Summary
Inferior vena cava (IVC) leiomyosarcomas are rare smooth muscle neoplasms that account for 0.5% of adult soft tissue sarcomas. They present with nonspecific symptoms and have poor prognosis. We present a case of leiomyosarcoma arising from the retrohepatic IVC that was difficult to diagnose on imaging, showing similar characteristics to intrahepatic cholangiocarcinoma including heterogenous arterial phase enhancement and delayed enhancement on contrast-enhanced magnetic resonance imaging. Important differentiating features of IVC leiomyosarcomas on imaging include dilated IVC, imperceptible IVC lumen, and development of prominent venous collaterals. Despite this, imaging features may be similar to other retrohepatic mass etiologies so IVC leiomyosarcoma should be included in the differential diagnosis of any retrohepatic mass and biopsy should be pursued.
Keywords: inferior vena cava leiomyosarcoma, magnetic resonance imaging
Vascular leiomyosarcomas are rare smooth muscle neoplasms of the vessel wall, accounting for 5% of all leiomyosarcomas (1). Specifically, primary leiomyosarcoma of the inferior vena cava (IVC) make up 0.5% of adult soft tissue sarcomas (2,3). Characteristics of IVC leiomyosarcomas include a female-to-male ratio of 3 to 1, a peak incidence in the sixth decade of life, predilection for arising from the middle segment of the IVC (between the hepatic and renal veins) and extraluminal growth (3-5).
Common presenting symptoms including abdominal pain, weight loss, an abdominal mass, nausea, and vomiting are non-specific and can lead to delayed diagnosis (2,6). Symptomatology may depend on tumor location. Tumors arising from the upper segment of the IVC (from the right atrium to the hepatic veins) may cause valvular obstruction, lower limb edema, and constrictive pericarditis. Tumors arising from the middle segment may cause Budd-Chiari syndrome. Tumors arising from the lower segment of the IVC (below the renal veins to the iliac confluence) may cause renovascular hypertension due to renal vein obstruction (2,3,6).
Ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) are typically used to diagnose, stage, and surveil IVC leiomyosarcomas. US generally shows a hypoechoic mass with tumoral vascularity. The IVC may demonstrate abnormal flow due to the intraluminal tumor. Lower extremity doppler may show abnormal waveform due to upstream tumoral obstruction. CT typically demonstrates an irregularly distended IVC with an enhancing lobulated soft tissue mass. While it is often difficult to differentiate IVC leiomyosarcomas from other retroperitoneal etiologies, important imaging findings include a dilated IVC and an imperceptible IVC lumen (7,8). In contrast, a negative embedded organ sign, where the IVC is narrowed due to extrinsic compression, suggests that the mass does not arise from the IVC (7). On MRI, the tumor is typically T1 hypointense, with heterogenous enhancement on post-contrast T1 images. The tumor also demonstrates T2 hyperintensity and diffusion restriction. Additional features include a prominent collateral circulation (2). There is typically no internal fat or calcification (8).
Prognosis is generally poor, with five-year disease-free survival and overall survival ranging from 6-28% and 34-55%, respectively (3,5). Surgical resection remains the mainstay of treatment. Larger tumor size, resection with positive margins, and older patient age are associated with decreased disease-free survival. Isolated involvement of the middle segment of the IVC is associated with increased disease-free survival (5). The use of adjuvant and neoadjuvant chemoradiotherapy is not well studied, likely related to tumor rarity.
A 68-year-old woman presented with chronic right upper quadrant pain. She reported a 10-pound weight loss in the past year. She had no jaundice, nausea, vomiting or change in abdominal girth. Her laboratory results showed a normal blood count, electrolytes and liver function tests. On US, a heterogeneously echogenic mass with mild internal vascularity was seen and was initially thought to be arising from the left hepatic lobe. She was referred to gastroenterology and repeat blood work demonstrated normal alpha-fetoprotein, cancer antigen 19-9 and hepatitis serology. MRI demonstrated a large mass along the posterior aspect of segment 4A of the liver. There was low-grade heterogeneous arterial enhancement with more progressive hyperenhancement on the portal and delayed phases (Figure 1A). The mass abutted the anterior wall of the intrahepatic IVC with no definite evidence of invasion. The MR findings were non-specific with the main differentials being an exophytic intrahepatic cholangiocarcinoma (ICC) or IVC leiomyosarcoma.
Figure 1.
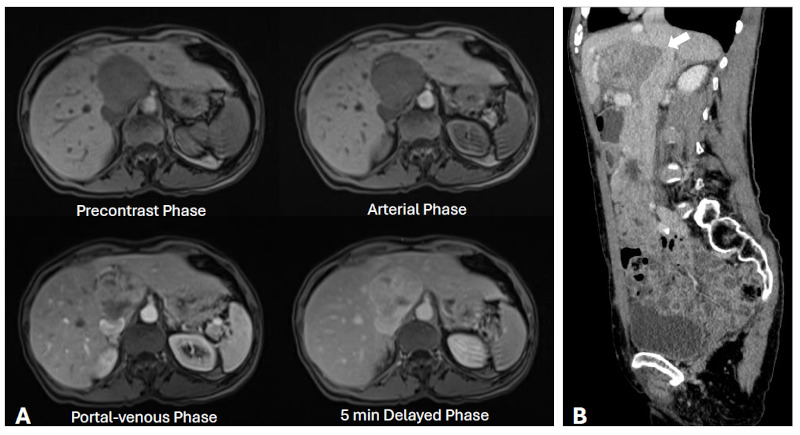
Imaging features of an IVC leiomyosarcoma. (A) Axial T1-weighted pre- and post-gadolinium contrast MRI images demonstrate delayed hyperenhancement of the large retrohepatic mass abutting the IVC; (B) Portal-venous phase sagittal CT image shows suspected intraluminal invasion (arrow) along the anterior IVC.
At the time of the proposed US-guided biopsy 1.5 months after initial presentation, the mass was found to move independently from the liver and was intimately associated with the intrahepatic IVC. The biopsy showed an atypical smooth muscle tumor consistent with either a primary hepatic leiomyosarcoma or an atypical smooth muscle tumor from elsewhere. A staging CT could not definitively determine whether the mass was an exophytic hepatic lesion or a mass of extrahepatic origin (Supplemental Figure S1, https://www.irdrjournal.com/supplementaldata/214). There was suspicion of intraluminal invasion along the anterior IVC (Figure 1B).
The patient underwent in vivo primary resection of the tumor 2.5 months after initial presentation including excision of a portion of IVC with concurrent primary repair and cholecystectomy. No hepatectomy was required. Final pathology revealed a FNCLCC grade 2 leiomyosarcoma (Figure 2) with negative margins; however, the distance from the tumor to the closest margin was less than 0.1 cm. The patient received a dose of adjuvant external beam radiation to the surgical bed post-operatively. The patient remained disease-free at the 8-month follow-up CT (Supplemental Figure S2, https://www.irdrjournal.com/supplementaldata/214).
Figure 2.
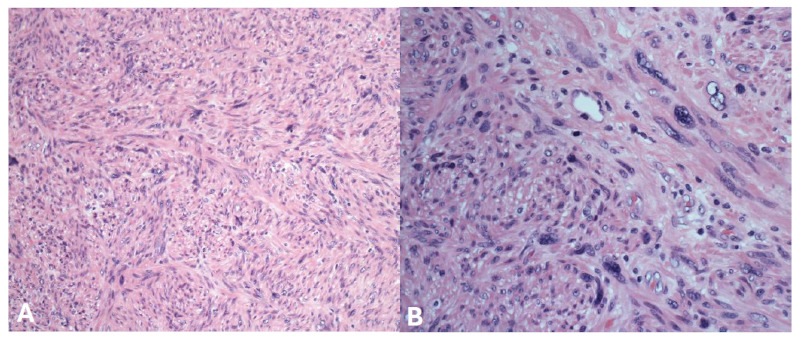
Pathologic characteristics of the IVC leiomyosarcoma. (A) 200×; (B) 400×. The sections show infiltration by a malignant neoplasm showing interlacing bundles of atypical smooth muscles with associated markedly atypical spindle cells with moderate amount of eosinophilic cytoplasm and occasional large, bizarre nuclei.
In our case, the delayed centipedal enhancement on MRI confounded diagnosis as both sarcomatous tumors and ICC can show delayed hyperenhancement due to abundant fibrous stroma. Although definite intraluminal tumor was not identified on initial imaging, IVC leiomyosarcomas are often predominantly extraluminal. As a result, the diagnosis of IVC leiomyosarcoma must be considered in the differential when evaluating a retrohepatic mass, despite its rarity. Potential differentiating features on imaging between IVC leiomyosarcoma and other retrohepatic masses include dilated IVC, imperceptible IVC lumen, and development of a prominent collateral venous system from IVC obstruction. Any liver lesion with suspicious imaging features should be recommended for biopsy.
Acknowledgements
We would like to thank the patient for participating in this study.
Funding:
None.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Matsuyama A, Hisaoka M, Hashimoto H. Vascular leiomyosarcoma: Clinicopathology and immunohistochemistry with special reference to a unique smooth muscle phenotype. Pathol Int. 2010; 60:212-216. [DOI] [PubMed] [Google Scholar]
- 2. Wang MX, Menias CO, Elsherif SB, Segaran N, Ganeshan D. Current update on IVC leiomyosarcoma. Abdom Radiol N Y. 2021; 46:5284-5296. [DOI] [PubMed] [Google Scholar]
- 3. Laskin WB, Fanburg-Smith JC, Burke AP, Kraszewska E, Fetsch JF, Miettinen M. Leiomyosarcoma of the inferior vena cava: Clinicopathologic study of 40 cases. Am J Surg Pathol. 2010; 34:873-881. [DOI] [PubMed] [Google Scholar]
- 4. Mingoli A, Cavallaro A, Sapienza P, Di Marzo L, Feldhaus RJ, Cavallari N. International registry of inferior vena cava leiomyosarcoma: Analysis of a world series on 218 patients. Anticancer Res. 1996; 16:3201-3205. [PubMed] [Google Scholar]
- 5. Wachtel H, Gupta M, Bartlett EK, Jackson BM, Kelz RR, Karakousis GC, Fraker DL, Roses RE. Outcomes after resection of leiomyosarcomas of the inferior vena cava: A pooled data analysis of 377 cases. Surg Oncol. 2015; 24:21-27. [DOI] [PubMed] [Google Scholar]
- 6. Das SAP, Paleela PS, Kuppuswamy MK, Venugopal B, Krishnan E. Retrohepatic caval leiomyosarcoma antesitum resection: A case report and a review of literature. J Clin Exp Hepatol. 2021; 11:742-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Webb EM, Wang ZJ, Westphalen AC, Nakakura EK, Coakley FV, Yeh BM. Can CT features differentiate between inferior vena cava leiomyosarcomas and primary retroperitoneal masses? AJR Am J Roentgenol. 2013; 200:205-209. [DOI] [PubMed] [Google Scholar]
- 8. Bednarova I, Frellesen C, Roman A, Vogl TJ. Case 257: Leiomyosarcoma of the inferior vena cava. Radiology. 2018; 288:901-908. [DOI] [PubMed] [Google Scholar]


