Abstract
The increasing demand for disease modeling, preclinical drug testing, and long waiting lists for alternative organ substitutes has posed significant challenges to current limitations in organoid technology. Consequently, organoid technology has emerged as a cutting-edge tool capable of accurately recapitulating the complexity of actual organs in physiology and functionality. To bridge the gaps between basic research and pharmaceutical as well as clinical applications, efforts have been made to develop organoids from tissue-derived stem cells or pluripotent stem cells. These developments include optimizing starting cells, refining culture systems, and introducing genetic modifications. With the rapid development of organoid technology, organoid composition has evolved from single-cell to multi-cell types, enhancing their level of biomimicry. Tissue structure has become more refined, and core challenges like vascularization are being addressed actively. These improvements are expected to pave the way for the construction of organoid atlases, automated large-scale cultivation, and universally compatible organoid biobanks. However, major obstacles remain to be overcome before urgently proof-of-concept organoids can be readily converted to practical applications. These obstacles include achieving structural and functional summarily to native tissue, remodeling the microenvironment, and scaling up production. This review aims to summarize the status of organoid development and applications, highlight recent progress, acknowledge existing limitations and challenges, and provide insights into future advancements. It is expected that this will contribute to the establishment of a reliable, scalable, and practical platform for organoid production and translation, further promoting their use in the pharmaceutical industry and regenerative medicine.
Keywords: Organoid, Up-scaling, Expansion, Disease modeling, Transplantation, Bioreactor, Gene-editing, Universal biobanking, Induced pluripotent stem cells, Somatic stem cells
Introduction
With recent technological advances, organoids have emerged as the leading in vitro model for the detailed exploration of the molecular landscape of human organs. This advancement enables in-depth and systematic dissection of human biological systems and disease mechanisms, accelerating drug discovery and the development of therapeutic strategies. Organoids are in vitro organ substitutes generated exclusively from either somatic stem cells (SSC) or pluripotent stem cells (PSCs) through self-organization, which forms a complex three-dimensional (3D) architecture with physiological features that closely resemble native organs. These features make organoid models more accessible and practical compared to animal models, providing deeper insights into organ biology and the progression of related disease development (Rossi, Manfrin & Lutolf, 2018).
Organoids derived from SSCs are biocompatible with the host tissue or organ, making them convenient sources, particularly for autologous transplantation. However, SSCs present practical challenges, including difficulties in separation and purification, as well as limited capacity for in vitro expansion and lineage differentiation. As an alternative, PSC-derived induced pluripotent stem cells (iPSCs) offer significant potential for broad applications due to their theoretically permanent replication power (Cao et al., 2021). More importantly, their unique multilineage differentiation potential allows the generation of multiple organ-forming cell components, enabling the reconstruction of vascularized multicellular organoids with neuroendocrine (Lamers et al., 2021) and immune systems (Xu et al., 2018) under specific differentiation and co-culture protocols. These organoids can mimic the physiological compositions and functions of native organs, expanding their potential for pharmacological and therapeutic application (Takebe et al., 2017). However, preparing individual cell types remains time-consuming, labor-intensive, and impractical for widespread use. Recently, gene editing has enabled a single initial PSC population to differentiate into multiple cell composition under pre-designed gene network regulation, ultimately forming engineered tissue with expansion capabilities. Although still in its early stages, this breakthrough offers important insights for constructing a more efficient, labor-reduced, and scalable organoid production system.
In the past 20 years, emerging evidence has shown that organ-like substitutes can recapitulate human pathologies, offering breakthroughs in disease modeling and drug development (Rossi, Manfrin & Lutolf, 2018). Several pioneering studies have demonstrated that patient-derived organoids could mimic the genetic and pathological features of the original diseased tissue (Dekkers et al., 2013; Dutta, Heo & Clevers, 2017; Huch et al., 2015; Lancaster et al., 2013; Nie et al., 2018a; Ouchi et al., 2019; Zhou et al., 2017). More recently, gene modification techniques, such as CRISPR/Cas9, have enabled the use of organoids from healthy donors to establish disease models including cancer (Matano et al., 2015; Sun et al., 2019). Proof-of-concept studies also suggest that organoids can serve as alternative grafts for regenerative medicine, helping to rescue or recovery damaged issues (Nie et al., 2018b; Shirai et al., 2016), offering new hope for treating previously incurable diseases. However, variations in cell sources and protocols between research groups lead to differences in organoid structure and function, affecting the accuracy and reproducibility of these reported disease models. This inconsistency is a major challenge for rapidly growing organoid industry (Rossi, Manfrin & Lutolf, 2018).
In recent years, expectations for the practical applications of organoids have grown steadily. However, this fulfillment relies greatly on critical breakthroughs in the reliability, reproducibility, and practicability of organoid generation. Therefore, the key challenges remain in bridging the gap between in vitro organoids and native organs, as well as translating laboratory studies into practical production and applications. This review summarizes recent progress in organoid generation, focusing on disease modeling and transplantation therapies. Simultaneously, we discuss challenges related to addressing architectural and functional complexity, enhancing maturation and establishing reproducible and scalable culture systems. Notably, we highlight advances in organoid atlases, automated cultures, and universally compatible iPSC-organoid biobanks, which could greatly improve drug development and personalized treatments in the future.
Survey Methodology
We searched PubMed for articles on trends and challenges in organoid modeling and expansion with pluripotent stem cells and somatic tissue. Keywords included “Organoid, up-scaling, expansion, disease modeling, transplantation, bioreactor, gene-editing, universal biobanking, induced pluripotent stem cells, somatic stem cells, three-dimension, multicellular organization, extracellular matrix” yielding over 8,000 results. The articles were screened individually to assess relevance to our research. After organizing and analyzing the results, we downloaded 240 literature reviews. Of these, 178 articles were cited in this review, while 62 articles were excluded as irrelevant. Most of the literature cited was published in the past decade. This review aims to serve as a reference for researchers working on organoid research and developing tools for drug screening and transplantation therapy using iPSC-derived multicellular organoids.
Current achievements
Here we summarize the current state of research on organoid production, the impact of co-culture systems, the in vitro microenvironment on organoid production, and current research hotspots in organoid culture. Additionally, we reviewed the current applications of organoids in disease modeling and their potential as disease therapeutic tools.
Organoid microenvironment simulation (multicellular organization and extracellular matrix)
Co-culturing isolated tissue stem cells or dissected tissue fragments is the principal strategy for generating SSC-derived organoids. Without additional modifications, such as gene editing, these organoids are relatively easy to manage and maintain, showing strong potential for mimicking adult tissue biology. Among pioneering studies, a single LGR5+ stem cell population was shown to reconstitute mouse and human intestines or liver organoids when cultured with defined niche factors (mainly growth factors and Matrigel) (Huch et al., 2015; Sato et al., 2009). Using single-cell sequencing, a novel protein C receptor-positive (Procr+) cell population was identified from an adult mouse pancreas, which robustly formed islet-like organoids when cultured at clonal density (Wang et al., 2020). Notably, these SSC-derived organoids could be expanded in a defined culture system without genome instability and could be differentiated into functional cells in vitro or upon transplantation in vivo (Huch et al., 2015; Wang et al., 2020). However, identifying SSC markers and isolating and purifying SSCs are often challenging and labor-intensive. In addition, SSCs exclusively produce organoids with a single epithelial population, lacking the complex multilineage compositions found in real organs, such as the vascular, immune, and nervous systems (Calandrini & Drost, 2021; Mohammadi et al., 2021). Although technically challenging, PSC-derived organoids are becoming more accessible and practical. With proper differentiation protocols, PSCs could develop into various desired cell types within specific tissues. Notably, complex multilineage organoid systems could be developed from a single PSC source, capturing cellular heterogeneity and interactions necessary to replicate the pathology of human organs (Silva et al., 2019). To date, multiple organoid types have been generated from PSCs (Table 1), demonstrating their wide-ranging applications.
Table 1. Summary for PSC or tissue derived organoids and their application.
| Organoid types | Initial cells | 3D culture: embedded in gel or suspended in a plate | Applications & Significance | Author(s),year |
|---|---|---|---|---|
| Liver | PHHs & liver NPCs | BME | Hepatotoxicity test | Messner et al., 2013 |
| hiPSCs | Matrigel | Generation of a vascularized and functional human liver bud from PSCs | Takebe et al., 2013 | |
| Patient liver cells | BME | Modelling of primary liver cancer | Broutier et al., 2017 | |
| hiPSCs | ULA plate | Modelling of liver development | Takebe et al., 2017 | |
| PMHs | ULA plate | Recapitulation of liver regeneration potential | Peng et al., 2018 | |
| PMH & PHH | Matrigel | Recapitulation of the proliferative damage-response of hepatocytes | Zilch et al., 2018 | |
| hiPSCs | ULA plate | Modelling of hepatitis B virus infection | Nie et al., 2018a | |
| hPSCs | Matrigel | Prediction of toxicity and the evaluation of drugs for hepatic steatosis | Mun et al., 2019 | |
| Patient liver cells | BME | Drug screening for anti-HBV activity and drug-induced toxicity | De Crignis et al., 2021 | |
| PHHs | Matrigel | High-throughput screening of chemical and food-derived compounds with anti-hyperuricemic bioactivity | Hou et al., 2022 | |
| hiPSCs | Matrigel | High-throughput | Shrestha et al., 2024 | |
| Pancreas | Mouse pancreatic epithelial cells | Matrigel | Modelling of pancreatic development | Huch et al., 2013 |
| Patient tumor cells | Matrigel | Modelling of pancreatic tumorigenesis | Boj et al., 2015 | |
| Mouse islet EpCAM+ cells | Matrigel | Rescuing streptozotocin (STZ)-induced diabetes in mice | Wang et al., 2020 | |
| hiPSCs | Matrigel | Rescuing streptozotocin (STZ)-induced diabetes in mice | Yoshihara et al., 2020 | |
| hPSCs | Matrigel | Modelling of the development of exocrine pancreas | Huang et al., 2021 | |
| hPSCs | Matrigel | Modelling of the development of hepato-biliary-pancreatic | Koike et al., 2019 | |
| Lung | hPSCs | Matrigel | Modelling of lung development | Dye et al., 2015 |
| hPSCs | Matrigel | Modelling of lung development | Miller et al., 2018 | |
| hPSCs | Matrigel | Modelling of fibrotic lung disease | Strikoudis et al., 2019 | |
| Patient pulmonary cells | Matrigel | Modelling of non-small cell lung cancer | Shi et al., 2020 | |
| Patient pulmonary cells | Matrigel | Prediction of the targeted and the chemotherapeutic drugs | Hu et al., 2021 | |
| hPSCs | ULA plate & Matrigel | Modelling of SARS-CoV-2 infection on lung | Han et al., 2021 | |
| hPSCs | Matrigel | Modeling fibrotic alveolar transitional cells | Ptasinski et al., 2023 | |
| Intestine | mASCs | Matrigel | Building crypt-villus structures in vitro without a mesenchymal niche | Sato et al., 2009 |
| hiPSCs | Matrigel | Modelling of human intestine development | Spence et al., 2011 | |
| hiPSCs | Matrigel | Modelling of congenital loss of intestinal enter-oe ndocrine cells | Fordham et al., 2013 | |
| hPSCs | Hydrogel | Repairing of intestinal injury | Cruz-Acuña et al., 2017 | |
| Patient intestinal cells | Matrigel | Testing of anti-inflammatory drugs | d’Aldebert et al., 2020 | |
| Patient intestinal cells | Matrigel | Drug screening for intestinal diseases | Cho et al., 2021 | |
| hPSCs | ULA plate & Matrigel | Modelling of SARS-CoV-2 infection on colon | Han et al., 2021 | |
| Patient intestinal cells | Matrigel | Modelling of Cronkhite-Canada Syndrome | Poplaski et al., 2023 | |
| Brain | mESCs | ULA plate | Modelling of the development of polarized cortical tissue | Eiraku et al., 2008 |
| hPSCs | ULA plate | Modeling of microcephaly | Lancaster et al., 2013 | |
| hPSCs | ULA plate | Modelling of neural development and disease progressing | Birey et al., 2017 | |
| Patient glioblastoma cells | ULA plate | Modelling of glioblastomas | Jacob et al., 2020b | |
| hPSCs | ULA plate | Modelling of SARS-CoV-2 infection on brain | Jacob et al., 2020a | |
| hiPSCs | Matrigel | Modelling of brain development | Gabriel et al., 2021 | |
| hiPSCs | Matrigel in a perfusion plate | Assessment of developmental neurotoxicity | Acharya et al., 2024 | |
| hiPSCs | Matrigel | Modeling of HIV-1 infection and NeuroHIV | Donadoni et al., 2024 | |
| Retina | hESCs | ULA plate & Matrigel | Modelling of optic cups and layered stratified neural retina development | Nakano et al., 2012 |
| hiPSCs | Geltrex | Modelling of retinal development | Xie et al., 2020 | |
| hESCs | ULA plate | Modelling of retinal development | Savoj et al., 2022 | |
| hiPSCs | ULA plate | Modelling of Alzheimer’s disease neuropathology | James et al., 2024 | |
| Skin | mPSCs | ULA plate | Modelling of skin diseases and revealing of hair follicle induction, hair growth | Lee et al., 2018 |
| hPSCs | ULA plate | Modelling of the cellular dynamics of developing human skin | Lee et al., 2020a | |
| hiPSCs | Matrigel | Testing of skin-related drugs | Ebner-Peking et al., 2021 | |
| Mouse epidermal cells | ULA plate | Modelling of self-organization into tissue patterns of stem cells in organoids | Lei et al., 2023 | |
| hiPSCs | ULA plate | Modelling of human skin development, disease and reconstructive surgeries | Shafiee et al., 2023 | |
| Kidney | Embryonic kidney cells | Cell pellet | Modelling of organotypic renal structures by self-organization | Unbekandt & Davies, 2010 |
| mESCs & hiPSCs | ULA plate | Modelling of kidney organogenesis | Taguchi et al., 2014 | |
| hiPSCs | Matrigel | Screening of nephrotoxicity | Takasato et al., 2015 | |
| Human kidney tubular epithelial cells | Matrigel & BME | Modelling of infectious, malignant and hereditary kidney diseases | Schutgens et al., 2019 | |
| Patient renal cells | Matrigel | Modelling of renal cancer | Grassi et al., 2019 | |
| hESCs | ULA plate | Modelling of flow-enhanced vascularization | Homan et al., 2019 | |
| Mouse ureteric bud progenitors | Matrigel | Modelling of congenital anomalies of kidney and urinary tract | Zeng et al., 2021 | |
| hiPSCs | Matrigel | Modeling of Fabry disease nephropathy | Cui et al., 2023 | |
| hiPSCs | Matrigel | Modeling of FAN1-deficient kidney disease | Lim et al., 2023 | |
| Bone | hPDCs | Agarose microwell | Rescue tibia defects of mice | Nilsson Hall et al., 2020 |
| hPSCs | Matrigel | Bone healing | Tam et al., 2021 | |
| PHOs | Matrigel | Modelling of skeletal development | Abraham et al., 2022 | |
| Human cartilage and bone tissues | Matrigel | Modeling of tissue development and disease | Abraham et al., 2022 | |
| BMSCs | Hydrogel | Rapid bone defect regeneration and recovery | Xie et al., 2022 | |
| Heart | hPSCs | Matrigel | Two pro-proliferative small molecules without detrimental impacts | Mills et al., 2019 |
| mESCs | Matrigel | Modelling of carcinogenesis | Lee et al., 2020b | |
| hESCs | ULA plate & Matrigel | Modelling of the development of early heart and foregut | Drakhlis et al., 2021 | |
| hPSCs | ULA plate | Modeling of cardiac development and congenital heart disease | Lewis-Israeli et al., 2021 | |
| hiPSCs | ULA dish & Matrigel | Recapitulate morphological/functional aspects of the heart | Lee et al., 2022 | |
| hPSCs | ULA plate | Modeling of syntheticheart development and cardiac disease | Volmert et al., 2023 |
Notes.
- BME
- basement membrane extract
- D
- dimensional
- ESC
- embryonic stem cell
- h
- human
- iPSC
- induced pluripotent stem cell
- m
- mouse
- NA
- not available
- PHCs
- primary human cholangiocytes
- NPCs
- non-parenchymal cells
- PHHs
- primary human hepatocytes
- PHOs
- primary human osteocytes
- PMHs
- primary mouse hepatocytes
- PSCs
- pluripotent stem cells (iPSC & ESC)
- ASCs
- adult stem cells
- ULA
- ultra-low attachment
Single-cell population organoids do not fully replicate the complexity of real organs because they lack native stromal cells and blood vessels, which are essential for tissue development and maturation (Yu, 2020). To recapitulate the multicellular interactions in the liver, initial attempts used human mesenchymal stem cells (MSCs) and umbilical vein endothelial cells (HUVECs) to substitute the liver’s intrinsic stromal components, such as hepatic stellate cells, and endothelial cells. This approach successfully established vascularized multicellular liver organoids through self-cell sorting and architectural rearrangements, and these organoids exhibited enhanced liver function due to their multicellular system-autonomous endogenous signaling (Takebe et al., 2013). Subsequently, to avoid allogeneic cell source integration, the generation of liver parenchymal and major supportive cell lineages was induced from a single PSC. Interestingly, this all-iPSC-based multicellular organoid demonstrated a higher level of structural and functional similarity to primary liver tissue compared to the former model, suggesting that self-assembly with an autologous cell population may promote maturation in general, although the underlying mechanism remains to be clarified (Takebe et al., 2017).
However, organoids created by co-culturing separate pre-established cell types are considered structurally irregular and disordered compared to native organs, where multilineages are developed simultaneously. Moreover, the asynchronously developed aggregation may lack specific intercellular signal interactions found in tissues, which are essential for fully recapitulating biological functions. Therefore, multicellular co-development was recently achieved when gene editing was adopted. By precisely regulating gene networks through PROX1 and ATF5 overexpression and CYP3A4 activation, a single iPSC population can now develop into both liver parenchymal and nonparenchymal cell populations at the same time during cell aggregation. Importantly, these liver organoids were well vascularized, exhibited mature hepatic functions, and responded effectively to perturbations and feedback regulation (Velazquez et al., 2021). However, current multicellular organoid systems still face challenges. Notably, they lack immune cells and exhibit differences in cell distribution and ratios compared to natural organs, which vary depending on the protocols used in different laboratories (Ouchi et al., 2019; Velazquez et al., 2021). To improve organoid models, a deeper understanding of the multilineage developmental trajectories in a specific organ and the development of advanced gene editing tools are needed. This will help build precise cell types in organoids with faithful ratios, spatial distributions, and organization patterns.
Among in vitro culture environments, the extracellular matrix (ECM) may be the most crucial and adjustable factor that influences organoid features such as spatial architecture, growth, maturation, and even carcinogenesis. Matrigel is currently the most used natural ECM and is known for promoting organoid constitution and growth. However, its undefined composition and potential risks from immunogen and pathogen limit its clinical applications (Rossi, Manfrin & Lutolf, 2018). The development of designer matrices, particularly synthetic hydrogels with fine-tunable and controlled biophysical properties, has rapidly advanced in recent years. For instance, modular synthetic polyethylene glycol (PEG) hydrogels have been designed for culturing intestinal organoids. Notably, regulating the stiffness of the matrix backbone, known as mechanically dynamic system, researchers can influence the expansion, differentiation, and organogenesis of these organoids (Gjorevski et al., 2016). Subsequently, a composition-defined PEG-based hydrogel system was designed based on functional analysis of cellular adhesion in pancreatic cancer cells. This system revealed the functional role of critical ECM signaling in supporting both normal and cancerous pancreatic organoid growth (Below et al., 2022). Despite these efforts, identifying all the relevant ECM signaling molecules require for mimicking native tissue developmental trajectory or disease progression remains a major challenge. For this purpose, naturally derived matrices from decellularized tissues are being explored. An ECM hydrogel derived from decellularized porcine small intestine mucosa/submucosa was found to support the formation and growth of a wide range of endoderm-lineage organoids (Giobbe et al., 2019). In addition, several studies have identified the supportive roles of ECM from various tissues, including the liver (Zahmatkesh et al., 2021), pancreas (Bi et al., 2020), kidneys (Garreta et al., 2024) and brain (Simsa et al., 2021) in promoting the formation and maturation of PSC-organoids in specific germ layers. While the tissue ECM provides the most supportive and comprehensive signaling for organoid culture, closely mimicking the native microenvironment, the undefined compositions of these tissues necessitate thorough identification and rigorous biosafety verification before they can be used in clinical application.
Notably, the native organ microenvironment plays a crucial role in regulating the dynamic development of tissue homeostasis, regeneration, and pathogenesis, with each organ requiring a specific microenvironment. To address this, researchers have turned to microfluidic culture systems because of their advantages in miniaturization, integration, and low reagent consumption. These systems not only model the dynamic 3D in vivo microenvironment but also enable precise control of multiple parameters of the variables in the environment, such as the concentration gradient of the fluid shear stress. This allows for the creation of a controllable physiological environment for specific organoid development and maintenance (Jalili-Firoozinezhad, Miranda & Cabral, 2021). However, most established microfluidic culture systems cannot satisfy all the elements that make up a complex in vivo microenvironment. For example, while some reports have revealed the unique cellular organization, ECM composition, and signaling in organoids at specific growth or differentiation stages, aspects such as blood flow, oxygen, and metabolic exchange are often overlooked in most culture system designs. Combining the utility of 3D scaffolds, micropatterning, and advanced culture technologies such as organ-on-chip systems to more accurately mimic in vivo dynamics remains a significant challenge (Zhang et al., 2017). With optimized parameter design and intelligent controls, an integrated culture system would undoubtedly enhance the resemblance between organoids and native organs.
Applications of organoids (disease modeling and transplantation therapy)
Undoubtedly, ongoing research efforts to promote the structural and functional similarity between organoids and natural organs are aimed at realizing their vast potential for biomedical applications, particularly in drug testing and therapy. To some extent, in vitro models could recapitulate important aspects of human organs in physiology and pathology, providing a valuable tool for studying organ development, pathogenesis, and drug responses, areas that are difficult or impossible to explore directly in human subjects (Bock et al., 2021).
Challenges in cancer research and drug development is mainly due to their heterogeneity, including diverse mutational, epigenetic, and metabolic profiles, as well as the complexity of the tumor environment (McGranahan & Swanton, 2017). Tumor organoids, directly derived from patient-resected tumors and biopsies, offer a novel approach to capturing the original characteristics of tumors. They are considered more cost-effective and efficient compared to traditional animal models or patient-derived tumor xenografts. Pancreatic cancer is one of the most lethal malignancies owing to its late diagnosis and limited treatment option. To better understand the developmental cues of pancreatic tumorigenesis, patient-derived pancreatic organoids have been established as a tractable system to identify molecular and cellular characteristics at various stages of the disease. Both in vitro and transplantation experiments have confirmed a similar cluster of genes and pathways altered during disease progression, suggesting the faithfulness of this organoid model (Boj et al., 2015). In another study, a more detailed comparison between tumor and tumor-derived organoids were identified, including differentiation status, histoarchitecture, phenotypic heterogeneity, and patient-specific physiological changes. Notably, the observed correlation between tumors and their matched organoids in terms of sensitivity to histone methyltransferase EZH2 inhibitors highlights the potential of organoids for personalized drug screening and precise therapy. Moreover, the same group demonstrated these results using PSC-derived pancreatic tumors with mutations in KRAS and TP53 (Sun et al., 2019). Another group established human CRC tumor-derived organoids that well represent both morphological and molecular heterogeneities of original tumors. A robust organoid-based drug screening system was developed to efficiently identify repurposed drugs for CRC (Mao et al., 2024).Similarly, liver organoids generated from patients with Alagille syndrome were used to model in vivo pathology (Huch et al., 2015). Collectively, PSCs combined with gene editing largely broadens the organoid source, not limiting it to patient donors, and are particularly practical for establishing cancer models with defined mutation signatures.
Organoids have been extensively used for hereditary and infectious disease modeling. For instance, intestinal organoids generated from patients with cystic fibrosis, a disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR), were used for drug screening for individual patients (Dekkers et al., 2013). Similarly, liver organoids generated from patients with alpha-1-antitrypsin deficiency and Alagille syndrome have been used to model in vivo pathology (Huch et al., 2015). Extensive research has been conducted on these pathogens since the emergence of a new coronary pneumonia ailment. Lung organoids and brain organoids (Cakir et al., 2019; Velasco et al., 2019) have proven to be effective tools for studying SARS-CoV-2-related pathogenesis and treatment strategies. Brain organoids are also used to model microcephaly (Lancaster et al., 2013) and Zika infection (Zhou et al., 2017). Kidney organoids have significantly enhanced the capability to discover novel disease mechanisms and validate candidate drugs for clinical translation in polycystic kidney disease (PKD) (Liu et al., 2024). Many research groups, including ours, have explored the potential of hPSC-derived liver organoids to model hepatitis B virus (HBV) infection and steatohepatitis (Nie et al., 2018a; Ouchi et al., 2019). Our findings highlight the importance of using multicellular organoids to increase susceptibility to HBV infection, which is believed to be the key step in recapitulating the virus life cycle (Cao et al., 2021). Nevertheless, additional cellular components, such as immune cells, are required to create a more accurate modeling system. Another promising application of organoids is in the study of rare diseases, where CRISPR-based gene editing and patient-derived iPSCs offer a personalized approach to disease modeling, such as alpha-1-antitrypsin deficiency and Rett syndrome (Gomes et al., 2020; Gómez-Mariano et al., 2020). These models allow researchers to explore rare genetic conditions at the molecular level, often revealing new therapeutic strategies for diseases that were previously under-researched.
Organoids play a crucial role in drug metabolism and toxicology research by offering human-relevant models that simulate the absorption, distribution, metabolism, and excretion of drugs (Wang et al., 2021a). Liver organoids, which exhibit key drug-metabolizing enzymes such as cytochrome P450, provide a more accurate platform for predicting drug behavior in preclinical trials, improving the drug development pipeline. Additionally, liver and kidney organoids are increasingly used in toxicology studies to predict organ-specific toxicities. This approach reduces reliance on animal models and enhancing the precision of safety evaluations (Czerniecki et al., 2018; Zhang et al., 2023).
Functional organoids hold promise as alternative substitutes for transplantation in therapeutic strategies. Our group is among the first to perform the transplantation of multicellular PSC-derived liver organoids to treat liver damage in a mouse model. We confirmed the integration and maturation of these vascularized organoids within the host, and demonstrated that they could improve survival and liver function in mice with acute liver failure (ALF), providing a proof-of-concept regimen for treating severe or late-stage liver diseases (Nie et al., 2018b; Nie et al., 2018a). Importantly, our findings of in vivo environment-conducted organoid maturation were consistent with the results of another transplantation trial, in which cholangiocyte organoids displayed transcriptional diversity from primary human cholangiocytes after culture; furthermore, they could regain their in vivo signatures when transplanted back in their physiological position (Sampaziotis et al., 2021). Similarly, PSC-derived kidney organoids were found to induce neovascularization and significant maturation of glomeruli and tubules after subrenal transplantation (Hickey et al., 2019). ESCs- derived retinal organoids have been used to transplant organoid-derived RGCs into the murine eyes, achieving long-distance regeneration and functional connectivity remains a challenge (Rao et al., 2025). Despite the considerable potential of regenerative medicine, generating a sufficient number of high-quality organoids remains a significant challenge for most research groups.
Difficulties and challenges
Scaled culture system
Over the years, organoid culture systems have proven to be a revolutionary paradigm for drug development and regenerative medicine, but they have not yet been widely applied in the pharmaceutical and industrial fields. One major obstacle is the scalability and reproducibility. To amplify batch production, a microwell-array culture platform was initially proposed for massive organoid production in a single culture, with over 20,000 micro spots in a single well with an optimized size and space design, which would theoretically support a clinically relevant batch scale (>108 cells/batch). However, this production system did not resolve the substantial issues associated with scaling organoid quantities. Moreover, the labor-intensive and inefficient manual operation for iPSC differentiation and the co-culturing of multiple cell populations was barely feasible and reproducible for practical batch-to-batch applications (Cao et al., 2021).
Expanding the number of organoids in scaled culture systems is considered a more practical and effective strategy for organoid production. As listed in Table 2, various pioneering studies have shown that organoids derived from certain tissue-derived stem and fetal cells (especially from the liver) have long-term expansion capabilities in vitro, although their lifespan is often limited. As a promising source, PSC-derived organoids have demonstrated a more powerful expansion capability, with increasing achievements, including those in the endodermal layer (Akbari et al., 2019; Giobbe et al., 2019; Mun et al., 2019; Yamamoto et al., 2017). However, these seemingly promising results have common drawbacks. Organoids are exclusively cultured in Matrigel or tissue-derived hydrogel layers. This method hampers organoid manipulation and testing, as well as clinically relevant applications such as transplantation and post-tissue engineering. Additionally, the static culture system restricts timely material and signaling transport between organoids and the culture environment.
Table 2. Up-to-date strategies for organoid expansion of tissue derived cells from the three germ layers.
| Organoid types | Initial cells | 3D Expansion systems: Embedded in a gel or suspension in a plate | Expansion capability: Passage days/expansion duration | Medium and supplements | Author(s),year |
|---|---|---|---|---|---|
| Liver | hiPSC-Heps, HUVECs, hMSCs | Matrigel | 4–6 d/NA | EGM, HCM, dexamethasone, OSM, HGF | Takebe et al., 2013 |
| PMHs & PHHs | Matrigel | 7–10 d/>6 mo | AdDMEM/F12 medium, B27, N-Acetylcysteine, gastrin, RSPO1, Noggin, Wnt, EGF, FGF7, FGF10, HGF, TGFa, Nicotinamide, A83-01, CHIR99021, Y27632 | Hu et al., 2018 | |
| PHHs | BME gel | 7-10d/9–12 mo | AdDMEM/F12 medium, B27, N-Acetylcysteine, gastrin, RSPO1, Noggin, Wnt, EGF, FGF10, FGF19, HGF, Nicotinamide, A83-01, FSK, Y27632 | Artegiani et al., 2019 | |
| hiPSC-derived EpCAM+hepatic progenitors | Matrigel | 7d/3 mo | AdDMEM/F12 medium, B27, N-Acetylcysteine, gastrin, RSPO1, Noggin, Wnt, EGF, FGF10, HGF, Nicotinamide, A83-01, FSK, Y27632 | Akbari et al., 2019 | |
| hPSCs | Matrigel | 10d/17 d | AdDMEM/F12 medium, N2, B27, N-Acetylcysteine, gastrin, RSPO1, EGF, FGF10, HGF, Nicotinamide, A83-01, FSK | Mun et al., 2019 | |
| hPSCs transduced with PROX1, ATF5 and CYP3A4 | Matrigel | 48h/NA | APEL medium | Velazquez et al., 2021 | |
| hESCs & hiPSCs | Matrigel/ULA Plate | 5–6d/>48d | DMEM/F12 medium, GlutaMAX, HEPES, N2, B27, BSA, N-Acetylcysteine, gastrin, Nicotinamide, CHIR99021, FSK, FGF10, HGF, A03-01, R-spondin1, EGF | Kim et al., 2022 | |
| Patient liver cancer cells | Matrigel | 14–21d/NA | DMEM/F12, GlutaMAX, PS, N-Acetylcysteine, HEPES, EGF, FGF7, FGF10, HGF, Dex, Y27632 | Sun et al., 2024 | |
| Pancreas | Mouse adult duct cells | Matrigel | 7d/9mo | AdDMEM/F12 medium, B27, N-Acetylcysteine, gastrin, EGF, RSPO1, Noggin, FGF10, Nicotinamide | Huch et al., 2013 |
| Patient tumor cells | Matrigel | 7–8d/NA | AdDMEM/F12 medium, HEPES, GlutaMAX, PS, Primocin, N-Acetylcysteine, Wnt3a, RSPO1, Noggin, EGF, gastrin, FGF10, Nicotinamide, A83- 01 | Boj et al., 2015 | |
| Mouse islet EpCAM+cells | Matrigel | NA | DMEM/F12 medium, PS, B27, ITS, EGF, heparin, FGF2, VEGFa | Wang et al., 2020 | |
| hiPSCs | Matrigel | 6-7d/30d | 3D Kelco Gel Stem TeSR, FSK, dexamethasone, TGF- β RI kinaseinhibitor II/Alk5 inhibitor II, Nicotinamide, 3,3′,5-triiodo-l-thyronine sodium salt (T3), B27, R428, zinc sulfate, N-Cys | Yoshihara et al., 2020 | |
| hESCs & hiPSCs | Feeder cells | 3–5d/>11d | DMEM, B27, EGF, bFGF, 616452, I-BET151 | Ma et al., 2022 | |
| Patient pancreatic cancer cells | Matrigel | NA | DMEM/F12, HEPES, Glutamax, Primocin, A83–01, EGF, mNoggin, FGF10, Gastrin, N-Acetylcysteine, Nicotinamide, B27, R-spondin1 CM, Afamin/Wnt3A CM | Demyan et al., 2022 | |
| Colon | mASCs | Matrigel | 7–8d/NA | AdDMEM/F12 medium, Crypt culture medium, EGF, RSPO1, Noggin | Sato et al., 2009 |
| hPSCs | Matrigel | 13–14d/>140d | RPMI1640 media, dFBS-DMEM/F12, FGF4, Wnt3a, Activin A, RSPO1, Noggin, EGF, L-Glutamine, HEPES, N2, B27, PS | Spence et al., 2011 | |
| hiPSCs | Matrigel | NA/2mo | AdDMEM/F12 medium, GlutaMAX, HEPES, PS, B27, Y-27632, Streptomycin, Noggin, EGF, RSPO1, Wnt3a | Fordham et al., 2013 | |
| hPSCs | Hydrogel | 10–14d/40d | AdDMEM/F12 medium, N2, B27, HEPES, L-Glutamine, PS, Noggin, SB431542, FGF2, Sant-2, SU5402, SHH, SAG | Cruz-Acuña et al., 2017 | |
| hPSCs | Matrigel & ULA plate | 2–3d/6mo | DMEM/F12 medium, LDN193189, CHIR99021, EGF, B27, GlutaMAX, HEPES, PS | Han et al., 2021 | |
| Patient intestinal cells | Matrigel | NA | Wnt-3a or hAFM/Wnt-3a conditioned medium, RSPO1, Noggin, EGF, B27, N-Acetylcysteine, Nicotinamide, SB202190, A83-01, prostaglandin E2, gastrin, Primocin | Cho et al., 2021 | |
| Patient colon cancer cells | Matrigel | 7–10d/NA | DMEM/F12, GlutaMAX, PS, N-Acetylcysteine, HEPES, B27, Noggin, EGF, A83-01, gastrin, SB202190 | Parseh et al., 2022 | |
| Kidney | Mouse embryonic kidney cells | Cell pellet | NA | KCM, MEM, FBS, PS, Y27632, Glycyl-H1152, | Unbekandt & Davies, 2010 |
| mESCs & hiPSCs | ULA plate | 2 d/18d | IMDM, F12 medium, N2, B27, PS, BSA, glutamine, ascorbic acid, 1-thioglycerol | Taguchi et al., 2014 | |
| hiPSCs | Matrigel | 2–3d/3mo | APEL medium, CHIR99021, FGF9, bFGF, heparin | Takasato et al., 2015 | |
| hESCs | ULA plate | 2-3d/43d | DMEM/F12 medium, CHIR99021, FGF9, Noggin. Dorsomorphin | Homan et al., 2019 | |
| Patient renal cell carcinomas cells | Matrigel | 14–21d/NA | AdDMEM/F-12, Antibiotic-Antimycotic, GlutaMAX, HEPES, B-27, N-Acetylcysteine, Nicotinamide, SB202190, Y-27632, EGF | Li et al., 2022 | |
| Human fetal kidney cells | Matrigel | NA | Advanced DMEM, HEPES, Glutamax, Pen/Strep, B-27 supplement minus Vitamin A, N-acetylcysteine, R-spondin 1, EGF, A8301, CHIR99021, FGF10, GDNF, Heparin, LDN193189 dihydrochloride, Y27632 | Gerli et al., 2024 | |
| Brain | mESCs | ULA plate | NA/25d | DMEM/F12 medium, Neurobasal, pyruvate, 2-mercaptoethanol, Dkk-1, Lefty-1, Y27632, BMPRIA-Fc, SB431542, L-glutamine, B27 | Eiraku et al., 2008 |
| hPSCs | ULA plate | NA/10mo | DMEM/F12 medium, Neurobasal, N2, GlutaMAX, NEAA, Heparin, B27, 2-mercaptoethanol, insulin, retinoic acid | Lancaster et al., 2013 | |
| hPSCs | ULA plate | NA/>50d | DMEM/F12 medium, KSR, NEAA, GlutaMAX, 2-mercaptoethanol, PS, FGF2 | Birey et al., 2017 | |
| hPSCs | ULA plate | 2-3d/30d | Cortical differentiation medium, Glasgow-MEM, KSR, NEAA, pyruvate, 2-mercaptoethanol, PS | Velasco et al., 2019 | |
| hiPSCs | Matrigel | NA/>42d | DMEM/F12 medium, Neural basal medium, N2, B27, RA, GlutaMAX, MEM, Dorsomorphin, insulin, SB431542, PS, 2-mercaptoethanol | Gabriel et al., 2021 | |
| hESCs | ULA Plate | 19d/>25d | DMEM/F12 medium, Neurobasal medium, PS, GlutaMAX, B27 without Vit A, EGF, FGF2 | Pagliaro et al., 2023 | |
| Human fetal central nervous system (brain and spinal cord) cells | ULA Plate | 14-21d/NA | AdDMEM/F12 medium, Neurobasal medium, PS, GlutaMAX, HEPES, B27 without VA, N2, MEM, FGF10, EGF, Primocin | Hendriks et al., 2024 | |
| Retina | hESCs | ULA plate & Matrigel | NA/18d | NR culture medium, G-MEM, KSR, NEAA, pyruvate, 2-mercaptoethanol, PS, IWR1e, FBS, SAG, CHIR99021 | Nakano et al., 2012 |
| hPSCs | Matrigel | 2d/24d | DMEM/F12 medium, B27 (without vitamin A), antibiotic-antimycotic, GlutaMAX, NEAA | Regent et al., 2020 | |
| hiPSCs | Geltrex | 2d/>30d | DMEM/F12 medium, FBS, taurine, B27, NEAA, GlutaMAX, antibiotic-antimycotic, retinoic acid | Xie et al., 2020 | |
| hESCs | ULA plate | 3d/>80d | GMEM, KSR, N2, ascorbic acid | Savoj et al., 2022 | |
| hiPSCs | Maxgel | 8d/>120d | DMEM/F12, N2, NEAA, GlutaMAX, heparin, BMP4 | Bohrer et al., 2023 | |
| hiPSCs | rhVTN-N | NA/>42d | E6 medium, N2 | Gozlan et al., 2023 | |
| Skin | mPSCs | ULA plate | NA/>56d | AdDMEM/F12 medium, N2, GlutaMAX, Normocin, LDN, FGF2, BMP4, SB431542 | Lee et al., 2018 |
| hPSCs | ULA plate | NA | AdDMEM/F12 medium, Neurobasal, E6 basal medium, GlutaMAX, B27, N2, 2-mercaptoethanol, Normocin, BMP4, SB431542, bFGF | Lee et al., 2020a | |
| Human primary epidermal cells from foreskintissues | Matrigel | NA/42d | AdDMEM/F12 medium, BSA, B27, HEPES, GlutaMAX, N-Acetyl-Lcysteine,Forskolin, EGF, Wnt3a, A83-01 | Wang et al., 2021b | |
| miPSCs | Matrigel | 2d/29d | AdDMEM/F12 medium, HEPES, Glutamax, B27, N-acetylcysteine-1, Noggin, Rspondin-1, FGF1, heparin, Forskolin | Kwak et al., 2024 | |
| Bone | hPSCs | Matrigel | 2–3d/NA | DMEM, FBS, L-glutamine, NEAA, SP, ITS-X, ascorbic acid, 2-mercaptoethanol, bFGF, TGF- β1, BMP2, GDF5, PS | Tam et al., 2021 |
| PHOs | Matrigel | NA/>4mo | DMEM, Endothelial medium, FBS, GlutaMAX, ascorbic acid, BOM, MCSF, RANKL | Abraham et al., 2022 | |
| hiPSCs | ULA plate | 14d/>62d | APEL2, PFHM II, FGF2, BMP4 | Lamandé et al., 2023 | |
| BMSCs from rats | ULA plate | NA | Chondrogenic Induction, sodium pyruvate, TGF- β3, dexamethasone, ITS premix, ascorbic acid-2-phosphate | Shen et al., 2024 | |
| Heart | hPSCs | Matrigel | NA/15d | DMEM, B27, GlutaMAX, L-ascorbic acid 2-phosphate, PS, glucose, palmitic acid | Mills et al., 2019 |
| mESCs | Matrigel | NA/15d | DMEM/F12 medium, PS, KSR, sodium pyruvate, 2-mercaptoethanol, l-glutamine, progesterone, β-estradiol, insulin, transferrin, selenite, FGF4 | Lee et al., 2020b | |
| hPSCs | ULA plate | NA/21d | CGM media, B27, thrombin, cardiotrophin-1, EGF, FGF-2, Wnt-3A, EDN1 | Ho et al., 2022 | |
| hiPSCs | gelatin | NA/25d | RPMI 1640, BSA, lascorbic acid 2-phosphate, sodium DL-lactate | Seguret et al., 2024 |
Notes.
- BME
- basement membrane extract
- D
- dimensional
- d
- day
- ESC
- embryonic stem cell
- h
- human
- iPSCs
- induced pluripotent stem cells
- KSR
- Knockout Serum Replacement
- m
- mouse
- mo
- month
- NA
- not available
- PHCs
- primary human cholangiocytes
- PHHs
- primary human hepatocytes
- PHOs
- primary human osteocytes
- PMHs
- primary mouse hepatocytes
- PS
- penicillin streptomycin
- PSCs
- pluripotent stem cells (iPSCs &ESCs)
- ULA
- ultra-low attachment
Given the significant challenges in optimizing conditions for organoid expansion, bioreactor-based suspension culture systems have recently attracted attention. These systems, which are widely used for large-scale cell culture in the pharmaceutical industry, offer potential solutions. The dynamic culture model of the bioreactor enhances the exchange of oxygen, nutrients, and metabolites. This improvement is believed to solve the limitations of static culture and markedly improve organoid survival and development (Schneeberger et al., 2020). More importantly, the relatively homogeneous spatial distribution of these components and signaling molecules greatly improves the homogeneity and reproducibility of the organoid products. Transferring static 3D culture to a dynamic spinner flask results in the growth of LGR5-positive liver stem cells achieved a dramatic 7-fold expansion enhancement. This new system also markedly upregulates functional maturation following differentiation (Schneeberger et al., 2020). The success of hPSCs suspension expansion over the past decade (Burrell et al., 2019) has inspired the possibility of extending the 3D culture system to include direct lineage differentiation. In this context, a 3D hPSC expansion system efficiently differentiated definitive endoderm (DE) cells—common intermediates in endoderm lineage differentiation—into 3D floating aggregates in a single batch using a bioreactor. This process yielded 1× 108 DE cells with over 92% purity, facilitating downstream production of various endodermal lineages, including hepatic, pancreatic, and intestinal lineages (Sahabian et al., 2021). Recently, a cascade 3D suspension system was developed that enables both the expansion and subsequent hepatic differentiation of hPSC-DEs. This system facilitated the massive production of hepatic organoids with high purity, over 85% and 93% for hepatocyte and cholangiocyte specification, respectively, in a 300 mL spinner flask (Feng et al., 2020). Although not specifically mentioned, this system may also permit the differentiation of other endodermal lineages under proper downstream differentiation conditions. Additionally, scaling up of cultures for various other lineages, including macrophages, pancreatic cells, and endothelial cells, is rapidly developing (Dossena et al., 2020; Gutbier et al., 2020; Takebe et al., 2017).
Nevertheless, it is worth noting that agitating bioreactors, which allow precise control of dissolved oxygen and nutrients, turbulence, and shear stress, have been rarely reported except in the context of iPSC and iPSC-platelet production (Suzuki et al., 2020). One possible reason is the limitations in refining the optimal bioreactor parameters for distinct iPSC-derived lineage progenitors. Additionally, the high cost and complexity of stage-specific medium supplements may further hinder scaling. A comprehensive understanding of the dynamic culture conditions required for organoid expansion and differentiation, along with integrated automated and programmed culture systems, is urgently needed to scale up organoid production. Evaluating organoid quality—including size, cellular components, and functionality—should be emphasized to ensure reproducibility between different passages and batches.
Automated and controllable culture system
With the development of organoid generation strategies (Fig. 1), the corresponding culture systems have seen significant improvements. However, the reproducibility and consistency of organoid culture systems remain major bottlenecks. Conventional culture processes involve a large number of human factors, low automation, poor organoid controllability, and human error, which lead to significant differences between different cell lines and organisms, resulting in numerous uncertainties and differences in organoid structure and function (Jiang et al., 2020). Automated culture may offer a solution to avoid variable errors caused by inconsistent manual handling during tedious experiments, allowing for precise mechanical automation (Park, Georgescu & Huh, 2019). For example, using an automated liquid-handling robot system, researchers established a fully automated and high-throughput screening-compatible platform with integrated imaging and analysis processes, which for the first time enabled the differentiation and formation of organoids (Czerniecki et al., 2018). Importantly, the Swiss Federal Institute of Technology in Lausanne has developed a high-throughput automated microcavity array technology. This technology is used for the high-throughput derivation of epithelial organoids within a polymer-hydrogel substrate. It clearly demonstrates that organoids generated by automated manipulation display reduced variability and increased time efficiency. Therefore, extending the scope of research relies on stable and reliable organoid culture and facilitates the scaling of culture systems (Brandenberg et al., 2020). Recently, a high-content screening (HCS) platform that allows researchers to screen drugs or other compounds against three-dimensional (3D) cell culture systems in a 384-well multi-well format has been established. This platform enabled automated, imaging-based HCS of 3D cellular models in a non-destructive manner, opening the path to complementary analysis through integrated downstream methods (Bozal et al., 2024).
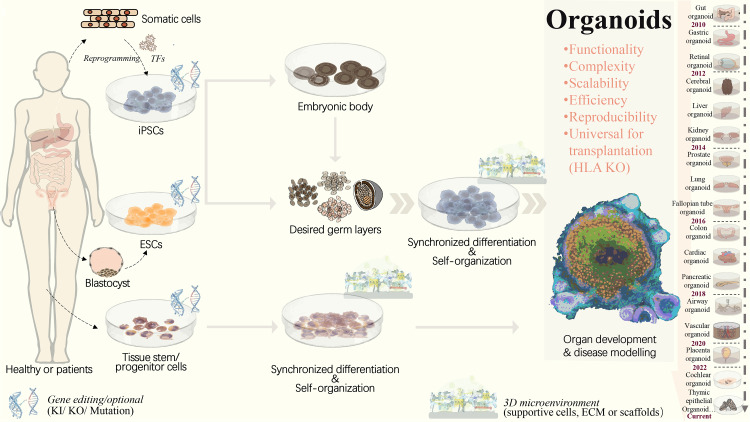
Figure 1. Strategies to generate organoid systems.
Under specific 3D microenvironment (suspension culture, ECM, microparticles, etc.), tissue-derived stem/progenitor cells have been used for generating organoids with the aid of supportive cells. However, the limited cell source, along with challenges in scalability and reproducibility, presents significant hurdles. Pluripotent stem cells, including ESCs and iPSCs, offer a promising alternative due to their potential for efficient and scalable organoid production. PSCs could be synchronously differentiated towards three dermal layers, which facilitates the generation of more complex organoid structure with multiple cellular components. Following embryonic body formation, the organoid functionality and maturation could be significantly improved. With recent advancements in gene editing technologies, such as CRISPR/Cas9, increasing types of iPSCs-derived diseased organoids have been established by means of gene mutation/ knock-in or out. This progress greatly extends the applications in personalized disease modeling and drug testing. In addition, for ESC or iPSC-derived organoids, HLA knockout is expected to create universal organoids, which are expected to be useful in organ transplantation. ECM, extracellular matrix; ESCs, embryonic stem cells; HLA, human leukocyte antigen; iPSCs, induced pluripotent stem cells; KI, knock in; KO, knock out; PSCs, pluripotent stem cells, included iPSCs and ESCs; TF, transcription factors.
To achieve precise and automatic control over organoid generation, culture, and analysis conditions, an organoid-on-chip system has been developed, which is based on a microfluidic cell culture device manufactured using a microchip fabrication method. This system consists of multiple microchambers with fluid flow, a variety of living cells, mechanical force stimulation, and other complex factors in vitro. It simulates the main structural and functional characteristics of human organs] by implanting human cells into microfluidic chips for 3D culture (Shirure, Hughes & George, 2021). However, microenvironments such as blood vessels, stromal components, immune cells, and neuroendocrine microenvironments are commonly lacking and need to be further complemented to create more realistic conditions (Schuster et al., 2020). The Tsinghua-Berkeley Shenzhen Institute (TBSI) has combined organoid generation with an organ-on-a-chip system and 3D printing technologies to open up a new field for organoid scaling. In this study, a microfluidic droplet system was used to shear cell-containing Matrigel into homogeneous microspheres, which were then followed by 3D printing. This enabled the rapid generation, culture, and automated manipulation of organoids, leading to the development of homogeneous, controlled, high-throughput, and scalable tumor organoid systems. Nevertheless, this high-throughput and automated organoid culture system still has some limitations, such as a relatively low success rate of organoid printing, incomplete automation, and the need for additional manual transfer (Jiang et al., 2020). Recently, a systematic approach has been taken to investigate the initial seeding density of endothelial cells and its effects on interconnected networks, which has been combined with hepatic spheroids to develop a liver-on-a-chip model. This system provides insight into potential hepatotoxicity caused by various drugs and allows for the assessment of vascular dysfunction in a high-throughput manner (Wang, Andrade & Smith, 2023). In addition, since the organoid microarray model is constructed in a predefined manner, its ability to capture the dynamics of organoid development in response to drugs or environmental changes is very limited. Integrated engineering techniques are needed to monitor and analyze the dynamic development in micro-engineered organoid cultures. Furthermore, due to the complexity of multicellular nutrient and signal requirements in organoids, future optimization of media composition and stepwise culture conditions are necessary for the co-culture system. On this basis, the establishment of standardized good manufacturing practice (GMP) guidelines is expected to further ensure the quality and biosafety of organoids, eventually driving the shift from laboratory research to clinical or industrial applications.
Frontiers and perspectives
Organoid atlas
Organoids have tremendous potential for biomedical research due to their unique advantage of organ-like three-dimensional structures to mimic the physiology and function of native organs (Ashok et al., 2020; Lancaster & Knoblich, 2014). To fully realize their potential and address practical application challenges, organoids should be characterized and validated as reliable organ substitutes (Bock et al., 2021). However, current organoid techniques still face many limitations, including inadequate multilineage development, incomplete neuroendocrine and immune systems, undeveloped vascularization networks, suboptimal physiological functions, and drug responses. A suite of recently developed integration of single-cell and spatial profiling may offer new prospects for addressing these existing problems. These methods allow for identifying the spatial distribution of multiple cell populations within tissues or organoids, and capturing individual cell physiological characteristics and intercellular communication networks by physically localizing cell transcriptomic information within specific spatial locations (Longo et al., 2021). On this basis, comprehensive spatial mapping of liver tissue has identified transcriptome-wide zonation of parenchymal and non-parenchymal liver cells, including previously unknown subpopulations (Aizarani et al., 2019). Moreover, in-depth bioinformatic analysis revealed that the heterogeneous EPCAM+ liver population includes hepatocyte- and cholangiocyte-biased cells, as well as a unique TROP2int population that exhibits bipotency and organoid formation capability, potentially providing a novel liver progenitor source for generating organoids. Notably, the atlas also revealed the differences in gene expression and function between normal and hepatocellular carcinoma livers across multiple cell types, providing new insights into inter-cellular communications during liver cancer development and aiding in the design of in vitro modeling (Aizarani et al., 2019). Additionally, single-cell sequencing and spatial transcriptomics are increasingly used to characterize tissue architecture and biological mechanisms in various normal and cancerous tissue/organs (Mutuku et al., 2022; Rao et al., 2021; Yamada & Nomura, 2020) and to deconvolute the microenvironment for tissue homeostasis and cancer progression (Ayyaz et al., 2019; Baccin et al., 2020; Wang et al., 2021a).
On this basis, comparative spatial molecular profiling of organoids with their corresponding tissues or organs may fundamentally provide references for the revolutionary outbreak of current protocols and strategies for organoid generation, culture, and even disease modeling. For example, this approach can identify the specific roles of individual cell populations and reveal key regulatory mechanisms in organogenesis or carcinogenesis. Indeed, many previously unobservable discrepancies in gene expression and organization of particular cellular composition, have been confirmed between cultured organoids and relevant organs by in-depth transcriptomic comparison at the single-cell level. These findings offer significant clues for improving organoid models through advanced engineering and culture systems (Kanton et al., 2019) Moreover, the organoid atlas provides a scalable tool for evaluating organoids in terms of constructure, functionality, and even unexpected mutations, which is crucial for quality control, particularly in terms of regenerative therapy (Sridhar et al., 2020). To create comprehensive reference maps for all human cells as a basis for understanding human biology and treating diseases, an Organoid Cell Atlas pilot project was recently launched in Europe. This project is expected to complement the profiling of primary tissues with perdurable models for studies in biomedical discovery and regenerative therapies (Bock et al., 2021). Although spatially resolved transcriptomic technologies are now being widely adopted, their application is still facing long-term challenges. Current approaches cannot provide deep transcriptomic information on precisely localized single cells in tissues or organoids (Rao et al., 2021).
Moreover, there is an urgent need to develop novel computational methods for analyzing spatially resolved transcriptomic data. These methods should characterize the heterogeneity of cells within their spatial contexts and to derive biological insights into organoids and their derivation models, as well as the corresponding primary tissues (Longo et al., 2021).
Universally compatible iPSC-organoids and biobank
Organoids can be established from autologous iPSCs, which are immunologically identical to the donor, offering significant immunological advantages in transplantation therapy. However, creating autologous iPSC from each patient’s somatic cells is difficult for standardized treatments due to low efficiency and high cost (Murata et al., 2020). With the development of gene editing tools, the possibility of iPSCs transplantation without allogeneic rejection has become a key focus in regenerative medicine (Ichise et al., 2017; Koga, Wang & Kaneko, 2020; Morizane et al., 2017; Zhao et al., 2011). In particular, CRISPR/Cas9 gene editing tool enables the creation of universally compatible iPSCs by remodulating immune-related antigens via gRNA targeting and cas9 nuclease-mediated shearing (Chen et al., 2019). Human leukocyte antigen (HLA), which plays an important role in distinguishing self from non-self, is a major barrier in organ and cell-based transplantation. It is commonly believed that HLA mismatch between the donor and recipient is a major barrier to organ or cell-based transplantation, while matched HLA can significantly reduce the risk of graft rejection and graft-versus-host disease (GVHD), and improve allograft survival (Koga, Wang & Kaneko, 2020). HLA class I and II complexes mediate antigen-specific adaptive immune responses and act as ligands for T and NK cells, which differentiate between self and non-self components (Long et al., 2013). To overcome immune rejection, β2-microglobulin (B2M), a common protein subunit, essential for HLA class I expression, is commonly knocked out using traditional editing. However, knocking out B2M silences of all HLA class I molecules, causing “miss self” and leading to NK cell attack (Flahou et al., 2021). To address this, immune rejection was suppressed by disrupting the HLA-A and -B alleles and HLA class II molecules, while retaining HLA-C, which helps avoids NK cell-mediated self-attack. This approach enables iPSCs to evade T and NK cell attacks in vitro and in vivo (Lee et al., 2020a). iPSCs produced by the iPS Cell Research and Application Center of Kyoto University using a gene knockout strategy with CRISPR/Cas9 exhibited extremely low immunogenicity and could evade attack in vitro and in vivo after T and NK cells differentiate into platelets (Xu et al., 2019). Similarly, another group used CRISPR-Cas9 to knock out beta-2-microglobulin (B2M) in kidney organoids, successfully protecting kidney organoids derived from these iPSCs against T-cell rejection (Gaykema et al., 2024). These successes highlight the possibility of using universally compatible iPSC sources to generate highly biocompatible and available organoid derivatives to solve the current extreme shortage of organs for transplantation, with dramatically reduced GVHD.
However, challenges remain in current HLA knockout strategies. Precise targeting of HLA-A and HLA-B while retaining HLA-C is crucial to avoid off-target effects on HLA-C homologous sequences. In addition, the potential reduction in cell viability, proliferation, and pluripotency of PSCs should be monitored and controlled to maintain the full differentiation potential of PSCs. Moreover, the general problems of low transfection efficiency and off-target phenomena in gene editing must be optimized (Chen et al., 2019). To enhance on-target specificity, scientists have attempted to modify the Cas9 protein to alter PAM preferences or enhance target DNA recognition and developed systems to regulate Cas9 expression during transcription and translation (Kleinstiver et al., 2016; Kleinstiver et al., 2015; Shen et al., 2018). Research on trophoblast organoids has advanced the understanding of placental development. Organoid models using CRISPR/Cas9 technology examined the role of HLA-G in trophoblast function and differentiation. JEG-3 trophoblast organoids (JEG-3-ORGs) were established, expressing key trophoblast representative markers and had the capacity to differentiate into EVT. HLA-G knockout (KO) via CRISPR/Cas9 significantly altered the trophoblast immunomodulatory effect on NK cell cytotoxicity, as well as the trophoblast regulatory effect on HUVEC angiogenesis (Zhuang et al., 2023). However, the current technology is still immature, and future improvements in specificity, targeting efficiency, and use of highly efficient, biocompatible, and non-immunogenic delivery vehicles are needed. Considering the overall usefulness of the CRISPR-Cas9 gene editing tool in terms of efficiency and biocompatibility, its use in in vivo transplantation is believed to enhance safety and efficacy (Chen et al., 2019).
Given the rapid demand for organ/tissue models and transplantation grafts for diverse research and clinical applications, the establishment of organoid biobanks offers extensive opportunities for ready-to-use tools and sources (Perrone & Zilbauer, 2021). Large-scale production of universally compatible iPSC-organoid is expected to expand transplantation therapies to many patients with different HLA backgrounds (Fig. 2). However, due to HLA’s high polymorphic and variation among different ethnic groups in different regions, creating organoid banks with sufficient HLA haplotypes that match a wide range of populations remains challenging (Flahou et al., 2021). Recruiting HLA-homozygous donors to cover diverse populations is particularly difficult. Biobanks must consider rare frequency alleles and include rare donors, with each cell source carefully characterized and evaluated for regulatory safety (Flahou et al., 2021). Recently, a PLC biobank with 399 tumor organoids derived from 144 patients was established, which recapitulates histopathology and genomic landscape of parental tumors, and is reliable for drug sensitivity screening. This study explored PLC heterogeneity, developed predictive biomarker panels, and identified a lenvatinib-resistant mechanism for combination therapy (Yang et al., 2024). Beyond identifying clinical biocompatibility and safety, considerable work remains to establish standard, verified clinical-grade allogeneic organoid biobanks. Global collaborative efforts from the scientific, clinical, and industrial communities are required to accelerate the development of this encouraging field.
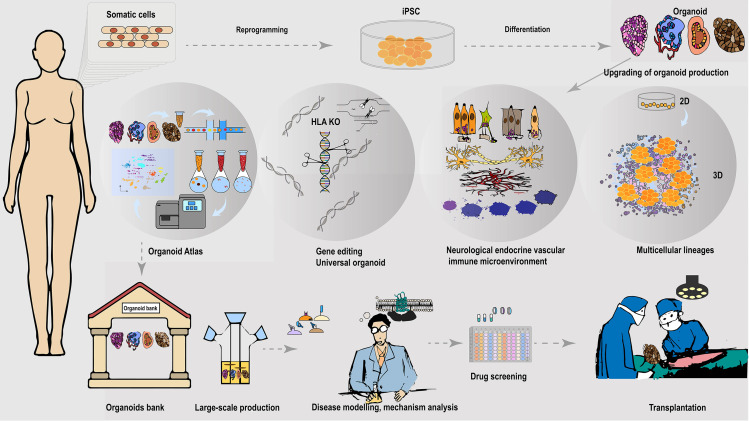
Figure 2. Universally compatible iPSC-organoid biobanking and applications.
iPSC could be reprogrammed from a patient’s somatic cells and used as a starting source for producing patient-derived multiple desired organoids. Advanced 3D organoid culture system contains multiple supportive cell populations such as stromal cells, endothelial cells, as well as the neuroendocrine and immune system, allowing for a closer approximation to in vivo organs. The inclusion of multiple supportive cell populations contributes to the construction of disease models and the development of pharmaceutical products at this stage. The automated culture system provides the possibility to overcome the variable errors caused by manual inconsistency, and scale-up of support organoid production, and is expected to provide a solution to the difficult breakthrough of large-scale expansion of standardized organoids at the GMP level. In addition, the use of gene-editing tools to knock out immune response antigens such as HLA is expected to generate universally compatible iPSC-organoids ideal for allogeneic transplantation. Combining single-cell and spatial profiling, organoid mapping can provide structural and molecular profiles of organoids in comparison with corresponding tissues or organs. This approach enhances the high simulation of current organoid construction and cultivation. Additionally, it contributes to further optimization of disease modeling. The establishment of organoid libraries will greatly contribute to the provision of ready-to-use disease models for drug screening. These libraries are also expected to provide immediate organoid substitutes for the treatment of malignant or advanced diseases, such as cancer. The establishment of organoid banks will greatly help to supply ready-to-use disease models for drugs screening, and is expected to provide immediate organ substitutes for treating malignant or late-stage diseases such as cancer.
Interdisciplinary collaboration
The future of organoid research is deeply intertwined with interdisciplinary collaboration, which integrates expertise from diverse fields to overcome current limitations in scalability, functionality, and clinical applications. While the biological sciences provide the foundation for understanding the molecular and cellular mechanisms of organoid formation, other disciplines, such as bioengineering, materials science, and computational biology, play essential roles in advancing this technology.
Bioengineering and material science.
One of the most promising areas of collaboration is between bioengineers and materials scientists, particularly in the development of synthetic scaffolds and extracellular matrices. These artificial matrices mimic the natural environment of human tissues, promoting the growth, differentiation, and organization of cells within organoids. For example, bioengineers are utilizing 3D bioprinting technologies to construct scaffolds that provide mechanical support and guide the spatial organization of organoid structures (Deng et al., 2024). These innovations are critical for scaling up organoid cultures for high-throughput drug screening and clinical-grade tissue production.
Material scientists contribute by designing tunable hydrogels with adjustable stiffness, porosity, and biochemical signals to simulate the tissue-specific extracellular matrix, improving organoid maturation and functionality (Nerger et al., 2024). These advancements enable the generation of more complex organoid models that better mimic the in vivo environment, an essential step for applications in regenerative medicine and disease modeling.
Computational biology and systems medicine.
The advent of big data and artificial intelligence is revolutionizing organoid data analysis, making collaboration with computational biologists increasingly vital. Organoids generate vast datasets from high-throughput genomics, proteomics, and transcriptomics studies. Computational biologists are developing advanced algorithms and machine learning models to analyze these data, identifying key signaling pathways in organoid development and disease progression (Santamaria et al., 2023; Wahle et al., 2023). This collaboration supports precision modeling, allowing organoids to be tailored to reflect patient-specific genetics or disease conditions, a powerful approach in personalized medicine.
In addition, systems biology approaches are integrating multi-omics data from organoid studies to map cellular networks and predict drug responses. For instance, modeling the interactions between different cell types within an organoid (e.g., immune cells in liver or brain organoids) is crucial for understanding diseases like cancer and neurodegeneration. These insights may reveal new therapeutic targets that traditional models cannot capture.
Ethical and regulatory concerns
Use of human stem cells.
Organoids are often derived from induced pluripotent stem cells (iPSCs) or embryonic stem cells (ESCs), raising ethical concerns about the use of human embryos or reprogramming adult cells. Regulatory frameworks governing stem cell research vary across countries, with some enforcing stricter guidelines on the sourcing and manipulation of human cells (Park et al., 2024). For instance, research involving ESCs may conflict with certain cultural or religious beliefs, necessitating transparent and culturally sensitive regulations to address these concerns.
Clinical applications.
While organoids hold significant potential for regenerative medicine, concerns about safety, efficacy, and the long-term impacts of transplanting lab-grown tissues into humans remain. Regulatory bodies like the FDA and EMA have yet to fully establish guidelines specific to organoid-based therapies, complicating the path to clinical application. Navigating these regulatory challenges requires strict quality control measures, ethical sourcing of stem cells, and comprehensive preclinical testing.
Consent and data privacy.
The use of iPSCs involves obtaining consent from donors, as their genetic information is encoded within the cells. Ensuring informed consent, especially regarding the future uses of organoids derived from their cells, while also protecting donor privacy in light of genomic data sharing is critical regulatory concern. This issue is particularly significant in precision medicine, where organoids might be used to model individual patients’ conditions.
To address these ethical and regulatory challenges, interdisciplinary collaboration is essential not only within scientific fields but also with ethicists, legal experts, and policymakers. Regulatory frameworks must be updated to keep pace with advancements in organoid technology, ensuring that innovation remains both ethically and scientifically sound. This might involve creating new standards for informed consent, safety regulations for organoid-based therapies, and defining ethical boundaries for the extent of human tissue mimicry.
Conclusions
As organoid research progresses, ensuring reliability, efficiency, and scalability has become the focus of organoid research and applications. Although challenges remain, iPSC-derived multicellular organoids hold promise for drug screening and transplantation therapy. The integration of bioreactors with automated culture systems may greatly increase the scale of organoid production. Additionally, it is expected that future advances in organoid atlas and organoid biobanking may contribute to more reliable and practical applications in drug development and regenerative medicine.
Acknowledgments
We appreciate Drs. Li-Ping Liu, Yu-Mei Li, Di Cao, Mei Fang and Hang Zhou in Jiangsu University, Mr. Shang-Ping Tian, Mr. Yu-Mu Song and Ms Ji-Yue Yan in Wuyi University for contributing research assistance and discussion.
Funding Statement
All the external funding or sources of support received during this study: National Natural Science Foundation of China (82270697, 82070638 and 82370517) and Guangdong Basic Applied Basic Research Foundation (2023A1515012574), Jiangsu Provincial Medical Key Discipline Cultivation Unit (JSDW202229), the Science and Technology Planning Project of Guangdong Province of China (2021B1212040016), and the Grant for International Joint Research Project of the Institute of Medical Science, University of Tokyo. No other external funding was received for this study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Jian-Yun Ge performed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft.
Yun Wang performed the experiments, analyzed the data, prepared figures and/or tables, and approved the final draft.
Qi-Lin Li analyzed the data, prepared figures and/or tables, and approved the final draft.
Fan-Kai Liu analyzed the data, prepared figures and/or tables, and approved the final draft.
Quan-Kai Lei analyzed the data, authored or reviewed drafts of the article, and approved the final draft.
Yun-Wen Zheng conceived and designed the experiments, authored or reviewed drafts of the article, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
This is a literature review.
References
- Abraham et al. (2022).Abraham DM, Herman C, Witek L, Cronstein BN, Flores RL, Coelho PG. Self-assembling human skeletal organoids for disease modeling and drug testing. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2022;110:871–884. doi: 10.1002/jbm.b.34968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acharya et al. (2024).Acharya P, Shrestha S, Joshi P, Choi NY, Lekkala VKR, Kang SY, Ni G, Lee MY. Dynamic culture of cerebral organoids using a pillar/perfusion plate for the assessment of developmental neurotoxicity. BioRxiv. 2024 doi: 10.1101/2024.03.11.584506. [DOI] [PMC free article] [PubMed]
- Aizarani et al. (2019).Aizarani N, Saviano A, Sagar, Mailly L, Durand S, Herman JS, Pessaux P, Baumert TF, Grun D. A human liver cell atlas reveals heterogeneity and epithelial progenitors. Nature. 2019;572:199–204. doi: 10.1038/s41586-019-1373-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akbari et al. (2019).Akbari S, Sevinc GG, Ersoy N, Basak O, Kaplan K, Sevinc K, Ozel E, Sengun B, Enustun E, Ozcimen B, Bagriyanik A, Arslan N, Onder TT, Erdal E. Robust, long-term culture of endoderm-derived hepatic organoids for disease modeling. Stem Cell Reports. 2019;13:627–641. doi: 10.1016/j.stemcr.2019.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artegiani et al. (2019).Artegiani B, van Voorthuijsen L, Lindeboom RGH, Seinstra D, Heo I, Tapia P, López-Iglesias C, Postrach D, Dayton T, Oka R, Hu H, van Boxtel R, van Es JH, Offerhaus J, Peters PJ, van Rheenen J, Vermeulen M, Clevers H. Probing the tumor suppressor function of BAP1 in CRISPR-engineered human liver organoids. Cell Stem Cell. 2019;24 doi: 10.1016/j.stem.2019.04.017. [DOI] [PubMed] [Google Scholar]
- Ashok et al. (2020).Ashok A, Choudhury D, Fang Y, Hunziker W. Towards manufacturing of human organoids. Biotechnology Advances. 2020;39:107460. doi: 10.1016/j.biotechadv.2019.107460. [DOI] [PubMed] [Google Scholar]
- Ayyaz et al. (2019).Ayyaz A, Kumar S, Sangiorgi B, Ghoshal B, Gosio J, Ouladan S, Fink M, Barutcu S, Trcka D, Shen J, Chan K, Wrana JL, Gregorieff A. Single-cell transcriptomes of the regenerating intestine reveal a revival stem cell. Nature. 2019;569:121–125. doi: 10.1038/s41586-019-1154-y. [DOI] [PubMed] [Google Scholar]
- Baccin et al. (2020).Baccin C, Al-Sabah J, Velten L, Helbling PM, Grunschlager F, Hernandez-Malmierca P, Nombela-Arrieta C, Steinmetz LM, Trumpp A, Haas S. Combined single-cell and spatial transcriptomics reveal the molecular, cellular and spatial bone marrow niche organization. Nature Cell Biology. 2020;22:38–48. doi: 10.1038/s41556-019-0439-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Below et al. (2022).Below CR, Kelly J, Brown A, Humphries JD, Hutton C, Xu J, Lee BY, Cintas C, Zhang X, Hernandez-Gordillo V, Stockdale L, Goldsworthy MA, Geraghty J, Foster L, O’Reilly DA, Schedding B, Askari J, Burns J, Hodson N, Smith DL, Lally C, Ashton G, Knight D, Mironov A, Banyard A, Eble JA, Morton JP, Humphries MJ, Griffith LG, Jorgensen C. A microenvironment-inspired synthetic three-dimensional model for pancreatic ductal adenocarcinoma organoids. Nature Materials. 2022;21:110–119. doi: 10.1038/s41563-021-01085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bi et al. (2020).Bi H, Karanth SS, Ye K, Stein R, Jin S. Decellularized tissue matrix enhances self-assembly of islet organoids from pluripotent stem cell differentiation. ACS Biomaterials Science & Engineering. 2020;6:4155–4165. doi: 10.1021/acsbiomaterials.0c00088. [DOI] [PubMed] [Google Scholar]
- Birey et al. (2017).Birey F, Andersen J, Makinson CD, Islam S, Wei W, Huber N, Fan HC, Metzler KRC, Panagiotakos G, Thom N, O’Rourke NA, Steinmetz LM, Bernstein JA, Hallmayer J, Huguenard JR, Paşca SP. Assembly of functionally integrated human forebrain spheroids. Nature. 2017;545:54–59. doi: 10.1038/nature22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock et al. (2021).Bock C, Boutros M, Camp JG, Clarke L, Clevers H, Knoblich JA, Liberali P, Regev A, Rios AC, Stegle O, Stunnenberg HG, Teichmann SA, Treutlein B, Vries RGJ, Human Cell Atlas’ Biological Network O The organoid cell Atlas. Nature Biotechnology. 2021;39:13–17. doi: 10.1038/s41587-020-00762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohrer et al. (2023).Bohrer LR, Stone NE, Mullin NK, Voigt AP, Anfinson KR, Fick JL, Luangphakdy V, Hittle B, Powell K, Muschler GF, Mullins RF, Stone EM, Tucker BA. Automating iPSC generation to enable autologous photoreceptor cell replacement therapy. Journal of Translational Medicine. 2023;21:161. doi: 10.1186/s12967-023-03966-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boj et al. (2015).Boj SF, Hwang C-I, Baker LA, Chio IIC, Engle DD, Corbo V, Jager M, Ponz-Sarvise M, Tiriac H, Spector MS, Gracanin A, Oni T, Yu KH, Van Boxtel R, Huch M, Rivera KD, Wilson JP, Feigin ME, Öhlund D, Handly-Santana A, Ardito-Abraham CM, Ludwig M, Elyada E, Alagesan B, Biffi G, Yordanov GN, Delcuze B, Creighton B, Wright K, Park Y, Morsink FHM, Molenaar IQ, Borel Rinkes IH, Cuppen E, Hao Y, Jin Y, Nijman IJ, Iacobuzio-Donahue C, Leach SD, Pappin DJ, Hammell M, Klimstra DS, Basturk O, Hruban RH, Offerhaus GJ, Vries RGJ, Clevers H, Tuveson DA. Organoid models of human and mouse ductal pancreatic cancer. Cell. 2015;160:324–338. doi: 10.1016/j.cell.2014.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozal et al. (2024).Bozal SB, Sjogren G, Costa AP, Brown JS, Roberts S, Baker D, Gabriel P, Ristau BT, Samuels M, Flynn WF, Robson P, Courtois ET. Development of an automated 3D high content cell screening platform for organoid phenotyping. SLAS Discovery: Advancing Life Sciences R & D. 2024;29:100182. doi: 10.1016/j.slasd.2024.100182. [DOI] [PubMed] [Google Scholar]
- Brandenberg et al. (2020).Brandenberg N, Hoehnel S, Kuttler F, Homicsko K, Ceroni C, Ringel T, Gjorevski N, Schwank G, Coukos G, Turcatti G, Lutolf MP. High-throughput automated organoid culture via stem-cell aggregation in microcavity arrays. Nature Biomedical Engineering. 2020;4:863–874. doi: 10.1038/s41551-020-0565-2. [DOI] [PubMed] [Google Scholar]
- Broutier et al. (2017).Broutier L, Mastrogiovanni G, Verstegen MM, Francies HE, Gavarró LM, Bradshaw CR, Allen GE, Arnes-Benito R, Sidorova O, Gaspersz MP, Georgakopoulos N, Koo B-K, Dietmann S, Davies SE, Praseedom RK, Lieshout R, Ijzermans JNM, Wigmore SJ, Saeb-Parsy K, Garnett MJ, van der Laan LJ, Huch M. Human primary liver cancer-derived organoid cultures for disease modeling and drug screening. Nature Medicine. 2017;23:1424–1435. doi: 10.1038/nm.4438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burrell et al. (2019).Burrell K, Dardari R, Goldsmith T, Toms D, Villagomez DAF, King WA, Ungrin M, West FD, Dobrinski I. Stirred suspension bioreactor culture of porcine induced pluripotent stem cells. Stem Cells and Development. 2019;28:1264–1275. doi: 10.1089/scd.2019.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cakir et al. (2019).Cakir B, Xiang Y, Tanaka Y, Kural MH, Parent M, Kang Y-J, Chapeton K, Patterson B, Yuan Y, He C-S, Raredon MSB, Dengelegi J, Kim K-Y, Sun P, Zhong M, Lee S, Patra P, Hyder F, Niklason LE, Lee S-H, Yoon Y-S, Park I-H. Engineering of human brain organoids with a functional vascular-like system. Nature Methods. 2019;16:1169–1175. doi: 10.1038/s41592-019-0586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calandrini & Drost (2021).Calandrini C, Drost J. Generation of human kidney tubuloids from tissue and urine. Journal of Visualized Experiments. 2021;170:e62404. doi: 10.3791/62404. [DOI] [PubMed] [Google Scholar]
- Cao et al. (2021).Cao D, Ge JY, Wang Y, Oda T, Zheng YW. Hepatitis B virus infection modeling using multi-cellular organoids derived from human induced pluripotent stem cells. World Journal of Gastroenterol. 2021;27:4784–4801. doi: 10.3748/wjg.v27.i29.4784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen et al. (2019).Chen M, Mao A, Xu M, Weng Q, Mao J, Ji J. CRISPR-Cas9 for cancer therapy: opportunities and challenges. Cancer Letters. 2019;447:48–55. doi: 10.1016/j.canlet.2019.01.017. [DOI] [PubMed] [Google Scholar]
- Cho et al. (2021).Cho Y-W, Min D-W, Kim H-P, An Y, Kim S, Youk J, Chun J, Im JP, Song S-H, Ju YS, Han S-W, Park KJ, Kim T-Y. Patient-derived organoids as a preclinical platform for precision medicine in colorectal cancer. Molecular Oncology. 2021 doi: 10.1002/1878-0261.13144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Acuña et al. (2017).Cruz-Acuña R, Quirós M, Farkas AE, Dedhia PH, Huang S, Siuda D, García-Hernández V, Miller AJ, Spence JR, Nusrat A, García AJ. Synthetic hydrogels for human intestinal organoid generation and colonic wound repair. Nature Cell Biology. 2017;19:1326–1335. doi: 10.1038/ncb3632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui et al. (2023).Cui S, Fang X, Lee H, Shin YJ, Koh ES, Chung S, Park HS, Lim SW, Lee KI, Lee JY, Yang CW, Chung BH. Modeling of Fabry disease nephropathy using patient derived human induced pluripotent stem cells and kidney organoid system. Journal of Translational Medicine. 2023;21:138. doi: 10.1186/s12967-023-03992-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czerniecki et al. (2018).Czerniecki SM, Cruz NM, Harder JL, Menon R, Annis J, Otto EA, Gulieva RE, Islas LV, Kim YK, Tran LM, Martins TJ, Pippin JW, Fu H, Kretzler M, Shankland SJ, Himmelfarb J, Moon RT, Paragas N, Freedman BS. High-throughput screening enhances kidney organoid differentiation from human pluripotent stem cells and enables automated multidimensional phenotyping. Cell Stem Cell. 2018;22:P929–P940. doi: 10.1016/j.stem.2018.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Aldebert et al. (2020).d’Aldebert E, Quaranta M, Sébert M, Bonnet D, Kirzin S, Portier G, Duffas J-P, Chabot S, Lluel P, Allart S, Ferrand A, Alric L, Racaud-Sultan C, Mas E, Deraison C, Vergnolle N. Characterization of human colon organoids from inflammatory bowel disease patients. Frontiers in Cell and Developmental Biology. 2020;8:363. doi: 10.3389/fcell.2020.00363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Crignis et al. (2021).De Crignis E, Hossain T, Romal S, Carofiglio F, Moulos P, Khalid MM, Rao S, Bazrafshan A, Verstegen MM, Pourfarzad F, Koutsothanassis C, Gehart H, Kan TW, Palstra R-J, Boucher C, Ijzermans JN, Huch M, Boj SF, Vries R, Clevers H, Laan LJvander, Hatzis P, Mahmoudi T. Application of human liver organoids as a patient-derived primary model for HBV infection and related hepatocellular carcinoma. ELife. 2021;10:e60747. doi: 10.7554/eLife.60747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekkers et al. (2013).Dekkers JF, Wiegerinck CL, De Jonge HR, Bronsveld I, Janssens HM, De Winter-de Groot KM, Brandsma AM, De Jong NW, Bijvelds MJ, Scholte BJ, Nieuwenhuis EE, Van den Brink S, Clevers H, Van Eer Ent CK, Middendorp S, Beekman JM. A functional CFTR assay using primary cystic fibrosis intestinal organoids. Nature Medicine. 2013;19:939–945. doi: 10.1038/nm.3201. [DOI] [PubMed] [Google Scholar]
- Demyan et al. (2022).Demyan L, Habowski AN, Plenker D, King DA, Standring OJ, Tsang C, St Surin L, Rishi A, Crawford JM, Boyd J, Pasha SA, Patel H, Galluzzo Z, Metz C, Gregersen PK, Fox S, Valente C, Abadali S, Matadial-Ragoo S, DePeralta DK, Deutsch GB, Herman JM, Talamini MA, Tuveson DA, Weiss MJ. Pancreatic cancer patient-derived organoids can predict response to neoadjuvant chemotherapy. Annals of Surgery. 2022;276:450–462. doi: 10.1097/SLA.0000000000005558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng et al. (2024).Deng B, Ma Y, Huang J, He R, Luo M, Mao L, Zhang E, Zhao Y, Wang X, Wang Q, Pang M, Mao Y, Yang H, Liu L, Huang P. Revitalizing liver function in mice with liver failure through transplantation of 3D-bioprinted liver with expanded primary hepatocytes. Science Advances. 2024;10:eado1550. doi: 10.1126/sciadv.ado1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donadoni et al. (2024).Donadoni M, Cakir S, Bellizzi A, Swingler M, Sariyer IK. Modeling HIV-1 infection and NeuroHIV in hiPSCs-derived cerebral organoid cultures. Journal of NeuroVirology. 2024. [DOI] [PMC free article] [PubMed]
- Dossena et al. (2020).Dossena M, Piras R, Cherubini A, Barilani M, Dugnani E, Salanitro F, Moreth T, Pampaloni F, Piemonti L, Lazzari L. Standardized GMP-compliant scalable production of human pancreas organoids. Stem Cell Research & Therapy. 2020;11:94. doi: 10.1186/s13287-020-1585-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drakhlis et al. (2021).Drakhlis L, Biswanath S, Farr C-M, Lupanow V, Teske J, Ritzenhoff K, Franke A, Manstein F, Bolesani E, Kempf H, Liebscher S, Schenke-Layland K, Hegermann J, Nolte L, Meyer H, de la Roche J, Thiemann S, Wahl-Schott C, Martin U, Zweigerdt R. Human heart-forming organoids recapitulate early heart and foregut development. Nature Biotechnology. 2021;39:737–746. doi: 10.1038/s41587-021-00815-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta, Heo & Clevers (2017).Dutta D, Heo I, Clevers H. Disease modeling in stem cell-derived 3d organoid systems. Trends in Molecular Medicine. 2017;23:393–410. doi: 10.1016/j.molmed.2017.02.007. [DOI] [PubMed] [Google Scholar]
- Dye et al. (2015).Dye BR, Hill DR, Ferguson MA, Tsai YH, Nagy MS, Dyal R, Wells JM, Mayhew CN, Nattiv R, Klein OD, White ES, Deutsch GH, Spence JR. In vitro generation of human pluripotent stem cell derived lung organoids. Elife. 2015;4:05098. doi: 10.7554/eLife.05098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner-Peking et al. (2021).Ebner-Peking P, Krisch L, Wolf M, Hochmann S, Hoog A, Vári B, Muigg K, Poupardin R, Scharler C, Schmidhuber S, Russe E, Stachelscheid H, Schneeberger A, Schallmoser K, Strunk D. Self-assembly of differentiated progenitor cells facilitates spheroid human skin organoid formation and planar skin regeneration. Theranostics. 2021;11:8430–8447. doi: 10.7150/thno.59661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiraku et al. (2008).Eiraku M, Watanabe K, Matsuo-Takasaki M, Kawada M, Yonemura S, Matsumura M, Wataya T, Nishiyama A, Muguruma K, Sasai Y. Self-organized formation of polarized cortical tissues from ESCs and its active manipulation by extrinsic signals. Cell Stem Cell. 2008;3:519–532. doi: 10.1016/j.stem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- Feng et al. (2020).Feng S, Wu J, Qiu WL, Yang L, Deng X, Zhou Y, Chen Y, Li X, Yu L, Li H, Xu ZR, Xiao Y, Ren X, Zhang L, Wang C, Sun Z, Wang J, Ding X, Chen Y, Gadue P, Pan G, Ogawa M, Ogawa S, Na J, Zhang P, Hui L, Yin H, Chen L, Xu CR, Cheng X. Large-scale generation of functional and transplantable hepatocytes and cholangiocytes from human endoderm stem cells. Cell Reports. 2020;33:108455. doi: 10.1016/j.celrep.2020.108455. [DOI] [PubMed] [Google Scholar]
- Flahou et al. (2021).Flahou C, Morishima T, Takizawa H, Sugimoto N. Fit-for-all iPSC-derived cell therapies and their evaluation in humanized mice with NK cell immunity. Frontiers in Immunology. 2021;12:662360. doi: 10.3389/fimmu.2021.662360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fordham et al. (2013).Fordham RP, Yui S, Hannan NRF, Soendergaard C, Madgwick A, Schweiger PJ, Nielsen OH, Vallier L, Pedersen RA, Nakamura T, Watanabe M, Jensen KB. Transplantation of expanded fetal intestinal progenitors contributes to colon regeneration after injury. Cell Stem Cell. 2013;13:734–744. doi: 10.1016/j.stem.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel et al. (2021).Gabriel E, Albanna W, Pasquini G, Ramani A, Josipovic N, Mariappan A, Schinzel F, Karch CM, Bao G, Gottardo M, Suren AA, Hescheler J, Nagel-Wolfrum K, Persico V, Rizzoli SO, Altmüller J, Riparbelli MG, Callaini G, Goureau O, Papantonis A, Busskamp V, Schneider T, Gopalakrishnan J. Human brain organoids assemble functionally integrated bilateral optic vesicles. Cell Stem Cell. 2021;28(10):1740–1757. doi: 10.1016/j.stem.2021.07.010. [DOI] [PubMed] [Google Scholar]
- Garreta et al. (2024).Garreta E, Moya-Rull D, Marco A, Amato G, Ullate-Agote A, Tarantino C, Gallo M, Esporrín-Ubieto D, Centeno A, Vilas-Zornoza A, Mestre R, Kalil M, Gorroñogoitia I, Zaldua AM, Sanchez S, Izquierdo Reyes L, Fernández-Santos ME, Prosper F, Montserrat N. Natural hydrogels support kidney organoid generation and promote in vitro angiogenesis. Advanced Materials. 2024;36:e2400306. doi: 10.1002/adma.202400306. [DOI] [PubMed] [Google Scholar]
- Gaykema et al. (2024).Gaykema LH, Van Nieuwl RY, Lievers E, Moerkerk WBJ, De Klerk JA, Dumas SJ, Kers J, Zaldumbide A, Van den Berg CW, Rabelink TJ. T-Cell mediated immune rejection of beta-2-microglobulin knockout induced pluripotent stem cell-derived kidney organoids. Stem Cells Translational Medicine. 2024;13:69–82. doi: 10.1093/stcltm/szad069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerli et al. (2024).Gerli MFM, Calá G, Beesley MA, Sina B, Tullie L, Sun KY, Panariello F, Michielin F, Davidson JR, Russo FM, Jones BC, Lee DDH, Savvidis S, Xenakis T, Simcock IC, StraatmanIwanowska AA, Hirst RA, David AL, O’Callaghan C, Olivo A, Eaton S, Loukogeorgakis SP, Cacchiarelli D, Deprest J, Li VSW, Giobbe GG, De Coppi P. Single-cell guided prenatal derivation of primary fetal epithelial organoids from human amniotic and tracheal fluids. Nature Medicine. 2024;30:875–887. doi: 10.1038/s41591-024-02807-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giobbe et al. (2019).Giobbe GG, Crowley C, Luni C, Campinoti S, Khedr M, Kretzschmar K, De Santis MM, Zambaiti E, Michielin F, Meran L, Hu Q, Van Son G, Urbani L, Manfredi A, Giomo M, Eaton S, Cacchiarelli D, Li VSW, Clevers H, Bonfanti P, Elvassore N, De Coppi P. Extracellular matrix hydrogel derived from decellularized tissues enables endodermal organoid culture. Nature Communications. 2019;10:5658. doi: 10.1038/s41467-019-13605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjorevski et al. (2016).Gjorevski N, Sachs N, Manfrin A, Giger S, Bragina ME, Ordonez-Moran P, Clevers H, Lutolf MP. Designer matrices for intestinal stem cell and organoid culture. Nature. 2016;539:560–564. doi: 10.1038/nature20168. [DOI] [PubMed] [Google Scholar]
- Gomes et al. (2020).Gomes AR, Fernandes TG, Vaz SH, Silva TP, Bekman EP, Xapelli S, Duarte S, Ghazvini M, Gribnau J, Muotri AR, Trujillo CA, Sebastião AM, Cabral JMS, Diogo MM. Modeling rett syndrome with human patient-specific forebrain organoids. Frontiers In Cell and Developmental Biology. 2020;8:610427. doi: 10.3389/fcell.2020.610427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Mariano et al. (2020).Gómez-Mariano G, Matamala N, Martínez S, Justo I, Marcacuzco A, Jimenez C, Monzón S, Cuesta I, Garfia C, Martínez MT, Huch M, Pérez De Castro I, Posada M, Janciauskiene S, Martínez-Delgado B. Liver organoids reproduce alpha-1 antitrypsin deficiency-related liver disease. Hepatology International. 2020;14:127–137. doi: 10.1007/s12072-019-10007-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozlan et al. (2023).Gozlan S, Batoumeni V, Fournier T, Nanteau C, Potey A, Clémençon M, Orieux G, Sahel JA, Goureau O, Roger JE, Reichman S. Bankable human iPSC-derived retinal progenitors represent a valuable source of multipotent cells. Communications Biology. 2023;6:762. doi: 10.1038/s42003-023-04956-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassi et al. (2019).Grassi L, Alfonsi R, Francescangeli F, Signore M, De Angelis ML, Addario A, Costantini M, Flex E, Ciolfi A, Pizzi S, Bruselles A, Pallocca M, Simone G, Haoui M, Falchi M, Milella M, Sentinelli S, Di Matteo P, Stellacci E, Gallucci M, Muto G, Tartaglia M, De Maria R, Bonci D. Organoids as a new model for improving regenerative medicine and cancer personalized therapy in renal diseases. Cell Death & Disease. 2019;10:201. doi: 10.1038/s41419-019-1453-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutbier et al. (2020).Gutbier S, Wanke F, Dahm N, Rümmelin A, Zimmermann S, Christensen K, Köchl F, Rautanen A, Hatje K, Geering B, Zhang JD, Britschgi M, Cowley SA, Patsch C. Large-scale production of human iPSC-derived macrophages for drug screening. International Journal of Molecular Sciences. 2020;21:4808. doi: 10.3390/ijms21134808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han et al. (2021).Han Y, Duan X, Yang L, Nilsson-Payant BE, Wang P, Duan F, Tang X, Yaron TM, Zhang T, Uhl S, Bram Y, Richardson C, Zhu J, Zhao Z, Redmond D, Houghton S, Nguyen D-HT, Xu D, Wang X, Jessurun J, Borczuk A, Huang Y, Johnson JL, Liu Y, Xiang J, Wang H, Cantley LC, tenOever BR, Ho DD, Pan FC, Evans T, Chen HJ, Schwartz RE, Chen S. Identification of SARS-CoV-2 inhibitors using lung and colonic organoids. Nature. 2021;589:270–275. doi: 10.1038/s41586-020-2901-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks et al. (2024).Hendriks D, Pagliaro A, Andreatta F, Ma Z, van Giessen J, Massalini S, López-Iglesias C, van Son GJF, DeMartino J, Damen JMA, Zoutendijk I, Staliarova N, Bredenoord AL, Holstege FCP, Peters PJ, Margaritis T, Chuva de Sousa Lopes S, Wu W, Clevers H, Artegiani B. Human fetal brain self-organizes into long-term expanding organoids. Cell. 2024;187(3):712–732. doi: 10.1016/j.cell.2023.12.012. [DOI] [PubMed] [Google Scholar]
- Hickey et al. (2019).Hickey RD, Nicolas CT, Allen K, Mao S, Elgilani F, Glorioso J, Amiot B, Van Lith C, Guthman R, Du Z, Chen H, Harding CO, Kaiser RA, Nyberg SL, Lillegard JB. Autologous gene and cell therapy provides safe and long-term curative therapy in a large pig model of hereditary tyrosinemia type 1. Cell Transplant. 2019;28:79–88. doi: 10.1177/0963689718814188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho et al. (2022).Ho BX, Pang JKS, Chen Y, Loh YH, An O, Yang HH, Seshachalam VP, Koh JLY, Chan WK, Ng SY, Soh BS. Robust generation of human-chambered cardiac organoids from pluripotent stem cells for improved modelling of cardiovascular diseases. Stem Cell Research & Therapy. 2022;13:529. doi: 10.1186/s13287-022-03215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan et al. (2019).Homan KA, Gupta N, Kroll KT, Kolesky DB, Skylar-Scott M, Miyoshi T, Mau D, Valerius MT, Ferrante T, Bonventre JV, Lewis JA, Morizane R. Flow-enhanced vascularization and maturation of kidney organoids in vitro. Nature Methods. 2019;16:255–262. doi: 10.1038/s41592-019-0325-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou et al. (2022).Hou C, Hu Y, Jiang H, Xu Z, Sha W, Liu J, Ren J, Yao M. Establishment of a 3D hyperuricemia model based on cultured human liver organoids. Free Radical Biology & Medicine. 2022;178:7–17. doi: 10.1016/j.freeradbiomed.2021.11.023. [DOI] [PubMed] [Google Scholar]
- Hu et al. (2018).Hu H, Gehart H, Artegiani B, Löpez-Iglesias C, Dekkers F, Basak O, van Es J, Chuva de Sousa Lopes SM, Begthel H, Korving J, van den Born M, Zou C, Quirk C, Chiriboga L, Rice CM, Ma S, Rios A, Peters PJ, de Jong YP, Clevers H. Long-term expansion of functional mouse and human hepatocytes as 3D organoids. Cell. 2018;175(6):1591–1606. doi: 10.1016/j.cell.2018.11.013. [DOI] [PubMed] [Google Scholar]
- Hu et al. (2021).Hu Y, Sui X, Song F, Li Y, Li K, Chen Z, Yang F, Chen X, Zhang Y, Wang X, Liu Q, Li C, Zou B, Chen X, Wang J, Liu P. Lung cancer organoids analyzed on microwell arrays predict drug responses of patients within a week. Nature Communications. 2021;12:2581. doi: 10.1038/s41467-021-22676-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang et al. (2021).Huang L, Desai R, Conrad DN, Leite NC, Akshinthala D, Lim CM, Gonzalez R, Muthuswamy LB, Gartner Z, Muthuswamy SK. Commitment and oncogene-induced plasticity of human stem cell-derived pancreatic acinar and ductal organoids. Cell Stem Cell. 2021;28(6):1090–1104. doi: 10.1016/j.stem.2021.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huch et al. (2013).Huch M, Bonfanti P, Boj SF, Sato T, Loomans CJ, van de Wetering M, Sojoodi M, Li VS, Schuijers J, Gracanin A, Ringnalda F, Begthel H, Hamer K, Mulder J, van Es JH, de Koning E, Vries RG, Heimberg H, Clevers H. Unlimited in vitro expansion of adult bi-potent pancreas progenitors through the Lgr5/R-spondin axis. The EMBO Journal. 2013;32:2708–2721. doi: 10.1038/emboj.2013.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huch et al. (2015).Huch M, Gehart H, Van Boxtel R, Hamer K, Blokzijl F, Verstegen MM, Ellis E, Van Wenum M, Fuchs SA, De Ligt J, Van de Wetering M, Sasaki N, Boers SJ, Kemperman H, De Jonge J, Ijzermans JN, Nieuwenhuis EE, Hoekstra R, Strom S, Vries RR, Van der Laan LJ, Cuppen E, Clevers H. Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell. 2015;160:299–312. doi: 10.1016/j.cell.2014.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichise et al. (2017).Ichise H, Nagano S, Maeda T, Miyazaki M, Miyazaki Y, Kojima H, Yawata N, Yawata M, Tanaka H, Saji H, Masuda K, Kawamoto H. NK cell alloreactivity against KIR-ligand-mismatched HLA-haploidentical tissue derived from HLA haplotype-homozygous iPSCs. Stem Cell Reports. 2017;9:853–867. doi: 10.1016/j.stemcr.2017.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob et al. (2020a).Jacob F, Pather SR, Huang W-K, Zhang F, Wong SZH, Zhou H, Cubitt B, Fan W, Chen CZ, Xu M, Pradhan M, Zhang DY, Zheng W, Bang AG, Song H, Carlos de la Torre J, Ming G-L. Human pluripotent stem cell-derived neural cells and brain organoids reveal SARS-cov-2 neurotropism predominates in choroid plexus epithelium. Cell Stem Cell. 2020a;27(6):937–950. doi: 10.1016/j.stem.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob et al. (2020b).Jacob F, Salinas RD, Zhang DY, Nguyen PTT, Schnoll JG, Wong SZH, Thokala R, Sheikh S, Saxena D, Prokop S, Liu D-A, Qian X, Petrov D, Lucas T, Chen HI, Dorsey JF, Christian KM, Binder ZA, Nasrallah M, Brem S, O’Rourke DM, Ming G-L, Song H. A patient-derived glioblastoma organoid model and biobank recapitulates inter- and intra-tumoral heterogeneity. Cell. 2020b;180(1):188–204. doi: 10.1016/j.cell.2019.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalili-Firoozinezhad, Miranda & Cabral (2021).Jalili-Firoozinezhad S, Miranda CC, Cabral JMS. Modeling the human body on microfluidic chips. Trends in Biotechnology. 2021;39:838–852. doi: 10.1016/j.tibtech.2021.01.004. [DOI] [PubMed] [Google Scholar]
- James et al. (2024).James E, Vielle A, Cusato K, Li H, Lee B, Parween S, Howell A, Johnson NR, Chial HJ, Potter H, Vergara MN. Human iPSC-derived retinal organoids develop robust Alzheimer’s disease neuropathology. Frontiers in Cellular Neuroscience. 2024;18:1340448. doi: 10.3389/fncel.2024.1340448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang et al. (2020).Jiang S, Zhao H, Zhang W, Wang J, Liu Y, Cao Y, Zheng H, Hu Z, Wang S, Zhu Y, Wang W, Cui S, Lobie PE, Huang L, Ma S. An automated organoid platform with inter-organoid homogeneity and inter-patient heterogeneity. Cell Reports Medicine. 2020;1:100161. doi: 10.1016/j.xcrm.2020.100161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanton et al. (2019).Kanton S, Boyle MJ, He Z, Santel M, Weigert A, Sanchis-Calleja F, Guijarro P, Sidow L, Fleck JS, Han D, Qian Z, Heide M, Huttner WB, Khaitovich P, Paabo S, Treutlein B, Camp JG. Organoid single-cell genomic atlas uncovers human-specific features of brain development. Nature. 2019;574:418–422. doi: 10.1038/s41586-019-1654-9. [DOI] [PubMed] [Google Scholar]
- Kim et al. (2022).Kim H, Im I, Jeon JS, Kang E-H, Lee H-A, Jo S, Kim J-W, Woo D-H, Choi YJ, Kim HJ, Han J-S, Lee B-S, Kim J-H, Kim SK, Park H-J. Development of human pluripotent stem cell-derived hepatic organoids as an alternative model for drug safety assessment. Biomaterials. 2022;286:121575. doi: 10.1016/j.biomaterials.2022.121575. [DOI] [PubMed] [Google Scholar]
- Kleinstiver et al. (2016).Kleinstiver BP, Pattanayak V, Prew MS, Tsai SQ, Nguyen NT, Zheng Z, Joung JK. High-fidelity CRISPR–Cas9 nucleases with no detectable genome-wide off-target effects. Nature. 2016;529:490–495. doi: 10.1038/nature16526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinstiver et al. (2015).Kleinstiver BP, Prew MS, Tsai SQ, Nguyen NT, Topkar VV, Zheng Z, Joung JK. Broadening the targeting range of Staphylococcus aureus CRISPR-Cas9 by modifying PAM recognition. Nature Biotechnology. 2015;33:1293–1298. doi: 10.1038/nbt.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koga, Wang & Kaneko (2020).Koga K, Wang B, Kaneko S. Current status and future perspectives of HLA-edited induced pluripotent stem cells. Inflammation and Regeneration. 2020;40:23. doi: 10.1186/s41232-020-00132-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koike et al. (2019).Koike H, Iwasawa K, Ouchi R, Maezawa M, Giesbrecht K, Saiki N, Ferguson A, Kimura M, Thompson WL, Wells JM, Zorn AM, Takebe T. Modelling human hepatobiliary-pancreatic organogenesis from the foregut-midgut boundary. Nature. 2019;574:112–116. doi: 10.1038/s41586-019-1598-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak et al. (2024).Kwak S, Song CL, Lee J, Kim S, Nam S, Park YJ, Lee J. Development of pluripotent stem cell-derived epidermal organoids that generate effective extracellular vesicles in skin regeneration. Biomaterials. 2024;307:122522. doi: 10.1016/j.biomaterials.2024.122522. [DOI] [PubMed] [Google Scholar]
- Lamandé et al. (2023).Lamandé SR, Ng ES, Cameron TL, Kung LHW, Sampurno L, Rowley L, Lilianty J, Patria YN, Stenta T, Hanssen E, Bell KM, Saxena R, Stok KS, Stanley EG, Elefanty AG, Bateman JF. Modeling human skeletal development using human pluripotent stem cells. Proceedings of the National Academy of Sciences of the United States of America. 2023;120:e2211510120. doi: 10.1073/pnas.2211510120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers et al. (2021).Lamers MM, Vaart J, Knoops K, Riesebosch S, Breugem TI, Mykytyn AZ, Beumer J, Schipper D, Bezstarosti K, Koopman CD, Groen N, Ravelli RBG, Duimel HQ, Demmers JAA, Verjans GMGM, Koopmans MPG, Muraro MJ, Peters PJ, Clevers H, Haagmans BL. An organoid-derived bronchioalveolar model for SARS-CoV-2 infection of human alveolar type II-like cells. The EMBO Journal. 2021;40:e105912. doi: 10.15252/embj.2020105912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster & Knoblich (2014).Lancaster MA, Knoblich JA. Organogenesis in a dish: modeling development and disease using organoid technologies. Science. 2014;345:1247125. doi: 10.1126/science.1247125. [DOI] [PubMed] [Google Scholar]
- Lancaster et al. (2013).Lancaster MA, Renner M, Martin C-A, Wenzel D, Bicknell LS, Hurles ME, Homfray T, Penninger JM, Jackson AP, Knoblich JA. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2018).Lee J, Böscke R, Tang P-C, Hartman BH, Heller S, Koehler KR. Hair follicle development in mouse pluripotent stem cell-derived skin organoids. Cell Reports. 2018;22:242–254. doi: 10.1016/j.celrep.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2020a).Lee J, Rabbani CC, Gao H, Steinhart MR, Woodruff BM, Pflum ZE, Kim A, Heller S, Liu Y, Shipchandler TZ, Koehler KR. Hair-bearing human skin generated entirely from pluripotent stem cells. Nature. 2020a;582:399–404. doi: 10.1038/s41586-020-2352-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2020b).Lee J, Sutani A, Kaneko R, Takeuchi J, Sasano T, Kohda T, Ihara K, Takahashi K, Yamazoe M, Morio T, Furukawa T, Ishino F. In vitro generation of functional murine heart organoids via FGF4 and extracellular matrix. Nature Communications. 2020b;11:4283. doi: 10.1038/s41467-020-18031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee et al. (2022).Lee SG, Kim YJ, Son MY, Oh MS, Kim J, Ryu B, Kang KR, Baek J, Chung G, Woo DH, Kim CY, Chung HM. Generation of human iPSCs derived heart organoids structurally and functionally similar to heart. Biomaterials. 2022;290:121860. doi: 10.1016/j.biomaterials.2022.121860. [DOI] [PubMed] [Google Scholar]
- Lei et al. (2023).Lei M, Harn HI, Li Q, Jiang J, Wu W, Zhou W, Jiang TX, Wang M, Zhang J, Lai YC, Juan WT, Widelitz RB, Yang L, Gu ZZ, Chuong CM. The mechano-chemical circuit drives skin organoid self-organization. Proceedings of the National Academy of Sciences of the United States of America. 2023;120:e2221982120. doi: 10.1073/pnas.2221982120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Israeli et al. (2021).Lewis-Israeli YR, Wasserman AH, Gabalski MA, Volmert BD, Ming Y, Ball KA, Yang W, Zou J, Ni G, Pajares N, Chatzistavrou X, Li W, Zhou C, Aguirre A. Self-assembling human heart organoids for the modeling of cardiac development and congenital heart disease. Nature Communications. 2021;12:5142. doi: 10.1038/s41467-021-25329-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2022).Li Z, Xu H, Yu L, Wang J, Meng Q, Mei H, Cai Z, Chen W, Huang W. Patient-derived renal cell carcinoma organoids for personalized cancer therapy. Clinical and Translational Medicine. 2022;12:e970. doi: 10.1002/ctm2.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim et al. (2023).Lim SW, Na D, Lee H, Fang X, Cui S, Shin YJ, Lee KI, Lee JY, Yang CW, Chung BH. Modeling of FAN1-deficient kidney disease using a human induced pluripotent stem cell-derived kidney organoid system. Cell. 2023;12(18):2319. doi: 10.3390/cells12182319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu et al. (2024).Liu M, Zhang C, Gong X, Zhang T, Lian MM, Chew EGY, Cardilla A, Suzuki K, Wang H, Yuan Y, Li Y, Naik MY, Wang Y, Zhou B, Soon WZ, Aizawa E, Li P, Low JH, Tandiono M, Montagud E, Moya-Rull D, Rodriguez Esteban C, Luque Y, Fang M, Khor CC, Montserrat N, Campistol JM, Izpisua Belmonte JC, Foo JN, Xia Y. Kidney organoid models reveal cilium-autophagy metabolic axis as a therapeutic target for PKD both in vitro and in vivo. Cell Stem Cell. 2024;31:P52–P70. doi: 10.1016/j.stem.2023.12.003. [DOI] [PubMed] [Google Scholar]
- Long et al. (2013).Long EO, Sik Kim H, Liu D, Peterson ME, Rajagopalan S. Controlling natural killer cell responses: integration of signals for activation and inhibition. Annual Review of Immunology. 2013;31:227–258. doi: 10.1146/annurev-immunol-020711-075005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo et al. (2021).Longo SK, Guo MG, Ji AL, Khavari PA. Integrating single-cell and spatial transcriptomics to elucidate intercellular tissue dynamics. Nature Reviews Genetics. 2021;22:627–644. doi: 10.1038/s41576-021-00370-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma et al. (2022).Ma X, Lu Y, Zhou Z, Li Q, Chen X, Wang W, Jin Y, Hu Z, Chen G, Deng Q, Shang W, Wang H, Fu H, He X, Feng X-H, Zhu S. Human expandable pancreatic progenitorderived β cells ameliorate diabetes. Science Advances. 2022;8:eabk1826. doi: 10.1126/sciadv.abk1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao et al. (2024).Mao Y, Wang W, Yang J, Zhou X, Lu Y, Gao J, Wang X, Wen L, Fu W, Tang F. Drug repurposing screening and mechanism analysis based on human colorectal cancer organoids. Protein & Cell. 2024;15:285–304. doi: 10.1093/procel/pwad038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matano et al. (2015).Matano M, Date S, Shimokawa M, Takano A, Fujii M, Ohta Y, Watanabe T, Kanai T, Sato T. Modeling colorectal cancer using CRISPR-Cas9-mediated engineering of human intestinal organoids. Nature Medicine. 2015;21:256–262. doi: 10.1038/nm.3802. [DOI] [PubMed] [Google Scholar]
- McGranahan & Swanton (2017).McGranahan N, Swanton C. Clonal heterogeneity and tumor evolution: past, present, and the future. Cell. 2017;168:613–628. doi: 10.1016/j.cell.2017.01.018. [DOI] [PubMed] [Google Scholar]
- Messner et al. (2013).Messner S, Agarkova I, Moritz W, Kelm JM. Multi-cell type human liver microtissues for hepatotoxicity testing. Archives of Toxicology. 2013;87:209–213. doi: 10.1007/s00204-012-0968-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller et al. (2018).Miller AJ, Hill DR, Nagy MS, Aoki Y, Dye BR, Chin AM, Huang S, Zhu F, White ES, Lama V, Spence JR. In vitro induction and in vivo engraftment of lung bud tip progenitor cells derived from human pluripotent stem cells. Stem Cell Reports. 2018;10:101–119. doi: 10.1016/j.stemcr.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills et al. (2019).Mills RJ, Parker BL, Quaife-Ryan GA, Voges HK, Needham EJ, Bornot A, Ding M, Andersson H, Polla M, Elliott DA, Drowley L, Clausen M, Plowright AT, Barrett IP, Wang Q-D, James DE, Porrello ER, Hudson JE. Drug Screening in human PSC-cardiac organoids identifies pro-proliferative compounds acting via the mevalonate pathway. Cell Stem Cell. 2019;24 doi: 10.1016/j.stem.2019.03.009. [DOI] [PubMed] [Google Scholar]
- Mohammadi et al. (2021).Mohammadi S, Morell-Perez C, Wright CW, Wyche TP, White CH, Sana TR, Lieberman LA. Assessing donor-to-donor variability in human intestinal organoid cultures. Stem Cell Reports. 2021;16:2364–2378. doi: 10.1016/j.stemcr.2021.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morizane et al. (2017).Morizane A, Kikuchi T, Hayashi T, Mizuma H, Takara S, Doi H, Mawatari A, Glasser MF, Shiina T, Ishigaki H, Itoh Y, Okita K, Yamasaki E, Doi D, Onoe H, Ogasawara K, Yamanaka S, Takahashi J. MHC matching improves engraftment of iPSC-derived neurons in non-human primates. Nature Communications. 2017;8:385. doi: 10.1038/s41467-017-00926-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mun et al. (2019).Mun SJ, Ryu JS, Lee MO, Son YS, Oh SJ, Cho HS, Son MY, Kim DS, Kim SJ, Yoo HJ, Lee HJ, Kim J, Jung CR, Chung KS, Son MJ. Generation of expandable human pluripotent stem cell-derived hepatocyte-like liver organoids. Journal of Hepatology. 2019;71:970–985. doi: 10.1016/j.jhep.2019.06.030. [DOI] [PubMed] [Google Scholar]
- Murata et al. (2020).Murata K, Ikegawa M, Minatoya K, Masumoto H. Strategies for immune regulation in iPS cell-based cardiac regenerative medicine. Inflammation and Regeneration. 2020;40:36. doi: 10.1186/s41232-020-00145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutuku et al. (2022).Mutuku SM, Spotbeen X, Trim PJ, Snel MF, Butler LM, Swinnen JV. Unravelling prostate cancer heterogeneity using spatial approaches to lipidomics and transcriptomics. Cancers. 2022;14:1702. doi: 10.3390/cancers14071702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakano et al. (2012).Nakano T, Ando S, Takata N, Kawada M, Muguruma K, Sekiguchi K, Saito K, Yonemura S, Eiraku M, Sasai Y. Self-formation of optic cups and storable stratified neural retina from human ESCs. Cell Stem Cell. 2012;10:771–785. doi: 10.1016/j.stem.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Nerger et al. (2024).Nerger BA, Sinha S, Lee NN, Cheriyan M, Bertsch P, Johnson CP, Mahadevan L, Bonventre JV, Mooney DJ. 3D hydrogel encapsulation regulates nephrogenesis in kidney organoids. Advanced Materials. 2024;36:e2308325. doi: 10.1002/adma.202308325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie et al. (2018a).Nie Y-Z, Zheng Y-W, Miyakawa K, Murata S, Zhang R-R, Sekine K, Ueno Y, Takebe T, Wakita T, Ryo A, Taniguchi H. Recapitulation of hepatitis B virus-host interactions in liver organoids from human induced pluripotent stem cells. EBioMedicine. 2018a;35:114–123. doi: 10.1016/j.ebiom.2018.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie et al. (2018b).Nie YZ, Zheng YW, Ogawa M, Miyagi E, Taniguchi H. Human liver organoids generated with single donor-derived multiple cells rescue mice from acute liver failure. Stem Cell Research & Therapy. 2018b;9:5. doi: 10.1186/s13287-017-0749-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nilsson Hall et al. (2020).Nilsson Hall G, Mendes LF, Gklava C, Geris L, Luyten FP, Papantoniou I. Developmentally engineered callus organoid bioassemblies exhibit predictive in vivo long bone healing. Advanced Science. 2020;7:1902295. doi: 10.1002/advs.201902295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouchi et al. (2019).Ouchi R, Togo S, Kimura M, Shinozawa T, Koido M, Koike H, Thompson W, Karns RA, Mayhew CN, McGrath PS, McCauley HA, Zhang R-R, Lewis K, Hakozaki S, Ferguson A, Saiki N, Yoneyama Y, Takeuchi I, Mabuchi Y, Akazawa C, Yoshikawa HY, Wells JM, Takebe T. Modeling steatohepatitis in humans with pluripotent stem cell-derived organoids. Cell Metabolism. 2019;30:374–384.e376. doi: 10.1016/j.cmet.2019.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaro et al. (2023).Pagliaro A, Finger R, Zoutendijk I, Bunschuh S, Clevers H, Hendriks D, Artegiani B. Temporal morphogen gradient-driven neural induction shapes single expanded neuroepithelium brain organoids with enhanced cortical identity. Nature Communications. 2023;14:7361. doi: 10.1038/s41467-023-43141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, Georgescu & Huh (2019).Park SE, Georgescu A, Huh D. Organoids-on-a-chip. Science. 2019;364:960–965. doi: 10.1126/science.aaw7894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park et al. (2024).Park SJ, Kim YY, Han JY, Kim SW, Kim H, Ku S-Y. Advancements in human embryonic stem cell research: clinical applications and ethical issues. Tissue Engineering and Regenerative Medicine. 2024;21:379–394. doi: 10.1007/s13770-024-00627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parseh et al. (2022).Parseh B, Khosravi A, Fazel A, Ai J, Ebrahimi-Barough S, Verdi J, Shahbazi M. 3-dimensional model to study apoptosis induction of activated natural killer cells conditioned medium using patient-derived colorectal cancer organoids. Frontiers in Cell and Developmental Biology. 2022;10:895284. doi: 10.3389/fcell.2022.895284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng et al. (2018).Peng WC, Logan CY, Fish M, Anbarchian T, Aguisanda F, Álvarez Varela A, Wu P, Jin Y, Zhu J, Li B, Grompe M, Wang B, Nusse R. Inflammatory cytokine TNFα promotes the long-term expansion of primary hepatocytes in 3D culture. Cell. 2018;175(6):1607–1619. doi: 10.1016/j.cell.2018.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrone & Zilbauer (2021).Perrone F, Zilbauer M. Biobanking of human gut organoids for translational research. Experimental & Molecular Medicine. 2021;53:1451–1458. doi: 10.1038/s12276-021-00606-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poplaski et al. (2023).Poplaski V, Bomidi C, Kambal A, Nguyen-Phuc H, Di Rienzi SC, Danhof HA, Zeng XL, Feagins LA, Deng N, Vilar E, McAllister F, Coarfa C, Min S, Kim HJ, Shukla R, Britton R, Estes MK, Blutt SE. Human intestinal organoids from Cronkhite-Canada syndrome patients reveal link between serotonin and proliferation. Journal of Clinical Investigation. 2023;133(21):e166884. doi: 10.1172/JCI166884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptasinski et al. (2023).Ptasinski V, Monkley SJ, Ost K, Tammia M, Alsafadi HN, Overed-Sayer C, Hazon P, Wagner DE, Murray LA. Modeling fibrotic alveolar transitional cells with pluripotent stem cell-derived alveolar organoids. Life Science Alliance. 2023;6(8):e202201853. doi: 10.26508/lsa.202201853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao et al. (2021).Rao A, Barkley D, Franca GS, Yanai I. Exploring tissue architecture using spatial transcriptomics. Nature. 2021;596:211–220. doi: 10.1038/s41586-021-03634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao et al. (2025).Rao M, Liu C-C, Wang S, Chang K-C. Generating ESC-derived RGCs for cell replacement therapy. Methods in Molecular Biology. 2025;2848:187–196. doi: 10.1007/978-1-0716-4087-6_12. [DOI] [PubMed] [Google Scholar]
- Regent et al. (2020).Regent F, Chen HY, Kelley RA, Qu Z, Swaroop A, Li T. A simple and efficient method for generating human retinal organoids. Molecular Vision. 2020;26:97–105. [PMC free article] [PubMed] [Google Scholar]
- Rossi, Manfrin & Lutolf (2018).Rossi G, Manfrin A, Lutolf MP. Progress and potential in organoid research. Nature Reviews Genetics. 2018;19:671–687. doi: 10.1038/s41576-018-0051-9. [DOI] [PubMed] [Google Scholar]
- Sahabian et al. (2021).Sahabian A, Dahlmann J, Martin U, Olmer R. Production and cryopreservation of definitive endoderm from human pluripotent stem cells under defined and scalable culture conditions. Nature Protocols. 2021;16:1581–1599. doi: 10.1038/s41596-020-00470-5. [DOI] [PubMed] [Google Scholar]
- Sampaziotis et al. (2021).Sampaziotis F, Muraro D, Tysoe OC, Sawiak S, Beach TE, Godfrey EM, Upponi SS, Brevini T, Wesley BT, Garcia-Bernardo J, Mahbubani K, Canu G, Gieseck 3rd R, Berntsen NL, Mulcahy VL, Crick K, Fear C, Robinson S, Swift L, Gambardella L, Bargehr J, Ortmann D, Brown SE, Osnato A, Murphy MP, Corbett G, Gelson WTH, Mells GF, Humphreys P, Davies SE, Amin I, Gibbs P, Sinha S, Teichmann SA, Butler AJ, See TC, Melum E, Watson CJE, Saeb-Parsy K, Vallier L. Cholangiocyte organoids can repair bile ducts after transplantation in the human liver. Science. 2021;371:839–846. doi: 10.1126/science.aaz6964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santamaria et al. (2023).Santamaria X, Roson B, Perez-Moraga R, Venkatesan N, Pardo-Figuerez M, Gonzalez-Fernandez J, Llera-Oyola J, Fernández E, Moreno I, Salumets A, Vankelecom H, Vilella F, Simon C. Decoding the endometrial niche of Asherman’s syndrome at single-cell resolution. Nature Communications. 2023;14:5890. doi: 10.1038/s41467-023-41656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato et al. (2009).Sato T, Vries RG, Snippert HJ, Van de Wetering M, Barker N, Stange DE, Van Es JH, Abo A, Kujala P, Peters PJ, Clevers H. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- Savoj et al. (2022).Savoj S, Esfahani MHN, Karimi A, Karamali F. Integrated stem cells from apical papilla in a 3D culture system improve human embryonic stem cell derived retinal organoid formation. Life Sciences. 2022;291:120273. doi: 10.1016/j.lfs.2021.120273. [DOI] [PubMed] [Google Scholar]
- Schneeberger et al. (2020).Schneeberger K, Sanchez-Romero N, Ye S, Van Steenbeek FG, Oosterhoff LA, Pla Palacin I, Chen C, Van Wolferen ME, Van Tienderen G, Lieshout R, Colemonts-Vroninks H, Schene I, Hoekstra R, Verstegen MMA, Van der Laan LJW, Penning LC, Fuchs SA, Clevers H, De Kock J, Baptista PM, Spee B. Large-scale production of LGR5-positive bipotential human liver stem cells. Hepatology. 2020;72:257–270. doi: 10.1002/hep.31037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster et al. (2020).Schuster B, Junkin M, Kashaf SS, Romero-Calvo I, Kirby K, Matthews J, Weber CR, Rzhetsky A, White KP, Tay S. Automated microfluidic platform for dynamic and combinatorial drug screening of tumor organoids. Nature Communications. 2020;11:5271. doi: 10.1038/s41467-020-19058-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutgens et al. (2019).Schutgens F, Rookmaaker MB, Margaritis T, Rios A, Ammerlaan C, Jansen J, Gijzen L, Vormann M, Vonk A, Viveen M, Yengej FY, Derakhshan S, de Winter-de Groot KM, Artegiani B, van Boxtel R, Cuppen E, Hendrickx APA, Van den Heuvel-Eibrink MM, Heitzer E, Lanz H, Beekman J, Murk J-L, Masereeuw R, Holstege F, Drost J, Verhaar MC, Clevers H. Tubuloids derived from human adult kidney and urine for personalized disease modeling. Nature Biotechnology. 2019;37:303–313. doi: 10.1038/s41587-019-0048-8. [DOI] [PubMed] [Google Scholar]
- Seguret et al. (2024).Seguret M, Davidson P, Robben S, Jouve C, Pereira C, Lelong Q, Deshayes L, Cerveau C, Le Berre M, Rodrigues Ribeiro RS, Hulot JS. A versatile high-throughput assay based on 3D ring-shaped cardiac tissues generated from human induced pluripotent stem cell-derived cardiomyocytes. Elife. 2024;12:RP87739. doi: 10.7554/eLife.87739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafiee et al. (2023).Shafiee A, Sun J, Ahmed IA, Phua F, Rossi GR, Lin CY, Souza-Fonseca-Guimaraes F, Wolvetang EJ, Brown J, Khosrotehrani K. Development of physiologically relevant skin organoids from human induced pluripotent stem cells. Small. 2023;20(16):e2304879. doi: 10.1002/smll.202304879. [DOI] [PubMed] [Google Scholar]
- Shen et al. (2018).Shen C-C, Hsu M-N, Chang C-W, Lin M-W, Hwu J-R, Tu Y, Hu Y-C. Synthetic switch to minimize CRISPR off-target effects by self-restricting Cas9 transcription and translation. Nucleic Acids Research. 2018;47:e13-e13. doi: 10.1093/nar/gky1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen et al. (2024).Shen C, Wang J, Li G, Hao S, Wu Y, Song P, Han Y, Li M, Wang G, Xu K, Zhang H, Ren X, Jing Y, Yang R, Geng Z, Su J. Boosting cartilage repair with silk fibroin-DNA hydrogel-based cartilage organoid precursor. Bioactive Materials. 2024;35:429–444. doi: 10.1016/j.bioactmat.2024.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi et al. (2020).Shi R, Radulovich N, Ng C, Liu N, Notsuda H, Cabanero M, Martins-Filho SN, Raghavan V, Li Q, Mer AS, Rosen JC, Li M, Wang Y-H, Tamblyn L, Pham N-A, Haibe-Kains B, Liu G, Moghal N, Tsao M-S. Organoid cultures as preclinical models of non-small cell lung Cancer. Clinical Cancer Research. 2020;26:1162–1174. doi: 10.1158/1078-0432.CCR-19-1376. [DOI] [PubMed] [Google Scholar]
- Shirai et al. (2016).Shirai H, Mandai M, Matsushita K, Kuwahara A, Yonemura S, Nakano T, Assawachananont J, Kimura T, Saito K, Terasaki H, Eiraku M, Sasai Y, Takahashi M. Transplantation of human embryonic stem cell-derived retinal tissue in two primate models of retinal degeneration. Proceedings of the National Academy of Sciences of the United States of America. 2016;113:E81–E90. doi: 10.1073/pnas.1512590113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirure, Hughes & George (2021).Shirure VS, Hughes CCW, George SC. Engineering vascularized organoid-on-a-chip models. Annual Review of Biomedical Engineering. 2021;23:141–167. doi: 10.1146/annurev-bioeng-090120-094330. [DOI] [PubMed] [Google Scholar]
- Shrestha et al. (2024).Shrestha S, Acharya P, Kang SY, Vanga MG, Lekkala VKR, Liu J, Yang Y, Joshi P, Lee MY. Regenerative human liver organoids (HLOs) in a pillar/perfusion plate for hepatotoxicity assays. BioRxiv. 2024 doi: 10.1101/2024.03.25.586638. [DOI]
- Silva et al. (2019).Silva TP, Cotovio JP, Bekman E, Carmo-Fonseca M, Cabral JMS, Fernandes TG. Design principles for pluripotent stem cell-derived organoid engineering. Stem Cells International. 2019;2019:1–17. doi: 10.1155/2019/4508470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simsa et al. (2021).Simsa R, Rothenbucher T, Gurbuz H, Ghosheh N, Emneus J, Jenndahl L, Kaplan DL, Bergh N, Serrano AM, Fogelstrand P. Brain organoid formation on decellularized porcine brain ECM hydrogels. PLOS ONE. 2021;16:e0245685. doi: 10.1371/journal.pone.0245685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence et al. (2011).Spence JR, Mayhew CN, Rankin SA, Kuhar MF, Vallance JE, Tolle K, Hoskins EE, Kalinichenko VV, Wells SI, Zorn AM, Shroyer NF, Wells JM. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro. Nature. 2011;470:105–109. doi: 10.1038/nature09691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sridhar et al. (2020).Sridhar A, Hoshino A, Finkbeiner CR, Chitsazan A, Dai L, Haugan AK, Eschenbacher KM, Jackson DL, Trapnell C, Bermingham-McDonogh O, Glass I, Reh TA. Single-cell transcriptomic comparison of human fetal retina, hPSC-derived retinal organoids, and long-term retinal cultures. Cell Reports. 2020;30:1644–1659. doi: 10.1016/j.celrep.2020.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strikoudis et al. (2019).Strikoudis A, Cieślak A, Loffredo L, Chen Y-W, Patel N, Saqi A, Lederer DJ, Snoeck H-W. Modeling of fibrotic lung disease using 3D organoids derived from human pluripotent stem Cells. Cell Reports. 2019;27(12):3709–3723. doi: 10.1016/j.celrep.2019.05.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun et al. (2024).Sun L, Wan AH, Yan S, Liu R, Li J, Zhou Z, Wu R, Chen D, Bu X, Ou J, Li K, Lu X, Wan G, Ke Z. A multidimensional platform of patient-derived tumors identifies drug susceptibilities for clinical lenvatinib resistance. Acta Pharmaceutica Sinica B. 2024;14:223–240. doi: 10.1016/j.apsb.2023.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun et al. (2019).Sun L, Wang Y, Cen J, Ma X, Cui L, Qiu Z, Zhang Z, Li H, Yang RZ, Wang C, Chen X, Wang L, Ye Y, Zhang H, Pan G, Kang JS, Ji Y, Zheng YW, Zheng S, Hui L. Modelling liver cancer initiation with organoids derived from directly reprogrammed human hepatocytes. Nature Cell Biology. 2019;21:1015–1026. doi: 10.1038/s41556-019-0359-5. [DOI] [PubMed] [Google Scholar]
- Suzuki et al. (2020).Suzuki D, Flahou C, Yoshikawa N, Stirblyte I, Hayashi Y, Sawaguchi A, Akasaka M, Nakamura S, Higashi N, Xu H, Matsumoto T, Fujio K, Manz MG, Hotta A, Takizawa H, Eto K, Sugimoto N. iPSC-derived platelets depleted of HLA class i are inert to anti-HLA class i and natural killer cell immunity. Stem Cell Reports. 2020;14:49–59. doi: 10.1016/j.stemcr.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taguchi et al. (2014).Taguchi A, Kaku Y, Ohmori T, Sharmin S, Ogawa M, Sasaki H, Nishinakamura R. Redefining the in vivo origin of metanephric nephron progenitors enables generation of complex kidney structures from pluripotent stem cells. Cell Stem Cell. 2014;14:53–67. doi: 10.1016/j.stem.2013.11.010. [DOI] [PubMed] [Google Scholar]
- Takasato et al. (2015).Takasato M, Er PX, Chiu HS, Maier B, Baillie GJ, Ferguson C, Parton RG, Wolvetang EJ, Roost MS, Chuva de Sousa Lopes SM, Little MH. Kidney organoids from human iPS cells contain multiple lineages and model human nephrogenesis. Nature. 2015;526:564–568. doi: 10.1038/nature15695. [DOI] [PubMed] [Google Scholar]
- Takebe et al. (2013).Takebe T, Sekine K, Enomura M, Koike H, Kimura M, Ogaeri T, Zhang RR, Ueno Y, Zheng YW, Koike N, Aoyama S, Adachi Y, Taniguchi H. Vascularized and functional human liver from an iPSC-derived organ bud transplant. Nature. 2013;499:481–484. doi: 10.1038/nature12271. [DOI] [PubMed] [Google Scholar]
- Takebe et al. (2017).Takebe T, Sekine K, Kimura M, Yoshizawa E, Ayano S, Koido M, Funayama S, Nakanishi N, Hisai T, Kobayashi T, Kasai T, Kitada R, Mori A, Ayabe H, Ejiri Y, Amimoto N, Yamazaki Y, Ogawa S, Ishikawa M, Kiyota Y, Sato Y, Nozawa K, Okamoto S, Ueno Y, Taniguchi H. Massive and reproducible production of liver buds entirely from human pluripotent stem cells. Cell Reports. 2017;21:2661–2670. doi: 10.1016/j.celrep.2017.11.005. [DOI] [PubMed] [Google Scholar]
- Tam et al. (2021).Tam WL, Freitas Mendes L, Chen X, Lesage R, Van Hoven I, Leysen E, Kerckhofs G, Bosmans K, Chai YC, Yamashita A, Tsumaki N, Geris L, Roberts SJ, Luyten FP. Human pluripotent stem cell-derived cartilaginous organoids promote scaffold-free healing of critical size long bone defects. Stem Cell Research & Therapy. 2021;12:513. doi: 10.1186/s13287-021-02580-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unbekandt & Davies (2010).Unbekandt M, Davies JA. Dissociation of embryonic kidneys followed by reaggregation allows the formation of renal tissues. Kidney International. 2010;77:407–416. doi: 10.1038/ki.2009.482. [DOI] [PubMed] [Google Scholar]
- Velasco et al. (2019).Velasco S, Kedaigle AJ, Simmons SK, Nash A, Rocha M, Quadrato G, Paulsen B, Nguyen L, Adiconis X, Regev A, Levin JZ, Arlotta P. Individual brain organoids reproducibly form cell diversity of the human cerebral cortex. Nature. 2019;570:523–527. doi: 10.1038/s41586-019-1289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velazquez et al. (2021).Velazquez JJ, LeGraw R, Moghadam F, Tan Y, Kilbourne J, Maggiore JC, Hislop J, Liu S, Cats D, Chuva De Sousa Lopes SM, Plaisier C, Cahan P, Kiani S, Ebrahimkhani MR. Gene regulatory network analysis and engineering directs development and vascularization of multilineage human liver organoids. Cell Systems. 2021;12:41–55 e11. doi: 10.1016/j.cels.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volmert et al. (2023).Volmert B, Kiselev A, Juhong A, Wang F, Riggs A, Kostina A, O’Hern C, Muniyandi P, Wasserman A, Huang A, Lewis-Israeli Y, Panda V, Bhattacharya S, Lauver A, Park S, Qiu Z, Zhou C, Aguirre A. A patterned human primitive heart organoid model generated by pluripotent stem cell self-organization. Nature Communications. 2023;14:8245. doi: 10.1038/s41467-023-43999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahle et al. (2023).Wahle P, Brancati G, Harmel C, He Z, Gut G, Del Castillo JS, Xavier da Silveira Dos Santos A, Yu Q, Noser P, Fleck JS, Gjeta B, Pavlinić D, Picelli S, Hess M, Schmidt GW, Lummen TTA, Hou Y, Galliker P, Goldblum D, Balogh M, Cowan CS, Scholl HPN, Roska B, Renner M, Pelkmans L, Treutlein B, Camp JG. Multimodal spatiotemporal phenotyping of human retinal organoid development. Nature Biotechnology. 2023;41:1765–1775. doi: 10.1038/s41587-023-01747-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2020).Wang D, Wang J, Bai L, Pan H, Feng H, Clevers H, Zeng YA. Long-Term expansion of pancreatic islet organoids from resident procr(+) progenitors. Cell. 2020;180:1198–1211. doi: 10.1016/j.cell.2020.02.048. [DOI] [PubMed] [Google Scholar]
- Wang, Andrade & Smith (2023).Wang E, Andrade MJ, Smith Q. Vascularized liver-on-a-chip model to investigate nicotine-induced dysfunction. Biomicrofluidics. 2023;17:064108. doi: 10.1063/5.0172677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2021a).Wang N, Li X, Wang R, Ding Z. Spatial transcriptomics and proteomics technologies for deconvoluting the tumor microenvironment. Biotechnology Journal. 2021a;16:e2100041. doi: 10.1002/biot.202100041. [DOI] [PubMed] [Google Scholar]
- Wang et al. (2021b).Wang X, Wang S, Guo B, Su Y, Tan Z, Chang M, Diao J, Zhao Y, Wang Y. Human primary epidermal organoids enable modeling of dermatophyte infections. Cell Death and Disease. 2021b;12:35. doi: 10.1038/s41419-020-03330-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie et al. (2022).Xie C, Liang R, Ye J, Peng Z, Sun H, Zhu Q, Shen X, Hong Y, Wu H, Sun W, Yao X, Li J, Zhang S, Zhang X, Ouyang H. High-efficient engineering of osteo-callus organoids for rapid bone regeneration within one month. Biomaterials. 2022;288:121741. doi: 10.1016/j.biomaterials.2022.121741. [DOI] [PubMed] [Google Scholar]
- Xie et al. (2020).Xie H, Zhang W, Zhang M, Akhtar T, Li Y, Yi W, Sun X, Zuo Z, Wei M, Fang X, Yao Z, Dong K, Zhong S, Liu Q, Shen Y, Wu Q, Wang X, Zhao H, Bao J, Qu K, Xue T. Chromatin accessibility analysis reveals regulatory dynamics of developing human retina and hiPSC-derived retinal organoids. Science Advances. 2020;6:eaay5247. doi: 10.1126/sciadv.aay5247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu et al. (2018).Xu H, Lyu X, Yi M, Zhao W, Song Y, Wu K. Organoid technology and applications in cancer research. Journal of Hematology & Oncology. 2018;11:116. doi: 10.1186/s13045-018-0662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu et al. (2019).Xu H, Wang B, Ono M, Kagita A, Fujii K, Sasakawa N, Ueda T, Gee P, Nishikawa M, Nomura M, Kitaoka F, Takahashi T, Okita K, Yoshida Y, Kaneko S, Hotta A. Targeted disruption of HLA genes via CRISPR-Cas9 generates iPSCs with enhanced immune compatibility. Cell Stem Cell. 2019;24:566–578 e567. doi: 10.1016/j.stem.2019.02.005. [DOI] [PubMed] [Google Scholar]
- Yamada & Nomura (2020).Yamada S, Nomura S. Review of single-cell RNA sequencing in the heart. International Journal of Molecular Sciences. 2020;21:8345. doi: 10.3390/ijms21218345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto et al. (2017).Yamamoto Y, Gotoh S, Korogi Y, Seki M, Konishi S, Ikeo S, Sone N, Nagasaki T, Matsumoto H, Muro S, Ito I, Hirai T, Kohno T, Suzuki Y, Mishima M. Long-term expansion of alveolar stem cells derived from human iPS cells in organoids. Nature Methods. 2017;14:1097–1106. doi: 10.1038/nmeth.4448. [DOI] [PubMed] [Google Scholar]
- Yang et al. (2024).Yang H, Cheng J, Zhuang H, Xu H, Wang Y, Zhang T, Yang Y, Qian H, Lu Y, Han F, Cao L, Yang N, Liu R, Yang X, Zhang J, Wu J, Zhang N. Pharmacogenomic profiling of intra-tumor heterogeneity using a large organoid biobank of liver cancer. Cancer Cell. 2024;42:P531–P551. doi: 10.1016/j.ccell.2024.03.004. [DOI] [PubMed] [Google Scholar]
- Yoshihara et al. (2020).Yoshihara E, O’Connor C, Gasser E, Wei Z, Oh TG, Tseng TW, Wang D, Cayabyab F, Dai Y, Yu RT, Liddle C, Atkins AR, Downes M, Evans RM. Immune-evasive human isletlike organoids ameliorate diabetes. Nature. 2020;586:606–611. doi: 10.1038/s41586-020-2631-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu (2020).Yu J. Vascularized organoids: a more complete model. International Journal of Stem Cells. 2020;14:127–137. doi: 10.15283/ijsc20143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahmatkesh et al. (2021).Zahmatkesh E, Ghanian MH, Zarkesh I, Farzaneh Z, Halvaei M, Heydari Z, Moeinvaziri F, Othman A, Ruoss M, Piryaei A, Gramignoli R, Yakhkeshi S, Nussler A, Najimi M, Baharvand H, Vosough M. Tissue-specific microparticles improve organoid microenvironment for efficient maturation of pluripotent stem-cell-derived hepatocytes. Cells. 2021;10:1274. doi: 10.3390/cells10061274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng et al. (2021).Zeng Z, Huang B, Parvez RK, Li Y, Chen J, Vonk AC, Thornton ME, Patel T, Rutledge EA, Kim AD, Yu J, Grubbs BH, McMahon JA, Pastor-Soler NM, Hallows KR, McMahon AP, Li Z. Generation of patterned kidney organoids that recapitulate the adult kidney collecting duct system from expandable ureteric bud progenitors. Nature Communications. 2021;12:3641. doi: 10.1038/s41467-021-23911-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2023).Zhang CJ, Meyer SR, O’Meara MJ, Huang S, Capeling MM, Ferrer-Torres D, Childs CJ, Spence JR, Fontana RJ, Sexton JZ. A human liver organoid screening platform for DILI risk prediction. Journal of Hepatology. 2023;78:998–1006. doi: 10.1016/j.jhep.2023.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang et al. (2017).Zhang YS, Aleman J, Shin SR, Kilic T, Kim D, Mousavi Shaegh SA, Massa S, Riahi R, Chae S, Hu N, Avci H, Zhang W, Silvestri A, Nezhad ASanati, Manbohi A, De Ferrari F, Polini A, Calzone G, Shaikh N, Alerasool P, Budina E, Kang J, Bhise N, Ribas J, Pourmand A, Skardal A, Shupe T, Bishop CE, Dokmeci MR, Atala A, Khademhosseini A. Multisensor-integrated organs-on-chips platform for automated and continual in situ monitoring of organoid behaviors. Proceedings of the National Academy of Sciences of the United States of America. 2017;114:E2293–E2302. doi: 10.1073/pnas.1612906114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao et al. (2011).Zhao T, Zhang Z-N, Rong Z, Xu Y. Immunogenicity of induced pluripotent stem cells. Nature. 2011;474:212–215. doi: 10.1038/nature10135. [DOI] [PubMed] [Google Scholar]
- Zhou et al. (2017).Zhou T, Tan L, Cederquist GY, Fan Y, Hartley BJ, Mukherjee S, Tomishima M, Brennand KJ, Zhang Q, Schwartz RE, Evans T, Studer L, Chen S. High-content screening in hPSC-neural progenitors identifies drug candidates that inhibit zika virus infection in fetal-like organoids and adult brain. Cell Stem Cell. 2017;21:274–283.e275. doi: 10.1016/j.stem.2017.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang et al. (2023).Zhuang B-M, Cao D-D, Liu X-F, Wang L, Lin X-L, Duan Y-G, Lee C-L, Chiu PCN, Yeung WSB, Yao Y-Q. Application of a JEG-3 organoid model to study HLA-G function in the trophoblast. Frontiers In Immunology. 2023;14:1130308. doi: 10.3389/fimmu.2023.1130308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zilch et al. (2018).Zilch A, Rien C, Weigel C, Huskobla S, Gluck B, Spengler K, Sauerbrei A, Heller R, Graler M, Henke A. Influence of sphingosine-1-phosphate signaling on HCMV replication in human embryonal lung fibroblasts. Medical Microbiology and Immunology. 2018;207:227–242. doi: 10.1007/s00430-018-0543-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
This is a literature review.