Abstract
Objective
To determine the fears and myths related to blood donation in future health care workers.
Study Design
Cross-sectional study.
Place and Duration of Study
This study was carried out from October to December 2022 at the National University of Medical Sciences (NUMS), Rawalpindi, Pakistan. Donors were selected according to the, WHO recommended, Safe Blood Transfusion Program of Pakistan criteria.
Results
In total, 411 participants were included in the study. The individuals were 21–24 years of age, with a mean age of 21 years. In our study, females dominated (232/411); the remaining 179 were males. Out of the total 411, 145 participants had previously donated blood while the other 266 had never donated blood. Our study analyzed both of these groups. The most common symptoms experienced by blood donors were dizziness, post-donation weakness, and bodily aches and pains. Most non-donors feared problems related to their general health (42.3%) and developing infections (12.7%). P-value was 0.002, which reveals a significant association between fears and intention to donate blood.
Conclusion
These results suggest that fears and concerns related to blood donation play a leading role in forecasting donors’ attitudes and intentions. Motivation leads to inspiration and potential donors can be motivated by addressing their fear.
Keywords: blood donation, fears, myths, healthcare workers
Introduction
According to the World Health Organization, the overall rate of blood donation is 31.5 donations in high-income countries, 16.4 donations in upper-middle-income countries, 6.6 donations in lower-middle-income countries, and 5.0 donations in low-income countries.1 Although, in developed countries, blood management initiatives have successfully managed to decrease the demand for blood products, recent global environmental and biological changes have increased demand for blood and blood products.2 This was especially the case during the COVID-19 pandemic and Dengue fever outbreaks in our resource-strained country.3 The demand for blood components like fresh frozen plasma and platelets has increased markedly; thus, encouraging and improving the recruitment and retention of donors remains a high priority.4 This could be because of increases in the size of the general population, elderly individuals, hematological malignancies, and road traffic accidents.5
Young medical students, who are the healthcare workers of the future, should be motivated to donate blood because they are well aware of the misery patients experience.6 In this study we wanted to identify and document the reasons why some of them do not donate blood. Worldwide, advertising campaigns emphasize the positive aspects of donating while minimizing any possible negative aspects and busting the myths associated with it.7 To boost recruitment of blood donors, it is important to address the negative aspects directly.8 In developed countries, donors are unpaid volunteers; in contrast, developing countries have limited supplies so people only donate blood when a family member or friend needs it.9
Blood donation is associated with different variables like fear of needle prick, blood-borne diseases, and vasovagal reactions, and issues related to donor recruitment and retention.10 This study was done to assess medical students’ awareness of the need for blood, the donation process, and the impact of their donations on the community. It also explored the attitude of students towards blood donation so as to provide insights into their perceptions and beliefs. Investigating the reasons why some students choose not to donate blood is essential. Common barriers could include fear, lack of time, or concerns about health implications.11 Addressing these reasons can help in developing strategies to overcome these barriers.
Materials and Methods
A cross-sectional study was conducted at the department of Pathology, National University of Medical Sciences, Rawalpindi for a duration of three months, i.e. from October to December 2022. A non-probability consecutive sampling technique was used. Medical and dental undergraduate students attending the National University of Medical Sciences, aged between 21 and 24 years, were included in the study. Students not willing to participate in the study were excluded. Incompletely filled forms were also rejected. The sample size was approximately 411 participants.12 The study was approved by the ethics review committee of the National University of Medical Sciences. Our study complied with the tenets of the Declaration of Helsinki. Informed consent was obtained from all students who took part. Donors were selected according to the WHO recommended Safe Blood Transfusion Program. A detailed history was taken from the students by means of proformas completed by them. The proforma included demographic data such as students’ age and gender, history of blood donation, and donation by family members; the time interval between blood donations was also noted. Their responses were stated as yes/no. In our blood collection center, donors are selected according to the WHO criteria that they bleed; components are prepared followed by hemovigilance. In the case of blood donation, a history of headache, dizziness, palpitations, anxiety, vasovagal syncope, post-donation weakness and bodily aches and pains were noted on the proforma. If there was no history of blood donation, then any cultural issues or fears related to needle prick, contacting infections, or problems related to general health were noted. The proforma also included questions related to myths about blood donation, such as fear of weight gain, specific diet plans, or contracting diseases, or any recent vaccinations that might halt the blood-donation process. Statistical analysis was done using SPSS version 22. Descriptive statistics were used for gender distribution; for age, a percentage was calculated. Associations among gender and blood donations were determined using the chi-square test. A chi-square test was also used to evaluate the association of each student’s response with their blood donation status. A p-value of ˂ 0.05 was considered to be statistically significant.
Results
A total of 411 students participated in the study. The students were 21 to 24 years of age, with a mean age of 21 years. In our study females dominated (232/411). Out of the total 411 students, 143 had previously donated blood while 268 students had never donated blood. In our study, we analysed both groups. We were interested to know whether the participants who had donated blood experienced any post-donation symptoms and, if so, what was the most common symptom they experienced. Of all participants, 270 had family members who were also donors. (See Tables 1–9 and Figure 1.)
Table 1.
Time Interval Between Blood Donations
| Sr. No | Time period | N (%) |
|---|---|---|
| 1 | 1 year | 17 (4.1) |
| 2 | 2 months | 7 (1.7) |
| 3 | 2 years | 8(1.9) |
| 4 | 3 months | 14 (3.4) |
| 5 | 4 months | 6 (1.5) |
| 6 | 5 months | 8 (1.9) |
| 7 | 6 months | 32 (7.8) |
| 8 | 0 | 305 (74.2) |
| 9 | Once | 14 (3.4) |
Table 2.
Following Blood Donation, Symptoms Experienced by Donors
| Sr. No | Symptoms | N (%) |
|---|---|---|
| 1 | Headache | 26 (17.1) |
| 2 | Dizziness | 49 (32.2) |
| 3 | Palpitations | 10 (6.6) |
| 4 | Anxiety | 13 (8.6) |
| 5 | Vasovagal syncope | 5 (3.3) |
| 6 | Post-donation weakness, bodily aches and pains | 49 (32.2) |
| Mean+SD | 3.45+1.986 | |
Table 3.
Reasons for Not Donating Blood
| Sr. No | Reasons | N (%) |
|---|---|---|
| 1 | Cultural issues | 5 (1.2) |
| 2 | Fear of needle prick | 37 (9.0) |
| 3 | Fear of contracting infections | 52 (12.7) |
| 4 | Fear of problems related to general health | 174 (42.3) |
Table 4.
Influencing Factors
| Sr. No | Do you think that your decision regarding blood donation can be influenced by the following factors: | N (%) |
|---|---|---|
| 1 | You are on any type of medication (multivitamins/antibiotics)? | 53 (12.9) |
| 2 | Fear of weight gain? | 42 (10.2) |
| 3 | If you are on specific diets? | 28 (6.8) |
| 4 | Any active disease? | 155 (37.7) |
| 5 | If you have received any type of vaccine recently? | 41 (10) |
Table 5.
Association Between Previous History of Blood Donation and Gender (Significance)
| Previous history of blood donation | P-value | ||
|---|---|---|---|
| Yes | No | ||
| Male | 98 (54.7%) | 81 (45.3%) | 0.000 |
| Female | 47 (20.3%) | 185 (79.7%) | |
Table 6.
Association Between History of Donation in Family Members and Gender (Significance)
| History of donation in family members | P-value | ||
|---|---|---|---|
| Yes | No | ||
| Male | 105 (59.7%) | 71 (40.3%) | 0.023 |
| Female | 161 (69.7%) | 70 (30.3%) | |
Table 7.
Associations Between Gender, History of Donation in Family Members, and Previous History of Blood Donation
| Following blood donation, have you ever experienced the following symtoms? | P-value | |||||||
|---|---|---|---|---|---|---|---|---|
| Headache | Dizziness | Palpitations | Anxiety | Vasovagal syncope | Post-donation weakness, bodily aches, and pains | |||
| Gender | Male | 17 (20.5%) | 22 (26.5%) | 6 (7.2%) | 8 (9.6%) | 0 (0) | 30 (36.1%) | 0.066 |
| Female | 9 (13.0%) | 27 (39.1%) | 4 (5.8%) | 5 (7.2%) | 5 (7.2%) | 19 (27.5%) | ||
| History of donation in family members | Yes | 16 (15.7%) | 34 (33.3%) | 5 (4.9%) | 8 (7.8%) | 3 (2.9%) | 36 (35.3%) | 0.670 |
| No | 10 (20.4%) | 14 (28.6%) | 5 (10.2%) | 5 (10.2%) | 2 (4.1%) | 13 (26.5%) | ||
| Previous history of blood donation | Yes | 21 (21.4%) | 24 (24.5%) | 6 (6.1%) | 5 (5.1%) | 4 (4.1%) | 38 (38.8%) | 0.006 Significant |
| No | 5 (9.3%) | 25 (46.3%) | 4 (7.4%) | 8 (14.8%) | 1 (1.9%) | 11 (20.4%) | ||
Table 8.
Association Between Previous History of Blood Donation & Gender with Reasons for Not Donating Blood (1st Significant & 2nd Not Significant)
| Religious issues | Fear of needle prick | Fear of contracting infections | Fear of general health-related problems | P-value | ||
|---|---|---|---|---|---|---|
| Previous history of blood donation | Yes | 1 (0.7%) | 9 (6.2%) | 17 (11.7%) | 39 (26.9%) | 0.000 |
| No | 4 (1.5%) | 28 (10.5%) | 35 (13.2%) | 135 (50.8%) | ||
| Gender | Male | 3 (1.7%) | 14 (7.8%) | 20 (11.2%) | 68 (38%) | 0.0141 |
| Female | 2 (0.9%) | 23 (9.9%) | 32 (13.8%) | 106 (45.7%) | ||
Table 9.
Association Between Previous History of Blood Donation and Gender: Do You Think That Your Decision Regarding Blood Donation Can Be Influenced by the Following Factors (1st Not Significant and 2nd iSignificant)?
| You are on any type of medication | Fear of weight gain | You are on a specific diet | You have an active disease | You have received any type of vaccine recently | P-value | ||
|---|---|---|---|---|---|---|---|
| Previous history of blood donation | Yes | 15 (10.3%) | 18 (12.4%) | 12 (8.3%) | 64 (44.1%) | 13 (9%) | 0.080 |
| No | 38 (14.3%) | 24 (9.0%) | 16 (6%) | 91 (34.8%) | 28 (10.5%) | ||
| Gender | Male | 13 (7.3%) | 22 (12.3%) | 19 (10.6%) | 60 (33.3%) | 20 (11.2%) | 0.002 |
| Female | 40 (17.2%) | 20 (8.6%) | 9 (3.9%) | 95 (40.9%) | 21 (9.1%) | ||
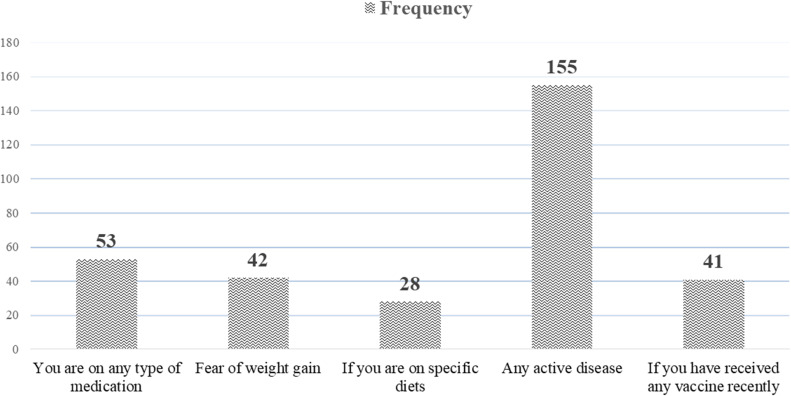
Figure 1.
Participant responses to questioning whether their decision regarding blood donation can be influenced.
Discussion
According to our hypotheses, stronger medical fears were associated with lower intention to donate blood; this effect was influenced by attitudes to donation as well as self-confidence (e.g. belief in one’s ability to manage fear).13 In terms of predictors of lower blood donation rates, blood-related fears were among the strongest, despite the fact that fear of needles and venipuncture pain are very noticeable and common concerns during blood donation, these fears strongly contribute to why fewer people donate blood.14 Seeing blood being drawn from your arm and accumulating in a large bottle was another source of fear.15 Some of these specific fears related to blood are most evident in existing literature, that is, predicting vasovagal reactions and other adverse responses.16 When compared to other medical treatments that also involve needles, like dental examinations and flu or other vaccinations, people may be less willing to donate blood because it does not positively impact their health.17
It was also noteworthy that students from families where blood donation was associated with less medical fear and who had a blood-dependent patient (with thalassemia, for example) and knew the misery they suffered donated blood more regularly than people who experienced a high level of fear related to their general health.18 Therefore, non-donors can improve their behaviour by first acknowledging their fears and then engaging with specific strategies such as reading material on educational websites and other recruitment materials, engaging in distraction, and making blood donation a normal process, thus boosting their self-confidence.19 The motivation of non-donors could be boosted by making the donation process less time-consuming, giving them a reward for donating, informing them that blood supplies are low or actually showing them transfusion-dependent patients getting better.20 Addressing blood-related fears is important for both clinics and promotional campaigns. Donation clinics should be advised to make the environment comfortable, avoid having blood bags and needles within full view, and educate donors with appropriate coping strategies (e.g. distraction or relaxing activities) to overcome their apprehension.21
The current findings in our study show that most of the donors were male and have donors in their family. Psychologically, fear reduction would improve attitudes towards blood donation. As a lower economic status country, donations are made by mostly repeat or paid donors. There are far fewer volunteer donors. Promotional campaigns could consider avoiding prompting blood-related fears (e.g. limiting images related to blood on relevant media) and providing some level of reassurance to eligible donors where possible.
The most common reason not to donate blood was fear of general health-related problems, fear of contracting infections because, in Pakistan, there are very few blood centers where all internationally recommended facilities are available. Offering reassurance and facilitating good quality services can increase the number of volunteer donors. Intention to donate is a consequence of attitude and self-efficacy. It is likely that donation history influences attitude, and attitude influences donation. Donors may be able to reconsider their thoughts, feelings, and attitudes. Acknowledging the fears of donors, especially blood drawing and blood-related fears, is critical to develop improved recruitment and retention strategies. Reducing the fears and boosting the self-confidence of potential donors may help improve donation intention. We have to improve our donor management services and maintain them according to international recommendations in order to establish a more stable blood supply.
Conclusion
Our results suggest that most people refrain from donating blood because of various fears and myths such as fear of needle prick, contracting infections, religious issues, health issues, headache, dizziness, weight gain, medications and active diseases. These fears and concerns related to blood donation play a major role in forecasting donor attitude and intention. Motivation leads to inspiration and potential donors can be motivated by addressing their fears.
Acknowledgment
Abstract published in International Society of Blood Transfusion (Vox Sanguinis), Volume 118, Issue S2, Abstracts of the 34th Regional ISBT Congress, Cape Town, South Africa 18–21 November 2023 (pp. 77–78).
Funding Statement
No funding was received for this study.
Disclosure
The authors have disclosed no conflicts of interest.
References
- 1.World Health Organization. Global status report on blood safety and availability. 2021.
- 2.Allain JP. Current approaches to increase blood donations in resource‐limited countries. Transfus Med. 2019;29(5):297–310. doi: 10.1111/tme.12629 [DOI] [PubMed] [Google Scholar]
- 3.Thijsen A, Masser B, Davison TE, van Dongen A, Williams LA. Beyond fear: a longitudinal investigation of emotions and risk of a vasovagal reaction in first‐time whole‐blood donors. Transfusion. 2023;63(1):163–170. doi: 10.1111/trf.17169 [DOI] [PubMed] [Google Scholar]
- 4.Estcourt LJ. Why has demand for platelet components increased? A review. Transfus Med. 2014;24(5):260–268. PMID: 25327286. doi: 10.1111/tme.12155 [DOI] [PubMed] [Google Scholar]
- 5.Klinkenberg EF, Fransen MP, de Kort WL, van Weert JC, Huis EM. Blood donation among individuals of African origin in the Netherlands: how are barriers and motivators associated with intention? Blood Transfus. 2021;19(1):24. doi: 10.2450/2020.0049-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guglielmetti Mugion R, Pasca MG, Di Di Pietro L, Renzi MF. Promoting the propensity for blood donation through the understanding of its determinants. BMC Health Serv Res. 2021;21(1):1–20. doi: 10.1186/s12913-021-06134-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enawgaw B, Yalew A, Shiferaw E. Blood donors’ knowledge and attitude towards blood donation at North Gondar district blood bank, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):1–6. doi: 10.1186/s13104-019-4776-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salazar-Concha C, Ramírez-Correa P. Predicting the intention to donate blood among blood donors using a decision tree algorithm. Symmetry. 2021;13(8):1460. doi: 10.3390/sym13081460 [DOI] [Google Scholar]
- 9.Saltzmann C, Boenigk S. On consciousness of the decision to discontinue blood donation: intention to return and effective recovery activities. Transfus Med. 2022;32(3):193–209. doi: 10.1111/tme.12859 [DOI] [PubMed] [Google Scholar]
- 10.Greffin K, Schmidt S, Schönborn L, Muehlan H. “Blood for blood”? Personal motives and deterrents for blood donation in the German population. Int J Environ Res Public Health. 2021;18(8):4238. doi: 10.3390/ijerph18084238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang L, Yao M, Liu H, Zheng S. The effect of functional motivation on future intention to donate blood: moderating role of the blood donor’s stage. Int J Environ Res Public Health. 2021;18(17):9115. doi: 10.3390/ijerph18179115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohanty N, Biswas SN, Mishra D. Message framing and perceived risk of blood donation. J Nonprofit Public Sect Mark. 2023;35(2):165–193. doi: 10.1080/10495142.2021.1959488 [DOI] [Google Scholar]
- 13.Gilchrist PT, Masser BM, Horsley K, Ditto B. Predicting blood donation intention: the importance of fear. Transfusion. 2019;59(12):3666–3673. doi: 10.1111/trf.15554 [DOI] [PubMed] [Google Scholar]
- 14.Kassie A, Azale T, Nigusie A. Intention to donate blood and its predictors among adults of Gondar city: using theory of planned behavior. PLoS One. 2020;15(3):e0228929. doi: 10.1371/journal.pone.0228929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melián-Alzola L, Martín-Santana JD. Service quality in blood donation: satisfaction, trust and loyalty. Serv Bus. 2020;14(1):101–129. doi: 10.1007/s11628-019-00411-7 [DOI] [Google Scholar]
- 16.Duh HI, Dabula N. Millennials’ socio-psychology and blood donation intention developed from social media communications: a survey of university students. Telematic Inf. 2021;58:101534. doi: 10.1016/j.tele.2020.101534 [DOI] [Google Scholar]
- 17.Zakarevičiūtė B, Juodžentė D, Karvelienė B, Riškevičienė V. Awareness, motivation, and fear towards canine blood donation—a survey of dog owners in Lithuania. Animals. 2021;11(11):3229. doi: 10.3390/ani11113229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaafar JR, Kamarudin NH, Zakaria NH, Seong KW. Empowering humanity behavior among university students through blood donation activity. Malays J Soc Sci Humanit. 2023;8(1):e002097. doi: 10.47405/mjssh.v8i1.2097 [DOI] [Google Scholar]
- 19.Hossain MS, Siam MH, Hasan MN, Jahan R, Siddiqee MH. Knowledge, attitude, and practice towards blood donation among residential students and teachers of religious institutions in Bangladesh–A cross-sectional study. Heliyon. 2022;8(10):e10792. doi: 10.1016/j.heliyon.2022.e10792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mugion RG, Giovina PM, Laura DP, Renzi MF. Promoting the propensity for blood donation through the understanding of its antecedents. 2020.
- 21.Yeung VW, Tam PC, Yau EK. The relative effectiveness of Altruistic vs. Egoistic messages in influencing non-donors’ intention to donate blood in Hong Kong. J Soc Psychol Res. 2022;23:97–110. [Google Scholar]