Abstract
We aimed to determine how a bout of resistance or aerobic exercise impacts physiological responses and performance during firefighting occupational tasks. Thirty-two non-firefighters completed two baseline assessments and three trials: resistance exercise (RE), aerobic exercise (AE), or a rested control (CON). Trials were followed by an occupational task assessment (OTA; four rounds of 10 deadlifts (38.6–61.4 kg) and 0.24-km 40lb-sandbag carry) in an environmental chamber (35 °C/50% humidity) while wearing standard municipal firefighter gear. Time to complete by condition was not statistically different (CON: 18.9 ± 4.4, AE: 20.0 ± 3.6, RE: 20.2 ± 5.0 min; p = 0.16). During the OTA average heart rate (CON: 149 ± 16, AE: 166 ± 12, RE: 160 ± 13 bpm; p < 0.01), estimated core temperature (CON: 37.6 ± 0.4, AE: 38.7 ± 0.3, RE: 38.4 ± 0.5 °C; p < 0.01), and skin temperature (CON: 36.3 ± 0.5, AE: 37.5 ± 0.6, RE: 36.9 ± 0.9 °C; p < 0.01) were elevated following AE and RE compared to CON, and higher following AE compared to RE. Our findings suggest job performance may not be impacted, although physiological stress during the tasks may be elevated, following on-shift exercise, and more prominently following aerobic exercise.
Keywords: Environmental stress, Occupational stress, Fire services, Strength training, Endurance training, HIIT
Subject terms: Physiology, Health occupations
Introduction
Firefighters are exposed to a broad spectrum of environments typically divided into two types: fireground (vehicle fires, wildfires, structural fires) and non-fireground (medical emergencies, vehicle accidents, natural disasters). Both can present a risk for heat stress ranging from hot summer temperatures upwards of 32 °C, and structural fires reaching extreme temperatures of 300 °C1. During such occupational tasks, personal protective equipment (PPE) is worn to protect firefighters from extreme heat2,3. The added weight (17–25 kg) and cumbersome nature of PPE can exacerbate the stress imposed on the firefighters due to the external load and limited mobility. Additionally, the insulative properties of PPE inhibit proper dissipate heat through evaporation of sweat. Combined, these limitations can lead to impairments in occupational performance2,4,5. Exertional heat stress is of particular concern when considering almost 75% of firefighters experiencing heat injury symptoms in a calendar year6. The high levels of physical and environmental stress imposed on firefighters reinforce the need for fitness training opportunities and physical fitness standards.
A study looking at the adaptations to fire academy training saw significant improvements in fitness during the training period that were subsequently lost when reassessed following firefighters’ probationary period (8 months later). Declines in aerobic capacity, muscular strength, muscular endurance, and increases in percent body fat suggest overall health and fitness declined once firefighters left the academy7. A National Fire Prevention Association (NFPA) report notes that 70% of firefighters do not meet recommended health and fitness guidelines8. As research suggests, poor fitness and lack of a well-designed training program decrease occupational performance and increase firefighters’ risk for overexertion injuries9,10 and cardiovascular disease/event risk11–13.
Research on exercise interventions in firefighters has revealed promising improvements in occupationally relevant fitness parameters, including general health outcomes14–17 and occupational performance18. However, only 27% of fire departments across the United States provide health and fitness programs8. Research has shown that firefighters who participated in on-shift (within the station) physical activity accumulated a higher level of total physical activity on a weekly basis and had better cardiovascular health indicators over those that do not15. Therefore, the importance of maintaining physical fitness despite the hectic work schedule makes it crucial that firefighters are provided time to exercise while on shift. However, it is crucial to consider the cumulative exertional stress this may impose.
Current literature indicates physiological measures (i.e., heart rate, skin temperature, ventilation, and core temperature) are intensified when performing simulated firefighting tasks19–24. Core temperature, heart rate, lactate concentrations, and workload are all increased in heated environments25–27. Firefighters have expressed uncertainty about adding the physiological stress of on-shift exercise to the stress of their daily job tasks28–30, concerned the added stress response may lead to decrements in occupational performance. Therefore, understanding the additional physiological stress that prior acute exercise could induce when a firefighter is performing occupational tasks is important in determining best exercise practice in firefighters. Two studies have investigated the effects of exercise training-induced fatigue on simulated firefighting tasks and the physiological stress experienced after a bout of acute exercise. These two studies reported a 9.6%31 and 45%32 increase in time to complete 10 min after acute exercise and a 9.8% increase in time to complete 60 min after exercise32, suggesting that a single on-shift exercise session may transiently impair the ability to meet occupational requirements. While one of these studies used circuit style training and the other involved high-intensity resistance training, no study to our knowledge has directly compared the acute impact of resistance training and aerobic endurance training on the physiological readiness of firefighters.
Therefore, the purpose of our study was to investigate the impact of resistance and aerobic endurance exercise on physiological outcomes and performance related to firefighter occupational performance. We hypothesized that aerobic exercise would have a greater impact on occupational performance compared to resistance training, by increasing time to complete and markers of physiological stress (heart rate, skin temperature, ventilation, estimated core temperature, and blood lactate concentrations (BLC)). A secondary aim was to determine if the acute exercise bouts would impair recovery following occupational tasks. We hypothesized that aerobic exercise would result in elevated physiological variables during recovery following occupational task compared to resistance training, in part due to increased cardiovascular demands and cumulative heat stress.
Methods
Study design
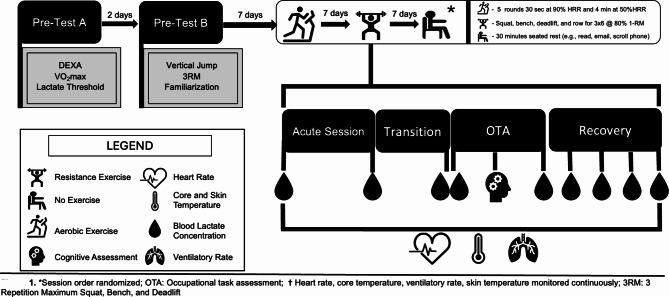
A repeated measures quasi-randomized control trial was used in the current investigation. Participants were local members of the community rather than firefighters in order to obtain an adequate sample size for the statistical analysis. Each participant completed a series of baseline assessments for cognitive, physiological, aerobic, and anaerobic performance outcome measures as a part of the larger study that was approved by the Institutional Review Board at Auburn University (IRB protocol code #22–479 AR 2211, 05/05/2022). Baseline assessments (Day A and B) have been outlined below as we will utilize values to quantify the fitness level of the population. Participants then completed three exercise sessions in quasi-randomized order: (1) resistance exercise (RE); (2) aerobic high-intensity interval training (AE); or (3) rested control (CON). Each exercise session was directly followed by an occupational task assessment (OTA). A seven-day wash-out period was included between trials to reduce the risk of fatigue from previous sessions impacting subsequent trial performance. Participants completed the CON condition second to reduce the number of potential unique trial order group comparisons. Block randomization of trial order of exercise type was generated in Microsoft® Excel (Microsoft Corporations, Redmond, WA USA) by a co-investigator and reported allocations to the lead author (P.J.A.). Independent variables included Pre-OTA condition (RE, AE, CON). The primary dependent variable was OTA time to complete, with secondary dependent variables including estimated core temperature, BLC, skin temperature, heart rate, and ventilatory rate. An overview of the study design can be found in Fig. 1.
Fig. 1.
*Denotes the exercise condition was randomized; OTA Occupational Task Assessment; heart rate, estimated core temperature, skin temperature, and ventilatory rate were monitored continuously.
Participants
Forty-one individuals were enrolled in the study. Thirty-two (15 males, 17 females) participants completed all study requirements (25.19 ± 4.12 yrs., 173.78 ± 9.84 cm, 75.57 ± 13.22 kg, 23.28 ± 7.43% body fat). All participants were individuals from the local community, none of which were current firefighters. Additionally, all participants met the following inclusion criteria: (i) 19–45 years of age, (ii) free of musculoskeletal injury, (iii) available to complete the full 5-week study timeline, (iv) comfortable carrying out exercise tasks while in a heat chamber, (v) agreed to adhere to study requirements, and (vi) passed a health screening. Participants were excluded if they: (i) had a known medical condition, physical or psychological condition, preventing participation in exercise, (ii) had a current musculoskeletal injury or were rehabilitating from a recent one, (iii) had been diagnosed with asthma (defined as experienced symptoms, or prescribed any form of treatment within the past 4 years), (iv) had a history of heart condition or high blood pressure, (v) experienced pain in their chest at rest, during activities of daily living, or when performing physical activity or exercise, (vi) had been prescribed medically supervised physical activity only by a primary care physician, or (vii) had recently experienced a heat related illness or injury (i.e., heat exhaustion, heat stroke, etc.). Informed consent was obtained by lead author (P.J.A.) prior to enrollment in the study. All interested participants were included. Out of the forty-one enrolled, five participants withdrew due to scheduling conflicts, three withdrew due to difficulty with the occupational task, one was withdrawn for their own safety due to lack of adhering to study protocols.
Procedures
All study procedures occurred in the School of Kinesiology buildings starting in January of 2023 and ending in August of 2023 when appropriate power was obtained. Each participant completed a baseline fitness assessment (Day A and B) prior to completing the acute exercise trials (Trials 1–3). Participants were asked to refrain from caffeine and recent exercise for 24 h leading up to Day A and Day B. Urine specific gravity was utilized as an indicator of hydration (USG < 1.02) of each participant and was assessed before testing on Day A and Day B. The urine sample was analyzed with a refractometer (V-Resourcing, Hunan, China). If the participant had a high USG which is an indicator of dehydration (USG = > 1.02), they were given 16 oz of water to drink and provided a new urine sample after 20 min. Participants were allowed to begin the visit if the second USG reading was below 1.02. Participants were encouraged to schedule visits at the same time of day and maintain a consistent diet during the duration of the study, however, it was not controlled.
Day A (body composition and aerobic fitness)
Body composition (fat, muscle, and bone mineral density) was measured with a full-body dual-energy X-ray absorptiometry (DXA) scan (Lunar Prodigy; GE Healthcare, Chicago, IL, USA). Participant’s height and weight were obtained utilizing a digital scale and stadiometer (SECA, Hamburg, Germany).
Peak oxygen consumption (VO2peak) was assessed as a measure of cardiorespiratory fitness level utilizing a modified Bruce protocol33 for treadmill (Woodway, Waukesha, WI, USA) graded exercise testing. During the test, oxygen consumption and carbon dioxide were monitored using indirect calorimetry with an automated open circuit system (Parvo Medics, Sandy UT). Before each test, gas analyzers were calibrated with standard gases (16% O2, 4.05% CO2) and the pneumotach flowmeter calibration was completed using a standard volume of air (3 L). Participants were asked to give their best effort and continue until they could go no longer. The test was terminated once participants reached volitional fatigue. VO2peak was determined as the maximal oxygen consumption achieved during the test. Respiratory exchange ratio (RER > 1.15), HRmax (within 10 bpm of age-predicted max), BLC (> 8.0 mM), and volitional fatigue, were utilized to verify a valid maximal effort was given by the participant.
At the end of each stage the participants’ fingertip were disinfected using an alcohol wipe and dried with a gauze pad. Once dried, a fingerstick was administered using a BD Microtainer ® auto-lancet (BD, Franklin Lakes, NJ USA) to draw a drop of blood from the participant’s fingertip. The first drop was wiped by the gauze pad and the second drop of blood was placed on the lactate test strip and inserted into the Nova Biomedical Lactate Plus Meter (Nova Biomedical, Waltham, MA USA) for measurement. The Lactate Plus Meter was calibrated bi-weekly during testing with low and high control solutions and the accuracy was confirmed to be within acceptable limits (i.e., low control solution: 1.0–1.6 mMol; high control solution: 4.0–5.4 mMol). Data collected from the Lactate Plus Meter was used to estimate lactate threshold as part of the larger study.
Day B (muscular strength, power, and familiarization)
Participants completed a counter-movement vertical jump on a Leonardo Mechanograph force platform (Novotec Medical GmbH, Pforzheim, Germany) as an assessment of lower body muscular power. The participant stepped onto the platform and was instructed by the research team to jump as high as possible. The vertical jump task was completed three times with a one-minute rest between attempts.
Three repetition maximum testing (3RM) performance was used to determine training load during the acute resistance training session, as well as an indicator of muscular strength. The squat, bench press, and hex-bar deadlift movements were used to assess upper and lower body strength. During each attempt, participants were provided spotters. For the squat exercise, participants were asked to place the barbell and attached weights on the top of the shoulders behind the head and complete a full squat. If the participant’s back angle began to change during the repetition, it was not counted. For the bench press exercise, they started by laying on their back on a lifting bench with five points of contact (head, shoulders, buttocks, and both feet flat on the floor). To complete the lift, participant touched the bar to their chest (with a slight pause on the chest) and raised back up to the starting position. For the hex-bar deadlift, participants lifted the weight bar from the ground, with both knees and hips bent while maintaining a constant back angle throughout. If the weight was hiked or slid up the thighs, or their back angle changed, the repetition was not counted. The hex-bar deadlift was utilized to reduce technical errors and potential injury risk in inexperienced lifters34. The participants were monitored by a certified strength and conditioning specialist (author - P.J.A.) to ensure they performed each exercise completely and with proper form. Participants started the 3RM protocol by completing the lift with a series of warm-up lifts (20.5 kg bar for 8–10 reps, 50% of projected 1-repetition maximum (1RM) for 6–8 reps, 75% for 3–5 reps, and 85% for 1–3 reps). Their first attempt was at 95% of self-reported 3RM. Each set included a minimum of two minutes of rest and a maximum of five minutes of rest. The maximum weight completed for three reps while maintaining good form was utilized to project 1RM based on the National Strength and Conditioning Association’s (NSCA) guidelines35. If participants only achieved one or two reps at attempted weight, that value was taken and utilized to project 1RM. During Day B, participants were also familiarized with the Occupational Task Assessment (OTA). They were instructed on how to don the standard firefighter PPE, including turn-out gear, gloves, boots, and a helmet. After which, they entered the chamber that was set at 35 °C (95 °F) with 50% relative humidity and practiced one round of the OTA to reduce any learning effect associated with the OTA.
Experimental trials
After the fitness assessments (Day A and B), the participants completed the acute exercise trials (Trials 1–3). Participants were asked to refrain from caffeine and exercise during the 24 h leading up to each of the three trials. Participant USG was measured as an indicator of hydration status before each trial. If the participant had a high USG which is an indicator of dehydration (USG = > 1.02), they were given 16 oz of water to drink and provided a new urine sample after 20 min. Participants were allowed to begin the visit if the second USG reading was below 1.02. Each of the acute exercise sessions were lead and monitored by a certified strength and conditioning professional (P.J.A.) and at least one other researcher.
Acute exercise and control trials
The full-body resistance exercise session was programmed utilizing NSCA guidelines for strength training36. Prior to starting the RE session, participants completed a structured warm-up. The warm-up protocol followed the NSCA’s recommended structure of a general and specific warm-up protocol, which involved a moderate-paced walk (4.8 kph) on a treadmill36 and dynamic movements that mimicked and prepared the participant for the movement patterns of the acute resistance exercises, including bodyweight squats, hip rotations, and scapular protraction and retraction36. After the warm-up, participants completed four exercises emphasizing each major movement in the following order:1) back squat, 2) barbell bench press, 3) hex-bar deadlift, and 4) barbell bent-over rows. Participants completed three sets of six repetitions of each exercise at ~ 80% of their projected 1-RM from baseline testing with two minutes of rest between sets. If a participant was unable to complete a set at the prescribed weight, the weight was lowered until the set was finished and remained at that weight for subsequent sets. BLC measurements were taken pre- and post-exercise. Total exercise time during resistance sessions varied between participants due to variability in the number of warm-up sets needed to reach working set weight.
The AE condition involved high-intensity interval training (HIIT), which was programmed utilizing aspects of the NSCA guidelines for aerobic endurance training and a 2018 investigation of a cycling HIIT protocol37,38. Prior to starting the AE session, participants completed a structured warm-up. The warm-up protocol followed the NSCA’s recommended structure of a general warm-up, involving a moderate-paced walk (4.8 kph) on a treadmill37. Each participant completed five rounds of low-intensity exercise for four minutes at approximately 50% of heart rate reserve (HRR) and 30 s of high intensity at approximately 90% of HRR on a treadmill. The HRR values were calculated with the Karvonen method39 utilizing resting and max heart rate values from the baseline assessments. Speed was self-selected by participants and then adjusted to match the prescribed heart rate zones listed above. BLC measurements were taken pre- and post-exercise. The aerobic exercise session was programmed to take approximately 27 min.
A control session was completed to assess any effect of exercise in general, regardless of modality. The control session involved participants sitting in our laboratory in a quiet, controlled environment where they could work on their laptops, scroll on their phones, browse the internet, or read a book. However, participants were told to avoid any stressful or overstimulating work (i.e., cognitively demanding tasks, competitive games, or dramatic/thriller television) and activities during the 30-minute time frame were recorded. The activity choices were decided in tandem with what the local Fire Department described as activities firefighters typically partake in during their on-duty downtime. BLC measurements were taken pre- and post-control session.
Transition period
Participants then donned standard municipal firefighting turnout gear and PPE for non-structural fire emergencies (boots, gloves, turnout jacket, turnout pants, and helmet; ~10.0 kg). BLC was once again assessed prior to entering the environmental chamber where participants completed the simulated occupational task assessment. Participants were encouraged to transition with a sense of urgency, but transition times were designed in order to closely reflect the expected response time of fire services. NFPA’s goal response time is 5 min and 20 s for 90% of incidences40, including 80 s to don gear and 240 s to travel while also accounting for the fact that there is additional time between arrival and entering the emergency situation not designated in the report.
Occupational task assessment (OTA)
The environmental chamber conditions were set to 35 °C (95 °F) with 50% relative humidity to mimic temperatures experienced during highway extractions on a hot summer day, other outdoor emergencies, and salvage41,42. 35 °C (95 °F) with 50% relative humidity was chosen, rather than hotter temperatures, to replicate non-fireground scenarios known to constitute ~ 80% of firefighters’ emergency calls in the southeastern United States28. Inside the chamber participants completed a series of tactically relevant physical exertion tasks involving repeated lifts, carrying, and walking movements. A Rogue Fitness® sandbag (Rogue Fitness, Columbus, OH, USA) was loaded to either 61.4 kg–38.6 kg. Sandbag loads were determined based on the frequency firefighters have to lift, drag, and carry objects of a similar size during emergency calls43. Participants utilized the 61.4 kg sandbag if their 3-RM deadlift was greater than 79.5 kg and if their deadlift to body weight ratio was greater than 1.25. Those that did not meet these criteria used a 38.6 kg sandbag. Once in the environmental chamber, participants completed 10 repeated sandbag deadlifts with the prescribed sandbag load. They then lifted a lighter Rogue Fitness® sandbag, loaded to 18.2 kg to mimic the average weight of a firehose, onto their shoulder and carried it while walking on a treadmill for 0.24 km. These movements were completed in a circuit twice, before stopping to promptly begin a cognitive assessment (part of the larger study). The cognitive assessment took on average 4.5 min to complete. Immediately after completing the cognitive assessment, participants then completed two additional rounds of the OTA. They were instructed to complete all tasks to the best of their ability and as quickly and safely as possible. Termination criteria included volitional fatigue. Additionally, for the safety of participants, they were removed from the environmental chamber if they reached an estimated core temperature of 39.4 °C due to the risk of heat stroke when participants reach a core temperature of 40 °C44.
Recovery protocol
Upon completion of the heat chamber protocol, participants were escorted out of the chamber and into an open area where they removed their helmet, gloves, and turnout jacket and sat in a chair. While recovering, they were allowed to roll their pants down below their knees. Boots were kept on to mimic the procedures firefighters follow during emergency call recovery. Participants were provided one bottle of room temperature water to rehydrate. Heart rate, skin temperature, ventilatory rate, and estimated core temperature were monitored continuously during the recovery period. BLC was assessed at immediate post-simulated firefighting, 5-, 10-, 20-, and 40-minute post-OTA.
Physiological monitoring and perceived exertion measurements
Heart rate, ventilatory rate, skin temperature, and estimated core temperature were monitored in real-time to assess the physiological stress and intensity of response during the entirety of each trial utilizing the Eq. 02 + LifeMonitor (Equivital Eq. 02, Hidalgo, UK). A validated heart-rate-derived algorithm45,46 is used by the Equivital Black Ghost software to estimate core temperature. The Equivital Black Ghost system has recently been shown as a valid alternative to gold-standard rectal temperature monitoring in similar environments and exercise conditions47. The Equivital measures skin temperature at the torso using an infrared temperature sensor on the back of the Equivital device, which is in contact with the individual’s skin, under the individual’s arm (at the mid-axillary line of the thorax in line with the individual’s xiphoid process of the sternum). BLC was measured before and after AE, RE, CON, and OTA. BLC was also measured during recovery at 5-, 10-, 20-, 30-, and 40-minute timepoints. BLC measurements were obtained using the Nova Biomedical Lactate Plus Meter and procedures are outlined above regarding lactate threshold testing during Day A. The OMNI 0–10 Rating of Perceived Exertion (RPE) scale was used during acute exercise, at the end of RE sets, at the end of both high and low intervals during AE, and the beginning and end of the control session. The Borg 6–20 RPE scale48 was also collected after each OTA task (i.e., sandbag deadlifts and sandbag carry) and every five minutes during recovery. The OMNI scale was used during RE to correlate to the number of Reps in Reserve (RIR)49 and to provide an accurate training intensity. It was also used during AE, allowing comparisons with RE perceived exertion. However, the Borg scale was used during the OTA because of its correlation to heart rate50.
Statistical analysis
The Shapiro-Wilks Test, Q-Q plot inspection, and Mauchly’s Test were used to evaluate normality and sphericity respectively. First, we conducted a traditional repeated measures analysis of variance (ANOVA) to compare total time to complete the OTA by condition, followed by an equivalence test for ANOVA to determine if the exercise conditions resulted in practically equivalent changes in time to complete OTA. A practical effect size to determine equivalence bounds was calculated based on the mean difference in time to complete OTA based on the recommendations of the local fire departments on the meaningful difference in time to complete the outlined tasks in an actual occupational scenario. The final value was then divided by the pooled standard deviation of time to complete OTA from the actual data collected in this study to obtain a practical effect size, which was then converted to a partial eta squared (η2p) utilizing the equation provided below.
Practical effect size equation:
 |
 |
The equivalence test was completed using the TOSTER package for R to compare the largest effect size observed between exercise conditions against a practical effect size of η2p = 0.11 (f = 1.382). Additional variables assessed to describe the physiological mechanisms behind performance changes included heart rate, estimated core temperature, skin temperature, ventilatory rate, blood lactate concentration, and rating of perceived exertion (RPE). Average values were calculated based on the minute-to-minute values for heart rate, estimated core temperature, skin temperature, and ventilatory rate during OTA and recovery. Additionally, the time to get to the environmental chamber and put on the firefighter gear (gear time) was compared between AE, RE, and CON to understand differences in time taken from exercise to OTA. Four-minute averages were calculated for each of these variables for graphic representation and area under the curve (AUC) calculations. The AUC was used as a metric of cumulative heat stress experienced accounting for the maximum temperature reached and the time spent at elevated estimated core temperatures. Five-minute change scores underwent trapezoidal summation to calculate the total AUC for both OTA and recovery. A repeated measures analysis of variance (ANOVA) was performed on average values for each of the measures to determine differences across conditions and recovery. Estimated core temperature was the only peak value assessed due to its relation to exertional heat illness risk51. Other peak values were not assessed to reduce the risk of type I error from multiple testing. Equivalence tests were not used for variables other than time to complete because it is unclear what a practically significant difference for these physiological variables would be. For any significant main effects detected, post-hoc comparisons with Bonferroni adjustments were utilized for multiple comparisons. If sphericity was violated, statistical interpretations were made utilizing Greenhouse-Geisser adjusted degrees of freedom. Data is expressed as mean ± standard deviation. Significance in this investigation was set a priori at a p-value ≤ 0.05 for all measurements. R Statistical Programming Software Version 4.1.2 (RStudio; Boston, MA) was used for all statistical analyses52. The application, G*Power, was utilized a priori to determine a sample size of 28 total participants necessary for a sufficiently powered study. The following values were used to estimate sample size: test family = F tests, repeated measures ANOVA, one group, three measurements, correlation among repeated measures = 0.5, non-sphericity correction ε = 1.0, α = 0.05, 1-β = 0.80, η2p = 0.06. Effect size classifications included a small effect (η2p = 0.010–0.059), moderate effect (η2p = 0.060–0.139), and large effect (η2p > 0.14). The effect size used to determine power was chosen based on previous research observing effect sizes from 0.01 to 0.56 with similar outcomes31,32.
Results
Baseline values
Pre-trial USG (F(2, 62) = 0.752; p = 0.475, η2p = 0.02) and Pre-BLC (F(2, 62) = 0.281; p = 0.281, η2p = 0.04) were not significantly different. Full demographic information can be found in Table 1.
Table 1.
Participant demographics.
| Variable | N | Mean ± SD | Min – Max [Range] | |
|---|---|---|---|---|
| Age (yrs) | Overall | 32 | 25.2 ± 4.1 | 19.0–35.0 [16.0] |
| Female | 15 | 26.1 ± 4.2 | 20.0–35.0 [15.0] | |
| Male | 17 | 24.4 ± 4.1 | 19.0–31.0 [12.0] | |
| Height (cm) | Overall | 32 | 173.8 ± 9.8 | 153.5–193.0 [39.5] |
| Female | 15 | 165.2 ± 5.7 | 153.5–175.3 [21.8] | |
| Male | 17 | 181.3 ± 5.4 | 171.5–193.0 [21.5] | |
| Weight (kg) | Overall | 32 | 75.6 ± 13.2 | 52.4–103.0 [50.6] |
| Female | 15 | 64.5 ± 6.5 | 52.4–76.3 [23.9] | |
| Male | 17 | 85.4 ± 9.2 | 66.8–103.0 [36.2] | |
| Body fat percentage | Overall | 32 | 23.3 ± 7.4 | 11.0–43.6 [32.6] |
| Female | 15 | 27.8 ± 6.2 | 20.3–43.6 [23.3] | |
| Male | 17 | 19.3 ± 6.1 | 11.0–38.1 [27.1] | |
| VO2max (mL/kg/min) | Overall | 32 | 46.2 ± 7.4 | 31.2–62.6 [31.4] |
| Female | 15 | 42.1 ± 5.8 | 32.5–50.6 [18.1] | |
| Male | 17 | 49.68 ± 7.03 | 31.20–62.6 [31.4] | |
| Projected 1-RM squat (kg) | Overall | 32 | 108.2 ± 38.4 | 56.25–224.53 [168.28] |
| Female | 15 | 80.2 ± 15.2 | 56.4–105.0 [48.6] | |
| Male | 17 | 133.3 ± 35.5 | 73.2–225.0 [151.8] | |
| Projected 1-RM bench (kg) | Overall | 32 | 77.1 ± 36.0 | 26.8–142.9 [116.1] |
| Female | 15 | 46.2 ± 11.9 | 26.8–68.6 [41.8] | |
| Male | 17 | 104.7 ± 26.5 | 51.4–143.2 [91.8] | |
| Projected 1-RM deadlift (kg) | Overall | 32 | 119.0 ± 42.3 | 59.0–221.8 [162.8] |
| Female | 15 | 87.7 ± 20.6 | 59.1–124.6 [65.5] | |
| Male | 17 | 147.2 ± 36.6 | 95.9–221.3 [146.4] | |
Values Reported as mean ± standard deviation.
M males, F females, 1-RM 1 repetition maximum.
Acute exercise intensity
Average heart rate (F(2, 62) = 395.57; p < 0.001, η2p = 0.93), estimated core temperature (F(2, 62) = 132.16; p < 0.001, η2p = 0.81), skin temperature (F(2, 62) = 34.70; p < 0.001, η2p = 0.53), ventilatory rate (F(2, 62) = 160.68; p < 0.001, η2p = 0.84) were all significantly higher following AE and RE compared to CON. Additionally, post-exercise BLC (F(2, 62) = 102.36; p < 0.001, η2p = 0.77) was all significantly higher following AE and RE compared to CON. Average heart rate (p < 0.001) and ventilatory rate (p < 0.001) were significantly higher during AE compared to RE. BLC (p = 1.000), estimated core temperature (p = 1.000), and skin temperature (p = 1.000) did not significantly differ between AE and RE. Duration of exercise session was significantly different between conditions (F(2,62) = 60.04; p < 0.001, η2p = 0.66). Post-hoc analysis suggests that RE duration was significantly longer than AE and CON (ps < 0.001) and AE duration was significantly longer than CON (p < 0.001). The gear time (time to transition from acute exercise, donning firefighter gear and starting the OTA) was significantly different between conditions (CON: 6.03 ± 1.79, AE: 6.00 ± 1.51; RE: 8.81 ± 2.19; p = 0.001). Post-hoc analysis suggests the RE gear time was significantly longer than AE and CON (p < 0.001). Full report including mean and standard deviations of average as well as peak values for each of these variables can be found in Tables 2 and 3.
Table 3.
Physiological response to acute exercise.
| Variable | Control session | Aerobic exercise | Resistance exercise |
|---|---|---|---|
| Peak heart rate (bpm) | 106 ± 20 | 186 ± 10 | 172 ± 20 |
| Average heat rate (bpm) | 74 ± 17 | 144 ± 8* | 127 ± 20*† |
| Peak ventilation rate (brpm) | 24.9 ± 6.2 | 50.6 ± 7.4 | 37.8 ± 7.2 |
| Average ventilation rate (brpm) | 15.5 ± 6.2 | 33.8 ± 4.7* | 27.1 ± 4.1*† |
| Peak skin temperature (°C) | 34.6 ± 0.8 | 36.6 ± 1.0 | 35.9 ± 2.1 |
| Average skin temperature (°C) | 33.2 ± 0.9 | 34.7 ± 1.3 | 34.7 ± 1.3 |
| Peak estimated core temperature (°C) | 37.1 ± 0.3 | 38.4 ± 0.2 | 38.1 ± 0.5 |
| Average estimated core temperature (°C) | 36.9 ± 0.3 | 37.9 ± 0.2 | 37.8 ± 0.4 |
| Post-exercise BLC (mMol/L) | 1.4 ± 0.5 | 8.3 ± 2.8 | 8.4 ± 3.4 |
| Duration (minutes) | 30.0 ± 0.2 | 27.0 ± 1.1 | 36.7 ± 6.1 |
Post-exercise BLC immediate post-exercise blood lactate concentration, Bpm Beats/minute, Brpm breaths/minute, °C degrees Celsius, mMol milliMol.
Statistical significance was set at p < 0.05.
*Denotes significantly different than control session.
† Denotes significantly different than aerobic session.
Table 2.
Exercise prescription values.
| Aerobic session | Low interval | High interval | |||||
|---|---|---|---|---|---|---|---|
| RPE | 3.9 ± 1.3 | 8.3 ± 1.1 | |||||
| Speed (km/h) | 7.0 ± 1.4 | 19.8 ± 3.0 | |||||
| Resistance session | Squat | Bench | Deadlift | Bent row |
|---|---|---|---|---|
| RPE | 7.9 ± 1.0 | 7.9 ± 0.9 | 8.3 ± 0.8 | 7.4 ± 1.0 |
| Reps | 6.0 ± 0.0 | 6.0 ± 0.3 | 5.9 ± 0.2 | 6.0 ± 0.0 |
| Load (kg) | 191.2 ± 67.0 | 135.2 ± 63.6 | 206.7 ± 73.7 | 109.5 ± 44.7 |
RPE Rating of Perceived Exertion (OMNI 0–10 scale) .
Statistical significance was set at p < 0.05.
*Denote significantly different than control session.
† Denotes significantly different than aerobic session.
Occupational task assessment results
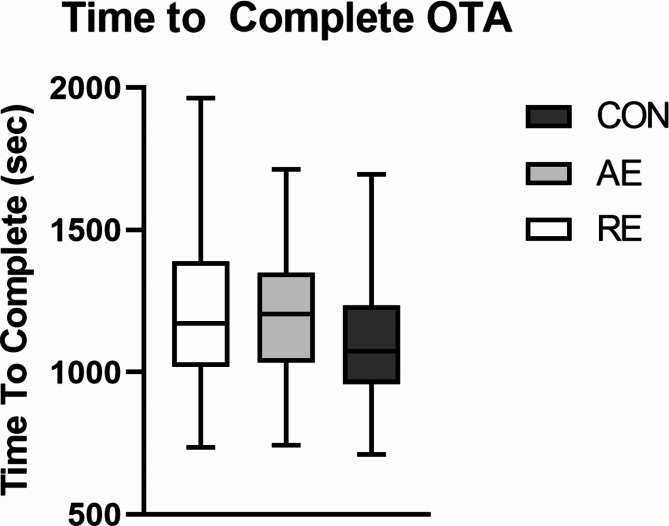
Average time to complete was 18.9 ± 4.4 min after CON compared to 20.0 ± 3.6 min after AE and 20.19 ± 5.0 min after RE. ANOVA results suggest that there was not a significant difference between pre-OTA conditions (F(2,54) = 1.88; p = 0.162; η2p = 0.07). Based on our equivalence test, we rejected the presence of differences in time to complete OTA between conditions more extreme than η2p = 0.11, or 3 min (p = 0.014). Visual representation of the average time to complete the OTA between conditions can be found in Fig. 2.
Fig. 2.
Occupational Task Assessment (OTA); Differences in time to complete across each pre-OTA condition. CON resting control, AE aerobic exercise, RE resistance exercise. No significant differences present (ps > 0.05).
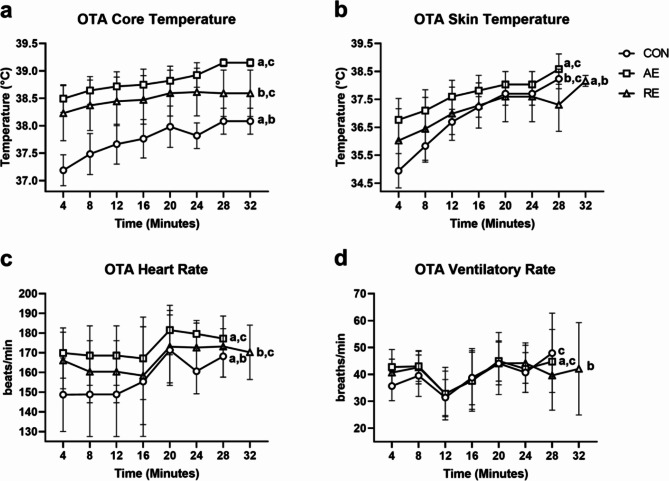
Heart rate (F(2, 62) = 47.04; p < 0.001, η2p = 0.60), estimated core temperature (F(2, 62) = 195.00; p < 0.001; η2p = 0.86), skin temperature (F(2, 62) = 38.69; p < 0.001; η2p = 0.56), and ventilatory rate (F(2, 62) = 7.98; p < 0.001; η2p = 0.21) were all significantly different between conditions during OTA. BLC immediate-post OTA was not significantly different (F(1, 62) = 2.794; p = 0.072; η2p = 0.09). Post-hoc analysis revealed heart rate during the OTA was significantly higher following AE and RE compared to CON and significantly lower after RE compared to AE (ps < 0.002). Estimated core temperature was significantly higher during OTA following RE and AE compared to CON, and RE was significantly lower than AE (ps < 0.002). Skin temperature was significantly higher during OTA following AE and RE compared to CON, and RE was also significantly lower than AE (ps < 0.001). Ventilatory rate was significantly higher during OTA following AE and RE compared to CON (ps < 0.004), but AE was not different from RE (p = 1.000). When comparing peak physiological response experienced, max estimated core temperature was significantly different by condition (F(2, 62) = 102.12; p < 0.001, η2p = 0.77). Post-hoc analysis indicated max estimated core temperature was significantly higher following AE compared to both CON (p < 0.001) and RE (p = 0.002) and RE was significantly higher than CON (p < 0.001).
Average RPE was significantly different by condition (F(2, 62) = 26.83; p < 0.001; η2p = 0.46). Post-hoc analysis revealed RPE during OTA was significantly higher following AE and RE compared to CON (ps < 0.001), but not significantly different between AE and RE (p = 1.000). Additionally, gear time (time between acute exercise and OTA) was significantly longer (F(2, 56) = 31.55; p < 0.001, η2p = 0.53). Post-hoc analysis showed gear time was significantly longer following RE compared to AE and CON (p < 0.001), but AE was not significantly different from CON (p = 1.000). AUC (cumulative heat stress experienced during OTA) was significantly different by condition (F(2, 60) = 15.66; p < 0.001, η2p = 0.34). Post-hoc analysis revealed AUC was significantly higher following AE and RE compared to CON (ps < 0.010), but not different between AE and RE (p = 0.092). Mean and standard deviations for average in these physiological variables and perception of exertion can be found in Table 4. Graphs highlighting the physiological responses during the OTA can be found in Fig. 3.
Table 4.
Physiological response and perceived exertion during OTA.
| Variable | Control | Aerobic exercise | Resistance exercise |
|---|---|---|---|
| Average heart rate (bpm) | 149 ± 16† | 166 ± 12* | 160 ± 13*† |
| Average ventilation rate (brpm) | 37.2 ± 4.8† | 40.2 ± 6.6* | 39.7 ± 5.5* |
| Average skin temperature (°C) | 36.3 ± 0.5† | 37.5 ± 0.6* | 36.9 ± 0.9*† |
| Average core temperature (°C) | 37.6 ± 0.4† | 38.7 ± 0.3* | 38.4 ± 0.5*† |
| Pre-OTA BLC (mMol/L) | 1.5 ± 0.6 | 7.1 ± 2.5 | 6.2 ± 2.7 |
| Post-OTA BLC (mMol/L) | 7.9 ± 3.9 | 7.1 ± 2.6 | 8.6 ± 3.7 |
| Average RPE | 12.7 ± 1.8 | 14.3 ± 1.6* | 14.7 ± 1.6* |
Bpm Beats/minute, Brpm breaths/minute, °C degrees Celsius, RPE Rating of Perceived Exertion (Borg 6–20).
Statistical significance was set at p < 0.05.
*Denotes significantly different than control session.
† Denotes significantly different than aerobic session.
Fig. 3.
Physiological Stress during the Occupational Task Assessment (OTA) based on pre-OTA conditions. CON resting control, AE aerobic exercise, RE resistance exercise. aDenotes significant difference from aerobic; bDenotes significant difference from resistance; cDenotes significant difference from control; (p < 0.05); Values represented are 4-minute mean and standard deviation.
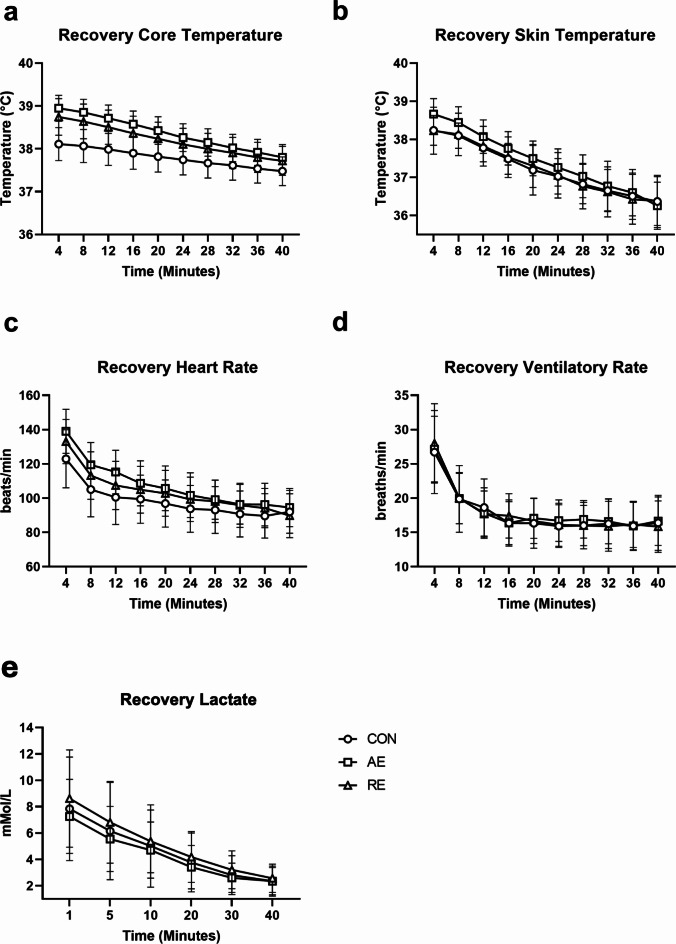
Recovery responses
During recovery, there were not statistically significant differences in average heart rate (F(2, 62) = 1.17; p = 0.318; η2p = 0.04), estimated core temperature (F(2, 62) = 1.85; p = 0.165; η2p = 0.06), skin temperature (F(2, 62) = 0.10; p = 0.905; η2p < 0.01), ventilatory rate (F(2, 62) = 0.49; p = 0.618; η2p = 0.02), or change in BLC between conditions (F(2, 62) = 1.84; p = 0.168; η2p = 0.06). There was a significant difference in AUC between conditions (F(2, 62) = 70.94; p < 0.001; η2p = 0.70). Post-hoc analysis indicated CON recovery AUC was significantly lower than AE and RE (ps > 0.001), but AE and RE were not significantly different (p = 0.630). A visual representation of the time course of recovery for these variables is included in Fig. 4.
Fig. 4.
Recovery of physiological variables following Occupational Task Assessment (OTA) based pre-OTA condition. CON resting control, AE aerobic exercise, RE resistance exercise. No significant differences present (ps > 0.05). Values represented are mean and standard deviation.
Discussion
NFPA recommends firefighters exercise on-shift53. Previous research suggests firefighters frequently have on-site access to barbells and treadmills allowing them to complete both aerobic and resistance exercise on shift28. However, firefighters have expressed concerns that exercising on-shift may decrease their ability to respond to emergency calls30,54, making it important to understand the impact acute on-shift exercise has on firefighter occupational performance. Therefore, our study aimed to determine if resistance or aerobic exercise impacts occupational performance and physiological stress.
Contrary to our primary hypothesis, we did not find evidence that exercise modality impacted occupational performance, despite finding evidence of elevated markers of physiological and perceptual stress (elevated skin temperature, estimated core temperature, heart rate, and RPE) in both AE and RE conditions compared to CON. These findings differed from previous research investigating the effect of acute exercise on occupational performance31,32, which can likely be attributed to methodological differences. The aim of both previous investigations involved an acute exercise prescription of high-intensity circuit-style resistance training31,32. The circuit-style prescription has good application, as many firefighters currently engage in this form of exercise training. Comparatively, our study aimed to add to these findings through the comparison of conventional resistance exercises and high-intensity interval training (HIIT), to help elucidate how the two exercise stressors may impact occupational performance differently. The divergence in findings may also relate to the circuit-style fashion, which can replicate more similar demands (repeated lifting and moving tasks with minimal rest) resulting in fatigue of the same musculature and depletion of the same substrates utilized during occupational tasks to a greater degree than traditional resistance or aerobic exercise, therefore leading to larger interference with occupational performance. Taken together, the findings from each study provide a more comprehensive understanding of how different training methods may have unique impacts on occupational performance.
Estimated core temperature, heart rate, and skin temperature were all elevated in the acute exercise conditions when compared to CON, suggesting that participants experienced greater physiological stress during the occupational tasks when aerobic exercise was performed beforehand. These same variables were significantly higher during the OTA after the AE condition; even though RPE was numerically higher and time to complete occupational tasks was ~ 30 s slower following RE. These findings suggest that prior acute aerobic exercise may result in a divergence between perceived and experienced exertion during occupational tasks. Additionally, some participants in our investigation reached estimated core temperatures > 39 °C which is an important consideration because a core temperature > 40 °C is a key risk factor of heat injury44. Furthermore, due to high prevalence of heat injury in firefighters6 this is a primary concern of fire services44,55. The elevated physiological responses observed in our study warrant future investigations to further elucidate risk or heat injury.
Unlike the previously mentioned variables, BLC was not significantly different between conditions, possibly due to the use of a high-intensity interval-based aerobic workout. A long, slow continuous aerobic workout may have resulted in lower lactate levels going into the OTA, leading to lower immediate post-OTA BLC. An interesting observation was that participants, on average, experienced almost no change (0.03 mMol decrease) in BLC following AE; while there was a 2.4 mMol increase following RE. The elevated lactate concentrations could be a result of increased reliance on rapid glycolysis aerobic metabolism and subsequently higher lactate accumulation during the OTA following RE, compared to AE. The difference in lactate concentration was not statistically significant, although there was a moderate effect (η2p = 0.09). Future investigations should consider the lactate response and its influence on occupational demands, specifically in higher intensity or even longer duration situations where higher lactate levels may limit occupational performance.
When considering the physiological responses experienced, it is worth considering the average time to complete the tasks and the type of tasks completed in this study compared to previous work. In previous investigations, the times to complete occupational tasks were ~ 7 min or less31,32, whereas we aimed to understand acute exercise’s impact on extended occupational tasks (~ 20 min in duration). Taken together, the physiological variables measured across our study and previous work suggest that acute exercise may decrease performance of short, high-intensity occupational demands through increased fatigue and potentially increased heat stress during longer, moderately high-intensity tasks due to increases in core temperature, which is supported by the lower levels of blood lactate concentrations following our occupational tasks compared to previous studies31,32 and elevated estimated core temperatures observed in the current investigation. While the current and previous investigations provide an understanding of acute exercise’s impact on both short and moderate duration occupational tasks31,32, firefighting scenarios can extend to longer durations. When considering a firefighter’s self-contained breathing apparatus lasts on average 30–60 min56, it worth investigating occupational scenarios of this duration in future work. In addition to the increased physiological stress experienced during the OTA, as previously mentioned perceived exertion was elevated following both RE and AE when compared to CON. The elevated perceived exertion could be a consequence of the elevated core temperature estimates and skin temperature increasing perceived thermal stress, resulting in the OTA feeling more demanding even though participants were able to complete the tasks at the same rate.
Acute exercise bouts did not impair the participant’s recovery following occupational task performance, contrary to our secondary hypothesis. Our findings indicate heart rate, estimated core temperature, skin temperature, ventilatory rate, and blood lactate concentrations were not significantly different on average or at the end of the 40-minute recovery. Although, estimated core temperature AUC between conditions was elevated during recovery from AE and RE. Elevated AUC suggests the individuals’ estimated core temperature spent a larger portion of the recovery at an elevated state. Elevated estimated core temperature AUC could elevate perceived fatigue or perceived thermal stress experienced which may impact subsequent occupational readiness for future calls during shift. However, perceived thermal stress and fatigue was not accounted for in the current investigation, and should be considered in future research.
An important limitation of this study to note is the choice to use members of the community rather than current firefighters. We acknowledge that firefighters may have unique experiences working in the heat57 and career firefighters may experience specific heat adaptations that differ from the general population58. Additionally, previous literature suggests that firefighters are on average older and have poorer cardiovascular outcomes59 than our relatively young and healthy sample which may impact the responses seen. However, the recruitment from the general population was an intentional decision to improve the inclusion of women with the knowledge that our local fire departments in our area are younger60 and more physically active28 than the national average, similar to the sample presented in our investigation. It is also important to recognize that the Equivital Black Ghost system is only able to provide an estimate of core temperature rather than actual core temperature values. However, the Equivital Black Ghost system has been previously validated to rectal temperature monitoring45–47. Additionally, the movements chosen for the OTA in this study were based on recommendations of the local fire department, which were limited based on the confines of our environmental chamber and do not represent all firefighting task demands nor was this task assessment previously validated for content or construct validity. We also did not measure thermal sensation, which would have provided supplemental information to better understand potential behavioral thermoregulatory measures (i.e., slowing pace down or stopping between tasks) that may have been impacted by an acute exercise bout. Lastly, the gear time was ~ 2–3 min longer following the resistance training session compared to aerobic and resting control partly due to the location of our weight room being further from our environmental chamber than our aerobic and control testing area. The time to put on the firefighter gear time was not standardized as we wanted to replicate immediate post-exercise conditions with no rest. While the gear time difference could have had a small impact on OTA responses; had we standardized the rest period, participants would have had 2–3 min of passive rest prior to entering the chamber after the aerobic and resting control conditions, which would have likely had a larger impact on OTA responses. We also acknowledge the potential limitation of USG and its ability to determine whole body hydration status.
The current study sought to determine immediate decrements from acute exercise on occupational performance, as this was perceived to be the largest threat to occupational performance due to immediate post-exercise fatigue and heat stress. However, if the call comes in hours after on-shift exercise, fatigue, delayed onset muscle soreness, and other factors may differentially influence occupational readiness. Previous research aimed to address the difference between a 10-minute and 60-minute post-exercise occupational task assessment32. Their findings suggested that while there were impairments at 10-minutes, they were statistically recovered by 60-minutes post-exercise32. Due to the possibility that an emergency call can arrive at any time during their work shift, further investigation into the time course of the impact of acute exercise on occupational tasks is warrented. In addition to the considerations of on-shift exercise, off-shift exercise presents its own considerations in future research, specifically for factors related to substrate availability and delayed on-set muscle soreness. Lastly, we chose conventional strength training and high-intensity interval training based on the common equipment resources accessible28 and preferred methods of aerobic training of firefighters as well as the demand for both strength and aerobic capacity in firefighters. However, there are a multitude of different exercise prescription choices that could influence the acute response to exercise (i.e., sets, reps, intensity, rest intervals, and movements chosen). Future investigation of different on-shift exercise prescriptions and their impact on subsequent occupational demands will help optimize improvements in occupationally relevant fitness while minimizing decrements in occupational readiness in fire services.
Conclusions
The data presented suggest a firefighter may be able to exercise while on-shift and respond to a call without meaningful decrements in performance. However, higher physiological stress, specifically higher estimated core temperature, does warrant precaution that individuals should be aware of potential increases in core temperature and fatigue while completing occupational tasks if they exercised immediately beforehand. Their core temperature may be even higher after aerobic high-intensity interval exercise even though their rating of perceived exertion, blood lactate concentrations, and time to complete were numerically higher after strength-based-barbell resistance exercise. The presentation of the risks are not a recommendation to avoid exercise on-shift, but rather to raise awareness of the physiological responses and to guide on-shift exercise prescription choices in fire departments and fitness professionals working with fire services. With the knowledge that aerobic fitness and muscular strength are required for overall health and for firefighters to meet the demands of their occupations, it is important that we understand how to address both aspects of fitness most effectively and efficiently without interfering with their occupational readiness. Even though there was a larger numeric decrease in time to complete occupational tasks when resistance exercise was performed prior (2.5% longer than when aerobic exercise was performed), the risk for heat stress should be considered by fire services. Therefore, it may be beneficial for fire service strength and conditioning professionals to prescribe aerobic exercise off-shift and focus on resistance exercise on-shift to reduce potential increases in heat stress during subsequent occupational tasks while still working toward improvements in fitness through the implementation of on-shift exercise. However, limitations related to adherence to unsupervised exercise may make this difficult; therefore, when performing high-intensity aerobic exercise on-shift, firefighters should be aware of the potential increased heat stress.
Acknowledgements
We would like to thank Auburn City Fire Department for their support and contributions to this project, our research volunteers for assisting with data collection, and the participants for their time and efforts.
Author contributions
Conceptualization, PJA, JMS, CBM, MWM, WMM; Data curation, PJA and NCB; Formal analysis, PA.; Investigation PJA, NCB, PLJ, AMR., LFR; Methodology, PJA, JMS, CBM, MWM, WMM; Project administration, PJA, JMS, NCB, PLJ, AMR, LFR; Supervision, JMS; Visualization, PJA; Writing—original draft, PJA, NCB; JMS Writing—review and editing, all authors.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Auburn University (protocol code #22–149 MR 2205, 05/05/2022).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Willi, J. M. et al. Characterizing a firefighter’s immediate thermal environment in live-fire training scenarios. Fire Technol.52 (6), 1667–1696 (2016). [Google Scholar]
- 2.Orr, R. et al. Impact of various clothing variations on firefighter mobility: a pilot study. Safety5 (4), 78 (2019). [Google Scholar]
- 3.Dreger, R. W. et al. Effects of the self-contained breathing apparatus and fire protective clothing on maximal oxygen uptake. Ergonomics49 (10), 911–920 (2006). [DOI] [PubMed] [Google Scholar]
- 4.Park, K. et al. Assessing gait changes in firefighters due to fatigue and protective clothing. Saf. Sci.49 (5), 719–726 (2011). [Google Scholar]
- 5.Park, K. et al. Effect of load carriage on gait due to firefighting air bottle configuration. Ergonomics53 (7), 882–891 (2010). [DOI] [PubMed] [Google Scholar]
- 6.Kim, S. et al. Frequency of firefighters’ heat-related illness and its association with removing personal protective equipment and working hours. Ind. Health57 (3), 370–380 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cornell, D. J. et al. Changes in Health and Fitness in Firefighter Recruits: An Observational Cohort Study49 2223–2233 (Medicine & Science in Sports & Exercise, 2017). [DOI] [PubMed]
- 8.National Fire Protection Association, Fourth Needs Assessment of the U.S. Fire Service. Conducted in 2015 and Including Comparisons to the 2001, 2005, and 2010 Needs Assessment Surveys., in National Fire Proection Association, Fire Analysis and Research Division : Quincy, MA. (2016).
- 9.Campbell, R. et al. United States Firefighter Injuries in 2019 (National Fire Protection Association. Research, Data and Analytics Division, 2020).
- 10.Langford, E. L. Physiological Profile of Rural Structural Firefighters in Southeast Georgia. (Georgia Southern University: Electronic Theses and Dissertations, 2019).
- 11.Gendron, P. et al. Cardiovascular disease risk in female firefighters. J. Occup. Environ. Med.68 (6), 412–414 (2018). [DOI] [PubMed] [Google Scholar]
- 12.Gendron, P. et al. Cardiovascular disease risk factors in Québec male firefighters. J. Occup. Environ. Med.60 (6), e300–e306 (2018). [DOI] [PubMed] [Google Scholar]
- 13.Smith, D. L. et al. Cardiovascular strain of firefighting and the risk of sudden cardiac events. Exerc. Sport Sci. Rev.44 (3), 90–97 (2016). [DOI] [PubMed] [Google Scholar]
- 14.Frost, D. M. et al. Exercise-based performance enhancement and injury prevention for firefighters: contrasting the fitness- and movement-related adaptations to two training methodologies. J. Strength. Condition. Res.29 (9), 2441–2459 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Gendron, P. et al. Physical training in the fire station and firefighters’ cardiovascular health. Occup. Med.70 (4), 224–230 (2020). [DOI] [PubMed] [Google Scholar]
- 16.Leary, M. et al. Evaluation of an occupational exercise training program for firefighters: mixed methods pilot study. J. Med. Internet Res. Form. Res.4 (9), e17835 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moon, T. Y. et al. Effects of exercise therapy on muscular strength in firefighters with back pain. J. Phys. Therapy Sci.27 (3), 581–583 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pawlak, R. et al. The effect of a novel tactical training program on physical fitness and occupational performance in firefighters. J. Strength. Condition. Res.29 (3), 578–588 (2015). [DOI] [PubMed] [Google Scholar]
- 19.Zare, S. et al. Comparison of the effect of typical firefighting activities, live fire drills and rescue operations at height on firefighters’ physiological responses and cognitive function. Ergonomics61 (10), 1334–1344 (2018). [DOI] [PubMed] [Google Scholar]
- 20.Morley, J. et al. Cognitive function following treadmill exercise in thermal protective clothing. Eur. J. Appl. Physiol.112 (5), 1733–1740 (2012). [DOI] [PubMed] [Google Scholar]
- 21.Horn, G. P. et al. Core temperature and heart rate response to repeated bouts of firefighting activities. Ergonomics56 (9), 1465–1473 (2013). [DOI] [PubMed] [Google Scholar]
- 22.Horn, G. P. et al. Physiological responses to simulated firefighter exercise protocols in varying environments. Ergonomics58 (6), 1012–1021 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Johnson, Q. R. et al. Heart rate responses during simulated fire ground scenarios among full-time firefighters. Int. J. Exerc. Sci.13 (2), 374–382 (2020). [PMC free article] [PubMed] [Google Scholar]
- 24.Ebersole, K. T. et al. Contribution of the autonomic nervous system to recovery in firefighters. J. Athl. Train.55 (9), 1001–1008 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Barros, C. L. M. et al. Maximal lactate steady state is altered in the heat. Int. J. Sports Med.32 (10), 749–753 (2011). [DOI] [PubMed] [Google Scholar]
- 26.González-Alonso, J. et al. The cardiovascular challenge of exercising in the heat. J. Physiol.586 (1), 45–53 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gleeson, M. Temperature regulation during exercise. Int. J. Sports Med.19 (Suppl 2), S96–S99 (1998). [DOI] [PubMed] [Google Scholar]
- 28.Agostinelli, P. et al. Exercise habits and resources for Southeastern US firefighters. J. Occup. Environ. Med.65 (5), e351–e357 (2023). [DOI] [PubMed] [Google Scholar]
- 29.Langford, E. et al. Physical fitness initiatives in the Fire service–barriers and benefits. TSAC Rep.54 (1). (2019).
- 30.Lovejoy, S. et al. Exploring Physical Health in a Sample of Firefighters63 253–258 (Workplace Health & Safety, 2015). [DOI] [PubMed]
- 31.Dennison, K. J. et al. The effect of fatigue and training status on firefighter performance. J. Strength. Condition. Res.26 (4), 1101–1109 (2012). [DOI] [PubMed] [Google Scholar]
- 32.Mason, M. R. et al. The acute effect of high-Intensity resistance training on subsequent firefighter performance. J. Strength. Condition. Res.37 (7), 1507–1514 (2023). [DOI] [PubMed] [Google Scholar]
- 33.Trabulo, M. et al. [Does the modified Bruce protocol induce physiological stress equal to that of the Bruce protocol?]. Rev. Port Cardiol.13 (10), p753–60735 (1994). [PubMed] [Google Scholar]
- 34.Swinton, P. A. et al. A biomechanical analysis of straight and hexagonal barbell deadlifts using submaximal loads. J. Strength. Condition. Res.25 (7), 2000–2009 (2011). [DOI] [PubMed] [Google Scholar]
- 35.Landers, J. Maximum based on reps. Natl. Strength. Condition. Assoc. J.6 (6), 60 (1984). [Google Scholar]
- 36.Sheppard, J. & Triplett, T. Program Design for Resistance Training. In: Essentials of Strength and Conditioning, (G.G. Haff and T. Triplett, Eds). Human Kinetics: Champaign, IL. 439–468. (2016).
- 37.Reuter, H., Benjamin & Dawes, J. J. Program Design and Technique for Aerobic Endurance Training. In: Essentials of Strength and Conditioning, (G.G. Haff and T. Triplett, Eds). Human Kinetics: Champaign, IL. 439–468. (2016).
- 38.de Sousa, A. F. M. et al. Improvements in Attention and Cardiac Autonomic Modulation after a 2-Weeks Sprint Interval Training Program: A Fidelity Approach9 (Frontiers in Physiology, 2018). [DOI] [PMC free article] [PubMed]
- 39.Karvonen, M. J. et al. The effects of training on heart rate; a longitudinal study. Ann. Med. Exp. Biol. Fenn.35 (3), 307–315 (1957). [PubMed] [Google Scholar]
- 40.National Fire Protection Association. 1710. Organization and Deployment of Fire Suppression Operations, EMS and Special Operations in Career Fire Departments, in National Fire Protection Association Analysis and Research Division (Quincy, 2022).
- 41.Aisbett, B. et al. Awake, smoky, and hot: providing an evidence-base for managing the risks associated with occupational stressors encountered by wildland firefighters. Appl. Ergon.43, 916–925. 10.1016/j.apergo.2011.12.013 (2012). [DOI] [PubMed] [Google Scholar]
- 42.Williams-Bell, F. M. et al. The effects of simulated Wildland Firefighting tasks on Core temperature and cognitive function under very hot conditions. Front. Physiol.810.3389/fphys.2017.00815 (2017). [DOI] [PMC free article] [PubMed]
- 43.Gledhill, N. & Jamnik, V. K. Characterization of the physical demands of firefighting. Can. J. Sport Sci.17 (3), 207–213 (1992). [PubMed] [Google Scholar]
- 44.Binkley, H. M. et al. National athletic trainers’ association position statement: Exertional heat illnesses. J. Athl Train.37 (3), 329–343 (2002). [PMC free article] [PubMed] [Google Scholar]
- 45.Buller, M. J. et al. Estimation of human core temperature from sequential heart rate observations. Physiol. Meas.34 (7), 781–798 (2013). [DOI] [PubMed] [Google Scholar]
- 46.Buller, M. J. et al. Real-time core body temperature estimation from heart rate for first responders wearing different levels of personal protective equipment. Ergonomics58 (11), 1830–1841 (2015). [DOI] [PubMed] [Google Scholar]
- 47.Agostinelli, P. J. et al. Validity of heart rate derived core temperature estimation during simulated firefighting tasks. Sci. Rep.13 (1), 22503 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Borg, G. A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc.14 (5), 377–381 (1982). [PubMed] [Google Scholar]
- 49.Zourdos, M. C. et al. Novel resistance training–specific rating of perceived exertion scale measuring repetitions in reserve. J. Strength. Condition. Res.30 (1), 267–275 (2016). [DOI] [PubMed] [Google Scholar]
- 50.Zinoubi, B. et al. Relationships between rating of perceived exertion, heart rate and blood lactate during continuous and alternated-intensity cycling exercises. Biol. Sport35 (1), 29–37 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bynum, G. D. et al. Induced hyperthermia in sedated humans and the concept of critical thermal maximum. Am. J. Physiol. Regul. Integr. Comp. Physiol.235 (5), R228–R236 (1978). [DOI] [PubMed] [Google Scholar]
- 52.RStudio & Team RStudio: Integrated Development for R Studio. RStudio, PBC: Boston, MA. (2020).
- 53.National Fire Protection Association. 1582. Standard on Health Related Fitness Programs for Firefighters, in National Fire Protection Association Analysis and Research Division (Quincy, 2022).
- 54.Agostinelli, P. et al. Exercise habits and resources for Southeastern US firefighters. J. Occup. Environ. Med.65, e351–e357. 10.1097/jom.0000000000002822 (2023). [DOI] [PubMed] [Google Scholar]
- 55.Smith, D. L. et al. Firefighter fatalities and injuries: the role of heat stress and PPE. (2008).
- 56.Kesler, R. M. et al. Physiological response to firefighting activities of various work cycles using extended duration and prototype SCBA. Ergonomics61 (3), 390–403 (2018). [DOI] [PubMed] [Google Scholar]
- 57.Poplin, G. S. et al. Fire fit: assessing comprehensive fitness and injury risk in the fire service. Int. Arch. Occup. Environ. Health89 (2), 251–259 (2016). [DOI] [PubMed] [Google Scholar]
- 58.Wright, H. E. et al. Do older firefighters show long-term adaptations to work in the heat? J. Occup. Environ. Hyg.10 (12), 705–715 (2013). [DOI] [PubMed] [Google Scholar]
- 59.Moffatt, S. M. et al. Cardiometabolic health among United States firefighters by age. Prev. Med. Rep.23, 101492 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Games, K. E. et al. Functional performance of firefighters after exposure to environmental conditions and exercise. J. Athl. Train.55 (1), 71–79 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.