Abstract
Tethered cord syndrome is a rare form of spinal dysraphism. We present the case of a 24-year-old female patient who was admitted with chronic urinary symptoms, including dysuria and pollakiuria, which had persisted since puberty, along with lower back pain (lumbago). Due to the progression and increased severity of the lumbago, a lumbar MRI was performed. The imaging revealed a low-lying conus medullaris at the S1-S2 spinal level, tethered to a sacral spinal canal lipoma, without any signal abnormalities in the spinal cord. This led to the diagnosis of closed spinal dysraphism. The key takeaway from this case is the importance of raising awareness among clinicians and radiologists to consider tethered cord syndrome as a potential cause of urinary symptoms in young adults.
Keywords: Tethered spinal cord, Spinal dysraphism, Sacral spinal canal lipoma, MRI, Case report
Introduction
Spinal dysraphisms encompass a broad group of malformations that affect the spine and/or adjacent structures in the embryonic dorsum. They are considered a form of neural tube defect [1]. The overall prevalence of spinal dysraphism varies across populations, but it is generally around 1 in 1000 pregnancies. The birth prevalence is lower, primarily due to regional and cultural differences in termination rates [2].
The purpose of this case report is to emphasize this rare malformation, particularly in terms of its imaging characteristics.
Case presentation
A 24-year-old female patient, with no significant past medical or surgical history, was admitted for chronic urinary disorders that had been evolving since puberty. She presented with dysuria and pollakiuria, accompanied by persistent lower back pain (lumbago) that had gradually intensified over the past year.
The patient's family history was unremarkable, with no known hereditary diseases or relevant neurological disorders reported. Upon admission, she described her urinary symptoms as bothersome, with increased frequency of urination and occasional episodes of incontinence. The lower back pain was characterized as dull and persistent, without radiation to the lower extremities.
A thorough clinical examination revealed normal findings, and a biological assessment, including a complete blood count and metabolic panel, showed no abnormalities. The laboratory results were as follows: White blood cell count: 7600 cells/µL (normal), Red blood cell count: 4.1 million cells/µL (normal), Hemoglobin: 12.1 g/dL (normal), Creatinine: 0.9 mg/dL (normal), Urinalysis: No signs of infection, with white blood cells at 1 cells/µL and red blood cells at 1 cells/µL.
A renovesical ultrasound was performed to assess for any structural abnormalities of the kidneys and bladder, which revealed no significant findings.
Due to the persistence of her symptoms and the increasing intensity of her lower back pain, a lumbar MRI was conducted. The MRI findings indicated a low-lying conus medullaris at the S1-S2 spinal level, tethered to a sacral spinal canal lipoma, with no signal abnormalities observed in the spinal cord (see Figs. 1 and 2). Based on these findings, the diagnosis of tethered cord syndrome was established, identifying the sacral spinal canal lipoma as the causative factor.
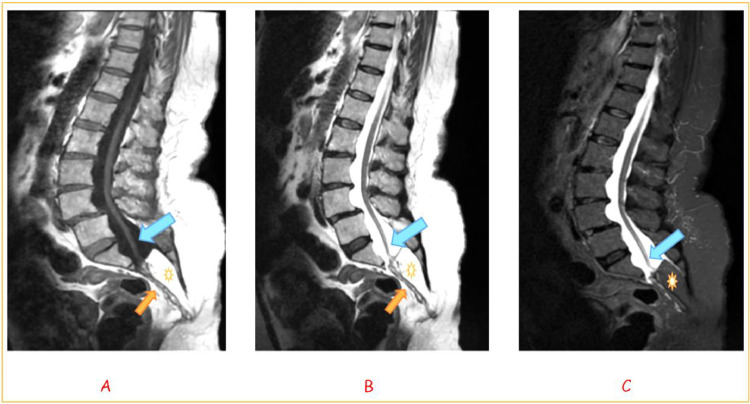
Fig. 1.
Lumbar MRI in sagittal section, displaying T1-weighted (A), T2-weighted (B), and STIR (C) sequences.
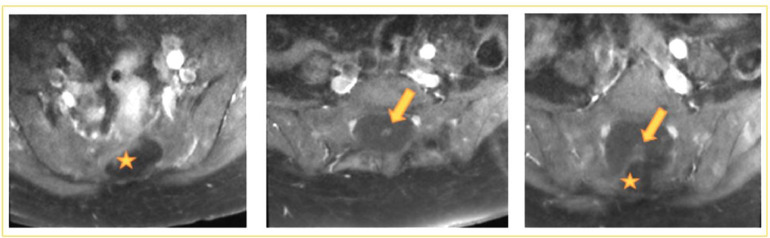
Fig. 2.
Lumbar MRI in axial section with T1-weighted gadolinium FAT-SAT sequence.
Unfortunately, the patient was lost to follow-up after the diagnosis, and no further management or outcome data are available.
-
➢
T1-weighted image: The sacral vertebrae from S2 to S5 exhibit a hypoplastic appearance (orange arrow). An intra-canal sacral mass is well-defined, displaying hyper intensity on T1-weighted imaging (star), indicative of a lipoma. This mass causes enlargement of the sacral canal and leads to cerebrospinal fluid (CSF) retention upstream, resulting in marked scalloping of the anterior vertebral bodies at the levels of L3, L4, and S1.
-
➢
T2-weighted image: The sacral lipoma demonstrates hyper intensity on T2-weighted imaging, with reduced signal intensity observed on the STIR sequence (C), further supporting the diagnosis of lipoma.
-
➢
STIR image: The terminal medullary cone appears low in position and is tethered to the sacral lipoma, with the conus medullaris located at the S1 level (blue arrow).
-
➢
Additionally, L4-L5 spondylolisthesis is noted, accompanied by bilateral isthmic lysis.
-
➢
The sacral lipoma is visualized as a hypo intense mass on the STIR sequence (star), demonstrating no contrast enhancement following gadolinium injection, consistent with a benign fatty lesion.
-
➢
Additionally, the conus medullaris is noted to be located low at the S1 level (arrow), confirming the diagnosis of tethered cord syndrome.
Discussion
Spinal dysraphism is a general term for a group of congenital defects that can cause progressive neurological damage. These defects are classified into 2 main categories: open forms, which involve cutaneous interruption or a subcutaneous mass, and closed forms (occult spinal dysraphism, OSD), which lack cutaneous openings or posterior masses [3].
Tethered cord syndrome is a complication of spinal dysraphism. It is a progressive functional disorder caused by the abnormal pathological attachment of the terminal conus of the spinal cord to the spinal column [4]. Tethered cord syndrome can be either primary (related to conditions such as a short and thickened filum terminale, an intra-canal sacral lipoma, spina bifida occulta, or diastematomyelia) or secondary (related to scarring adhesions following postnatal surgical closure of a meningocele) [5].
In our case, the cause was an intra-canal sacral lipoma.
Children and adolescents with tethered cord syndrome typically exhibit motor and sensory dysfunction, such as gait disturbances or difficulty running. Some may experience regressive changes in bowel or bladder habits. Occasionally, there may be pain in the back or lower extremities. Teenagers and adults often present with scoliosis, lower extremity deformities, pain, and sphincter dysfunction [6].
Three key syndromes associated with tethered cord syndrome can be distinguished [7]:
-
•
Neuro-orthopedic syndrome: This syndrome includes sensory, motor, and trophic deficits, with pain being the predominant symptom in adults. It often presents with muscle weakness and abnormal reflexes.
-
•
Lumbo-sacral cutaneous syndrome: Characterized by skin abnormalities such as dermal sinuses, subcutaneous swellings, or angiomas. These symptoms are absent in about 70% of adults but occur in approximately 90% of children.
-
•
Sphincter disorders: Affecting 80% of cases, these disorders involve bladder and bowel control issues, significantly impacting daily life.
The dominant manifestations in our patient were lower back pain and urinary problems. The diagnosis is primarily neuro-radiological [8].
Magnetic Resonance Imaging (MRI) is considered the superior imaging modality for assessing spinal cord lesions, including spinal dysraphism. This technique is essential for preoperative evaluation due to its excellent soft tissue contrast, which surpasses that of computed tomography (CT) scans. Unlike CT, MRI provides detailed visualization of the spinal cord and its associated structures, including the relationship between the spinal cord and any present lipomas, thus facilitating precise surgical planning [7].
MRI allows for a comprehensive and precise assessment by visualizing the position of the terminal conus medullaris, which is often found low, below L2, and determining the presence of any associated congenital anomalies, particularly intra- or extradural lipomas, along with their anatomical relationships [9].
In our case, we clearly identified an intra-canal extra medullary sacral lipoma and a terminal conus medullaris located at the level of S1. On MRI scans, lipomas typically appear hyperintense on T1-weighted images and isointense with subcutaneous fat on both T1 and T2-weighted images. The use of gadolinium contrast is unnecessary, as it does not alter the signal of the lipomas [7].
Evaluating the urological impact is part of the systematic assessment for any tethered spinal cord. Urodynamic abnormalities are found in 93% of cases, highlighting the importance of these explorations for therapeutic and prognostic purposes [8].
Treatment consists of neurosurgical release of the terminal conus medullaris via a posterior approach for symptomatic patients [8]. If left untreated, tethered cord syndrome follows a progressively worsening trajectory. Surgical release of the tethered spinal cord, when performed on carefully selected patients, has the potential to halt the progression of the syndrome and, in some cases, improve neurological function and overall patient outcomes [10].
Conclusion
Tethered cord syndrome is a rare condition, but it is crucial to consider, particularly in cases of persistent urinary symptoms that arise during puberty, as seen in our patient. Spinal MRI is the key examination for establishing a definitive diagnosis, determining the etiology, and assessing the severity of the condition.
Patient consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Footnotes
Competing Interests: All authors disclose any financial or personal relationships that may be perceived as influencing this work.
References
- 1.Radswiki T, Gaillard F, Glick Y, et al. Spinal dysraphism. Radiopaedia.org. 2011 doi: 10.53347/rID-14966. [DOI] [Google Scholar]
- 2.Mitchell L. Epidemiology of neural tube defects. Am J Med Genet Part C. 2005;135C(1):88–94. doi: 10.1002/ajmg.c.30057. [DOI] [PubMed] [Google Scholar]
- 3.Modruz N, Rivoal E. Imager les dysraphismes spinaux: quand et comment?. Presented at: Congrès SFIPP; September 9-10; Quimper, France; 2011. [Google Scholar]
- 4.Hsieh MH, Perry V, Gupta N, Pearson C, Nguyen HT. The effects of detethering on the urodynamics profile in children with a tethered cord. J Neurosurg Pediatr. 2006;105(5 suppl):391–395. doi: 10.3171/ped.2006.105.5.391. [DOI] [PubMed] [Google Scholar]
- 5.Cabraja M, Thomale U, Vajkoczy P. Spinal disorders and associated CNS anomalies: tethered cord and Arnold-Chiari malformation. Der Orthopäde. 2008;37(4):347–355. doi: 10.1007/s00132-008-1232-6. [DOI] [PubMed] [Google Scholar]
- 6.Fenton DS Tethered spinal cord . Imaging painful spine disorders. Elsevier; 2011. [DOI] [Google Scholar]
- 7.Horrion J, Houbart MA, Georgiopoulos A, Bottosso N. Adult intradural lipoma with tethered spinal cord syndrome. JBR-BTR. 2014;97:121. doi: 10.5334/jbr-btr.43. [DOI] [PubMed] [Google Scholar]
- 8.Bouchenaki F, Boustil K, Benachour S, Bakhti S. Le syndrome de la moelle attachée chez l'enfant: le filum lipomateux. J Neurochir. 2021;16(2):26–30. [Google Scholar]
- 9.Ghozlani I, El Kharras A, Badaoui M, El Maghraoui A. Syndrome de moelle bas attachée: à propos d'un cas. Rev Mar Rhum. 2015;33:38–40. [Google Scholar]
- 10.Ramina R, Aguiar PHP, Tatagiba M. ISBN 978-3-540-49249-8 Springer Berlin Heidelberg New York; 2008. Samii’s essentials in neurosurgery. [Google Scholar]