Abstract
Background
Total knee arthroplasty (TKA) offers substantially improved function for patients with severe osteoarthritis, but long-term success can be overshadowed by aseptic loosening, a complication with a multifactorial etiology. This study aims to investigate the association between BMI and the rate of aseptic loosening and other complications in patients undergoing primary TKA.
Methods
This retrospective cohort study examined 354 TKA patients, evenly categorized by BMI (≤ 30 kg/m² and > 30 kg/m²). Demographics, imaging findings, surgical details, and postoperative complications were assessed. Survival for postoperative complications was compared between the two BMI cohorts using Kaplan-Meier analysis.
Results
The mean age of patients in the BMI ≤ 30 group was 62.44 years, while it was 62.84 years in the BMI > 30 group. The number of patients with short-stemmed tibial components was comparable in the two groups. Out of the total patients, 350 cases showed no loosening, while four experienced aseptic loosening. There was no statistically significant difference in the rate of aseptic loosening or other complications between the two groups.
Conclusion
While a high BMI may contribute to aseptic loosening, it does not appear to be the sole determinant. A multifactorial approach to prevention and management is essential, considering patient-specific factors and prosthetic considerations. Future research with larger cohorts and extended follow-up periods is needed to better elucidate the interplay between BMI and aseptic loosening in patients undergoing TKA.
Keywords: Total knee arthroplasty, Aseptic loosening, Body mass index, Obesity, Surgical outcomes
Introduction
Total knee arthroplasty (TKA) represents a major advancement in orthopedic surgery, offering substantial improvement in mobility and function for patients with severe knee osteoarthritis. However, as with any surgical procedure, it is not without potential complications. Aseptic loosening occurs in 3% of primary TKA patients over a 15-year postoperative period and is responsible for 31% of revisions following primary TKA [1–3].
Aseptic loosening in TKA results from a complex interplay of various factors, broadly categorized into three main subgroups: patient-related, surgical technique-related, and Implant design-related [4].
In recent decades, the global prevalence of obesity (one of the patient-related factors) has reached alarming levels due to sedentary lifestyles. The World Health Organization (WHO) defines obesity as a BMI ≥ 30 Kg/m² [5]. This observation is noteworthy, given the established association between elevated BMI and an increased risk of degenerative osteoarthritis, particularly in individuals aged 65 years and older. Consequently, this anthropomorphic feature often leads to a heightened demand for TKA [6].
patient-related factors, particularly patient’s BMI have received significant attention in recent TKA research endeavors due to their potential impact on outcomes. Currently, a controversy exists regarding the influence of BMI on aseptic loosening in primary TKA. Some studies report a two-fold increased risk of aseptic loosening within a 5 to 10-year postoperative follow-up period for individuals with a BMI exceeding 35 [7]. This led some researchers to advocate for stemmed tibial components in obese patients, However, conflicting findings from other studies highlight the need for further investigation [8, 9]. On the other hand, findings from other studies suggest there is no significant association between aseptic loosening and high BMI in patients, which contributes to the ongoing controversy regarding the primary outcome of TKA in obese individuals [10, 11].
The lack of consensus and agreement on the impact of this anthropometric factor, which is also increasing over time, on TKA outcomes necessitates further research in this area. The goal of this study is to elucidate the role of patient-related factors, especially BMI in TKA outcomes and develop more informed clinical decision-making strategies to improve the durability of TKA and reduce the burden of aseptic loosening on patients and the healthcare system.
Materials and methods
Study design and patient selection
We conducted a retrospective cohort study, examining the electronic records of patients with unilateral knee degenerative osteoarthritis who underwent primary TKA at the Imam Khomeini Hospital Complex, Tehran, Iran, which was affiliated with the Tehran University of Medical Sciences between 2011 and 2020.
This study included 354 patients, evenly divided into two groups based on their BMI: one group with a BMI above 30 kg/m² and another with a BMI below 30 kg/m² [5]. To be included in this study, patients needed to meet the following criteria: they had to be between 40 and 80 years of age and had undergone primary TKA due to advanced knee osteoarthritis.
To ensure study integrity and focus on the isolated impact of BMI, several exclusion criteria were applied. These criteria excluded patients with:
History of septic arthritis of the knee.
Previous knee surgery.
Congenital musculoskeletal diseases.
Neuromuscular disorders.
Prosthetic Joint Infections (PJIs).
Follow-up period less than 2 years.
Knee instability.
Bone defects of more than 15 mm.
These surgeries were performed by two highly specialized knee surgeons. Both surgeons utilized the subvastus approach. Defects measuring less than 5 mm were managed with orthopedic cement, while those within the range of 5–10 mm were addressed using screws, and defects exceeding 10 mm were treated with autologous bone grafts.
The decision to utilize a stemmed tibial component during TKA hinged on radiographic parameters. If a patient exhibited a normal medial proximal tibial angle (MPTA) (above 85°) but an abnormal joint convergence angle (JCA) (above 7°), indicative of intra-articular severe defects, a stemmed tibial component was deemed necessary, likewise, if the surgeon intraoperatively faced a bone defect extending beyond 50% of the tibial plateau or involving the area where the tibial tray would sit (tibial keel component), a stemmed tibial component was employed [7, 12, 13].
Cementation of the components was performed full (not just surface) using an orthopedic cement gun and with the assistance of a spatula.
A standardized physical therapy and weight-bearing protocol was implemented following surgery to optimize functional recovery. However, for patients with severe bone defects requiring autograft, a modified weight-bearing protocol was employed due to the potential for delayed union. These patients underwent weight-bearing restrictions during the initial post-operative month. This was followed by a period of partial weight-bearing with assistive devices for an additional 15 days. Finally, upon radiographic confirmation at 45 days post-surgery, full weight bearing was permitted.
All patients received prostheses from a single manufacturer (Zimmer® NexGen® LPS-Flex). For cases requiring a stemmed tibial component, a 15 × 30 mm prosthesis was utilized.
Variables and data collection
Demographic and anthropometric Data: Essential demographic data, including age and gender, were collected for all patients. The study placed particular emphasis on anthropometric data, notably BMI, a key indicator of the patients’ physical characteristics.
Preoperative radiological evaluations were performed on all patients using three-joint alignment view X-rays. We measured specific preoperative radiologic parameters including the JCA, lateral distal femoral angle (LDFA), and MPTA. These variables were categorized into various subgroups based on established references [14–16] to facilitate analysis.
-
Varus alignment (VA):
- Class 1 (VA ≤ 10).
- Class 2 (VA 10–20).
- Class 3 (VA > 20).
-
Joint convergence angle (JCA):
- Class 1 (JCA ≤ 5).
- Class 2 (JCA > 5).
-
Medial proximal tibial angle (MPTA):
- MPTA ≤ 80
- MPTA > 80
For each patient, a matched control was identified in the other BMI group based on the same preoperative radiological variable categories.
Surgical Parameters: Data on surgical parameters was collected, with a focus on the type of prosthesis design employed. Specifically, we differentiated between patients who received a short-stemmed tibial component and those who underwent surgery with a stemless tibia component. This differentiation allowed for an assessment of the potential influence of the implant design on the study’s outcomes.
Postoperative Complications: The Knee Society Roentgenographic Evaluation and Scoring System (KSRES) was used in this study to evaluate aseptic loosening probability based on post-surgical X-rays [17]. The KSRES assigns scores by considering the total number of radiolucent lines seen on both front (AP) and side (lateral) X-rays. Higher scores (10 or greater) indicate a greater number of radiolucent lines, potentially indicating loosening, while lower scores (4 or less) suggest good implant stability with few or no radiolucent lines. The recommended postoperative follow-up program for patients with a score of 4 or less includes visits at one month, three months, one year, and then annually, while for patients with a score of 5–9, more frequent visits were conducted.
Progressive increases in KSRES scores and malposition of the implant components are indicators of aseptic loosening in TKA. All suspected cases of loosening underwent an examination that included measurements of ESR and CRP, as well as joint arthrocentesis, with a focus on PJI.
Additionally, the study monitored the occurrence of other postoperative complications, including periprosthetic fractures, surgical site complications, as well as joint stiffness and instability.
Statistical analysis
Descriptive statistics were applied to categorical variables, providing frequencies and percentages, while continuous variables were subjected to mean and standard deviation calculations. We explored the relationships between various groups using independent samples student’s T-tests for continuous variables and chi-square and Fisher’s exact tests for categorical variables. The survival rate free from all postoperative complications was compared between the two BMI cohorts using Kaplan-Meier analysis. The log-rank test was used to assess for statistically significant differences in survival curves over time.
P values less than 0.05 were assumed to be statistically significant, but clinical significance was assessed by examining the magnitude of the effect and the 95% confidence intervals.
A post-hoc power analysis was conducted to assess the achieved power of the study in detecting statistically significant differences in overall complication rates after TKA. The entire analytical process was performed utilizing IBM SPSS version 27 software.
Ethical considerations
This study received the ethical approval from the ethical committee at Tehran University of Medical Sciences (code: IR.TUMS.IKHC.REC.1400.265). Given the retrospective nature of our study, which did not involve direct human intervention or breach patient confidentiality, the need for obtaining individual patient consent was waived by our ethical committee. Study investigators were committed to save patients data private and use them only for the conducted study.
Results
A total of 354 patients who underwent primary TKA were included in this study. Among them, 177 patients had a BMI above 30, while the remaining 177 patients had a BMI below 30 (Table 1).
Table 1.
Demographic characteristics of study participants
| Demographic Features | BMI Above 30 (n = 177) | BMI Below 30 (n = 177) | Total (n = 354) |
|---|---|---|---|
| Women (n, %) | 165 (46.6%) | 118 (33.3%) | 283 (79.9%) |
| Men (n, %) | 12 (3.4%) | 59 (16.7%) | 71 (20.1%) |
| Age (Mean ± SD) | 62.84 ± 8.33 | 62.44 ± 11.14 | 62.64 ± 9.83 |
In the high BMI group, the mean follow-up was 3.0 years (range: 2.2 to 6.4 years), and in the low BMI group, the mean follow-up was 3.2 years (range: 2.9 to 6.5 years).
Preoperative radiographic assessment revealed no significant differences in JCA, MPTA, and LDFA between patients with BMI above 30 kg/m² and those below 30 kg/m² You can see a summary of these results in Table 2.
Table 2.
Comparison of radiological variables in patients with BMI above and below 30
| Radiological Variables | BMI > 30 (Mean ± SD) | BMI ≤ 30 (Mean ± SD) | p-value |
|---|---|---|---|
| Joint Convergence Angle (JCA) | 9.05° ± 5.81° | 8.81° ± 6.13° | 0.711 |
| Medial Proximal Tibial Angle (MPTA) | 84.99° ± 3.73° | 84.98° ± 4.25° | 0.973 |
| Lateral Distal Femoral Angle (LDFA) | 90.98° ± 3.46° | 91.01° ± 4.56° | 0.937 |
There were no significant differences in the use of short-stemmed tibial components between the two BMI groups (p = 0.162). Among all participants, 105 (29.7%) received a short-stemmed component, with a similar distribution in both groups (59 in the low BMI group and 46 in the high BMI group).
Among this population, 350 cases presented without loosening, while a minority of 4 did. One of these cases had a BMI below 30, while three had a BMI above 30. However, none of these differences yielded statistically significant results (p = 0.623).
Additionally, a small number of cases reported various complications, including tibial pain (6 cases), post-surgical infectious complications (12 cases), periprosthetic fractures (2 cases), rigidity after surgery (6 cases), Surgical site complication (10 cases), and joint instability (5 cases) (Table 3).
Table 3.
Summary of prosthesis characteristics and complications
| Characteristic | Cases (n) | BMI ≤ 30 (n) | BMI > 30 (n) |
|---|---|---|---|
| Total Cases | 354 | 177 | 177 |
| Tibial Pain | 6 | 2 | 4 |
| Post-surgical Infectious Complications | 12 | 5 | 7 |
| Periprosthetic Fractures | 2 | 1 | 1 |
| Rigidity After Surgery | 6 | 2 | 4 |
| Surgical site complication | 10 | 3 | 7 |
| Joint Instability | 5 | 1 | 4 |
The post hoc power analysis calculated for overall complications after TKA was 68%. It’s important to acknowledge that post-hoc power analyses provide an estimate of achieved power based on observed effect sizes, and may not be as reliable as a priori power calculations.
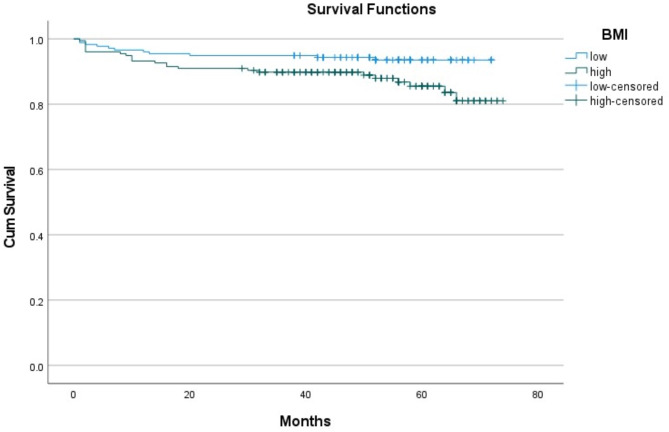
Kaplan-Meier survival analysis demonstrated a mean survival time free from any postoperative complication for the high BMI cohort of 66.2 months (95% CI: 63.3–69.2) compared to 68.3 months (95% CI: 66.2–70.5) in the low BMI cohort (Fig. 1). Results of the Log Rank test demonstrated a statistically significant difference (p = 0.02) between the Kaplan-Meier survival curves over time, indicating a longer survival free from complications in the low BMI cohort.
Fig. 1.
Kaplan-Meier survival curve comparing survival free from postoperative complications between high BMI and low BMI cohorts
Discussion
TKA is known as a highly effective surgical intervention for managing degenerative knee osteoarthritis and improving patients’ quality of life [18]. However, despite its benefits, concerns remain regarding the durability of prosthetic implants and the potential for complications, particularly aseptic loosening [19].
Aseptic loosening, a leading cause of revisions in TKA, results from various factors including patient-related factors, prosthesis design, surgical techniques, and other factors [20]. Among the patient-related factors, obesity stands out as a condition not only associated with an increased prevalence of degenerative knee osteoarthritis but also with a potentially heightened risk of aseptic loosening, as supported by some previous studies [3, 21]. However, other studies have reported different results and did not find a significant association between obesity and the increased risk of aseptic loosening, and this has caused ambiguities and disagreement in this field [10].
Given the growing prevalence of obesity worldwide and the critical role of patient selection for successful TKA outcomes, this study investigates the potential association between obesity and aseptic loosening in TKA [22].
While we identified four cases of aseptic loosening among the 354 participants, the anticipated association between a BMI above 30 and a higher incidence of aseptic loosening did not reach statistical significance. This finding suggests that BMI may not be the sole or primary factor influencing aseptic loosening, highlighting the multifactorial nature of this complication.
We also investigated the influence of tibial component design on aseptic loosening. All of the loosened components were stemless tibial components, but the difference was not statistically significant. This finding aligns with some prior research [23]. This outcome may also suggest that routinely using a short-stemmed tibial component could be a form of overtreatment solely based on the patient’s high BMI.
It’s important to acknowledge that the study’s post-hoc power analysis was lower than 80%, which might have limited our ability to detect an effect of the observed size.
Our study contributes to the growing knowledge of aseptic loosening in TKA, particularly regarding the limited role of BMI as a sole predictor. The multifactorial nature of this complication necessitates a comprehensive approach to its prevention and management. Future research could explore the combined effects of high BMI with biomechanical analyses that might influence susceptibility to aseptic loosening.
Certain limitations existed in this study, including a relatively limited sample size which limits the generalizability of the findings, the exclusive focus on a single medical center which might introduce a selection bias, and its retrospective design which inherently carries the risk of unmeasured confounding variables such as preoperative life style and activity level.
Future research studies may benefit from larger sample sizes, and multicenter cohorts to further elucidate the role of BMI in aseptic loosening. Additionally, prospectively investigating the interaction between BMI and other patient-related factors may offer valuable insights into the complexities of this complication.
Conclusion
Our study underscores the importance of considering multiple factors in the assessment of aseptic loosening risk in TKA patients. While BMI remains a noteworthy contributor, it is but one piece of a puzzle surrounding this complication.
Acknowledgements
The authors appreciate the support of all colleagues and instituitions who made this study possible.
Abbreviations
- TKA
Total knee arthroplasty
- BMI
Body Mass Index
- WHO
World Health Organization
- MPTA
Medial proximal tibial angle
- JCA
Joint convergence angle
- PJI
Prosthetic Joint Infections
- LDFA
Lateral distal femoral angle
- VA
Varus alignment
- KSRES
Knee Society Roentgenographic Evaluation and Scoring System
Author contributions
Seyyed Mohammad Javad Mortazavi and Mohammad Ayati Firoozabadi conceptualized and designed the study. Amir Hossein Mafi, Shahabaldin Beheshti Fard, and Ali Bozorgsavoji collected the data. Sina Afzal drafted the initial manuscript. Sina Afzal and Homayoon Khaledian analyzed the data. Mohammad Ayati Firoozabadi and Sina Azadnajafabad performed the final revision. All authors approved the final version of the manuscript for publication.
Funding
This study received no funding support.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was conducted per the Declaration of Helsinki and the study protocol was reviewed and approved by the Research Ethics Committee of Tehran University of Medical Sciences (code: IR.TUMS.IKHC.REC.1400.265). The patient was informed of the study, and provided the written informed consent prior to decision for publication of the results.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Jorgensen NB, McAuliffe M, Orschulok T, Lorimer MF, de Steiger R. Major aseptic revision following total knee replacement: a study of 478,081 total knee replacements from the Australian Orthopaedic Association National Joint Replacement Registry. JBJS. 2019;101(4):302–10. [DOI] [PubMed] [Google Scholar]
- 2.Gothesen O, Lygre SHL, Lorimer M, Graves S, Furnes O. Increased risk of aseptic loosening for 43,525 rotating-platform vs. fixed-bearing total knee replacements: a Norwegian–Australian registry study, 2003–2014. Acta Orthop. 2017;88(6):649–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schiffner E, Latz D, Thelen S, Grassmann JP, Karbowski A, Windolf J, et al. Aseptic loosening after THA and TKA - do gender, tobacco use and BMI have an impact on implant survival time? J Orthop. 2019;16(3):269–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buller LT, Rao V, Chiu Y-F, Nam D, McLawhorn AS. Primary Total Knee Arthroplasty Performed Using High-Viscosity Cement is Associated with higher odds of revision for aseptic loosening. J Arthroplast. 2020;35(6):S182–9. [DOI] [PubMed] [Google Scholar]
- 5.Organization WH. Global database on Body Mass Index: BMI Classification. 2006. World Health Organization: Geneva, Switzerland. 2015.
- 6.Wendelboe AM, Hegmann KT, Biggs JJ, Cox CM, Portmann AJ, Gildea JH, et al. Relationships between body mass indices and surgical replacements of knee and hip joints. Am J Prev Med. 2003;25(4):290–5. [DOI] [PubMed] [Google Scholar]
- 7.Abdel MP, Bonadurer GF III, Jennings MT, Hanssen AD. Increased aseptic tibial failures in patients with a BMI ≥ 35 and well-aligned total knee arthroplasties. J Arthroplast. 2015;30(12):2181–4. [DOI] [PubMed] [Google Scholar]
- 8.Parratte S, Ollivier M, Lunebourg A, Verdier N, Argenson JN. Do stemmed Tibial Components in total knee arthroplasty improve outcomes in patients with obesity? Clin Orthop Relat Res. 2017;475(1):137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parratte S, Ollivier M, Lunebourg A, Verdier N, Argenson JN. Do stemmed Tibial Components in total knee arthroplasty improve outcomes in patients with obesity? Clin Orthop Relat Research®. 2017;475(1):137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cherian JJ, Jauregui JJ, Banerjee S, Pierce T, Mont MA. What host factors affect aseptic loosening after THA and TKA? Clin Orthop Relat Research®. 2015;473(8):2700–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naziri Q, Issa K, Malkani AL, Bonutti PM, Harwin SF, Mont MA. Bariatric orthopaedics: total knee arthroplasty in super-obese patients (BMI > 50 kg/m2). Survivorship and complications. Clin Orthop Relat Research®. 2013;471(11):3523–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Durig N, Pace T, Broome B, Osuji O, Harman MK. Clinical outcomes of tibial components with modular stems used in primary TKA. Adv Orthop. 2014;2014. [DOI] [PMC free article] [PubMed]
- 13.Scott CEH, Biant LC. The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br Volume. 2012;94–B(8):1009–15. [DOI] [PubMed] [Google Scholar]
- 14.Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop. 2014;38(2):273–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ho JPY, Merican AM, Ayob KA, Sulaiman S-H, Hashim MS. Tibia vara in asians: myth or fact? Verification with three-dimensional computed tomography. J Orthop Surg. 2021;29(1):2309499021992618. [DOI] [PubMed] [Google Scholar]
- 16.Xie T, Jiao X, Yao X, Li Z, An S, Cao G. How much the leg length has changed after the MOUKA through measurement of the full length radiographs? Beware of splicing error. BMC Musculoskelet Disord. 2023;24(1):343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Research®. 1989;248:9–12. [PubMed] [Google Scholar]
- 18.Uivaraseanu B, Vesa CM, Tit DM, Abid A, Maghiar O, Maghiar TA, et al. Therapeutic approaches in the management of knee osteoarthritis (review). Exp Ther Med. 2022;23(5):328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menken LG, Fleuriscar J, Weiner T, Berliner ZP, Rodriguez JA. Aseptic Tibial Implant Loosening after total knee arthroplasty: Preventable? J Am Acad Orthop Surg. 2021;29(8):326–30. [DOI] [PubMed] [Google Scholar]
- 20.Stotter C, von Roth P. [Diagnosis of loosening after knee arthroplasty]. Orthopade. 2021;50(12):972–8. [DOI] [PubMed] [Google Scholar]
- 21.Longawa L, Buller LT, Ziemba-Davis M, Meneghini RM. Incidence and Causes of Tibial Component Loosening Based on Level of Obesity in a Large Consecutive Cohort of Cemented Primary TKAs without Stem Extensions. Proceedings of IMPRS. 2020;3(1).
- 22.Nicholls A, Kiran A, Javaid MK, Hart D, Spector T, Carr A, Arden N. Change in body mass index during middle age affects risk of total knee arthoplasty due to osteoarthritis: a 19-year prospective study of 1003 women. Knee. 2012;19(4):316–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elcock KL, MacDonald DJ, Clement ND, Scott CEH. Total knee arthroplasty in patients with severe obesity: outcomes of standard keeled tibial components versus stemmed universal base plates. Knee Surg Relat Res. 2023;35(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.