Abstract
Background: Unhealthy commodity industries (UCIs) engage in political practices to influence public health policy, which poses barriers to protecting and promoting public health. Such influence exhibits characteristics of a complex system. Systems thinking would therefore appear to be a useful lens through which to study this phenomenon, potentially deepening our understanding of how UCI influence are interconnected with one another through their underlying political, economic and social structures. As such this study developed a qualitative systems map to depict the complex pathways through which UCIs influence public health policy and how they are interconnected with underlying structures.
Methods: Online participatory systems mapping workshops were conducted between November 2021 and February 2022. As a starting point for the workshops, a preliminary systems map was developed based on recent research. Twenty-three online workshops were conducted with 52 geographically diverse stakeholders representing academia, civil society (CS), public office, and global governance organisations (CGO). Analysis of workshop data in NVivo and feedback from participants resulted in a final systems map.
Results: The preliminary systems map consisted of 40 elements across six interdependent themes. The final systems map consisted of 64 elements across five interdependent themes, representing key pathways through which UCIs impact health policy-making: (1) direct access to public sector decision-makers; (2) creation of confusion and doubt about policy decisions; (3) corporate prioritisation of commercial profits and growth; (4) industry leveraging the legal and dispute settlement processes; and (5) industry leveraging policy-making, norms, rules, and processes.
Conclusion: UCI influence on public health policy is highly complex, involves interlinked practices, and is not reducible to a single point within the system. Instead, pathways to UCI influence emerge from the complex interactions between disparate national and global political, economic and social structures. These pathways provide numerous avenues for UCIs to influence public health policy, which poses challenges to formulating a singular intervention or limited set of interventions capable of effectively countering such influence. Using participatory methods, we made transparent the interconnections that could help identify interventions in future work.
Keywords: Systems Mapping, Complex Adaptive Systems, Participatory Research, Unhealthy Commodities, Commercial Determinants of Health, Non-communicable Diseases
Background
Key Messages
Implications for policy makers
Industry influence on public health policy is not reducible to a single point, but is dispersed throughout a system, and inextricably linked to different political practices and underlying structures.
The interdependent and complex pathways through which industries influence public health policy suggest that they can adapt to changes in the system, limiting intervention effectiveness over time.
Strategies to address industry influence on public health policy should cohere with each other and aim to tackle the underlying political, economic and social structures that give rise to unhealthy commodity industry (UCI) influence.
If the structures underlying UCI influence are not addressed, industry influence may continue despite the implementation of well-intended interventions.
Implications for the public
Industries that produce and sell tobacco, alcohol, and unhealthy foods engage in political practices designed to influence public health policy-making, leading to industries remaining insufficiently regulated and policy that is made in industries’ favour. Interventions to address such influence would likely help safeguard public health policy-making and improve its effectiveness in protecting and promoting public health. Interventions should not only be aimed at policy-making, such as accountability and lobbying measures, but should also be aimed at the underlying political, economic and social structures that enable unhealthy commodity industries (UCIs) to exert power and influence. These structures may include privatisation, international trade and investment, and norms on multistakeholder governance. Public health professionals and civil society (CS) actors should support interventions that both improve policy-making processes and aim to change the wider system that drives the accumulation of UCI power. If not, interventions may be ineffective at addressing industry influence on public health policy.
The political practices used by unhealthy commodity industries (UCIs) pose a significant barrier to advancing public health policy and goals. Recent research on the commercial determinants of health (CDoH) has outlined how corporate political practices help shape the policies, policy environments, and underlying political, economic and social structures that drive unhealthy commodity consumption (eg, tobacco, alcohol, and ultra-processed foods), ultimately leading to poor health outcomes and widespread health inequalities.1 Similarly, a recent evidence-based taxonomy shows how different UCIs use analogous corporate political practices to influence public health policy at various levels of governance across the world,2 which is supported with an increasingly extensive and growing volume of literature.3-35 Scholars have suggested that UCI influence is a complex problem, derived from a complex system, and have called for systems thinking approaches to be applied to it.1,3,36,37 Systems thinking may therefore help to deepen our understanding of this problem and identify the key solutions. However, to date, no study has explicitly applied systems thinking methods this phenomenon. To answer this call, we aimed to apply systems thinking to map out the complexity and pathways through which UCIs influence public health policy.
Systems thinking is an approach to studying complex systems,38-44 defined as a composition of many interconnected and interdependent elements that function together as a whole.38,44-47 These elements interact with one another in such a way that their combined behaviour produces emergent properties and patterns.41,44,46,48-51 Systems thinking views phenomena as more than just the sum of its parts; it emphasises understanding the relationships, feedback loops, and dynamic behaviour of a system as a whole.41,46,48,49,51 Complex systems are characterised by adaptivity and unpredictability of how a system reacts to change.44,45,52,53 They are also characterised by the heterogeneity and interactivity between stakeholders, processes and structures that produce results that may otherwise not exist if these things functioned independently of each other.44,53,54
One key characteristic of a complex system is that it can adapt to change and there is some evidence that industry actors do so. One example is how the tobacco industry adapted to the introduction of the World Health Organization (WHO) Framework Convention on Tobacco Control (FCTC). The WHO FCTC’s Article 5.3 restricted the tobacco industry’s access to policy-makers and, alongside the tobacco industry’s growing denormalisation, reduced its ability to influence policy.55-57 In response to this denormalisation, the tobacco industry adapted by investing heavily in corporate social responsibility practices and later increased the establishment and use of third-party and front groups.58-61 They also reframed their corporate goals in terms of ‘harm reduction’ to renormalise,61-65 investing in alternative tobacco products, such as heated tobacco products and vapes.61,66,67 Such adaptivity is also apparent in the “greenwashing” undertaken by the fossil fuel industry68 and in the lower strength alcohol products marketed by the alcohol industry.69 This adaptivity is therefore important to take into consideration when developing interventions to UCI influence on public health policy. In this context, by “interventions,” we mean deliberate and structured actions, strategies, policies or organisational arrangements designed to change the system to reduce UCI’s ability to influence public health policy, thereby facilitating the advancement of policies that more closely align with public health objectives.
A key component underlying UCI influence is corporate power, which is conceived of in various ways. One such way is that it stems from “material” (ie, financial) and “ideational” (ie, ideas) sources that manifest in different forms, namely instrumental (eg, use of lobbying and access to policy-makers), structural (eg, controlling the policy agenda and shaping institutional rules), and discursive (eg, framing policy in free market terms and emphasising personal responsibility).7,70-73 Drawing on theories of power, Gilmore et al argue that UCI practices influence the global structures in which public health policies are made, such as capitalism, globalisation, asymmetrical governance arrangements, international trade and investment practices, and regulatory frameworks – that ensure rules and norms favour industry.1,7,70-72,74-82 This suggests a reinforcing system — or feedback loop — that is both influenced by, and facilitates, UCI engagement in political practices. Such a system makes it challenging to advance effective public health policies, such as guidelines for consumption, or restrictions on the marketing, availability, and affordability of, and access to, unhealthy commodities. Instead of these policies, UCIs argue for deregulation, co-regulation, or neoregulation (ie, where states restructure supply chains according to public-private management83-85), despite the lack of evidence that these promote and protect public health.1,86,87
To advance public health policies, changes are needed to curtail UCI power72,75 and prevent or mitigate their influence in the system.4,35,88-90 Recent literature has begun to explore this topic by, for example, suggesting or documenting various strategies or governance mechanisms to counter UCI influence on public health policy.88,90,91 These mechanisms aim to increase transparency; disclose industry influence and conflict of interest; identify, monitor, and educate policy-makers and the public about industry’s harmful practices; and manage or prohibit interactions with industry.88 Although these changes are needed, research lacks the consideration of industry adaptivity and the other complexities surrounding UCI influence on public health policy, including the underlying political, economic and social structures77,84,92 that enable UCI to engage in political practices.
Systems mapping is a systems thinking approach involving a process of visually depicting the interactions, relationships, and feedback loops within a system, thus facilitating a comprehensive understanding of a phenomenon’s elements, dynamics and complexity.41,45,51,93 These maps can help to clarify the relationships between disparate parts of a system, and in this case, the pathways through which UCIs influence public health policy.49 In so doing, systems mapping could make explicit these interlinkages, rendering them more understandable in ways that might help to address UCI influence on public health policy.44,52,94,95 Using participatory systems mapping methods, this study fills a gap by making transparent the specific interrelationship between various parts of the system.
In this study we focused on tobacco alcohol, and ultra-processed foods as they are the major preventable risk factors for non-communicable diseases (NCDs),96,97 which account for approximately 71% (41 million) of global deaths per year.98 These risk factors cause metabolic changes in the human body, such as increased blood pressure, obesity, hyperglycaemia and hyperlipidaemia, which increase the risk of developing NCDs.99
Although previous studies have argued that UCI influence on public health policy is part of a complex system,3,36,37 as far as the authors are aware, this study represents a first attempt at explicitly applying participatory systems mapping methods to this phenomenon, thereby making a needed methodological contribution.
Methods
Study Design
We conducted participatory systems mapping workshops to map the complex pathways through which UCIs influence policy. These workshops are interactive events where stakeholders collectively create a visual representation, fostering a holistic and shared understanding of a complex system.38,39,43,46,49,51,95,100-102 In this case, the workshop brought together participants with knowledge of UCI influence to review a preliminary map, and identify, comment on and refine the linkages between UCIs, political practices, underlying structures, and other key actors that enable such influence.
Development of Preliminary Map
To create a starting point for the participatory systems mapping workshops, a preliminary systems map was developed (See Supplementary file 1) by synthesising two recent publications: (i) The Lancet commissioned conceptual model of the CDoH,1 and (ii) an evidence-based taxonomy of political practices used by UCIs to influence public health policy.2 The latter paper, in turn, drew significantly from Legg et al who developed a model of corporate influence on science.103 These papers represent the most recent thinking and conceptualisation of the intersection between CDoH and UCI political practices. This involved identifying key elements (ie, the tangible or intangible components that constitute a system)44 and interconnections (ie, the “relationship [between the elements] that hold the elements together”).44 These were extracted into a table to compare the differences or similarities between elements, and then inputted to Kumu. Kumu is an online visualisation tool for creating system elements and drawing connections between them to produce an interactive diagram or map depicting complex relationships between various parts of a system or network. Kumu was used here because it allows one to visually depict the various interactions and dependencies surrounding UCI influence, and it has features that allow the creators to customise the map for the project’s purpose.
As a starting point, a ‘target element’ was placed at the centre of the map to represent the extent to which industry successfully ‘influences policy.’ An ‘outcome element’ was then placed below to signify the outcome of UCI influence (ie, deregulation and regulation that favours industry and in the final map, implementation of UCI preferred laws, regulations, processes and norms). The target and outcome elements helped to distinguish them from other elements and remind the reader that this is the central purpose of the map – to explore the complexities surrounding UCI influence on public health policy. Each element in the systems map represents a variable (ie, a factor that can range between high and low values). Elements were clustered and synthesised if necessary and interconnections were linked to ensure that they reflected the narrative of each of the two studies. This process of clustering and integrating elements led to the identification of key distinct (yet interconnected and interdependent) themes that appeared to lead to successful UCI influences on public health policy.
Participatory Systems Mapping
This study adapted in-person participatory systems mapping workshops95 by conducting a series of online “small group” workshops.104,105 Two pilot workshops were conducted to test the workshop design and refine the preliminary systems map.
Two weeks prior to the workshops, a digital copy of the preliminary systems map was shared with participants, including a description of elements and interconnections, so that participants could become familiar with the map to maximise the time available for discussions. Participants were also sent a workshop brief that provided the purpose of the study, workshop agenda and questions, and some basic systems thinking terminology. Participants did not come back with queries.
Workshop activities were adapted from the Causal Mapping with Seed Structure scripts.106,107 Participants were asked to consider the preliminary systems map and whether any elements or interconnections needed amending, removing, adding, or clarifying. The facilitator [AB] guided the participants around the various sections of the preliminary map using an online whiteboard. Participants’ views were captured by asking them to insert their comments using the sticky note function in the corresponding location on the map, after which comments were discussed. Each workshop focused on parts of the map where stakeholders had expertise. Stakeholder’s contributions were treated equally. Participants were also able to review, comment on and discuss other parts of the systems map if they felt they had insights to contribute. Workshops ranged between 60 minutes and 90 minutes in duration, were conducted on Microsoft Teams and were recorded and transcribed by the application. The transcriptions were then checked and amended, if necessary, by [AB, AvdA, or SD].
Participant Recruitment
In an attempt to gain diversity of insights and perspectives, participants were purposefully sampled108 from a variety of backgrounds [academia (A), civil society (CS), former public officials (FPO), or global governance organisations (GGO)], covering different knowledge areas (tobacco, alcohol and ultra-processed food industries and/or CDoH), including all WHO geographical regions, and policy levels (eg, regional, national, and global).
Stakeholders and their expertise were initially identified through a literature review and authors’ networks, and then through snowballing. Participants were selected if they had conducted research in the field of public health policy, UCI influence, or tobacco, alcohol or food policy, or issues underlying political, economic and social structures in which UCIs function; engaged in or represented organisations that engage in activities directly related to public health advocacy and awareness campaigns concerning tobacco, alcohol or food or other reform efforts concerning the CDoH; experience in policy-making or regulatory roles with a focus on health and industry influence issues; or involvement in global health governance or provided policy advice to national governments. Industry representatives were excluded because it was considered that they would have a conflict of interest.
A total of 83 email invitations were sent to stakeholders. Fifteen declined to participate and 16 were unresponsive. Fifty-two stakeholders agreed to participate from different WHO regions (Africa = 17, Americas = 17, South-East Asia = 4, Europe = 27, Eastern Mediterranean = 1, and Western Pacific = 15) (See Supplementary file 2). Twenty-three small group workshops were conducted ranging between one and five stakeholders each between November 2021 and February 2022. Consent to participate was obtained from all stakeholders. They were also all given the option of being openly acknowledged for taking part in the workshops.
Analysis
Workshop analysis involved reviewing workshop data (ie, workshop notes, whiteboard comments, and transcripts) in NVivo. Elements were extracted from the workshop data into a table to constantly compare their conceptual differences or similarities and how they interacted with each other. If a participant suggested that an element was important to UCI influence, it was included in the map. If there were to be a new element, it was inputted onto Kumu. Elements were then either amended, or new elements were added, clustered (if there were repetitions of the same or similar concepts), and then integrated if needed. Connections were drawn between elements to reflect participants’ views on the interrelationships between elements. Analysis did not assess the quantity or strength of evidence supporting each element or connection.
Elements that are directly connected to the target element — we call “proximal elements” — represent the key issues that enabled UCIs to influence policy decisions. Elements were identified and connected to the proximal elements when stakeholders suggested what enabled these preceding elements. The entire analysis process was repeated until elements formed thematic clusters. Themes were named after proximal elements to represent the cluster of elements that were most closely interconnected. Illustrative quotes were used to embody the elements and resultant themes.
The lead author emailed participants for clarification if needed. Once the analysis of workshop data was completed, a draft version of the full systems map, and a table describing the systems elements and interconnections were sent to all stakeholders for final sense checking. Responses to the final systems map were received from 14 participants, of whom 10 provided detailed feedback and four indicated they had nothing further to add. Feedback was then integrated into a final systems map.
Results
System Overview
The preliminary systems map (Supplementary file 1) consisted of 40 elements across six interconnected themes. Each theme symbolised a pathway through which UCIs influence public health policy. As the main purpose of this study is to present the final map, changes to the preliminary map are provided in Supplementary file 1.
The final map consists of 64 elements across five themes (Figures 1–6 and online), namely: direct access to public sector decision-makers (Theme 1); creation of confusion and doubt about policy decisions (Theme 2); corporate prioritisation of commercial profits and growth (Theme 3); industry leveraging legal and dispute settlement processes (Theme 4); and industry leveraging policy-making, norms, rules, and processes (Theme 5).
Figure 1.
Full Systems Map. The solid lines represent the same direction of change between elements (eg, an increase in element A leads to an increase in element B. The dotted lines with a plus (+) or minus (-) sign represent an opposite direction of change between elements [eg, increasing (+) element A decreases (-) element B or vice versa]. There are also interconnections that are mutually directed ie, the arrows go in both directions, where an increase in one element leads to an increase in the other and vice versa. Abbreviation: UCI, unhealthy commodity industry.
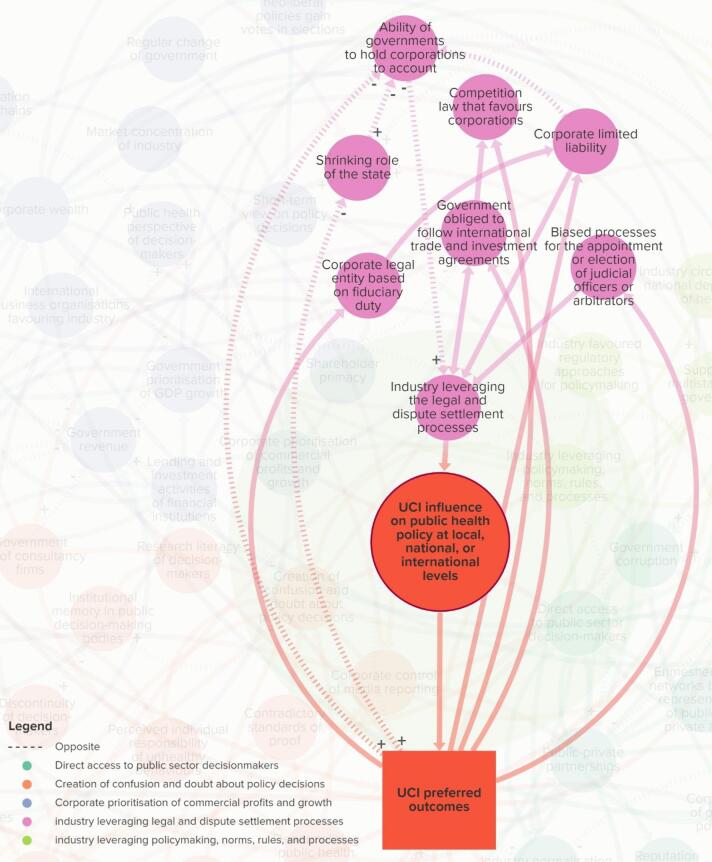
Figure 6.
Industry Leveraging Policy-Making, Norms, Rules, and Processes. Abbreviation: UCI, unhealthy commodity industry.
Figure 4.
Corporate Prioritisation of Commercial Profits and Growth. Abbreviation: UCI, unhealthy commodity industry.
Figure 5.
Industry Leveraging Legal and Dispute Settlement Processes. Abbreviation: UCI, unhealthy commodity industry.
The “target element” (large red circle) represents the extent to which UCIs influence (ie, suppress, shape, weaken, block, or delay) policy at subnational, national, regional, or international levels. This leads to policies that favour UCIs — represented by the red rectangle (UCI preferred outcomes) — which in turn, connects to various pathways that are dispersed throughout the system. The proximal elements that connect directly to the large red circle — UCI influence on public health policy — are key pathways, and each element theoretically varies in value. A full list of element descriptions and their interconnections are provided in Supplementary file 3.
Theme 1. Direct Access to Public Sector Decision-Makers
The elements in Theme 1 affect the extent to which public sector decision-makers (policy-makers, civil servants, and public officials) can be directly accessed by industry actors (Figure 2). Stakeholders noted that industry achieves this through both formal (eg, being part of a policy committee) and informal (eg, through interpersonal relationships) means.
Figure 2.
Direct Access to Public Sector Decision-Makers. Abbreviation: UCI, unhealthy commodity industry.
Some of the key elements that affect direct access to decision-makers include government corruption (ie, extent to which corruption is endemic in a government), revolving doors (ie, extent to which individuals move between public office and industry jobs), and enmeshed social networks between representatives of public and private actors (ie, extent to which public sector decision-makers’ social networks are intertwined with senior corporate management35).
Stakeholders noted that government corruption may feature more prominently within certain contexts. For example, “[in] South Africa, we have a sort of different experience…corruption is endemic, but corruption of public officials is a big issue, so the officials who manage decision-making are very vulnerable to influence…” (A13). Corporate wealth was also an important and interconnected element for this theme, “…money is such an enabler for all of this, when you can buy big public affairs agencies and you can buy big comms campaigns and you’ve got access to the underground lobbying places…money buys access in multiple ways” (CS16). Similarly, another stakeholder said, “they have a ‘just-pick-up-the-phone’ kind of relationships that NGOs and civil society organisations wouldn’t even dream of having. But it’s because they’re normalised that this is an actor we have to consult. They’re at the table...” (FPO2). This suggests that close interpersonal relationships between decision-makers and industry representatives, together with industry as a normalised governance stakeholder, facilitated direct access to decision-makers.
Within this theme, stakeholders also suggested that there was a reinforcing interaction between public-private partnerships (ie, extent to which public and private sector actors enter into partnerships) and industry normalisation and legitimation (ie, extent to which an industry is seen as socially acceptable and thus a legitimate policy actor). For example, a stakeholder said, “…it’s almost like a sort of…vicious circle… the industry’s image is of a normal and legitimate policy actor. Therefore, it can be involved in public-private partnerships and governments mechanisms, which then reinforces its image” (A23). Another stakeholder said, “they’re actually sitting on advisory groups and panels around how to devise the policies and what’s acceptable to their members…we could never possibly even feasibly think about doing something without talking to industry and having them at the table” (FPO2). This indicates that norms have shifted thus far in favour of UCIs that it does not need to expend political capital to secure access to policy-makers.
Theme 2. Creation of Confusion and Doubt About Policy Decisions
Elements in Theme 2 affect the extent to which decision-makers, and the public are confused about whether the proposed policy is needed and will lead to public value (Figure 3). Key elements that affect creation of confusion and doubt about policy decisions include industry influence on evidence and science2,103 (ie, extent to which industry funds, produces, controls, and manages information and research); displacing and usurping of public health actors by industry2,103 (ie, extent to which industry attempts to marginalise and take over the role of public health actors); denormalising public health policy2 (ie, extent to which industry creates the perception that public health policy interventions are unnecessary or socially unacceptable); and perceived individual responsibility of unhealthy behaviours (ie, extent to which individuals are perceived as being responsible for their own patterns of consumption behaviours).
Figure 3.
Creation of Confusion and Doubt About Policy Decisions. Abbreviation: UCI, unhealthy commodity industry.
Stakeholders pointed out the complex dynamic between elements, such as marketing practices (ie, extent to which marketing is unrestricted and poorly monitored and enforced), industry normalisation and legitimisation, and product and brand normalisation (ie, extent to which a product is seen as socially acceptable or desirable). For example, one stakeholder said, “[industries] promote brands rather than products. But using products in a way that normalises the product so… they can use brands instead of products … because when you advertise to children, you’re not supposed to advertise unhealthy things, so you don’t advertise the actual product, you just advertise the unhealthy brand. And sometimes the brands have healthy and unhealthy foods under them, so it creates confusion….” (A15). This suggests that corporate branding is a means to normalise an industry, making it challenging to refute their claims and arguments and enabling access to decision-makers.
Stakeholders also highlighted the complex relationship between industry influence on evidence and science; corporate control of media reporting (ie, extent to which corporations control what is reported in the media through, for example, media ownership and marketing or sponsorships); credible dissemination of industry arguments (ie, extent to which industry creates a perception of producing credible information, disseminated through networks of actors); and generating support for industry position (ie, extent to which corporate actors fabricate or galvanise support with stakeholders) (Theme 5). For example, a stakeholder noted, “media reporting will kind of pick up on these kinds of oversimplistic arguments and not really interrogate them further…maybe that’s because of who owns the media outlets” (CS15). Another stakeholder noted that “[industries]…are big spenders and big sources of income for media in terms of advertising in all sorts of media…that might also discourage the journalists within those media to just put the critical light on these industries” (CS4). Moreover, another stakeholder said, “[when industry] get a bit of bad publicity, they change their name… But they’re back again…but on front groups [sic] and other funded organisations, which include [their funded] research” (A26). Stakeholders suggest that underlying the confusion and doubt about policy decisions is the cumulative impact of industry research disseminated through biased media, thereby entrenching industry support.
In response to contradictory standards of proof (ie, extent to which evidentiary standards of proof are applied inconsistently to industry and public health actors and evidence), a stakeholder remarked, “we’re held to these ridiculously high standards of evidence that just doesn’t affect the other side [industry]” (CS16). The same stakeholder suggested that discontinuity of decision-makers (ie, extent to which public officials remain in their positions as decision-makers over time) was an important aspect that was linked to institutional memory in public decision-making bodies (ie, extent to which a decision-maker represents a public institution over time), “… voluntary reformulation programme on sugar [industry] hasn’t worked. Yet the government is still going down this path because it’s a different set of politicians who think, ‘well, we can make it work because we’re not like those ones who did it and got it wrong’” (SC16). This indicates that confusion and doubt can be worsened by a lack of knowledge on effective public health measures.
Theme 3. Corporate Prioritisation of Commercial Profits and Growth
Elements in Theme 3 affect the extent to which corporations prioritise their own profits and growth above other economic costs associated with consuming unhealthy commodities (or other societal values, such as health, well-being, human rights, and the natural environment). Some of the key elements that affect this element are shareholder primacy (ie, extent to which corporations maximise the value of their company for shareholders); government prioritisation of GDP [gross domestic product] growth (ie, extent to which government prioritises the notion of GDP growth as a measure of economic growth); lending and investment activities of financial institutions (ie, extent to which public and private financial institutions provide capital for UCIs);and short-term view on policy decisions (ie, extent to which politicians adopt a short-term view on policy decisions).
Stakeholders mentioned the externalities of costs and the need to structure the economy by using taxes “…to better reflect the externalities…” (CS11), is linked to how UCIs use arguments to “emphasise the benefits that they bring [to economic growth] but hide completely the costs…” (A8). Although industries make these economic arguments, stakeholders noted that the converse was the case, “NCDs in general and alcohol harm… undermine economic growth. So, the harm, the costs of the harm…are…bigger than what the industry brings in through tax revenue” (CS6). Similarly, another stakeholder said, “…[the] choice between public health and the good economy is a completely [sic] false dichotomy, because clearly a healthier workforce would be a more productive workforce” (CS11). Additionally, to make the link that shareholder primacy is an important part of this theme, a stakeholder said, “…it’s not just the ideology of economic growth...the wealthiest – like the shareholders – [is] really where the wealth is accumulated” (CS6).
Stakeholders suggested a relationship between government use of consultancy firms and privatisation, which is related to the shrinking role of the state, and governance capability. For example, a stakeholder said, “we’re now outsourcing government policymaking to a consultancy firm to write a policy for government. And of course, when you look at what they write, they often recommend privatisation, which, they have such a strong interest in. So, there is this kind of perfect loop for the corporation between recommending privatisation and then public sectors get deskilled” (A9). Moreover, in discussing the relationship between corporate prioritisation of commercial profits and growth and the creation of confusion and doubt about policy decisions, a stakeholder noted that “the failure to achieve growth is an important story…” (A4). Thisfinding alludes to industry arguments or narratives that regulations on UCIs inhibit economic development, which creates doubt about advancing public health policies.
It is important to note that some stakeholders challenged the element acceptance of neoliberalism (ie, extent to which governing bodies subscribe to the political ideology of market fundamentalism1). For example, a stakeholder said that they were, “uncomfortable with use of terms like ‘neoliberalism’” because it “implies a partisan political dimension” (A26). Similarly, another stakeholder suggested that the term ‘neoliberalism’ was divisive as it alienated policy actors who required it as a fundamental prerequisite for international cooperation — for example, in trade agreement negotiations, “so we can’t point fingers at the whole concept of free trade agreements, but we could say that fine, free trade agreements could provide a lot of benefit, but definitely not for products that have zero benefit like tobacco…” (CS17). In contrast, another stakeholder said, “neoliberalism is not even perceived as an ideology anymore – and I feel that is the most powerful form of ideological persuasion – is you simply take it off the table as a subject” (A4). This indicates the view that the term ‘neoliberalism’ is also important to retain in the system maps so that it continues to be a topic for discussion and debate.
Theme 4. Industry Leveraging Legal and Dispute Settlement Processes
Elements in Theme 4 affect the extent to which industry leverages legal and dispute settlement processes, for example, by bringing or threatening to bring litigation against governments to prevent, undermine, or reverse public health policy. Some of the key elements that affect these processes are biased processes for the appointment or election of judicial officers or arbitrators; government obliged to follow international trade and investment agreements; ability of governments to hold corporations to account (ie, extent to which governments have the ability to investigate, prosecute and sanction problematic corporate behaviours in domestic and extra-territorial jurisdictions),and corporate limited liability (ie, extent to which the owners or management of commercial entities are liable for corporate debt, damages, or wrongdoing).
For the preliminary map, the elements pertaining to international trade and investment agreements were initially itself a proximal element. However, stakeholders suggested that it should be integrated within Theme 4 because how industry influences international trade and investment agreements are the same pathways that lead to the target element (large red circle). For example, one stakeholder said, “when I was thinking about how the industry lobbies through… direct access – so they have direct access to policy-makers nationally, but also in the regional…and international trade agreements...” (A2). Stakeholders also highlighted the importance of unpacking what lay within international trade and investment rules, norms and processes. Stakeholders suggested connecting competition law that favours corporations (ie, extent to which competition law favours corporations, including mergers and acquisitions and intellectual property), with government obliged to follow international trade and investment agreements, and monopoly concentration. For example, a stakeholder noted, “competition policy…gets used in trade and investment agreements…” (A1) and that “when you’re talking about food, alcohol, and tobacco, we see mergers and acquisitions happening across those sectors” (A1). Similarly, a stakeholder said, “monopoly concentration is a really important dynamic of the last few decades that has significantly increased the power of industry...” (CS6), which shows how UCI’s legal structures help to entrench their trade and economic power.
Another important concept stakeholders noted was the effect of industry bringing, or threatening to bring, litigation, which causes regulatory chill. It is a powerful deterrent for governments developing public health policy, as one stakeholder said, “in terms of governments not wanting to try something because they fear litigations or they fear repercussions in related to their trade agreements – so even without governments pushing or the industry asking their governments to raise concerns with other governments, they still might hold back on regulations due to the fear of this happening” (CS4). Similarly, another stakeholder said, “we don’t know what the chilling effect is on public health legislation simply because people are scared of being sued…” (A9). Lastly a stakeholder noted, “leveraging the legal system… all comes down to budgets, we’re aware that a big multinational food company is bringing a legal challenge”(CS16). This highlights, as noted above, that corporate wealth is a crucial element that leads to various other elements, including using UCI resources to take legal action.
Theme 5. Industry Leveraging Policy-Making, Norms, Rules, and Processes
Elements in Theme 5 affect the extent to which industry leverages national and international policy-making norms, rules and processes that favour their participation in policy-making. Some of the key elements that affect these are industry favoured regulatory approaches for policy-making (ie, extent to which governments establish regulatory approaches that mandate industry favoured policy-making procedures, such as business impact assessments, stakeholder consultations, and risk assessments109); industry circumventing national departments of health; support for multistakeholder governance (ie, extent to which national and global governance institutions support the norm for including non-public sector stakeholders in decision-making processes, including corporations); and generating support for industry position.
Stakeholders suggested that UCIs leverage the norm on multistakeholder governance by arguing for the involvement of UCIs in policy-making processes, which is now incumbent upon decision-makers to fulfil. In this theme, participants suggested that UCIs therefore do not necessarily need to use “political practices” to influence public health policy, but the predominant norm for decision-makers is to always involve industry in policy decisions, despite potential conflicts of interest. For example, a stakeholder said, “…when I consult with governments, they say that because of the… [Sustainable Development Goal 17, SDG 17] we have to involve industry and we have to follow the SDGs” (GGO1). The same stakeholder said, “…industry does not need to lobby at all…[public-private partnerships] are sold without any evidence. It’s just the prevailing idea…” (GGO1). Stakeholders also noted that industry involvement in policy processes is already normalised “…they are a natural, normal part of the policy-making and policy implementation process” (A23) and “have this privilege sort of access over other kinds of ‘natural citizens’ into these decision-making processes” (A23). Stakeholders noted that depending on the policy-making spaces, industry actors may go unchallenged due to the lack of CS actors representing public health interests; for example, in international trade negotiations, “public health [actors are]…not in the WTO [World Trade Organisation]” (CS6). Importantly, stakeholders suggested that industry was instrumental in creating this norm of industry involvement in policy discussions, “the private sector was involved in the development of the SDGs” (GGO1) and industries argue, “… ‘well, but we live in a democracy. We are a social actor just like anybody else. Why can’t we participate in the decision-making process?’” (CS9). This suggests how UCIs contribute to developing the frameworks in which policy is made, thus creating feedback loops that perpetuate the ability of UCIs to influence policy.
Stakeholders suggested that there is a disparity between government departments specifically those involved in the economics or finance. For example, a stakeholder said, “government finance, the treasury really does have a veto over [other departments]… They really do control everything across government departments” (FPO4). This is represented by the linked elements industry circumventing national departments of health, and policy incoherence (ie, extent to which there are inconsistent policy goals between government departments).
Stakeholders acknowledged that at the international level, industry is easily represented in policy-making, such as when negotiating trade and investment agreements, whereas this is not the case for public health representatives, “the balance between industry and public health influence on trade agreements [is] very hard for public health people to get on the agenda, whereas industry has an open door in those trade agreements…” (A9). Similarly, stakeholders said, “trade is really like a competing policy arena compared to global health” (CS6), and “industry and trade policies tend to trump out the public health concerns” (CS4). This indicates that trade issues crowd out public health concerns in policy-making spaces.
Discussion
This study aimed to build a systems map depicting the complex pathways through which UCIs influence public health policy. As such influence exhibits characteristics of a complex system, a systems map could help to visualise this complexity, thereby helping to identify ways to change the system. Although previous studies have suggested that UCI influence are complex systems problems,1,3,36,37 to the best of the authors’ knowledge, this study represents the first attempt to explicitly apply participatory systems mapping methods to understand this phenomenon, thus making a methodological contribution. Importantly, this map is neither intended to be comprehensive nor exhaustive, but seeks to provide a starting point for applying systems thinking to explore the complexities surrounding this problem.
We identified five distinct, yet interdependent, themes through which UCIs influence public health policy, which collectively comprise a complex web of interconnected and diverse underlying structures dispersed throughout the system. UCI influence therefore does not have a single point of origin, but is inextricably linked to different parts of the system. This suggests that reducing UCI influence may require disrupting more than one pathway, as is suggested by those within systems science.38,44,45,52,95
One interesting implication from this work is that maps such as these can be used to demonstrate the many interconnections between parts of the system and thus the range of pathways industry could adapt to change (as is known to have occurred after the implementation of Article 5.3, mentioned above58-67). As a hypothetical example, although a change may aim to reduce UCIs’ direct access to public sector decision-makers, UCIs may generate support for their position using front groups to access policy-makers on their behalf. Broader lobbying regulations and transparency policies should therefore be implemented to ascertain whether front groups represent UCIs to manage their access. This systems map helps to make this complexity apparent; it could help to better predict how the system responds to changes,41,51 demonstrate why some changes may be unpredictable110-112 and lead to unintended outcomes.41,44,113
Importantly, while this map offers valuable insights into the complexity surrounding UCI influence, some parts of this map may be less relevant in specific settings, such as authoritarian regimes114 versus liberal democracies,115 or free markets116,117 versus mixed or controlled economies.117,118 For example, given the global prioritisation of GDP growth as a key driver of development,119 Theme 3 (…prioritisation of commercial profits and growth) may be more widely applicable. Conversely, given that varying degrees of authoritarianism and freedom of expression may control the flow of information,120 Theme 2 (creation of confusion and doubt…) may be less applicable in some contexts.
A key question is whether UCI influence is a feature, or a bug, of these underlying structures. If it is a feature, to address UCI influence on public health policy, global society needs to be prepared to change these structures. If society is not prepared to do this, then we need to come to terms with the fact that UCIs will pose a constant barrier to developing effective public health policy, and we need to be realistic about how effective a limited set of interventions can actually be. If, however, it is a bug, then the question is what are the necessary and sufficient conditions to prevent and mitigate UCI influence on public health policy without changing these underlying structures?
This map also depicts how corporate power manifests in different parts of the system. Consistent with the public health literature, this map shows the pathways in which the sources of power (material and ideational) are manifested into instrumental, structural and discursive forms of power, and the overall feedback in which corporate power is perpetuated.7,70-73 UCI influence is clearly a cumulative outcome of these power asymmetries that are upheld, in large part, by the current global political-economic system, which is a key driving force behind the prioritisation of economic/trade policies over public health goals.84,92,121-127 Researchers have suggested leveraging the economic/trade sectors and supply chain actors84,121,125,128,129 to incentivise a system toward prioritising public health outcomes.130-132 However, there may be a fundamental conflict between aspects of economic/trade goals and public health goals,92 which system changes may need to focus on resolving, such as ways of measuring economic growth,92,133,134 the legal status of corporations,8 and UCI fiduciary duties to maximise profits for shareholders.135
Consistent with the literature, this systems map shows the interdependence between different parts of the system. For example, governments are obligated to abide by competition law (including intellectual property protections) through international trade and investment agreements […legal and dispute settlement processes (Theme 4)], leading to the market concentration of UCIs136-138 and dominance over their supply chains137,139-141 […prioritisation of commercial profits and growth (Theme 3)]. Similarly, the literature suggests that UCIs use market-based practices (ie, business practices) to gain a competitive advantage in the market,74,142,143 increasing market concentration.74,75 However, the literature does not always make apparent — which this map helps to do — the cumulative impacts of factors, such as poor labour laws,144,145 pricing strategies,146,147 tax cuts,148 tax avoidance and evasion,149 government subsidies,150,151 intellectual property laws,1 and externalities.152 These together enable corporations to amass a vast amount of wealth, which they, in turn, use to fund their political practices,8,74,75 thus perpetuating a feedback loop between UCI political practices and underlying structures.
Other independencies between systems mapping themes are consistent with the literature. For example, arguments by UCIs in policy consultations at international forums, such as the WHO and WTO, and in national forums […policy-making norms, rules, and processes (Theme 5)], where they use ideological precepts of neoliberalism […prioritisation of commercial profits and growth (Theme 3)] to downplay UCI responsibility in individuals’ consumption of unhealthy products77,153-155 [creation of confusion and doubt… (Theme 2)]. Moreover, the literature illustrates how UCIs use both the threat of litigation and the act of litigating in both domestic and international courts (ie, Investor-State Dispute Settlements) as a long-term strategy to delay the implementation of policy and as a means to achieve regulatory chill.137,156-159 In such spaces they may create confusion and doubt by, for example, attacking evidence that support public health measures156 or arguing that regulations will have a negative impact on smaller businesses, or disproportionately impact vulnerable groups.157
Lastly, UCI influence on public health policy is inextricably linked to how they attempt to influence science, which is a powerful source of industry discursive strategies (ie, industry arguments) for creating confusion and doubt about the harms of their products, legitimising their role as key contributors to science, and advocating for their preferred policy solutions.103 Similarly, UCIs use their involvement in the production of evidence and science to make equivalent arguments in policy processes at national and international levels,29,35,103,154,155,160 which are compounded by industry favoured regulatory approaches, such as the use of impact assessments, stakeholder consultations, and risk assessments — as seen in “Better Regulations” approaches in the UK and EU109,161 […policy-making norms, rules, and processes (Theme 3)]. These regulatory approaches are easily dominated by UCIs, which frame issues in terms of economic or financial costs as opposed to social or health costs.109,161
Strengths and Limitations
This study gathered insights from diverse stakeholders from varied geographic backgrounds and expertise to balance different perspectives. Despite this diversity, stakeholders generally agreed with the broader pattern of UCI influence on public health policy, and the cumulative impact of multiple interacting elements that enable such influence. This study achieves a unique level of inclusivity and representation to ensure a comprehensive understanding of the system, enriching the depth and breadth, and enhancing the credibility, of the results. Additionally, the participatory nature of the workshops foster a sense of ownership and collaboration among stakeholders, making them active contributors to the research process.162
There were also several limitations to this study. Firstly, the systems map is subjective, based on purposively sampled stakeholders, the theoretical lens and knowledge of the facilitator,95,163 and provides only a static visualisation. Although this study achieves a diverse geographical spread, some regions were overrepresented (eg, Europe) whereas others were underrepresented (eg, the East Mediterranean), which may have affected the overall generalisability of the map to different countries and jurisdictions. It is likely that the map will change depending on the period it is captured, the sample of participants, and as different perspectives and knowledge are incorporated. Importantly, this map also does not capture the quantity of evidence supporting each element or the strength of the links between elements. Lastly, participants’ input was welcomed and given equal weight if they felt that they could provide helpful input. This may have adversely affected the map as some participants may have limited knowledge on some parts of the system in which they contributed. However, in practice, participants generally provided input into the areas for which they were selected. Secondly, there was also a broad range of views regarding the language in which to frame elements, the need to balance element granularity (more detail) versus integration (less detail) and its generalisability across context versus being context specific. Indeed, it is important to note that the map depicts broad patterns across different industries and contexts and, as such, a degree of interpretation is needed when applying the map to specific cases.
Thirdly, although this study successfully conducted small group participatory systems mapping workshops for the online environment, it would have benefited from in-person workshops. Stakeholders between workshops were unable to engage with each other directly, which was mitigated by the facilitator relaying ideas across groups. Moreover, stakeholders did not always make themselves clear in workshop discussions. Analysis at times needed to rely on interpreting stakeholder meanings, making it challenging to capture participants’ views and translating them into a systems map. This was mitigated by emailing participants for clarification and seeking feedback from participants on the systems map — although the map would have benefited from further and repeated participant input.
Finally, when stakeholders prepared for workshops by reviewing the preparatory materials, workshop discussions were richer and more constructive. As some stakeholders did not always prepare for workshops, some discussions became stagnant, or more time was needed to explain systems mapping concepts.
Conclusion
This systems map helps to communicate the complexity of UCI influence, namely how pathways to influence are interconnected with each other and their underlying political, economic and social structures. This complexity poses challenges for formulating a singular intervention or limited set of interventions capable of effectively countering such UCI influence. To further help identify areas for systems change, future research could refine or condense this map. Elements or connections could also be weighted, or one may develop a systems-dynamic-model to vary inputs to show which strategies may have more impact on limiting UCI influence. Additionally, to help understand the differences in UCI influence in particular contexts or jurisdictions, further research could adapt or directly apply this map as a conceptual framework in case studies investigating UCI influence, or for testing the relationship between factors that enable influence. Finally, to understand the differences and similarities between systems of influence, researchers could apply systems mapping methods to other industries that seek to influence public health policy in ways that negatively impact public health outcomes, such as the firearms, automobile, pharmaceutical, gambling, or extractive industries, and compare findings.
Acknowledgements
This article is dedicated to the memory of Mateusz Zatoński. Mateusz was a wonderful colleague, and his sad death leaves a gap in tobacco control research which will be hard to fill. He was committed to helping countries worldwide strengthen their tobacco control measures and improving public health for all. He will be much missed.
The authors would like to thank all the participants for giving their time and sharing their invaluable expertise. Fully acknowledged participants are placed in alphabetical order: Alice Fabbri, Tobacco Control Research Group, University of Bath; Andrew Rowell, Tobacco Control Research Group; Angela Carriedo, World Public Health Nutrition Association; Belinda Townsend, Australian National University; Ben Hawkins, MRC Epidemiology Unit, University of Cambridge; Britta Katharina Matthes, Tobacco Control Research Group, University of Bath; Caroline Cerny, Obesity Health Alliance; Charles DH Parry, Alcohol, Tobacco & Other Drug Research Unit, South African Medical Research Council; Crispin Acton, former civil servant, United Kingdom; Daniel Dorado, Corporate Accountability; Debby Sy, Global Centre for Good Governance in Tobacco Control, a STOP Partner; Dhamaravelli ( Vimla ) Moodley, former civil servant South Africa; Fran Baum, Stretton Health Equity, University of Adelaide; Hazel Cheeseman, Deputy Chief Executive, ASH; Jaime Arcila, Corporate Accountability; Jane Martin, Obesity Policy Coalition; Jennifer Lacy-Nichols, University of Melbourne; Kate Oldridge Turner, World Cancer Research Fund International; Kathrin Lauber, University of Edinburgh; Kathryn Reilly, former member of Irish Parliament, Leigh Haynes, Framework Convention on Global Health Alliance; Leslie London, School of Public Health and Family Medicine, University of Cape Town; Lilia Olefir, NGO Advocacy Centre “LIFE”; Lori Lake, The Children’s Institute; Lucy Westerman, VicHealth; Maik Dünnbier, Movendi International; Marian Lorena Ibarra, Food Policy Program, Global Health Advocacy Incubator; Mark Tomlinson, Institute for Life Course Health Research, Department of Global Health, Stellenbosch University; Martin McKee, Professor of European Public Health, LSHTM; Mateusz Zatoński, Tobacco Control Research Group, University of Bath; Mike Daube, Curtin University, Western Australia; Mindaugas Štelemėkas, Head of Health Research Institute, Faculty of Public Health, Lithuanian University of Health Science; Nason Maani, Global Health Policy Unit, University of Edinburgh; Nicholas Freudenberg, CUNY School of Public Health; Nina Renshaw, NCD Alliance; Øystein Bakke, Global Alcohol Policy Alliance; Patricia Lambert, International Legal Consortium at the Campaign for Tobacco-Free Kids; Paula Johns, ACT Health Promotion, Brazil; Pepita Barlow, Department of Health Policy, LSE; Peter Rice, European Alcohol Policy Alliance; Petronell Kruger, The SAMRC/Wits Centre for Health Economics and Decision Science (PRICELESS SA); Raquel Burgess, Department of Social & Behavioural Sciences, Yale School of Public Health; Rima Nakkash, George Mason University; Sarah Dance, Tobacco Control Research Group, University of Bath; Sebastian Rositano, Commercial and Economic Determinants of Health Unit, World Health Organization; Sharon Friel, Australian National University; Sulakshana Nandi, Public Health Resource Network Chhattisgarh India; Susan Goldstein, SAMRC Centre for Health Economics and Decision Science PRICELESS, School of Public Health University of the Witwatersrand; Tara Van Ho, University of Essex; William F Lamb, Mercator Research Institute on Global Commons and Climate Change (MCC). The following participant prefer to be acknowledged by only their affiliation: Oregon State University. One participant preferred not to be acknowledged.
Authors would also like to acknowledge Melissa Mialon and Mark Petticrew for early discussions prior to the development of the study, and Bryan Clift, Selda Ulucanlar, and Harry Rutter for their input on analytical methods.
Ethical issues
Ethical approval (EP20/21002) was granted by Research Ethics Approval Committee for Health (REACH), University of Bath.
Competing interests
The authors declare that they have no competing interests, financial or otherwise, related to the current work. To the best of our ability, this also includes the late Mateusz Zatoński.
Funding
AB received a PhD studentship from University of Bath. AG is supported by the UK Prevention Research Partnership (MR/S037519/1), which is funded by the British Heart Foundation, Cancer Research UK, Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Health and Social Care Research and Development Division (Welsh Government), Medical Research Council, National Institute for Health Research, Natural Environment Research Council, Public Health Agency (Northern Ireland), The Health Foundation and Wellcome. KB is supported by the UK Prevention Research Partnership (MR/S037586/1). AVDA is funded through PhD funding from the University of Bath, in affiliation with the SPECTRUM consortium (MR/S037519/1). SPECTRUM is funded by the UK Prevention Research Partnership (UKPRP). SD and MZ were funded through Bloomberg Philanthropies’ Stopping Tobacco Organizations and Products funding (http://www.bloomberg.org/). None of the funders had any role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Additional Information
Our dear co-author Mateusz Zatoński, PhD, sadly died on January 17, 2022.
Supplementary files
Supplementary file 1. Preliminary Systems Map.
Supplementary file 2. Participant Knowledge Areas and Workshop Groups.
Supplementary file 3. Element Descriptions and Interconnections.
Citation: Bertscher A, Nobles J, Gilmore AB, et al. Building a systems map: applying systems thinking to unhealthy commodity industry influence on public health policy. Int J Health Policy Manag. 2024;13:7872. doi:10.34172/ijhpm.2024.7872
References
- 1.Gilmore AB, Fabbri A, Baum F, et al. Defining and conceptualising the commercial determinants of health. Lancet. 2023;401(10383):1194–1213. doi: 10.1016/s0140-6736(23)00013-2. [DOI] [PubMed] [Google Scholar]
- 2.Ulucanlar S, Lauber K, Fabbri A, et al. Corporate political activity: taxonomies and model of corporate influence on public policy. Int J Health Policy Manag. 2023;12:7292. doi: 10.34172/ijhpm.2023.7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knai C, Petticrew M, Capewell S, et al. The case for developing a cohesive systems approach to research across unhealthy commodity industries. BMJ Glob Health. 2021;6(2):e003543. doi: 10.1136/bmjgh-2020-003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Lacy-Vawdon C, Livingstone C. Defining the commercial determinants of health: a systematic review. BMC Public Health. 2020;20(1):1022. doi: 10.1186/s12889-020-09126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savell E, Fooks G, Gilmore AB. How does the alcohol industry attempt to influence marketing regulations? A systematic review. Addiction. 2016;111(1):18–32. doi: 10.1111/add.13048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wiist WH. Public health and the anticorporate movement: rationale and recommendations. Am J Public Health. 2006;96(8):1370–1375. doi: 10.2105/ajph.2005.072298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madureira Lima J, Galea S. Corporate practices and health: a framework and mechanisms. Global Health. 2018;14(1):21. doi: 10.1186/s12992-018-0336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wiist WH. The Bottom Line or Public Health: Tactics Corporations Use to Influence Health and Health Policy, and What We Can Do to Counter Them. Oxford: Oxford University Press; 2010.
- 9. Freudenberg N. Lethal but Legal: Corporations, Consumption, and Protecting Public Health. Oxford University Press; 2014.
- 10.Freudenberg N. The manufacture of lifestyle: the role of corporations in unhealthy living. J Public Health Policy. 2012;33(2):244–256. doi: 10.1057/jphp.2011.60. [DOI] [PubMed] [Google Scholar]
- 11.Freudenberg N, Galea S. The impact of corporate practices on health: implications for health policy. J Public Health Policy. 2008;29(1):86–104. doi: 10.1057/palgrave.jphp.3200158. [DOI] [PubMed] [Google Scholar]
- 12.Jahiel RI. Corporation-induced diseases, upstream epidemiologic surveillance, and urban health. J Urban Health. 2008;85(4):517–531. doi: 10.1007/s11524-008-9283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savell E, Gilmore AB, Fooks G. How does the tobacco industry attempt to influence marketing regulations? A systematic review. PLoS One. 2014;9(2):e87389. doi: 10.1371/journal.pone.0087389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mialon M, Swinburn B, Sacks G. A proposed approach to systematically identify and monitor the corporate political activity of the food industry with respect to public health using publicly available information. Obes Rev. 2015;16(7):519–530. doi: 10.1111/obr.12289. [DOI] [PubMed] [Google Scholar]
- 15.Mialon M, da Silva Gomes F. Public health and the ultra-processed food and drink products industry: corporate political activity of major transnationals in Latin America and the Caribbean. Public Health Nutr. 2019;22(10):1898–1908. doi: 10.1017/s1368980019000417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mialon M, McCambridge J. Alcohol industry corporate social responsibility initiatives and harmful drinking: a systematic review. Eur J Public Health. 2018;28(4):664–673. doi: 10.1093/eurpub/cky065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mialon M, Mialon J. Analysis of corporate political activity strategies of the food industry: evidence from France. Public Health Nutr. 2018;21(18):3407–3421. doi: 10.1017/s1368980018001763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mialon M, Mialon J. Corporate political activity of the dairy industry in France: an analysis of publicly available information. Public Health Nutr. 2017;20(13):2432–2439. doi: 10.1017/s1368980017001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mialon M, Swinburn B, Allender S, Sacks G. Systematic examination of publicly-available information reveals the diverse and extensive corporate political activity of the food industry in Australia. BMC Public Health. 2016;16:283. doi: 10.1186/s12889-016-2955-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mialon M, Swinburn B, Wate J, Tukana I, Sacks G. Analysis of the corporate political activity of major food industry actors in Fiji. Global Health. 2016;12(1):18. doi: 10.1186/s12992-016-0158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paixão MM, Mialon M. Help or hindrance? The alcohol industry and alcohol control in Portugal. Int J Environ Res Public Health. 2019;16(22):4554. doi: 10.3390/ijerph16224554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanrikulu H, Neri D, Robertson A, Mialon M. Corporate political activity of the baby food industry: the example of Nestlé in the United States of America. Int Breastfeed J. 2020;15(1):22. doi: 10.1186/s13006-020-00268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson SJ. Marketing of menthol cigarettes and consumer perceptions: a review of tobacco industry documents. Tob Control. 2011;20(Suppl 2):ii20–28. doi: 10.1136/tc.2010.041939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith KE, Fooks G, Collin J, Weishaar H, Mandal S, Gilmore AB. “Working the system”--British American tobacco’s influence on the European Union treaty and its implications for policy: an analysis of internal tobacco industry documents. PLoS Med. 2010;7(1):e1000202. doi: 10.1371/journal.pmed.1000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costa H, Gilmore AB, Peeters S, McKee M, Stuckler D. Quantifying the influence of the tobacco industry on EU governance: automated content analysis of the EU Tobacco Products Directive. Tob Control. 2014;23(6):473–478. doi: 10.1136/tobaccocontrol-2014-051822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Legresley E, Lee K, Muggli ME, Patel P, Collin J, Hurt RD. British American Tobacco and the “insidious impact of illicit trade” in cigarettes across Africa. Tob Control. 2008;17(5):339–346. doi: 10.1136/tc.2008.025999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ong EK, Glantz SA. Constructing “sound science” and “good epidemiology”: tobacco, lawyers, and public relations firms. Am J Public Health. 2001;91(11):1749–1757. doi: 10.2105/ajph.91.11.1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lawrence S, Collin J. Competing with kreteks: transnational tobacco companies, globalisation, and Indonesia. Tob Control. 2004;13(Suppl 2):ii96–103. doi: 10.1136/tc.2004.009340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bertscher A, London L, Orgill M. Unpacking policy formulation and industry influence: the case of the draft control of marketing of alcoholic beverages bill in South Africa. Health Policy Plan. 2018;33(7):786–800. doi: 10.1093/heapol/czy049. [DOI] [PubMed] [Google Scholar]
- 30.Brownell KD, Warner KE. The perils of ignoring history: big tobacco played dirty and millions died. How similar is big food? Milbank Q. 2009;87(1):259–294. doi: 10.1111/j.1468-0009.2009.00555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Vogli R, Kouvonen A, Gimeno D. The influence of market deregulation on fast food consumption and body mass index: a cross-national time series analysis. Bull World Health Organ. 2014;92(2):99–107A. doi: 10.2471/blt.13.120287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dorfman L, Cheyne A, Friedman LC, Wadud A, Gottlieb M. Soda and tobacco industry corporate social responsibility campaigns: how do they compare? PLoS Med. 2012;9(6):e1001241. doi: 10.1371/journal.pmed.1001241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Monteiro CA, Cannon G. The impact of transnational “big food” companies on the South: a view from Brazil. PLoS Med. 2012;9(7):e1001252. doi: 10.1371/journal.pmed.1001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nestle M. Food Politics: How the Food Industry Influences Nutrition and Health. Berkeley: University of California Press; 2013.
- 35.Ulucanlar S, Fooks GJ, Gilmore AB. The policy dystopia model: an interpretive analysis of tobacco industry political activity. PLoS Med. 2016;13(9):e1002125. doi: 10.1371/journal.pmed.1002125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Knai C, Petticrew M, Mays N, et al. Systems thinking as a framework for analyzing commercial determinants of health. Milbank Q. 2018;96(3):472–498. doi: 10.1111/1468-0009.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Milsom P, Smith R, Walls H. A systems thinking approach to inform coherent policy action for NCD prevention: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(5):212–214. doi: 10.15171/ijhpm.2019.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nobles JD, Radley D, Mytton OT. The Action Scales Model: a conceptual tool to identify key points for action within complex adaptive systems. Perspect Public Health. 2022;142(6):328–337. doi: 10.1177/17579139211006747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barbrook-Johnson P, Penn A. Participatory systems mapping for complex energy policy evaluation. Evaluation. 2021;27(1):57–79. doi: 10.1177/1356389020976153. [DOI] [Google Scholar]
- 40.Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet. 2017;390(10112):2602–2604. doi: 10.1016/s0140-6736(17)31267-9. [DOI] [PubMed] [Google Scholar]
- 41. Stroh DP. Systems Thinking for Social Change: A Practical Guide to Solving Complex Problems, Avoiding Unintended Consequences, and Achieving Lasting Results. Chelsea Green Publishing; 2015.
- 42. The Health Foundation. Evidence Scan: Complex Adaptive Systems. London, UK: The Health Foundation; 2010.
- 43.Sterman JD. Learning from evidence in a complex world. Am J Public Health. 2006;96(3):505–514. doi: 10.2105/ajph.2005.066043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Meadows DH. Thinking in Systems: A Primer. London, UK: Chelsea Green Publishing; 2008.
- 45. Jebb SA, Finegood DT, Diez Roux AV, et al. Systems-Based Approaches in Public Health: Where Next? The Academy of Medical Sciences, Canadian Academy of Health Sciences; 2020.
- 46. Checkland P. Systems thinking and soft systems methodology. In: Galliers RD, Currie WL, eds. The Oxford Handbook of Management Information Systems. Oxford University Press; 2011.
- 47. Checkland P. Systems thinking, systems practice. In: Currie WL, Galliers B, eds. Rethinking Management Information Systems. Oxford: Oxford University Press; 1999:45-56.
- 48.Carey G, Malbon E, Carey N, Joyce A, Crammond B, Carey A. Systems science and systems thinking for public health: a systematic review of the field. BMJ Open. 2015;5(12):e009002. doi: 10.1136/bmjopen-2015-009002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peters DH. The application of systems thinking in health: why use systems thinking? Health Res Policy Syst. 2014;12:51. doi: 10.1186/1478-4505-12-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leischow SJ, Best A, Trochim WM, et al. Systems thinking to improve the public’s health. Am J Prev Med. 2008;35(2 Suppl):S196–203. doi: 10.1016/j.amepre.2008.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kim DH. Systems Thinking Tools: A User’s Reference Guide. Waltham, MA: Pegasus Communications Inc; 1994.
- 52. Meadows DH. Leverage Points: Places to Intervene in a System. The Sustainability Institute; 1999.
- 53.Diez Roux AV. Complex systems thinking and current impasses in health disparities research. Am J Public Health. 2011;101(9):1627–1634. doi: 10.2105/ajph.2011.300149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Johnston LM, Matteson CL, Finegood DT. Systems science and obesity policy: a novel framework for analyzing and rethinking population-level planning. Am J Public Health. 2014;104(7):1270–1278. doi: 10.2105/ajph.2014.301884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fooks GJ, Gilmore AB. Corporate philanthropy, political influence, and health policy. PLoS One. 2013;8(11):e80864. doi: 10.1371/journal.pone.0080864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fooks G, Gilmore A, Collin J, Holden C, Lee K. The limits of corporate social responsibility: techniques of neutralization, stakeholder management and political CSR. J Bus Ethics. 2013;112(2):283–299. doi: 10.1007/s10551-012-1250-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fooks GJ, Gilmore AB, Smith KE, Collin J, Holden C, Lee K. Corporate social responsibility and access to policy élites: an analysis of tobacco industry documents. PLoS Med. 2011;8(8):e1001076. doi: 10.1371/journal.pmed.1001076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Peeters S, Costa H, Stuckler D, McKee M, Gilmore AB. The revision of the 2014 European tobacco products directive: an analysis of the tobacco industry’s attempts to ‘break the health silo. ’ Tob Control. 2016;25(1):108–117. doi: 10.1136/tobaccocontrol-2014-051919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tobacco Tactics. Third Party Techniques. 2019. https://tobaccotactics.org/wiki/Third-Party-Techniques/. Accessed June 11, 2020.
- 60.Thomas SL, David J, Randle M, Daube M, Senior K. Gambling advocacy: lessons from tobacco, alcohol and junk food. Aust N Z J Public Health. 2016;40(3):211–217. doi: 10.1111/1753-6405.12410. [DOI] [PubMed] [Google Scholar]
- 61.Hird TR, Gallagher AWA, Evans-Reeves K, et al. Understanding the long-term policy influence strategies of the tobacco industry: two contemporary case studies. Tob Control. 2022;31(2):297–307. doi: 10.1136/tobaccocontrol-2021-057030. [DOI] [PubMed] [Google Scholar]
- 62.Peeters S, Gilmore AB. Understanding the emergence of the tobacco industry’s use of the term tobacco harm reduction in order to inform public health policy. Tob Control. 2015;24(2):182–189. doi: 10.1136/tobaccocontrol-2013-051502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peeters S, Gilmore AB. Transnational tobacco company interests in smokeless tobacco in Europe: analysis of internal industry documents and contemporary industry materials. PLoS Med. 2013;10(9):e1001506. doi: 10.1371/journal.pmed.1001506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tobacco Tactics. Harm Reduction. 2020. https://tobaccotactics.org/wiki/harm-reduction/#:~:text=A%20harm%20reduction%20approach%20to,ultimately%20quitting%20nicotine%20use%20altogether. Accessed June 12, 2020.
- 65.Fitzpatrick I, Bertscher A, Gilmore AB. Identifying misleading corporate narratives: the application of linguistic and qualitative methods to commercial determinants of health research. PLOS Glob Public Health. 2022;2(11):e0000379. doi: 10.1371/journal.pgph.0000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Tobacco Tactics. Newer Nicotine and Tobacco Products: British American Tobacco. 2022. https://tobaccotactics.org/wiki/newer-nicotine-and-tobacco-products-british-american-tobacco/. Accessed April 26, 2022.
- 67.Fitzpatrick I, Dance S, Silver K, Violini M, Hird TR. Tobacco industry messaging around harm: narrative framing in PMI and BAT press releases and annual reports 2011 to 2021. Front Public Health. 2022;10:958354. doi: 10.3389/fpubh.2022.958354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li M, Trencher G, Asuka J. The clean energy claims of BP, Chevron, ExxonMobil and Shell: a mismatch between discourse, actions and investments. PLoS One. 2022;17(2):e0263596. doi: 10.1371/journal.pone.0263596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson P, Kokole D, Jané Llopis E, Burton R, Lachenmeier DW. Lower strength alcohol products-a realist review-based road map for European policy making. Nutrients. 2022;14(18):3779. doi: 10.3390/nu14183779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Thorn M. Addressing power and politics through action on the commercial determinants of health. Health Promot J Austr. 2018;29(3):225–227. doi: 10.1002/hpja.216. [DOI] [PubMed] [Google Scholar]
- 71.Milsom P, Smith R, Baker P, Walls H. Corporate power and the international trade regime preventing progressive policy action on non-communicable diseases: a realist review. Health Policy Plan. 2021;36(4):493–508. doi: 10.1093/heapol/czaa148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wood B, Baker P, Sacks G. Conceptualising the commercial determinants of health using a power lens: a review and synthesis of existing frameworks. Int J Health Policy Manag. 2022;11(8):1251–1261. doi: 10.34172/ijhpm.2021.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McKee M, Stuckler D. Revisiting the corporate and commercial determinants of health. Am J Public Health. 2018;108(9):1167–1170. doi: 10.2105/ajph.2018.304510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wood B, Williams O, Nagarajan V, Sacks G. Market strategies used by processed food manufacturers to increase and consolidate their power: a systematic review and document analysis. Global Health. 2021;17(1):17. doi: 10.1186/s12992-021-00667-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wood B, Williams O, Baker P, Nagarajan V, Sacks G. The influence of corporate market power on health: exploring the structure-conduct-performance model from a public health perspective. Global Health. 2021;17(1):41. doi: 10.1186/s12992-021-00688-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lacy-Nichols J, Marten R. Power and the commercial determinants of health: ideas for a research agenda. BMJ Glob Health. 2021;6(2):e003850. doi: 10.1136/bmjgh-2020-003850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barlow P, Thow AM. Neoliberal discourse, actor power, and the politics of nutrition policy: a qualitative analysis of informal challenges to nutrition labelling regulations at the World Trade Organization, 2007-2019. Soc Sci Med. 2021;273:113761. doi: 10.1016/j.socscimed.2021.113761. [DOI] [PubMed] [Google Scholar]
- 78.Townsend B, Schram A, Labonté R, Baum F, Friel S. How do actors with asymmetrical power assert authority in policy agenda-setting? A study of authority claims by health actors in trade policy. Soc Sci Med. 2019;236:112430. doi: 10.1016/j.socscimed.2019.112430. [DOI] [PubMed] [Google Scholar]
- 79.Sula-Raxhimi E, Butzbach C, Brousselle A. Planetary health: countering commercial and corporate power. Lancet Planet Health. 2019;3(1):e12–e13. doi: 10.1016/s2542-5196(18)30241-9. [DOI] [PubMed] [Google Scholar]
- 80.Kentikelenis A, Rochford C. Power asymmetries in global governance for health: a conceptual framework for analyzing the political-economic determinants of health inequities. Global Health. 2019;15(Suppl 1):70. doi: 10.1186/s12992-019-0516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Battams S, Townsend B. Power asymmetries, policy incoherence and noncommunicable disease control - a qualitative study of policy actor views. Crit Public Health. 2019;29(5):596–609. doi: 10.1080/09581596.2018.1492093. [DOI] [Google Scholar]
- 82.Abdul Mu’eez AS, Arifah AR, Azreena MB, Farahana MP, Mustafa AD, Juni MH. Agenda setting and power in policy making: a case study of tobacco policy in developing countries. Int J Public Health Clin Sci. 2018;5(3):1–16. [Google Scholar]
- 83.Pechlaner G, Otero G. The neoliberal food regime: neoregulation and the new division of labor in North America. Rural Sociol. 2010;75(2):179–208. doi: 10.1111/j.1549-0831.2009.00006.x. [DOI] [Google Scholar]
- 84.Lencucha R, Thow AM. How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention. Int J Health Policy Manag. 2019;8(9):514–520. doi: 10.15171/ijhpm.2019.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Otero G. The neoliberal food regime in Latin America: state, agribusiness transnational corporations and biotechnology. Rev Can Etudes Dev. 2012;33(3):282–294. doi: 10.1080/02255189.2012.711747. [DOI] [Google Scholar]
- 86.Parker LA, Zaragoza GA, Hernández-Aguado I. Promoting population health with public-private partnerships: where’s the evidence? BMC Public Health. 2019;19(1):1438. doi: 10.1186/s12889-019-7765-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Erzse A, Karim SA, Foley L, Hofman KJ. A realist review of voluntary actions by the food and beverage industry and implications for public health and policy in low- and middle-income countries. Nat Food. 2022;3(8):650–663. doi: 10.1038/s43016-022-00552-5. [DOI] [PubMed] [Google Scholar]
- 88.Mialon M, Vandevijvere S, Carriedo-Lutzenkirchen A, et al. Mechanisms for addressing and managing the influence of corporations on public health policy, research and practice: a scoping review. BMJ Open. 2020;10(7):e034082. doi: 10.1136/bmjopen-2019-034082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mialon M. An overview of the commercial determinants of health. Global Health. 2020;16(1):74. doi: 10.1186/s12992-020-00607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lacy-Nichols J, Marten R, Crosbie E, Moodie R. The public health playbook: ideas for challenging the corporate playbook. Lancet Glob Health. 2022;10(7):e1067–e1072. doi: 10.1016/s2214-109x(22)00185-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Friel S, Collin J, Daube M, et al. Commercial determinants of health: future directions. Lancet. 2023;401(10383):1229–1240. doi: 10.1016/s0140-6736(23)00011-9. [DOI] [PubMed] [Google Scholar]
- 92.Labonté R. Neoliberalism 40: the rise of illiberal capitalism: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(4):175–178. doi: 10.15171/ijhpm.2019.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Willis CD, Mitton C, Gordon J, Best A. System tools for system change. BMJ Qual Saf. 2012;21(3):250–262. doi: 10.1136/bmjqs-2011-000482. [DOI] [PubMed] [Google Scholar]
- 94. Williams B, Hummelbrunner R. Systems Concepts in Action: A Practitioner’s Toolkit. Stanford University Press; 2010.
- 95. Barbrook-Johnson P, Penn AS. Systems Mapping: How to Build and Use Causal Models of Systems. Cham, Switzerland: Palgrave Macmillan; 2022.
- 96. World Health Organization (WHO). Global Status Report on Noncommunicable Diseases 2014. Geneva: WHO; 2014. [DOI] [PubMed]
- 97. World Health Organization (WHO). Four Noncommunicable Diseases, Four Shared Risk Factors. https://www.who.int/ncdnet/about/4diseases/en/. Accessed July 21, 2020.
- 98. World Health Organization (WHO). Noncommunicable Diseases Country Profiles 2018. Geneva: WHO; 2018.
- 99. World Health Organization (WHO). Noncommunicable Diseases. 2018. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases. Accessed June 9, 2020.
- 100.Burke JG, O’Campo P, Peak GL, Gielen AC, McDonnell KA, Trochim WM. An introduction to concept mapping as a participatory public health research method. Qual Health Res. 2005;15(10):1392–1410. doi: 10.1177/1049732305278876. [DOI] [PubMed] [Google Scholar]
- 101.Trani JF, Ballard E, Bakhshi P, Hovmand P. Community based system dynamic as an approach for understanding and acting on messy problems: a case study for global mental health intervention in Afghanistan. Confl Health. 2016;10:25. doi: 10.1186/s13031-016-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Glenn J, Kamara K, Umar ZA, Chahine T, Daulaire N, Bossert T. Applied systems thinking: a viable approach to identify leverage points for accelerating progress towards ending neglected tropical diseases. Health Res Policy Syst. 2020;18(1):56. doi: 10.1186/s12961-020-00570-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Legg T, Hatchard J, Gilmore AB. The science for profit model-how and why corporations influence science and the use of science in policy and practice. PLoS One. 2021;16(6):e0253272. doi: 10.1371/journal.pone.0253272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kurnaz FB, Ergün E, Ilgaz H. Participation in online discussion environments: is it really effective? Educ Inf Technol. 2018;23(4):1719–1736. doi: 10.1007/s10639-018-9688-4. [DOI] [Google Scholar]
- 105.Chavez-Ugalde Y, Toumpakari Z, White M, De Vocht F, Jago R. Using group model building to frame the commercial determinants of dietary behaviour in adolescence - proposed methods for online system mapping workshops. BMC Med Res Methodol. 2022;22(1):84. doi: 10.1186/s12874-022-01576-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Scriptapedia. Causal Mapping with Seed Structure. 2013. https://en.wikibooks.org/wiki/Scriptapedia/Causal_Mapping_with_Seed_Structure. Accessed April 27, 2022.
- 107. Andersen DF, Calhoun A, Hovmand PS, et al. Scriptapedia. 2021. https://en.wikibooks.org/wiki/Scriptapedia. Accessed April 27, 2022.
- 108.Campbell S, Greenwood M, Prior S, et al. Purposive sampling: complex or simple? Research case examples. J Res Nurs. 2020;25(8):652–661. doi: 10.1177/1744987120927206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Smith KE, Fooks G, Gilmore AB, Collin J, Weishaar H. Corporate coalitions and policy making in the European Union: how and why British American Tobacco promoted “better regulation”. J Health Polit Policy Law. 2015;40(2):325–372. doi: 10.1215/03616878-2882231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chandler J, Rycroft-Malone J, Hawkes C, Noyes J. Application of simplified complexity theory concepts for healthcare social systems to explain the implementation of evidence into practice. J Adv Nurs. 2016;72(2):461–480. doi: 10.1111/jan.12815. [DOI] [PubMed] [Google Scholar]
- 111.Keshavarz N, Nutbeam D, Rowling L, Khavarpour F. Schools as social complex adaptive systems: a new way to understand the challenges of introducing the health promoting schools concept. Soc Sci Med. 2010;70(10):1467–1474. doi: 10.1016/j.socscimed.2010.01.034. [DOI] [PubMed] [Google Scholar]
- 112.Rickles D, Hawe P, Shiell A. A simple guide to chaos and complexity. J Epidemiol Community Health. 2007;61(11):933–937. doi: 10.1136/jech.2006.054254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bonell C, Jamal F, Melendez-Torres GJ, Cummins S. ‘Dark logic’: theorising the harmful consequences of public health interventions. J Epidemiol Community Health. 2015;69(1):95–98. doi: 10.1136/jech-2014-204671. [DOI] [PubMed] [Google Scholar]
- 114. Linz JJ. Totalitarian and Authoritarian Regimes. Lynne Rienner Publishers; 2000.
- 115.Fukuyama F. Liberal democracy as a global phenomenon. PS Polit Sci Polit. 1991;24(4):659–664. doi: 10.2307/419399. [DOI] [Google Scholar]
- 116. Schrecker T, Bambra C. How Politics Makes Us Sick: Neoliberal Epidemics. Springer; 2015.
- 117. Harvey D. A Brief History of Neoliberalism. USA: Oxford University Press; 2007.
- 118. Chang HJ. 23 Things They Don’t Tell You About Capitalism. USA: Bloomsbury Publishing; 2012.
- 119.Hickel J, Kallis G. Is green growth possible? New Political Econ. 2020;25(4):469–486. doi: 10.1080/13563467.2019.1598964. [DOI] [Google Scholar]
- 120. Stockmann D. Media Commercialization and Authoritarian Rule in China. Cambridge University Press; 2013.
- 121.Lencucha R, Thow AM. Intersectoral policy on industries that produce unhealthy commodities: governing in a new era of the global economy? BMJ Glob Health. 2020;5(8):e002246. doi: 10.1136/bmjgh-2019-002246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Herrick C. On the perils of universal and product-led thinking: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(5):209–211. doi: 10.15171/ijhpm.2019.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Krzyżanowski M. Normalization and the discursive construction of “new” norms and “new” normality: discourse in the paradoxes of populism and neoliberalism. Soc Semiot. 2020;30(4):431–448. doi: 10.1080/10350330.2020.1766193. [DOI] [Google Scholar]
- 124.Lee K, Crosbie E. Understanding structure and agency as commercial determinants of health: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(7):315–318. doi: 10.15171/ijhpm.2019.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Schram A, Goldman S. Paradigm shift: new ideas for a structural approach to NCD prevention: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(3):124–127. doi: 10.15171/ijhpm.2019.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Smith J. Towards critical analysis of the political determinants of health: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(3):121–123. doi: 10.15171/ijhpm.2019.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Townsend B. Next steps for elevating health on trade and investment policy agendas: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(7):312–314. doi: 10.15171/ijhpm.2019.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Battams S. Neo-Liberalism, Policy incoherence and discourse coalitions influencing non-communicable disease strategy: Comment on “How neoliberalism is shaping the supply of unhealthy commodities and what this means for NCD prevention”. Int J Health Policy Manag. 2020;9(3):116–118. doi: 10.15171/ijhpm.2019.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Glasgow S, Schrecker T. The double burden of neoliberalism? Noncommunicable disease policies and the global political economy of risk. Health Place. 2015;34:279–286. doi: 10.1016/j.healthplace.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 130.Collin J. Tobacco control, global health policy and development: towards policy coherence in global governance. Tob Control. 2012;21(2):274–280. doi: 10.1136/tobaccocontrol-2011-050418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lencucha R, Drope J, Chavez JJ. Whole-of-government approaches to NCDs: the case of the Philippines Interagency Committee-Tobacco. Health Policy Plan. 2015;30(7):844–852. doi: 10.1093/heapol/czu085. [DOI] [PubMed] [Google Scholar]
- 132.Blouin C. Trade policy and health: from conflicting interests to policy coherence. Bull World Health Organ. 2007;85(3):169–173. doi: 10.2471/blt.06.037413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Raworth K. Doughnut Economics: Seven Ways to Think Like a 21st-Century Economist. Chelsea Green Publishing; 2017.
- 134. Hickel J. Less is More: How Degrowth Will Save the World. Random House; 2020.
- 135.Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–679. doi: 10.1016/s0140-6736(12)62089-3. [DOI] [PubMed] [Google Scholar]
- 136.Room R, Gleeson D, Miller M. Alcoholic beverages in trade agreements: industry lobbying and the public health interest. Drug Alcohol Rev. 2021;40(1):19–21. doi: 10.1111/dar.13214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Milsom P, Smith R, Baker P, Walls H. International investment liberalization, transnational corporations and NCD prevention policy non-decisions: a realist review on the political economy of tobacco, alcohol and ultra-processed food. Global Health. 2021;17(1):134. doi: 10.1186/s12992-021-00784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hawkins B, Holden C, Eckhardt J, Lee K. Reassessing policy paradigms: a comparison of the global tobacco and alcohol industries. Glob Public Health. 2018;13(1):1–19. doi: 10.1080/17441692.2016.1161815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schram A, Townsend B. International trade and investment and food systems: what we know, what we don’t know, and what we don’t know we don’t know. Int J Health Policy Manag. 2021;10(12):886–895. doi: 10.34172/ijhpm.2020.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Miller M, Wilkinson C, Room R, et al. Industry submissions on alcohol in the context of Australia’s trade and investment agreements: a content and thematic analysis of publicly available documents. Drug Alcohol Rev. 2021;40(1):22–30. doi: 10.1111/dar.13219. [DOI] [PubMed] [Google Scholar]
- 141.Gleeson D, Friel S. Emerging threats to public health from regional trade agreements. Lancet. 2013;381(9876):1507–1509. doi: 10.1016/s0140-6736(13)60312-8. [DOI] [PubMed] [Google Scholar]
- 142.Eastmure E, Cummins S, Sparks L. Non-market strategy as a framework for exploring commercial involvement in health policy: a primer. Soc Sci Med. 2020;262:113257. doi: 10.1016/j.socscimed.2020.113257. [DOI] [PubMed] [Google Scholar]
- 143.Baum FE, Sanders DM, Fisher M, et al. Assessing the health impact of transnational corporations: its importance and a framework. Global Health. 2016;12(1):27. doi: 10.1186/s12992-016-0164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Labonté R, Schrecker T. Globalization and social determinants of health: the role of the global marketplace (part 2 of 3) Global Health. 2007;3:6. doi: 10.1186/1744-8603-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ramos AK. Child labor in global tobacco production: a human rights approach to an enduring dilemma. Health Hum Rights. 2018;20(2):235–248. [PMC free article] [PubMed] [Google Scholar]
- 146.Sheikh ZD, Branston JR, Gilmore AB. Tobacco industry pricing strategies in response to excise tax policies: a systematic review. Tob Control. 2023;32(2):239–250. doi: 10.1136/tobaccocontrol-2021-056630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bennett R, Zorbas C, Huse O, et al. Prevalence of healthy and unhealthy food and beverage price promotions and their potential influence on shopper purchasing behaviour: a systematic review of the literature. Obes Rev. 2020;21(1):e12948. doi: 10.1111/obr.12948. [DOI] [PubMed] [Google Scholar]
- 148.Gechert S, Heimberger P. Do corporate tax cuts boost economic growth? Eur Econ Rev. 2022;147:104157. doi: 10.1016/j.euroecorev.2022.104157. [DOI] [Google Scholar]
- 149. Tax Justice Network. Tax avoidance and evasion-The scale of the problem. Tax Justice Network; 2017.
- 150. UNEP, UNDP, FAO. A Multi-Billion-Dollar Opportunity: Repurposing Agricultural Support to Transform Food Systems. Food and Agriculture Organization; 2021.
- 151.Anderson K, Meloni G, Swinnen J. Global alcohol markets: evolving consumption patterns, regulations, and industrial organizations. Annu Rev Resour Economics. 2018;10:105–132. doi: 10.1146/annurev-resource-100517-023331. [DOI] [Google Scholar]
- 152. Blecher E, Bertram M. The economics and control of tobacco, alcohol, food products, and sugar-sweetened beverages. In: Vaccarella S, Lortet-Tieulent J, Saracci R, Conway DI, Straif K, Wild CP, eds. Reducing Social Inequalities in Cancer: Evidence and Priorities for Research. Lyon, FR: International Agency for Research on Cancer; 2019. [PubMed]
- 153.Lauber K, Ralston R, Mialon M, Carriedo A, Gilmore AB. Non-communicable disease governance in the era of the sustainable development goals: a qualitative analysis of food industry framing in WHO consultations. Global Health. 2020;16(1):76. doi: 10.1186/s12992-020-00611-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lauber K, Rutter H, Gilmore AB. Big food and the World Health Organization: a qualitative study of industry attempts to influence global-level non-communicable disease policy. BMJ Glob Health. 2021;6(6):e005216. doi: 10.1136/bmjgh-2021-005216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lauber K, McGee D, Gilmore AB. Commercial use of evidence in public health policy: a critical assessment of food industry submissions to global-level consultations on non-communicable disease prevention. BMJ Glob Health. 2021;6(8):e006176. doi: 10.1136/bmjgh-2021-006176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhou S, Ricafort E, Bressler D, Devotsu RK. Litigation in tobacco control: past, present and future. Tob Control. 2022;31(2):291–295. doi: 10.1136/tobaccocontrol-2021-056561. [DOI] [PubMed] [Google Scholar]
- 157.Roache SA, Platkin C, Gostin LO, Kaplan C. Big food and soda versus public health: industry litigation against local government regulations to promote healthy diets. Fordham Urban Law J. 2017;45(4):1051–1089. [Google Scholar]
- 158.Hawkins B, Holden C. A corporate veto on health policy? Global constitutionalism and investor-state dispute settlement. J Health Polit Policy Law. 2016;41(5):969–995. doi: 10.1215/03616878-3632203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Milsom P, Smith R, Modisenyane SM, Walls H. Do international trade and investment agreements generate regulatory chill in public health policymaking? A case study of nutrition and alcohol policy in South Africa. Global Health. 2021;17(1):104. doi: 10.1186/s12992-021-00757-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ulucanlar S, Fooks GJ, Hatchard JL, Gilmore AB. Representation and misrepresentation of scientific evidence in contemporary tobacco regulation: a review of tobacco industry submissions to the UK government consultation on standardised packaging. PLoS Med. 2014;11(3):e1001629. doi: 10.1371/journal.pmed.1001629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Berry C, Devlin S. Threat to Democracy: The Impact of ‘Better Regulation’ in the UK. London: New Economics Foundation; 2008.
- 162.Boaz A, Hanney S, Borst R, O’Shea A, Kok M. How to engage stakeholders in research: design principles to support improvement. Health Res Policy Syst. 2018;16(1):60. doi: 10.1186/s12961-018-0337-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Jacobson D, Mustafa N. Social Identity Map: A reflexivity tool for practicing explicit positionality in critical qualitative research. Int J Qual Methods. 2019;18:1609406919870075. doi: 10.1177/1609406919870075. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file 1. Preliminary Systems Map.
Supplementary file 2. Participant Knowledge Areas and Workshop Groups.
Supplementary file 3. Element Descriptions and Interconnections.