Abstract
[Purpose] To analyze the correlation between the timed up-and-go time and functional independence measure total score in postoperative elderly patients with vertebral and hip fractures. [Participants and Methods] The total functional independence measure scores and timed up-and-go times of 87 Japanese patients aged ≥65 years with a history of vertebral or hip fracture surgery were analyzed. Patients were classified based on age (<85 or ≥85 years), sex (female or male), fracture type (vertebral or hip fracture), and postoperative period (early or late). [Results] In the comparative analyses between the two datasets within the groups, significant differences were observed in functional independence measure scores and timed up-and-go times between patients in the early and late postoperative periods. In the correlation analyses using functional independence measure scores and timed up-and-go times, significant negative correlations were observed in all groups, except for one group of patients in the late postoperative period. In the contingency table analyses, several patients with low functional independence measure scores had a timed up-and-go time of >35 s. Receiver operating characteristic curve analysis indicated that a timed up-and-go time of >35 s can be a predictive marker of nursing care requirement in the early postoperative period. [Conclusion] In the present study, we clarified the relationship between functional independence measure score and timed up-and-go time in postoperative elderly patients with vertebral and hip fractures and confirmed that timed up-and-go time is a predictive marker of nursing care requirement.
Keywords: Postoperative elderly patients with vertebral/hip fractures, Functional independence measure (FIM), Timed up & go (TUG)
INTRODUCTION
The aging of the population in developed countries is progressing rapidly1). Among developed countries, Japan has the highest aging rate1). Therefore, in Japan, there is high demand for nursing care for elderly people. Within the elderly population, the more fractures caused by falls that they sustain, the more nursing care they will require2). When elderly people experience vertebral/hip fractures caused by falls, they will certainly require complete nursing care in the acute period. However, it is also necessary to predict whether patients will need nursing care in the postoperative period. In this study, we intended to evaluate postoperative elderly patients with vertebral/hip fractures using a combined assessment of the Functional Independence Measure (FIM) score and the Timed Up & Go (TUG) time.
The FIM score is widely used throughout the world3). In addition to the FIM score, there are several other assessment tools for evaluating daily life activities including the Barthel Index4). However, among these measures, the FIM is the most widely accepted functional assessment measure in the rehabilitation community because the FIM exhibits the best evaluation in terms of reliability, validity, and responsiveness4). The prototype of the FIM was reported by Keith et al. in 19875), but the items within this prototype were not identical to those of the current version. The current version of the FIM has a total of 18 items (13 motor items and 5 cognitive items), and each item is scored on a 7-point scale based on the degree of dependency. When the degree of dependency is “no helper”, the examinee receives 6 or 7 points. When the degree of dependency is “modified dependence on a helper”, the examinee receives 3, 4, or 5 points. When the degree of dependency is “complete dependence on a helper”, the examinee receives 1 or 2 points.
The TUG test is a mobility measure that assesses balance and the risk of falling. The TUG test measures the time it takes for a person to stand up from a chair, walk to a target point 3 meters away, turn around, and sit back down in a chair. This test was first reported by Podsiadlo et al. in 19916). There have been many reports on the use of the TUG time to evaluate motor impairment in aging7), stroke8), chronic obstructive pulmonary disease9), Parkinson disease10), and hip fractures11), among other conditions. However, Barry reported that the TUG time has limited ability to predict falls in community-dwelling elderly people12). Thus, we questioned whether the TUG time is useful for predicting the necessity of nursing care in postoperative elderly patients with vertebral/hip fractures caused by falls.
In order to answer the above question, we conducted a study with elderly patients in Japan who had undergone spinal or hip fracture surgery and investigated the possibility of predicting the nursing care requirement (NCR) by the TUG time.
PARTICIPANTS AND METHODS
We conducted a two-center, retrospective observational study at Komenoyama Hospital (Omuta, Japan) and Sakata Orthopedic Clinic (Okayama, Japan). Patients with a history of vertebral or hip fracture surgery were collected from January to December 2019. In this study, we included only patients with an interval of less than 1 week between FIM score measurement and the TUG test. The exclusion criteria were (1) patients younger than 65 years, (2) patients with dementia who were unable to follow simple instructions, and (3) patients with motor dysfunction who were unable to get up from a chair.
Eighty-nine patients with a history of vertebral or hip fracture surgery were enrolled in this study, among whom 87 were included in the analyses. All patients who participated in this study were already in a stable postoperative condition and undergoing rehabilitation. The patients were classified by age (<85 or ≥85 years), sex (female or male), fracture type (vertebral or hip fracture), and postoperative period (early or late). This study was approved by the Kobe Gakuin University Research Ethics Committee on October 27, 2023 (reference no. 23-06). Informed consent was obtained from all patients involved in this study.
We used the Japanese form of the FIM™ version 3.013, 14), which has culturally relevant modifications for some of the items15, 16). The FIM score was determined by physical therapists. We initiated this study with the hypothesis that a total FIM score of >90 points reflects an independent condition (requiring no nursing care) and that a total FIM score of ≤90 points reflects a dependent condition (requiring nursing care). Thus, the operational definition of requiring nursing care was the condition of having a total FIM score of ≤90 points for the motor and cognitive items.
Participants in this study were administered the TUG test in accordance with the original method reported by Podsiadlo and Richardson6). The participants were asked to walk at their usual walking speed. All movements in the TUG test were performed at a comfortable and safe pace. Whether the participant turned around in a clockwise versus a counterclockwise direction was left to the individual patient, and the TUG time was measured twice, with the second value used as the result.
In this paper, for analysis, patients with vertebral fractures who had passed the acute phase were considered as postoperative patients, regardless of whether they underwent surgery or not. The Shapiro–Wilk test was used to confirm normality. Continuous and normally distributed data are presented as the mean value with standard deviation. Normally distributed data were compared using Student’s t-test or Welch’s t-test, while non-normally distributed data were compared using the Mann–Whitney U test. Correlations between two variables were evaluated by the Spearman correlation coefficient (non-normally distributed data). Categorical data were compared using Fisher’s exact test (contingency table analysis). Receiver operating characteristic (ROC) analysis was performed using the cut-off value determined by crosstabulation analysis. R program (ver.4.3.2) was used to test for significant differences17). All statistical tests were two-tailed, and a p-value <0.05 was considered statistically significant.
RESULTS
The demographics information of the patients who participated in this study is shown in Table 1. We analyzed 87 patients with a mean age of 82.3 ± 6.9 years. Regarding sex, there were 67 women and 20 men. It should be noted that the number of women was three times higher than that of men. All patients had a medical history of vertebral or hip fracture; 40 had a vertebral fracture, and 47 had a hip fracture. They had undergone surgery before participating in the study; 49 had less than 2 months of postoperative follow-up time (early postoperative period), and 38 patients had more than 12 months of postoperative follow-up time (late postoperative period). The mean total FIM score was 110 ± 20.0, and the mean TUG time (s) was 20.8 ± 13.8.
Table 1. Demographic backgrounds of the patients (n=87).
| Age (years) | 82.3 ± 6.9 |
| Number of patients by sex (Female : Male) | 67 : 20 |
| Weight (kg) | 48.4 ± 6.9 |
| Heigt (cm) | 152.7 ± 8.1 |
| Number of patients by type of fracture (Vertebral : Hip) | 40 : 47 |
| Number of patients by postoperative period (Early : Late) | 49 : 38 |
| Total FIM score | 110.0 ± 20.0 |
| TUG (s) | 20.8 ± 13.8 |
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go.
Comparative analyses between two datasets within the groups were conducted. Table 2 shows the results of the comparative analyses between the old and young patients. The proportion of patients with hip fractures was significantly higher in the old patient group (≥85 years of age) than in the young patient group (<85 years of age). However, there were no significant differences in the total FIM scores or TUG times between these two patient groups. Table 3 showed the results of comparative analyses between female and male patients. The mean age of the female patients was significantly higher than that of the male patients. However, there were no significant differences in the total FIM scores or TUG times between these two groups. Table 4 showed the results of comparative analyses between patients with vertebral fracture and patients with hip fracture. There were no significant differences in the total FIM scores or TUG times between these two groups. Table 5 showed the results of comparative analyses between patients in the early postoperative period and patients in the late postoperative period. There were significant differences in the total FIM scores (p<0.01) and TUG times between these two groups (p<0.01).
Table 2. Comparative analysis between old and young patients.
| Old (n=37) | Young (n=50) | ||
| Number of patients by sex (Female : Male) | 32 : 5 | 35 : 15 | |
| Weight (kg) | 47.9 ± 5.9 | 48.9 ± 7.6 | |
| Heigt (cm) | 152.6 ± 47.9 | 152.8 ± 9.0 | |
| Number of patients by type of fracture (Vertebral : Hip) | 12 : 25 | 28 : 22 | * |
| Number of patients by postoperative period (Early : Late) | 17 : 20 | 32 : 18 | |
| Total FIM score | 109.0 ± 21.5 | 110.7 ± 18.8 | |
| TUG (s) | 23.4 ± 15.9 | 18.8 ± 11.8 |
*p<0.05.
Young (<85 years of age), Old (≥85 years of age).
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go.
Table 3. Comparative analysis between female and male patients.
| Female (n=67) | Male (n=20) | ||
| Age (years) | 83.3 ± 6.6 | 79.2 ± 6.8 | * |
| Weight (kg) | 47.9 ± 6.9 | 50.5 ± 6.8 | |
| Heigt (cm) | 151.1 ± 8.3 | 158.0 ± 4.7 | |
| Number of patients by type of fracture (Vertebral : Hip) | 28 : 39 | 12 : 8 | |
| Number of patients by postoperative period (Early : Late) | 35 : 32 | 14 : 6 | |
| Total FIM score | 109.8 ± 20.5 | 110.6 ± 18.3 | |
| TUG (s) | 20.2 ± 13.2 | 22.5 ± 15.9 |
*p<0.05.
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go.
Table 4. Comparative analysis between patients with vertebral and hip fractures.
| Vertebral (n=40) | Hip (n=47) | |
| Age (years) | 80.3 ± 6.4 | 84.0 ± 6.9 |
| Number of patients by sex (Female : Male) | 28 : 12 | 39 : 8 |
| Weight (kg) | 49.9 ± 5.8 | 47.2 ± 7.6 |
| Heigt (cm) | 152.5 ± 9.1 | 152.8 ± 7.3 |
| Number of patients by postoperative period (Early : Late) | 10 : 10 | 29 : 18 |
| Total FIM score | 113.4 ± 18.1 | 107.1 ± 21.1 |
| TUG (s) | 18.5 ± 12.4 | 22.7 ± 14.7 |
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go.
Table 5. Comparative analysis between early and late postoperational periods.
| Early (n=49) | Late (n=38) | ||
| Age (years) | 81.3 ± 7.7 | 83.7 ± 5.3 | |
| Number of patients by sex (Female : Male) | 35 : 14 | 32 : 6 | |
| Weight (kg) | 48.3 ± 8.7 | 48.7 ± 3.7 | |
| Heigt (cm) | 150.4 ± 9.3 | 155.6 ± 5.1 | |
| Number of patients by type of fracture (Vertebral : Hip) | 20 : 29 | 20 : 18 | |
| Total FIM score | 97.9 ± 19.3 | 125.5 ± 0.9 | *** |
| TUG (s) | 26.5 ± 15.3 | 13.4 ± 6.4 | *** |
***p<0.001.
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go.
To examine the possibility of prediction of nursing care requirement (NCR), a correlation analysis was conducted. Table 6 shows the results of correlation analyses between the TUG time and total FIM score in all patients and each group categorized by age, sex, fracture type, and postoperative period. Significant correlations were observed in all patient groups except one. The late postoperative period group showed no correlation between the TUG time and total FIM score.
Table 6. Correlation analysis for TUG time and FIM score.
| Groups | Correlation coefficient and 95% CI | |||
| All patients | (n=87) | −0.69*** | (−0.79, 0.56) | |
| Age | Young | (n=50) | −0.52*** | (−0.70, 0.29) |
| Old | (n=37) | −0.85*** | (−0.91, 0.72) | |
| Sex | Female | (n=67) | −0.64*** | (−0.77, 0.48) |
| Male | (n=20) | −0.87*** | (−0.95, 0.70) | |
| Fracture | Vertebral | (n=40) | −0.50** | (−0.70, 0.22) |
| Hip | (n=47) | −0.80*** | (−0.88, 0.66) | |
| Postoperative period | Early | (n=49) | −0.61*** | (−0.76, 0.40) |
| Late | (n=38) | 0.17 | (−0.16, 0.46) | |
***p<0.001.
Young (<85 years of age), Old (≥85 years of age).
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go; CI: confidence interval.
Then, we tested whether a TUG time of 35 s can be the prediction marker of NCR. Table 7 shows the contingency table analysis results for the TUG time. The odds ratio for a TUG time of >35 s when comparing early postoperative period patients with late postoperative period patients was 34.6 (95% CI, 3.9–1080.2, p<0.001). The odds ratio for a TUG time of >35 s when comparing a total FIM score of ≤90 points with a total FIM score of >90 points was 71.5 (95% CI, 11.1–701.1, p<0.001).
Table 7. Fisher’s exact test for frequency of patients with TUG time of >35 s.
| Groups | Odds | 95% CI | |
| Age | Young | 1 | − |
| Old | 3.29 | 0.91, 13.62 | |
| Sex | Female | 1 | − |
| Male | 0.79 | 0.20, 3.85 | |
| Fracture | Vertebral | 1 | − |
| Hip | 2.72 | 0.72, 12.83 | |
| Postoperative period | Late | 1 | − |
| Early | 34.60*** | 3.86, 1080.2 | |
| FIM score | >90 points | 1 | − |
| ≤90 points | 71.5*** | 11.1, 701.1 | |
***p<0.001.
Young (<85 years of age), Old (≥85 years of age).
Early (less than 2 months), Late (more than 12 months).
FIM: functional independence measure; TUG: timed up & go; CI: confidence interval.
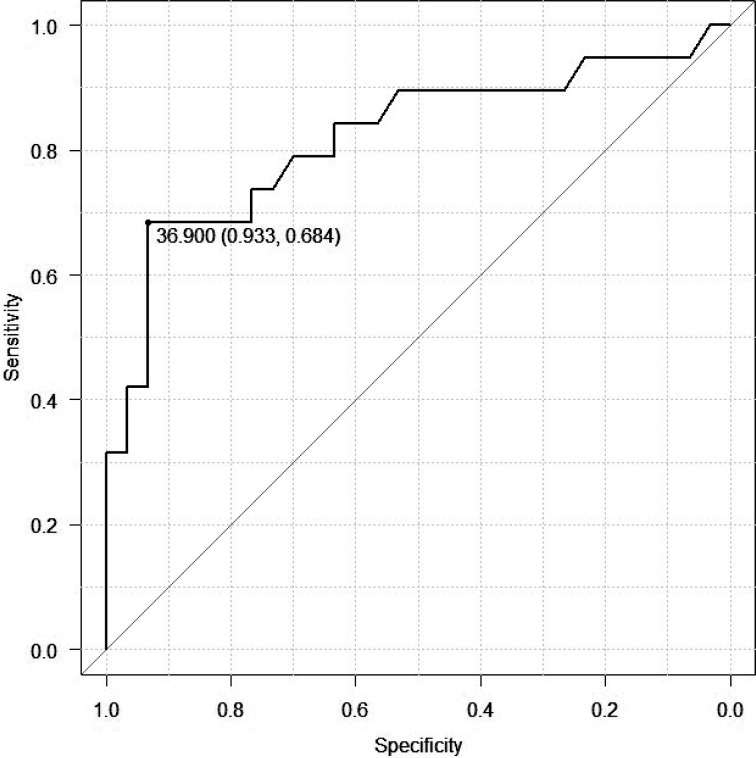
Finally, we performed ROC analysis using the data from patients in the early postoperative period (Fig. 1). The objective variable was a total FIM score of ≤90 points, and the explanatory variable was the TUG time. Here, the data from patients in the late postoperative period were omitted because no correlation was observed in this group (Table 6). Figure 1 shows the ROC analysis results in this study. The area under the curve (AUC) was 0.82, and the Youden Index was 36.9 s, which was close to the cut-off value (35 s) used in the contingency table analysis. The results confirmed that a TUG time of >35 s could be considered as a predictive factor for a total FIM score of £90 points (requiring nursing care).
Fig. 1.
Receiver operating characteristic (ROC) analysis between timed up & go (TUG) time and functional independence measure (FIM) scores of the patients in the early postoperative period.
The area under the curve (AUC) was 0.82, and the Youden Index was 36.9 s.
DISCUSSION
The TUG time and total FIM score are usually correlated with increasing age in community-dwelling people18). However, in our study, there were no significant differences in the total FIM scores or TUG times between the older patient group (≥85 years of age) and the younger patient group (<85 years of age). This result may reflect the effect of fractures and/or surgeries on the TUG time and total FIM score in elderly people. Nonetheless, we did not observe any significant differences in the total FIM scores or TUG times between patients with vertebral fractures and patients with hip fractures.
Thus, we sought to examine the relationship between the TUG time and total FIM score. According to our study, the TUG time (>35 s) was closely related to the total FIM score (≤90 points) in patients in the early postoperative period. This finding was observed in all groups regardless of categorization by age, sex, or fracture type (Table 6). Lee et al. reported a relationship between the TUG time and FIM scores in patients with stroke19) and suggested that the TUG time and FIM scores are closely related in patients with motor dysfunction in the lower extremities. Thus, the TUG time can be a good marker to predict the NCR of postoperative elderly patients with vertebral/hip fractures, especially for patients in the early postoperative period.
Next, the validity of the cutoff value of TUG time used in this study needs to be confirmed. As mentioned in the Methods section, we began this study with the hypothesis that a total FIM score of >90 points reflects an independent condition (requiring no nursing care) and that a total FIM score of ≤90 points reflects a dependent condition (requiring nursing care). The cut-off of the TUG test has not been clearly defined yet, and distributions of the TUG test results depend on the specific protocols (usual pace or maximal effort for walking speed) employed and patient demographics, according to previous studies20,21,22) In this study, patients were asked to walk at their usual walking speed in the TUG test, and the cut-off value of the TUG was 35 s.
A contingency table analysis in our study showed that a TUG time of greater than 35 s was often observed in patients with a total FIM score of ≤90 points, that is, in those patients requiring nursing care (Table 4). The ROC analysis results also suggested (with a high AUC value: 0.82) that a TUG time of >35 s can predict the NCR of early postoperative patients with vertebral/hip fractures (Youden Index: 36.9 s) (Fig. 1).
Interestingly, a long TUG time (>35 s) was not always related to a low total FIM score (≤90 points) for patients in the late postoperative period. Some of the late postoperative period patients had high total FIM scores and long TUG times, suggesting that they walk slowly but that they can do things independently in their daily lives. The postoperative period may be a major factor determining the level of independence in daily activities among patients with vertebral/hip fractures.
Although it is commonly known, elderly people do not need to walk fast to prevent fractures caused by falls. A slow walking speed and/or walking with a cane are beneficial for improving the lives of elderly people with diseases22, 23). Our study has confirmed two important points: (1) independent living is possible even if the TUG-related abilities have not fully recovered, and (2) elderly people do not need to walk fast to prevent fractures caused by falls. Therefore, this work should send an important message to late postoperative patients.
The limitations of this study include the small number of patients who participated in this study and the unavailability of longitudinal observations for each patient.
In conclusion, we found that the TUG time can be a predictive marker of NCR in early postoperative period patients with vertebral or hip fractures. Interestingly, some patients in the late postoperative period exhibited long TUG times, but they could function independently in their daily lives.
Funding
This study received no external funding.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We are deeply grateful to Mr. Kitamura (Physiotherapist at Komenoyama Hospital), Dr. Sakiyama (Director of Komenoyama), Dr. Sakata (Director of Sakata Orthopedic Clinic), and all patients who participated in this study. We also thank Jenna MacArthur, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
REFERENCES
- 1.Noto S: Perspectives on aging and quality of life. Healthcare (Basel), 2023, 11: 2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shapiro MJ, Partridge RA, Jenouri I, et al. : Functional decline in independent elders after minor traumatic injury. Acad Emerg Med, 2001, 8: 78–81. [DOI] [PubMed] [Google Scholar]
- 3.Linacre JM, Heinemann AW, Wright BD, et al. : The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil, 1994, 75: 127–132. [PubMed] [Google Scholar]
- 4.Cohen ME, Marino RJ: The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil, 2000, 81: S21–S29. [DOI] [PubMed] [Google Scholar]
- 5.Keith RA, Granger CV, Hamilton BB, et al. : The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil, 1987, 1: 6–18. [PubMed] [Google Scholar]
- 6.Podsiadlo D, Richardson S: The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 7.Beauchet O, Fantino B, Allali G, et al. : Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging, 2011, 15: 933–938. [DOI] [PubMed] [Google Scholar]
- 8.Chan PP, Si Tou JI, Tse MM, et al. : Reliability and validity of the timed up and go test with a motor task in people with chronic stroke. Arch Phys Med Rehabil, 2017, 98: 2213–2220. [DOI] [PubMed] [Google Scholar]
- 9.Albarrati AM, Gale NS, Munnery MM, et al. : The Timed Up and Go test predicts frailty in patients with COPD. NPJ Prim Care Respir Med, 2022, 32: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vieira de Moraes Filho A, Chaves SN, Martins WR, et al. : Progressive resistance training improves bradykinesia, motor symptoms and functional performance in patients with Parkinson’s disease. Clin Interv Aging, 2020, 15: 87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rix A, Lawrence D, Raper E, et al. : Measurement of mobility and physical function in patients hospitalized with hip fracture: a systematic review of instruments and their measurement properties. Phys Ther, 2022, 103: pzac142. [DOI] [PubMed] [Google Scholar]
- 12.Barry E, Galvin R, Keogh C, et al. : Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr, 2014, 14: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Data management service of the Uniform Data System for Medical Rehabilitation and the Center for Functional Assessment Research; Guide for use of the uniform data set for medical rehabilitation, State University of New York at Buffalo, version 3.0, March 1990.
- 14.Liu M, Sonoda S, Domen K: Stroke Impairment Assessment Set (SIAS) and Functional Independence Measure (FIM) and their practical use. In: Chino N, ed. Functional assessment of stroke patients: practical aspects of SIAS and FIM. Tokyo: SpringerVerlag, 1997: 17–139. [Google Scholar]
- 15.Tsuji T, Sonoda S, Domen K, et al. : ADL structure for stroke patients in Japan based on the functional independence measure. Am J Phys Med Rehabil, 1995, 74: 432–438. [DOI] [PubMed] [Google Scholar]
- 16.Yamada S, Liu M, Hase K, et al. : Development of a short version of the motor FIM for use in long-term care settings. J Rehabil Med, 2006, 38: 50–56. [DOI] [PubMed] [Google Scholar]
- 17.R Core Team (2023). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
- 18.Hayashi C, Ogata S, Okano T, et al. : Long-term participation in community group exercise improves lower extremity muscle strength and delays age-related declines in walking speed and physical function in older adults. Eur Rev Aging Phys Act, 2021, 18: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee JE, Chun H, Kim YS, et al. : Association between timed up and go test and subsequent functional dependency. J Korean Med Sci, 2020, 35: e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamide N, Takahashi K, Shiba Y: Reference values for the Timed Up and Go test in healthy Japanese elderly people: determination using the methodology of meta-analysis. Geriatr Gerontol Int, 2011, 11: 445–451. [DOI] [PubMed] [Google Scholar]
- 21.Schoene D, Wu SM, Mikolaizak AS, et al. : Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc, 2013, 61: 202–208. [DOI] [PubMed] [Google Scholar]
- 22.Sutin AR, Cajuste S, Stephan Y, et al. : Purpose in life and slow walking speed: cross-sectional and longitudinal associations. Geroscience, 2024, 46: 3377–3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avelino PR, Nascimento LR, Menezes KK, et al. : Effect of the provision of a cane on walking and social participation in individuals with stroke: protocol for a randomized trial. Braz J Phys Ther, 2018, 22: 168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]