Abstract
E-cigarettes gained popularity globally through the promotion of e-cigarettes as a risk-free way to stop traditional smoking. However, new evidence suggests that they may have a detrimental effect on the nervous system and ultimately adverse neurological manifestations. Seizures have been reported among both new and experienced e-cigarette users. In several cases, the seizure presented immediately after its use, while others reported continuous use for weeks before seizures occurred. This review presents a deeper insight into the clinical management, implications, and public health considerations of seizure susceptibility in e-cigarette users. Using recent case reports, epidemiological studies, and experimental research, we highlight the role of likely etiological mechanisms such as how nicotine’s convulsive effects are linked to α7- nicotinic acetylcholine receptors (nAChRs), the varied clinical presentations, and the potential nicotine toxicity linked to seizures. Furthermore, we discuss the existing debates and controversies, diagnostic directions, and potential role in individual susceptibility to e-cigarette-associated seizures. Importantly, we address how seizures may be accompanied by both physical and psychological sequelae, which may impair the quality of life for individuals presenting for emergency care. We also address the limitations and challenges in the etiology of e-cigarette-associated seizures and the non-criteria for defining seizures caused by e-cigarettes. The review concludes with an insight into public health considerations and policy recommendations by highlighting the importance of mass awareness and clinical considerations that could guide patient management.
Keywords: E-cigarette/electronic cigarette, vaping-related seizures, seizure risk, electronic nicotine delivery systems, e-cigarette-related seizures
Introduction
In recent years, e-cigarettes have gained popularity all over the world. 1 In the US and Canada, the proportion of young people who vape regularly has at least doubled between 2017 and 2019. 2 This is the case for a variety of reasons. These include its use as a healthier substitute for smoking cigarettes, 3 as well as its social recognition as a more refined option. E-cigarettes, or electronic cigarettes, are battery-operated devices that resemble traditional tobacco cigarettes but do not operate by burning tobacco. Rather, the devices vaporize e-liquid, which consists of vegetable glycerin (VG), propylene glycol (PG), and nicotine. Additionally, various aldehydes such as ethyl vanillin, trace elements, volatile organic compounds (VOCs) like thujone, phenols, polycyclic aromatic hydrocarbons (PAHs), and heavy metals like chromium and lead may be present.4,5 It is also frequently enhanced with different flavorings and/or ethanol. 6
Although e-cigarettes were once promoted as a safe method to quit smoking conventional cigarettes, recent evidence continues to speculate that they may have numerous detrimental effects on the body, particularly on the cardiovascular and respiratory systems. 7 Research examining the effects of vaping on the nervous system includes investigations into the development of seizures. A seizure is defined as a transient, involuntary alteration of consciousness, behavior, motor activity, sensation, or autonomic function caused by an excessive rate and hypersynchrony of discharges from a group of cerebral neurons. 7
The utilization of e-cigarettes has raised concerns about their neurological implications, with seizures emerging as a significant consequence of this concern. Reports have highlighted instances of seizures occurring after exposure to nicotine-infused vape fluids or vapor. 8 This association between e-cigarette use and seizures is particularly alarming in individuals lacking a medical or familial seizure history, along with other risk factors. It may also exacerbate seizure frequency in those with pre-existing conditions. 9
Despite advancements in research, the exact mechanisms underlying e-cigarette-related seizures remain elusive. Emerging evidence suggests potential contributors, including nicotine toxicity, chronic exposure-induced neuroadaptations, and the neurotoxic effects of e-liquid components. However, debates persist regarding the timing of seizure presentations and the specific role of nicotine versus other constituents in e-cigarettes.
Despite progress in an attempt to understand the relationship, several challenges exist, such as the underreporting of cases and the reliance on self-reported data. Understanding the clinical relevance of e-cigarette-related seizures is crucial for public health in the areas of policy development and public awareness. By delving into the existing literature, examining potential mechanisms, and highlighting public health implications, we aim to contribute to a deeper understanding of this emerging issue and facilitate evidence-based interventions to safeguard neurological medicine.
Methodology
This is a narrative review that analyzes the role of e-cigarette use in the development and susceptibility of seizures. As e-cigarettes are a relatively new topic, the review includes only studies reviewed in the last twenty years (January 2004 to 2024) to provide a holistic perspective on e-cigarette usage, seizure development, and the existing controversies between them. Using keywords such as “e-cigarette/ electronic cigarette” “seizures and epilepsy” “Vaping-related seizures” “Seizure risk,” “Electronic nicotine delivery systems (ENDS)” “E-cigarette-related seizures” “Nicotine-induced convulsions,” the database searched included ScienceDirect, Medline, PubMed, and Google Scholar. To manage duplicate articles retrieved from multiple databases, duplicates were identified and removed using reference management software. Selected articles from reading the abstracts were those that were in English or French that could be analyzed with full paper and had sufficient contribution to the topics.
Neurological manifestations/associations in e-cigarette users
A few case reports have shed light on the clinical presentation of this condition and these reports unveil the severity of seizures and aim to characterize their adverse outcomes. Documented symptoms include tonic-clonic seizures associated with loss of consciousness (LOC), tongue biting, and urinary incontinence, which typically manifest abruptly within minutes to hours of vaping, with many reported cases occurring within 30 minutes of vaping.10 -12 These seizure episodes are generally brief, lasting less than 5 minutes, and are followed by a postictal state characterized by amnesia, confusion, and altered consciousness.10 -12 Seizures may occur at rest or during various activities, such as walking, climbing stairs, driving, or swimming in open water, leading to potentially life-threatening accidents. Complications resulting from falls have been reported and include scalp bruises, concussions, skull fractures, traumatic brain injury, and skeletal fractures. Seizure disorders can potentially lead to a cascade of psychosocial consequences for individuals. These consequences may include stigmatization, unemployment, and loss of driving privileges, which have all been reported in association with e-cigarette-related seizures. 13
There is a need for further investigation into the complexities of e-cigarette-associated seizures, as seizures have been reported among both new and experienced e-cigarette users. In some cases, the seizure started immediately after the first “puff,” while in others, it occurred after weeks of continuous use.12,13 Several individuals experienced recurrent seizures until vaping was discontinued. 12 A significant portion of these cases, approximately two-thirds, reported to the Food and Drug Administration’s (FDA) in the USA, involves youths and young adults, potentially reflecting the demographic distribution of e-cigarette users.12,13 Although research is ongoing to identify risk factors for e-cigarette use-associated seizures, many cases did not have documented preexisting conditions or comorbidities. However, among those cases where comorbidities were identified, the most common were psychiatric disorders such as depression, anxiety, and ADHD. A recent study found that the majority of users of ENDS were young adults aged 14 to 24 years, with 41% of this group reporting underlying medical conditions. Seizures were common, with 85% occurring within 24 hours of the last use and 62% occurring within 30 minutes. 12 Additionally, it was also reported that some individuals exhibited concurrent abuse of cocaine, alcohol, and marijuana. In contrast, others had a prior history of seizure disorders or were taking medications known to cause seizures such as tricyclic antidepressants. 12
Possible mechanism and existing controversies
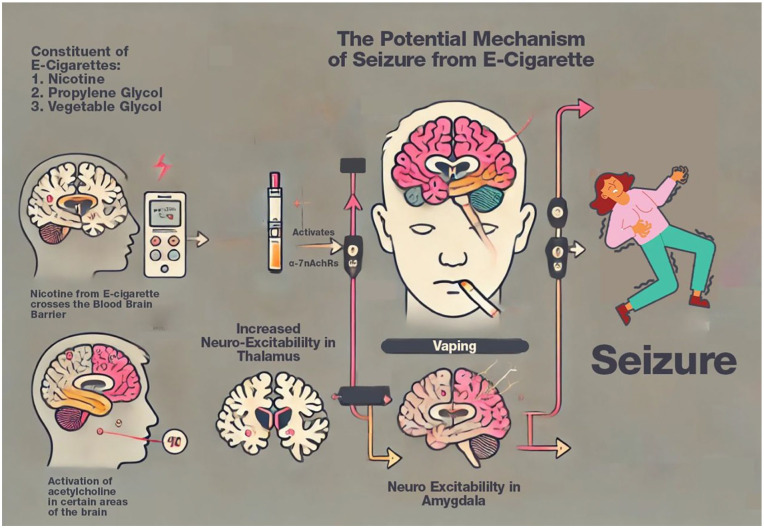
The mechanism underscoring how the use of e-cigarettes leads to seizures is still poorly understood. It is widely believed that nicotine toxicity can affect neuronal excitability and lower seizure thresholds. The inhalation of e-cigarette vapor results in nicotine, which rapidly crosses the blood-brain barrier and produces its euphoric effects by attaching to nicotinic acetylcholine receptors (nAChRs). 14 Nicotine acetylcholine receptors are then activated by a conformational change that opens the internal pore, allowing sodium and calcium ions to enter, 15 leading to glutamate release through the calcium-calmodulin cascades (see Figure 1). The nicotine acetylcholine receptors located in the neocortex, amygdala, hippocampus, and thalamus cause neuronal excitability by later activating the NMDA receptors and nitric oxide production. 16 The amygdala is already known for epileptogenesis and seizure generation, and it is most likely the medial amygdala.
Figure 1.
This diagram illustrates the potential mechanism of seizures caused by e-cigarette use. E-cigarettes contain nicotine, propylene glycol, and vegetable glycol and other substances, which play key roles in triggering adverse effects. Nicotine from e-cigarettes crosses the blood-brain barrier and activates α7-nicotinic acetylcholine receptors (α-7nAChRs) in the brain, specifically in regions like the thalamus and amygdala. This activation leads to increased neuro-excitability in these areas, which can contribute to seizure onset. Additionally, propylene glycol and vegetable glycol, 2 other key components of e-cigarettes, may further increase the risk of seizures. Propylene glycol is known to cause hyperosmolar metabolic acidosis at toxic levels, while the osmotic properties of vegetable glycol can lead to dehydration, both of which could exacerbate seizure risk.
Consequently, a spontaneous oscillation in the thalamocortical circuits leads to seizure presentation. Specifically, the alpha-7 subunits (α7) involved in seizure activation are usually expressed in the amygdala. While several studies report that nicotine’s convulsive effects are linked to α7-nAChRs, the specific subtypes of nACh receptors responsible for nicotine-induced seizures remain undefined. 17 Interestingly, in vitro models have reported that nicotine may have anticonvulsant effects by impairing seizure generation after repeated and chronic exposure to nAchR. 18 This effect is seen in Autosomal dominant sleep-related hypermotor (hyperkinetic) epilepsy (ADHSE), a rare epilepsy syndrome characterized by mutations in the gene that encodes the nAchR subunit. 19
E-cigarettes are known to have a variety of compositions, including concentrated mixtures of propylene glycol and vegetable glycol. Propylene glycol has the potential to cause serious adverse effects at various levels. PG has been reported to cause seizures and cause hyperosmolar metabolic acidosis at toxic levels.3,20 PG and its interactions with other chemical constituents may be likely to cause seizure induction in e-cigarettes. Moreover, the osmotic characteristics of VG may cause dehydration and, if severe enough could potentially trigger seizures. 3 Other substances in e-cigarettes such as cannabidiol, THC, and ethanol, may have additive or synergistic effects, further increasing the risk of seizures. 21
Prolonged exposure to nicotine causes an increase in the number of nAChR receptors in the brain. 22 This is achieved by changes in the way the receptors are assembled, transported, and broken down. The neuroadaptations occurring in neurotransmitter systems due to nicotine exposure are considered to directly contribute to nicotine addiction. These modifications may alter neuronal excitability, synaptic plasticity, and neurotransmitter release, thereby modulating seizure susceptibility. 22 The inhalation of vaporized flavorings and chemicals in e-liquids may have neurotoxic effects, leading to neuronal hyperexcitability and aberrant synaptic transmission. Studies have shown that flavored e-cigarettes produce aerosols that include reactive oxygen species (ROS), which contribute to the development of oxidative stress-induced damage in lung cells.23,24 Emerging empirical evidence indicates that oxidative stress may contribute to the underlying mechanisms of seizures, epilepsy, and epileptogenesis. 25 The excessive production of reactive oxygen species (ROS) during seizures results in lipid peroxidation (LPO), DNA damage, enzyme inhibition, and mitochondrial damage, eventually resulting in the death of neurons. 26
An individual’s vulnerability to vaping-induced seizures may be influenced by a combination of genetic predisposition, pre-existing neurological disorders, and environmental factors.27,28 Genetic polymorphisms in the genes responsible for ion channels, neurotransmitter receptors, and metabolic enzymes that are involved in the metabolism of nicotine and e-liquid may also affect the likelihood of developing seizures after using e-cigarettes. Genes such as SCN1A, SCN2A, and SCN1B encode voltage-gated sodium channels, while GABRA1, GABRB3, GABRG2 which encode subunits of the GABA-A receptor to mediate inhibitory neurotransmission can increase the risk of seizures and linked to various forms of epilepsy.29,30 Polymorphisms that alter channel function could predispose individuals to seizures, especially when exposed to stimulants like nicotine.
Existing controversies
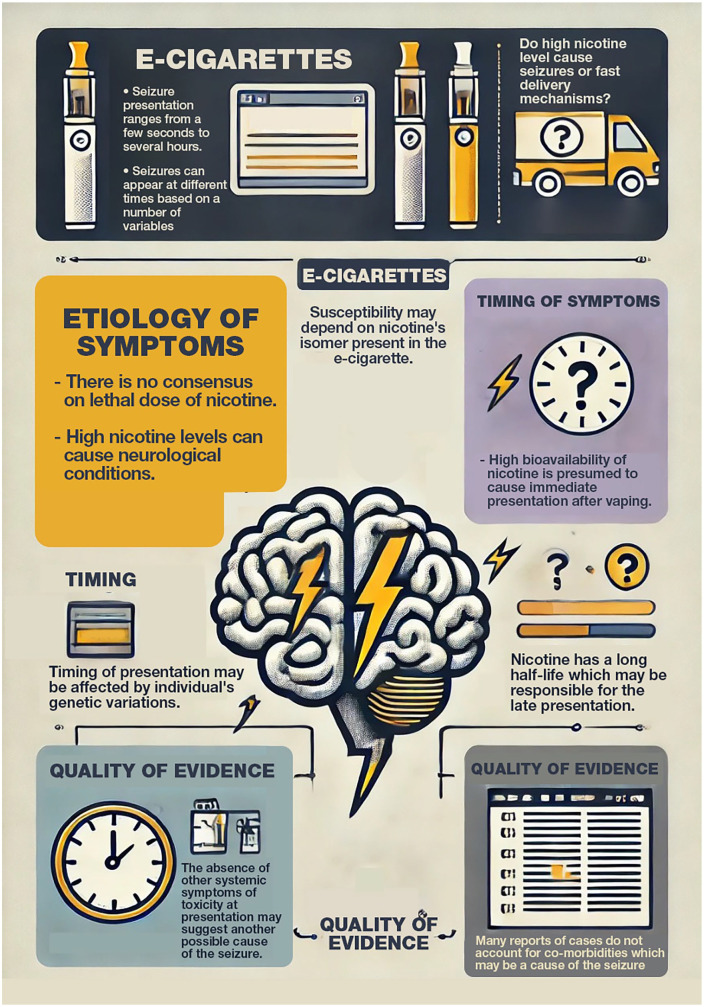
With the rising popularity of e-cigarettes amongst youths and adolescents, literature continues to evolve; however, it still presents a myriad of controversies ranging from the presentation timing, quality of reported data, and etiology of symptoms.
Etiology of symptoms
There is no general agreement on the lethal dose in adults, but it is estimated to range between 0.5 and 1 mg/kg of body weight. This estimated lethal dose refers to the amount of nicotine that could be potentially fatal if ingested as high nicotine levels can cause significant adverse side effects such as neurological complications. 31 However, the use of e-cigarettes, which are believed to have a similar or higher rapidity of delivery of nicotine than conventional cigarettes, 32 raises questions as to how these seemingly small amounts of nicotine can lead to toxic-level complications such as seizures. While it is generally unclear whether toxicity from e-cigarettes stems from higher nicotine concentrations or rapid delivery mechanisms, it is hypothesized that increased plasma concentration and higher bioavailability of nicotine, depending on the isomer of nicotine, make it faster to be absorbed into circulation, hence why its effects may be exaggerated.
Timing of presentation
Another leading question on its symptomatology surrounds the timing of presentations. Several case reports indicate varied times of presentation of seizures, from a few seconds after use to 30 minutes and several hours. It is envisaged that nicotine possesses increased bioavailability, which suggests the highest point activity of nicotine is immediately after use when brain levels are highest. 16 This makes the presentation of seizures immediately after the use of e-cigarettes plausible since its nicotine levels and brain activity are presumably still at their highest (see Figure 2).
Figure 2.
This figure outlines key factors related to seizures induced by e-cigarettes. The etiology of symptoms remains unclear, with no consensus on a lethal dose of nicotine. High nicotine levels may cause neurological conditions, and symptoms can vary based on nicotine’s isomer and genetic differences in users. The timing of seizure presentation can be immediate due to nicotine’s high bioavailability or delayed due to its long half-life. The quality of evidence is impacted by the absence of other symptoms and the failure to account for co-morbidities in many case reports.
However, nicotine metabolism and elimination half-life must also be considered. Nicotine is rapidly absorbed and reaches peak plasma concentration within minutes, but its effects can persist as it is metabolized into cotinine, which has a longer half-life. This ongoing presence of nicotine and its metabolites in the bloodstream could explain why seizures can occur several hours after vaping,
Additionally, variations in individual metabolism, genetic polymorphisms affecting nicotine metabolism, and the presence of other substances in e-cigarette liquids could influence the timing and severity of seizure presentations. Therefore, while the highest risk period for seizures may be immediately after vaping due to peak nicotine levels, the extended effects of nicotine and its metabolites can account for delayed presentations. This variability demonstrates the complexities of nicotine’s impact on the body and emphasizes the need for additional research to fully understand the timing and mechanisms of seizure presentations associated with e-cigarette use.
Quality of evidence
Furthermore, another ongoing curiosity among scholars is why, in cases where seizures were the only presentation, no other symptoms of potential toxicity from e-cigarette use were observed. Nicotine toxicity presents with neurological, cardiovascular, and respiratory complications, and it raises questions as to why seizures were the only presentations without accompanying systemic toxicity. This leads to further debate on the quality of reported seizures in existing literature (see Table 1). Could it be that the reported seizures were not seizures? To date, no study has described the causal link between e-cigarettes and seizures, and many of the existing data consists of self-reported data, making it unreliable. Since neurological complications of toxicity include tremors and muscle fasciculations, 33 it can be envisaged that the seizures were tremors.
Table 1.
Existing debates and controversies with e-cigarettes as a cause of seizures.
| Controversy | Description |
|---|---|
| Etiology of symptoms | There is consensus on the adverse effects of high nicotine levels, but questions remain about how e-cigarettes deliver nicotine rapidly and whether this leads to toxic-level complications like seizures. It is hypothesized that increased plasma concentration and higher bioavailability of nicotine contribute to the exaggerated effects. |
| Timing of presentation | Varied times of seizure presentation have been reported, ranging from immediately after e-cigarette use to several hours later. The immediate post-use presentation is plausible due to peak nicotine levels, but the existence of delayed seizures challenges this hypothesis. |
| Quality of evidence | Scholars question why seizures are the only reported toxicity of e-cigarette use, as nicotine toxicity typically presents with systemic symptoms. Doubts persist regarding the reliability of reported seizures, with some cases suggesting misdiagnosis or unreported concurrent conditions. Normal investigations in some cases contradict nicotine toxicity, raising further doubts. Individual susceptibility may also play a role in seizure presentation, suggesting the need for investigation into usage patterns and medical conditions. |
Many of these presentations also do not account for co-morbid or concurrent medical conditions. This was proven in a pediatric case report in which the patient vaped the entire contents of an e-cigarette cartridge and developed seizures soon after. 34 While nicotine toxicity was the initial diagnosis since it was consistent with patient symptoms, her toxicology profile revealed a severe diphenhydramine overdose, which was consistent with her symptoms. In this case, no nicotine or its metabolites were detected.
Delving deeper into nicotine toxicity as a likely cause of seizures, it is interesting to note that many of these case reports show normal investigations that do not support nicotine toxicity. It is expected that clinical findings such as pulmonary infiltrates on chest imaging, signs of oxidative stress, cardiovascular effects like impaired vascular flow and high blood pressure, and immune effects are present along with seizures. 35 One theory that could be investigated is that smokers’ susceptibility to e-cigarette-induced seizures differs. Case reports suggesting e-cigarette-induced seizures revealed only a small fraction of people who take e-cigarettes. This brings up the notion that individual susceptibility plays a role in seizure presentation. Differences in the frequency of usage, patterns, synergistic interaction with other drugs, and concurrent medical conditions may contribute to differences in how seizures present. Ultimately, investigating these factors could play a role in understanding individual susceptibility.
Clinical relevance and management protocol of selected case reports
A study by Harden et al, 36 highlights a crucial link between seizures and the quality of life in epilepsy patients, a relationship that persists even when considering the impact of depression. Severe recurring seizures can lead to increased worry, anxiety, and avoidance behaviors, ultimately affecting patients’ independence and daily functioning. 36 Seizure clusters may result in increased emergency room visits and hospitalization, thus negatively impacting and disrupting other daily activities such as work and studies. 37 Also, the influence of seizures on quality of life may likely be due to the physical dangers posed by severe seizures, as well as concerns about future episodes and potential side effects of medications. 36
Seizures are accompanied by psychosocial challenges that can profoundly impair the quality of life of vapers. 38 Research has consistently shown that as seizure severity increases, health-related quality-of-life scores decrease, highlighting the pervasive impact of epilepsy on well-being. 39 Even patients with infrequent seizures, typically considered to have good control, experience compromised quality of life compared to those who are seizure-free. 38
Furthermore, the connection between feelings of stigma and medication side effects adds another layer to the clinical picture. Stigma related to seizures can impact patients’ self-esteem and well-being, albeit not conclusively supported by all findings. There is a substantial impact of seizures on patients’ psychological well-being. 39 Studies like this consistently highlight the substantial impact of seizure activity on patients’ psychological well-being. This is reflected in measurements using scales like the HAD Scale, indicating a clear relationship between seizure activity levels and patients’ emotional health. 40
Multiple episodes of seizures lower the seizure threshold in a person, increasing the likelihood of experiencing status epilepticus, a potentially life-threatening seizure event. Recurring seizure episodes may trigger a malignant epilepsy syndrome, which may also be accompanied by gradual cognitive impairment and resistance to anticonvulsant drugs. 41 Many variables, including a causal etiology like vaping, may combine to affect how an epileptic seizure develops. Additionally, there is a heightened risk of seizure-related injuries such as falls, head injuries, fractures, and other physical traumas. 37
Ultimately, these findings underscore the critical importance of addressing seizure severity in the clinical management of seizures due to vaping. The impact of seizures on various aspects of patient’s lives, from social functioning to mental well-being, can guide clinicians in developing comprehensive treatment plans aimed at improving the overall quality of life for the population.
While a definitive consensus or guideline for the assessment and treatment of seizures resulting from e-cigarette use remains lacking, several case reports indicate a consistent management protocol for such cases. This alignment could potentially stem from the wealth of literature available on the management of seizures and epilepsy.42 -45
It is conceivable that a general approach to history-taking and seizure evaluation was employed, which might not necessitate detailed reporting. However, the prevalent comorbidity noted across these cases was the presence of mental disorders such as depression, eating disorders, and ADHD.9,10,46,47 For the examinations conducted, the case reports primarily centered on the findings of neurological examinations, all of which yielded unremarkable results. Notable features of the seizures, as documented in these cases, included generalized tonic-clonic seizures, 10 often followed by a typical post-ictal state without accompanying neurological manifestations. Some individuals additionally described experiencing visual auras and anxiety attacks.9,48 The duration of these seizures typically lasted under 2 minutes, occurring within minutes to several hours after vaping.
The management of seizures resulting from vaping has been the subject of various case reports, each revealing a recurring pattern in investigative approaches. In a study by Liu and McIntosh, 46 2 cases of vaping-associated seizures were documented, involving a 17-year-old and a female patient. The investigations conducted included a urine drug screen, electroencephalogram (EEG), brain MRI without contrast, and electrocardiography (ECG). Additionally, the female patient underwent a urine hCG test to rule out pregnancy, mirroring the approach seen in a study by Liu-Zarzuela and Sun. 10 Their report of multiple seizure episodes included a comprehensive evaluation with a drug screen, head CT scan without contrast, brain MRI, EEG, and ECG, with the addition of transesophageal echocardiography (TTE).
A different but similarly thorough assessment was described in the case of the 16-year-old female with a history of generalized epilepsy. Here, an epilepsy panel was incorporated alongside the aforementioned investigations from other case reports. It is important to highlight that all investigations yielded unremarkable results across these cases (see Supplementary Figure 1 for detailed breakdowns of other cases). Notably, despite a history of vaping before the seizure events and hospital presentation, urine drug tests were consistently negative. This underscores the complexity of diagnosing and managing seizures associated with vaping, urging further investigation into the mechanisms underlying these events.
To date, no studies or trials have specifically investigated pharmacological and non-pharmacological treatments for seizures associated with e-cigarette use. However, many reports draw treatment inferences from the established knowledge of seizures related to other causes, such as epilepsy.42 -45 In a case report detailing 2 cases, 10 no pharmacological intervention or antiepileptic drugs were prescribed. This decision may have been influenced by the absence of any identifiable pathological cause, the recording of a single seizure episode, and the unremarkable results of investigations.
Conversely, 3 separate case reports documented the administration of levetiracetam to patients experiencing seizures following e-cigarette use.9,10,47 Levetiracetam is an anti-epileptic drugs that involves modulatuing neurotransmitter release making its frequent use in seizure management. 49
Interestingly, a recurring pattern of seizure episodes persisted in some individuals until they discontinued vaping entirely. 10 Additionally, in the case of a 16-year-old female with a history of epilepsy, her medication regimen was modified from Levetiracetam, Zonisamide, and Ethosuximide to Lamotrigine. Lamotrigine is involved in modulating activity of voltage-gated ion channels as well as its neuro-protective effects. 50 Despite 7 months free of seizures and vaping, the seizures returned upon resuming e-cigarette use. It is possible that Levetiracetam was preferred in the reported cases due to its broad-spectrum efficacy and favorable side effect profile, which makes it suitable for managing various seizure types, including those potentially triggered by the neurotoxic effects of nicotine.
The management protocol for seizures associated with vaping remains multifaceted and largely reliant on the existing knowledge of seizures, particularly those stemming from epilepsy. There are no general guidelines or consensus on the approach toward the evaluation and management of patients with seizures as a result of e-cigarettes.
In clinical practice, it is also essential for physicians to consider the assessment of pre-existing psychiatric conditions when evaluating patients, as the treatment of these conditions with certain pharmacological agents can potentially induce seizures. Clinical complications resulting from the treatment of psychiatric disorders are well-documented. For instance, paroxetine, used in treating social anxiety disorder, has been associated with hair loss. 51 Additionally, isotretinoin has been reported to induce psychotic mania, 52 and bupropion intoxication has led to acute dystonia following epileptic seizures. 53
While these cases may not directly diagnose e-cigarette-induced seizures, they underscore the importance of a thorough differential diagnosis. By ruling out psychiatric conditions and their treatments as potential causes, physicians can more accurately attribute seizures to e-cigarette use, thereby contributing to a diagnosis of exclusion. This comprehensive assessment approach ensures a more precise identification of e-cigarette-induced seizures, emphasizing the need for vigilance in monitoring the neurological effects of both psychiatric treatments and e-cigarette usage.
Public health directions
The implications for public health are profound, particularly given the rise in e-cigarette use among young people. Vaping products are widely marketed as smoking cessation aids and are prominently displayed in various retail settings in countries like the UK, the US, and many others. The extensive marketing and advocacy through various channels, such as social media, broadens exposure to e-cigarette products. The accessibility to these products puts young people, especially children and adolescents, at risk of being introduced to e-cigarettes. The acute toxicity associated with e-cigarettes and their recent link to seizures raises concerns, highlighting the need for urgent policies to protect young individuals from the adverse effects of these products.
FDA’s actions, such as the marketing denial orders issued to JUUL Lab Inc. in 2022 (which were later rescinded), reflect the need to address these concerns in various countries. The FDA of the USA is currently compiling data and reports on seizures associated with vaping. According to publicly available information, there have been 129 reported cases from 2010 to 2019. 54 As of March 2021, more than 250 reports of e-cigarette-associated seizures have been documented, further underscoring the need for awareness and intervention. 13 Such interventions should be targeted at young people and adolescents who are known to be primary users of the product while ensuring that all perspectives on the consequent use of e-cigarettes are properly demonstrated. This should include targeted educational campaigns and engagement with community members and healthcare providers to enhance prevention and intervention measures. The educational campaigns should focus on informing young people about the potential neurological risks associated with e-cigarette use, including seizures, and the long-term implications, such as addiction.
There is evidence that those who use e-cigarettes and have seizures have an increased risk of developing spontaneous or neurologically triggered epilepsy. Several variables, including a causal etiology like vaping, may combine to affect how an epileptic seizure develops. Anticonvulsant medication does not seem to affect the long-term prognosis in terms of short-term seizure suppression. Recurring seizure episodes following vaping may trigger a malignant epilepsy syndrome, which may also be accompanied by gradual cognitive impairment and resistance to anticonvulsant drugs. 41
To control the use of e-cigarettes, debates around e-cigarette regulation have intensified. While some advocate for complete bans on e-cigarette sales to curb youth usage, others argue for a nuanced approach. Banning sales in gas stations and convenience stores while allowing them in specialty tobacco and vape shops is proposed as a balanced strategy. 47 Regulatory agencies such as the FDA should conduct and disseminate the latest research on vaping, which shows that nicotine used in vaping devices has potential to cause seizures, may be harmful to attention, learning, and memory in young people, and that people who vape may be more susceptible to long term addiction. Policymakers and other interested parties should be informed about these facts for informed evidence-based decision-making and public and mental health education efforts. It is also essential that manufacturers of ENDS are held to a stricter transparency standards. Regulatory bodies should impose measures such as clearer labeling of e-cigarettes components to ensure proper information on health risks as well as more rigorous testing to identify and quantify chemical constituents while also minimizing the potential for harmful additive effects of various ingredients.
To highlight the importance of addressing psychological sequelae in patients with seizures, it is imperative to draw parallels with other medical conditions where psychological impacts are well-documented. Evidence shows that psychological sequelae are significant in various health conditions, such as contact dermatitis, resistant epilepsy, acne vulgaris, and beta-thalassemia. For example, contact dermatitis can lead to social appearance anxiety, 55 while resistant epilepsy has been linked to heightened psychological distress due to its chronic and debilitating nature. 56 Similarly, patients with acne vulgaris often experience social appearance anxiety, 55 and those with beta-thalassemia major suffer from anxiety and depression. 57
Applying these findings to patients with seizures suggests that the psychological burden can be considerable, necessitating comprehensive management strategies that address both the physical and mental health aspects of the condition. This holistic approach ensures that patients receive the necessary support to improve their overall quality of life.
Policymakers and other stakeholders should be informed about these facts for evidence-based decision-making and public health education efforts. Specifically, policies could include:
Restrictions on e-cigarette marketing and sales to minors.
Implementation of warning labels on e-cigarette products highlights the risk of seizures and other neurological effects.
Development of school-based educational programs to inform students about the risks of e-cigarette use.
Establishment of support services for young people looking to quit vaping.
Enhanced surveillance and reporting systems to monitor adverse effects related to e-cigarette use.
These targeted efforts would help to mitigate the public health risks associated with e-cigarette use and protect young individuals from its harmful effects.
Limitations of study
This narrative review has several strengths: it provides a comprehensive review of the current state of knowledge using recent research findings, case reports, and epidemiological data. Moreover, we adopt a multi-faceted approach by delving into both clinical aspects and the public health implications of these health concerns while identifying research gaps in e-cigarette-associated seizures.
A foremost limitation is that many cases are unreported/underreported, potentially skewing the data towards more severe cases that warrant medical attention, and cases from geographical locations with access to healthcare services. Consequently, our study may not fully capture the spectrum of seizure activity related to e-cigarette use, limiting our ability to make definitive conclusions about its prevalence and characteristics. Furthermore, the reliance on case reports and self-reported data for identifying seizure incidents linked to e-cigarette usage may be inherently prone to biases, including recall bias and reporting bias. Individuals may not accurately remember or choose to report all relevant details about their e-cigarette use, seizure episodes, and any associated factors. Given the objectives and large scope of this review, it is not viable to undertake it using a structured methodological approach (ie, systematic or review).
Conclusion
Our study revealed a range of neurological symptoms, including sudden tonic-clonic seizures, tongue biting, and urinary incontinence linked to e-cigarette use, highlighting the potential dangers of neurotoxic substances like propylene glycol and nicotine in e-liquids. These ingredients may disrupt neuronal function and increase seizure risk, pointing to the necessity of further research to understand their interactions with the brain. Additionally, the significant use of e-cigarettes among young people also brings to the fore an urgent need for effective public health policies and regulations to address this growing concern.
Building on the insights gathered by our study, some recommendations will potentially address the identified limitations and pave the way for increased opportunities for enhanced safety of e-cigarette use. To address the challenge of underreporting and to better understand the prevalence of e-cigarette-associated seizures, there is an urgent need to enhance existing FDA reporting systems for adverse events. Healthcare professionals should be encouraged to report cases through these established channels, thereby strengthening the national reporting network. The development and dissemination of comprehensive clinical guidelines for the management of e-cigarette-associated seizures are also crucial. These guidelines should outline best practices for the evaluation, classification, diagnosis, and treatment of individuals presenting with seizures potentially linked to e-cigarette use. They should also address the management of e-cigarette use in individuals with pre-existing seizure disorders. This would make findings such as clinical management outcomes more consistent, robust, and comparable across studies. Specifically, the diagnostic guidelines should review a seizure-vaping specific history, which would include details of the seizure episodes, including (date and time of occurrence, activities before the seizure, including vaping, description of the seizure from the patient, and, if possible, from witnesses, duration of the seizure, frequency of seizures, recovery period, and any postictal symptoms), and investigation of patterns or triggers noticed by the patient, including association with vaping.
Ultimately, a multidisciplinary approach culminating in clinical vigilance, policy regulatory action, and public health awareness is imperative to address the association between e-cigarette use and seizure susceptibility, thereby safeguarding both individual well-being and public health. Longitudinal studies are also needed to establish causal and temporal relationships between seizures and e-cigarette usage as users will be monitored over time to assess the incidence of seizures, to account for bias and confounding influences, and to take into account changes in e-cigarette use patterns or devices.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_29768357241304298 for Seizure Susceptibility in E-cigarette Users: Navigating the Clinical Management and Public Health Considerations by Soyemi Toluwalashe, Olusola Aremu, Olabode Ekerin, Abdulqudus Lawal, Faniyi Oluwatobi, Victor Adebayo, Adewunmi Akingbola, Simon Olaniyan, Agboola Progress and Abdullahi Tunde Aborode in Substance Use: Research and Treatment
Footnotes
Author Contributions: T. S: Study concept, literature review, writing manuscript, reviewing and editing. O.E: Literature review, writing manuscript, reviewing and editing. V.A: Writing manuscript, literature review, reviewing O.A: Writing manuscript, literature review, reviewing A.L: Writing manuscript, literature review, reviewing S.O: Writing manuscript, literature review, reviewing, A.A: Writing manuscript, literature review, reviewing. O.F: Writing manuscript, literature review, reviewing. P.A and A.A: Reviewing final draft.
Author’s Note: Olabode Ekerin is also affiliated to College of Education and Human Sciences, University of Nebraska-Lincoln, Nebraska, USA.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Soyemi Toluwalashe  https://orcid.org/0000-0003-0615-3190
https://orcid.org/0000-0003-0615-3190
Availability of Data and Materials: All data sources are from publicly available literature and can be accessed through their respective citations.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Farsalinos KE, Poulas K, Voudris V, Le Houezec J. Prevalence and correlates of current daily use of electronic cigarettes in the European Union: analysis of the 2014 Eurobarometer survey. Intern Emerg Med. 2017;12:757-763. doi: 10.1007/s11739-017-1643-7 [DOI] [PubMed] [Google Scholar]
- 2. Indriani RC, Aulia F, Sianturi PA, et al. The phenomenon of vaping in female students. Indones J Med Anthropol. 2023;4(2):44-49. doi: 10.32734/ijma.v4i2.12282 [DOI] [Google Scholar]
- 3. Maessen GC, Wijnhoven AM, Neijzen RL, et al. Nicotine intoxication by e-cigarette liquids: a study of case reports and pathophysiology. Clin Toxicol. 2020;58:1-8. doi: 10.1080/15563650.2019.1636994 [DOI] [PubMed] [Google Scholar]
- 4. Hahn J, Monakhova YB, Hengen J, et al. Electronic cigarettes: overview of chemical composition and exposure estimation. Tob Induc Dis. 2014;12:23. doi: 10.1186/s12971-014-0023-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kulhánek A, Baptistová A. Chemical composition of electronic cigarette e-liquids: overview of current evidence of toxicity. Addictology/Adiktologie. 2020;20:137. doi: 10.35198/01-2020-002-0007 [DOI] [Google Scholar]
- 6. Hammond D, Rynard VL, Reid JL. Changes in prevalence of vaping among youths in the United States, Canada, and England from 2017 to 2019. JAMA Pediatr. 2020;174:797-800. doi: 10.1001/jamapediatrics.2020.0901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Friedman MJ, Sharieff GQ. Seizures in children. Pediatr Clin North Am. 2006;53:257-277. doi: 10.1016/j.pcl.2005.09.010 [DOI] [PubMed] [Google Scholar]
- 8. Tehrani H, Rajabi A, Ghelichi-Ghojogh M, Nejatian M, Jafari A. The prevalence of electronic cigarettes vaping globally: a systematic review and meta-analysis. Arch Public Health. 2022;80:240. doi: 10.1186/s13690-022-00998-w [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9. Tatum PS, Oster JM. Seizures and vaping—a report of two cases. Mil Med. 2023;188:e1307-e1309. doi: 10.1093/milmed/usab270 [DOI] [PubMed] [Google Scholar]
- 10. Liu-Zarzuela JA, Sun R. Three seizures provoked by e-cigarette use in a five-year period: a case report. Cureus. 2022;14:e27616. doi: 10.7759/cureus.27616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vaping and seizure risk: a case report (1814). Neurology. 2020. Accessed May 2, 2024. https://n.neurology.org/content/94/15_Supplement/1814
- 12. Faulcon LM, Rudy S, Limpert J, Wang B, Murphy I. Adverse experience reports of seizures in youth and young adult electronic nicotine delivery systems users. J Adolesc Health. 2020;66:15-17. doi: 10.1016/j.jadohealth.2019.10.002 [DOI] [PubMed] [Google Scholar]
- 13. Weidner AS, Imoisili O, Rudy S. E-cigarette-associated seizure reports to food and drug administration lack medical information. Ann Emerg Med. 2021;78:802-803. doi: 10.1016/j.annemergmed.2021.08.001 [DOI] [PubMed] [Google Scholar]
- 14. Brunzell DH, Stafford AM, Dixon CI. Nicotinic receptor contributions to smoking: insights from human studies and animal models. Curr Addict Rep. 2015;2:33-46. doi: 10.1007/s40429-015-0042-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Feduccia AA, Chatterjee S, Bartlett SE. Neuronal nicotinic acetylcholine receptors: neuroplastic changes underlying alcohol and nicotine addictions. Front Mol Neurosci. 2012;5:83. doi: 10.3389/fnmol.2012.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shao XM, Fang ZT. Severe acute toxicity of inhaled nicotine and e-cigarettes: seizures and cardiac arrhythmia. Chest. 2020;157:506-508. doi: 10.1016/j.chest.2019.10.008 [DOI] [PubMed] [Google Scholar]
- 17. Iha HA, Kunisawa N, Shimizu S, et al. Nicotine elicits convulsive seizures by activating amygdalar neurons. Front Pharmacol. 2017;8:57. doi: 10.3389/fphar.2017.00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Becchetti A, Aracri P, Meneghini S, Brusco S, Amadeo A. The role of nicotinic acetylcholine receptors in autosomal dominant nocturnal frontal lobe epilepsy. Front Physiol. 2015;6:22. doi: 10.3389/fphys.2015.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Narrett JA, Khan W, Funaro MC, Moeller JJ. How do smoking, vaping, and nicotine affect people with epilepsy and seizures? A scoping review protocol. PLoS One. 2023;18:e0288120. doi: 10.1371/journal.pone.0288120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zar T, Graeber C, Perazella MA. Recognition, treatment, and prevention of propylene glycol toxicity. Semin Dial. 2007;20:217-219. doi: 10.1111/j.1525-139X.2007.00280.x [DOI] [PubMed] [Google Scholar]
- 21. Krishnasamy VP, Hallowell BD, Ko JY, et al. Update: characteristics of a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury - United States, August 2019-January 2020. MMWR Morb Mortal Wkly Rep. 2020;69:90-94. doi: 10.15585/mmwr.mm6903e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holliday ED, Nucero P, Kutlu MG, et al. Long-term effects of chronic nicotine on emotional and cognitive behaviors and hippocampus cell morphology in mice: comparisons of adult and adolescent nicotine exposure. Eur J Neurosci. 2016;44:2818-2828. doi: 10.1111/ejn.13398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yogeswaran S, Muthumalage T, Rahman I. Comparative reactive oxygen species (ROS) content among various flavored disposable vape bars, including cool (iced) flavored bars. Toxics. 2021;9:235. doi: 10.3390/toxics9100235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Anderson C, Majeste A, Hanus J, Wang S. E-cigarette aerosol exposure induces reactive oxygen species, DNA damage, and cell death in vascular endothelial cells. Toxicol Sci. 2016;154:332-340. doi: 10.1093/toxsci/kfw166 [DOI] [PubMed] [Google Scholar]
- 25. Shekh-Ahmad T, Kovac S, Abramov AY, Walker MC. Reactive oxygen species in status epilepticus. Epilepsy Behav. 2019;101(Pt B):106410. doi: 10.1016/j.yebeh.2019.07.011 [DOI] [PubMed] [Google Scholar]
- 26. Łukawski K, Czuczwar SJ. Oxidative stress and neurodegeneration in animal models of seizures and epilepsy. Antioxidants (Basel). 2023;12:1049. doi: 10.3390/antiox12051049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ottman R, Annegers JF, Risch N, Hauser WA, Susser M. Relations of genetic and environmental factors in the etiology of epilepsy. Ann Neurol. 1996;39:442-449. doi: 10.1002/ana.410390406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Esteban-Lopez M, Perry MD, Garbinski LD, et al. Health effects and known pathology associated with the use of E-cigarettes. Toxicol Rep. 2022;9:1357-1368. doi: 10.1016/j.toxrep.2022.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ademuwagun IA, Rotimi SO, Syrbe S, Ajamma YU, Adebiyi E. Voltage gated sodium channel genes in epilepsy: mutations, functional studies, and treatment dimensions. Front Neurol. 2021;12:600050. doi: 10.3389/fneur.2021.600050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Feng Y, Wei ZH, Liu C, et al. Genetic variations in GABA metabolism and epilepsy. Seizure. 2022;101:22-29. doi: 10.1016/j.seizure.2022.07.007 [DOI] [PubMed] [Google Scholar]
- 31. Nelson LS, Goldfrank LR. Goldfrank’s toxicologic emergencies. 2019. https://lccn.loc.gov/2009049183
- 32. Solingapuram Sai KK, Zuo Y, Rose JE, et al. Rapid brain nicotine uptake from electronic cigarettes. J Nucl Med. 2020;61:928-930. doi: 10.2967/jnumed.119.230748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Scarpino M, Rosso T, Lanzo G, et al. Severe neurological nicotine intoxication by e-cigarette liquids: systematic literature review. Acta Neurol Scand. 2021;143:121-130. doi: 10.1111/ane.13338 [DOI] [PubMed] [Google Scholar]
- 34. Hughes A, Hendrickson RG. Does vaping cause seizures? The need for comprehensive drug testing. Clin Toxicol. 2020;58:217-218. doi: 10.1080/15563650.2019.1618468 [DOI] [PubMed] [Google Scholar]
- 35. Overbeek DL, Kass AP, Chiel LE, Boyer EW, Casey AMH. A review of toxic effects of electronic cigarettes/vaping in adolescents and young adults. Crit Rev Toxicol. 2020;50:531-538. doi: 10.1080/10408444.2020.1794443 [DOI] [PubMed] [Google Scholar]
- 36. Harden CL, Maroof DA, Nikolov B, et al. The effect of seizure severity on quality of life in epilepsy. Epilepsy Behav. 2007;11:208-211. doi: 10.1016/j.yebeh.2007.05.002 [DOI] [PubMed] [Google Scholar]
- 37. Jafarpour S, Hirsch LJ, Gaínza-Lein M, Kellinghaus C, Detyniecki K. Seizure cluster: definition, prevalence, consequences, and management. Seizure. 2019;68:9-15. doi: 10.1016/j.seizure.2018.05.013 [DOI] [PubMed] [Google Scholar]
- 38. Fawale M, Owolabi M, Ogunniyi A. Effects of seizure severity and seizure freedom on the health-related quality of life of an African population of people with epilepsy. Epilepsy Behav. 2014;32:9-14. doi: 10.1016/j.yebeh.2013.12.026 [DOI] [PubMed] [Google Scholar]
- 39. Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurol. 2005;4:171-178. doi: 10.1016/S1474-4422(05)01014-8 [DOI] [PubMed] [Google Scholar]
- 40. Jacoby A, Baker GA, Steen N, Potts P, Chadwick DW. The clinical course of epilepsy and its psychosocial correlates: findings from a U.K. Community study. Epilepsia. 1996;37:148-161. doi: 10.1111/j.1528-1157.1996.tb00006.x [DOI] [PubMed] [Google Scholar]
- 41. Blume WT. The progression of epilepsy. Epilepsia. 2006;47:71-78. doi: 10.1111/j.1528-1167.2006.00665.x [DOI] [PubMed] [Google Scholar]
- 42. Liu G, Slater N, Perkins A. Epilepsy: treatment options. Am Fam Physician. 2017;96:87-96. Accessed August 4, 2024. https://www.ncbi.nlm.nih.gov/pubmed/28762701 [PubMed] [Google Scholar]
- 43. Chaplin S. Updated guideline on diagnosing and managing epilepsies. Prescriber. 2022;33:28-30. Accessed August 4, 2024. doi: 10.1002/psb.2010 [DOI] [Google Scholar]
- 44. García Morales I, Fernández Alonso C, Behzadi Koochani N, et al. Emergency management of epileptic seizures: a consensus statement. Emergencias. 2020;32:353-362. Accessed August 4, 2024. https://www.ncbi.nlm.nih.gov/pubmed/33006837 [PubMed] [Google Scholar]
- 45. Bank AM, Bazil CW. Emergency management of epilepsy and seizures. Semin Neurol. 2019;39:73-81. doi: 10.1055/s-0038-1677008 [DOI] [PubMed] [Google Scholar]
- 46. Liu EN, McIntosh A. First seizure in adolescent immediately following E-cigarette use: two patient cases. Neurol Clin Neurosci. 2020;8:158-159. doi: 10.1111/ncn3.12371 [DOI] [Google Scholar]
- 47. Benowitz NL. Seizures after vaping nicotine in youth: a canary or a red herring? J Adolesc Health. 2020;66:1-2. doi: 10.1016/j.jadohealth.2019.10.016 [DOI] [PubMed] [Google Scholar]
- 48. Wharton JD, Kozek LK, Carson RP. Increased seizure frequency temporally related to vaping: where there’s vapor, there’s seizures? Pediatr Neurol. 2020;104:66-67. doi: 10.1016/j.pediatrneurol.2019.10.006 [DOI] [PubMed] [Google Scholar]
- 49. Surges R, Volynski KE, Walker MC. Is levetiracetam different from other antiepileptic drugs? Levetiracetam and its cellular mechanism of action in epilepsy revisited. Ther Adv Neurol Disord. 2008;1:13-24. doi: 10.1177/1756285608094212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Costa B, Vale N. Understanding lamotrigine’s role in the CNS and possible future evolution. Int J Mol Sci. 2023;24:6050. doi: 10.3390/ijms24076050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kurhan F, Kamış GZ. Hair loss associated with paroxetine use: a case report. Turk Psikiyatri Derg. 2021;32:61-64. doi: 10.5080/u24955 [DOI] [PubMed] [Google Scholar]
- 52. Kurhan F, Kamiş GZ. Isotretinoin induced psychotic mania: a case report. Turk Psikiyatri Derg. 2021;32:214-218. doi: 10.5080/u25066 [DOI] [PubMed] [Google Scholar]
- 53. Kurhan F, Kamış GZ, Çim EFA. Acute dystonia following epileptic seizure after bupropion intoxication. Neurol Sci. 2021;42:4381-4386. doi: 10.1007/s10072-021-05139-9 [DOI] [PubMed] [Google Scholar]
- 54. Office of the Commissioner. FDA In Brief: FDA encourages continued submission of reports related to seizures following e-cigarette use as part of agency’s ongoing scientific investigation of potential safety issue. U.S. Food and Drug Administration. Published December 20, 2019. Accessed May 3, 2024. https://www.fda.gov/news-events/fda-brief/fda-brief-fda-encourages-continued-submission-reports-related-seizures-following-e-cigarette-use
- 55. Kurhan F. Social appearance anxiety in patients with contact dermatitis. East J Med. 2021;26:589-594. doi: 10.5505/ejm.2021.52280 [DOI] [Google Scholar]
- 56. Yilgör A, Kurhan F. Is childhood trauma a risk factor for resistant epilepsy? J Interpers Violence. 2024;39:1228-1244. doi: 10.1177/08862605231203964 [DOI] [PubMed] [Google Scholar]
- 57. Yengil E, Acipayam C, Kokacya MH, Kurhan F, Oktay G, Ozer C. Anxiety, depression and quality of life in patients with beta thalassemia major and their caregivers. Int J Clin Exp Med. 2014;7:2165-2172. Accessed August 4, 2024. https://www.ncbi.nlm.nih.gov/pubmed/25232402 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_29768357241304298 for Seizure Susceptibility in E-cigarette Users: Navigating the Clinical Management and Public Health Considerations by Soyemi Toluwalashe, Olusola Aremu, Olabode Ekerin, Abdulqudus Lawal, Faniyi Oluwatobi, Victor Adebayo, Adewunmi Akingbola, Simon Olaniyan, Agboola Progress and Abdullahi Tunde Aborode in Substance Use: Research and Treatment