Abstract
Objective:
Examination of the impact of the COVID-19 pandemic on rates of antipsychotic medication use, initiation and discontinuation, among newly admitted long-term care residents.
Design:
Repeated cross-sectional study.
Settings and Participants:
Long-term care home residents in Alberta, British Columbia and Ontario, Canada assessed with the Minimum Data Set (MDS) 2.0 assessment. The cohort was segmented according to admission during the pandemic (March 2020/2021) and 2 pre-pandemic (March 2018/2019 and March 2019/2020) periods.
Methods:
Multivariable logistic regression models were fit to characterize the association between long-term care admission during the COVID-19 pandemic and the use of antipsychotic medications. A second set of logistic regression models were fit among residents with follow-up assessments to characterize the association between long-term care admission and antipsychotic initiation/discontinuation at follow-up. All models were adjusted for resident characteristics including sex, age group, Aggressive Behaviour Scale score, Cognitive Performance Scale score, and diagnoses of Alzheimer’s disease and related dementias, anxiety disorder, depression, and bipolar disorder.
Results:
21 612 residents admitted during the pandemic and over 30 000 in each pre-pandemic period were included. Antipsychotic use increased during the pandemic period among newly admitted residents from both community (adjusted odds ratio [aOR] 1.20-1.29) and hospital settings (aOR 1.21-1.23). Residents admitted during the pandemic period were more likely to have antipsychotic medications initiated (aOR 1.25-1.26) and less likely to have had them discontinued (aOR 0.74-0.76) at the time of follow-up assessment.
Conclusion and Implications:
Multiple factors contributed to the observed increase in antipsychotic medication use among newly admitted long-term care home residents during the COVID-19 pandemic: increased medication use at the time of admission, increased medication initiation at follow-up, and decreased medication discontinuation at follow-up. A whole-systems approach that extends beyond long-term care into hospital and community settings is necessary to address this prevalent issue.
Keywords: COVID-19, long-term care, antipsychotic medications, measurement, quality of care
Brief summary
Examination of antipsychotic use among newly admitted long-term care residents revealed an increase in use at admission during the COVID-19 pandemic, with higher initiation and lower discontinuation rates within the first 3 months of stay.
Introduction
The COVID-19 pandemic had a profound impact on the health and well-being of long-term care home residents in Canada and worldwide. In addition to high rates of resident infection and mortality, 1 performance on some quality of care indicators worsened during the pandemic period.2,3 This includes an increase in the use of antipsychotic medications to manage symptoms of dementia, particularly responsive behaviours that are used to communicate needs and concerns.2 -5 This trend has been noted in other jurisdictions.6 -9
Antipsychotic medications are associated with a greater risk of falls, 10 stroke, 11 and all-cause mortality in persons living with dementia.12,13 Choosing Wisely Canada, a national initiative to reduce overprescribing and unnecessary diagnostic testing, advises against their use as the first choice for treating symptoms of dementia. 14 Encouragingly, the risk of receiving an antipsychotic medication in long-term care has decreased significantly over the past decade in Canada.15 -17 For example, in Ontario, 25% of residents received these medications in 2019 compared to 31% in 2010. 15
The Canadian Institute for Health Information’s (CIHI) quality indicator for inappropriate antipsychotic medications measures use among long-term care residents without a diagnosis of psychosis. 18 Residents with schizophrenia, Huntington’s disease, hallucinations, delusions, or end-stage disease (ie, estimated survival of less than 6 months) are excluded from the indicator. 19 Newly admitted residents are also excluded from the indicator. This allows 3 months to evaluate resident medication needs before inclusion in the denominator of the publicly reported rate. This is particularly important for persons living with dementia waiting in hospital to access long-term care because antipsychotic medication use is prevalent in hospital settings. 20
Antipsychotic use increased in hospitals during the initial wave of the pandemic. 21 Thus, we questioned whether worse performance on CIHI’s inappropriate antipsychotic medication use quality indicator.2,3 could be explained by a greater proportion of admissions from hospitals (vs the community) compared to prior years. 2 Unless long-term care providers were able to maintain pre-pandemic levels of medication deprescribing, an increase in medication use at admission would result in worse performance on the quality indicator once these newly admitted residents were included in the denominator 3 months later.
The objective of this study was to characterize the association between pandemic exposure and potentially inappropriate antipsychotic medication use among newly admitted long-term care home residents in 3 large Canadian provinces. Additionally, we examined how the COVID-19 pandemic influenced patterns of antipsychotic medication initiation and discontinuation within the first 3 months of a resident’s stay in long-term care.
Methods
We conducted a repeated cross-sectional study of persons admitted to long-term care homes in the Canadian provinces of Alberta, British Columbia and Ontario (combined population of 23.5 million) between March 5th, 2018, and March 4th, 2021. Ethics approval for secondary data analysis was provided by the University of Waterloo Office of Research Ethics (File #: 43618). In accordance with the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans – TCPS 2 (2022), Article 5.5B, informed consent from participants was not required, as this study relied solely on the secondary analysis of anonymized and non-identifiable clinical assessment records. 22 We reported our findings in accordance with the REporting of studies Conducted using Observational Routinely collected health Data statement for pharmacoepidemiology (RECORD-PE). 23
Data source
We used interRAI Minimum Data Set (MDS) 2.0 24 assessment records reported to CIHI’s Continuing Care Reporting System (CCRS). The MDS 2.0 is a comprehensive health assessment that is administered as part of routine practice in most Canadian provinces and territories. All residents are assessed with the MDS 2.0 within 14 days of admission to long-term care, and routine follow-up assessments are administered quarterly thereafter, or sooner in the case of substantial clinical change. Information from the MDS 2.0 assessment is used to tailor an individual’s care plan, 25 monitor health status and outcomes, evaluate home-level quality using risk-adjusted quality indicators, 18 and assign residents to case-mix groups for needs-based funding allocation. 26
Study cohort
We identified newly admitted long-term care home residents (ie, first ever admission) in Alberta, British Columbia and Ontario, Canada between March 5, 2018, and March 4, 2021. The first COVID-19 outbreak in a Canadian long-term care home was declared on March 5, 2020. We used this date to segment the cohort into 3 exposure periods: 2 pre-pandemic periods (March 5, 2018, to March 4, 2019 and March 5, 2019 to March 4, 2020) and 1 pandemic period (March 5, 2020 to March 4, 2021).
We excluded residents who were under 18 years of age, comatose, or expected to have a short length of stay of less than 90 days, as determined by the assessor and excluding discharge due to death. The final exclusion was based on the substantial decrease in admissions for convalescent care and other short-stay programmes during the first year of the pandemic. 2 We employed the same resident characteristic exclusion criteria as CIHI’s publicly reported quality indicator for potentially inappropriate antipsychotic medication use. 18 These exclusions included diagnoses of schizophrenia and Huntington’s disease, as well as the presence of hallucinations, delusions, end-stage disease (6 months or less to live) or receipt of hospice care.
We also created a sub-cohort of residents remaining in the same long-term care home who were reassessed 70 to 110 days after the initial assessment as part of usual care. For this sub-cohort, we excluded residents admitted between November 5th and March 4th in each exposure period because the routine follow-up assessment would occur in a subsequent exposure period. The same quality indicator exclusion criteria (eg, schizophrenia, hallucinations) were also applied to the follow-up assessments.
Outcomes and measures
We observed the use of any antipsychotic medications using the MDS 2.0 assessment. Trained assessors are required to indicate the number of days in which the resident used a medication belonging to the antipsychotic class in the 7 days preceding the MDS 2.0 admission assessment date. For the subset of residents with follow-up assessments, we observed longitudinal change in antipsychotic medication relative to the prior admission assessment. Evidence from Alberta indicates that the quality of the antipsychotic medication items was not affected during the pandemic period. 27
We categorized residents into 5 groups based on the care setting from which they were admitted. These admission source groups were defined as hospital (ie, inpatient acute care), community (ie, assisted living facility and private home settings, either with or without publicly delivered home care services), post-acute care (ie, inpatient continuing care and inpatient rehabilitation), inpatient psychiatry and other (ie, ambulatory care and other unclassified services).
Independent variables of interest were admission source, age category, sex, neuropsychiatric diagnosis (Alzheimer’s disease and related dementias, anxiety, depression, bipolar disorder, stroke), behaviours (verbal and physical abuse, social inappropriateness or disruptiveness, resistance to care), care in a specialized dementia care unit, behaviour symptom evaluation programme and mental health evaluation within the last 90 days.
Previously validated summary scales calculated from MDS 2.0 assessment items included the Cognitive Performance Scale, 28 the Activities of Daily Living Hierarchy Scale, 29 and the Aggressive Behaviour Scale. 30 We measured frailty status using the 72-item frailty index defined by Campitelli et al 31 and classified residents as ‘fit’, ‘average’ and ‘frail’ using the age-specific cut-offs proposed by Romero-Ortuno. 32
Statistical analysis
We used descriptive statistics to compare the sociodemographic and clinical characteristics of residents admitted to long-term care during each of the exposure periods. We identified clinically meaningful differences between the exposure periods using a standardized mean difference statistic threshold of 0.10. This threshold has been used previously to assess balance between treatment groups in propensity score matched samples.33,34
We reported the percentage of residents in the overall cohort who used antipsychotic medications during each exposure period. For residents with follow-up assessments, we reported the rates of antipsychotic medication initiation and discontinuation relative to the baseline admission assessment.
We fit multivariable logistic regression models with interaction terms to characterize the association between the use of antipsychotic medications, exposure period and admission source. These models were adjusted for resident characteristics including sex, age group, Aggressive Behaviour Scale score, Cognitive Performance Scale score, Activities of Daily Living Hierarchy Scale score, and diagnoses of Alzheimer’s disease and related dementias, anxiety disorder, depression, and bipolar disorder. Additional models were fit for each provincial stratum. These models were fit among the full cohort, but only statistics for admissions to long-term care from community and hospital settings were included in forest plot diagrams because they represent the majority of admissions and were directly related to our hypotheses.
We fit a second set of multivariable logistic regression models to characterize the relationship between the exposure period and both the initiation and discontinuation of antipsychotic medications, adjusted for the same set of resident characteristics as the initial models.
Statistical analysis was performed using SAS 9.4 (SAS Institute, Inc., Cary, NC). All hypothesis tests used a two-tailed approach with an alpha of 0.05.
Results
Clinical profile of newly admitted long-term care residents
During the COVID-19 pandemic period (2020/2021), a total of 26 228 residents were newly admitted to long-term care. After applying exclusions for age, comatose status and short stays, 16.5% of residents were excluded because they met at least one exclusion criterion from CIHI’s inappropriate antipsychotic medication use indicator. In comparison, 39 854 residents were admitted in the first pre-pandemic period (2018/2019), and 39 997 in the second (2019/2020). After applying other exclusions, 13.1% of residents in 2018/2019 and 14.1% in 2019/2020 were excluded based on the same CIHI indicator criteria (Table 1).
Table 1.
Description of newly admitted long-term care home residents meeting study inclusion and exclusion criteria by admission period.
| Cohort selection step | 2018/2019 | 2019/2020 | Pandemic 2020/2021 |
|---|---|---|---|
| Total long-term care residents admitted within period and assessed with MDS 2.0 assessment | 39 854 | 39 997 | 26 228 |
| Exclusions | |||
| Age < 18 | 31 | 21 | 8 |
| Comatose | 5 | 13 | 19 |
| Expected short (<90 d) length of stay | 4136 | 3852 | 323 |
| Met CIHI DRG01 quality indicator exclusion criteria (not mutually exclusive) | 4683 | 5094 | 4266 |
| Schizophrenia | 15.9% | 14.1% | 12.4% |
| Huntington’s disease | 1.8% | 1.1% | 1.2% |
| End-stage disease | 25.5% | 26.4% | 28.6% |
| Hospice care | 3.7% | 4.4% | 3.4% |
| Hallucinations | 25.8% | 25.8% | 27.7% |
| Delusions | 48.4% | 50.7% | 50.1% |
| Total long-term care residents meeting primary study cohort inclusion criteria | 30 999 | 31 017 | 21 612 |
| Total long-term care residents assessed with follow-up MDS 2.0 assessment 70-110 d later | 24 919 | 24 999 | 17 057 |
| Exclusions | |||
| Follow-up MDS 2.0 assessment occurred during subsequent period | 6269 | 5839 | 4375 |
| Met CIHI DRG01 quality indicator exclusion criteria at follow-up (not mutually exclusive) | 1667 | 1800 | 1327 |
| Schizophrenia | 2.0% | 2.1% | 1.7% |
| Huntington’s disease | 0.2% | 0.2% | 0.2% |
| End-stage disease | 30.8% | 31.2% | 34.1% |
| Hospice care | 4.3% | 5.6% | 4.5% |
| Hallucinations | 25.0% | 27.4% | 24.3% |
| Delusions | 54.7% | 53.8% | 52.7% |
| Total long-term care residents meeting secondary study cohort inclusion criteria | 16 983 | 16 860 | 11 355 |
DRG01 = Percentage of residents on antipsychotics without a diagnosis of psychosis.
Long-term care residents in Ontario accounted for a lower proportion (50.0%) of the pandemic period cohort than prior years (62.2%-61.2%). The most notable difference between these periods was in the admission source, with 44.8% of residents admitted from a hospital during the pandemic, compared to 31.3-32.0% in the pre-pandemic periods. There was a meaningful increase in the percentage of residents who were dependent in activities of daily living (ADL-Hierarchy 5-6 38.2% vs 21.0-21.5%) and frail (33.6% vs 28.9-29.4%; Table 2). These differences may be partially explained by outbreak-related restrictions on resident movement within the facility during the pandemic period. While there was a small increase in the percentage of residents who did not walk within their rooms (39.9% vs 34.6-34.9%) during the pandemic, the percentage of residents who did not walk outside their rooms on the unit was significantly higher during the pandemic (55.9% vs 37.4-38.0%), as was the number of residents who did not engage in locomotion on the unit, including using a wheelchair (22.0% vs 2.0-2.1%). Only the latter of these three assessment items is used to score the Activities of Daily Living Hierarchy scale and frailty index. Otherwise, residents across all three periods were comparable in age, sex, disease diagnoses, severity of cognitive impairment, behaviour frequency and programmes.
Table 2.
Characteristics of newly admitted long-term care home residents by admission period.
| Resident characteristic | 2018/2019 admissions (n = 30 999) | 2019/2020 admissions (n = 31 017) | Pandemic (2020/2021) admissions (n = 21 612) | SMD pandemic vs 2018/2019 | SMD pandemic vs 2019/2020 |
|---|---|---|---|---|---|
| Province (%) | |||||
| Alberta | 5277 (17.0) | 5227 (16.9) | 4525 (20.9) | 0.263 | 0.238 |
| British Columbia | 6427 (20.7) | 6801 (21.9) | 6383 (29.5) | ||
| Ontario | 19 295 (62.2) | 18 989 (61.2) | 10 704 (49.5) | ||
| Admission source (%) | |||||
| Hospital (inpatient acute) | 9935 (32.0) | 9719 (31.3) | 9684 (44.8) | 0.368 | 0.386 |
| Community | 16 574 (53.5) | 16 746 (54.0) | 7738 (35.8) | ||
| Post-acute care | 1838 (5.9) | 1717 (5.5) | 2059 (9.5) | ||
| Inpatient psychiatry | 178 (0.6) | 166 (0.5) | 162 (0.7) | ||
| Other | 2474 (8.0) | 2669 (8.6) | 1969 (9.1) | ||
| Female sex (%) | 19 000 (61.3) | 18 843 (58.3) | 12 594 (60.8) | 0.065 | 0.052 |
| Age category (%) | |||||
| 18-64 y | 1529 (4.9) | 1554 (5.0) | 1220 (5.6) | 0.065 | 0.072 |
| 65-74 y | 3400 (11.0) | 3359 (10.8) | 2722 (12.6) | ||
| 75-84 y | 9293 (30.0) | 9141 (29.5) | 6477 (30.0) | ||
| 85-94 y | 13 968 (45.1) | 14 046 (45.3) | 9316 (43.1) | ||
| 95+ years | 2809 (9.1) | 2917 (9.4) | 1877 (8.7) | ||
| Diagnosis (%) | |||||
| Anxiety disorder | 3743 (12.1) | 3962 (12.8) | 2684 (12.4) | 0.011 | 0.011 |
| ADRD | 18 601 (60.0) | 18 275 (58.9) | 12 718 (58.8) | 0.024 | 0.001 |
| Bipolar disorder | 468 (1.5) | 463 (1.5) | 381 (1.8) | 0.020 | 0.021 |
| Depression | 7268 (23.4) | 7257 (23.4) | 5087 (23.5) | 0.002 | 0.003 |
| Stroke | 5753 (18.6) | 5628 (18.1) | 4174 (19.3) | 0.019 | 0.030 |
| Traumatic brain injury | 351 (1.1) | 377 (1.2) | 315 (1.5) | 0.029 | 0.021 |
| Parkinson’s disease | 1916 (6.2) | 1935 (6.2) | 1342 (6.2) | 0.001 | 0.001 |
| Cognitive Performance Scale (%) | |||||
| 0 (intact) | 2890 (9.3) | 2923 (9.4) | 2069 (9.6) | 0.034 | 0.037 |
| 1-2 (mild impairment) | 10 870 (35.1) | 10 794 (34.8) | 7260 (33.6) | ||
| 3-4 (moderate impairment) | 13 939 (45.0) | 14 098 (45.5) | 9841 (45.5) | ||
| 5-6 (severe impairment) | 3202 (10.3) | 2442 (11.3) | 3300 (10.6) | ||
| Activities of Daily Living Hierarchy Scale (%) | |||||
| 0 (independent) | 1083 (3.5) | 1096 (3.5) | 733 (3.4) | 0.374 | 0.386 |
| 1-2 (limited assistance) | 6685 (21.6) | 6591 (21.2) | 3832 (17.7) | ||
| 3-4 (extensive assistance) | 16 575 (53.5) | 16 809 (54.2) | 8800 (40.7) | ||
| 5-6 (dependent) | 6656 (21.5) | 6521 (21.0) | 8247 (38.2) | ||
| Frailty status (%) | |||||
| Fit for their age | 6580 (21.2) | 6617 (21.3) | 4047 (18.7) | 0.097 | 0.107 |
| Average for their age | 15 299 (49.4) | 15 436 (49.8) | 10 297 (47.6) | ||
| Frail for their age | 9120 (29.4) | 8964 (28.9) | 7268 (33.6) | ||
| Aggressive Behaviour Scale (%) | |||||
| 0 (no behaviours) | 19 632 (63.3) | 19 759 (63.7) | 13 726 (63.5) | 0.011 | 0.026 |
| 1-4 (mild behaviours) | 9652 (31.1) | 9659 (31.1) | 6647 (30.8) | ||
| 5-14 (severe behaviours) | 1715 (5.5) | 1599 (5.2) | 1239 (5.7) | ||
| Behaviours on 4+ days (%) | |||||
| Wandering | 6773 (21.8) | 6549 (21.1) | 4292 (19.9) | 0.049 | 0.031 |
| Verbal abuse | 3174 (14.7) | 4172 (13.5) | 4173 (13.5) | 0.035 | 0.035 |
| Physical abuse | 2801 (9.0) | 2768 (8.9) | 2083 (9.6) | 0.021 | 0.025 |
| Socially inappropriate or disruptive | 4289 (13.8) | 4342 (14.0) | 3061 (14.2) | 0.009 | 0.005 |
| Resists care | 9403 (30.3) | 9233 (29.8) | 6328 (29.3) | 0.023 | 0.011 |
| Programmes (%) | |||||
| Dementia care unit | 4943 (15.9) | 5072 (16.4) | 3401 (15.7) | 0.006 | 0.017 |
| Behaviour symptom evaluation program | 2012 (6.5) | 2373 (7.7) | 1364 (6.3) | 0.007 | 0.053 |
| Mental health evaluation in last 90 d | 829 (2.7) | 811 (2.6) | 501 (2.3) | 0.023 | 0.019 |
SMD = standardized mean difference.
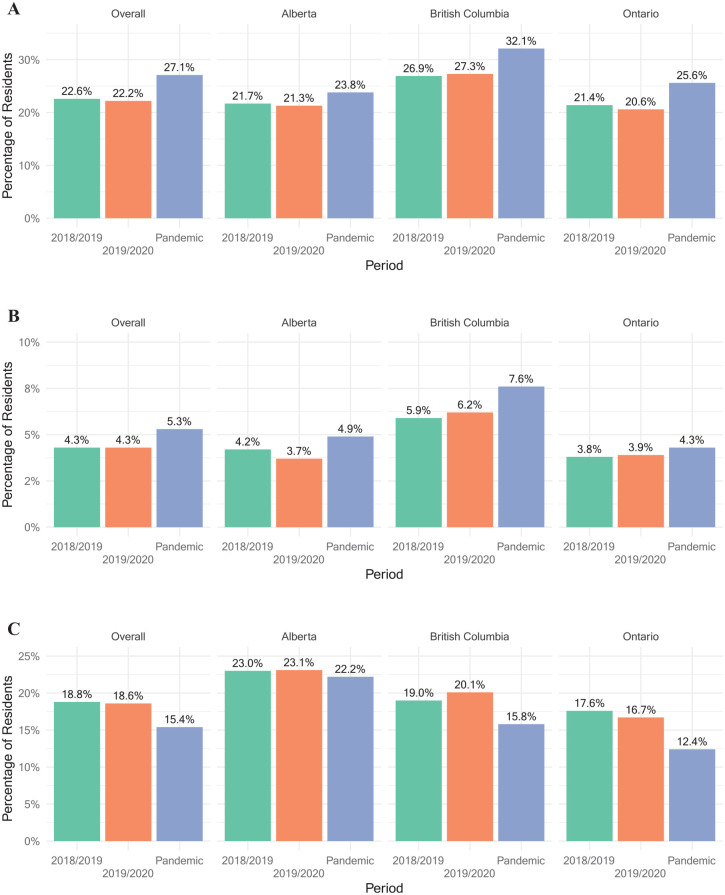
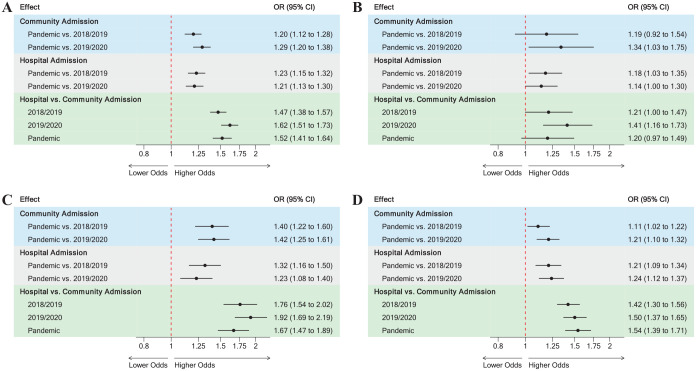
Antipsychotic use at admission to long-term care
The absolute percentage of newly admitted residents who used antipsychotic medications by period is presented in Panel A of Figure 1. In comparison to both pre-pandemic periods, the adjusted odds of antipsychotic medication use among the overall cohort were significantly greater during the pandemic period for residents admitted from both community (OR range 1.20-1.29) and hospital settings (OR range 1.21-1.23) (Figure 2, Panel A). Residents admitted from hospitals were consistently more likely to use antipsychotic medications in all periods (OR range 1.47-1.52; Figure 2 Panel A). These patterns were similar in British Columbia and Ontario (Figure 2 Panels C and D). In contrast, only some of the adjusted odds ratios were significantly greater in Alberta (Figure 2, Panel B). Also, the odds of receiving antipsychotic medications in Alberta were not significantly different between hospital and community admissions during the pandemic period (OR 1.20, 95% CI 0.97-1.49). Adjusted odds ratio statistics for the remaining admission settings are presented in Supplemental Table 1.
Figure 1.
Percentage of residents who received antipsychotic medications at time of admission MDS 2.0 assessment in long-term care (n = 83 628 residents; Panel A), percentage of residents where antipsychotic medications were initiated (n = 35 223 residents; Panel B) and discontinued (n = 9 975 residents; Panel C) at time of follow-up MDS 2.0 assessment in long-term care.
Figure 2.
Adjusted odds of receiving antipsychotic medications at time of admission MDS 2.0 assessment in long-term care: (A) Overall (n = 83 628 residents), (B) Alberta (n = 15 029 residents), (C) British Columbia (n = 19 611 residents) and (D) Ontario (n = 48 988 residents)
Models adjust for age, sex, Aggressive Behaviour Scale, Cognitive Performance Scale, Activities of Daily Living Hierarchy Scale, Alzheimer’s disease and related dementias diagnosis, anxiety disorder diagnosis, depression diagnosis and bipolar disorder diagnosis.
Antipsychotic initiation and discontinuation at follow-up
In the overall cohort, antipsychotic medications were newly initiated within the first three months of stay among 5.3% of residents during the pandemic compared to 4.3% before the pandemic (Figure 1, Panel B). After controlling for differences in resident characteristics between periods, the adjusted odds of newly initiating antipsychotic medications increased by 25% to 26% during the pandemic (OR range 1.25-1.26). The pandemic period was associated with a significant increase in antipsychotic medication initiation for at least one comparison in each of the provincial strata (Figure 3, Panel A).
Figure 3.
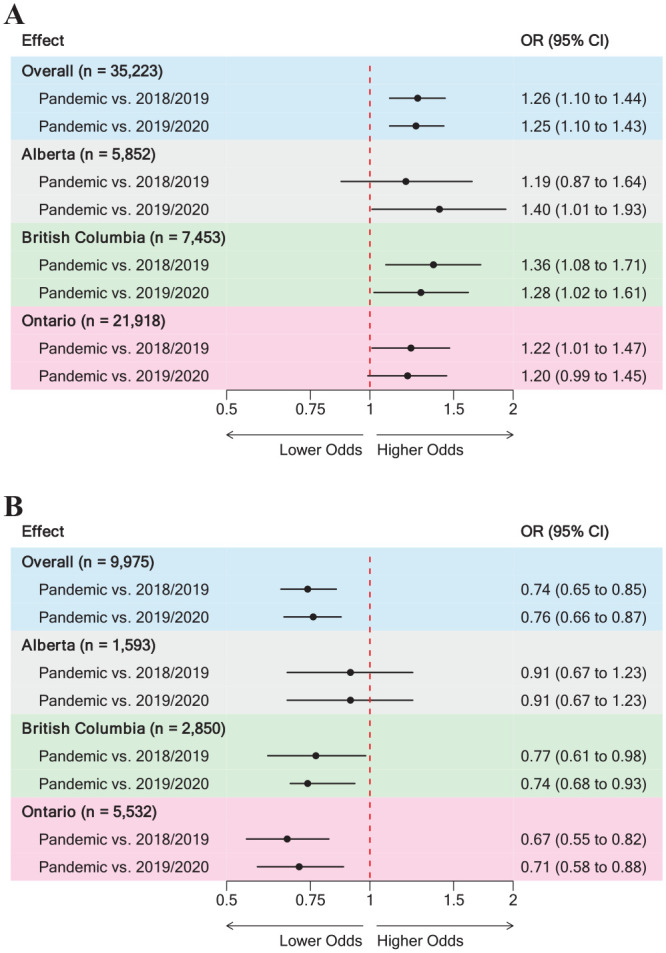
Adjusted odds of antipsychotic medication initiation (Panel A) and discontinuation (Panel B) at time of follow-up MDS 2.0 assessment in long-term care.
Models adjust for age, sex, Aggressive Behaviour Scale, Cognitive Performance Scale, Activities of Daily Living Hierarchy Scale, Alzheimer’s disease and related dementias diagnosis, anxiety disorder diagnosis, depression diagnosis and bipolar disorder diagnosis.
In the overall cohort, antipsychotic medications were discontinued within the first three months of stay among 15.4% of residents during the pandemic compared to 18.6-18.8% before the pandemic (Figure 1, Panel C). After controlling for differences in resident characteristics between periods, the adjusted odds of discontinuing antipsychotic medications decreased by 32% to 35% during the pandemic (OR range 0.74-0.76). Within the provincial strata, this significant decrease was only observed in British Columbia (OR range 0.74-0.77) and Ontario (OR range 0.67-0.71; Figure 3, Panel B).
Discussion
We compared the rate of antipsychotic medication use among newly admitted long-term care home residents without a diagnosis of psychosis during the first year of the COVID-19 pandemic against two pre-pandemic periods using routinely collected MDS 2.0 comprehensive health assessments in three large Canadian provinces. There was a significant increase in antipsychotic medication use during the pandemic period among residents admitted from both hospital and community settings. Among these residents, we also observed a significant increase in initiation and a decrease in discontinuation at the time of the routine quarterly re-assessment. Our findings were generally consistent across each of the provincial strata.
Antipsychotic medications prescribed for non-psychiatric diagnoses in acute care are often used to manage symptoms of agitation and delirium. 35 The use of these medications often persists post-discharge36 -40 and was more prevalent among residents in our cohort who were admitted from hospitals. Antipsychotic medication use has been a quality improvement priority in Canadian long-term care homes for the past decade, in part because of the availability of publicly reported quality indicators from CIHI. interRAI assessments can be used to measure antipsychotic use in both hospital and community settings 20 ; however, these measures are not routinely reported by CIHI. In this regard, our results serve as a lagging indicator of the prevalent use of antipsychotic medications outside of long-term care and suggest that quality improvement initiatives to reduce their use should apply a whole-systems approach. As a first step to addressing this broader issue, organizations like CIHI should report on the use of these medications using existing interRAI assessments in home care, acute care and post-acute care settings.
Within this whole-systems approach, and in alignment with Canada’s National Long-term Care Services standard, 41 long-term care homes should continue to undertake medication review and reconciliation during the initial transition period for newly admitted residents. Long-standing care staff shortages, exacerbated by COVID-19 through increased workloads and single-site work mandates, further intensified conditions for staff burnout and workforce instability. 42 This was compounded by no-visitor policies that prevented essential family caregivers from assisting in direct care tasks. 43 Our finding that antipsychotic medication discontinuation rates decreased significantly during the pandemic period suggests that the strain placed on the long-term care system and staff led to at least some suspension of routine care practices. Our provincial-level analysis indicates that Ontario long-term care homes were most affected in this regard. This is consistent with the provincial-level impact during the first year of the pandemic. 1
We observed an increase in antipsychotic medication use at admission among residents admitted from both hospital and community settings during the pandemic period. Thus, we conclude that a greater proportion of patients admitted from hospital settings cannot be the sole reason for decreased performance on the CIHI quality indicator measuring potentially inappropriate antipsychotic use during the pandemic period. Apart from functional impairment and frailty, the clinical profile of newly admitted residents during the pandemic period was comparable to prior years. Our models controlled for factors previously associated with antipsychotic initiation, including sex, age, marital status and the Aggressive Behaviour Scale. 44
Considering that the community accounts for half of the total admissions, our finding that more residents admitted from the community are receiving antipsychotic medications without a diagnosis of psychosis highlights a need to increase supports for informal caregivers. For example, a decrease in home care service visits for personal care at the beginning of the pandemic period21,45 may have contributed to unmet needs leading to behaviours among persons that were previously well managed in the community. This is supported by a marked increase in burden,46,47 depressive symptoms, and anxiety48,49 among informal caregivers during this period.
Although our analysis focused on antipsychotic medications, it is important to acknowledge that off-label use of other psychotropic medications such as gabapentin and trazodone has increased dramatically in recent years among long-term care residents, 43 accelerating during the pandemic period. 5 These agents lack strong evidence as effective treatments for behavioural and psychological symptoms of dementia and are associated with similar rates of harm as antipsychotics. 43 Given the demonstrated effectiveness of non-pharmacological interventions for residents with behaviours,19,50 as part of the pandemic recovery effort, health systems should focus on implementing policies that support long-term care staff and enhance their ability to provide resident-centred care.
Strengths and limitations
Our results are a population-level representation of patterns of potentially inappropriate antipsychotic medication use, initiation and discontinuation during the COVID-19 pandemic. We used the same MDS 2.0 data and exclusion criteria as CIHI’s publicly reported quality indicator, and we were able to control for differences in antipsychotic use risk factors (including responsive behaviours) over time. However, using these data, we were unable to identify whether newly admitted residents were prescribed antipsychotic medications prior to, or at the time of entry to long-term care. We excluded residents with clinical characteristics for which the use of antipsychotic medications is considered appropriate. In our cohort this was predominantly for delusions. A recent time series analysis of Ontario long-term care homes indicates that the percentage of residents exhibiting delusions increased from 3.5% to 10.2% in less than 5 years. 15 As others have noted, 15 it remains unclear whether this increase is the result of more accurate coding practices, or if it represents a deliberate effort to positively bias results on CIHI’s publicly reported quality indicator. In the latter case, our results may underestimate the true increase in antipsychotic medication use during the pandemic. Lastly, we were unable to link facility-level measures of COVID-19 impact (eg, outbreak intensity and duration) and staffing patterns to the MDS 2.0 data, which limited our ability to examine variations in pandemic exposure on patterns of antipsychotic initiation and discontinuation.
Conclusion
Antipsychotic medication use among long-term care residents who were newly admitted from hospital and community settings increased during the COVID-19 pandemic in Canada. As such, a whole-systems approach that extends beyond long-term care is necessary to address this quality issue. The pandemic placed significant strain on human health resources in the long-term care sector49,51 and is consistent with a decline in antipsychotic discontinuation within the first 3 months of stay. This underscores the importance of multidisciplinary care team members for medication review, deprescribing, and the use of non-pharmacological interventions among newly admitted long-term care residents.
Supplemental Material
Supplemental material, sj-docx-1-his-10.1177_11786329241300827 for Antipsychotic Medication Use Among Newly Admitted Long-term Care Residents During the COVID-19 Pandemic in Canada by Luke A Turcotte, George A Heckman, Caitlin McArthur, Margaret Saari, Chi-Ling Joanna Sinn, Krista Mathias, Asif Khowaja, Nathan M Stall and John P Hirdes in Health Services Insights
Acknowledgments
None.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study is supported in part by funding from the Government of Canada’s New Frontiers in Research Fund (NFRF; NFRFG-2020-00500) for collaboration in the EU Horizon 2020 research and innovation project Individualized CARE for Older Persons with Complex Chronic Conditions in Home Care and Nursing Homes (I-CARE4OLD, Grant Agreement No 965341).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals. Study concept and design: LAT, JPH; Acquisition of data: JPH; Analysis and interpretation of data: LAT; Drafting of the manuscript: LAT; Critical revision of the manuscript: LAT, GAH, CM, MS, CJS, KM, AK, NMS, JPH.
ORCID iD: Luke Andrew Turcotte  https://orcid.org/0000-0001-5678-7234
https://orcid.org/0000-0001-5678-7234
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Canadian Institute for Health Information. Impact of COVID-19 on Long-Term Care, March 2020 to June 2021 — Data Tables. Canadian Institute for Health Information; 2021. https://www.cihi.ca/sites/default/files/document/impact-covid-19-long-term-care-mar-2020-jun-2021-data-tables-en.xlsx [Google Scholar]
- 2. Turcotte LA, McArthur C, Poss JW, et al. Long-term care resident health and quality of care during the COVID-19 pandemic: a synthesis analysis of Canadian Institute for Health Information Data Tables. Health Serv Insights. 2023;16:11786329231174745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoben M, Hogan DB, Poss JW, et al. Comparing quality of care outcomes between assisted living and nursing homes before and during the COVID-19 pandemic. J Am Geriatr Soc. 2023;71:3467-3479. [DOI] [PubMed] [Google Scholar]
- 4. Stall NM, Zipursky JS, Rangrej J, et al. Assessment of psychotropic drug prescribing among nursing home residents in Ontario, Canada, during the COVID-19 pandemic. JAMA Intern Med. 2021;181:861-863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Campitelli MA, Bronskill SE, Maclagan LC, et al. Comparison of medication prescribing before and after the COVID-19 pandemic among nursing home residents in Ontario, Canada. JAMA Netw Open. 2021;4:e2118441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ferro Uriguen A, Laso Lucas E, Sannino Menicucci C, et al. Psychotropic drug prescription in nursing homes during the COVID-19 pandemic. Drugs Aging. 2022;39:467-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coe AB, Montoya A, Chang C, et al. Behavioral symptoms, depression symptoms, and medication use in Michigan nursing home residents with dementia during COVID-19. J Am Geriatr Soc. 2023;71:414-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McDermid J, Ballard C, Khan Z, et al. Impact of the Covid-19 pandemic on neuropsychiatric symptoms and antipsychotic prescribing for people with dementia in nursing home settings. Int J Geriatr Psychiatry. 2023;38:e5878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ali MM, Oliveira I, Blanco M. Prescriptions of antipsychotics dispensed in long-term care facilities during the COVID-19 pandemic. Gen Hosp Psychiatry. 2022;78:141-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Papola D, Ostuzzi G, Thabane L, et al. Antipsychotic drug exposure and risk of fracture: a systematic review and meta-analysis of observational studies. Int Clin Psychopharmacol. 2018;33:181-196. [DOI] [PubMed] [Google Scholar]
- 11. Zivkovic S, Koh CH, Kaza N, Jackson CA. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry. 2019;19:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306:1359. [DOI] [PubMed] [Google Scholar]
- 13. Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294:1934. [DOI] [PubMed] [Google Scholar]
- 14. Canadian Nurses Association. Twelve tests and treatments to question in nursing. Choosing Wisely Canada. August 2024. Accessed October 16, 2024. https://choosingwiselycanada.org/recommendation/nursing/
- 15. Harris DA, Maclagan LC, Iaboni A, et al. Potential unintended consequences of antipsychotic reduction in Ontario nursing homes. J Am Med Dir Assoc. 2022;23:1066-1072.e7. [DOI] [PubMed] [Google Scholar]
- 16. Giovannini-Green ZEM, Gamble JM, Barrett B, Gao Z, Stuckless S, Parfrey PS. Variation and appropriateness of antipsychotic use in long-term care facilities across Newfoundland and Labrador. Can Pharm J (Ott). 2021;154:205-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Turcotte LA, McArthur C, Poss JW, et al. Acknowledging the complexity of antipsychotic use in long-term care during the COVID-19 pandemic. Health Serv Insights. 2023;16:11786329231195211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jones RN, Hirdes JP, Poss JW, et al. Adjustment of nursing home quality indicators. BMC Health Serv Res. 2010;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hirdes JP, Major J, Didic S, et al. A Canadian cohort study to evaluate the outcomes associated with a multicenter initiative to reduce antipsychotic use in long-term care homes. J Am Med Dir Assoc. 2020;21:817-822. [DOI] [PubMed] [Google Scholar]
- 20. Rios S, Perlman CM, Costa A, Heckman G, Hirdes JP, Mitchell L. Antipsychotics and dementia in Canada: a retrospective cross-sectional study of four health sectors. BMC Geriatr. 2017;17:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jones A, Mowbray FI, Falk L, et al. Variations in long-term care home resident hospitalizations before and during the COVID-19 pandemic in Ontario. PLoS One. 2022;17:e0264240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Government of Canada. Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans – TCPS 2 (2022). Secretariat on Responsible Conduct of Research; 2022. [Google Scholar]
- 23. Langan SM, Schmidt SA, Wing K, et al. The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE). BMJ. 363:k3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bernabei R, Landi F, Onder G, Liperoti R, Gambassi G. Second and Third Generation Assessment Instruments: The Birth of Standardization in Geriatric Care. The Journals of Gerontology: Series A. 2008;63(3):308–313. doi: 10.1093/gerona/63.3.308 [DOI] [PubMed] [Google Scholar]
- 25. Heckman GA, Gray LC, Hirdes JP. Addressing health care needs for frail seniors in Canada: the role of interRAI instruments. CGS J CME. 2013;3(1):8–16. [Google Scholar]
- 26. Turcotte LA, Poss J, Fries B, Hirdes JP. An overview of international staff time measurement validation studies of the RUG-III case-mix system. Health Serv Insights. 2019;12:117863291982792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poss J, Silvius J, Hoben M, et al. Agreement between 2 sources of antipsychotic coding before and during the COVID-19 pandemic in long-term care. J Am Med Dir Assoc. 2023;24:923-925.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morris JN, Fries BE, Mehr DR, et al. MDS Cognitive Performance Scale. J Gerontol. 1994;49:M174-M182. [DOI] [PubMed] [Google Scholar]
- 29. Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54:M546-M553. [DOI] [PubMed] [Google Scholar]
- 30. Perlman CM, Hirdes JP. The Aggressive Behavior Scale: a new scale to measure aggression based on the minimum data set. J Am Geriatr Soc. 2008;56:2298-2303. [DOI] [PubMed] [Google Scholar]
- 31. Campitelli MA, Bronskill SE, Hogan DB, et al. The prevalence and health consequences of frailty in a population-based older home care cohort: a comparison of different measures. BMC Geriatr. 2016;16:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Romero-Ortuno R. An alternative method for Frailty Index cut-off points to define frailty categories. Eur Geriatr Med. 2013;4:299-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly. J Clin Epidemiol. 2001;54:387-398. [DOI] [PubMed] [Google Scholar]
- 35. Jaworska N, Moss SJ, Krewulak KD, et al. A scoping review of perceptions from healthcare professionals on antipsychotic prescribing practices in acute care settings. BMC Health Serv Res. 2022;22:1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Riester MR, Goyal P, Jiang L, et al. New antipsychotic prescribing continued into skilled nursing facilities following a heart failure hospitalization: a retrospective cohort study. J Gen Intern Med. 2022;37:3368-3379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Herzig SJ, Rothberg MB, Guess JR, et al. Antipsychotic use in hospitalized adults: rates, indications, and predictors. J Am Geriatr Soc. 2016;64:299-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hakala A, Tolppanen AM, Koponen M, et al. Does recent hospitalization increase antipsychotic initiation among community dwellers with alzheimer’s disease? J Am Med Dir Assoc. 2021;22:1543-1547.e3. [DOI] [PubMed] [Google Scholar]
- 39. Marshall J, Herzig SJ, Howell MD, et al. Antipsychotic utilization in the intensive care unit and in transitions of care. J Crit Care. 2016;33:119-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Burry LD, Bell CM, Hill A, et al. New and persistent sedative prescriptions among older adults following a critical illness. Chest. 2023;163:1425-1436. [DOI] [PubMed] [Google Scholar]
- 41. Health Standards Organization. Long-Term Care Services - CAN/HSO 21001:2023 (E). Health Standards Organization; 2023. [Google Scholar]
- 42. Gray KL, Birtles H, Reichelt K, James IA. The experiences of care home staff during the COVID-19 pandemic: a systematic review. Aging Ment Health. 2022;26:2080-2089. [DOI] [PubMed] [Google Scholar]
- 43. Reppas-Rindlisbacher C, Stall NM, Rochon PA. Psychotropic substitutions: out of the frying pan and into the fire. J Am Geriatr Soc. 2023;71:2013-2016. [DOI] [PubMed] [Google Scholar]
- 44. Maclagan LC, Maxwell CJ, Harris DA, et al. Sex differences in antipsychotic and benzodiazepine prescribing patterns: a cohort study of newly admitted nursing home residents with dementia in Ontario, Canada. Drugs Aging. 2020;37:817-827. [DOI] [PubMed] [Google Scholar]
- 45. Sinn CLJ, Sultan H, Turcotte LA, McArthur C, Hirdes JP. Patterns of home care assessment and service provision before and during the COVID-19 pandemic in Ontario, Canada. PLoS One. 2022;17:e0266160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cohen SA, Kunicki ZJ, Drohan MM, Greaney ML. Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontol Geriatr Med. 2021;7:233372142199927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Budnick A, Hering C, Eggert S, et al. Informal caregivers during the COVID-19 pandemic perceive additional burden: findings from an ad-hoc survey in Germany. BMC Health Serv Res. 2021;21:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wister A, Li L, Mitchell B, et al. Levels of depression and anxiety among informal caregivers during the COVID-19 pandemic: a study based on the Canadian longitudinal study on aging. J Gerontol B Psychol Sci Soc Sci. 2022;77:1740-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Altieri M, Santangelo G. The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. Am J Geriatr Psychiatry. 2021;29:27-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hanson HM, Léveillé T, Cole M, et al. Effect of a multimethod quality improvement intervention on antipsychotic medication use among residents of long-term care. BMJ Open Qual. 2021;10:e001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Estabrooks CA, Duan Y, Cummings GG, et al. Changes in health and well-being of nursing home managers from a prepandemic baseline in February 2020 to December 2021. J Am Med Dir Assoc. 2023;24:148-155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-his-10.1177_11786329241300827 for Antipsychotic Medication Use Among Newly Admitted Long-term Care Residents During the COVID-19 Pandemic in Canada by Luke A Turcotte, George A Heckman, Caitlin McArthur, Margaret Saari, Chi-Ling Joanna Sinn, Krista Mathias, Asif Khowaja, Nathan M Stall and John P Hirdes in Health Services Insights