Abstract
Background
Suicidal behaviors are prevalent public health concerns, and we need to improve our predictive ability to better inform prevention efforts.
Methods
Using nationwide longitudinal Swedish registers, we included 344,490 males and 323,177 females born 1982–1990 with information on genetic liability and environmental exposures from birth to age 16: perinatal variables, parental psychopathology (suicide attempt, substance use disorder, major depression), family status, socioeconomic difficulties, peers' psychopathology, and school grades. We conducted sex‐specific analysis and developed data‐driven predictive models including risk factors that occurred between ages 0 and 16 using structural equation modeling.
Results
In both females and males, the best‐fitting models reveal a complex risk pathway to suicide attempt. In females, the model indicates four direct effects on suicide attempt risk: the occurrence of suicide attempt in parents during childhood (β = 0.159, 95% CI: 0.118; 0.199) and adolescence (β = 0.115, 95% CI: 0.077; 0.153), suicide attempt in peers (β = 0.068, 95% CI: 0.057; 0.079), and low academic achievement (β = 0.166, 95% CI: 0.156; 0.175). In males, aggregate genetic liability for suicide attempt (β = 0.130, 95% CI: 0.111; 0.148), suicide attempt in parents during adolescence (β = 0.099, 95% CI: 0.074; 0.124), suicide attempt in peers (β = 0.118, 95% CI: 0.108; 0.129), and low academic achievement (β = 0.61, 95% CI: 0.152; 0.171) were related to later suicide attempt. These factors also acted as mediators to explain the association between environmental exposures in childhood and later suicide attempt.
Conclusions
These findings illustrate sex‐specific pathways to suicide attempt by including risk factors that occur during the development. Results highlight the importance of genetic and family environment but also the prominent role of academic achievement.
Keywords: academic achievement, family genetic risk, psychopathology, suicide attempt
Significant outcomes
This study revealed sex‐specific and complex pathways to suicide attempt risk, with the importance of childhood and adolescent environmental exposures in females, and the prominence of genetic risk and adolescent exposures in males.
Aggregate genetic liability was among the strongest risk factors in both sexes, but in females, the effect of aggregate genetic liability acted through the occurrence of parental suicide attempt, emphasizing the important counterpart of environmental adversity.
Academic achievement at age 16 was related to an increased risk of later suicide attempt in both males and females and acted as a mediator between socioeconomic adversity and suicide attempt.
Limitations
The use of registry data limits the study to inclusion of suicide attempts that came to the attention of medical workers, potentially missing attempts that did not require medical attention.
Though we considered a large amount of risk factors over the childhood and adolescence periods, the total amount of variance explaining suicide attempt in these models remains quite low, underscoring the complexity of suicide etiology.
1. INTRODUCTION
Reducing suicidal behaviors is among the top public health priorities of many countries, 1 but current meta‐analytic findings suggest that our predictive power is only slightly better than chance. 2 This limits our ability to prevent suicidal behaviors. To improve risk prediction, theoretical models inform about different ways to conceptualize risk factors. 3 , 4 Three main constructs are described: distal/predisposing, developmental/mediating, and precipitating factors. The two first categories broadly reflect genetic liability and environmental exposures that happen during development. The last category implicates the influence of stressful life events and their possible interactions with genetic liability, psychopathology, and suicide capability. A crucial way to move the field forward is to provide a better understanding of the complex relationships among these risk factors using empirical data. Prior studies also indicate that risk for non‐fatal and fatal suicide attempts only partially overlaps. 5 , 6 Accordingly, this study focused on non‐fatal suicide attempt.
The role of genetic liability for suicide phenotypes has been supported in many studies. First, twin research indicates heritability estimates for suicidal thoughts and behaviors between 30% and 55%. 5 , 7 Genome‐wide association studies are currently expanding and also support the importance of genetic factors in the etiology of suicide attempt. 8 Second, using family/genetic risk scores, computed based on phenotypic occurrence in the family and corrected for cohabitation effects, research shows the importance of genetic risk for suicide attempt and underscores the additional roles of genetic liability for substance use disorder and major depression. 9
Environmental risk factors include exposures as early as during the pre‐ and perinatal periods. 10 For example, being small for gestational age was related to increased risk of suicide attempt even after controlling for parental education and psychopathology. 11 Various family‐related exposures may also increase the risk of suicide attempt. One of the strongest risk factors is parental psychopathology, 12 , 13 , 14 , 15 especially substance use disorder. 16 This suggests that, in addition to the effect of genetic liability, the familial environment related to having parents with substance use disorder provides additional risk for suicide attempt. Generally, interpersonal difficulties and family conflicts are associated with suicide attempt risk during adolescence, 16 , 17 , 18 , 19 , 20 while supportive and positive family environments are important protective factors. 21 Other risk factors for suicide attempt include socioeconomic (i.e., living in a deprived neighborhood and receiving public assistance) and relational (i.e., separation, divorce, and death of parents) difficulties. 15 , 16 However, how the timing of these exposures is related to suicide attempt risk remains an active area of research. Though some studies suggested greater importance of early childhood adversity on risk for psychopathology, 22 adversity during adolescence also plays an important role in adult mental health. 23 Additionally, it is possible that the impact of perinatal and childhood exposures operates through adolescent risk factors rather than directly.
Beyond the family, the peer environment may have adverse effects on risky behaviors during adolescence. The influence of peers has been strongly documented in the substance use literature. 24 , 25 , 26 Studies focused on suicidal behaviors, however, have mainly indicated the adverse role of peers' victimization and bullying. 27 , 28 Initial evidence suggested that suicide attempt in peers increased the risk of suicide attempt in individuals from the same sex. 29 Studies in clinical populations also showed that adolescents who attempted suicide were more likely to be exposed to suicidal behaviors in friends and family. 30 , 31 Nevertheless, it remains unclear whether suicide attempt in peers is directly related to increased rates of suicide attempt in youth. Finally, poor academic achievement has been shown to be an important indicator of environmental adversity during adolescence. 32 Previous studies support inverse associations between academic achievement and suicide attempt, 33 , 34 but did not consider its interrelations with genetic and environmental risk factors. Considering these risk factors all together in a developmental model could improve our understanding of the complex pathways to non‐fatal suicide attempt.
We used Swedish national registries to evaluate the influence of genetic and various environmental factors from birth to age 16 on later risk for suicide attempt. We capitalized on longitudinal data to categorize risk factors into five groups: family/genetic, perinatal, early childhood (ages 0–6), childhood (ages 7–12), and adolescence (ages 13–16). 35 , 36 To account for the complexity of suicidal behavior, we used a data‐driven pathway analysis. 37 This approach combines risk factors from different domains into an integrated model.
1.1. Aims of the study
Our goal was to clarify the developmental pathways through which risk factors lead to suicide attempt by elucidating direct effects and possible mediational pathways. Providing a better understanding of the relationships between genetic and environmental risk factors and their association with suicide attempt may help improve suicide prevention and screening procedures.
2. MATERIALS AND METHODS
We collected information on individuals from Swedish population‐based registers with national coverage linking each person's unique personal identification number which, to preserve confidentiality, was replaced with a serial number by Statistics Sweden. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human subjects/patients were approved by the Regional Ethical Review Board in Lund and no participant consent was required (No. 2008/409 and later amendments).
We selected all individuals born from 1982 to 1990 in Sweden, and followed them until December 2018. In the database, we included several variables from different registers. An extended description can be found in the Supplement. Briefly, we included individual family genetic risk scores (FGRS) for four different disorders: suicide attempt, drug use disorder, alcohol use disorder, and major depression. The FGRSs are calculated from morbidity risks for disorders in first‐degree through fifth‐degree relatives. Information on registration for specific disorders in relatives is available in the registry data. FGRS arise from phenotypes in extended pedigrees and are weighted according to the numbers and type of relatives (e.g., the shared additive genetic effect is 0.5 for parents and 0.25 for aunts and uncles) and controlled for cohabitation effects. 38 , 39 To evaluate environmental exposures, we first included information from the Swedish Medical Birth register: smoking during pregnancy, parental age at birth, Apgar index, pre‐term birth, birth weight, birth length, and family status (i.e., parental co‐residence) at birth. Then, we included information on environmental exposures during three specific time periods: early childhood (0–6 years old), childhood (7–12 years old), and adolescence (13–16 years old). For each period, we included information on parental psychopathology (major depression, substance use disorder, and suicide attempt in parents) and social welfare assistance. For the adolescent period (age 16) we also included information on psychopathology in peers (rates of major depression, substance use disorder, and suicide attempt among individuals from the same school), individual school grades, neighborhood of residence, and family status (residing with both parents between 0 and 15 years). Overall, we included 29 different variables that have been previously related to suicidal behavior and underscored as important predictors in theoretical models (Table S1). Note that some variables are the same (e.g., social welfare) but evaluated at different time periods. Because we included variables from the family environment and the occurrence of suicide attempt in parents, we also conducted a sensitivity analysis using a modified FGRS for suicide attempt that excluded the parents' phenotypes (see Supplement). For males we have complete information on all variables for 344,490 of all 482,779 (71.3%) individuals, and for females we have complete information on all variables for 323,177 of all 456,222 (70.8%) individuals.
2.1. Statistical analysis
The path model consisted of path and correlation coefficients connecting the 29 observed variables of the model. We followed a data‐driven approach developed in previous studies 37 , 40 , 41 , 42 : We began with a fully saturated model and used a combination of three approaches to produce a model with the optimal balance of explanatory power and parsimony. In the first step, observing the significance levels of individual paths, we fixed sets of paths to zero when the associated z‐value was <1.96. Second, we set all path estimates with a value of <0.05 to zero, regardless of z‐value, as those paths were significant but too small to be meaningful. Third, we added and subtracted paths that were marginal by significance and/or magnitude to see if we could arrive at a better overall fit and indeed produced a modest improvement in fit and explanatory power. We utilized two fit indices that reflect the success of the model in balancing explanatory power and parsimony: the Tucker–Lewis index (TLI) and the root mean square error of approximation (RMSEA). For the TLI, values between 0.90 and 0.95 are considered acceptable and values ≥0.95 as good. For the RMSEA, good models have values ≤0.05. This is detailed in the Appendix and based on prior literature and theoretical models. We conducted sex‐specific analyses. To evaluate the predictive power of our model variables, we estimated the model in a random half of the sample and then applied it on the other half of the sample. The fit function was weighted least squares. Model fitting was done by using Mplus, version 7.31. Results are presented as standardized partial regression coefficients and 95% Confidence Intervals (CI). Note that the 4 FGRSs are interconnected by correlations, rather than partial regression coefficients.
3. RESULTS
3.1. Descriptive analyses
Table 1 reports the prevalence for the different risk factors. During the follow‐up period, 5% of females and 4.5% of males attempted suicide.
TABLE 1.
Descriptive statistics.
| Females | Males | |
|---|---|---|
| Family genetic risk score | ||
| FGRSSA (4 groups based on K‐means clustering) | ||
| Very low genetic risk | 64% | 64% |
| Low genetic risk | 27% | 27% |
| High genetic risk | 8% | 8% |
| Very high genetic risk | 2% | 2% |
| FGRSDUD (4 groups based on K‐means clustering) | ||
| Very low genetic risk | 72% | 72% |
| Low genetic risk | 22% | 22% |
| High genetic risk | 6% | 6% |
| High genetic risk | 1% | 1% |
| FGRSAUD (4 groups based on K‐means clustering) | ||
| Very low genetic risk | 60% | 60% |
| Low genetic risk | 28% | 28% |
| High genetic risk | 9% | 9% |
| Very high genetic risk | 2% | 2% |
| FGRSMD (4 groups based on K‐means clustering) | ||
| Very low genetic risk | 37% | 37% |
| Low genetic risk | 41% | 41% |
| High genetic risk | 18% | 18% |
| Very high genetic risk | 4% | 4% |
| Perinatal factors | ||
| Smoking during pregnancy | 27.9% | 28.0% |
| Family status at birth (not living with father) | 5.0% | 5.0% |
| Younger age at birth (below 35) | 89.1% | 89.5% |
| Early birth (<37 weeks) | – | 4.9% |
| Birth weight (5 groups based on the empirical distribution) | – | |
| Very low weight | 23% | 24% |
| Low weight | 22% | 22% |
| Medium weight | 21% | 19% |
| High weight | 18% | 18% |
| Very high weight | 16% | 17% |
| Birth length (5 groups based on the empirical distribution) | ||
| Very short length | 21% | 21% |
| Short length | 16% | 36% |
| Medium length | 40% | 18% |
| High length | 12% | 11% |
| Very high length | 11% | 14% |
| Apgar score (score between 5 and 7) | 1.3% | 1.7% |
| Early childhood factors (age 0–6) | ||
| Social welfare | 15.5% | – |
| Depression in parents | 0.4% | 0.4% |
| Substance use disorder in parents | 2.6% | 2.7% |
| Suicide attempt in parents | 1.0% | 1.0% |
| Childhood factors (ages 7–12) | ||
| Social Welfare | 20.2% | 20.1% |
| Depression in parents | 1.0% | 1.0% |
| Substance use disorder in parents | 3.4% | 3.4% |
| Suicide attempt in parents | 1.1% | – |
| Adolescence factors (ages 13–16) | ||
| Social Welfare | 13.7% | 13.6% |
| Depression in parents | 2.9% | 2.8% |
| Substance use disorder in parents | 3.4% | 3.4% |
| Suicide attempt in parents | 1.0% | 1.0% |
| Age 16 factors | ||
| Low grades (mean/SD) | −0.025 (0.95) | −0.026 (0.95) |
| Type of neighborhood | ||
| Deprived area | 27% | 27% |
| Medium area | 60% | 60% |
| Affluent area | 13% | 13% |
| Depression in peers (3 groups based on the empirical distribution) | ||
| Low depression | 33% | 33% |
| Medium depression | 33% | 33% |
| High depression | 34% | 34% |
| Substance use disorder in peers (3 groups based on the empirical distribution) | ||
| Low SUD | 33% | 33% |
| Medium SUD | 33% | 33% |
| High SUD | 34% | 34% |
| Suicide attempt in peers (3 groups based on the empirical distribution) | ||
| Low suicide attempt | 33% | 33% |
| Medium suicide attempt | 33% | 33% |
| High suicide attempt | 34% | 34% |
3.2. Path model in females
3.2.1. Model fitting
Model fitting resulted in a final model with good fit in both the training (RMSEA = 0.013 [0.013, 0.014], TLI = 0.978) and validation (RMSEA = 0.012 [0.011, 0.012], TLI = 0.984) samples. The model explained 11.6% of the total variance of suicide attempt in the training sample, and 11.7% in the validation sample. The model‐fitting process led to the exclusion of perinatal predictors (preterm birth, birth weight, birth length, and Apgar index) and family status during childhood. Variables included in the final model and path estimates are reported in Table S3, whereas the description below focuses on the most meaningful paths, that is, direct effects and mediational pathways (Figure 1).
FIGURE 1.
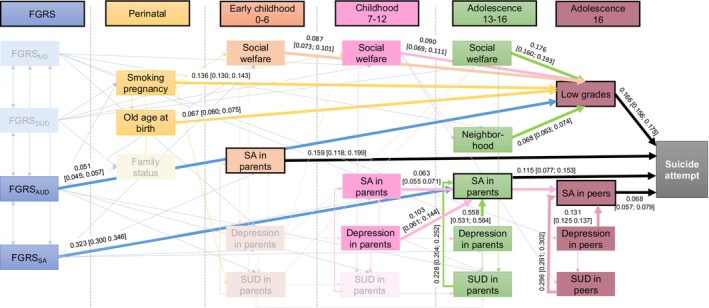
Path model in females.
3.2.2. Model description
First, the final model indicates that four risk factors were directly related to suicide attempt in females: suicide attempt in parents during early childhood (0–6 years; direct effect = 0.159, 95% CI = 0.118, 0.199) and adolescence (13–16 years; direct effect = 0.115, 95% CI = 0.077, 0.153), low school grades at age 16 (direct effect = 0.166, 95% CI = 0.156, 0.175), and suicide attempt in peers at age 16 (direct effect = 0.068, 95% CI = 0.057, 0.079). Though we did not observe a direct effect of genetic risk for suicide attempt in this model, FGRSSA was highly associated with suicide attempts in parents at all ages (see Table S3 for all path estimates) and was among the strongest total effects (total effect = 0.126, 95% CI = 0.118, 0.133).
Second, we identified three risk factors that may act as mediators—that is, variables that lie on indirect paths between other predictors and SA: academic achievement (low school grades), suicide attempt in parents during adolescence, and suicide attempt in peers.
Low grades at age 16 were related to genetic as well as perinatal and childhood factors: higher FGRS for alcohol use disorder (0.051, 95% CI = 0.045, 0.057), having a mother who smoked during pregnancy (0.136, 95% CI = 0.130, 0.143), being a mother who was older while pregnant (0.067, 95% CI = 0.060, 0.075), social welfare at all ages (0–6 years = 0.087, 95% CI = 0.073, 0.101; 6–12 years = 0.090 95% CI = 0.069, 0.111; 13–16 years = 0.176, 95% CI = 0.160, 0.193), and living in a deprived neighborhood in adolescence (0.068, 95% CI = 0.063, 0.074). These variables had indirect effects on suicide attempt risk via their association with low school grades.
Similarly, having parents who attempted suicide during adolescence was related to FGRS for suicide attempt (0.323, 95% CI = 0.300, 0.346), depression in parents during childhood (7–12 years: 0.103, 95% CI = 0.061, 0.144) and adolescence (13–16 years: 0.558, 95% CI = 0.531, 0.584). These factors were indirectly associated with increased suicide attempt risk through parental suicidal behavior.
Two measures of peer psychopathology at age 16 – depression (0.131, 95% CI = 0.125, 0.137) and substance use disorders (0.296, 95% CI = 0.291; 0.302)—were indirectly associated with risk of suicide attempt: Their effects were mediated through peers' suicide attempt.
We conducted a sensitivity analysis using a FGRS for suicide attempt that excluded the parents' phenotypes. Results did not differ substantially (Supplement). The most important difference was the increase in the variance explained by the model (from 11.7% to 13.7%), which can be related to the fact that after adjusting the FGRS, the effect of parental and environmental variables increased.
3.3. Path model in males
3.3.1. Model fitting
Model fitting indicated a final model with good fit in both the training (RMSEA = 0.013 [0.012, 0.014], TLI = 0.990) and validation (RMSEA = 0.012 [0.012, 0.012], TLI = 0.991) samples. The model explained 9.8% of the total variance of suicide attempt in the training sample, and 9.7% in the validation sample. The model‐fitting process led to the exclusion of three potential predictors: social welfare during early childhood (0–6 years), suicide attempt in parents during childhood (7–12 years), and family status between 0 and 15 years. Variables retained in the final model are depicted in Table S5. Below, we describe the direct effects and key mediational pathways (Figure 2).
FIGURE 2.
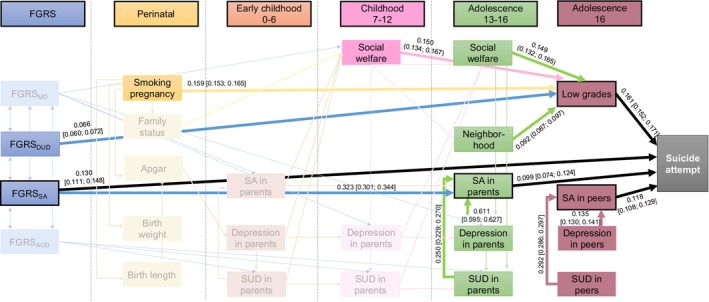
Path model in males.
3.3.2. Model description
There were four variables with significant direct effects on suicide attempt: aggregate genetic risk for suicide attempt (FGRSSA: direct effect = 0.130, 95% CI = 0.111; 0.148), suicide attempt in parents during adolescence (13–16 years: direct effect = 0.099, 95% CI = 0.074, 0.124), suicide attempt in peers at age 16 (direct effect = 0.118, 95% CI = 0.108, 0.129), and low school grades at age 16 (direct effect = 0.161, 95% CI = 0.152, 0.171).
Findings from this model highlight three central mediators, explaining the association between pre/perinatal variables, childhood factors, and suicide attempt risk: academic achievement, suicide attempt in parents during adolescence, and suicide attempt in peers.
Academic achievement was related to genetic risk for drug use disorder (0.066, 95% CI = 0.060, 0.072), maternal smoking during pregnancy (0.159, 95% CI = 0.153, 0.165), and socioeconomic difficulties such as social welfare during childhood (7–12 years: 0.150, 95% CI = 0.134, 0.167) and adolescence (13–16 years: 0.149, 95% CI = 0.132, 0.165), and living in a deprived neighborhood (0.092, 95% CI = 0.087, 0.097). All these variables had indirect effects on suicide attempt risk via the influence of school grades at age 16.
Suicide attempt in parents during the proband's adolescence (ages 13–16) was predicted by aggregate genetic risk for suicide attempt (0.323, 95% CI = 0.301, 0.344) and concurrent psychopathology in parents (depression [0.611, 95% CI = 0.595, 0.627] and substance use disorder [0.250, 95% CI = 0.229, 0.270]), which, therefore, had indirect effects on suicide attempt risk in offspring.
Similarly, suicide attempt in peers was predicted by psychopathology in peers, i.e., depression (0.135, 95% CI = 0.130, 0.141) and substance use disorder (0.292, 95% CI = 0.286, 0.297), those variables thus had indirect effects on proband's suicide attempt risk.
A sensitivity analysis was conducted using a FGRS that excluded the parents' phenotypes, but results did not differ substantially (Supplement).
4. DISCUSSION
The current study investigated the roles of genetic liability and several environmental exposures from early childhood to adolescence in risk for later suicide attempt. We developed data‐driven prediction models for suicide attempt and showed the distinct and combined effects of genetic and environmental exposures, providing important insights into the pathways to non‐fatal suicide attempt.
By conducting sex‐specific analyses, we found that the best‐fitting models differ in males and females. Though the existence of two different models precluded us from formally testing statistical differences between males and females, two points should be highlighted. First, we found sex‐specific effects regarding the role of genetic liability: In males, genetic liability was directly related to suicide attempt, while in females, the effect of genetic liability was indirect, mediated through parental suicide attempt in childhood. As FGRS are corrected for cohabitation effects, 38 they allow us to partially distinguish whether part of the risk arises from genetic factors or the environmental adversity of parental psychopathology. Consistent with prior evidence, 5 , 7 , 14 , 43 the current results indicate that both genetics and the family environment play a role in suicide attempt risk. Though the effect of genetics is complex and varies across the life course, it suggests that in females, the family environment might moderate the effect of genetic risk and constitute an interesting target for prevention. 43 Second, our results provide insights regarding the timing of risk with distinct observations in males and females. In females, though most of the perinatal factors could be removed from the model, childhood adversity plays a role in later suicide attempt. In males, both the direct and strongest total effects reflect risk factors during adolescence, suggesting that proximal risk factors are more important than earlier ones. Although childhood is an important developmental period where children build their knowledge and cognitive skills, 22 adolescence is a central period of maturation that leads to the construction of identity. 44 Both are strongly influenced by relationship quality and life events. In females, adversity in childhood and adolescence matter to define the risk of suicide attempt, but in males, difficulties experienced during the construction of identity seem to be more related to suicide attempt risk.
In addition to sex differences, these findings underscore the importance of three risk factors directly associated with suicide attempt in both sexes: parental suicide attempt during adolescence, peers' suicide attempt at age 16, and academic achievement. The role of peers' behaviors expands previous work suggesting an association between suicide attempt in peers and individual suicide attempt 29 , 30 , 31 by showing a direct effect of peers' behaviors in both sexes, with higher effect sizes in males. The role of peers may be understood through the contagion/imitation model, which is particularly prominent in adolescence. 45 Indeed, believing that peers endorse suicidal thoughts/behaviors is sufficient to increase the rate of self‐reported suicidal thoughts/behaviors in adolescence. 46 Our results emphasized peers' psychopathology and behaviors as important components of risk for later suicide attempt. This observation leads to clinical implications for the prevention of suicide attempt by encouraging strong monitoring of people who have been exposed to peers' suicidal behaviors. This could be done in school settings for adolescents but could also be asked in consultation as part of a screening for exposure to potential risk factors.
Moreover, the effect of academic achievement on suicide attempt risk was particularly salient in both sexes. This result is in line with previous studies, 33 , 47 , 48 including one using the Swedish registry data to demonstrate the potential causality of this association. 34 By considering a wide range of risk factors, the current study further shows how genetic liability (e.g., for substance use disorder) and environmental exposures (smoking during pregnancy, socioeconomic difficulties, deprivation in the neighborhood) were related to low school grades 32 and involved in the pathway to suicide attempt. Academic achievement constitutes an important direct and modifiable risk factor to prevent non‐fatal suicide attempt. Clinical trials indicate that improving academic achievement may help to delay suicidal thoughts and behaviors in youth, though adjustment for covariates attenuated these effects. 49 By showing the potential covariates associated with low school grades, our results may help improve the design of new interventions (e.g., include a component to target environmental adversity).
Finally, considering genetic liability and a wide range of environmental exposures did not support previous findings showing associations between suicide attempt and (1) familial difficulties, 15 , 16 here measured as having lived in a non‐intact family (divorce, separation, death, and single‐parent) from birth to age 15; and (2) perinatal factors, 11 here reflected by preterm birth, birth weight, length, and the Apgar index. This suggests that, when including other relevant risk factors, these factors rather have indirect effects on suicide attempt and might not be useful targets for suicide prevention.
The current results should be considered in the context of some limitations. First, we leveraged registry data to thoroughly document the influence of environmental exposures but other potentially important variables were not available to us (e.g., childhood neglect/abuse). Second, the use of registry data provides an objective measure of suicide attempt but is limited to including attempts that came to the attention of medical workers, either through self‐disclosure or due to medical care necessary in the wake of the attempt. We also included events of undetermined intent in our definition of suicide attempt. Though this is in line with previous recommendations, 50 this limits our information on true suicidal intent and estimates from this study should be considered conservative. Third, to construct our prediction models, we had to order the inclusion of risk factors, which assume causal rather than correlation paths between our predictors. Finally, the total amount of variance explaining suicide attempt in these models remains low (9%–11%). This reinforces the complexity of suicidal behaviors 2 but should also encourage future studies to build comprehensive prediction models focused on proximal risk factors such as stressful life events or psychopathology, 3 , 4 while including the main predisposing factors emphasized in the current study (genetic liability, familial and peer environment, and academic achievement). Another potential way to improve predictive power would be to increase specificity in the outcome definition, for example, focusing on high lethality attempts.
To Conclude, this study used Swedish registry data to explore the roles of genetic and environmental exposures in suicide attempt risk. We developed data‐driven prediction models for females and males which highlighted (i) the importance of direct risk factors (suicide attempt in parents, suicide attempt in peers during adolescence, and academic achievement; genetic liability in males) and (ii) meaningful mediation paths articulating the roles of socioeconomic difficulties and parental psychopathology. These findings may pave the way for future research and could inform public health actions about which factors to include in screening and prioritize in prevention.
AUTHOR CONTRIBUTIONS
Séverine Lannoy was responsible for conceptualization and writing (original draft); Henrik Ohlsson was responsible for conceptualization, data analysis, and writing (review and editing); Mallory Stephenson and Kenneth S. Kendler were responsible for writing (review and editing); Jan Sundquist and Kristina Sundquist were responsible for data access and writing (review and editing), and Alexis C. Edwards was responsible for conceptualization and writing (original draft, review and editing).
FUNDING INFORMATION
This project was supported by the National Institutes of Health (NIMH; to AE, grant number MH129356; NIAAA; to SL, grant number AA030611) and funding from the Swedish Research Council (2020‐01175).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
PEER REVIEW
The peer review history for this article is available at https://www.webofscience.com/api/gateway/wos/peer‐review/10.1111/acps.13761.
Supporting information
Data S1: Supporting Information.
Lannoy S, Ohlsson H, Stephenson M, et al. Prediction of suicide attempt in a Swedish population‐based cohort. Acta Psychiatr Scand. 2025;151(1):92‐101. doi: 10.1111/acps.13761
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as registry data are not publicly available.
REFERENCES
- 1. WHO . Suicide worldwide in 2019: global health estimates. 2021.
- 2. Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: a meta‐analysis of 50 years of research. Psychol Bull. 2017;143(2):187‐232. [DOI] [PubMed] [Google Scholar]
- 3. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387(10024):1227‐1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Díaz‐Oliván I, Porras‐Segovia A, Barrigón ML, Jiménez‐Muñoz L, Baca‐García E. Theoretical models of suicidal behaviour: a systematic review and narrative synthesis. Eur J Psychiatry. 2021;35(3):181‐192. [Google Scholar]
- 5. Edwards AC, Ohlsson H, Moscicki E, et al. On the genetic and environmental relationship between suicide attempt and death by suicide. Am J Psychiatry. 2021;178(11):1060‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mullins N, Kang J, Campos AI, et al. Dissecting the shared genetic architecture of suicide attempt, psychiatric disorders and known risk factors. Biol Psychiatry. 2022;91(3):313‐327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Voracek M, Loibl LM. Genetics of suicide: a systematic review of twin studies. Middle Eur J Med. 2007;119(15–16):463‐475. [DOI] [PubMed] [Google Scholar]
- 8. Docherty AR, Mullins N, Ashley‐Koch AE, et al. GWAS meta‐analysis of suicide attempt: identification of 12 genome‐wide significant loci and implication of genetic risks for specific health factors. Am J Psychiatry. 2023;180(10):723‐738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kendler KS, Ohlsson H, Mościcki EK, Sundquist J, Edwards AC, Sundquist K. Genetic liability to suicide attempt, suicide death, and psychiatric and substance use disorders on the risk for suicide attempt and suicide death: a Swedish national study. Psychol Med. 2021;1‐10:1639‐1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mittendorfer‐Rutz E, Wasserman D. Pregnancies in high psychosocial risk groups: research findings and implications for early intervention. Psychiatr Clin North Am. 2008;31(2):205‐212. [DOI] [PubMed] [Google Scholar]
- 11. Niederkrotenthaler T, Rasmussen F, Mittendorfer‐Rutz E. Perinatal conditions and parental age at birth as risk markers for subsequent suicide attempt and suicide: a population based case‐control study. Eur J Epidemiol. 2012;27(9):729‐738. [DOI] [PubMed] [Google Scholar]
- 12. King RA, Schwab‐Stone M, Flisher AJ, et al. Psychosocial and risk behavior correlates of youth suicide attempts and suicidal ideation. J Am Acad Child Adoesc Psychiatry. 2002;40(7):837‐846. [DOI] [PubMed] [Google Scholar]
- 13. Mok PL, Pedersen CB, Springate D, et al. Parental psychiatric disease and risks of attempted suicide and violent criminal offending in offspring: a population‐based cohort study. JAMA Psychiatry. 2016;73(10):1015‐1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kendler KS, Ohlsson H, Sundquist J, Sundquist K, Edwards AC. The sources of parent‐child transmission of risk for suicide attempt and deaths by suicide in Swedish National Samples. Am J Psychiatry. 2020;177(10):928‐935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bjorkenstam C, Kosidou K, Bjorkenstam E. Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. BMJ. 2017;357:j1334. [DOI] [PubMed] [Google Scholar]
- 16. Zygo M, Pawlowska B, Potembska E, Dreher P, Kapka‐Skrzypczak L. Prevalence and selected risk factors of suicidal ideation, suicidal tendencies and suicide attempts in young people aged 13‐19 years. Ann Agric Environ Med. 2019;26(2):329‐336. [DOI] [PubMed] [Google Scholar]
- 17. Hollis C. Depression, family environment, and adolescent suicidal behavior. J Am Acad Child Adoesc Psychiatry. 1996;35(5):622‐630. [DOI] [PubMed] [Google Scholar]
- 18. Janiri D, Doucet GE, Pompili M, et al. Risk and protective factors for childhood suicidality: a US population‐based study. Lancet Psychiatry. 2020;7(4):317‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu RT, Walsh RFL, Sheehan AE, Cheek SM, Sanzari CM. Prevalence and correlates of suicide and nonsuicidal self‐injury in children: a systematic review and meta‐analysis. JAMA Psychiatry. 2022;79(7):718‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson JG, Cohen P, Gould MS, Kasem S, Brown J, Brook JS. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen Psychiatry. 2002;59:741‐749. [DOI] [PubMed] [Google Scholar]
- 21. Zwald ML, Annor FB, Wilkinson A, et al. Suicidal ideation and attempts among students in grades 8, 10, and 12—Utah, 2015. 2018. Contract No.: 15. [DOI] [PMC free article] [PubMed]
- 22. Hertzman C. The significance of early childhood adversity. Paediatr Child Health. 2013;18(3):127‐128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pollmann A, Fritz J, Barker E, Fuhrmann D. Networks of adversity in childhood and adolescence and their relationship to adult mental health. Res Child Adolesc Psychopathol. 2023;51(12):1769‐1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Edwards AC, Gardner CO, Hickman M, Kendler KS. A prospective longitudinal model predicting early adult alcohol problems: evidence for a robust externalizing pathway. Psychol Med. 2016;46(5):957‐968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kendler KS, Ohlsson H, Sundquist K, Sundquist J. Peer deviance, parental divorce, and genetic risk in the prediction of drug abuse in a nationwide Swedish sample: evidence of environment‐environment and gene‐environment interaction. JAMA Psychiatry. 2014;71(4):439‐445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mason MJ, Light JM, Mennis J, et al. Neighborhood disorder, peer network health, and substance use among young urban adolescents. Drug Alcohol Depend. 2017;178:208‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaminski JW, Fang X. Victimization by peers and adolescent suicide in three US samples. J Pediatr. 2007;155(5):683‐688. [DOI] [PubMed] [Google Scholar]
- 28. O'Reilly LM, Pettersson E, Quinn PD, et al. A Co‐twin control study of the association between bullying victimization and self‐harm and suicide attempt in adolescence. J Adolesc Health. 2021;69(2):272‐279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fletcher JM. Gender‐specific pathways of peer influence on adolescent suicidal behaviors. Socius: sociological research for a dynamic. World. 2017;3:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schlagbaum P, Tissue JL, Sheftall AH, Ruch DA, Ackerman JP, Bridge JA. The impact of peer influencing on adolescent suicidal ideation and suicide attempts. J Psychiatr Res. 2021;140:529‐532. [DOI] [PubMed] [Google Scholar]
- 31. Athey A, Overholser JC, Beale EE. Depressed adolescents' exposure to suicide attempts and suicide loss. Death Stud. 2022;46(8):1862‐1869. [DOI] [PubMed] [Google Scholar]
- 32. Duke NN. Adolescent adversity, school attendance and academic achievement: school connection and the potential for mitigating risk. J Sch Health. 2020;90(8):618‐629. [DOI] [PubMed] [Google Scholar]
- 33. Sorberg Wallin A, Sorjonen K, Lager A, Falkstedt D. Academic performance, subsequent socioeconomic status and suicide attempt in adulthood: path analyses on Swedish cohort data. J Epidemiol Community Health. 2020;74(12):1002‐1007. [DOI] [PubMed] [Google Scholar]
- 34. Lannoy S, Ohlsson H, Kendler KS, Sundquist J, Sundquist K, Edwards AC. The causal effect of education and cognitive performance on risk for suicide attempt: a combined instrumental variable and co‐relative approach in a Swedish national cohort. J Affect Disord. 2022;305:115‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schroeder A, Slopen N, Mittal M. Accumulation, timing, and duration of early childhood adversity and behavior problems at age 9. J Clin Child Adolesc Psychol. 2020;49(1):36‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Edwards AC, Lonn SL, Karriker‐Jaffe KJ, Sundquist J, Kendler KS, Sundquist K. Time‐specific and cumulative effects of exposure to parental externalizing behavior on risk for young adult alcohol use disorder. Addict Behav. 2017;72:8‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry. 2002;159(7):1133‐1145. [DOI] [PubMed] [Google Scholar]
- 38. Kendler KS, Ohlsson H, Sundquist J, Sundquist K. The patterns of family genetic risk scores for eleven major psychiatric and substance use disorders in a Swedish national sample. Transl Psychiatry. 2021;11(1):326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kendler KS, Ohlsson H, Sundquist J, Sundquist K. Family genetic risk scores and the genetic architecture of major affective and psychotic disorders in a Swedish National Sample. JAMA Psychiatry. 2021;78(7):735‐743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kendler KS, Ohlsson H, Sundquist K, Sundquist J. Prediction of drug abuse recurrence: a Swedish National Study. Psychol Med. 2018;48(8):1367‐1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kendler KS, Ohlsson H, Edwards AC, Sundquist J, Sundquist K. A developmental model for alcohol use disorders in Swedish men. Psychol Med. 2016;46(13):2759‐2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kendler KS, Ohlsson H, Edwards AC, Sundquist J, Sundquist K. A developmental etiological model for drug abuse in men. Drug Alcohol Depend. 2017;179:220‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Brent DA, Melhem N. Familial transmission of suicidal behavior. Psychiatr Clin N Am. 2008;31(2):157‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Branje S. Adolescent identity development in context. Curr Opin Psychol. 2022;45:101286. [DOI] [PubMed] [Google Scholar]
- 45. Bilsen J. Suicide and youth: risk factors. Frontiers. Psychiatry. 2018;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reyes‐Portillo JA, Lake AM, Kleinman M, Gould MS. The relation between descriptive norms, suicide ideation, and suicide attempts among adolescents. Suicide Life Threat Behav. 2019;49(2):535‐546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gunnell D, Lofving S, Gustafsson JE, Allebeck P. School performance and risk of suicide in early adulthood: follow‐up of two national cohorts of Swedish schoolchildren. J Affect Disord. 2011;131(1–3):104‐112. [DOI] [PubMed] [Google Scholar]
- 48. Kosidou K, Dalman C, Fredlund P, et al. School performance and the risk of suicide attempts in young adults: a longitudinal population‐based study. Psychol Med. 2014;44(6):1235‐1243. [DOI] [PubMed] [Google Scholar]
- 49. Wilcox HC, Kellam SG, Brown CH, et al. The impact of two universal randomized first‐ and second‐grade classroom interventions on young adult suicide ideation and attempts. Drug Alcohol Depend. 2008;95(Suppl 1):S60‐S73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Randall JR, Roos LL, Lix LM, Katz LY, Bolton JM. Emergency department and inpatient coding for self‐harm and suicide attempts: validation using clinician assessment data. Int J Methods Psychiatr Res. 2017;26(3):e1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1: Supporting Information.
Data Availability Statement
Data sharing is not applicable to this article as registry data are not publicly available.


