Abstract
The issue of adolescent secondhand smoke (SHS) is globally significant, given that it serves as a preventable risk factor for disease prevalence and mortality rates among youth. This study evaluates trends in adolescent SHS across 27 countries from 2003 to 2021, aiming to identify global variations and sex-specific differences, providing insights for future policy recommendations. The data for this study were collected from the Global School-based Student Health Survey conducted by the World Health Organization, 2003–2021. The term SHS in this context denoted how many days people smoked in their presence for at least one day within the past 7 days. Linear regression models were employed to examine the trends of SHS exposure by country. In the present analysis based on 175,370 adolescents (male, 46.69%) aged between 13 and 15 years from 27 countries across the five continents, SHS decreased in 14 countries but exhibited an increasing trend in 3 countries (Benin [β, 3.20; 95% CI, 2.50–3.91]; Maldives [β, 0.93; 0.21–1.65]; Myanmar [β, 0.62; 0.29–0.95]). Significant increasing trends in females were observed in the Maldives (β, 1.18; 0.25–2.11) and Thailand (β, 0.36; 0.04–0.69) while males showed increasing trends in Kuwait (β, 1.90; 0.79-3.00) and Vanuatu (β, 1.95; 0.35–3.54). Our analysis of adolescents from 27 countries indicates that the majority of nations exhibited decreasing trends in SHS. This suggests that global efforts to prevent SHS are achievable through individual initiatives and international monitoring. However, the presence of increasing trends in certain countries underscores the need for stronger regulations and policies to address this issue.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-80713-7.
Keywords: Adolescent, Global trend, Secondhand smoke, WHO
Subject terms: Paediatric research, Public health
Introduction
Secondhand smoke (SHS) has negative effects on non-smokers, including increased susceptibility to lung cancer, respiratory infections, and hindered lung growth in children1,2. The reduction of SHS can be a critical factor in decreasing the prevalence of various diseases and mortality rates among both children and adults3. As the dangers of SHS and the need for preventive policies have become more prominent, international cooperation has also intensified4. Despite global efforts such as the World Health Organization’s (WHO) recommended tobacco control policies (MPOWER) strategy and the guidelines outlined in the Framework Convention on Tobacco Control (FCTC)5, a significant number of people continue to fall victim to tobacco, resulting in an annual death toll of 1.3 million non-smokers6. The exposure of SHS requires a thorough exploration of the landscape, to develop effective preventive measures.
Furthermore, pregnant females and children are known to be more vulnerable to SHS7–9. A study conducted in 2011, encompassing data from 192 countries, revealed that globally, 40% of children, 33% of adult males, and 35% of adult females are exposed to SHS10. Among children who are exposed to SHS, there is a higher incidence of severe asthma, respiratory infections, and ear infections11. As youth are involuntarily exposed to a smoking environment, it is essential to understand the extent of exposure to SHS among adolescents12,13.
In this study, we evaluated trends in SHS among adolescents utilizing data from representative national surveys conducted from 27 countries across the five continents between 2003 and 2021. This enabled us to explore regional variations and pinpoint potential cultural, economic, or policy factors impacting SHS. Since smoking rates vary by sex14, our study investigated sex-specific variations in SHS. By analyzing trends in SHS, we can discern national and regional differences, assessing the effectiveness of current WHO and country-specific policies.
Methods
Survey and participants
This research examined data from 27 countries, publicly accessible through the Global School-based Student Health Survey (GSHS). The GSHS, developed by the WHO and the U.S. Centers for Disease Control and Prevention (CDC), gathers data on health behaviors and protective factors among adolescents aged 13 to 17. The GSHS uses a standardized, school-based scientific sample selection process with a self-administered questionnaire and followed rigorous sampling. The survey covers ten key health areas, including alcohol use, dietary behaviors, drug use, hygiene, mental health, physical activity, protective factors, sexual behaviors, tobacco use, and violence/injury prevention. Each participating country selects at least six core areas and can add country-specific questions as needed. The questionnaire is translated and tested to ensure student understanding, with privacy maintained by avoiding skip patterns in responses. GSHS data are owned by the official country-level agency such as Ministry of Health conducting or sponsoring the survey. WHO and CDC provide ongoing technical support, including guidance in sample design, training, and data management. By using a consistent methodology, GSHS enables countries to track health behaviors in students, helping to shape policies and programs that support adolescent health. Additionally, we applied statistical weighting to the data to compensate for non-response bias and the varying probabilities of selection15.
For trend analysis, nationally representative datasets from the surveyed countries were chosen based on specific criteria: inclusion of necessary variables and surveys conducted in at least two different years. A total of 27 countries were scrutinized in this study (Argentina, Benin, Cook Islands, Fiji, Guyana, Indonesia, Jamaica, Jordan, Kuwait, Maldives, Mauritius, Mongolia, Morocco, Myanmar, Niue, Philippines, Saint Vincent and the Grenadines, Samoa, Seychelles, Suriname, Thailand, Tonga, Trinidad and Tobago, United Arab Emirates, United Republic of Tanzania, Uruguay, Vanuatu). Detailed information on each country’s characteristics during the survey year, such as sample size, response rate, male percentage, country income level, and the year of WHO FCTC ratification, is provided in Table 1 for reference16. All students were provided with an information paper about GSHS on the first day as well as an informed consent form to obtain written consent from parents or guardians. The study protocol was approved by the Institutional Review Board of Kyung Hee University and the U.S. CDC.
Table 1.
Characteristics of the surveys for secondhand smoke exposure based on data obtained from WHO GSHS between 2003 and 2021.
| Country | Survey year | Sample size | Response rate (%) | Boys (%) | Country income level** | Year WHO FCTC ratified*** |
|---|---|---|---|---|---|---|
| African Region (AFR) | ||||||
| Benin | 2009 | 1,095 | 99.63 | 63.29 | L | 2005 |
| 2016 | 686 | 99.42 | 45.77 | L | ||
| Mauritius | 2007 | 1,783 | 98.71 | 48.12 | UM | 2004 |
| 2011 | 1,891 | 98.63 | 46.38 | UM | ||
| 2017 | 1,947 | 98.61 | 48.48 | UM | ||
| Seychelles | 2007 | 0,928 | 98.38 | 46.98 | UM | 2003 |
| 2015 | 1,518 | 97.17 | 46.57 | H | ||
| United Republic of Tanzania | 2006 | 1,217 | 98.44 | 53.99 | L | 2007 |
| 2014 | 2,154 | 98.75 | 46.61 | L | ||
| Region of the Americas (AMR) | ||||||
| Argentina | 2007 | 1,512 | 98.41 | 47.55 | UM | Not ratified |
| 2012 | 20,890 | 98.34 | 47.22 | UM | ||
| 2018 | 36,332 | 98.94 | 48.24 | UM | ||
| Guyana | 2004 | 1,052 | 99.62 | 40.49 | LM | 2005 |
| 2010 | 1,953 | 98.21 | 44.91 | LM | ||
| Jamaica | 2010 | 1,192 | 98.74 | 48.83 | UM | 2005 |
| 2017 | 1,054 | 98.48 | 45.45 | UM | ||
| Saint Vincent and the Grenadines | 2007 | 1,029 | 99.22 | 46.16 | UM | 2010 |
| 2018 | 1,024 | 99.61 | 46.00 | UM | ||
| Suriname | 2009 | 956 | 99.06 | 47.59 | UM | 2008 |
| 2016 | 1,322 | 99.47 | 45.76 | UM | ||
| Trinidad and Tobago | 2007 | 2,095 | 98.57 | 49.26 | H | 2004 |
| 2011 | 1,836 | 98.42 | 54.47 | H | ||
| 2017 | 2,153 | 98.14 | 48.17 | H | ||
| Uruguay | 2006 | 2,372 | 99.66 | 45.36 | UM | 2004 |
| 2012 | 2,858 | 98.67 | 47.27 | H | ||
| Eastern Mediterranean Region (EMR) | ||||||
| Jordan | 2004 | 1,844 | 97.78 | 45.55 | LM | 2004 |
| 2007 | 1,631 | 97.18 | 56.41 | LM | ||
| Kuwait | 2011 | 2,254 | 99.02 | 49.29 | H | 2006 |
| 2015 | 1,990 | 94.32 | 45.98 | H | ||
| Morocco | 2006 | 1,866 | 98.55 | 48.93 | LM | Not ratified |
| 2010 | 1,997 | 99.00 | 51.53 | LM | ||
| 2016 | 3,262 | 97.92 | 52.21 | LM | ||
| United Arab Emirates | 2010 | 2,179 | 98.12 | 39.93 | H | 2005 |
| 2016 | 3,190 | 98.34 | 48.24 | H | ||
| South-East Asian Region (SEAR) | ||||||
| Indonesia | 2007 | 2,867 | 99.30 | 47.61 | LM | Not ratified |
| 2015 | 7,010 | 99.02 | 46.89 | LM | ||
| Maldives | 2009 | 1,971 | 97.16 | 44.04 | LM | 2004 |
| 2014 | 1,765 | 96.88 | 41.64 | UM | ||
| Myanmar | 2007 | 1,983 | 99.45 | 48.56 | LM | 2004 |
| 2016 | 1,957 | 99.49 | 46.96 | LM | ||
| Thailand | 2008 | 2,223 | 99.69 | 50.29 | LM | 2004 |
| 2015 | 3,492 | 97.74 | 47.31 | UM | ||
| 2021 | 3,621 | 99.48 | 45.32 | UM | ||
| Western Pacific Region (WPR) | ||||||
| Cook Islands | 2011 | 744 | 99.60 | 50.40 | Not classified | 2004 |
| 2015 | 363 | 99.17 | 49.31 | Not classified | ||
| Fiji | 2010 | 1,479 | 99.73 | 41.99 | LM | 2003 |
| 2016 | 1,525 | 98.03 | 50.23 | UM | ||
| Mongolia | 2010 | 3,129 | 99.20 | 44.14 | LM | 2004 |
| 2013 | 3,113 | 99.26 | 48.44 | LM | ||
| Niue | 2010 | 51 | 98.04 | 64.71 | UMIC | 2005 |
| 2019 | 68 | 100.00 | 50.00 | UMIC | ||
| Philippines | 2003 | 4,160 | 99.54 | 40.02 | LM | 2005 |
| 2007 | 3,433 | 98.66 | 40.37 | LM | ||
| 2011 | 3,640 | 99.70 | 41.46 | LM | ||
| 2015 | 5,635 | 99.75 | 43.87 | LM | ||
| Samoa | 2011 | 2,116 | 94.94 | 41.40 | LM | 2005 |
| 2017 | 960 | 98.02 | 33.23 | LM | ||
| Tonga | 2010 | 1,835 | 97.44 | 45.12 | LM | 2005 |
| 2017 | 1,599 | 98.25 | 48.03 | UM | ||
| Vanuatu | 2011 | 704 | 99.72 | 40.77 | LM | 2005 |
| 2016 | 1,225 | 99.10 | 41.06 | LM | ||
GSHS, Global school-based student health survey; H, High income; L, Low income; LM, Lower-middle income; UM, Upper-middle income; WHO, World Health Organization; WHO FCTC, World Health Organization Framework Convention on Tobacco Control.
*Response rate is for the current smoking questions. Data are for participants aged 13–15 years.
**Country income level was categorized by World bank income category.
***Data were from http://www.who.int/fctc/signatories_parties/zh/.
Secondhand smoke exposure
SHS was assessed using the question “During the past 7 days, how many days have people smoked in your presence?”. The response choices included ‘0 days’, ‘1 or 2 days’, ‘3 or 4 days’, ‘5 to 6 days’, and ‘all 7 days’. The collected data were transformed into a dichotomous format, where responses indicating ‘0 days’ were coded as ‘no,’ while all other options were coded as ‘yes’. This transformation resulted in the creation of a binary variable for subsequent analyses. To ensure analytical precision, our focus was specifically on participants aged 13–15 years, given that the majority of the surveyed students fell within this age bracket, and detailed age information beyond this range was not available.
Statistical analysis
The exposure of SHS in the past 7 days, along with its corresponding 95% confidence interval (CI), was computed for both the overall sample and sex-stratified subgroups in each survey. Linear regression models were utilized to assess linear trends in smoking within individual countries. Regression coefficients (β) and their associated 95% CI were calculated to signify the annual change in exposure of SHS within each country17,18. Additionally, analyses were conducted to investigate potential variations in exposure and trends based on sex. Throughout all analyses, sampling weights and the clustered sampling design of the surveys were taken into account. R software (version 4.3.2; R Foundation, Vienna, Austria) and Python (version 3.12.6; Python Software Foundation, Wilmington, DE, USA) were used for statistical analysis, and two-sided P < 0.05 was considered statistically significant. The demographic data used for Fig. 2 were sourced from Natural Earth, an open-source public domain resource.
Results
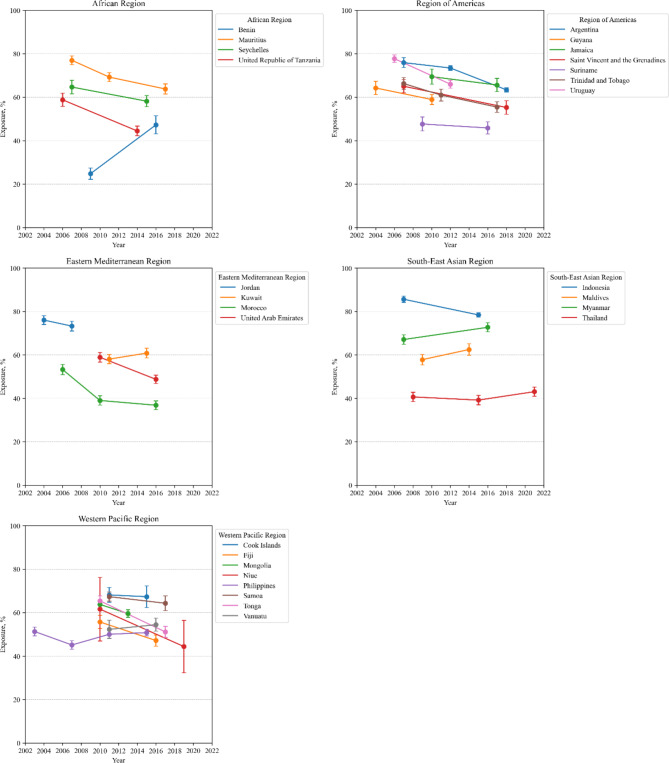
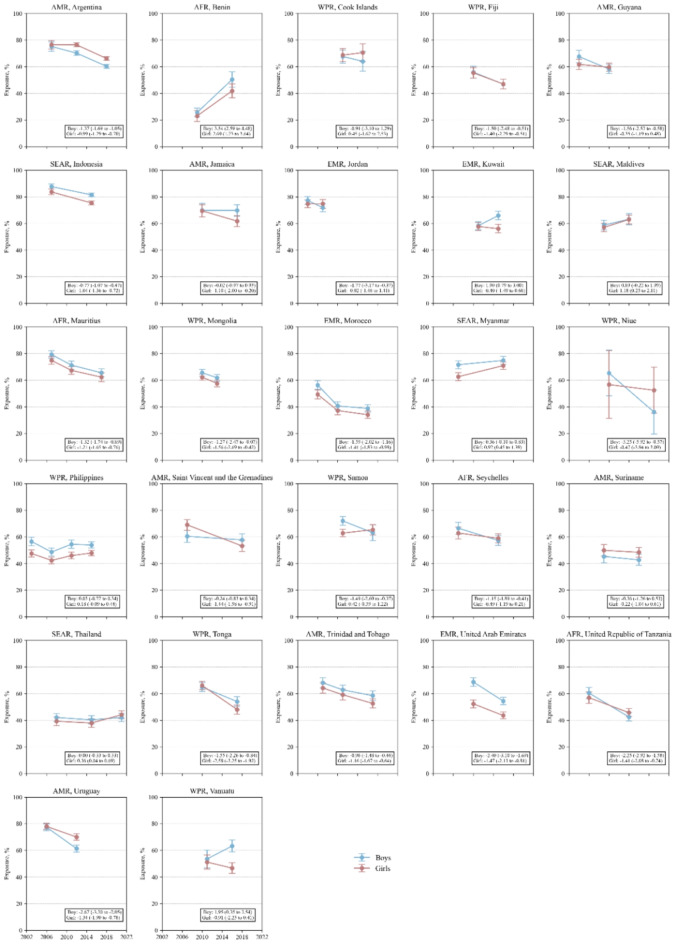
A total of 175,370 school-going adolescents aged 13–15 years from 27 countries across the five continents were included in the analytical sample (male: 47.19%). Characteristics of the representative sample data are depicted in Table 1. As shown in Table S1 and Figs. 1 and 2, Benin in 2009 and Indonesia in 2007 had the lowest (24.83%; [95% CI, 22.21–27.46%]) and highest (85.63%; [95% CI, 84.23–87.03%]) rates, respectively. Among the 27 analyzed countries, three countries exhibited an increasing trend, while 14 countries showed a decreasing trend, and the remaining 10 countries did not present any significant changes. Figure 3 presents the trends of SHS across 27 countries. Three countries showed an increasing trend. Benin had the most significant increasing trend between 2009 (24.83%) and 2016 (47.26%) (β, 3.20), followed by Maldives between 2009 (57.84%) and 2014 (62.49%) (β, 0.93), and Myanmar between 2007 (67.10%) and 2016 (72.71%) (β, 0.62). In contrast, decreasing trend was observed in Mauritius between 2007 (76.99%), 2011 (69.27%), and 2017 (63.80%) (β, -1.26), Seychelles between 2007 (64.68%) and 2015 (58.18%) (β, -0.81), United Republic of Tanzania between 2006 (58.81%) and 2014 (44.46%) (β, -1.79), Argentina between 2007 (75.92%), 2012 (73.44%) and 2018 (63.42%) (β, -1.18), Guyana between 2004 (64.25%) and 2010 (58.94%) (β, -0.89), Saint Vincent and the Grenadines between 2007 (65.04%) and 2018 (55.28%) (β, -0.89), Trinidad and Tobago between 2007 (66.29%), 2011 (60.97%) and 2017 (55.44%) (β, -1.08), Uruguay between 2006 (77.74%) and 2012 (66.01%) (β, -1.95), Morocco between 2006 (53.27%), 2010 (39.03%), and 2016 (36.83%) (β, -1.50), United Arab Emirates between 2010 (58.92%) and 2016 (48.76%) (β, -1.69), Indonesia between 2007 (85.63%) and 2015 (78.42%) (β, -0.90), Fiji between 2010 (55.70%) and 2016 (47.16%) (β, -1.42), Mongolia between 2010 (63.77%) and 2013 (59.58%) (β, -1.40), and Tonga between 2010 (65.42%) and 2017 (51.15%) (β, -2.04).
Fig. 1.
The global trend of secondhand smoke exposure among 175,370 adolescents aged 13–15 years from 27 countries between 2003 and 2021 according to WHO region. Abbreviations: WHO, World Health Organization.
Fig. 2.
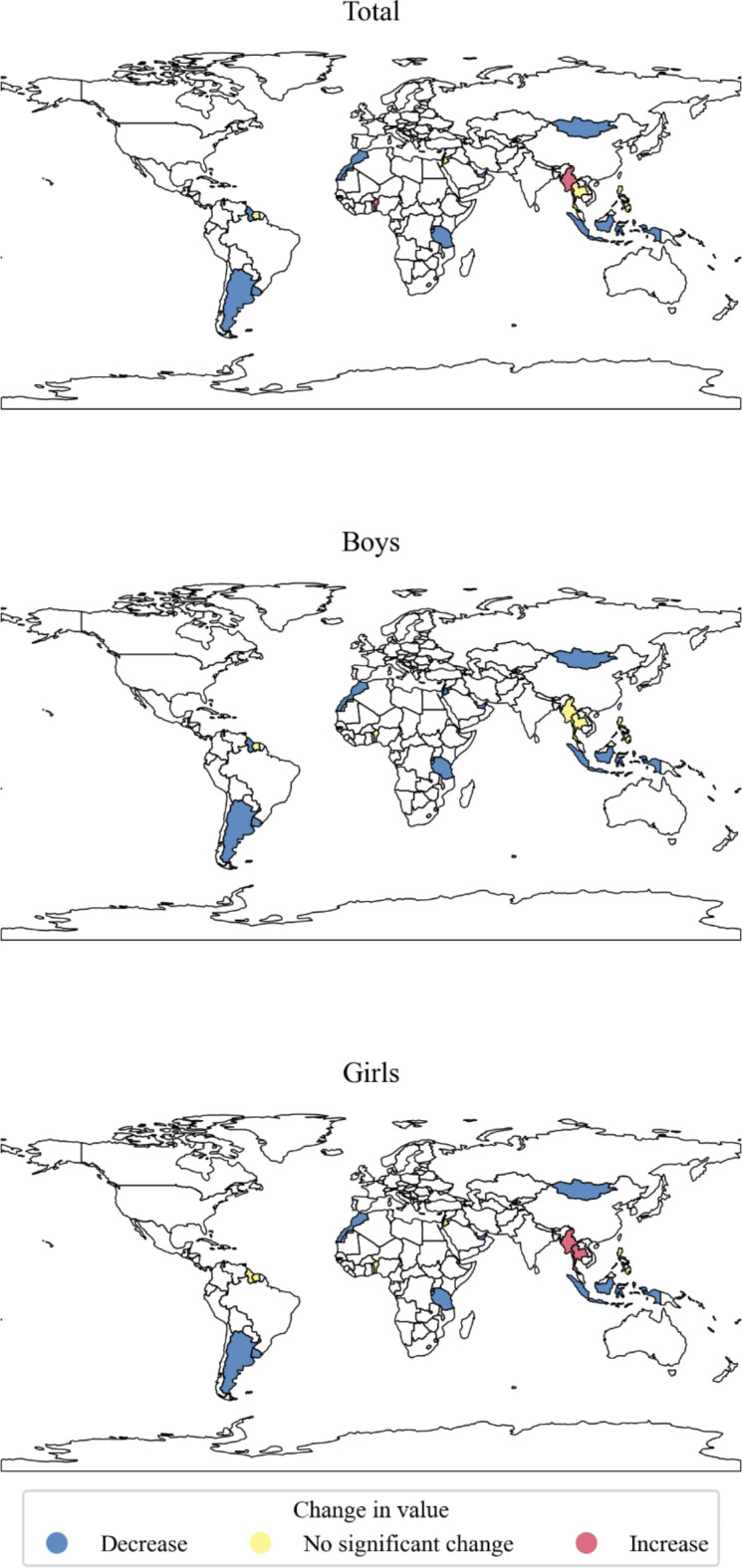
Global trends of secondhand smoke exposure in young adolescents aged 13–15 years in 27 countries between 2003 and 2021. This figure was created using Python (version 3.12.6; https://www.python.org) with GeoPandas (version 1.0.1) and Matplotlib (version 3.9.2) libraries. The underlying geographic data is from Natural Earth (1:110 m cultural vectors: Countries; https://www.naturalearthdata.com), which is in the public domain.
Fig. 3.
The global trend of secondhand smoke exposure among boys and girls in each country between 2003 and 2021. Abbreviations: AFR, African Region; AMR, Region of Americas; EMR, Eastern Mediterranean Region; SEAR, South-East Asian Region; WPR, Western Pacific Region.
Discussion
Key finding
This study, analyzing global trends in adolescent SHS exposure using worldwide data, is significant for its assessment of the risk of SHS exposure among adolescents globally. In this comprehensive study of adolescents aged 13–15 years from 27 countries across the five continents, prominent increasing and decreasing trends in SHS exposure were observed in one and 14 countries (Argentina, Fiji, Guyana, Indonesia, Mauritius, Mongolia, Morocco, Saint Vincent and the Grenadines, Seychelles, Tonga, Trinidad and Tobago, United Arab Emirates, United Republic of Tanzania, Uruguay), respectively. Benin, Maldives, and Myanmar presented significantly increasing trend, while other countries presented decreasing trends. Additionally, in certain nations, notable disparities in SHS trends were observed, which were significantly attributed to sex differences. Specifically, in the Maldives and Thailand, there was an exclusive upward trend in SHS exposure among females, while Kuwait and Vanuatu showed a similar increasing pattern solely among males. To the best of our understanding, this research represents the extensive global assessment of SHS trends among young adolescents, with a specific focus on sex-related variations.
Interpretation of findings
The global decreasing trend of SHS implies the success of worldwide effort to prevent SHS. This trend aligns with findings from prior studies, which have consistently shown a decrease in smoking prevalence subsequent to the enactment of comprehensive smoke-free laws19–21. The WHO Tobacco free initiative’s ongoing country-specific tobacco control assessments22, coupled with various policies implemented in each nation, have contributed to observable trends. Among the 14 countries that showed a decreasing trend in SHS, 12 countries established smoke-free environments in public places, including public transportation. Additionally, these results can be attributed to each country’s proactive measures such as implementing health warning labels on cigarette packs, raising taxes, conducting mass media campaigns, and regulating tobacco marketing on social media23.
Notably, even countries with historically high smoking prevalence that have not ratified the FCTC, such as Indonesia, presented a downward trend in SHS exposure. This decrease may be attributed to national tobacco control initiatives and government interventions. For instance, Indonesia, the only non-FCTC ratified country in the Asia-Pacific region, showed significant improvement after implementing smoke-free homes signage, with the proportion of smokers avoiding indoor smoking increasing from 11 to 54%. These findings suggest that policy initiatives promoting healthy lifestyle changes at the individual level, particularly those advocated by national governments, may effectively reduce SHS exposure, especially among vulnerable populations such as females and adolescents24.
However, in Benin an increasing trend was observed, and policy flaws seem to be a contributing factor. The failure to address the issue of SHS in the national health strategy, leading to a lack of specific regulatory measures, can increase exposure25. Furthermore, the availability of cigarettes at prices lower than WHO recommendations negates the effect of purchase restrictions, potentially increasing SHS26. The lack of tobacco control education in secondary schools also fails to educate minors about the dangers of tobacco, leading to greater leniency towards SHS and smoking27. Additionally, some countries only designate smoke-free areas in limited locations, raising concerns about SHS in public areas. According to the WHO Needs Assessment, Benin’s comprehensive policy formation is flawed, which can be attributed to the increasing trend in SHS28.
The observation of sex disparities in some countries can be attributed to varying socio-cultural characteristics across nations. For instance, Thailand experienced an increase in SHS exclusively among females, which corresponds with a notable rise in e-cigarette use among Thai adolescent females. E-cigarette smoking among female teenagers in Thailand rose from 2% in 2008 to 5% in 2015, while it consistently remained around 21% for males29. While the increase in e-cigarette smoking among female adolescents doesn’t directly explain the rise in SHS, it can be associated with it, considering that adolescents generally tend to interact primarily with same-sex peers30–32.
Strengths and limitations
This study offers an extensive analysis of adolescent SHS trends globally, yet it is subject to certain limitations inherent to the WHO GSHS database. Firstly, the reliance on self-reported SHS introduces the potential of underreporting or inaccurate recollection by adolescents, introducing possible social desirability and recall biases into our analysis. Secondly, the school-based nature of the surveys may omit insights into the SHS patterns of adolescents who are not in school. In addition, the survey years varied across countries, with some providing data from more time points than others. Thirdly, the interpretation of temporal trends warrants consideration, as the majority of countries in our analysis had limited time points, which can introduce some uncertainty in the trend analysis. Fourth, it is important to note that the GSHS question underlying our findings are derived from does not differentiate between traditional cigarette smoking and other forms of smoking such as e-cigarettes or shisha. Consequently, the interpretation of the results is limited to general secondhand smoke exposure. Further studies that incorporate more detailed assessments to distinguish between different types of SHS are needed. Lastly, it is important to consider that our findings may differ from the current situation. This suggests that the current trends might have changed, underscoring the need for further study.
Despite these limitations, this study’s significant strength lies in utilizing large, representative samples of adolescents from 27 countries across the five continents. This extensive coverage offers a thorough overview of adolescent SHS trends internationally. Additionally, acknowledging that SHS is influenced by factors beyond individual control, we analyzed the policies and their compliance, as reported by the WHO, to evaluate how effectively each country is implementing the WHO’s guidelines.
Policy implications
Nations witnessing a decline in SHS commonly enforce comprehensive smoke-free laws, a trend reflecting heightened awareness advocated by WHO’s Tobacco Free Initiative and FCTC. Out of the 14 countries experiencing this reduction, 12 have implemented designated smoke-free areas33. However, establishing these zones in all public spaces remains uncommon, and global efforts to extend regulations to private vehicles or outdoor children’s areas are limited34.
As previous studies have noted, adolescents are most likely to be exposed to SHS at home or in cars, with as much as 85% of exposure occurring in private vehicles35. This highlights the importance of considering exposure within private vehicles. Although existing research has differentiated between public places and homes, showing a decrease in home-based SHS exposure36, there is a lack of regulation and research concerning exposure in private vehicles37. Given this situation, it is now critical to implement regulations addressing SHS exposure in private vehicles.
Conclusion
Our comprehensive analysis, which included a representative sample of adolescents from 27 countries across the five continents, revealed a notable trend: 14 of these countries showed a decrease in SHS exposure, while Benin, the Maldives, and Myanmar had a significant increase. Additionally, the study highlighted the distinct sex disproportion of SHS in some countries. The expansion of smoke-free environments has likely contributed to the overall decrease in SHS exposure across the surveyed countries. However, there remain significant gaps, which underscore the urgency for more robust national and global policies. The establishment of comprehensive regulations, coupled with ongoing monitoring by international organizations, is critical to effectively reduce adolescent exposure to SHS. This approach is particularly important in addressing the diverse challenges and trends observed across different countries and demographic groups.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Dr. DKY had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version of the manuscript before submission. Study concept and design: SL, SH, SW, LS, and DKY; acquisition, analysis, or interpretation of data: SL, SH, SW, LS, and DKY; drafting of the manuscript: SL, SH, SW, LS, and DKY; critical revision of the manuscript for important intellectual content: all authors; statistical analysis: SL, SH, SW, LS, and DKY; study supervision: DKY. DKY supervised the study and served as a guarantor. SL and SH contributed equally as the first authors. SW and DKY contributed equally as corresponding authors. The corresponding author attests that all listed authors meet the authorship criteria and that no one meeting the criteria has been omitted.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (RS-2024-00460379). In addition, this work was supported by Institute of Information & communications Technology Planning & Evaluation (IITP) grant funded by the Korea government (MSIT) (RS-2022-00143911, AI Excellence Global Innovative Leader Education Program). The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Data availability
Data are available on reasonable request. Study protocol, statistical code: available from DKY (email: yonkkang@gmail.com). Data set: available from the World Health Organization and the US Centers for Disease Control and Prevention through a data use agreement. The Global School-based Student Health Survey is publicly accessible at the following link: https://extranet.who.int/ncdsmicrodata/index.php/catalog/gshs/?page=1&ps=15&repo=GSHS.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sooji Lee and Seohyun Hong contributed equally to this work.
Contributor Information
Selin Woo, Email: dntpfls@naver.com.
Dong Keon Yon, Email: yonkkang@gmail.com.
References
- 1.Flor, L. S. et al. Health effects associated with exposure to secondhand smoke: a Burden of Proof study. Nat. Med.10.1038/s41591-023-02743-4 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yon, D. K. et al. Indoor exposure and sensitization to Formaldehyde among Inner-City children with increased risk for Asthma and Rhinitis. Am. J. Respir Crit. Care Med.200, 388–393. 10.1164/rccm.201810-1980LE (2019). [DOI] [PubMed] [Google Scholar]
- 3.3 Mourino, N. et al. Pre- and postnatal exposure to secondhand tobacco smoke and cardiometabolic risk at 12 years: periods of susceptibility. Environ. Res.224, 115572. 10.1016/j.envres.2023.115572 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sathish, T. et al. Variations in risks from smoking between high-income, middle-income, and low-income countries: an analysis of data from 179 000 participants from 63 countries. Lancet Glob Health. 10, e216–e226. 10.1016/s2214-109x(21)00509-x (2022). [DOI] [PubMed] [Google Scholar]
- 5.Chung-Hall, J., Craig, L., Gravely, S., Sansone, N. & Fong, G. T. Impact of the WHO FCTC over the first decade: a global evidence review prepared for the Impact Assessment Expert Group. Tob. Control. 28, s119–s128. 10.1136/tobaccocontrol-2018-054389 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornelius, M. E. et al. Tobacco product use among adults - United States, 2021. MMWR Morb Mortal. Wkly. Rep.72, 475–483. 10.15585/mmwr.mm7218a1 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colyer-Patel, K., Kuhns, L., Weidema, A., Lesscher, H. & Cousijn, J. Age-dependent effects of tobacco smoke and nicotine on cognition and the brain: a systematic review of the human and animal literature comparing adolescents and adults. Neurosci. Biobehav Rev.146, 105038. 10.1016/j.neubiorev.2023.105038 (2023). [DOI] [PubMed] [Google Scholar]
- 8.Raghuveer, G. et al. Cardiovascular consequences of Childhood Secondhand Tobacco smoke exposure: prevailing evidence, Burden, and racial and socioeconomic disparities: A Scientific Statement from the American Heart Association. Circulation134, e336–e359. 10.1161/cir.0000000000000443 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou, W. et al. Association between secondhand smoke exposure in pregnant women and their socioeconomic status and its interaction with age: a cross-sectional study. BMC Pregnancy Childbirth. 22, 695 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oberg, M., Jaakkola, M. S., Woodward, A., Peruga, A. & Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet377, 139–146. 10.1016/s0140-6736(10)61388-8 (2011). [DOI] [PubMed] [Google Scholar]
- 11.Carreras, G. et al. Burden of disease attributable to second-hand smoke exposure: a systematic review. Prev. Med.129, 105833. 10.1016/j.ypmed.2019.105833 (2019). [DOI] [PubMed] [Google Scholar]
- 12.Lin, L. Z. et al. Pre-conceptional and prenatal exposure to secondhand smoke and autism spectrum disorder: a national multi-center study in China. World J. Pediatr.19, 761–769. 10.1007/s12519-022-00644-z (2023). [DOI] [PubMed] [Google Scholar]
- 13.Shin, H. et al. Estimated prevalence and trends in smoking among adolescents in South Korea, 2005–2021: a nationwide serial study. World J. Pediatr.19, 366–377. 10.1007/s12519-022-00673-8 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shakya, H. B. et al. Adolescent gender norms and adult health outcomes in the USA: a prospective cohort study. Lancet Child. Adolesc. Health. 3, 529–538. 10.1016/s2352-4642(19)30160-9 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong, S. et al. Global association of secondhand smoke exposure locations and smoking behaviour among adolescents in 99 countries. Acta Paediatr.113, 2048–2060. 10.1111/apa.17319 (2024). [DOI] [PubMed] [Google Scholar]
- 16.Lee, Y., Kim, S., Kim, M. K., Kawachi, I. & Oh, J. Association between Tobacco Industry Interference Index (TIII) and MPOWER measures and adult daily smoking prevalence rate in 30 countries. Global Health. 20, 6. 10.1186/s12992-023-01003-x (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith, L. et al. Global time trends of perceived loneliness among adolescents from 28 countries in Africa, Asia, and the Americas. J. Affect. Disord. 346, 192–199. 10.1016/j.jad.2023.11.032 (2024). [DOI] [PubMed] [Google Scholar]
- 18.Lee, S. W. Regression analysis for continuous independent variables in medical research: statistical standard and guideline of Life Cycle Committee. Life Cycle. 2, e3. 10.54724/lc.2022.e3 (2022). [Google Scholar]
- 19.Gorini, G., Costantini, A. S. & Paci, E. Smoking prevalence in Italy after the smoking ban: towards a comprehensive evaluation of tobacco control programs in Europe. Prev. Med.45, 123–124. 10.1016/j.ypmed.2007.06.019 (2007). [DOI] [PubMed] [Google Scholar]
- 20.Fernández, E. et al. Changes in secondhand smoke exposure after smoke-free legislation (Spain, 2006–2011). Nicotine Tob. Res.19, 1390–1394. 10.1093/ntr/ntx040 (2017). [DOI] [PubMed] [Google Scholar]
- 21.Cheong, C. et al. National trends in alcohol consumption, smoking, suicide attempts, and COVID-19 pandemic-related factors among South Korean adolescents, 2012–2022. Asian J. Psychiatr. 97, 104085. 10.1016/j.ajp.2024.104085 (2024). [DOI] [PubMed] [Google Scholar]
- 22.Organization, W. H. WHO report on the global tobacco epidemic, 2023: protect people from tobacco smoke, https://www.who.int/publications/i/item/9789240077164 (2023).
- 23.DeCicca, P., Kenkel, D. & Lovenheim, M. F. The Economics of Tobacco Regulation: a Comprehensive Review. J. Econ. Lit.60, 883–970. 10.1257/jel.20201482 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Padmawati, R. S., Prabandari, Y. S., Istiyani, T., Nichter, M. & Nichter, M. Establishing a community-based smoke-free homes movement in Indonesia. Tob. Prev. Cessat.4, 36. 10.18332/tpc/99506 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hong, S. et al. National prevalence of smoking among adolescents at tobacco tax increase and COVID-19 pandemic in South Korea, 2005–2022. Sci. Rep.14, 7823. 10.1038/s41598-024-58446-4 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flor, L. S., Reitsma, M. B., Gupta, V., Ng, M. & Gakidou, E. The effects of tobacco control policies on global smoking prevalence. Nat. Med.27, 239–243. 10.1038/s41591-020-01210-8 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Husain, M. J., English, L. M. & Ramanandraibe, N. An overview of tobacco control and prevention policy status in Africa. Prev. Med.91s, S16–s22. 10.1016/j.ypmed.2016.02.017 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Control, W. F. C. & o., C. Needs Assessment Factsheet: Benin, (2015). https://fctc.who.int/publications/m/item/needs-assessment-factsheet-benin
- 29.Jitnarin, N. et al. Socioeconomic status and smoking among Thai adults: results of the National Thai Food Consumption Survey. Asia Pac. J. Public. Health. 23, 672–681. 10.1177/1010539509352200 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kornienko, O., Santos, C. E., Martin, C. L. & Granger, K. L. peer influence on gender identity development in adolescence. Dev. Psychol.52, 1578–1592. 10.1037/dev0000200 (2016). [DOI] [PubMed] [Google Scholar]
- 31.Maccoby, E. E. Gender and relationships. A developmental account. Am. Psychol.45, 513–520. 10.1037/0003-066x.45.4.513 (1990). [DOI] [PubMed] [Google Scholar]
- 32.Woo, H. G. et al. Association of transitioning from combustible cigarettes to noncombustible nicotine or tobacco products with subsequent cancer risk: a nationwide cohort study in South Korea. Life Cycle. 4, e2. 10.54724/lc.2024.e2 (2024). [Google Scholar]
- 33.Mahase, E. Rising number of countries are controlling tobacco but progress is slowing, WHO warns. Bmj382, 1778. 10.1136/bmj.p1778 (2023). [DOI] [PubMed] [Google Scholar]
- 34.Boderie, N. W. et al. Public support for smoke-free policies in outdoor areas and (semi-)private places: a systematic review and meta-analysis. EClinicalMedicine59, 101982. 10.1016/j.eclinm.2023.101982 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cartmell, K. B. et al. Secondhand smoke exposure in young people and parental rules against smoking at home and in the car. Public. Health Rep.126, 575–582. 10.1177/003335491112600414 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma, C. et al. Global trends in the prevalence of secondhand smoke exposure among adolescents aged 12–16 years from 1999 to 2018: an analysis of repeated cross-sectional surveys. Lancet Glob Health. 9, e1667–e1678. 10.1016/s2214-109x(21)00365-x (2021). [DOI] [PubMed] [Google Scholar]
- 37.Kegler, M. C., Escoffery, C. & Butler, S. A qualitative study on establishing and enforcing smoking rules in family cars. Nicotine Tob. Res.10, 493–497. 10.1080/14622200801901963 (2008). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request. Study protocol, statistical code: available from DKY (email: yonkkang@gmail.com). Data set: available from the World Health Organization and the US Centers for Disease Control and Prevention through a data use agreement. The Global School-based Student Health Survey is publicly accessible at the following link: https://extranet.who.int/ncdsmicrodata/index.php/catalog/gshs/?page=1&ps=15&repo=GSHS.