [DOI] [PubMed] [Google Scholar]
- 45.Kim-Berman H, Bui D, Lee K, Mitchell V, Bonine B, Benavides E, et al. Student learning of head and neck anatomy using cone beam computed tomography and immersive virtual reality. J Dent Educ. 2023;87(8):1180–7. [DOI] [PubMed] [Google Scholar]
- 46.Alsufyani N, Alnamlah S, Mutaieb S, Alageel R, AlQarni M, Bukhari A, et al. Virtual reality simulation of panoramic radiographic anatomy for dental students. J Dent Educ. 2023;87(8):1200–9. [DOI] [PubMed] [Google Scholar]
- 47.Samuel S, Elvezio C, Khan S, Bitzer LZ, Moss-Salentijn L, Feiner S. Visuo-Haptic VR and AR Guidance for Dental Nerve Block Education. IEEE Trans Vis Comput Graph. 2024;30(5):2839–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.