Abstract
This article highlights the importance of optimizing the techniques used for isolating stromal vascular fraction cells from adipose tissue. Furthermore, by presenting key findings from the literature, it clarifies the effects of refined techniques on regenerative medicine and advocates for ongoing research and innovation to enhance therapeutic outcomes.
Keywords: Stromal vascular fraction, Adipose-derived stem cell, Regenerative medicine, Isolation technique, Mesenchymal stem cell
Core Tip: This article underscores the importance of improving stromal vascular fraction isolation from adipose-derived stem cells. By examining the advancements detailed in the referenced paper, it advocates for improving outcomes in regenerative medicine. The article emphasizes the necessity of refining techniques and continuing research to optimize clinical applications and achieve superior therapeutic results. This focus on ongoing innovation is crucial for the advancement of regenerative medicine and its potential to transform patient care.
TO THE EDITOR
This article presents insights from a minireview by Jeyaraman et al[1], who explored the isolation of stromal vascular fraction (SVF) cells from adipose tissue and their applications. The reviewers comprehensively analyzed current SVF isolation techniques and their implications for regenerative medicine and emphasized the need for precise optimization to enhance therapeutic outcomes[1]. Recent studies have highlighted the complexity and importance of SVF-based regenerative therapy. For example, Liu et al[2] demonstrated that different tissue sources and culture methods for mesenchymal stem cells (MSCs) differentially affect the composition of extracellular vesicles (EVs), influencing their angiogenic and immunomodulatory properties. This finding underscores the need for standardized protocols to ensure consistency and efficacy of SVF-based therapies[2]. Carr et al[3] elucidated the role of SVF by examining the secretomes of processed adipose grafts and SVF cells. The researchers revealed that certain SVF components strongly influence therapeutic outcomes, emphasizing the need for understanding molecular differences among SVF components[3]. Mundluru et al[4] explored advancements in nonenzymatic techniques for SVF isolation and indicated that further improvements in SVF yield and quality are needed to optimize SVF-based regenerative therapy. Qin et al[5] introduced a new protocol for isolating SVF by using clinical-grade materials, thereby bridging the gap between laboratory research and clinical practice. EVs derived from adipose-derived MSCs have various applications. For example, EVs can modulate cellular responses and promote wound healing, which highlights their potential in treating diabetic wounds and other conditions[6,7]. This finding has been corroborated by Soltani et al[8], who reviewed the efficacy of EVs in accelerating tissue regeneration. Badr et al[9] and Romano et al[10] have proposed expanding the clinical applications of SVF and adipose-derived MSCs to prevent skin aging and promote neural differentiation. The present editorial underscores the importance of continual innovation and rigorous research in the field of SVF. With technical advancements, leveraging these improvements is crucial for maximizing SVF’s clinical potential and improving therapeutic outcomes.
ADVANCEMENTS IN SVF ISOLATION TECHNIQUES
In their minireview, Jeyaraman et al[1] assessed the evolution of techniques for isolating SVF from adipose tissue, focusing on both traditional and emerging techniques. Traditional methods, such as mechanical disruption followed by enzymatic digestion, have proven effective but often lead to variations in yield and cell viability. Recent advancements have improved technical precision and efficiency, which are crucial for maximizing the therapeutic potential of SVF in regenerative medicine. Studies have reported considerable progress in research on SVF isolation techniques (Table 1). For instance, a new protocol involving the use of clinical-grade reagents has been developed to enhance yield consistency and cell viability, thereby addressing problems pertaining to variability in enzyme activity and cell damage[5]. Goulas et al[11] highlighted improvements in mechanical methods that reduce the need for harsh enzymatic treatments, thereby preserving cell integrity. These findings align with those of Mundluru et al[4], who reviewed nonenzymatic techniques and their potential for consistent SVF isolation with minimal cell damage. Evidence suggests the need for standardized protocols to ensure the reproducibility and reliability of SVF isolation techniques. Liu et al[2] demonstrated that tissue sources and cell culture methods influence the composition of EVs, thereby affecting their therapeutic efficacy. Carr et al[3] noted the differences in secretome profiles among processed adipose grafts, SVF components, and adipose-derived stem cells (ADSCs) and suggested that different secretome profiles differentially influence the functional capacities (e.g., angiogenic and immunomodulatory properties) of these adipose tissue components. These findings jointly underscore the importance of refining SVF isolation techniques to enhance cell quality and functionality. Automated closed systems for SVF isolation have garnered considerable scientific and clinical interest because of their ability to improve standardization and minimize contamination. Unlike traditional methods, which involve multiple manual steps and are prone to microbial contamination, automated systems operate within a closed environment, which markedly reduces contamination risks and ensures adherence to clinical-grade standards[4,5]. In addition, these systems offer enhanced efficiency and scalability, processing large volumes of adipose tissue more rapidly than do manual methods and fulfilling the regulatory requirements for good manufacturing practices[12,13]. This consistency is crucial for application in clinical settings, where technical reliability and reproducibility are essential. In summary, although traditional SVF isolation techniques have laid the groundwork for current practices, recent advancements offer substantial improvements in SVF yield, cell viability, and technical reproducibility. The development of standardized protocols and advanced techniques, such as automated closed systems, is essential for optimizing and expanding SVF’s clinical applications. With ongoing research and evolution, the aforementioned advancements would enhance the efficacy and safety of SVF-based therapies.
Table 1.
Various stromal vascular fraction isolation techniques and their effects on adipose-derived stem cell viability and functionality
|
Isolation techniques
|
Key features
|
ADSC viability
|
ADSC functionality
|
Ref.
|
| Enzymatic digestion (collagenase) | Commonly used method; effectively degrades extracellular matrix components | High initial viability; slight decrease in viability over time because of enzymatic exposure | Promotes adipogenesis and angiogenesis; weakens ADSCs’ immunomodulatory properties through enzymatic exposure | Jeyaraman et al[1], 2024; Garroni et al[13], 2024; Ruoss et al[14], 2024 |
| Nonenzymatic mechanical disruption | Utilizes physical methods such as centrifugation and filtration; avoids chemical agents | Generally lower initial viability than that achieved with enzymatic methods; weak effects on long-term cell viability | Maintains multipotency with fewer alterations in the secretome profile; improves preservation of native ADSC functions | Mundluru et al[4], 2024; Goulas et al[11], 2024; Tareen et al[15], 2024 |
| Centrifugation-based methods | Separates SVF on the basis of density; often combined with other techniques for enhanced purity | Moderate to high viability; dependent on centrifugation parameters, such as speed and duration | Retains adipogenic and osteogenic potential; weakens immunomodulatory properties through mechanical stress | Jeyaraman et al[1], 2024; Qin et al[5], 2024; Souza et al[6], 2024 |
| Microfluidic channel–based isolation | Advanced method utilizing microfluidic channels for precise cell sorting; minimal physical and chemical stress | High viability because of minimal manipulation; enhanced precision in the isolation of ADSCs from SVF | Preserves a wide range of cellular functions, such as differentiation potential and cytokine secretion | Liu et al[2], 2024; Carr et al[3], 2024; Li et al[12], 2024 |
| Automated closed systems | Fully automated systems with closed environments to reduce contamination; often used in clinical settings | High viability with reduced contamination risks; consistent and reproducible outcomes | Maintains functional properties, as do traditional methods; improves safety for greater clinical applicability | Soltani et al[8], 2024; Ruoss et al[14], 2024; Mohseni Meybodi et al[16], 2024 |
| Hybrid techniques (enzymatic + mechanical) | Combination of enzymatic and mechanical methods to enhance yield and viability | High viability because of the balance between enzymatic efficiency and mechanical preservation of cell integrity | Enhances functional outcomes - for example, by improving differentiation and paracrine effects; allows for tailored applications | Jeyaraman et al[1], 2024; Qin et al[5], 2024; Garroni et al[13], 2024 |
This table presents information on various stromal vascular fraction isolation techniques and their effects on adipose-derived stem cell viability and functionality. It summarizes the key features of individual techniques, indicating how they influence adipose-derived stem cells’ initial and long-term viability and functional capacities, such as differentiation potential, cytokine secretion, and immunomodulatory properties. References are provided to support the findings. ADSC: Adipose-derived stem cell; SVF: Stromal vascular fraction.
CLINICAL IMPLICATIONS OF REFINED TECHNIQUES
Advancements in SVF isolation techniques have profound clinical implications that extend well beyond the laboratory. Recent evidence suggests that refined SVF isolation techniques can markedly enhance the quality of SVF, thereby improving its regenerative properties and optimizing SVF-based therapies for various medical conditions (Table 2). Jeyaraman et al[1] emphasized the importance of these advancements for personalized medicine; higher levels of SVF purity and viability lead to better therapeutic outcomes and patient-specific responses. Refined SVF isolation techniques also enhance the consistency and reproducibility of therapeutic outcomes. Liu et al[2] demonstrated that tissue sources and culture methods affect the composition and regenerative capacity of EVs, underscoring the need for standardized protocols for optimal therapeutic efficacy[2]. Compared with traditional enzymatic techniques for SVF isolation, nonenzymatic techniques are safe because they preserve cell integrity and enhance functionality[4]. Souza et al[6] demonstrated that refined isolation techniques lead to improved clinical outcomes and enhance those cellular behaviors that are essential for achieving therapeutic objectives. Incorporating refined SVF isolation techniques into clinical practice can maximize therapeutic benefits. For instance, Carr et al[3] clarified how different SVF secretomes can be used to personalize treatment regimens. Qin et al[5] emphasized the potential of clinical-grade protocols to enhance the consistency and reliability of SVF-based therapies. Furthermore, refined techniques hold promise for treating specific conditions. In the treatment of osteoarthritis, SVF’s abundant MSCs, growth factors, and EVs ensure not only symptom relief but also cartilage repair and regeneration. Liu et al[2] suggested that optimizing MSC isolation through refined techniques can improve clinical outcomes for patients with osteoarthritis, delaying or preventing joint replacement surgery[2]. Chronic wounds, such as diabetic foot ulcers and pressure sores, present major clinical challenges. Souza et al[6] demonstrated that SVF can modulate inflammation, promote angiogenesis, and enhance tissue repair; the researchers further revealed that SVF-derived EVs influence key aspects of wound healing. Refined SVF isolation techniques ensure the retention of regenerative components, thus improving the therapeutic efficacy and reliability of SVF in chronic wound management. In cardiovascular medicine, SVF’s potential for regenerating damaged cardiac tissue is particularly compelling. SVF contains endothelial progenitor cells, which are essential for tissue repair and neovascularization. Carr et al[3] stated that optimizing SVF secretomes may enhance repair after myocardial infarction and reduce heart failure progression. Nonenzymatic techniques have been demonstrated to improve the safety and efficacy of SVF-based cardiovascular therapies by preserving cell functionality[4]. Overall, refined SVF isolation techniques have a wide range of clinical implications, offering improved therapeutic outcomes across conditions such as osteoarthritis, chronic wounds, and cardiovascular diseases. The aforementioned advancements in SVF isolation techniques represent a crucial step toward bringing SVF-based therapies from the lab to the clinic. Continual advancement and protocol standardization are essential for realizing SVF’s full potential in regenerative medicine.
Table 2.
Effects of mesenchymal stem cell source and processing protocols on extracellular vesicle composition and therapeutic efficacy
|
Variables
|
Description
|
Ref.
|
| MSC source | Different tissues (adipose, bone marrow, umbilical cord) produce EVs with different profiles. ADMSCs contain elevated levels of proregenerative factors, such as miRNAs that promote angiogenesis and modulate immune responses | Liu et al[2], 2024; Souza et al[6], 2024 |
| Processing protocols | Culture conditions and EV isolation techniques influence EV content and function. Suspension cultures improve EV yield and functionality. Hypoxic preconditioning enhances EVs with tissue repair and immunomodulatory factors | Jeyaraman et al[1], 2024; Suryawan et al[17], 2021 |
| Therapeutic efficacy | Therapeutic potential of MSC-derived EVs is associated with their specific compositional profiles. ADMSC-derived EVs are particularly effective in promoting wound healing and modulating immune responses because of their distinct miRNA and protein contents | Soltani et al[8], 2024; Symonds et al[18], 2023 |
| Challenges and considerations | Variability in EV composition necessitates careful MSC source selection and standardized processing protocols to optimize therapeutic outcomes. Standardization is essential for producing EVs with consistent therapeutic properties | Liu et al[2], 2024; Carr et al[3], 2024 |
This table summarizes the effects of different mesenchymal stem cell (MSC) sources and processing techniques on the composition and functionality of extracellular vesicle (EVs). MSCs derived from various tissues, particularly adipose tissue, yield EVs with distinct profiles. These EVs are enriched in proregenerative factors such as specific microRNAs. The methods used for cell culture and EV isolation strongly influence the yield, content, and therapeutic efficacy of EVs. For instance, suspension cultures and hypoxic preconditioning enhance the functionality of EVs. The therapeutic potential of EVs is closely associated with their compositional profiles. Therefore, selecting appropriate MSC sources and standardizing processing protocols are crucial for achieving consistent and optimal therapeutic outcomes. ADMSC: Adipose-derived mesenchymal stem cell; EV: Extracellular vesicle; miRNA: MicroRNA; MSC: Mesenchymal stem cell.
CHALLENGES AND FUTURE DIRECTIONS
Despite advancements in SVF isolation techniques, several challenges persist; these challenges must be addressed to expand SVF’s application in regenerative medicine (Table 3). Key problems in this context include scalability, automation, regulatory compliance, and protocol standardization. To improve scalability, automated systems for SVF isolation can be used to enhance consistency, reduce labor costs, and increase throughput, thereby increasing the accessibility of SVF-based therapies[1]. The application of laboratory findings to clinical practice necessitates the fulfillment of stringent regulatory requirements to ensure patient safety and therapeutic efficacy. Qin et al[5] unveiled the challenges associated with adopting new clinical-grade protocols and emphasized the need for rigorous validation to meet regulatory standards. Collaboration among researchers, clinicians, and regulatory bodies is essential to streamline approval processes and ensure that new techniques are safe and effective[5]. Tissue sources and processing conditions strongly influence the composition and functionality of SVF-derived EVs, affecting their therapeutic potential. Liu et al[2] recommended standardizing protocols to ensure the reproducibility and efficacy of SVF-based therapies. Understanding the variability in SVF components is crucial for optimizing therapies. Carr et al[3] and Souza et al[6] demonstrated that between-component differences in cellular response and secretome profile influence therapeutic outcomes. Thus, treatment personalization requires SVF components to be comprehensively profiled and subject to functional analysis. Nonenzymatic techniques optimize SVF isolation by preserving cell integrity and functionality. Mundluru et al[4] reviewed these techniques and highlighted their potential to improve the efficacy of SVF-based therapies. Continual research into nonenzymatic techniques and their clinical applicability is needed to optimize SVF-based therapies[4]. In summary, addressing challenges related to scalability, regulatory compliance, standardization, and characterization through ongoing research and collaboration is essential for successful integration of SVF-based therapies into clinical practice. By focusing on these areas, clinical researchers can overcome current barriers and fully realize the potential of SVF in regenerative medicine.
Table 3.
Recent advances in adipose-derived stem cell applications: Preconditioning techniques, clinical outcomes, and future directions
|
Preconditioning techniques
|
Clinical outcomes
|
Future directions
|
Ref.
|
| Pharmacological agent use | Increased regenerative capacity; improved immunomodulation | Exploration of novel agents and standardization of therapeutic dosages | Jeyaraman et al[1], 2024; Liu et al[2], 2024 |
| Hypoxic preconditioning | Enhanced ADSC survival; improved wound healing | Further investigation for optimizing hypoxia duration and conditions | Suryawan et al[17], 2021 |
| Mechanical stimulation | Enhanced tissue regeneration; increased cell viability | Development of standardized protocols for mechanical stimulation | Carr et al[3], 2024; Goulas et al[11], 2024 |
| EV modulation | Modulated macrophage polarization; improved anti-inflammatory effects | Investigation of EV content manipulation to optimize therapeutic effects | Souza et al[6], 2024; Symonds et al[18], 2023 |
| Chemical preconditioning | Improved angiogenic capacity; accelerated tissue repair | Identification of optimal chemical agents and concentrations | Qin et al[5], 2024; Li et al[12], 2024 |
| Cytokine preconditioning | Enhanced immunomodulatory properties; reduced inflammation | Further exploration of cytokine combinations for targeted therapies | Yin and Shen[7], 2024; Yang et al[19], 2024 |
Recent advances in adipose-derived stem cell preconditioning techniques highlight the efficacy of various methods in enhancing clinical outcomes. These techniques include hypoxic preconditioning, pharmacological agent use, mechanical stimulation, extracellular vesicle modulation, chemical preconditioning, and cytokine preconditioning. This table presents findings from recent studies, underscoring improvements in adipose-derived stem cell survival, tissue regeneration, and immunomodulation. In the future, these techniques must be optimized to maximize therapeutic efficacy. ADSC: Adipose-derived stem cell; EV: Extracellular vesicle.
CONCLUSION
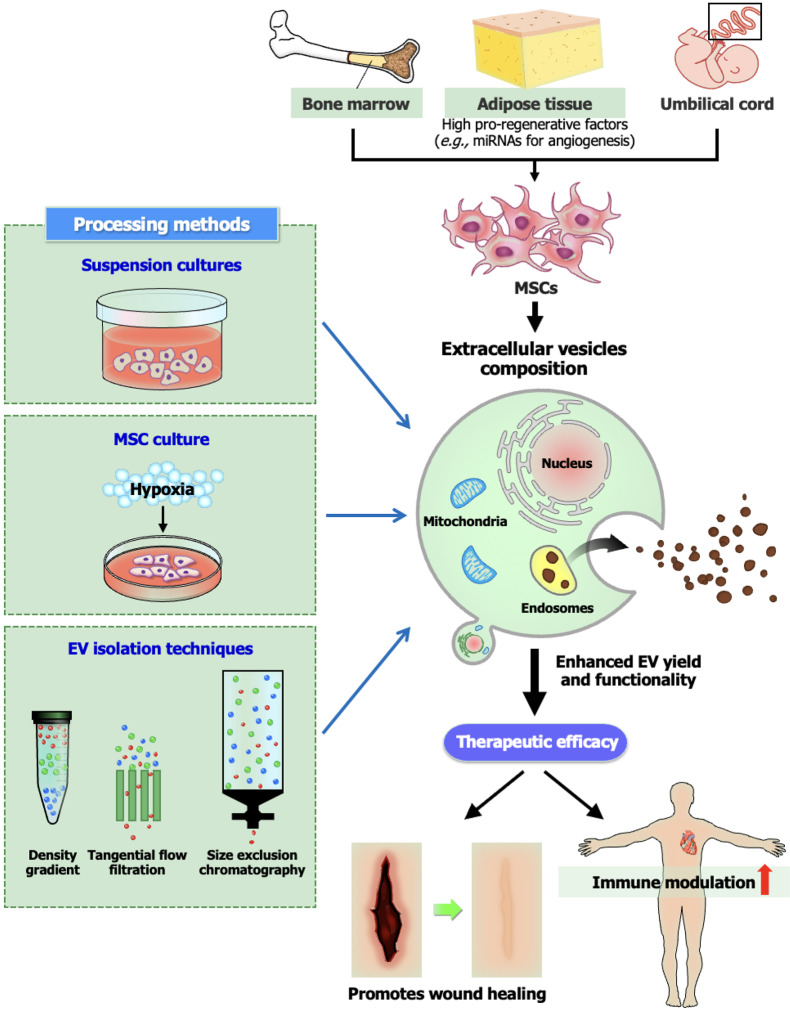
SVF isolation techniques must be refined further and standardized to maximize the therapeutic potential of ADSCs in regenerative medicine, as emphasized by Jeyaraman et al[1]. The sources of and processing protocols for MSCs strongly influence their functionality, including EV composition and therapeutic efficacy[2,3]. Findings on the differences in secretome profiles among processed adipose grafts, SVF components, and ADSCs can elucidate the clinical implications of these differences[3]. The choice of isolation techniques, such as nonenzymatic techniques, influences the viability and regenerative capacity of cells[4,5]. Systematic reviews and meta-analyses have suggested that optimizing EV-based therapies and exploring preconditioning techniques can help enhance the regenerative capacity of EVs in challenging scenarios such as diabetic wounds and peripheral nerve regeneration[8,12]. Nonetheless, challenges persist. Variability in isolation techniques as well as the lack of standardized protocols and advanced molecular analyses must be addressed to ensure consistent, high-quality clinical applications[1,13]. These problems should be addressed through continual innovation, collaborative research, and rigorous clinical testing to ensure the clinical usefulness of advances in SVF research. By overcoming the aforementioned challenges, clinical researchers can optimize regenerative medicine and develop reliable therapies for various medical conditions (Figure 1).
Figure 1.
Effects of various mesenchymal stem cell sources and processing protocols on extracellular vesicle composition and therapeutic efficacy. This figure presents key factors that influence the composition and therapeutic potential of mesenchymal stem cell (MSC)-derived extracellular vesicle (EVs), clarifying how MSCs from different tissue sources (e.g., adipose, bone marrow, and umbilical cord) produce EVs with different molecular profiles. It also depicts the effects of various processing protocols, such as culture conditions (e.g., suspension cultures and hypoxic preconditioning) and isolation techniques, on the yield and functionality of EVs. Furthermore, the figure underscores the importance of selecting appropriate MSC sources and standardizing processing protocols to optimize the therapeutic efficacy of EVs in regenerative medicine. EV: Extracellular vesicle; MSC: Mesenchymal stem cell; miRNAs: MicroRNAs.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cell and tissue engineering
Country of origin: Taiwan
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Ignatyeva N S-Editor: Wang JJ L-Editor: A P-Editor: Zhang XD
Contributor Information
Chun-Han Cheng, Department of Medical Education, Linkou Chang Gung Memorial Hospital, Taoyuan City 33305, Taiwan.
Wen-Rui Hao, Division of Cardiology, Department of Internal Medicine, Shuang Ho Hospital, Ministry of Health and Welfare, Taipei Medical University, New Taipei City 23561, Taiwan; Division of Cardiology, Department of Internal Medicine, School of Medicine, College of Medicine, Taipei Medical University, Taipei 11002, Taiwan.
Tzu-Hurng Cheng, Department of Biochemistry, School of Medicine, College of Medicine, China Medical University, Taichung City 404328, Taiwan. thcheng@mail.cmu.edu.tw.
References
- 1.Jeyaraman N, Shrivastava S, Ravi VR, Nallakumarasamy A, Pundkar A, Jeyaraman M. Understanding and controlling the variables for stromal vascular fraction therapy. World J Stem Cells. 2024;16:784–798. doi: 10.4252/wjsc.v16.i8.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y, Sun L, Li Y, Holmes C. Mesenchymal stromal/stem cell tissue source and in vitro expansion impact extracellular vesicle protein and miRNA compositions as well as angiogenic and immunomodulatory capacities. J Extracell Vesicles. 2024;13:e12472. doi: 10.1002/jev2.12472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carr H, Asaad M, Wu Y, Branch-Brooks C, Zhang Q, Hematti P, Hanson SE. Differential Secretomes of Processed Adipose Grafts, the Stromal Vascular Fraction, and Adipose-Derived Stem Cells. Stem Cells Dev. 2024;33:477–483. doi: 10.1089/scd.2024.0071. [DOI] [PubMed] [Google Scholar]
- 4.Mundluru VK, Naidu MJ, Mundluru RT, Jeyaraman N, Muthu S, Ramasubramanian S, Jeyaraman M. Non-enzymatic methods for isolation of stromal vascular fraction and adipose-derived stem cells: A systematic review. World J Methodol. 2024;14:94562. doi: 10.5662/wjm.v14.i2.94562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qin J, Cheng C, Huang RL, He J, Zhou S, Tan PC, Zhang T, Fang B, Li Q, Xie Y. Isolation of the Stromal Vascular Fraction Using a New Protocol with All Clinical-Grade Drugs: From Basic Study to Clinical Application. Aesthetic Plast Surg. 2024 doi: 10.1007/s00266-024-04221-9. [DOI] [PubMed] [Google Scholar]
- 6.Souza ILM, Suzukawa AA, Josino R, Marcon BH, Robert AW, Shigunov P, Correa A, Stimamiglio MA. Cellular In Vitro Responses Induced by Human Mesenchymal Stem/Stromal Cell-Derived Extracellular Vesicles Obtained from Suspension Culture. Int J Mol Sci. 2024;25 doi: 10.3390/ijms25147605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yin D, Shen G. Exosomes from adipose-derived stem cells regulate macrophage polarization and accelerate diabetic wound healing via the circ-Rps5/miR-124-3p axis. Immun Inflamm Dis. 2024;12:e1274. doi: 10.1002/iid3.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soltani S, Zahedi A, Vergara AJS, Noli M, Soltysik FM, Pociot F, Yarani R. Preclinical Therapeutic Efficacy of Extracellular Vesicles Derived from Adipose-Derived Mesenchymal Stromal/Stem Cells in Diabetic Wounds: a Systematic Review and Meta-Analysis. Stem Cell Rev Rep. 2024 doi: 10.1007/s12015-024-10753-z. [DOI] [PubMed] [Google Scholar]
- 9.Badr OI, Anter A, Magdy I, Chukueggu M, Khorshid M, Darwish M, Farrag M, Elsayed M, Amr Y, Amgad Y, Mahmoud T, Kamal MM. Adipose-Derived Mesenchymal Stem Cells and Their Derived Epidermal Progenitor Cells Conditioned Media Ameliorate Skin Aging in Rats. Tissue Eng Regen Med. 2024;21:915–927. doi: 10.1007/s13770-024-00643-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Romano IR, D'Angeli F, Gili E, Fruciano M, Lombardo GAG, Mannino G, Vicario N, Russo C, Parenti R, Vancheri C, Giuffrida R, Pellitteri R, Lo Furno D. Melatonin Enhances Neural Differentiation of Adipose-Derived Mesenchymal Stem Cells. Int J Mol Sci. 2024;25 doi: 10.3390/ijms25094891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goulas P, Karakwta M, Zatagias A, Bakoutsi M, Zevgaridis A, Ioannidis A, Krokou D, Michalopoulos A, Zevgaridis V, Koliakos G. A Simple and Effective Mechanical Method for Adipose-Derived Stromal Vascular Fraction Isolation. Cureus. 2024;16:e57137. doi: 10.7759/cureus.57137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Xu H, Li C, Guan Y, Liu Y, Zhang T, Meng F, Cheng H, Song X, Jia Z, He R, Zhao J, Chen S, Guan C, Yan S, Wang J, Wei Y, Zhang J, Tang J, Peng J, Wang Y. Biological characteristics of tissue engineered-nerve grafts enhancing peripheral nerve regeneration. Stem Cell Res Ther. 2024;15:215. doi: 10.1186/s13287-024-03827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garroni G, Cruciani S, Serra D, Pala R, Coradduzza D, Cossu ML, Ginesu GC, Ventura C, Maioli M. Effects of the MCF-7 Exhausted Medium on hADSC Behaviour. Int J Mol Sci. 2024;25 doi: 10.3390/ijms25137026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ruoss S, Nasamran CA, Ball ST, Chen JL, Halter KN, Bruno KA, Whisenant TC, Parekh JN, Dorn SN, Esparza MC, Bremner SN, Fisch KM, Engler AJ, Ward SR. Comparative single-cell transcriptional and proteomic atlas of clinical-grade injectable mesenchymal source tissues. Sci Adv. 2024;10:eadn2831. doi: 10.1126/sciadv.adn2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tareen WA, Saba E, Rashid U, Sarfraz A, Yousaf MS, Habib-Ur-Rehman, Rehman HF, Sandhu MA. Impact of multiple isolation procedures on the differentiation potential of adipose derived canine mesenchymal stem cells. Am J Stem Cells. 2024;13:27–36. doi: 10.62347/LEVZ7282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohseni Meybodi MA, Nilforoushzadeh MA, KhandanDezfully N, Mansouri P. The safety and efficacy of adipose tissue-derived exosomes in treating mild to moderate plaque psoriasis: A clinical study. Life Sci. 2024;353:122915. doi: 10.1016/j.lfs.2024.122915. [DOI] [PubMed] [Google Scholar]
- 17.Suryawan IGR, Pikir BS, Rantam FA, Ratri AK, Nugraha RA. Hypoxic Preconditioning Promotes Survival of Human Adipose Derived Mesenchymal Stem Cell. F1000Res. 2021;10:843. doi: 10.12688/f1000research.55351.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Symonds EKC, Black B, Brown A, Meredith I, Currie MJ, Hally KE, Danielson KM. Adipose derived stem cell extracellular vesicles modulate primary human macrophages to an anti-inflammatory phenotype in vitro. J Extracell Biol. 2023;2:e104. doi: 10.1002/jex2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang S, Sun Y, Yan C. Recent advances in the use of extracellular vesicles from adipose-derived stem cells for regenerative medical therapeutics. J Nanobiotechnology. 2024;22:316. doi: 10.1186/s12951-024-02603-4. [DOI] [PMC free article] [PubMed] [Google Scholar]