Abstract
Anterior tarsal tunnel syndrome, an infrequent entrapment neuropathy involving the deep peroneal nerve beneath the inferior extensor retinaculum in the anterior ankle, is often overlooked on medical images, leading to delayed diagnosis and treatment. We present the case of a 52-year-old male, an avid runner, who exhibited a sensation of burning and tingling in the dorsal region of both feet. Electrophysiologic studies suggested bilateral deep peroneal neuropathy. Subsequent magnetic resonance imaging revealed bilateral focal regions of signal alteration, consistent with scarring, encasing the deep peroneal nerves at the anterior tarsal tunnel. These regions were indented by the deep laminae of the inferior extensor retinacula, suggesting compression. The constellation of findings was consistent with anterior tarsal tunnel syndrome. This is a unique case of bilateral deep peroneal nerve entrapment exacerbated by repetitive microtrauma, culminating in anterior tarsal tunnel syndrome. Notably, this case represents the first instance in literature where MRI played a pivotal role in diagnosis.
Keywords: Anterior Tarsal Tunnel Syndrome, Inferior Extensor Retinaculum, MRI
Introduction
Anterior tarsal tunnel syndrome (ATTS), also known as deep peroneal nerve (DPN) entrapment, was initially documented in 1960[1]. This syndrome is a compression neuropathy of the DPN deep to the inferior extensor retinaculum. The DPN arises in the proximal lateral compartment of the lower leg as one of two terminal branches of the common peroneal nerve. The DPN pierces the intermuscular septum and travels down the leg within the anterior compartment. Just distal to the inferior extensor retinaculum, the DPN divides into the lateral and medial terminal branches. The lateral terminal branch innervates the extensor digitorum brevis (EDB) and extensor hallucis brevis (EHB) muscles, while the medial terminal branch accompanies the dorsalis pedis artery along the dorsal foot, primarily providing sensory innervation to the first webspace[2,3].
The anterior tarsal tunnel (ATT) is a fibro-osseous corridor distal and anterior to the ankle, with boundaries defined by the inferior extensor retinaculum (IER) superficially, the medial malleolus medially, the lateral malleolus laterally, and the talonavicular joint capsule on the deep border. The IER is a Y-shaped band, with the stem arising from the lateral superior surface of the calcaneus, anterior to the depression for the interosseous talocalcaneal ligament[4]. This stem has two laminae, with the superficial lamina passing superficial to the extensor digitorum longus (EDL) and peroneus tertius (PT) tendons, and the deep lamina deep to these tendons[4]. The contents of the ATT include (from medial to lateral), the tibialis anterior (TA) and extensor hallucis longus (EHL) tendons, dorsalis pedis artery and vein (DPA and DPV), DPN, and the EDL and PT (when present) tendons (Figure 1). Symptoms linked to anterior tarsal tunnel syndrome include pain or altered sensation involving the dorsum of the foot as well as motor dysfunction, potentially leading to atrophy of the intrinsic muscles of the foot and gait irregularities[2,3,5].
Figure 1.
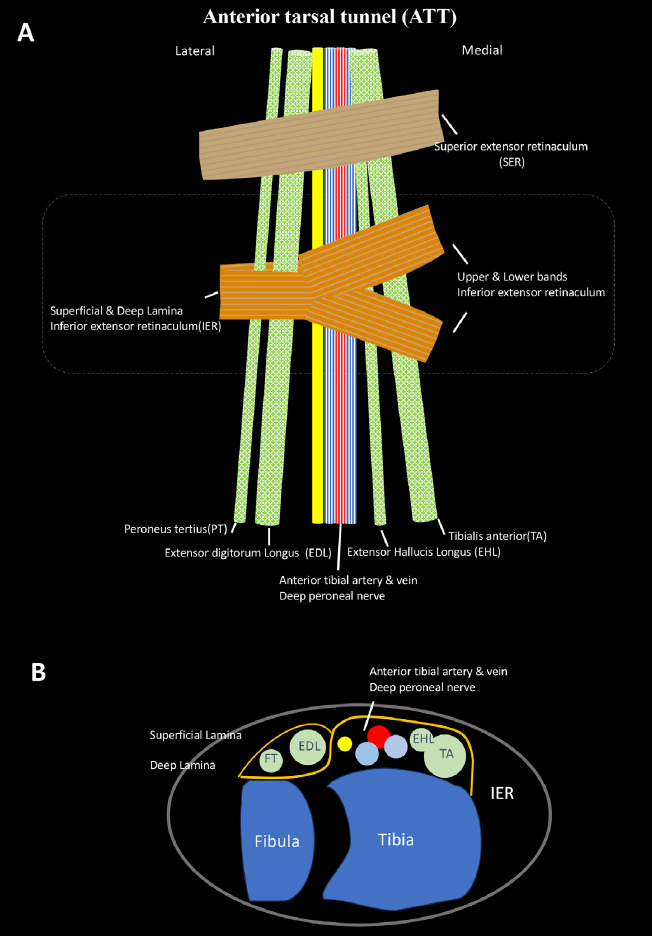
Anatomic illustration of the anterior tarsal tunnel (ATT) in coronal plane (A) and axial plane (B). Colour coding (yellow = DPN, orange = retinaculum, red = DPA, light blue = DPV).
ATTS results from compression or entrapment of the DPN in the anterior tarsal tunnel. Potential causes include a single episode of trauma, repetitive microtrauma, intraneural ganglia, and extrinsic compression, such as from ganglia arising from nearby articulations[6-8]. The prevalence of anterior tarsal tunnel syndrome is not known. Diagnosis primarily hinges on a thorough medical history and comprehensive physical examination, augmented by additional imaging as necessary[3]. In ambiguous clinical and imaging scenarios, nerve conduction velocity and electromyography assessments may be added. High-resolution musculoskeletal ultrasound is a viable diagnostic tool[9]. While MRI has been recommended to assess for extrinsic soft tissue compression within the tunnel, there are no such cases in the current literature. We present a case of bilateral MRI findings consistent with apparent scarring surrounding the deep peroneal nerve within the ATT, with evidence of impingement by the deep lamina of the IER, likely caused by repetitive microtrauma secondary to running, in a 52-year-old male.
Case Presentation
A 52-year-old man with a known medical history of thalassemia trait presented with a burning sensation and tingling in the dorsum of both feet, particularly aggravated by treadmill running. Additionally, he experienced swelling and high/low temperature sensitivity in the medial toes of both feet, exacerbated in cold weather and by attempted self-treatment with cold water soaks (Figure 2). There was no muscular weakness, and his upper and lower limb deep tendon reflexes were normal. While his pinprick sensation was intact, he exhibited reduced sensation to light touch in the first through third web spaces, greatest in the first web space. Tinel’s sign was elicited over the dorsum of the both feet. Previous testing for hemoglobin A1c, fasting glucose, vitamin B12, TSH, and protein electrophoresis were normal. Subsequently, he was referred to a neurologist and underwent an electrophysiological study (EPS).
Figure 2.

A picture of the patient’s feet after a soak in cold water during the initial presentation. Note the swelling in the bilateral medial toes.
The EPS revealed a normal right superficial peroneal sensory nerve action potential (SNAP) amplitude and conduction velocity. Right tibial nerve recordings from the abductor hallucis muscle showed normal onset latency, CMAP amplitude, and conduction velocity. Deep peroneal nerve conduction velocity was normal bilaterally throughout the lower leg and foot. The right deep peroneal nerve study recording from the EDB muscle showed prolonged distal latency (9.9) along with a reduced compound muscle action potential (CMAP) amplitude of 3.1. Similar findings were observed in the left EDB, with prolonged latency (8.9) and a CMAP amplitude of 2.6. The left EDB displayed large motor unit action potentials with rapid firing and reduced recruitment. Despite normal deep peroneal nerve conduction velocity bilaterally, the electrophysiological results in aggregate were considered consistent with ATTS according to the neurologist. To explore potential structural changes, an MRI of the ankle was recommended.
MRI of the ankle bilaterally showed the distal deep peroneal nerves (DPN) located superficial to DPA and DPVs at the level of anterior tarsal tunnel. The DPNs were encased by ill-defined T1 hypointense, proton density intermediate, and inversion recovery (IR) low signal material dorsolateral to the distal talus and talonavicular articulations (Figure 3A, B). This material appeared quite similar bilaterally and measured 17 x 6 mm on the right and 19 x 11 mm on the left (Figure 3 C, D) The lateral margins of this material appeared concave and indented the deep lamina of the inferior extensor retinaculum (Figure 4).
Figure 3.
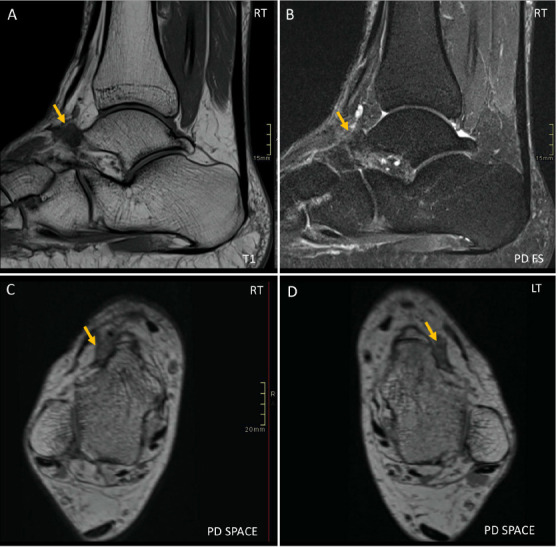
Sagittal T1 (A) and IR (B) and axial reformats of PD-weighted 3D space (C, D). MR images of bilateral ankles demonstrate focal ill-defined low to intermediate-signal regions dorsolateral to the talar head and talonavicular joints (yellow arrows), suggestive of scar tissue.
Figure 4.
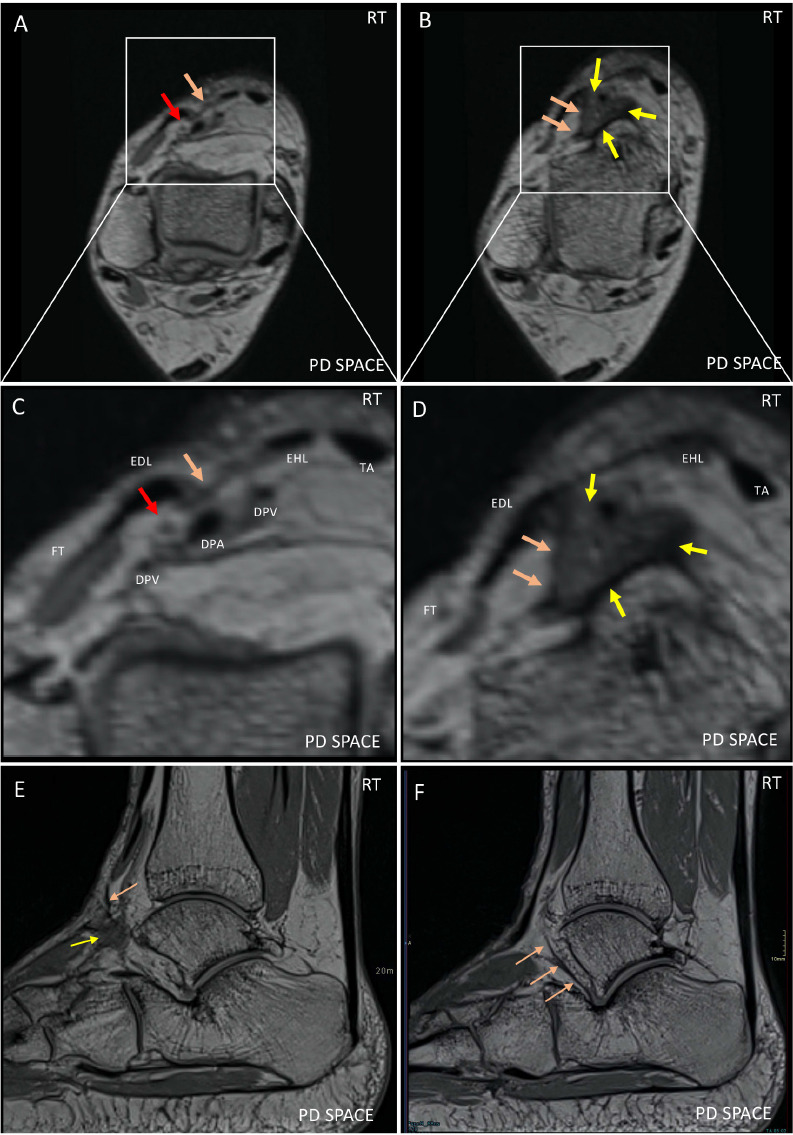
Axial reformats from PD-weighted 3D sequences of the right ankle above (A) and at the level of the IER (B) with additional magnified views (C, D) as well as the original sagittal images (E, F). C) highlights the arrangement of the deep peroneal neurovascular bundle, also containing the dorsalis pedis artery (DPA) and veins (DPV), proximal to the ATT. The deep peroneal nerve (DPN) is slightly superficial to the DPA and DPVs, indicated by the red arrow. The tibialis anterior (TA), extensor digitorum longus (EDL), extensor hallucis longus (EHL), and peroneus tertius tendons (PT) are located more superficially, as is the IER (orange arrow). D) highlights the geographic region of signal alteration (yellow arrow) encasing the DP neurovascular bundle, at the level of the ATT. The lateral border of the scarring is bordered by the deep lamina (orange arrows) of the IER. Sagittal PD-weighted 3D images of the right ankle (E, F) show the geographic area of signal alteration (yellow arrow) with lateral margin contacting the deep lamina of the inferior extensor retinaculum (orange arrows).
The patient was referred to an orthopedic surgeon who speculated that the patient’s ATTS resulted from ill-fitting running-related footwear and recommended more accommodative footwear with the addition of orthotics if required. The surgeon also discussed the option of exploration of the neurovascular bundle and potential neurolysis but the patient opted for nonoperative management.
At clinical follow-up one year after the MRI, the patient noted that he had always tied his shoelaces very tight, a habit formed from years of playing soccer. After receiving the diagnosis of ATTS and the advice of the orthopedic surgeon, the patient stopped running and started tying his shoelaces loosely. There was an immediate substantial improvement in his symptoms followed by more gradual further improvement. At the time of this follow-up, the symptoms had resolved during the summer and were only evident during the winter.
Discussion
We present the case of a 52-year-old male who reported a burning and tingling sensation in the dorsum of both feet. Electrophysiological studies revealed bilateral prolonged distal latency and reduced compound muscle action potential (CMAP) amplitude involving the deep peroneal nerve distribution, along with neuropathic chronic remodeling changes in the extensor digitorum brevis muscles. Subsequent MRI showed bilateral low signal material consistent with fibrous tissue in the ATTS indented by the deep laminae of the inferior extensor retinacula and encasing the deep peroneal nerves.
This subject had a clinical history and physical examination consistent with ATTS. The primary complaint was paresthesia in the distribution of the deep peroneal nerve in the foot, worsened by treadmill use in an avid runner. Physical examination revealed a positive dorsal foot Tinel’s sign and decreased sensation over the dorsal foot while electrophysiologic findings supported the diagnosis. The MRI findings provided further objective evidence of nerve compression at the anterior tarsal tunnel. In this context, it is likely that the low-signal area seen on imaging represented scar formation, presumably resulting from tightly fitting footwear during running.
ATTS is an infrequent neuropathic condition and lacks a single specific diagnostic test. Instead, the diagnosis relies on a thorough history, physical examination, and supporting EPS and/or medical imaging. The DPN nerve may be entrapped due to a single episode of trauma or repetitive micro-trauma. Imaging findings have described space-occupying lesions such as ganglion cysts, intraneural ganglions, varicosities of the anterior tibial veins, as well as adjacent osteophytes and accessory ossicles, such as the os intermetatarseum[6,7,10,11]. Clinically, hypertrophy of the nearby extensor hallucis brevis muscle or external compression from tight footwear, sports equipment, or military gear can also contribute to ATTS[12]. If structural causes are suspected clinically, supplementary imaging such as weight-bearing foot and ankle radiographs offer a cost-effective method for identifying contributing factors like bony hypertrophy or osteophytes that could be causing compression neuropathy[2]. MRI and high-resolution ultrasound can provide direct visualization of peripheral nerves in the lower extremities[9,13]. While the reliability of ultrasound can vary due to anatomic variation of peripheral nerves, some literature has suggested its usefulness in identifying intraneural ganglia[8].
Our paper is the first report of ATTS with MRI findings. MRI showed findings suggestive of fibrous tissue encasing the deep peroneal nerves within the anterior tarsal tunnels bilaterally, indented by the inferior extensor retinaculum bilaterally. This tissue could potentially have implications for surgical planning if conservative treatment is not effective. We note that this is the first report highlighting the potential role of the deep lamina of the inferior extensor retinaculum specifically as opposed to the IER generally. A study comparing MRI imaging in a large number of subjects with ATTS with asymptomatic controls would be helpful to determine if indentation of the ATT by the deep lamina of the IER is normal or abnormal, and if abnormal, whether it is unique to this case or is a common cause of impingement in ATTS.
This case report is limited by a lack of surgical/pathological confirmation as the patient opted for nonoperative management, namely cessation of running and loosening his shoelaces. Further, not all components of the clinical scenario could be explained by ATTS. Sensitivity to extremes of temperature have not been described as part of ATTS. We note that the patient had swelling of the medial toes bilaterally, also not previously described. We question whether encasement of the dorsalis pedis veins may have caused this swelling (Figure 2). Also, while the severity of decreased sensation was greatest in the first web space, the extent of sensory changes was greater than expected for the distribution of the deep peroneal nerve. However, several studies have shown variation in the share of the dorsum of the foot supplied by the DPN compared to the superficial peroneal nerve (SDN) with actual communication between the two nerves seen in up to 10% of subjects[14,15]. We feel that all considered, the patient’s history, physical examination, electrophysiologic study, imaging findings, and clinical improvement after foot-ware modification convincingly align with a diagnosis of bilateral anterior tarsal tunnel syndrome (ATTS).
In conclusion, this is the first case report of anterior tarsal tunnel syndrome (ATTS) that includes MRI findings. The MRI revealed low-signal tissue consistent with scarring surrounding the deep peroneal nerve/dorsalis pedis neurovascular bundle in the ATT, with apparent compression by deep lamina of the inferior extensor retinaculum. This suggests that scarring may potentially contribute to deep peroneal nerve entrapment in ATTS and that the deep lamina of the inferior extensor retinaculum may potentially contribute to impingement. Knowledge of the presence of scarring could potentially help with prognostication and treatment planning. Additionally, surgical planning in patients requiring operative management may be aided by knowledge of the presence of scarring and the specific structure/s impinging on the deep peroneal nerve.
Consent to publish
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
References
- 1.Kopell HP, Thompson WA. Peripheral entrapment neuropathies of the lower extremity. N Engl J Med. 1960;262:56–60. doi: 10.1056/NEJM196001142620202. [DOI] [PubMed] [Google Scholar]
- 2.DiDomenico LA, Masternick EB. Anterior tarsal tunnel syndrome. Clin Podiatr Med Surg. 2006;23:611–620. doi: 10.1016/j.cpm.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Dreyer MA, Gibboney MD. In:StatPearls. Treasure Island (FL) ineligible companies: Disclosure:Michael Gibboney declares no relevant financial relationships with ineligible companies; 2023. Anterior Tarsal Tunnel Syndrome. [Google Scholar]
- 4.Goldwyn RM. Gray's anatomy. Plast Reconstr Surg. 1985;76:147–148. doi: 10.1097/00006534-198507000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Aktan Ikiz ZA, Ucerler H, Uygur M. Dimensions of the anterior tarsal tunnel and features of the deep peroneal nerve in relation to clinical application. Surg Radiol Anat. 2007;29:527–530. doi: 10.1007/s00276-007-0229-x. [DOI] [PubMed] [Google Scholar]
- 6.Artico M, Stevanato G, Ionta B, et al. Venous compressions of the nerves in the lower limbs. Br J Neurosurg. 2012;26:386–391. doi: 10.3109/02688697.2011.631616. [DOI] [PubMed] [Google Scholar]
- 7.Milants C, Wang FC, Gomulinski L, et al. [The anterior tarsal tunnel syndrome:a case report. Rev Med Liege. 2015;70:400–404. [PubMed] [Google Scholar]
- 8.Sillat T, Pivec C, Bernathova M, et al. Unusual Cause of Anterior Tarsal Tunnel Syndrome:Ultrasound Findings. J Ultrasound Med. 2017;36:837–839. doi: 10.7863/ultra.16.03092. [DOI] [PubMed] [Google Scholar]
- 9.Chari B, McNally E. Nerve Entrapment in Ankle and Foot:Ultrasound Imaging. Semin Musculoskelet Radiol. 2018;22:354–363. doi: 10.1055/s-0038-1648252. [DOI] [PubMed] [Google Scholar]
- 10.Huang KC, Chen YJ, Hsu RW. Anterior tarsal tunnel syndrome:case report. Changgeng Yi Xue Za Zhi. 1999;22:503–507. [PubMed] [Google Scholar]
- 11.Nakasa T, Fukuhara K, Adachi N, et al. Painful os intermetatarseum in athletes:report of four cases and review of the literature. Arch Orthop Trauma Surg. 2007;127:261–264. doi: 10.1007/s00402-006-0195-5. [DOI] [PubMed] [Google Scholar]
- 12.Tennant JN, Rungprai C, Phisitkul P. Bilateral anterior tarsal tunnel syndrome variant secondary to extensor hallucis brevis muscle hypertrophy in a ballet dancer:a case report. Foot Ankle Surg. 2014;20:e56–58. doi: 10.1016/j.fas.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Visser LH. High-resolution sonography of the common peroneal nerve:detection of intraneural ganglia. Neurology. 2006;67:1473–1475. doi: 10.1212/01.wnl.0000240070.98910.bc. [DOI] [PubMed] [Google Scholar]
- 14.Madhavi C, Isaac B, Antoniswamy B, et al. Anatomical variations of the cutaneous innervation patterns of the sural nerve on the dorsum of the foot. Clin Anat. 2005;18:206–209. doi: 10.1002/ca.20094. [DOI] [PubMed] [Google Scholar]
- 15.Nayak VS, Bhat N, Nayak SS, et al. Anatomical variations in the cutaneous innervation on the dorsum of the foot. Anat Cell Biol. 2019;52:34–37. doi: 10.5115/acb.2019.52.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]


