Abstract
Introduction
Self‐expanding Y‐metal stents (SEMS) are best suited lesions with involvement of the carina and proximal main bronchi; however, Y‐stents can be difficult to place. These difficulties guided us to develop a modification of the classic technique that addresses some of the challenges during positioning. We present the Y reverse technique for Y stent insertion using a combination of rigid and flexible bronchoscopy.
Materials and Methods
This retrospective study included 15 consecutive patients, suffering from tracheal‐carina‐lower main bronchi complex, hospitalized at the Thoracic Surgery Unit of the Vanvitelli University of Naples between October 2021 and October 2023. Inclusion criteria: patients in which the length of the stenosis of the right bronchi was greater than that of the left bronchi, advanced oncological conditions, severe respiratory failure; exclusion criteria: Karnofsky scale with <40 points. All patients were admitted to the hospital and treated with Y‐stent insertion using the modified technique Y reverse.
Results
The comparison between the group undergoing the Y reverse technique with the group undergoing the traditional positioning of the Y prosthesis has shown an improvement in respiratory function; prolongation of the mean survival time; improvement in SpO2 in spontaneous breathing; reduction mean time procedure. p < 0.05 was considered as statistically significant.
Conclusion
Y Reverse is a safe and effective procedure that provides rapid symptom relief in individuals who have critical central airway obstruction near the distal portion of the trachea, carina, and main right and left bronchi.
Keywords: airway obstruction, flexible bronchoscopy, mediastinal tumors, rigid bronchoscopy, Y‐metal stents (SEMS)
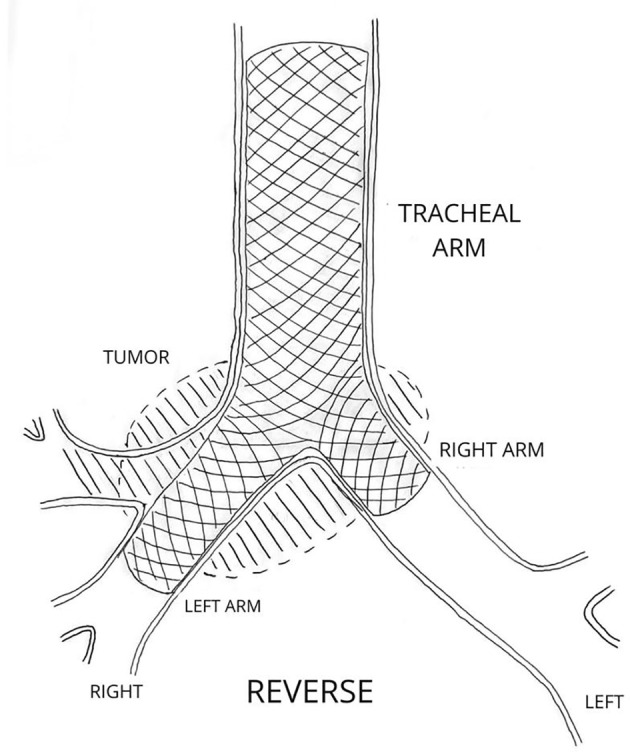
The inversion of the Y‐protesis limbs allowed the longest stenotic tract on the right to be covered with the left branch.
INTRODUCTION
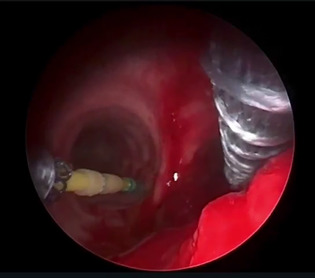
Extrinsic compression and endoluminal airway obstruction are usually caused by malignant processes: esophageal cancer, local primary lung cancer, and other mediastinal tumors. 1 Distal tracheal obstruction with involvement of the carina and proximal main bronchi is an extremely challenging problem 2 (Figure 1). It is frequently a life‐threatening condition, so prompt treatment is required. 3 Self‐expanding Y‐metal stents (SEMS) are best suited for these lesions; they can ensure an improvement in symptoms and quality of life, restoring luminal patency in central airway obstruction (CAO) and immediately relieving severe respiratory failure. 4 , 5 , 6 Y‐stents, while effective, can be difficult to place due to the inability to visualize the airway, loss of the airway, inability to ventilate during placement, and difficulty properly positioning the stent branches. 7 , 8 , 9 These difficulties guided us to develop a modification of the classic technique that addresses some of the challenges during positioning. 10 , 11 We present the Y reverse technique for Y stent insertion using a combination of rigid and flexible bronchoscopy. 12 The Y reverse technique, thanks to the inversion of the branches, allows covering the entire section of the bronchial lumen obstructed by the neoplastic tissue, which affects the left main bronchus, the carina, the right main bronchus, and the right upper lobar bronchus, allowing recanalization of the right lower lobar bronchus and the left main bronchus.
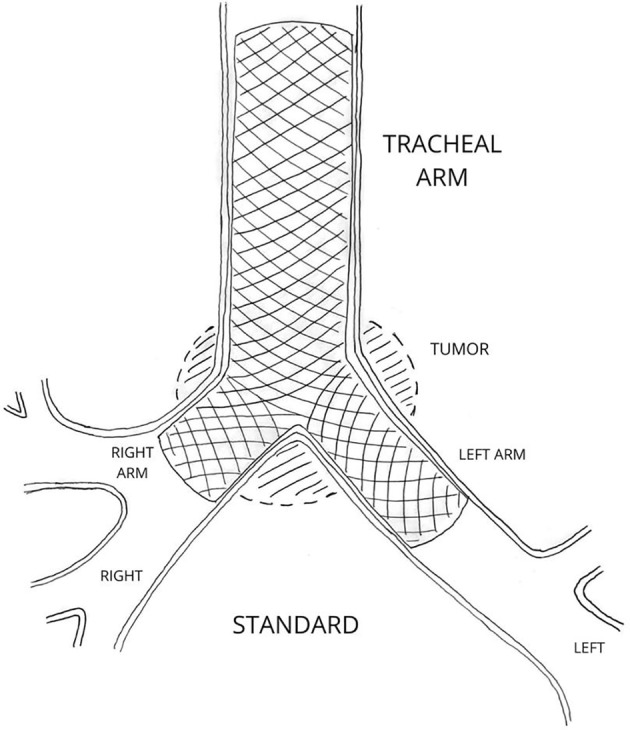
FIGURE 1.
Distal tracheal obstruction with involvement of the carina and proximal main bronchi.
MATERIALS AND METHODS
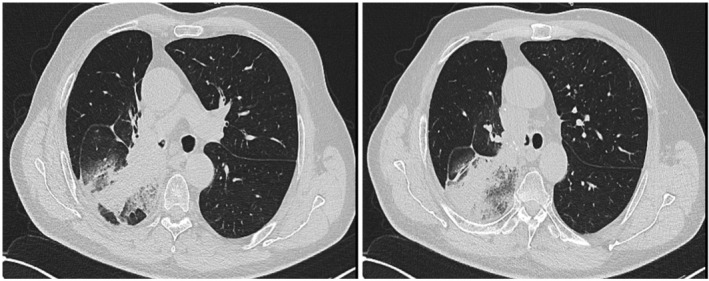
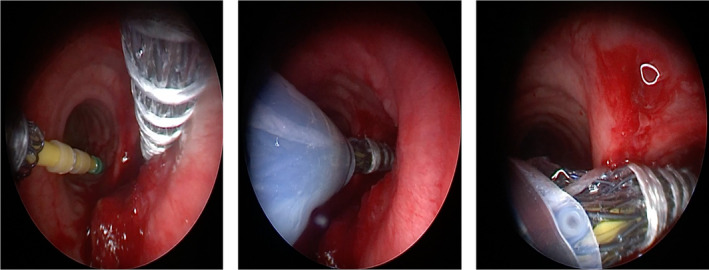
This retrospective study included 15 consecutive patients suffering from tracheal‐carinal‐lower main bronchi complex. All patients were admitted to the hospital and treated with Y‐stent insertion using the modified technique performed at the Thoracic Surgery Unit of the Vanvitelli University of Naples between October 2021 and October 2023. Written informed consent was signed by all the patients. Inclusion criteria: patients in which the length of the stenosis of the right bronchi was greater than that of the left bronchi, advanced oncological conditions, severe respiratory failure; exclusion criteria: Karnofsky scale <40 points. We have a modified technique for positioning without Seldinger‐type guideless tracheobronchial Y‐stents on a flexible bronchoscope for Y‐stent insertion. 13 , 14 The size and type of stents were chosen based on the results of chest CT 15 and three‐dimensional reconstruction of the airways. 16 , 17 , 18 A Y stent consists of a proximal limb located on the trachea and two distal limbs that extend into the two main bronchi, with the bifurcation positioned on the carina. 19 , 20 Stents Y are a self‐expanding nitinol mesh stent with an optional silicone coating and a dedicated loading device (the delivery catheter, 8 mm in diameter and 600 mm in length). The stent body had a length of 30–40 mm and a diameter of 18–24 mm; the bronchial branches were 11–14 mm in diameter for the right bronchus and 10–30 mm long for the left bronchus. 21 , 22 The procedure was performed by a team of thoracic surgeons and nurses experienced in rigid bronchoscopy. General anesthesia was used for rigid bronchoscopy. 23 , 24 First of all, the trachea was intubated with a rigid bronchoscope with an internal diameter of 14 mm; the large diameter working channel allows for controlled and safe passage of the Y Stent Delivery System while maintaining airway control. The site of the stenosis was visually localized with the flexible bronchoscope, always measuring the length of the stenotic area affected by disease of the left and right main bronchi and the trachea. 25 , 26 Through preventive evaluation with a flexible bronchoscope, it is possible to establish the stent release site more accurately. 13 , 27 The first phase of the procedure began with an assessment of the airways and was followed by the treatment of the endoluminal disease with the following techniques: mechanical debulking, using rigid bronchoscopes of progressively increased diameter, n. 6.5, 7.5, and 8.5, laser ablation, electrocoagulation, and balloon dilation. 28 , 29 The second phase of the procedure involves placing the stent in the airways. First, we released the locking of the first launch gear to free the two distal limbs, intended for the main bronchi; we brought the two branches of the prosthesis closer, thus inserting them easily into the bronchoscope; we advanced the delivery catheter into the rigid bronchoscope together with the optic under vision, proceeding delicately along the lumen of the trachea up to approximately 2 cm from the carina, assisting the entire procedure with an aspirator to make the vision clear, near the carina; we then rotated the delivery catheter by about 180° so as to insert the longest branch on the right and the shortest one on the left 30 , 31 (Figures 2 and 3). The delivery system is slowly rotated left and right, then the bifurcation of the two branches is positioned on the carina, anchoring it firmly, maneuvering the stent branches into the correct position. The stent was then gently pushed with a push rod while simultaneously retracting the rigid barrel of the bronchoscope until the entire stent was deployed 32 , 33 (Figure 4). Correct stent placement was confirmed by flexible bronchoscopy. If necessary, the stent was gently manipulated with stiff forceps. The flexible bronchoscope is passed consecutively through the rigid bronchoscope, exploring the tracheal branch of the stent and the two right and left bronchial branches of the stent. 34 Difficulties in passing the flexible endoscope through the deformed stent edges can be expected; however, in all our cases, we were able to pass a 5‐ to 6‐mm flexible bronchoscope through the bronchial limb. The flexible bronchoscope therefore allows you to check the position, help with orientation, and guide the progression of the stent branches. 35 , 36 Ideally, the length of the stent should be minimized by covering the entire stenotic region and the shape of the stent should be chosen to fit the anatomical structure of the airway 37 , 38 (Figure 5). The length of the limbs should be long enough to cover the lesion and be as short as possible to reduce the possibility of obstruction of the stent by secretions. There were no complications during procedure; however, only one patient exhibited a momentary drop in SpO2 to 61% during distal stent expansion due to obstruction in the right main bronchus, but it recovered soon after the removal of the obstruction. Follow‐up was performed with serial flexible bronchoscopies and high‐resolution computed tomography.
FIGURE 2.
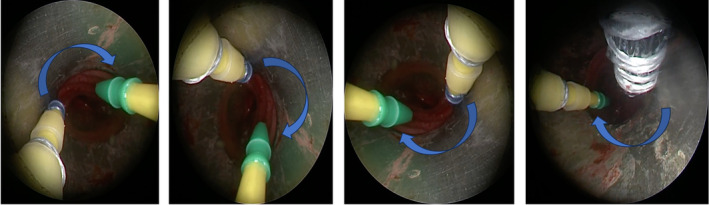
Advancement the delivery catheter into the rigid bronchoscope together with the optic under vision, until 2 cm from the carina, rotating the delivery catheter by about 180° so as to insert the longest branch on the right and the shortest one on the left.
FIGURE 3.
The delivery system is slowly rotated left and right, then the bifurcation of the two branches is positioned on the carina, maneuvering the stent branches into the correct position.
FIGURE 4.
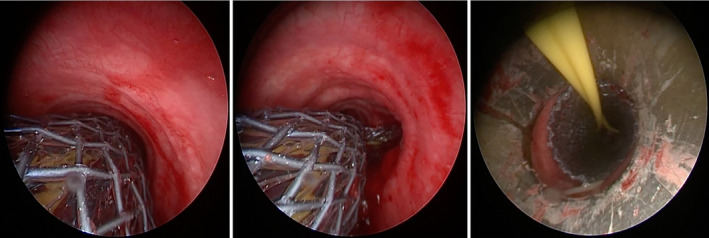
The bifurcation of the two branches is positioned on the carina, anchoring it firmly.
FIGURE 5.
The inversion of the limbs allowed the longest stenotic tract on the right to be covered with the left branch.
Statistical analysis
The group of patients undergoing the reverse metal Y stent (SEMS) technique (Table 1) was compared with the group of patients undergoing the conventional metal Y stent (SEMS) technique (Table 2). The analysis concerned an improvement in respiratory function (50.4 vs. 68.3; p = 0.012); an improvement of SpO2 in spontaneous breathing (0.94 vs. 0.78; p = 0.013); reduction in mean time procedure (26 min [21 ± 31 min] or 0.43 vs. 55 min or 0.92; p = 0.01); a reduction in CO2 (0.41 vs. 0.37; p = 0.004); an improvement in P/F (2 vs. 3; p = 0.02); a reduction in heart rate (0.91 vs. 0.83; p = 0.003); a reduction in respiratory rate (0.18 vs. 0.13; p = 0.001); and extension of the mean survival time (68.1 days [0.40 vs. 0.32; p = 0.008]). p < 0.05 was considered statistically significant (Figure 6).
TABLE 1.
Characteristics of patients undergoing Y reverse endoscopie treatment.
| Y‐metal stents [SEMS] reverse technique | |
|---|---|
| Total number of subjects | 15 |
| Rate of succes of Y‐metal stent [SEMS] placement with reverse technique a | 14 [93%] |
| Average age of subjects | 65 [35 + 71] |
| Data extraction period | Oct 2019–Sep 2023 [48 months] |
| Average follow‐up | 6 months [2 ± 14 months] |
| Signs and symptoms | |
| Dyspnea and stridor | 15 [100%] |
| Cough | 15 [100%] |
| Hemopthysis | 11 [73%] |
| Infections | 4 [27%] |
| Other (weightloss, asthenia) | 8 [53%] |
| Obstructive primary oncological disease | |
| Lung cancer (and/or metastases) | 8 [53%] |
| Esophageal cancer | 2 [13%] |
| Mediastinal lymphadenopathy | 5 [33%] |
| Degree of airway obstruction and impairment of respiratoryfunction b | |
| 0—airway stenosis <30%, without dyspnea | 0 |
| 1—airway stenosis 30%–50%, dyspnea during walking | 0 |
| 2—airway stenosis 50%–70%, dyspnea after several minutes of walking | 4 [27%] |
| 3—subtotal airway stenosis >70%, dyspnea at rest | 11 [73%] |
| Site and extension of obstruction | |
| Right [R] main bronchus | 9 [60%]—[14 ± 22 mm] |
| Left [L] main bronchus | 6 [40%]—[11 ± 18 mm] |
| Extraoperative complications | |
| Stent obstructions by secretions | 13 [87 %] |
| Granulation tissue formation | 9 [60%] |
| Case of stent loss | 0 |
Abbreviation: SEMS, self‐expanding Y‐metal stents.
Only one subject had procedure‐related complications that included dental trauma.
Patients with <40 points were excluded from the study according to Karnofsky scale.
TABLE 2.
Characteristics of patients undergoing conventional Y‐prosthesis placement.
| Y‐metal stents [SEMS] conventional technique | |
|---|---|
| Total number of subjects | 20 |
| Rate of succes of Y‐metal stent [SEMS] placement with reverse technique | 20 [100%] |
| Data extraction period | Oct 2019–Dec 2023 [50 months] |
| Signs and symptoms | |
| Dyspnea and stridor | 18 [90%] |
| Cough | 11 [55%] |
| Hemopthysis | 7 [35%] |
| Other (weightloss, asthenia) | 19 [95%] |
| Site of obstruction | |
| Right [R] main bronchus | 15 [75%] |
| Left [L] main bronchus | 5 [25%] |
Abbreviation: SEMS, self‐expanding Y‐metal stents.
FIGURE 6.
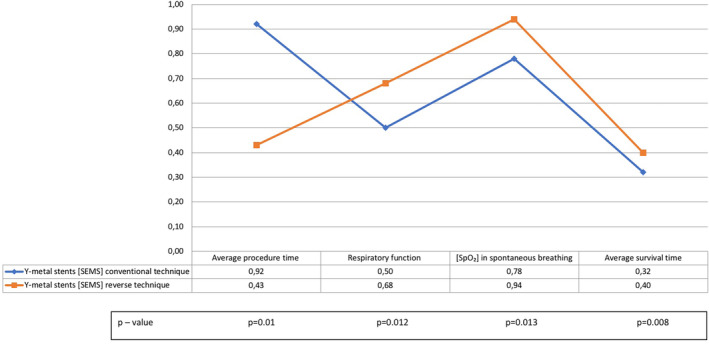
Statistical analysis.
RESULTS
The present study was designed as a single‐center retrospective study in which 15 patients underwent Y reverse procedures between October 2021 and October 2023. The average age of the patients was 65 years; the youngest patient was 35 years old and the oldest patient was 78 years old. There were six female patients and nine male patients. The most frequent symptoms were dyspnea and stridor in all patients (100%); cough in 15 (100%), hemoptysis in 11 (73%), infection in 4 (27%), and other symptoms (weightloss, asthenia) in 8 cases (53%). The obstruction was caused by intraluminal injury or external compression. Neoplasia, primary or metastatic lung, was the most frequent malignant diagnosis in eight patients (53%), followed by patients with esophageal cancer in two patients (13%) and mediastinal lymphadenopathy in five patients (33%). The degree of airway obstruction and impairment of respiratory function was assessed using a scale: 0—airway stenosis <30%, without dyspnea (0 patients); 1—airway stenosis 30%–50%, dyspnea during walking (0 patients); 2—airway stenosis 50%–70%, dyspnea after several minutes of walking (4 patients); 3—subtotal airway stenosis >70%, dyspnea at rest (11 patients). The patients' conditions before and after stent implantation were evaluated according to the Karnofsky scale. Patients with <40 points were excluded from the study. The diagnosis of airway stenosis was established by patient history, thoracic multislice spiral computed tomography, and three‐dimensional airway reconstruction. Flexible and rigid bronchoscopy was performed in all patients. All procedures were performed under general anesthesia.
The site of obstruction was located at the lower end of the trachea and carina in all subjects, involving the origin of the left main bronchus in six patients (40%), of the right main bronchus in nine patients (60%), upper right bronchus in all patients (100%). The extent of the stenosis was longer on the right (14 ± 22 mm) than on the left (11 ± 18 mm) in all patients.
In five subjects, both main bronchi were involved in malignant infiltration, which caused a luminal obstruction of approximately 80%–90% on the right and 60%–70% on the left. The degree of airway obstruction was Grades 3–4 in 13 of the 15 (86.6%) subjects with CAO. Stent dimensions were 15 × 14 × 13 mm in nine patients (60%) and 18 × 12 × 12 mm in six patients (40%). Thirteen subjects (87%) were extubated on the operating table, while two subjects (13%) required endotracheal intubation after the procedure for a mean duration of 11 h. During stent placement, SpO2 was above 91% in 11 patients but approximately 86% in 3 patients. Only one patient experienced a momentary drop in SpO2 to 61% during distal stent expansion due to obstruction in the right mainstem bronchus, but it recovered soon after the removal of the obstruction. The duration of the procedure from intubation to end was 21–29 min (), while the stent placement procedure to full deployment takes 6–9 min (). The most commonly used stent was the Y‐stent with an 11‐ to 15‐mm tracheal limb. Successful deployment of SEMYS with the above‐described technique was carried out in 14 patients (93%). Only one subject had procedure‐related complications that included dental trauma. Thirteen (87%) subjects experienced symptom relief after the procedure, and there was rapid resolution of respiratory failure after stent placement. In only one case was the stent removed immediately after insertion due to severe respiratory failure due to failure of the stent to re‐expand. All patients remained hospitalized for at least 24 h after the procedure (mean length of stay, 1 day; range, 1–2). Follow‐up bronchoscopic inspection 1 week after the procedure revealed the stents in place and no signs of migration. All patients stated that their clinical symptoms had improved significantly after surgery. The average follow‐up was 6 months (2 ± 14 months); two patients were followed up for 21 months (15 ± 28 months). The most frequent late complication was stent obstruction with secretions (13 patients, 87%), which was managed with bronchoscopic toileting. Granulation tissue formation at both ends of the stent was another common complication encountered during follow‐up in nine patients (60%). No case of stent loss was found. Five patients died during the follow‐up within 4 weeks of the procedure (33%). Two patients were lost to follow‐up (13%). Neoplastic progression was the most common cause of death during follow‐up. We compared the group of patients undergoing endoscopic Y reverse treatment with a second group of 20 patients undergoing conventional Y‐prosthesis placement (Figures 7 and 8). Patients in the second group had endoluminal obstruction localized at the lower end of the trachea and keel in all subjects, involving the origin of the left main bronchus (5 patients; 25%), of the right main bronchus (15 patients; 75%); they were referred to the Thoracic Surgery Unit of the Luigi Vanvitelli University of Naples between October 2021 and December 2023. The eligibility criteria for the referral of patients with the length of the stenosis of the right bronchi was greater than that of the left bronchi, advanced oncological conditions, severe respiratory failure; exclusion criteria: Karnofsky scale <40 points. The most common signs and symptoms were: dyspnea in 18 cases (90%), cough in 11 cases (55%), hemoptysis in 7 cases (35%), and other symptoms (weightloss, asthenia) in 19 cases (95%). There were no deaths on the operating table. In all these patients, we positioned the Y‐prosthesis in a conventional manner. The analysis between the two groups highlighted an improvement in respiratory function, improvement of SpO2 in spontaneous breathing, and procedure for reducing the average time in the group of patients undergoing Y reverse endoscopic treatment. p < 0.05 was considered statistically significant.
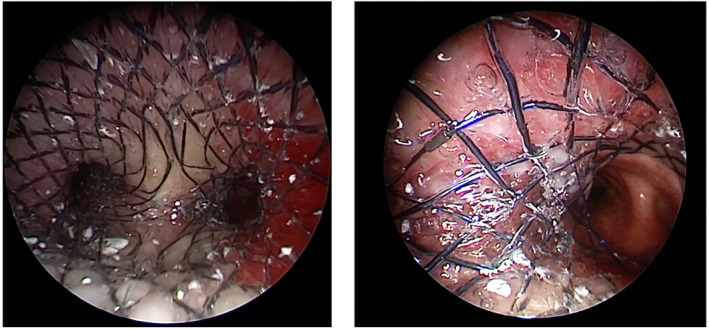
FIGURE 7.
Conventional Y‐prosthesis placement.
FIGURE 8.
Y Reverse placement.
DISCUSSION
Stent placement is necessary to restore airway patency after procedures such as laser photocoagulation, dilatation, electrocoagulation, and mechanical debridement, used for the treatment of endoluminal bronchial obstruction and in the treatment of airway stenosis from external compression. 39 , 40 These techniques restore ventilation and relieve symptoms. 41 Insertion of a Y stent provides relief from dyspnea and provides improved quality of life for patients with CAO involving the carina, distal trachea, and proximal main bronchi. 42 , 43 Several techniques for the placement of Y‐stents have been described. The “push” or “pullback” technique uses alligator clips to compress the bifurcation of the stent. With the “pullback” technique, both bronchial branches of the stent are placed in one of the main bronchi and the stent is pulled until the shorter branch into place in the contralateral bronchus. 44 Nowadays, the techniques used require distal advancement of the Y‐shaped stent into the trachea and main bronchi without direct vision of the airways. Therefore, blind advancement of the stent increases the risk of perforation of the membranous part of the trachea and injury to the tracheal wall or bronchia. 45 , 46 The greater number of patients requiring Y‐stent placement have very limited tolerance to hypoxia and poor respiratory reserve, thus increasing the risk of the procedure during the apnea time required for Y‐stent placement. 47 Therefore, timely stent placement and adequate ventilation are of utmost importance. 48 However, if major repositioning is necessary, the stent must be removed and a new stent used; the length and circumference of the stent cannot be adapted to patients; however, several stent sizes are available. The rigid tracheoscope (bronchoscope) after stent placement in the proximal trachea allows for rapid return of ventilation, and thus apnea time is minimized. The advantage of our procedure is that it allows you to view every moment in real time; thanks to the constant use of optics, it is possible to have a clear vision of each step of the positioning of the prosthesis. Adequate ventilation is ensured throughout the procedure. 49 Therefore, the procedural time using the modified technique was 37% shorter than the procedural time with the conventional technique, which compared with the procedure time reported by Oki and Saka. 50 In their case series, they described an average procedure time of 55 min for the conventional Y‐stent technique. Y Reverse by means of the 180° rotation of the branches of the prosthesis allows the inversion of the positioning of the longest branch on the right and the shortest on the left, thus covering the longest stenotic section ensures, saturation above 92% and reducing the onset of severe respiratory failure. 51 Therefore, this technique is safe, convenient, and easy to master. We did not use fluoroscopic guidance for the positioning of the stents, avoiding exposure to radiation of the patient and the personnel involved, but we ensured the correct positioning of the stent with direct visualization of the flexible bronchoscope during positioning. We preferred SEMS over silicone stents in cases where the obstruction turns out to be extraluminal; therefore, the external pressure cannot be relieved by silicone stents, and metallic stents with their better radial strength are preferred. The use of SEMS is preferred when bronchoscopic maneuvers cannot be possible and when the airway obstruction appears to be irregular. Metallic stents play an important role due to their thinner wall thickness and their ability to wrap the internal airway. However, while silicone stents can be customized on‐site during the procedure by changing their length, the length of a metal stent cannot be changed, while it is also possible to customize the lumen diameter of the metal stent more widely, which is not possible with a silicone stent. Given the different structures of silicone and metal stents, different complication rates occur. In cases of Y‐shaped silicone stents, the most common complications were mucostasis and granulation tissue. In cases of SEMS, the most common complications were granulation tissue formation, mucostasis, and minimal stent fractures. The positioning of the stent with the Y reverse technique ensured an improvement in respiratory failure immediately after the procedure. 52 The upper lobar bronchus in all patients is the site of neoplasms; therefore, it was only possible to recanalize the lower lobar bronchus, the inversion of the branches, which allows to ensure the patency of a longer section of the right bronchus, excluding the bronchus upper lobar, thus ensuring the recanalization of the lower lobar bronchus. However, the present study is limited by its single‐center nature and small sample size. Furthermore, the metal stent has some limitations, being difficult to remove and reposition after epithelialization, which usually occurs at around 8 weeks. Furthermore, the metal stent can become damaged and the broken filaments can damage the mucosa. Therefore, they are mainly indicated in conditions where patient survival is limited, such as in advanced cancer patients. During stent placement, the patient cannot be ventilated, the stent cannot be repositioned once inserted, although it can be gently moved for gentle repositioning. However, if major repositioning is necessary, the stent must be removed and a new stent used; the length of the stent cannot be adapted to patients; however, several stent sizes are available.
CONCLUSIONS
Y Reverse is a valuable tool in the palliative treatment of patients with CAO. Tracheobronchial stent implementation and maintenance practices vary widely around the world. The use of Y Reverse and its widespread use depends on the skills of the professional who places it. The engineering, design, and innovations of the Y Reverse in its implementation are an ever‐evolving process. Y Reverse is a safe procedure for improving quality of life, reducing CO2, improvement in respiratory and heart rate, increasing P/F, improvement in saturation; prolonging survival, and providing rapid symptom relief in individuals who have critical central airway obstruction near the distal portion of the trachea, carina, and main right and left bronchi. However, further studies are needed to corroborate our studies.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Supporting information
Video S1. Y Reverse placement, a demo video.
ACKNOWLEDGMENTS
This study was funded by the University of Campania “L. Vanvitelli.” Open access publishing facilitated by Universita degli Studi della Campania Luigi Vanvitelli, as part of the Wiley ‐ CRUI‐CARE agreement.
Messina G, Natale G, Pica DG, Vicario G, Giorgiano NM, Mirra R, et al. Y Reverse: Modified technique in challenging airway management. Thorac Cancer. 2024;15(34):2428–2436. 10.1111/1759-7714.15440
DATA AVAILABILITY STATEMENT
The authors confirm that all relevant data are included in the article and/or its Supporting Information files.
REFERENCES
- 1. Dutau H, Dumon JF. Airway stenting revisited: 30 years, the age of reason? J Bronchology Interv Pulmonol. 2017;24:257–259. [DOI] [PubMed] [Google Scholar]
- 2. Dutau H, Breen D, Bugalho A, Dalar L, Daniels J, Dooms C, et al. Current practice of airway stenting in the adult population in Europe: a survey of the European Association of Bronchology and Interventional Pulmonology (EABIP). Respiration. 2018;95:44–54. [DOI] [PubMed] [Google Scholar]
- 3. Facciolongo N, Piro R, Menzella F, Lusuardi M, Salio M, Agli LL, et al. Training and practice in bronchoscopy a national survey in Italy. Monaldi Arch Chest Dis. 2013;79:128–133. [DOI] [PubMed] [Google Scholar]
- 4. Sethi S, Gildea TR, Almeida FA, Cicenia JC, Machuzak MS. Clinical success stenting distal bronchi for “lobar salvage” in bronchial stenosis. J Bronchology Interv Pulmonol. 2018;25:9–16. [DOI] [PubMed] [Google Scholar]
- 5. Fruchter O, Abed El Raouf B, Rosengarten D, Kramer MR. Long‐term outcome of short metallic stents for lobar airway stenosis. J Bronchology Interv Pulmonol. 2017;24:211–215. [DOI] [PubMed] [Google Scholar]
- 6. Chung FT, Chen HC, Chou CL, Yu CT, Kuo CH, Kuo HP, et al. An outcome analysis of self‐expandable metallic stents in central airway obstruction: a cohort study. J Cardiothorac Surg. 2011;6:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Breen DP, Dutau H. On‐site customization of silicone stents: towards optimal palliation of complex airway conditions. Respiration. 2009;77:447–453. [DOI] [PubMed] [Google Scholar]
- 8. Kumar A, Inaty H, Kalanjeri S, Gildea T. Silicone stent customization for complex airway disorders—a single center experience. Chest. 2015;148:847A. [Google Scholar]
- 9. Sehgal IS, Dhooria S, Madan K, Pattabhiraman V, Mehta R, Goyal R, et al. Placement of tracheobronchial silicone Y‐stents: multicenter experience and systematic review of the literature. Lung India. 2017;34(4):311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Miyazawa T, Miyazu Y, Iwamoto Y, Ishida A, Kanoh K, Sumiyoshi H, et al. Stenting at the flow‐limiting segment in tracheobronchial stenosis due to lung cancer. Am J Respir Crit Care Med. 2004;169:1096–1102. [DOI] [PubMed] [Google Scholar]
- 11. Dutau H, Maldonado F, Laroumagne S, Astoul P. Silicone stents, the rigid bronchoscope, and the standard of care in central airway stenosis. Curr Respir Care Rep. 2012;1:46–53. [Google Scholar]
- 12. Begnaud A, Connett JE, Harwood EM, Jantz MA, Mehta HJ. Measuring central airway obstruction. What do bronchoscopists do? Ann Am Thorac Soc. 2015;12:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Herth F, Becker HD, LoCicero J 3rd, Thurer R, Ernst A. Successful bronchoscopic placement of tracheobronchial stents without fluoroscopy. Chest. 2001;119:1910–1912. [DOI] [PubMed] [Google Scholar]
- 14. Hayashi A, Takanashi S, Tsushima T, Denpoya J, Okumura K, Hirota K. New method for quantitative assessment of airway calibre using a stereovision fiberoptic bronchoscope. Br J Anaesth. 2012;108:512–516. [DOI] [PubMed] [Google Scholar]
- 15. Nobuyama S, Sato T, Handa H, Nishine H, Inoue T, Mineshita M, et al. Comparison of airway measurements for tracheobronchial stenosis between stereoscopic bronchoscope and MD‐CT. J Bronchology Interv Pulmonol. 2017;24:296–302. [DOI] [PubMed] [Google Scholar]
- 16. Young BP, Machuzak MS, Gildea RT. Initial clinical experience using 3D printing and patient‐specific airway stents: compassionate use of 3D printed patient‐specific airway stents. Am J Respir Crit Care Med. 2020;201:A1711. [Google Scholar]
- 17. Guibert N, Didier A, Moreno B, Mhanna L, Brouchet L, Plat G, et al. Treatment of post‐transplant complex airway stenosis with a three‐dimensional, computer‐assisted customized airway stent. Am J Respir Crit Care Med. 2017;195:e31–e33. [DOI] [PubMed] [Google Scholar]
- 18. Cheng GZ, Folch E, Wilson A, Brik R, Garcia N, Estepar RSJ, et al. 3D printing and personalized airway stents. Pulm Ther. 2017;3:59–66. [Google Scholar]
- 19. Folch E, Keyes C. Airway stents. Ann Cardiothorac Surg. 2018;7:273–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ayub A, Al‐Ayoubi AM, Bhora FY. Stents for airway strictures: selection and results. J Thorac Dis. 2017;9:S116–S121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Freitag L, Gördes M, Zarogoulidis P, Darwiche K, Franzen D, Funke F, et al. Towards individualized tracheobronchial stents: technical, practical and legal considerations. Respiration. 2017;94:442–456. [DOI] [PubMed] [Google Scholar]
- 22. Profili S, Manca A, Feo CF, Padua G, Ortu R, Canalis GC, et al. Palliative airway stenting performed under radiological guidance and local anesthesia. Cardiovasc Intervent Radiol. 2007;30(1):74–78. [DOI] [PubMed] [Google Scholar]
- 23. Madan K, Agarwal R, Aggarwal AN, Gupta D. Therapeutic rigid bronchoscopy at a tertiary care center in North India: initial experience and systematic review of Indian literature. Lung India. 2014;31:9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jones C, Crerar‐Gilbert AJ, Madden BP. Anaesthesia for endobronchial intervention and tracheobronchial stents. Curr Anaesth Crit Care. 2009;20:160–163. [Google Scholar]
- 25. Wei N, Fu YF, Zhang K, Wan HG, Xu H. Ventilation catheter‐assisted airway stenting under local anaesthesia for patients with airway stenosis: initial clinical experience. Radiol Med. 2015;120:338–344. [DOI] [PubMed] [Google Scholar]
- 26. Du Rand IA, Blaikley J, Booton R, Chaudhuri N, Gupta V, Khalid S, et al. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax. 2013;68(Suppl 1):1–44. [DOI] [PubMed] [Google Scholar]
- 27. Murgu S, Stoy S. The when, the how and the why of metallic stent removal. J Bronchology Interv Pulmonol. 2016;23:266–271. [DOI] [PubMed] [Google Scholar]
- 28. Innabi A, Mcclelland S, Raman T, Alzghoul B, Meena N. No stent left behind: a review of stent removal and related complications. EMJ Respir. 2017;5:78–84. [Google Scholar]
- 29. Cao M, Zhu Q, Wang W, Zhang TX, Jiang MZ, Zang Q. Clinical application of fully covered self‐expandable meta stents in the treatment of bronchial fistula. Thorac Cardiovasc Surg. 2016;64(6):533–539. [DOI] [PubMed] [Google Scholar]
- 30. Conforti S, Durkovic S, Rinaldo A, Gagliardone MP, Montorsi E, Torre M. Self‐expanding Y stent for the treatment of malignant tracheobronchial stenosis. Retrospective study. Arch Bronconeumol. 2016;52(11):e5–e7. [DOI] [PubMed] [Google Scholar]
- 31. Fang Y, Li T, Han X, Wu G, Ren J, Ren K, et al. The application of Y‐shaped selfexpandable covered metal stents in the thoracostomachairway fistula: a single center, 11 years experience. Zhonghua Jie He He Hu Xi Za Zhi. 2015;38(8):562–565. [PubMed] [Google Scholar]
- 32. Qiao Y, Fu Y‐F, Cheng L, Niu S, Cao C. Placement of integrated self‐expanding Y‐shaped airway stent in management of carinal stenosis. Radiol Med. 2016;121(9):744–750. [DOI] [PubMed] [Google Scholar]
- 33. Li T‐F, Duan X‐H, Han X‐W, Wu G, Ren JZ, Ren KW, et al. Application of combined‐type Y‐shaped covered metallic stents for the treatment of gastrotracheal fistulas and gastrobronchial fistulas. J Thorac Cardiovasc Surg. 2016;152(2):557–563. [DOI] [PubMed] [Google Scholar]
- 34. McGrath EE, Warriner D, Anderson P. The insertion of self expanding metal stents with flexible bronchoscopy under sedation for malignant tracheobronchial stenosis: a singlecenter retrospective analysis. Arch Bronconeumol. 2012;48(2):43–48. [DOI] [PubMed] [Google Scholar]
- 35. Hochheimer CJ, Sabo RT, Krist AH, Day T, Cyrus J, Woolf SH. Methods for evaluating respondent attrition in web‐based surveys. J Med Internet Res. 2016;18:e301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Debourdeau A, Gonzalez J‐M, Dutau H, Benezech A, Barthet M. Endoscopic treatment of nonmalignant tracheoesophageal and bronchoesophageal fistula: results and prognostic factors for its success. Surg Endosc. 2019;33(2):549–556. [DOI] [PubMed] [Google Scholar]
- 37. Dutau H, Musani AI, Laroumagne S, Darwiche K, Freitag L, Astoul P. BiodegradableAirway stents—bench to bedside: a comprehensive review. Respiration. 2015;90:512–521. [DOI] [PubMed] [Google Scholar]
- 38. Fuehner T, Suhling H, Greer M, Wiesner O, Dierich M, Warnecke G, et al. Biodegradable stents after lung transplantation. Transpl Int. 2013;26:e58–e60. [DOI] [PubMed] [Google Scholar]
- 39. Madan K, Dhooria S, Sehgal IS, Mohan A, Mehta R, Pattabhiraman V, et al. A multicenter experience with the placement of self‐expanding metallic tracheobronchial Y stents. J Bronchology Interv Pulmonol. 2016;23:29–38. [DOI] [PubMed] [Google Scholar]
- 40. Han XW, Wu G, Li YD, Zhang QX, Guan S, Ma N, et al. Overcoming the delivery limitation: results of an approach to implanting an integrated self‐expanding Y‐shaped metallic stent in the carina. J Vasc Interv Radiol. 2008;19:742–747. [DOI] [PubMed] [Google Scholar]
- 41. Wang H, Ke M, Li W, Wang Z, Li H, Cong M, et al. Chinese expert consensus on diagnosis and management of acquired respiratorydigestive tract fistulas. Thorac Cancer. 2018;9:1544–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fiorelli A, Poggi C, Ardò NP, Messina G, Andreetti C, Venuta F, et al. Flow‐volume curve analysis for predicting recurrence after endoscopic dilation of airway stenosis. Ann Thorac Surg. 2019;108(1):203–210. [DOI] [PubMed] [Google Scholar]
- 43. Fiorelli A, Messina G, Capaccio D, Santini M. Recurrent spontaneous pneumomediastinum: a rare but possible event! J Thorac Dis. 2012;4(4):431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kazakov J, Khereba M, Thiffault V, Duranceau A, Ferraro P, Liberman M. Modified technique for tracheobronchial Y‐stent insertion using flexible bronchoscope for stent guidance. J Thorac Cardiovasc Surg. 2015;150(4):1005–1009. [DOI] [PubMed] [Google Scholar]
- 45. Fu Y‐F, Wei N, Zhang K, Xu H. Subcarinal ventilation‐assisted Y‐shaped stent insertion under local anesthesia for patients with complex tracheobronchial stenosis: initial clinical experience. Diagn Interv Radiol. 2014;20:330–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cozzolino I, Ronchi A, Messina G, Montella M, Morgillo F, Vicidomini G, et al. Adequacy of cytologic samples by ultrasound‐guided percutaneous transthoracic fine‐needle aspiration cytology of peripheral pulmonary nodules for morphologic diagnosis and molecular evaluations: comparison with computed tomography–guided percutaneous transthoracic fine‐needle aspiration cytology. Arch Pathol Lab Med. 2020;144(3):361–369. [DOI] [PubMed] [Google Scholar]
- 47. Guo S, Liu X, Li Y, Xiao Y, Xiao M, Jin X. Use of a modified endotracheal tube for self‐expandable metallic Y‐shaped airway stent deployment without rigid bronchoscope or fluoroscopic guidance. J Thorac Dis. 2019;11(9):3846–3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Özdemir C, Sökücü SN, Karasulu L, Önür ST, Dalar L. Placement of self‐expandable bifurcated metallic stents without use of fluoroscopic and guidewire guidance to palliate central airway lesions. Multidiscip Respir Med. 2016;11:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Monnier Y, Chollet‐Rivier M, Gonzalez M, Nicod L, Simon C, Lovis A. Use of combined suspension laryngoscopy and jet ventilation for Y‐shaped airway stents delivery. Ann Thorac Surg. 2014;97:2208–2210. [DOI] [PubMed] [Google Scholar]
- 50. Oki M, Saka H. Silicone Y‐stent placement on the secondary left carina. Respiration. 2015;90(6):493–498. 10.1159/000441305 [DOI] [PubMed] [Google Scholar]
- 51. Santini M, Fiorelli A, Messina G, Mazzella A, Accardo M. The feasibility of LigaSure to create intestinal anastomosis. Surg Innov. 2015;22(3):266–2736. [DOI] [PubMed] [Google Scholar]
- 52. Yang RM, Han XW, Wu G, Li YD, Li FB. Implantation of a self‐expandable metallic inverted Y‐stent to treat tracheobronchial stenosis in the carinal region: initial clinical experience. Clin Radiol. 2007;62:1223–1228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Y Reverse placement, a demo video.
Data Availability Statement
The authors confirm that all relevant data are included in the article and/or its Supporting Information files.


