Abstract
Purpose
Cervical cancer is a significant global health burden, with advancements in treatment modalities improving outcomes. However, vaginal toxicities following definitive chemoradiation remain a concern, impacting patients’ quality of life. The aim of this systematic review and meta-analysis was to estimate the incidence of vaginal toxicities, explore associated factors, and assess the relationship with radiation dose in intact cervical cancer patients undergoing radical chemoradiation.
Material and methods
A systematic search of PubMed, Google Scholar, and Cochrane databases was conducted. Studies reporting on vaginal toxicities post-radical chemoradiation in intact cervical cancer patients were included. Data extraction and analysis were performed according to PRISMA guidelines.
Results
Twenty-four studies with various designs were included. The meta-analysis revealed a pooled estimate of 39% (95% CI: 21-56%) for overall vaginal toxicities among cervical cancer patients following definitive chemoradiation. Vaginal stenosis was the most commonly reported toxicity, with a median incidence of 61.5% (range, 20-77.8%) across the studies. Severe toxicities (grade ≥ 3) were reported at rates of 12.74% (CTCAE v. 4.0), 0.98% (CTCAE v. 3.0), 10.41% (RTOG/EORTC), and 0% (LENT-SOMA). Factors, such as age, initial vaginal involvement, and radiation dose were associated with increased toxicity risk. Significant heterogeneity was observed in study populations and methodologies.
Conclusions
Vaginal toxicities are common following definitive chemoradiation in intact cervical cancer patients, with vaginal stenosis being predominant. Standardization of toxicity scoring methods and radiotherapy dose reporting parameters is crucial for accurate comparison and interpretation of findings. Future research should focus on optimizing treatment strategies to minimize vaginal toxicities while maximizing efficacy and patient outcomes.
Keywords: incidence, late toxicities, cancer cervix, chemoradiation, vaginal toxicities, vaginal stenosis, vaginal shortening, radical, definitive
Purpose
Cervical cancer is the fourth most common cancer among females globally, with approximately 662,301 new cases reported annually (GLOBOCAN 2022) [1]. Despite a declining trend worldwide, it remains a significant cause of morbidity and mortality, especially in low- and middle-income countries (LMICs) [2].
Advancements in treatment modalities over the past two decades have improved outcomes in cervical cancer, including enhanced survival rates and reduced toxicities. Radiation therapy (RT) has evolved from two-dimensional (2D) to three-dimensional (3D), encompassing external beam radiation therapy (EBRT) and brachytherapy (BT) [3]. Image-based adaptive BT, incorporating volume-based target delineation and dose prescription, aims to tailor treatment to individual tumor responses and minimize radiation doses to organs at risk (OARs), thereby reducing toxicities [4].
Traditionally, RT planning has considered doses to OARs, such as the rectum and urinary bladder [5]. Recently, the vagina has emerged as a critical OAR, with vaginal toxicities potentially impacting patients’ quality of life, particularly sexual function. Recto-vaginal point (ICRU rectal point) has been investigated as a dose-limiting point for vaginal toxicities [6]. The concept of posterior-inferior border of symphysis (PIBS) points has been introduced to define dose constraints for the vagina and mitigate toxicities to this organ [7].
The incidence of vaginal toxicities following definitive chemoradiation in cases of intact cervical cancer has been sparingly reported in the literature, with varied results. Therefore, the aim of the current systematic review was to address this knowledge gap, providing researchers with insights into radiation-induced toxicities in this vital organ for future studies.
Material and methods
Our review protocol was registered with Prospero, an international prospective register of systematic reviews (CRD42023396673) [8], and the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist 2020 guided our protocol development and review conduct [9, 10]. Institutional ethical review was not required, as patients’ identifiers were not disclosed. The primary objective was to estimate the incidence of vaginal toxicities following radical concomitant chemoradiation, with the end-point being the percentage of patients reporting any form or grade of vaginal toxicity. Secondary objectives included estimating the radiation tolerance dose to the vagina, and exploring associations between vaginal toxicities and other factors observed in individual studies.
Study selection
All studies, except for reviews, book chapters, systematic reviews, and meta-analyses, conducted on intact uterine cervical cancer patients post-radical chemoradiation reporting vaginal toxicities were included. Only English language full-text publications till the date of review were included.
Studies on post-operative cases or those undergoing surgery at any time during management were excluded. Also, studies omitting intra-cavitary radiation therapy (ICRT), or with transperineal implant/template brachytherapy were excluded. Other exclusion criteria were use of non-platinum chemotherapy agents or prior pelvic radiotherapy.
Search methodology
PubMed, Google Scholar, and Cochrane databases search using the following key words: “Vaginal Toxicity”, “Cancer Cervix”, “Radiotherapy”, “Vagina”, and “Tolerance”, was conducted. The searched references were imported to Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org) using Zotero reference manager. Careful screening by reading the title and abstract was done by two reviewers independently. Full texts were retrieved, and any unavailable texts were manually searched through journal websites or free retrieval sources. In studies with incomplete reporting of vaginal toxicities or RT doses to the organ, the corresponding authors were contacted via e-mail for additional inputs for the review.
Data extraction
Data were independently extracted by two reviewers and synthesized under pre-defined headings, including study characteristics, population, RT treatment details, toxicity criteria, vaginal toxicities, associated factors, and timing of toxicity recording. In case of any discrepancy, there was a discussion to reach a consensus, which was considered final. Data were tabulated and presented descriptively.
Statistical analysis
All statistical analyses were performed using Jamovi Project (version 2.3), with two-tailed p-values ≤ 0.05 considered significant. DerSimonian and Laird random effects models estimated pooled proportions of vaginal toxicities, and forest plots depicted individual and pooled effects of studies. Heterogeneity was assessed using Cochran Q, τ2, and I2 statistics. Publication bias was evaluated with fail-safe N analysis, Kendall’s tau rank correlation test, and regression test, with a funnel plot indicating bias presence.
Quality assessment
Risk of bias for incomplete outcome data was evaluated using Covidence software’s risk of bias assessment tool. Studies were categorized as high, low, or unsure risk based on outcome data completeness.
Results
Study search and characteristics
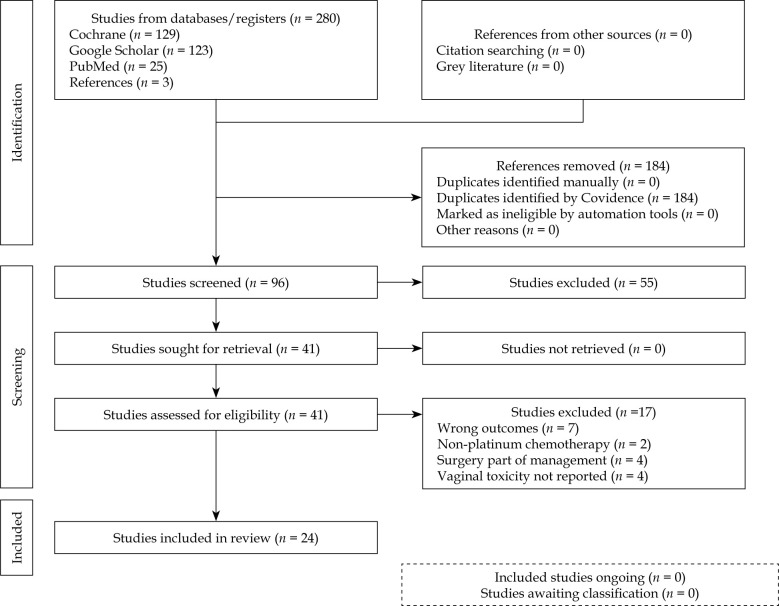
A total of 280 studies were retrieved, of which 24 were included after assessment. Thirteen were retrospective, eight prospective, two randomized controlled trials, and one qualitative research. The entire process is depicted in PRISMA flowchart (Figure 1).
Fig. 1.
PRISMA flowchart
Patient characteristics and treatment details
The included studies encompassed stage IB to IVB cervical cancer patients treated with external beam radiation therapy (chemoradiation), followed by intra-cavitary brachytherapy. Table 1 summarizes treatment details.
Table 1.
Patient characteristics and treatment details of included studies
| Study | Country | Study design | Population | No. of patients | Vaginal extension | EBRT dose | BT dose/EQD2 |
|---|---|---|---|---|---|---|---|
| Kirchheiner 2014 [16] | Austria | Prospective observational (EMBRACE) | IB to IVB | 588 | Upper 1/3: 236/588 (40%) Lower 2/3: 30/588 (5%) |
45-50 Gy in 1.8-2.0 Gy/fx. | – |
| Kirchheiner 2016 [6] | UK | Prospective (EMBRACE sub-study) | IB to IVB | 630 | Upper 1/3: 260/630 (41%) Middle 1/3: 19/630 (3%) Lower 1/3: 13/630 (2%) |
45 Gy (IQR, 45-46) | Median HR-CTV D90 EQD2 (Gy): 90 (IQR: 86-94) |
| Westerveld 2022 [17] | UK | Retrospective (sub-study of EMBRACE I study) | IB to IVA | 301 | Upper 1/3: 109/301 (36%) Lower 2/3: 17/301 (6%) |
45-50 Gy in 1.67 to 2.0 Gy/fx. with weekly cisplatin of 40 mg/m2 |
– |
| Kumar 2016 [11] | India | Prospective randomized | IIB to IIIB | 37 | – | 50.4 Gy in 28 fx. Inj. weekly cisplatin of 40 mg/m2 |
EQD2 EBRT and ICRT combined point A: 79.3 Gy HDR arm (7 Gy × 3 fx.), 78.9 Gy PDR arm (27 Gy/1 fx. over 39 hours, 0.7 Gy each) |
| Rai 2014 [21] | India | Prospective | IB2 to IIIB | 35 | Overall: 11/35 (31.4%) | 46 Gy in 23 fx. weekly cisplatin of 40 mg/m2 | 7 Gy × 4 fx. MRI-guided image-based |
| Tharavichitkul 2014 [22] | Thailand | Prospective cohort | IIB to IIIB | 26 | – | 45 Gy | – |
| Murakami 2021 [13] | Japan | Retrospective | IB2 to IVA | 469 | – | – | Median HR-CTV D90 EQD2 (Gy): 66.1 (51-102) low-risk, 67.5 (41.3-97.3) (others) |
| Kaidar- Person 2014 [23] | Israel | Retrospective | IB1 to IIB | 50 | – | 39.6-50.4 Gy | – |
| Gondi 2012 [12] | United States | Retrospective | IB1 to IVA | 374 (total) 179 (CRT arm) | – | 39.6-50.4 Gy | – |
| Okonogi 2022 [24] | Japan | Retrospective | IB3 to IVA | 36 | – | 45-50 Gy | Mean HR-CTV D90 EQD2 (Gy): 74.7 ±9.4 Gy (3D-IGBT) and 74.8 ±7.6 Gy (HBT) |
| Susko 2016 [14] | United States | Retrospective | IB to IIIB | 62 | – | – | – |
| Dankulchai 2022 [25] | Thailand | Retrospective cohort | IB2 to IVA | 97 | Overall: 81 (83.5%) Arm I: 59 (60.8%) Arm II: 22 (22.7%) |
– | – |
| Fidarova 2010 [26] | UK | Retrospective | IB to IV | 34 | – | 45.0-50.4 Gy | 7 Gy × 4 fx. |
| Conway 2020 [27] | Canada | Qualitative research | IB to IVA | 67 | – | Median: 45 Gy | Mean: 28 Gy Mean HR-CTV D90 EQD2 (Gy): 92 ±7 |
| Tse 2016 [28] | UK | Retrospective | – | 100 | – | 45.0-50.4 Gy in 25-28 fx. | Mean HR-CTV D90 EQD2: 88.2 |
| AtaseverAkkas 2021 [29] | Turkey | Retrospective | IA to IIIC2 (FIGO 2018) | 50 | Upper 1/3: 32 (64%) Arm I: 14 (28%) Arm II: 18 (36%) Lower 2/3: 3 (6%) Arm I: 2 (4%) Arm II: 1 (2%) |
Median 45 Gy in 25 fx. (45.0-50.4 Gy) |
7 Gy × 4 fx. Mean HR-CTV D90 EQD2 (Gy): Arm I: 85.58 ±7.32 Arm II: 82.73 ±6.73 |
| Tharavichitkul 2021 [30] | Thailand | Retrospective | IB to IV | 180 | Arm I: 47/92 (51.1%) Arm II: 60/88 (68.2%) | 45.0-50.4 Gy | 6-7 Gy × 4 fx. |
| Brand 2006 [15] | Australia | Retrospective | IB to IVA | 179 | Upper 2/3: 17/179 (9.5%) Lower 1/3: 3/179 (1.7%) |
Mean: 48.3 Gy | Mean: 23.4 Gy |
| Ruanla 2022 [31] | Thailand | Prospective observational | I to IV | 54 | – | – | 6-7 Gy × 4 fx. |
| Misra 2018 [32] | India | Randomized controlled trial | IB to IVA | 156 CTRT (n = 79) |
– | 50 Gy in 25 fx. cisplatin 35 mg/m2 (max, 50 mg) | 6 Gy × 3 fx. |
| Alam 2019 [33] | India | Randomized controlled trial | IIB to IIIB | 72 | – | 50 Gy in 25 fx. | 8 Gy × 3 fx. |
| Sadiq 2020 [34] | Pakistan | Prospective | – | 55 | – | 45 Gy in 25 fx. | 7 Gy × 4 fx. |
| Tharavichitkul 2015 [35] | Thailand | Prospective | IB to IVA | 29 | – | 50 Gy in 25 fx. | 6.5-7.0 × 4 fx. to point A (TAUS-guided) Mean total point A dose: 76 ±10 Gy |
| Saibishkumar 2006 [36] | India | Retrospective | I to IV | 1,069 | – | 35-46 Gy in 15-23 fx. | HDR: 9 Gy × 2 fx. LDR: 35-40 Gy LDR equivalent (1-2 sessions) Median total point A dose: 81 (46-91) Gy |
EMBRACE – image-guided intensity-modulated external beam radiochemotherapy and MRI-based adaptive brachytherapy in locally advanced cervical cancer, EBRT – external beam radiotherapy, BT – brachytherapy, EQD2 – equieffective dose at 2 Gy per fraction, HR-CTV D90 – high-risk clinical target volume dose to 90%, ICRT – intra-cavitary radiation therapy, HDR – high-dose-rate, LDR – low-dose-rate
Primary and secondary outcomes
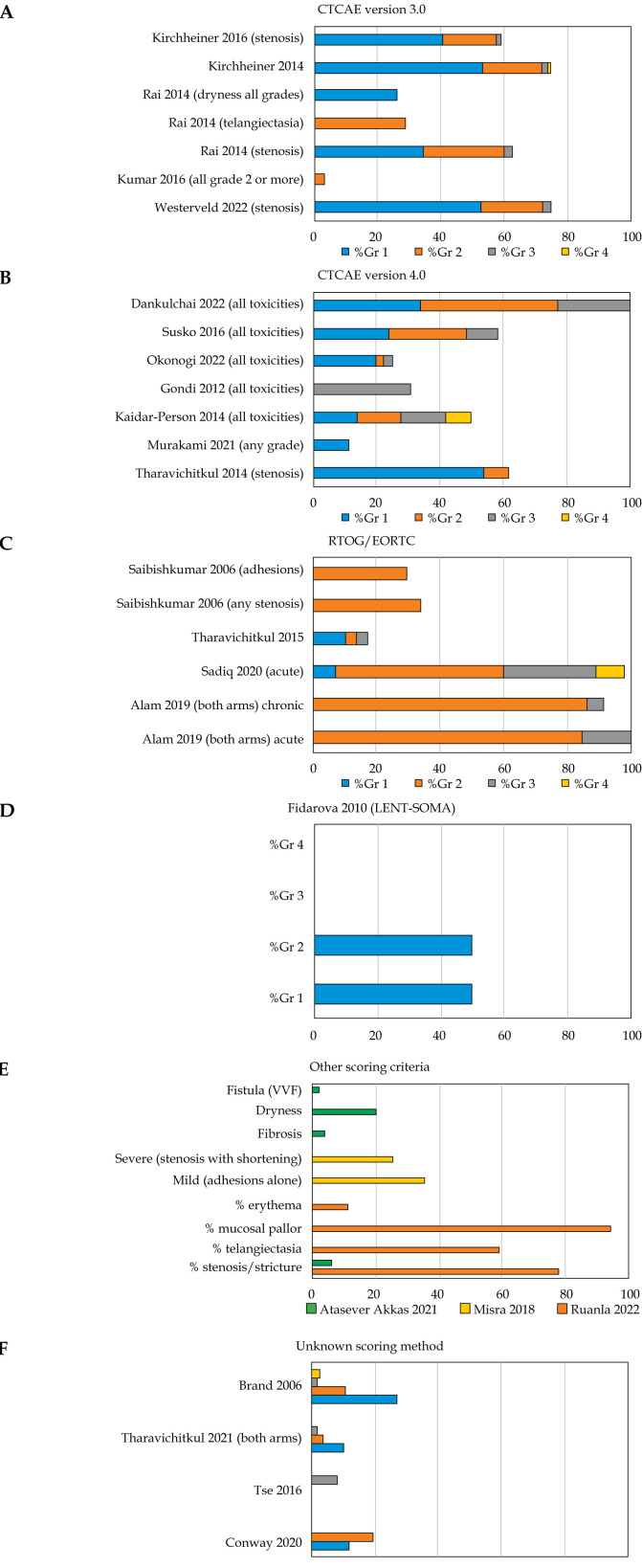
Table 2 illustrates vaginal toxicities, their correlations with radiation doses, and associated factors. Noteworthy was the considerable variability in the incidence of vaginal toxicities across studies, as shown in Figure 2.
Table 2.
Primary and secondary outcomes of the included studies in review
| Study | Vaginal RT doses (Gy) | Follow-up period | Timing of recording toxicities | Grading/scoring criteria | Vaginal toxicities reported, n (%) |
Significant correlation of toxicities with vaginal RT dose (Yes/No) | Associated factors |
|---|---|---|---|---|---|---|---|
| Kirchheiner 2014 | N.A. | 24 months (median, 15 months) | Baseline, First yr.: 3 monthly, Second yr.: 6 monthly |
CTCAE v. 3.0 |
Stenosis: Grade 1 = 256 (43) Grade 2 = 86 (15) Grade 3 = 5 (1) Telangiectasia and bleeding: Grade 1 = 175 (30) Grade 2 = 5 (1) Grade 3 = 1 Vaginal dryness: Grade 1 =244 (42) Grade 2 = 32 (5) Grade 3 = N.A. Mucositis: Grade 1 = 146 (25) Grade 2 = 23 (4) Grade 3 = 3 Grade 4 = 1 Vaginal fistula: Grade 1 = 2 Grade 2 = 0 Grade 3 = 4 (1) Others: 47 (8), 14 (2), 4 (1) Overall: Grade 1 = 309 (53) Grade 2 = 111 (19) Grade 3 = 12 (2) Grade 4 = 1 Actuarial 2 yr. estimate: ≥ grade 3 = 3.6%, ≥ grade 2 = 29%, ≥ grade 1 = 89% |
None | None reported |
| Kirchheiner 2016 | Median RV-Ref point (EQD2 Gy): 64 (IQR, 60-69) |
24 months (IQR, 12-36 months) | – | CTCAE v. 3.0 |
Stenosis: Grade 0 = 259 (41) Grade 1 = 255 (41) Grade 2 = 108 (17) Grade 3 = 8 (1) |
Yes | For grade 2 stenosis: 1. Initial vaginal extension 2. EBRT dose 3. Total EBRT and BT RV-Ref point dose |
| Westerveld 2022 | PIBS+2: 52.9 (IQR, 49.3-64.7) PIBS: 41.0 (IQR, 15.4-49.0) PIBS-2: 4.1 (IQR, 2.9-7.0) RV-RP: 64.6 (IQR, 60.0-70.6) |
49 months (median) | – | CTCAE v. 3.0 |
Stenosis: Grade 1 = 158 (52) Grade 2 = 59 (20) Grade 3 = 8 (3) Actuarial estimate for ≥ grade 2 stenosis: 3 yrs. = 24 5 yrs. = 26 |
Yes | Grade 2 stenosis significantly associated with: 1. Higher age 2. Vaginal involvement 3. Shorter VRL 4. TO (c/f TR applicator) 5. All vaginal dose points, except for PIBS+2 cm EBRT; inversely associated with higher VL at 5 mm point |
| Kumar 2016 | N.A. | 34 months (HDR), 29 months (PDR) |
90 days after RT completion till the last follow-up | CTCAE v. 3.0 |
All ≥ grade 2: HDR arm = 0 PDR arm = 1 (5.6) |
– | – |
| Rai 2014 | D2cc: 162.9 ±23.1 D1cc: 242.5 ±50.5 D0.1cc: 492.4 ±111.4 D5cc: 90.02 ±8.89 |
– | – | CTCAE v. 3.0 |
Shortening: 22 (62.8) Grade 1 = 12 (34.2) Grade 2 = 9 (25.7) Grade 3 = 1 (2.8) Telangiectasia: 10 (28.5) Dryness: 9 (25.7) Grade 1 = 9 (25.7) Grade 2 = 0 (0) Grade 3 = 0 (0) |
No | – |
| Tharavichitkul 2014 | Cumulative VR dose (EQD2): Point-based = 119.4 ±19.3 Vol-based = 101.5 ±18.4 (p < 0.001) Cumulative VL dose EQD2): Point-based = 117.5 ±18.8 Vol-based = 98.2 ±18.0 (p < 0.001) Maximal vaginal-point dose (EQD2): Point-based = 121.6 ±19.8 Vol-based: 101.1 ±19.4 (p < 0.001) |
22 months | 90 days after RT completion | CTCAE v. 4.0 |
Stenosis: Grade 0 = 10 (38.5) Grade 1 = 14 (53.8) Grade 2 = 2 (7.7) Grade 3 = 0 (0) |
No | – |
| Murakami 2021 | N.A. | – | – | CTCAE v. 4.0 |
Total ≥ grade 1 = 53 (11) | – | – |
| Kaidar- Person 2014 | Maximal surface HDR BT dose = 103 Lateral surface dose = 70 |
59 months (median) | – | CTCAE v. 4.0 |
All: Grade 1 = 7 (28) Grade 2 = 7 (28) Grade 3 = 7 (28) Grade 4 = 4 (16) |
No | – |
| Gondi 2012 | N.A. | 35.5 months (median) | ≥ 6 months follow-up | CTCAE v. 4.0 |
All grade 3 = 55 (30.7%) (CRT arm) |
– | Vaginal severe late toxicity associated with: 1. Moderate and poor dilator compliance (c/f high dilator compliance) 2. Age > 50 yrs. |
| Okonogi 2022 | N.A. | 39 months (median) |
– | CTCAE v. 4.0 |
All: Grade 1 = 7 (19.4) Grade 2 = 1 (2.8) Grade 3 = 1 (2.8) |
– | – |
| Susko 2016 | D2cc: 100.5 (IQR, 86.8-108.4) D1cc: 112.59 (IQR, 96.7-124.6) D0.1cc: 157.91 (134.4-196.5) D5cc: 81.68 (IQR, 74.3-91.1) D10cc: 68.98 (IQR, 61.8-76.4) |
12 months (median) | ≥ 30 days after completion of RT | CTCAE v. 4.0 |
All: Grade 1 = 15 (24.2) Grade 2 = 15 (24.2) Grade 3 = 6 (9.7) |
Yes | Significant association ≥ grade 2 vaginal toxicities – 1. Vaginal D2cc |
| Dankulchai 2022 | D2cc: 148.2 (125.7-181.4) D1cc: 191 (IQR, 154.1-243.0) D0.1cc: 359 (IQR, 280.6-601.8) D: 112.0 (99.1-139.8) D+5: 78.1 (72.5-87.7) L: 275.6 (167.2-534.3) L+5: 99.1 (88.2-125.2) R: 250.8 (151.6-519.2) R+5: 95.5 (84.6-117.0) V: 86.8 (78.2-101.8) V+5: 69.2 (64.9-74.7) PIB-2: 40.2 (9.4-52.4) PIBS: 51.9 (47.5-57.8) PIBS+2: 68.9 (58.8-128.5) |
20 months (median) | – | CTCAE v. 4.03 |
All: Grade 1 = 33 (34.0) Grade 2 = 42 (43.3) Grade 3 = 22 (22.7) |
Yes | Patient factors: Age, initial tumor size, initial vaginal involvement Dosimetric factors: PIBS+2, PIBS, PIBS-2, R+5, R and L vaginal doses; no association with use of vaginal dilatator or frequency of sexual intercourses |
| Fidarova 2010 | D2cc: 4 × 9.2 ±2.6 D1cc: 4 × 12.9 ±3.9 D0.1cc: 4 × 26.3 ±9.8 |
3-29 months | – | LENT- SOMA | All grade 1 = 17 (50) All grade 2 = 17 (50) Shortening: 22 (64.7) Telangiectasia: 30 (88.23) |
No | – |
| Conway 2020 | N.A. | 46 months (median) | – | Not clear | All: Grade 1 = 8 (11.9) Grade 2 = 13 (19.4) |
– | – |
| Tse 2016 | N.A. | 26.7 months (median) | – | Not clear | All: Grade 3 = 8 |
– | – |
| Atasever Akkas 2021 | Average fraction vaginal dose (Gy): TO arm: Upper = 1023.53 ±244.63 Middle = 372.97 ±203.51 Lower = 118.96 ±88.01 TR arm: Upper = 806.52 ±408.75 Middle = 197.14 ±114.50 Lower = 74.50 ±46.06 |
Median: 51.6 months (TO), 30.7 months (TR) |
– | Not clear | Fibrosis: 2 (4) Stricture: TO arm = 2 (4) TR arm = 1 (2) Dryness: TO arm = 10 (20) TR arm = 4 (8) VVF = 1 (2) |
– | Vaginal toxicities lesser in TR applicator use |
| Tharavichitkul 2021 | N.A. | Mean: 32 months | – | Not clear | All: Arm I: Grade 1 = 5 (5.4) Grade 2 = 1 (1.1) Grade 3 = 2 (2.2); Arm II: Grade 1 = 13 (14.8) Grade 2 = 5 (5.7) Grade 3 = 1 (1.1) |
– | Vaginal toxicities more in TAUS group |
| Brand 2006 | N.A. | – | – | Not clear (own) | All: Grade 1 = 48 (27) Grade 2 = 19 (11) Grade 3 = 3 (1.7) Grade 4 = 4 (2.3) |
– | Age > 50 years |
| Ruanla 2022 | Median (IQR) RV Pt: 67.73 Gy (IQR, 64.17-71.27) Mean vaginal surface dose: 152.83 (IQR, 114.7-3.9.2) Mean vaginal dose at 5 mm (Rt/Lt): 82.81 (IQR, 71.02-95.53) PIBS: 51.92 (50.34-54.33) PIBS+2: 67.23 (56.44-157.31) PIBS-2: 51.3 (50.87-51.72) |
18.5 months | 1 year follow-up | Others (modified Dische score) | Stenosis: 42 (77.8) Grade 1 = 29 Grade 2 = 13 Telangiectasia: 32 (59.2) Grade 1 = 24 Grade 2 = 8 Mucosal pallor: 51 (94.4) Grade 1 = 19 Grade 2 = 28 Grade 3 = 4 Erythema: Grade 1 = 6 (11.1) |
Yes | Association found with: 1. Age > 68.5 years 2. Point-based doses, such as mean dose lat 5 mm vagina, PIBS-2 cm; no association with volume-based parameters |
| Misra 2018 | N.A. | – | ≥ 90 days after initiation of RT | Other | All (CTRT arm): Mild = 28/79 (35.4) Severe = 20/79 (25.3) |
– | Bulky disease (p = 0.016) and vaginal involvement (p = 0.020) predicted greater incidence of grade 2 vaginal toxicity |
| Alam 2019 | N.A. | 3-18 months | – | RTOG/EORTC | Acute: Arm I (inter-digitated): Grades 1, 2 = 29 (82.9) Grade 3 = 6 (17.1) Arm II (sequential): Grades 1, 2 = 32 (86.5) Grade 3 = 5 (13.5) Late: Arm I: Grades 1, 2 = 33 (94.3) Grade 3 = 2 (5.7) Arm II: Grades 1, 2 = 35 (94.6) Grade 3 = 2 (5.4) |
– | – |
| Sadiq 2020 | N.A. | – | D1 to D90 of initiation of RT | RTOG/EORTC | Acute: Grade 1 = 4 (7.3) Grade 2 = 29 (52.7) Grade 3 = 16 (29.1) Grade 4 = 5 (9.1) |
– | No difference with age |
| Tharavichitkul 2015 | N.A. | 19 months (median) | – | RTOG/EORTC | All: Grade 1 = 3 (10.3) Grade 2 = 1 (3.4) Grade 3 = 1 (3.4) |
– | – |
| Saibishkumar 2006 | N.A. | 34 months (median) | – | RTOG/EORTC | Stenosis: 362 (33.9) Adhesions without stenosis: 316 (29.6) |
– | – |
CTCAE – common terminology criteria for adverse events, EBRT – external beam radiation therapy, BT – brachytherapy, RV-Ref point – recto-vaginal reference point, IQR – interquartile range, PIBS – posterior inferior border of symphysis pubis, VRL – vaginal reference length, TO – tandem ovoid, TR – tandem ring, HDR – high-dose-rate, PDR – pulsed-dose-rate; VLat 5 mm – vaginal dose at 5 mm lateral distance, D2cc – RT dose to 2 cc volume, D5cc – RT dose to 5 cc volume, D1cc – RT dose to 1 cc volume, D0.1cc – RT dose to 0.1 cc volume, EQD2 – equieffective dose at 2 Gy per fraction
Fig. 2.
Incidence (%) of vaginal toxicities based on different scoring criteria
– Grade: The mean incidence of grade 3 or higher toxicities was 12.74% (common toxicity criteria of adverse events, CTCAE version 4.0), 0.98% (CTCAE version 3.0), 10.41% (Radiation Therapy Oncology Group [RTOG] and European Organization for Research and Treatment of Cancer [EORTC]-RTOG/EORTC), and 0% (late effects normal tissue task force [LENT]-subjective, objective, management, analytic [LENT-SOMA]).
– Type: Vaginal stenosis was the most commonly reported condition, appearing in 9 out of 24 studies, with a median incidence of 61.5% (range, 20-77.8%) (different scoring criteria) (Figure 3). Most studies reported vaginal toxicities without specifying the type. The second most common reported toxicity was telangiectasia/bleeding (Table 2).
Fig. 3.
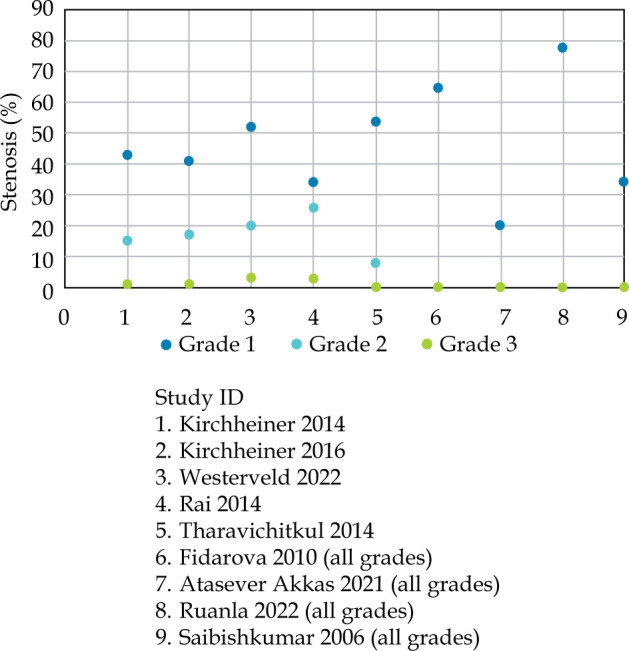
Incidence of vaginal stenosis reported in 9/24 studies
Incidence of vaginal toxicities
Among the studies reviewed, the incidence of vaginal toxicities varied depending on the grading criteria used. Kumar et al. reported only one patient with grade 2 or higher vaginal toxicity out of 37 patients treated with high-dose-rate (HDR) or pulsed-dose-rate (PDR) [11]. Conversely, Gondi et al. observed 30.7% severe late vaginal toxicity (grade 3 or higher, CTCAE v. 4.0) in their study cohort [12]. Murakami et al. reported an 11% incidence of grade 1 or higher vaginal toxicities out of 469 patients [13]. Susko et al. found that 58.06% of patients experienced sub-acute to late toxicities in their retrospective study that included both cervical and uterine cancer cases [14].
The variability in reported incidence can be attributed, in part, to differences in toxicity scoring criteria among studies. Various objective grading systems for vaginal toxicities were employed, including CTCAE (different versions) and institutional criteria. Notably, CTCAE v. 4.0 was the most commonly used toxicity scoring criteria, followed by CTCAE v. 3.0, RTOG/EORTC, and LENT-SOMA. This variation underscores the need for standardization in toxicity scoring methods to facilitate meaningful comparisons across studies.
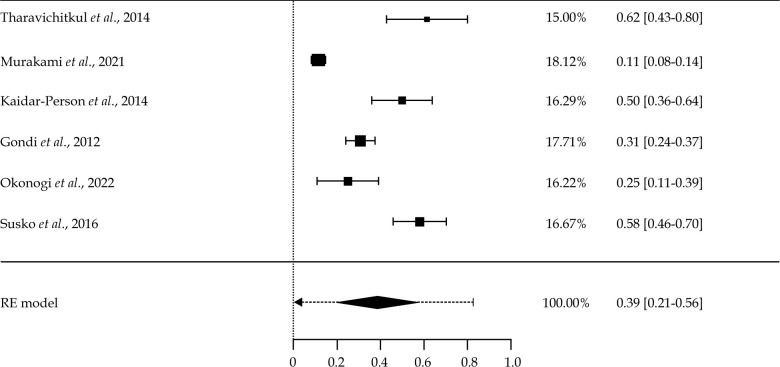
Out of the 24 articles reviewed, only six studies were assessed to estimate the pooled proportion of overall vaginal toxicities. All of these studies used the same toxicity scoring criteria, i.e., CTCAE v. 4. One study (Dankulchai 2022) using the same criteria had to be excluded due to potential data skewness (100% toxicities reported). Of these six studies, five (83%) were retrospective and one (17%) was prospective in nature. Given the significant heterogeneity in study populations and sizes, DerSimonian and Laird random effects (RE) model was utilized for the analysis.
A meta-analysis was conducted to estimate the incidence of overall vaginal toxicities among women. Individual estimates of toxicity proportion in each study and a pooled incidence estimate of toxicity are presented in Figure 4. The overall pooled estimate of vaginal toxicity proportion was 39% (95% confidence interval [CI]: 21-56%). The predictive interval ranged from 8% to 81%. High statistically significant heterogeneity was observed (Tau2 = 0.025, I2 = 95.75%, p < 0.001), indicating heterogeneity in the studies. The reasons for high heterogeneity may include differences in population, sample size, and types of epidemiological studies.
Fig. 4.
Forest plot showing incidence of overall vaginal toxicities among selected six studies and a pooled estimate
Timing of recording toxicities
The timing of recording vaginal toxicities varied among the studies, with majority focusing on late toxicities. However, there was inconsistency in reporting the specific timing of toxicity assessments. Notably, studies segregated based on reporting criteria also exhibited differences in follow-up intervals and timing of toxicity assessments, contributing to heterogeneity in reported outcomes.
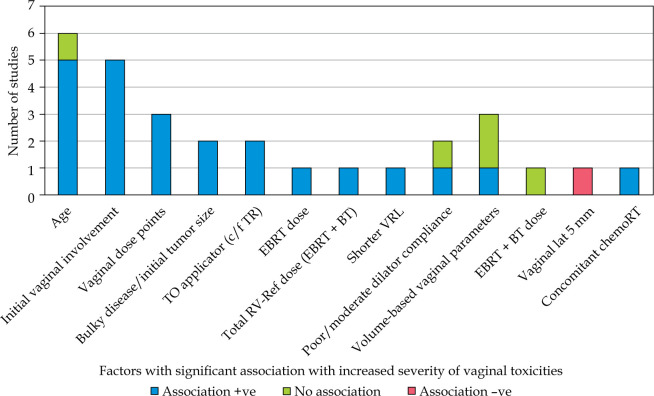
Factors associated with vaginal toxicities
Several factors were identified as potentially influencing the severity and incidence of vaginal toxicities (Figure 5). Age and initial vaginal involvement by disease were found to be significantly associated with increased vaginal toxicities in a subset of studies. Brand et al. noted that vaginal stenosis most commonly developed within the first year post-treatment [15]. Additionally, factors, such as the use of vaginal dilators, concurrent chemotherapy, and specific treatment modalities (e.g., type of brachytherapy applicators) were found to impact vaginal toxicity outcomes in various studies.
Fig. 5.
Factors associated with increased severity of vaginal toxicities
Relationship with radiation dose
Five studies included in the review demonstrated a significant correlation between vaginal radiation doses and toxicities (Table 2). Kirchheiner et al. observed a significant association between grade 2 vaginal stenosis and total EBRT and BT RV-Ref dose point in their study cohort [16]. Westerveld et al. similarly found associations between grade 2 vaginal stenosis and various vaginal dose points, with inverse associations observed for certain dose points [17]. Other studies reported associations between vaginal toxicities and point-based vaginal dose parameters, such as D2cc vaginal dose. However, the correlation between vaginal dose volume parameters and toxicity outcomes was not consistent across all the studies (Table 2).
Bias assessment
Publication bias assessment indicated minimal bias, with fail-safe N analysis, Kendall’s tau rank correlation test, and regression test, yielding no significant evidence of bias (Figure 6). However, it is essential to acknowledge potential sources of bias beyond publication bias, which could impact study outcome. Risk of bias was found to be low for majority (19/24) of the studies reviewed.
Fig. 6.
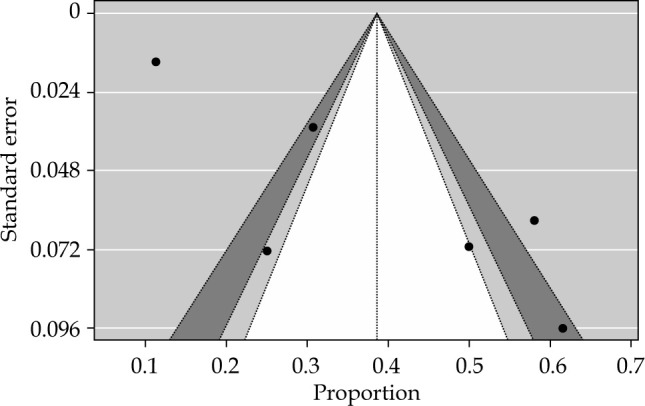
Funnel plot for publication bias
Discussion
Incidence of vaginal toxicities
The meta-analysis revealed a pooled estimate of 39% for the overall incidence of vaginal toxicities (CTCAE v. 4) among cervical cancer patients following definitive chemoradiotherapy. Vaginal stenosis emerged as the most commonly reported toxicity, affecting approximately one-third of all the studies. Notably, severe toxicities (grade 2 or higher) were generally reported at low rates across the studies, regardless of toxicity scoring criteria employed.
The variation in reported incidence rates underscores the importance of standardized toxicity scoring methods to facilitate accurate comparisons and interpretation of study findings. Recently, an Italian survey resulted in wide variation concerning recording and treating vaginal toxicities after chemoradiation, highlighting the need for guidelines in contouring and vaginal RT dose reporting [18]. Additionally, the use of novel approaches, such as the time-weighted adverse event reporting system, may provide valuable insights into temporal trends of toxicities and their impact on quality of life.
Timing of recording toxicities
The lack of uniformity in recording the timing of vaginal toxicities poses a challenge in interpreting study results and comparing outcomes across the studies. While majority of the studies focused on late toxicities, variations in follow-up intervals and timing of toxicity assessments contribute to heterogeneity in reported outcomes. Standardization of reporting protocols for timing of toxicity assessments would enhance the reliability and comparability of study findings. Though not qualified to be included in this review, a recent publication by Chopra et al., a post-hoc analysis of adverse events in PARCER trial on post-operative patients, a newly developed time-weighted adverse event reporting system is worth mentioning here. Instead of a snapshot of worst adverse toxicity grade, MOSES provides temporal trends of toxicity, which gives more valuable inputs to assess quality of life (QoL) [19, 20].
Factors associated with vaginal toxicities
Age and initial vaginal involvement by disease emerged as significant factors associated with increased severity and incidence of vaginal toxicities in several studies. The use of vaginal dilators, concurrent chemotherapy, and specific treatment modalities were also found to influence toxicity outcomes. These findings underscore the importance of considering patient-related and treatment-related factors in assessing and managing vaginal toxicities following chemoradiotherapy.
Relationship with radiation dose
The correlation between vaginal radiation doses and toxicities was evident in multiple studies in this analysis, with various dose points and parameters showing associations with toxicity outcomes. However, inconsistencies in reporting and variability in dose calculation methodologies highlight the need for standardized approaches in dose reporting and evaluation. Further research is warranted to elucidate the optimal dose-volume parameters and treatment strategies to minimize vaginal toxicities while optimizing treatment efficacy.
Limitations
Several limitations should be acknowledged in interpreting the findings of this review. Firstly, the retrospective design of majority of included studies introduces inherent biases and limitations in data collection and analysis. Additionally, the heterogeneity in dose reporting parameters and toxicity scoring criteria across the studies limits the comparability and generalizability of findings. Moreover, the lack of uniformity in recording the timing of toxicity assessments further complicates the interpretation of studies’ results.
Conclusions
In conclusion, this systematic review and meta-analysis provide valuable insights into the incidence and factors associated with vaginal toxicities following definitive chemoradiotherapy in cervical cancer patients. In our analysis, the pooled estimate of incidence of overall vaginal toxicities (CTCAE v. 4) was 39% among cancer cervix cases following definitive chemoradiotherapy. Vaginal stenosis is the most commonly reported toxicity (around one-third of all studies). Severe toxicities (grade 3 or more) are reported to be low in most studies, irrespective of toxicity scoring criteria. Factors, such as age, initial vaginal involvement, vaginal dose points are reported to be associated with vaginal toxicities. Standardization of toxicity scoring methods and dose reporting parameters is essential to facilitate accurate comparisons and interpretation of the studies’ findings. Future research efforts should focus on elucidating optimal treatment strategies to minimize vaginal toxicities while maximizing treatment efficacy and patient outcomes.
Footnotes
The authors report no conflict of interest.
Funding
This research received no external funding.
Disclosures
Approval of the Bioethics Committee was not required.
References
- 1.International Agency for Research on Cancer . Available online at: https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf (last accessed: June 10th 2024).
- 2.Singh D, Vignat J, Lorenzoni Vet al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health 2023; 11: E197-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sagae S, Toita T, Matsuura Met al. Improvement in radiation techniques for locally advanced cervical cancer during the last two decades. Int J Gynecol Cancer 2023; 33: 1295-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sturdza AE, Knoth J. Image-guided brachytherapy in cervical cancer including fractionation. Int J Gynecol Cancer 2022; 32: 273-280. [DOI] [PubMed] [Google Scholar]
- 5.Georg P, Potter R, Georg Det al. Dose effect relationship for late side effects of the rectum and urinary bladder in magnetic resonance image-guided adaptive cervix cancer brachytherapy. Int J Radiat Oncol Biol Phys 2012; 82: 653-657. [DOI] [PubMed] [Google Scholar]
- 6.Kirchheiner K, Nout RA, Lindegaard JCet al. Dose-effect relationship and risk factors for vaginal stenosis after definitive radio(chemo)therapy with image-guided brachytherapy for locally advanced cervical cancer in the EMBRACE study. Radiother Oncol 2016; 118: 160-166. [DOI] [PubMed] [Google Scholar]
- 7.Westerveld H, Pötter R, Berger Det al. Vaginal dose point reporting in cervical cancer patients treated with combined 2D/3D external beam radiotherapy and 2D/3D brachytherapy. Radiother Oncol 2013; 107: 99-105. [DOI] [PubMed] [Google Scholar]
- 8.Raj S, Prasad RR, Swati. Incidence of vaginal toxicities in definitive chemoradiotherapy in cancer of intact cervix: A systematic review. PROSPERO 2023, CRD42023396673. Available online at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023396673 (last accessed June 10th 2024).
- 9.Page MJ, McKenzie JE, Bossuyt PMet al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.PRISMA 2020 Checklist. Available online at: https://static1.squarespace.com/static/65b880e13b6ca75573dfe217/t/65d81881d8a48075f1fa7a3a/1708660865607/PRISMA_2020_checklist.pdf (last accessed June 10th 2024).
- 11.Kumar P, Sharma DN, Kumar Set al. Pulsed-dose-rate vs. high-dose-rate intracavitary radiotherapy for locally advanced carcinoma of cervix: A prospective randomized study. Brachytherapy 2016; 15: 327-332. [DOI] [PubMed] [Google Scholar]
- 12.Gondi V, Bentzen SM, Sklenar KLet al. Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: An inter-era analysis. Int J Radiat Oncol Biol Phys 2012; 84: 973-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murakami N, Ando K, Murata Met al. Why not de-intensification for uterine cervical cancer? Gynecol Oncol 2021; 163: 105-109. [DOI] [PubMed] [Google Scholar]
- 14.Susko M, Craciunescu O, Meltsner Set al. Vaginal dose is associated with toxicity in image guided tandem ring or ovoid-based brachytherapy. Int J Radiat Oncol Biol Phys 2016; 94: 1099-1105. [DOI] [PubMed] [Google Scholar]
- 15.Brand AH, Bull CA, Cakir B. Vaginal stenosis in patients treated with radiotherapy for carcinoma of the cervix. Int J Gynecol Cancer 2006; 16: 288-293. [DOI] [PubMed] [Google Scholar]
- 16.Kirchheiner K, Nout RA, Tanderup Ket al. Manifestation pattern of early-late vaginal morbidity after definitive radiation (chemo)therapy and image-guided adaptive brachytherapy for locally advanced cervical cancer: An analysis from the EMBRACE study. Int J Radiation Oncol Biol Phys 2014; 89: 88e95. [DOI] [PubMed] [Google Scholar]
- 17.Westerveld H, Kirchheiner K, Nout RAet al. Dose-effect relationship between vaginal dose points and vaginal stenosis in cervical cancer: An EMBRACE-I sub-study. Radiother Oncol 2022; 168: 8-15. [DOI] [PubMed] [Google Scholar]
- 18.De Felice F, Vicenzi L, Macchia Get al. Vaginal toxicity management in patients with locally advanced cervical cancer following exclusive chemoradiation-a nationwide survey on knowledge and attitudes by the Italian Association of Radiotherapy and Clinical Oncology (AIRO) Gynecology Study Group. Medicina (Kaunas) 2023; 59: 385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chopra S, Gupta S, Kannan Set al. Late toxicity after adjuvant conventional radiation versus image-guided intensity-modulated radiotherapy for cervical cancer (PARCER): A randomized controlled trial. J Clin Oncol 2021; 39: 3682-3692. [DOI] [PubMed] [Google Scholar]
- 20.Ranjan N, Chopra S, Mangaj Aet al. Months and severity score (MOSES) in a phase III trial (PARCER): A new comprehensive method for reporting adverse events in oncology clinical trials. eClinicalMedicine 2022; 47: 101390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rai B, Dhanireddy B, Patel FDet al. Vaginal dose, toxicity and sexual outcomes in patients of cervical cancer undergoing image based brachytherapy. Asian Pac J Cancer Prev 2014; 15: 3619-3623. [DOI] [PubMed] [Google Scholar]
- 22.Tharavichitkul E, Jayavasti R, Galalae RMet al. The associations for vaginal point doses of vaginal stenosis in image-guided brachytherapy. J Cancer Ther 2014; 2014. [Google Scholar]
- 23.Kaidar-Person O, Abdah-Bortnyak R, Amit Aet al. Tolerance of the vaginal vault to high-dose rate brachytherapy and concomitant chemo-pelvic irradiation: Long-term perspective. Rep Pract Oncol Radiother 2014; 19: 56-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okonogi N, Murakami N, Ando Ket al. An Asian multi-national, multi-institutional, retrospective study on image-guided brachytherapy in cervical adenocarcinoma and adenosquamous carcinoma. J Contemp Brachytherapy 2022; 14: 311-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dankulchai P, Harn-Utairasmee P, Prasartseree Tet al. Vaginal 11-point and volumetric dose related to late vaginal complications in patients with cervical cancer treated with external beam radiotherapy and image-guided adaptive brachytherapy. Radiother Oncol 2022; 174: 77-86. [DOI] [PubMed] [Google Scholar]
- 26.Fidarova EF, Burger D, Schussler Set al. Dose volume parameter D2cc does not correlate with vaginal side effects in individual patients with cervical cancer treated within a defined treatment protocol with very high brachytherapy doses. Radiother Oncol 2010; 97: 76-79. [DOI] [PubMed] [Google Scholar]
- 27.Conway JL, Felder S, Tang Jet al. Long-term patient-reported distress in locally advanced cervical cancer patients treated with definitive chemoradiation. Clin Transl Radiat Oncol 2020; 23: 1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tse V, Shiarli AM, Aldridge Set al. A review of practice and outcomes of external beam radiotherapy treatment with concurrent chemotherapy followed by MRI-assisted intracavitary brachytherapy for locally advanced cervix cancer. Brachytherapy 2016; 15: S93. [Google Scholar]
- 29.Atasever Akkas E, Altundag MB. Long-term clinical outcome and dosimetric comparison of tandem and ring versus tandem and ovoids intracavitary application in cervical cancer. J BUON 2021; 26: 698-706. [PubMed] [Google Scholar]
- 30.Tharavichitkul E, Muangwong P, Chakrabandhu Set al. Comparison of clinical outcomes achieved with image-guided adaptive brachytherapy for cervix cancer using CT or transabdominal ultrasound. Brachytherapy 2021; 20: 543-549. [DOI] [PubMed] [Google Scholar]
- 31.Ruanla J, Muangwong P, Kittidachanan Ket al. The association of vagina equivalent dose in 2Gy fraction (EQD(2)) to late vagina toxicity in patients of cervical cancer treated with WPRT plus IGABT. Brachytherapy 2022; 21: 658-667. [DOI] [PubMed] [Google Scholar]
- 32.Misra S, Lal P, Kumar ESet al. Comparative assessment of late toxicity in patients of carcinoma cervix treated by radiotherapy versus chemo-radiotherapy–Minimum 5 years follow up. Cancer Treat Res Commun 2018; 14: 30-36. [DOI] [PubMed] [Google Scholar]
- 33.Alam N, Akram M, Siddiqui SA, Hussain MB. Interdigitated versus sequential high-dose-rate intracavitary brachytherapy with external beam radiotherapy in locally advanced carcinoma cervix. J Cancer Res Ther 2019; 15: 1254-1259. [DOI] [PubMed] [Google Scholar]
- 34.Sadiq S, Shahid A, Masood Met al. Acute side effects with high dose rate computed tomography-guided three-dimensional brachytherapy in carcinoma cervix. J Coll Physicians Surg Pak 2020; 30: 638-642. [DOI] [PubMed] [Google Scholar]
- 35.Tharavichitkul E, Tippanya D, Jayavasti Ret al. Two-year results of transabdominal ultrasound-guided brachytherapy for cervical cancer. Brachytherapy 2015; 14: 238-244. [DOI] [PubMed] [Google Scholar]
- 36.Saibishkumar EP, Patel FD, Sharma SC. Evaluation of late toxicities of patients with carcinoma of the cervix treated with radical radiotherapy: an audit from India. Clin Oncol R Coll Radiol 2006; 18: 30-37. [DOI] [PubMed] [Google Scholar]