Abstract
Non-specific chronic low back pain (NSCLBP) with movement control impairment (MCI) subgroup often experiences postural pain and functional lumbar spine instability. This scoping review had two aims: 1) to map the evidence related to dynamic neuromuscular stabilization (DNS) efficacy as a spinal stabilization strategy and to identify gaps in the literature that may exist regarding the effectiveness of DNS in low back pain management and 2) to align the DNS approach as a potential intervention for MCI patients. The clinical trial studies related to DNS exercises were searched from inception until February 2024 through electronic databases, such as PubMed, Google Scholar, PEDro, and Science Direct. The Arksey and O’Malley methodology and PRISMA-ScR checklist were followed to report the findings. A total of 18 studies offering a total sample of 483, were included based on the inclusion criteria. The results of 14 studies summarized the DNS-related influence on neural substrates and core stability. The availability of only 4 studies on DNS efficacy in chronic low back pain indicates a dearth of evidence. This review highlighted the DNS efficacy in improving core muscle activation and pain-related symptoms in NSCLBP patients while emphasising the need for prospective research in the MCI subgroup.
Keywords: Breathing Exercises, Core Stability, Dynamic Neuromuscular Stabilization, Low Back Pain, Motor Activity
Introduction
Low back pain (LBP) is regarded as the most prevalent cause of years lived with disability worldwide. Nearly 90% of people with chronic low back pain (CLBP) are thought to have non-specific low back pain[1]. According to the recent GBD 2021 study, low back pain affected over half of the billion in 2020, with a projected affection of 843 million cases by 2050[2]. Hence, more focus is urgently required to lessen this growing load and its effects on the social and healthcare system.
Movement control impairment (MCI) as identified by O’Sullivan, a commonest and largest stratified subgroup of the NSCLBP population, is characterized by mechanically induced lower back pain and related psychosocial coping mechanisms[3]. MCI patients frequently experience postural pain and maladaptive movements, such as uncontrolled movement of the lumbar segments in the predominant direction of pain provocation, without any impairment in the physiological range of motion. Mechanically, the LBP of these patients has been associated with disproportionate movement contribution of associated segments of the spine, hip and legs while performing static or dynamic functional movements or tasks[3,4]. The presence of altered and repeated end-range maladaptive movements may not only induce the loss of functional dynamic control over lumbar motion segments around its neutral zone, i.e., clinical or functional lumbar instability, but it also contributes to pain-provoking excessive spinal tissue loading and strains[3,4].
With structural integrity in place, functional lumbar instability-induced pain is frequently caused by motor control impairments, specifically of deep spinal stabilizers such as transversus abdominis (TrA), multifidus (MF), and diaphragm muscles[5–7]. Optimal core muscle activation is crucial for efficient distal mobility on the lumbar spine, requiring anticipatory activation of these deep spinal stabilizers[8]. The synergistic activation of the diaphragm along with the co-activation of other deep core muscles (TrA/IO-pelvic floor-multifidus) offers spinal stability by increasing the intra-abdominal pressure (IAP) and thoracolumbar fascia tension, without any apparent activity of the abdominal and back muscles[9]. As a result, the spine has the relative stability it needs to support the activation of superficial muscles and gross motor movements[10].
MCI patients with maladaptive movement control and sensorimotor processing require stratified care for proper spine posture, stability, and movement[11,12]. Therapeutic stabilization programs have been developed to normalize motor control in NSCLBP patients[4,13,14], but no significant changes in pain, function, or lumbar movements have been observed[15–17]. However, a lack of meaningful changes is attributed to NSCLBP heterogeneity and interventions that focus on static stability exercises while completely disregarding functional dynamic stability and diaphragm synkinetic activation[18,19].
With due consideration of functional dynamic stability and diaphragmatic synkinetic activation, a recently emerging body of evidence indicates the existence of a Dynamic Neuromuscular Stabilization (DNS) functional approach to emphasize normal sensorimotor processing and movement control skills. The philosophy of DNS is based on the developmental physiology of a newborn using a human ontogenetic model. DNS emphasizes the co-activation of the integrated spinal stabilizing system (ISSS), generating adequate intra-abdominal pressure (IAP) through coordinated co-activation of deep and superficial core muscles. Such coordinated co-activation helps in distributing the internal muscle forces acting on each spinal segment as evenly as possible[20]. A static and dynamic DNS training program emphasizes preventing spinal tissue injury or strain by avoiding pain-provoking movements, incongruent joint alignments, and overloading compensatory movement behaviour in various static or dynamic developmental postures or even while transiting between them[7,20,21].
Despite the availability of growing evidence and practice of DNS, there is a limited understanding of its scope of spinal stabilization potential and implications in non-specific chronic low back pain management. This scoping review is an attempt to explore the scope of DNS as a spinal stabilization strategy. In addition, this review also aims to identify any existing gaps in the literature regarding the DNS efficacy in low back pain management and to align the DNS as a preferred spinal stabilization intervention for a subgroup of MCI patients who exhibit maladaptive movement patterns and decreased dynamic stability.
Methods
The study in concern is a scoping review and narrative synthesis conducted in a systematic way to extract relevant evidence following stages of Arksey and O’Malley’s methodology[22]. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR)[23] were followed for reporting the results. Moreover, the study design-specific methodological quality assessment of all included studies was done according to Joanna Briggs Institute (JBI) Critical Appraisal Checklists[24].
Stage 1: Identifying the research questions
To narratively synthesize this scoping review, the following questions were identified:
What is the influence of DNS on central neural control activation among individuals with core instability?
How do DNS approach-based breathing/exercises impact various core stability variables?
What were the implications of DNS approach-based breathing/exercises in improving pain-related symptoms in chronic low back pain?
Stage 2: Identifying relevant studies
To gain an understanding of the dynamic neuromuscular stabilization effects on core stability variables such as diaphragmatic excursion, IAP, synkinetic deep core muscle activation, anticipatory postural adjustment timings and spinal (core) stability, relevant literature was searched on Pubmed, PEDro, Google Scholar, and ScienceDirect databases. Keywords such as “Dynamic Neuromuscular Stabilization,” “Dynamic Core-Postural Chain Stabilization,” “Reflex-Mediated Core Stabilization”, “Core,” and “Stability” were used with Boolean operators such as AND, OR, and NOT, as given in Table 1. The search was limited to English language and human studies.
Table 1.
The Search Strategy.
| DATABASES | SEARCH STRATEGY | FILTERS |
|---|---|---|
| PubMed | Exact phrase “dynamic neuromuscular stabilization” | 1. Article type: Clinical trial, RCT, Review 2. Language: English |
| PEDro | ||
| Science Direct | (“core” OR “stability”) AND (“dynamic neuromuscular stabilization” OR “Dynamic core-postural chain stabilization” | Article type: Case reports, review articles, research articles, others |
| Google Scholar | “Core “ OR “Stability” AND “dynamic neuromuscular stabilization” OR “Dynamic core-postural chain stabilization” | English language |
Stage 3: Study selection
All retrieved references/records were imported directly to the Endnote 20 reference manager. The studies of interest were selected based on the inclusion and exclusion. All types of clinical trials, RCT, experimental or cross-sectional/observational (i.e. Cross-sectional, cohort, case-control) studies informing the practice about DNS since inception were identified and included in this review. Further, the full-text articles that were available in the English language and assessing either the interventional effects of DNS in individuals with low back pain or the study variables reflecting the core stability components in response to DNS technique or exercises irrespective of conditions were screened for their eligibility. Study protocols, reviews, trial registrations, case reports, conference abstracts/proceedings, editorial commentaries, letters to editors, book chapters and book reviews were excluded from this review.
Two independent reviewers selected studies for inclusion in a two-step process. First, articles were screened based on title and abstract. If there was no consensus between the two reviewers, the article was included in the second stage without deliberation. In the second stage, the screening of the full text was also conducted independently by both reviewers. In cases of disagreement, the reviewers came to a consensus during a deliberation session.
Stage 4: Charting the data
To address the review questions, the following data were extracted from the full-text screening of qualified studies: author, publication year, location of the study, study design, sample size, population, intervention/s, outcome measures, and main findings/results. The data was charted using a two-step process. The extracted data was preliminarily filled in tabular form independently by both reviewers. Eventually, the data was finally charted with mutual consensus and agreement.
Stage 5: Collating, summarizing, and reporting the results
As suggested by Levac et al. (2010)[25], the obtained quantitative data was summarized descriptively. Furthermore, a qualitative summarization was also done based on the developed themes after content analysis of available literature on the DNS. A thematic description that addressed the framed questions and purpose of the intended scoping review is described in the commencing section of the results.
Results
Search results
A total of 549 records were identified through initial database searching. All references were imported to Endnote 20 for further screening and duplicate removal. A total of 34 duplicate records were removed before undertaking further screening. A total of 515 left-out records were screened following the inclusion and exclusion criteria. A total of 490 records were excluded during the title, and abstract screening phase, leaving behind 25 eligible studies for full-text screening. During this phase, seven (7) more studies were further excluded on full-text screening to finally include 18 studies that met the inclusion criteria. The PRISMA flowchart summarizing the selection process of retrieved studies is shown in Figure 1. The data extraction chart exhibiting the characteristics of each qualified study is presented in Appendix A.
Figure 1.
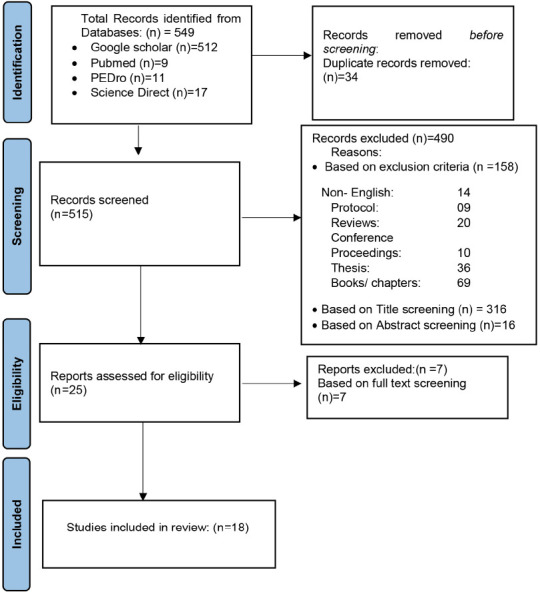
PRISMA flow diagram for study selection.
Scope and selected study characteristics
Most of the included studies were published between 2016 and 2023. Out of 18 studies, there were 9 RCTs, 5 observational, and 4 non-randomized experimental designs (1 quasi-experimental, 2 single-arm (Pretest-Posttest), 1 single-case study design). A sample size of a total of 483 participants was offered by all included studies. The location of the Included studies belongs to mainly 6 countries including the Republic of Korea or South Korea (n=10; 55.55%), Iran (n=3; 16.66%), Czech Republic (n=2; 11.11%), Taiwan (n=1; 5.55%), Turkey (n=1; 5.55%) and India (n=1; 5.55%).
All RCTs (n=9), non-randomized experimental (n=4) as well as observational (cross-sectional) (n=5) studies were assessed individually for their methodological quality. The quality assessment of studies was done by using the JBI Critical Appraisal Checklists specific to the study designs[26–28] with the final computation of appraisal score (%). The methodological quality of studies was further classified as per the obtained final % score; low (<50%), Moderate (50-70%) and high quality (>70%). Among all included studies, the level of methodological quality was identified as high in 4 studies (22.22%), moderate in 10 studies (55.55%) and low in 4 studies (22.22%). The quality assessment (risk of bias) of all included studies is presented in Table 2.
Table 2.
Levels of quality of individual studies: (JBI Critical Appraisal Checklist).
| Randomized Controlled Trials (Tufanaru et al., 2020 [27]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kim S.K. et al., 2017[31] | Lee et al., 2018[32] | Yoon H.S. et al., 2020[33 | Park et al., 2021[34] | Jung et al., 2021[35] | Sharma et al., 2023[36] | Ghavipanje V. et al., 2022[43] | Najafi Ghagholestani et al., 2022[45] | Kararti et al., 2023[44] | |||
| Was true randomization used for assignment of participants to treatment groups? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Was allocation to treatment groups concealed? | Yes | No | No | No | No | Yes | Yes | Yes | Yes | ||
| Were treatment groups similar at the baseline? | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | ||
| Were participants blind to treatment assignment? | No | Unclear | Unclear | Yes | Yes | Yes | No | No | No | ||
| Were those delivering treatment blind to treatment assignment? | Yes | Unclear | Unclear | No | No | No | Yes | Unclear | No | ||
| Were outcome assessors blind to treatment assignment? | Yes | Unclear | Unclear | No | No | No | Yes | No | Yes | ||
| Were treatment groups treated identically other than the intervention of interest? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Was follow-up complete and if not, were differences between groups in terms of their follow-up adequately described and analysed? | Yes | No | Yes | Yes | Yes | Yes | Yes | No | Yes | ||
| Were participants analysed in the groups to which they were randomized? | No | No | Yes | Yes | Yes | Yes | Yes | No | No | ||
| Were outcomes measured in the same way for treatment groups? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||
| Were outcomes measured in a reliable way? | No | Yes | No | No | No | Yes | Yes | No | Unclear | ||
| Was appropriate statistical analysis used? | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | ||
| Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial? | Yes | No | Unclear | Unclear | Unclear | Yes | Yes | Unclear | Unclear | ||
| % Score | 76.92% | 46.15% | 53.84% | 61.53% | 53.84% | 84.61% | 92.30% | 46.15% | 61.53% | ||
| Final appraisal (Quality) | High | Low | Moderate | Moderate | Moderate | High | High | Low | Moderate | ||
| Non-Randomized Experimental Studies (Tufanaru et al., 2020[28]) | |||||||||||
| D.H. Kim et al., 2018[29] | Son et al., 2017[37] | Mousavi et al., 2022[46] | Yoon H.S. & You J.S.H. 2017[42] | ||||||||
| Is it clear in the study what is the ‘cause’ and what is the ‘effect’? | Yes | Yes | Yes | Yes | |||||||
| Were the participants included in any comparisons similar? | Yes | N/A | Unclear | No | |||||||
| Were the participants included in any comparisons receiving similar treatment/ care, other than the exposure or intervention of interest? | Yes | N/A | Yes | Yes | |||||||
| Was there a control group? | No | No | Yes | Yes | |||||||
| Were there multiple measurements of the outcome both pre and post the interventions /exposure? | No | No | No | No | |||||||
| Was follow up complete or if not, were differences between groups in terms of their follow up adequately described and analysed? | N/A | No | Unclear | Yes | |||||||
| Were the outcomes of participants included in any comparison measured in the same way? | Yes | Yes | Unclear | Yes | |||||||
| Were outcomes measured in a reliable way? | Yes | Yes | No | No | |||||||
| Was appropriate statistical analysis used? | Yes | Yes | Yes | Yes | |||||||
| % score | 66.66% | 44.44% | 44.44% | 66.66% | |||||||
| Final Appraisal (Quality) | Moderate | Low | Low | Moderate | |||||||
| Observational studies (Analytical Cross-sectional) (Moola et al., 2017[26]) | |||||||||||
| D.H. Kim et al., 2016[30] | Lee J. et al., 2022[39] | Kuo et al., 2021[38] | Madle et al., 2022[40] | J. Novak et al., 2021[41] | |||||||
| Were the criteria for inclusion in the sample clearly defined? | Yes | Yes | Yes | Yes | Yes | ||||||
| Were the study subjects and the setting described in the detail? | Yes | Yes | Unclear | Unclear | Unclear | ||||||
| Was the exposure measured in a valid and reliable way? | Yes | Yes | No | Yes | Yes | ||||||
| Were objective, standard criteria used for measurement of the condition? | Yes | Yes | Yes | Yes | Yes | ||||||
| Were confounding factors identified? | No | No | Yes | No | No | ||||||
| Were strategies to deal with confounding factors stated? | No | No | No | No | No | ||||||
| Were the outcomes measured in a valid and reliable way? | Yes | Yes | No | Yes | Yes | ||||||
| Was appropriate statistical analysis used? | N/A | Yes | Yes | Yes | Yes | ||||||
| % Score | 62.5% | 75% | 50% | 62.5% | 62.5% | ||||||
| Final Appraisal (Quality) | Moderate | High | Moderate | Moderate | Moderate | ||||||
Narrative synthesis focused on problem-specific themes and questions that addressed the aims of the intended scoping review
After a content review of available literature on DNS, the following three themes were developed by the reviewers on mutual consultation.
Changes in neural (cortical and subcortical) sensorimotor control mechanisms in response to DNS
We could trace only two studies (11.11%) wherein DNS-based exercise performance was found to have the potential to activate the subconscious (implicit) and conscious (explicit) motor learning networks and neuroplasticity by respectively influencing the subcortical and cortical areas of the CNS in non-symptomatic core instability individuals[29,30].
Authors explored the neural substrates of core stabilization exercise strategies, focusing on subconscious DNS-based and conscious ADIM, in adults with lumbar instability. fMRI blood BOLD analysis showed ipsilateral subcortical and contralateral cortical activation during DNS exercises, while ADIM could activate contralateral cortical motor networks specifically. DNS-based activation of subcortical areas such as basal ganglia, cerebellum, thalamus and cingulate gyrus suggests subconscious, implicit procedural motor learning potentials that might essentially lead to motor skill acquisition and movement control normalization. Therefore, DNS, an intervention that targets both neurological substrates, might be considered a useful functional intervention strategy for patients whose spinal stability is compromised.
Changes in core stability variables in response to DNS
The DNS impacts on core stability variables such as diaphragmatic excursion, IAP, synkinetic deep core muscle activation, spinal (core) stability, and anticipatory postural adjustment timings were examined by 12 studies (66.66%) comprising six (n=6) RCTs[31–36], one (n=1) Non-randomized experimental trial[37] and five (n=5) cross-sectional observational studies[30,38–41].
Participants characteristic
All these 12 studies offered a total sample of 309. In terms of age groups, out of 12 studies, five studies included older adult participants[31–33,35,42], six included young adults[34,36,38–41] and one study included adolescent female participants[37].
Specific to the physical condition of the patients, subjects among these 12 studies are identified to be heterogeneous. Two studies enrolled subacute stroke[33,42] while two other enrolled chronic stroke participants[31,32]. Eight other individual studies examined DNS efficacy across heterogeneous populations such as individuals with CP diplegic[37], healthy participants with core instability[39], NSCLBP[38], mild to moderate stress urinary incontinence[36], COPD[35] as well as healthy participants[34,40,41].
Intervention characteristics
All 12 studies mainly explored the exposure effects of DNS breathing or exercises. Out of three RCT studies on stroke individuals, two studies compared DNS exercises efficacy against the NDT technique[33,42] whereas other one examined it against the core stability exercises (CSE)[39]. One study compared abdominal drawing-in (ADIM) and Diaphragmatic breathing (DBM) manoeuvres in stroke patients[31]. One study compared the immediate effects of DNS-based abdominal expansion (AE), ADIM and natural breathing in three different body positions among NSCLBP individuals[38]. Two individual studies examined DNS efficacy against the Abdominal Bracing (AB) techniques[34] and Kegal exercises[36]. Other two individual studies examined DNS-based breathing in comparison to diaphragmatic breathing[35] and abdominal bracing (AB) or ADIM[39]. One single-arm pretest-posttest study did not have any control or comparator group[37]. The remaining two studies explored the association between abdominal wall tension (AWT) and IAP in response to DNS breathing[41] and the comparative level of AWT in 5 basic postures of DNS[40].
Results of Outcome Variables
There was a great deal of variability across the studies in terms of measured outcomes, as summarized in Appendix A.
Changes in diaphragmatic excursion
Significant increases in the diaphragm movement/excursion were identified in response to DNS intervention by using ultrasound imaging[33,37,39] and Fluoroscopy radiographic measurement[35].
Change in DNS breathing-induced Intra-abdominal Pressure (IAP)
The results of two retrieved studies indicate the favourable potentials of DNS-based diaphragmatic breathing as a spine stabilizer in response to optimum IAP generation[40,41]. Evidence suggests that DNS breathing-based increased abdominal wall tension (AWT) is strongly correlated with increased intra-abdominal pressures that can stabilize the spine during dynamic tasks by providing stiffness around the spinal segments[41]. DNS principle-based verbal and manual instructions generated a significant rise in AWT compared to spontaneously assumed postures[40].
Changes in deep core muscle activation and thickness
DNS-based activation of the integrated spinal stabilizing system of core muscles has been explored in a total 9 studies[31–34,36–39,42]. These Studies employed surface EMG and ultrasound imaging for measuring change in deep core muscle activation and thickness respectively. The activation and thickness were measured mainly for the Transversus Abdominis (TrA); Internal Oblique (IO); External Oblique (EO); Rectus Abdominis (RA); Lumbar Multifidus (MF) and Pelvic Floor muscles.
Change in anticipatory postural adjustment timings
The change in anticipatory postural adjustment timings was examined in only one study, demonstrating the DNS impact on the feedforward strategy through subcortical activation[32].
Changes in spinal (core) stability
Two studies reported an improvement in dynamic Spinal (Core) stability as measured with a pressure biofeedback unit (PBU)[39,42].
DNS efficacy in non-specific chronic low back pain individuals
DNS efficacy in low back pain was examined by a total of 4 studies (22.22%), comprising three (n=3) RCTs single-blind (assessor)[43–45] and one (n=1) quasi-experimental study[46].
Participants’ characteristic
All four studies offered a total sample of 168 NSCLBP individuals. Out of four, three studies included adult participants[43,45,46], and one included elderly people over 65 years of age[44]. One of the studies included postpartum primiparous obese female patients[43]; two studies included middle-aged male patients[44,46]; and one study did not mention gender[45].
Intervention characteristics
Three studies provided DNS exercises to the experimental group against the control group for 6 weeks[43–45] and one for 8 weeks duration[46]. Three studies with a two-arm parallel design had a comparator control group involved in general exercises[43], core stability[46], and conventional general exercise with transcutaneous electrical nerve stimulation (TENS) and ultrasound (US) interventions[44]. One study with three parallel groups had a comparator group of aquatic exercises and no intervention control group[45].
Results of Outcome Variables
There was great variability in measured outcomes across the studies, as summarized in Appendix A. DNS intervention was found to improve pain significantly[43,45,46], functional disability[43,45], quality of life[44,46], quality of movement[44], lumbopelvic control[45], balance[44,46] abdominal strength[46], fear-avoidance belief, and respiratory functions[43].
Discussion
The undertaken scoping review was carried out systematically and the results were narratively synthesized and summarized to align with the problem-specific themes and review questions. The scoping review identified the interventional impacts of DNS on the diaphragmatic excursion, IAP, deep core muscle activation, and dynamic spinal stability. However, it highlighted the lack of robust quality studies targeting low back pain.
The review identified 18 clinical studies comprising nine RCTs, five observational, and four non-randomized experimental study designs with heterogeneity in study durations, target populations, intervention formats, and sample sizes, with low to moderate evidence quality. Given the significant differences in outcomes related to cultural context disparity, generalization of study findings may be a point of concern as most of the included studies were conducted in limited countries.
Despite significant clinical outcomes, this scoping review highlights the lack of evidence on the efficacy of DNS in managing low back pain. Very few studies were conducted over the last 7 years. All available studies on DNS training for low back pain fail to show subgroup-specific homogeneity or robust patient inclusion criteria, and that may pose a threat to the internal validity of evidence.
Only four clinical trials have used DNS training against the control comparator. Despite its potential for sensorimotor reorganization and neuroplasticity, there is a lack of quality literature on its efficacy in improving symptoms, even for non-stratified chronic low back pain.
The human brain’s nervous tissue, being plastic in nature, has a tremendous potential to respond and change its structure and function as per the received extrinsic and intrinsic stimuli[47]. This pain persists in response to altered somatosensory, nociceptive, and motor processing[48] secondary to maladaptive neuroplasticity in response to functional lumbar instability or maladaptive movement behaviour in MCI patients[3,49].
Interventions for MCI patients have been suggested to focus on normalizing posture and movement behaviour through cognitive and motor skill learning related to functional postures and movements[3,50–53]. Motor skill learning targeted interventions, involving cortical and subcortical neural communications, promote sensorimotor neuroplasticity in the population[54]. DNS-based exercises can tap into sensorimotor processing through these mechanisms[29,30].
Furthermore, MCI patients with functional lumbar instability require optimal postural control and dynamic stability training for spinal structure de-loading and motor learning[3,52,55]. Findings from this scoping review support and recommend the DNS approach as an effective strategy for lumbar stability with its potential for IAP optimization and efficient activation of the integrated spinal stabilizing system of core muscles.
The review emphasizes the need for high-quality studies on dynamic neuromuscular stabilization (DNS) in low back pain patients, particularly the MCI subgroup. Evidence suggests an intervention approach aiming to restore normal movement control and dynamically stable spine[56,57]. Effective motor learning and cognitive stimulation through proper instructions, self-identification, and fear avoidance can yield successful therapy outcomes. Therefore, MCI patients must seek to normalize movement behaviour through physical learning, not only to achieve a correct and meaningful static and dynamic spinal posture but also to transit or move between functional postures.
Considering all the available summarized facts of the undertaken scoping review, DNS training seems to be not only functionally meaningful but also an effective and pain-free spinal stability strategy. The DNS approach seems promising to achieve static and dynamic postural control in an MCI individual. DNS might be considered a matched- intervention for the MCI subgroup of the NSCLBP population as it encourages synergistic, well-coordinated, efficient muscle functions and low-load movements so that abnormal stresses are significantly reduced in the vulnerable areas of the spine.
Limitations
The undertaken systematic scoping review represents a structured, problem-specific, thematic summarization of information and evidence related to DNS-based synergism as a preferred intervention strategy for individuals with MCI who exhibit dynamic stability issues. While a thorough search of the literature was performed to retrieve the most relevant clinical and observational studies related to DNS intervention, exhaustive literature searches across various other databases or grey literature could not be performed, potentially resulting in a collection of evidence that may not be a true representative of all available evidence.
Implications and Future Research
Stabilization exercises are recommended for patients with functional lumbar instability or MCI subgroup to improve spinal motor control.
The DNS approach seems to achieve dynamic spinal stability through centrated spinal posture and an efficient movement pattern.
DNS aligns well with sensorimotor training for effective motor learning and movement normalization while tapping the physical and cognitive processes.
With due consideration of DNS as an impairment-matched intervention, future robust clinical trials on DNS efficacy in a clear homogeneous subgroup of MCI will add to the body of knowledge.
Conclusions
The existing vacuum for an effective treatment strategy that could benefit MCI subgroup patients by restoring normal movement control and posture has been a persistent concern for decades. Considering the existing knowledge, DNS seems to be a promising patient-matched intervention for the MCI subgroup of NSCLBP individuals. However, to fill this knowledge gap, further clinical trials of DNS intervention remain needed for the population of concern.
Acknowledgements
The authors extend their heartfelt appreciation to the Department of Physiotherapy, Faculty of Applied Health Sciences, MRIIRS, Faridabad, and the primary study setting, i.e., PDUNIPPD, New Delhi, for their unwavering support and assistance in the development and implementation of the study.
Appendix A
Supplementary Table.
Study characteristics.
| Author, Year and location | Study Design | Sample size | Population | Intervention | Outcome Measures | Results |
|---|---|---|---|---|---|---|
| Changes in neural (cortical and subcortical) sensorimotor control mechanisms in response to DNS | ||||||
| D.H. Kim et al., 2016[30] South Korea | Exp. study design. | Single case | 25 years old female with non-symptomatic core instability | Participant was trained for 4 exercise tasks with real time ultrasound guidance X 30 minutes/each day X 3 consecutive days before the experimental fMRI* for Identification of activated neural substrates during 4 exercise tasks: 1. Conscious ADIM (Abdominal Drawing -In Maneuver) 2. Conscious ADIM with hip flexion and extension (ADIM-HFE) 3. Subconscious hip flexion & extension (HFE) 4. Subconscious DNS-based HFE With a period of rest in between them | 3T Functional MRI (fMRI) BOLD (Blood Oxygen-Level Dependent) signal recording | Subconscious HFE and DNS-based HFE activated subcortical motor control network whereas “voluntary” conscious ADIM and ADIM- HFE motor tasks utilized cortical motor network |
| D.H. Kim et al., 2018[29] South Korea | Non randomized Experimental study | (n=5) | Non-symptomatic adults with core instability | Investigated the comparative effects of conscious (ADIM) and subconscious (DNS) core stabilization exercises on cortical changes in adults with core instability. Participant practiced the two different core exercises for 30 minutes/day for three consecutive days with real time ultrasound feedback | fMRI blood BOLD analysis | Subcortical and cortical activation pattern during the DNS exercises, whereas the cortical motor networks were activated during ADIM performance |
| Changes in Core Stability Variables | ||||||
| J. Novak et al., 2021[41] Czech Republic | Cross sectional | (n=31) Sample size was calculated. | Asymptomatic participants 15 male, 16 females mean age = 26.77 ± 3.01 yrs. | Evaluated the relationship between intra-abdominal pressure measured as anorectal pressure with objective abdominal wall tension recorded by mechanical-pneumatic-electronic sensors (DNS Brace) during five different standing postural-respiratory situations: resting breathing, Valsalva maneuver, Müller’s maneuver, instructed (DNS) breathing, loaded breathing when holding a dumbbell. | Anorectal manometry, sensors attached to a trunk brace (DNS Brace) | There is a strong correlation between intra-abdominal pressure and abdominal wall tension in all positional situations. |
| Madle et al., 2022[40] Czech Republic | Cross sectional | (n=30) Sample size was calculated. | Healthy individuals. 15 male, 15 females mean age = 22.73 ± 1.91 yrs. | Investigated the difference in abdominal wall tension (AWT) with respect to 5 basic DNS postures such as sitting, supine with legs raised, squat, bear and hang position. First, spontaneous AWT was measured, then again after manual and verbal instructions following DNS principles. | Sensor based Ohm belt device to record the abdominal wall activation | AWT increased significantly with DNS based instructions in comparison to spontaneous activation. Significant increases in activity were noted in the supine leg raise position and in the bear position compared to spontaneous activation in sitting. There were no statistically significant differences between women and men in any position. |
| Yoon H.S. & You J.S.H. 2017[42] Korea | Cross sectional design | (n=10) | First-ever stroke Mean months: 2.80 ± 0.83 Healthy: 5 males; 5 females Stroke: 2 females; 3male Mean Age: 50.8 ± 6.8 yrs. | Observed the effects of DNS and NDT* exercises in 5 healthy and 5 hemiparetic stroke individuals. All participants practiced both NDT* and DNS core stabilization exercise for 20 minutes per each session over 3 consecutive sessions before the post measurement | Core stability by Pressure biofeedback unit (PBU), muscular activity (TrA*, IQ*, EO* & RA*) and thickness (TrA & IO) with surface EMG* and ultrasound imaging respectively | DNS exercises had superior results compared to NDT both for healthy and hemiparetic stroke patients in all outcomes of interest. |
| Son et al., 2017[37] South Korea | A single-arm, Pretest-posttest clinical trial. | (n=15) | Spastic diplegic CP participant (7 females, 8 males) mean age (± SD) = 14.9 ± 3.4 yrs. | DNS intervention in the form of progressive lower extremity movement in baby rock position along with chest zone manual stimulation & real time US & EMG Biofeedback for accurate activation of diaphragm -abdominal core muscle chain. Time: 30 minutes/day, Frequency: 3 days a week, Duration: 4 weeks. | (GMFM-88*), ultrasound, & EMG were used to measure Gross motor function, diaphragm caudal movement and core muscle activity (EO, IO/TrA) respectively. | GMFM scores of standing, walking, and jumping domains; diaphragm descending movement and activation of the internal oblique and transversus abdominals were remarkably increased after the intervention |
| Kim S.K. et al., 2017[31] Korea | RCT | (n=19) Sample size was calculated | 6 months post- stroke individuals Mean age: ≥59years ADIM M/F: 6/4. DBM M/F. :7/2 | Compared the effects of the ADIM (n=10) and the DBM (Diaphragmatic Breathing Maneuver (n=9) on abdominal muscle thickness, trunk control, &balance in patients with chronic stroke. Protocol: three times per week for 4 weeks. | Ultrasonic imaging for TrA, IO & EO thickness, Trunk Impairment Scale (TIS) & Berg Balance Scale (BBS) | Both groups improved compared to baseline, however TIS score was sig. better in DBM in comparison to ADIM |
| Lee et al., 2018[32] South Korea | RCT | (n=28) | Chronic hemiparetic stroke patients 17 females; 11 males, Mean Age ≥57years | Evaluated the comparative effectiveness of DNS exercises and conventional CSE chronic hemiparetic stroke patients. Patients of both groups underwent respective exercises for 30 minutes/day, 5 days a week for 4 weeks. | APA (Anticipatory Postural Adjustment) time with EMG during rapid shoulder flexion, TIS*, BBS* and Falls Efficacy Scale (FES) | APA times for core muscles were shorter following DNS exercises in comparison with conventional exercises. Both groups improved in BBS, TIS scores and FES when compared with baseline scores |
| Yoon H.S. et al., 2020[33] Republic of Korea | RCT | (n=31) | Sub-acute stroke individuals (17 males, 14 females; mean age: 60.4 ± 14.58 yrs. Post-stroke onset, 7.22 ± 2.21 wks. | Evaluated comparative efficacy of DNS (n=16) & conventional NDT (n=15) exercises Both groups had respective treatment • Time: 30 minutes/day, • Frequency: 3sessions/ week • Duration: 4 weeks |
Abdominal muscle thickness and Diaphragm movement; postural control and gait ability were measured using Ultrasound imaging, TIS, BBS, FAC (Functional Ambulatory Category) respectively. | Superior effects of DNS over NDT were noted for all outcome measures except the TIS |
| Kuo et al., 2021[38] Taiwan | Cross-sectional | (n=30) Sample size was calculated | Non-specific low back pain individuals. Mean age: 26.7 ± 7.0 yrs. | Compared the immediate effects on lumbar stabilization muscles during the performance of DNS-based Abdominal Expansion (AE), Abdominal drawing-in (AD) and natural breathing (NB) strategies in three different body positions. | The muscle thickness and activity of the lumbar multifidus and lateral abdominal wall muscles by Ultrasonography and surface electromyography (EMG) respectively. | As AE and AD strategies both produced similar and higher EMG activity in lumbar stabilizers in comparison to NB strategy, it was suggested that AE could be an alternative strategy in improving the lumbar spine stability by facilitating the co-contraction of lumbar spine stabilizers in individuals with NSCLBP |
| Park et al., 2021[34] Republic of Korea | RCT (single-blind) | (n=36) | Healthy adults (8 females) Mean age: 24.16 ± 3.63 yrs. | Compared the effects of the DNS breathing technique and the abdominal bracing (AB) technique on upper trapezius (UT), anterior deltoid (AD), pectoralis major (PM), bilateral TrA, IO, and EO motor control in healthy participants during horizontal shoulder adduction. The DNS and AB core stabilization techniques were practiced for 30 min per day, five times a week for two weeks. | TrA/IO, EO, PM, UT, and AD muscle amplitudes during core stabilization was measured using Surface EMG. | DNS promoted significantly higher left and right IO/TrA activation while reducing UT, AD, and PM activation than during AB. DNS was found to effectively promote deep muscle activation and superficial muscle deactivation. Hence, promotes core chain dynamic stabilization and movement control. |
| Jung et al., 2021[35] Korea | RCT (Single blind) | n=14) | Acute COPD (6 women) Mean age, 69.4 ± 13.34 years | Examined the comparative effects of diaphragmatic breathing and respiratory and core-postural stabilization (DNS breathing) on diaphragmatic movement and pulmonary function test (PFT). Total 20 sessions with 30 minutes of session were carried out | Fluoroscopy radiographic measurement was done to measure diaphragmatic movement. mMRC (Modified Medical Research Council) measured dyspnea. Spirometry volume measurement was done for pulmonary function | Respiratory and core-postural stabilization was more effective in increasing diaphragmatic movements than abdominal breathing P. PFT revealed more significant differences in the forced vital capacity (FVC (%) predicted with DNS breathing. mMRC score was significantly reduced within the DSN breathing group |
| Lee J. et al., 2022[39] Korea | Cross-sectional design | (n=41) | Healthy Participants with core instability 7 females; | Compared the differential effects of ADIM, AB (Abdominal Bracing), and DNS in healthy individuals with core instability. Subjects performed ADIM, AB & DNS in random order | Simi Aktisys, PBU*, Ultrasound & sEMG were used to measure diaphragm movement, abdominal muscle thickness difference, and external abdominal oblique (EO) EMG amplitude. | Diaphragm descending movt. & Thickness of TrA & IO increased significantly with DNS compared to other two whereas IO amplitude was sig higher with AB than other two. |
| Sharma et al., 2023[36] India | RCT (single-blind) pilot study | (n=24) | Women aged 18-40 years with mild to moderate stress urinary incontinence (SUI). | Participants were divided into DNS (n=12) and Kegel exercise groups(n=12). Duration: 12 weeks | Perineometer, EMG and the Urogenital Distress Inventory-6 (UDI-6) were used to measure pelvic floor muscle strength, EMG (average, peak & maximum voluntary contraction) and quality of life respectively. | Both groups improved significantly in all outcome measures from baseline to end of 12 weeks. However, DNS group had significant improvement in all measures compared to Kegel exercises group. |
| DNS efficacy in non-specific chronic low back pain individuals | ||||||
| Ghavipanje V. et al., 2022[43] Iran | RCT (Single-blind: Assessor). | (n=40) Sample size was calculated | Obese postpartum primiparous women with LBP Age Range: 24-34 years BMI: >30 kg/m2 | Investigated the effects of 6 weeks of DNS training (n = 20) or General Exercise (GE, n = 20): • Time (min/d):45-60 min • Frequency (x/wk): 6 (3 supervised and 3 home based) • Duration(wk):6 weeks |
NPRS*, MODQ*, Fear-Avoidance Beliefs Questionnaire (FABQ), Breath Hold Time & Respiratory rate (RR) were used to measure pain intensity, disability, fear avoidance belief and respiratory functions respectively. | The rate of improvement for all outcome measures were significantly higher in the DNS group compared to the GE group. |
| Najafi Ghagholestani et al., 2022[45] Iran | RCT Single blind: (Assessor) | (n=36) | NSCLBP Gender not specified Age range :30-50 years Mean BMI<30 kg/m2 | Compared the effects of 6 weeks DNS (n = 15), Aquatic Exercises (AEs) (n = 15), and No intervention Control (n = 15) among NSCLBP individuals DNS & AE group protocol: • Time (min/d):50 min • Frequency (x/wk): 3 • Duration(wk): 6 weeks * Data was finally analyzed for 12 subjects in each group after 6 weeks subsequent to drop out |
VAS*, ODI*, Pressure biofeedback (during Lumbopelvic control tests performance) and spinal mouse device were used to measure pain intensity, disability, lumbopelvic control and spinal posture respectively. | Both DNS & AE groups showed a significant improvement in pain intensity, disability, and Lumbopelvic control. No changes across groups, nevertheless, were found |
| Mousavi et al; 2022[46] Iran | quasi-experimental study (pretest-posttest design) | (n=20) | Men with chronic non-specific low back pain Age range : 21-62 years | Investigated impacts of (DNS) and core stability (CS) exercises in men with non-specific chronic low back pain. • Time (min/d):45-60min • Frequency (x/wk): 3days/wk • Duration (wk):8 wks |
VAS, Flexibility Box, Y balance test, half sit up & SF-36*, (Persian version) were used to measure pain, hamstring flexibility, balance, abdominal muscle strength, and quality of life (QoL) | Both interventions led to significant improvement in pain, abdominal strength and static balance. However, hamstring flexibility and quality of life were improved specifically within CS and DNS respectively. No statistical difference between both training methods |
| Kararti et al., 2023[44] Turkey | RCT (Single blind: Assessor) | (n=72) | Old adult males having chronic non- specific low back pain with age group above 65 years | Examined the comparative effects of DNS and conventional control interventions in older adults with NSCLBP (36 subjects in each group). • Time (min/d):30-40 min • Frequency (x/wk): 3days/wk • Duration(wk): 6 wks Control group had TENS*, US* and strengthening and stretching exercises whereas experimental group had control along as well as DNS exercises |
FMS, 6- minute walk test (6MWT), TUG* & WHOQOL-OLD* module were used to measure Quality of movement, Exercise capacity, Functional balance & QoL respectively | DNS group had significant effects on total FMS* scoring and Functional balance. Though both groups had similar improvements in other measures. |
Abbreviations: fMRI: Functional Magnetic Resonance Imaging; NDT: Neurodevelopment Technique; TrA: Transversus Abdominis; IQ: Internal Oblique; EO: External Oblique; RA: Rectus Abdominis; GGFM: Gross Motor Function Measure; TUG: Timed up and Go test; FMS: Functional Movement Scale; VAS: Visual analogue score; TENS: Transcutaneous electrical nerve stimulation; US :Ultrasound; MODQ: Modified Oswestry disability questionnaire; ODI: Oswestry Disability Index; NPRS: Numeric Pain Rating Score; sEMG: surface Electromyography; SF-36: Short Form-36.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Balagué F, Mannion AF, Pellisé F, Cedraschi C. Seminar Non-specific low back pain Epidemiology and natural history. The Lancet. 2012;379:482–491. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 2.Ferreira ML, De Luca K, Haile LM, et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050:a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(6):e316–e329. doi: 10.1016/S2665-9913(23)00098-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Sullivan P. Diagnosis and classification of chronic low back pain disorders:Maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10(4):242–255. doi: 10.1016/j.math.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 4.O'Sullivan P. Lumbar segmental “instability”:clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5(1):2–12. doi: 10.1054/math.1999.0213. [DOI] [PubMed] [Google Scholar]
- 5.Hodges PW, Richardson CA. Feedforward contraction of transversus abdominis is not influenced by the direction of arm movement. Exp Brain Res. 1997;114:362–370. doi: 10.1007/pl00005644. [DOI] [PubMed] [Google Scholar]
- 6.Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region:Effect and possible mechanisms. Journal of Electromyography and Kinesiology. 2003;13(4):361–370. doi: 10.1016/s1050-6411(03)00042-7. [DOI] [PubMed] [Google Scholar]
- 7.Kolar P, Kobesova A, Valouchova P, Bitnar P. Treatment Methods. Second Edi. Elsevier Ltd; 2013. Dynamic Neuromuscular Stabilization. [Google Scholar]
- 8.Hodges PW, Richardson C. Inefficient Muscular Stabilization of the Lumbar Spine Associated With Low Back Pain. Spine (Phila Pa 1976) 1996;21(22):2640–2650. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 9.Hodges P, Eriksson A, Shirley D, Gandevia S. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38(9):1873–1880. doi: 10.1016/j.jbiomech.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 10.Hodges PW, Gandevia SC. Changes in intra-abdominal pressure during postural and respiratory activation of the human diaphragm. J Appl Physiol (1985) 2000;89(3):967–976. doi: 10.1152/jappl.2000.89.3.967. [DOI] [PubMed] [Google Scholar]
- 11.Foster NE, Hill JC, O'Sullivan P, Hancock M. Stratified models of care. Best Pract Res Clin Rheumatol. 2013;27(5):649–661. doi: 10.1016/j.berh.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Karayannis NV, Jull GA, Hodges PW. Physiotherapy movement based classification approaches to low back pain:Comparison of subgroups through review and developer/expert survey. BMC Musculoskelet Disord. 2012;13 doi: 10.1186/1471-2474-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dankaerts W, O'Sullivan P. The validity of O'Sullivan's classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI):Overview of a series of studies and review of the literature. Man Ther. 2011;16(1):9–14. doi: 10.1016/j.math.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Ferreira PH, Ferreira ML, Maher CG, Herbert RD, Refshauge K. Specific stabilisation exercise for spinal and pelvic pain:A systematic review. Australian Journal of Physiotherapy. 2006;52(2):79–88. doi: 10.1016/s0004-9514(06)70043-5. [DOI] [PubMed] [Google Scholar]
- 15.Gomes-Neto M, Lopes JM, Conceição CS, et al. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain:A systematic review and meta-analysis. Physical Therapy in Sport. 2017;23:136–142. doi: 10.1016/j.ptsp.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev. 2005;2005(3):CD000335. doi: 10.1002/14651858.CD000335.pub2. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain:A systematic review with meta-analysis. BMC Musculoskelet Disord. 2014;15(1) doi: 10.1186/1471-2474-15-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alrwaily M, Timko M, Schneider M, et al. Treatment-based Classification System for Patients With Low Back Pain:The Movement Control Approach. Phys Ther. 2017;97(12):1147–1157. doi: 10.1093/ptj/pzx087. [DOI] [PubMed] [Google Scholar]
- 19.Saragiotto BT, Maher CG, Yamato TP, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database of Systematic Reviews. 2016;2016(1) doi: 10.1002/14651858.CD012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization &sports rehabilitation. Int J Sports Phys Ther. 2013;8(1):62–73. [PMC free article] [PubMed] [Google Scholar]
- 21.Kobesova A, Kolar P. Developmental kinesiology:Three levels of motor control in the assessment and treatment of the motor system. J Bodyw Mov Ther. 2014;18(1):23–33. doi: 10.1016/j.jbmt.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Arksey H, O'Malley L. Scoping studies:Towards a methodological framework. International Journal of Social Research Methodology:Theory and Practice. 2005;8(1):19–32. [Google Scholar]
- 23.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR):Checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 24.Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z. JBI Manual for Evidence Synthesis. JBI. 2024. Available from: https://synthesismanual.jbi.global .
- 25.Levac D, Colquhoun H, O'Brien KK. Scoping studies:advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P-F. Aromataris E, Munn Z, editors. Chapter 7:Systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute. 2017. Available from https://reviewersmanual.joannabriggs.org/
- 27.Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3:Systematic reviews of effectiveness (Critical Appraisal Checklist for Randomized Controlled Trials) In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. Available from https://synthesismanual.jbi.global . [Google Scholar]
- 28.Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3:Systematic reviews of effectiveness (Critical Appraisal Checklist for Quasi-Experimental Studies) In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. Available from https://synthesismanual.jbi.global . [Google Scholar]
- 29.Kim DH, Lee JJ, You SH. Best core stabilization exercise to facilitate subcortical neuroplasticity:A functional MRI neuroimaging study. Technology and Health Care. 2018;26(3):401–407. doi: 10.3233/THC-171051. [DOI] [PubMed] [Google Scholar]
- 30.Kim DH, Lee JJ, Han BS, You JH. Cortical or subcortical neural networks during dynamic neuromuscular core stabilization:A fMRI blood oxygen-level dependent (BOLD) analysis. J Med Imaging Health Inform. 2016;6(7):1732–1734. [Google Scholar]
- 31.Kim kyung S, Kang woo T, Park hwan D, Lee hyun J, Cynn seock H. Four-Week Comparative Effects of Abdominal Drawing-In and Diaphragmatic Breathing Maneuvers on Abdominal Muscle Thickness, Trunk Control, and Balance in Patients With Chronic Stroke. Physical Therapy Korea. 2017;24(3):10–20. [Google Scholar]
- 32.Lee NG, You (Sung) JH, Yi CH, et al. Best Core Stabilization for Anticipatory Postural Adjustment and Falls in Hemiparetic Stroke. Arch Phys Med Rehabil. 2018;99(11):2168–2174. doi: 10.1016/j.apmr.2018.01.027. [DOI] [PubMed] [Google Scholar]
- 33.Yoon HS, Cha YJ, You JH. Effects of dynamic core-postural chain stabilization on diaphragm movement, abdominal muscle thickness, and postural control in patients with subacute stroke:A randomized control trial. NeuroRehabilitation. 2020;46(3):381–389. doi: 10.3233/NRE-192983. [DOI] [PubMed] [Google Scholar]
- 34.Park C, Yoon S, Yoon H, Kim K, Cha Y, Park I. Effects of core stabilization exercise on muscle activity during horizontal shoulder adduction with loads in healthy adults:a randomized controlled study. J Mech Med Biol. 2021;21(9) [Google Scholar]
- 35.Jung G, Park C, Hwang J, You JH, Yi C, Choi WJ. Effects of core-postural stabilisation on fluoroscopy diaphragmatic measurement and dyspnea in chronic obstructive pulmonary disease:A randomized single-blinded clinical trial. Technology and Health Care. 2021;29:S359–S366. doi: 10.3233/THC-218034. IOS Press BV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma K, Gupta M, Parasher RK, Chawla JK. Comparing the Efficacy of Dynamic Neuromuscular Stabilization Exercises and Kegel Exercises on Stress Urinary Incontinence in Women:A Pilot Study. Cureus. 2023 doi: 10.7759/cureus.50551. Published online December 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Son MS, Jung DH, You JH, Yi CH, Jeon HS, Cha YJ. Effects of dynamic neuromuscular stabilization on diaphragm movement, postural control, balance and gait performance in cerebral palsy. NeuroRehabilitation. 2017;41(4):739–746. doi: 10.3233/NRE-172155. [DOI] [PubMed] [Google Scholar]
- 38.Kuo YL, Kao CY, Tsai YJ. Abdominal expansion versus abdominal drawing-in strategy on thickness and electromyography of lumbar stabilizers in people with nonspecific low back pain:A cross-sectional study. Int J Environ Res Public Health. 2021;18(9) doi: 10.3390/ijerph18094487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee J, Kim D, Shin Y, et al. Comparison of core stabilization techniques on ultrasound imaging of the diaphragm, and core muscle thickness and external abdominal oblique muscle electromyography activity. J Back Musculoskelet Rehabil. 2022;35(4):839–847. doi: 10.3233/BMR-210051. [DOI] [PubMed] [Google Scholar]
- 40.Madle K, Svoboda P, Stribrny M, et al. Abdominal wall tension increases using Dynamic Neuromuscular Stabilization principles in different postural positions. Musculoskelet Sci Pract. 2022;62 doi: 10.1016/j.msksp.2022.102655. [DOI] [PubMed] [Google Scholar]
- 41.Novak J, Jacisko J, Busch A, et al. Intra-abdominal pressure correlates with abdominal wall tension during clinical evaluation tests. Clinical Biomechanics. 2021;88 doi: 10.1016/j.clinbiomech.2021.105426. [DOI] [PubMed] [Google Scholar]
- 42.Yoon HS, You JH. Technology and Health Care. Vol. 25. IOS Press; 2017. Reflex-mediated dynamic neuromuscular stabilization in stroke patients:EMG processing and ultrasound imaging; pp. S99–S106. [DOI] [PubMed] [Google Scholar]
- 43.Ghavipanje V, Rahimi NM, Akhlaghi F. Six Weeks Effects of Dynamic Neuromuscular Stabilization (DNS) Training in Obese Postpartum Women With Low Back Pain:A Randomized Controlled Trial. Biol Res Nurs. 2022;24(1):106–114. doi: 10.1177/10998004211044828. [DOI] [PubMed] [Google Scholar]
- 44.Karartı C, Özsoy İ, Özyurt F, Basat HÇ, Özsoy G, Özüdoğru A. The effects of dynamic neuromuscular stabilization approach on clinical outcomes in older patients with chronic nonspecific low back pain:a randomized, controlled clinical trial. Somatosens Mot Res. 2023;40(3):116–125. doi: 10.1080/08990220.2023.2191705. [DOI] [PubMed] [Google Scholar]
- 45.Ghagholestani BN, Gandomi F, Assar S, Spears LR. Effects of Dynamic Neuromuscular Stabilization and Aquatic Exercises on the Pain, Disability, Lumbopelvic Control, and Spinal Posture of Patients With Non-specific Low Back Pain. Iranian Rehabilitation Journal. 2022;20(3):333–344. [Google Scholar]
- 46.Mousavi SMS, Mirsafaei Rizi R. Effect of Central Stability and Dynamic Neuromuscular Stabilization Exercises on Pain, Flexibility, Balance, Muscle Endurance and Quality of Life in Men With Nonspecific Chronic Low Back Pain. Journal of Guilan University of Medical Sciences. 2022;31(2):136–149. [Google Scholar]
- 47.Mateos-Aparicio P, Rodríguez-Moreno A. The impact of studying brain plasticity. Front Cell Neurosci. 2019;13 doi: 10.3389/fncel.2019.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brumagne S, Diers M, Danneels L, Lorimer Moseley G, Hodges PW. Neuroplasticity of sensorimotor control in low back pain. Journal of Orthopaedic and Sports Physical Therapy. 2019;49(6):402–414. doi: 10.2519/jospt.2019.8489. [DOI] [PubMed] [Google Scholar]
- 49.Wand BM, Parkitny L, O'Connell NE, et al. Cortical changes in chronic low back pain:Current state of the art and implications for clinical practice. Man Ther. 2011;16(1):15–20. doi: 10.1016/j.math.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 50.Mang CS, Borich MR, Wadden KP, Boyd LA, Siengsukon CF. “Motor skill learning and its neurophysiology,''in Skill Acquisition in Sport:Research, Theory and Practice. In: Hodges J, Williams A. M., editors. Third Edi N. London, New York: Routledge; 2020. pp. 293–312. [Google Scholar]
- 51.Luomajoki H, Kool J, de Bruin ED, Airaksinen O. Improvement in low back movement control, decreased pain and disability, resulting from specific exercise intervention. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:11. doi: 10.1186/1758-2555-2-11. Published 2010 Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sahrmann SA. Does postural assessment contribute to patient care? J Orthop Sports Phys Ther. 2002;32(8):376–379. doi: 10.2519/jospt.2002.32.8.376. [DOI] [PubMed] [Google Scholar]
- 53.Salamat S, Talebian S, Bagheri H, et al. Effect of movement control and stabilization exercises in people with extension related non -specific low back pain- a pilot study. J Bodyw Mov Ther. 2017;21(4):860–865. doi: 10.1016/j.jbmt.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 54.Penhune VB, Doyon J. Dynamic cortical and subcortical networks in learning and delayed recall of timed motor sequences. J Neurosci. 2002;22(4):1397–1406. doi: 10.1523/JNEUROSCI.22-04-01397.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mottram S, Comerford M. A new perspective on risk assessment. Physical Therapy in Sport. 2008;9(1):40–51. doi: 10.1016/j.ptsp.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 56.O'Sullivan K, Dankaerts W, O'Sullivan L, O'Sullivan PB. Cognitive Functional Therapy for Disabling Nonspecific Chronic Low Back Pain:Multiple Case-Cohort Study. Phys Ther. 2015;95(11):1478–1488. doi: 10.2522/ptj.20140406. [DOI] [PubMed] [Google Scholar]
- 57.Vibe Fersum K, O'Sullivan P, Skouen JS, Smith A, Kvåle A. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain:A randomized controlled trial. European Journal of Pain (United Kingdom) 2013;17(6):916–928. doi: 10.1002/j.1532-2149.2012.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


