ABSTRACT
Objective
The detection of a fetal abdominal cyst at the first‐trimester ultrasound scan is a rare event, for which the natural history and prognosis are often unknown and unpredictable, owing to various underlying etiologies. The aim of this study was to evaluate the outcome of fetal abdominal cysts detected in the first trimester to better understand their possible clinical significance and improve their clinical management.
Methods
We present a case report of a fetal abdominal cyst detected in the first trimester, with subsequent diagnosis of congenital multiple arthrogryposis. We also performed a systematic review of the literature to determine the incidence and outcome of similar cases, which was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement and registered with PROSPERO (CRD42023491729). PubMed, Web of Science and EMBASE were searched from inception to December 2023 to identify case reports and case series documenting an ultrasound diagnosis of a single fetal abdominal cyst in the first trimester.
Results
Our case presented at 12 + 6 weeks' gestation with an isolated fetal abdominal cyst, which underwent spontaneous resolution in the second trimester, when multiple congenital arthrogryposis was observed. Data on a total of 60 cases of fetal abdominal cyst detected in the first trimester were extracted from the literature. Of these, 35% were associated with concurrent or late‐onset structural anomalies, as in our case, and 65% were isolated. In pregnancies with an isolated fetal abdominal cyst, 54% had a live birth with a normal outcome.
Conclusions
A fetal abdominal cyst in the first trimester is usually an isolated finding with a moderate‐to‐good prognosis, but it could also be an early sign of other associated abnormalities, including arthrogryposis. Increased ultrasound surveillance and additional genetic testing to rule out possible associated anomalies are necessary to assess the risk of adverse pregnancy outcome and provide appropriate parental counseling. © 2024 The Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of International Society of Ultrasound in Obstetrics and Gynecology.
Keywords: fetal abdominal cyst, fetal malformation, first‐trimester anomaly, first‐trimester screening, prenatal diagnosis, ultrasound
CONTRIBUTION —
What are the novel findings of this work?
Diagnosis of a fetal abdominal cyst in the first trimester is associated with a normal outcome in only 37% of cases. An isolated cyst may precede the development of associated abnormalities, such as arthrogryposis. Pregnancy outcome depends ultimately on cyst persistence and associated concurrent and late‐onset anomalies.
What are the clinical implications of this work?
Detection of a fetal abdominal cyst at the first‐trimester ultrasound scan should prompt immediate referral to a fetal medicine center. Our updated review highlights the importance of tailored management and counseling, including offering a detailed early second‐trimester scan and genetic testing to rule out related syndromes and anomalies.
INTRODUCTION
Routine first‐trimester ultrasonography, recommended between 11 + 0 and 14 + 0 weeks' gestation, aims to confirm viability, accurately establish gestational age, determine the number of fetuses, assess chorionicity and amnionicity in multiple pregnancies and detect major fetal abnormalities 1 . It also allows clinicians to measure nuchal translucency (NT) thickness and screen for aneuploidy and pre‐eclampsia 1 . Advances in ultrasound imaging have improved the diagnosis of major and minor fetal defects during this examination, with the reported detection rate for anomalies in the first trimester ranging from 32% in low‐risk groups to over 60% in high‐risk groups 2 . When an anomaly is detected in the first trimester, the first duty of a clinician is to assess the prognosis, which is related to the etiology, as well as evaluate the possible evolution of the anomaly and eventual association with other anomalies.
Intra‐abdominal cysts, whose natural history and prognosis are often unknown and unpredictable, can be related to various underlying conditions and originate from different structures, including the gastrointestinal, genitourinary, mesenteric, hepatic or biliary system 3 . Few papers reporting on the detection and natural history of abdominal cysts in the first trimester are available, and most are retrospective cohort studies with a limited number of cases, or case reports.
Herein, we report a case of a fetal abdominal cyst that subsequently developed multiple congenital arthrogryposis (AMC). AMC is defined as the presence of multiple joint contractures in more than one area of the body, thus representing a descriptive term that can be associated with many different medical conditions. The current available literature includes only three similar cases in which an abdominal mass detected in the first trimester was associated with AMC later in pregnancy 4 , 5 , 6 . AMC is usually detected on prenatal ultrasound examination during the second and third trimesters 7 , 8 .
There is currently no consensus on management and parental counseling in cases of abdominal cyst in the first trimester, given the uncertainty over the possible association with other congenital anomalies, including AMC. This study aimed to describe a rare case of a first‐trimester abdominal cyst associated with subsequent AMC and to review the available literature on fetal abdominal cysts in order to better define the prognosis and to improve management and counseling in the first trimester of pregnancy.
METHODS
We report a case of a fetal abdominal cyst detected on ultrasound at 12 + 6 weeks' gestation, with subsequent diagnosis of AMC at 17 + 6 weeks. The patient provided written informed consent for publication of the anonymized case report.
A systematic search strategy was developed and applied to PubMed, Web of Science and EMBASE to identify previous citations, from inception to December 2023, reporting the outcome of fetuses diagnosed in the first trimester with an abdominal cyst. We used medical subject heading (MeSH) terms with the following keywords alone or in combination: ‘abdominal cyst’ OR ‘prenatal diagnosis’ OR ‘cystic anomalies’ OR ‘anorectal malformation’ AND ‘first‐trimester’ OR ‘prenatal ultrasound’ AND ‘associated abnormalities’. Inclusion criteria were case reports and case series with an ultrasound diagnosis of a single fetal abdominal cyst in the first trimester. Exclusion criteria were the diagnosis of multiple cysts, megacystis or omphalocele. No language restrictions were applied. The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement 9 and registered with PROSPERO (CRD42023491729).
Study selection and data extraction were performed independently by two authors (E.P., G.d.M.) and reviewed by a third author (A.F.), and discrepancies were resolved by consensus. Data collected included gestational age at diagnosis, crown–rump length, NT thickness, other structural malformations, invasive testing, karyotype, second‐trimester ultrasound findings, fetal or neonatal outcome and postmortem findings, when available. Pregnancy outcomes were also collected. Data were recorded in a dedicated Excel database (Microsoft, Redmond, WA, USA).
Quality assessment of the included studies was performed using the National Institutes of Health tool for quality assessment of case series. Quality assessment was performed by two authors (E.P., G.d.M.), and disagreements were resolved by consultation with the senior author (A.F.).
RESULTS
Case report
A 31‐year‐old woman, gravida 1 para 0, was referred for a detailed ultrasound scan at the fetal medicine unit of IRCCS Fondazione Policlinico Gemelli, Rome, Italy, owing to the finding of a fetal anomaly on first‐trimester screening. The patient's medical history included hypothyroidism and previous metroplasty surgery. No family history of congenital anomaly or genetic syndrome was reported.
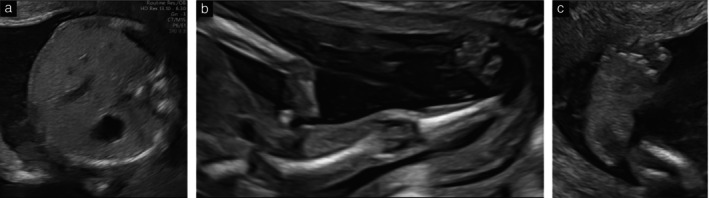
Ultrasound assessment at 12 + 6 weeks' gestation showed a singleton fetus with a normal NT of 1.5 mm and an anechoic avascular abdominal cyst measuring 6 × 5 × 7 mm with hyperechogenic walls (Figure 1). Ultrasound images were obtained using a Voluson E10 machine (GE Healthcare, Zipf, Austria). The cyst was isolated, located in the left upper abdomen, apparently subdiaphragmatic, had smooth and regular walls and was non‐infiltrating, with no connection to the stomach or umbilical‐cord insertion site. The stomach was visible but small, with slight medial displacement. No other fetal anomalies were detected. The patient was counseled about the possible association of this apparently isolated anomaly with evolving bowel or anorectal malformations (ARM). Determination of fetal karyotype and array comparative genomic hybridization (CGH) were offered, and chorionic villus sampling (CVS) was performed at 13 weeks. Genetic analysis returned normal results.
Figure 1.

Transabdominal ultrasound images at 12 + 6 weeks' gestation, showing fetal upper‐abdomen cyst (calipers) behind stomach in transverse (a) and longitudinal (b) views, and normal bladder in longitudinal view (c).
Considering the normal karyotype and array CGH results and the apparently isolated nature of the anomaly, the patient was scheduled for an early anomaly scan at 16–17 weeks' gestation. At this scan, which actually took place at 17 + 6 weeks, the abdominal cyst was no longer visible, but new findings were present: there was bilateral clubfoot, and the legs and wrists were bilaterally hyperextended and fixed, with clenched hands (Figure 2). The long bones had regular shape, echogenicity and measurements, without signs of fracture. Fetal movements were detected during the examination. Neurosonography did not reveal any structural abnormality, and the heart was apparently normal. These ultrasound findings supported the suspicion of fetal arthrogryposis.
Figure 2.
Transabdominal ultrasound images at follow‐up scan at 17 + 6 weeks' gestation. (a) Transverse view of normal fetal abdomen, with no sign of cyst. (b) Longitudinal view showing fetal arthrogryposis, with leg and wrist hyperextended and fixed, and with clenched hand. (c) Clubfoot.
After prenatal counseling, the parents decided to terminate the pregnancy at 21 weeks. The postmortem examination revealed a polymalformative pattern, which included partial agenesis (hypoplasia) of the corpus callosum, pulmonary valve dysmorphism, several skeletal malformations with clinodactyly of the fifth finger and hypoplasia of the phalanges of the second, third and fourth fingers of the left hand, aplasia of the left fibula and severe bilateral clubfoot, confirming the diagnosis of AMC. No gastrointestinal anomalies were found. As the risk of a genetic syndrome was very high, exome analysis was carried out to determine the possible future reproductive risk for the couple, but the results were negative.
Systematic review
The literature search of PubMed, Web of Science and EMBASE databases initially retrieved 462 potentially relevant studies, of which 432 were excluded based on their title/abstract, leaving 30 studies for full‐text review (Figure 3). Overall, 19 studies were included 3 , 4 , 5 , 6 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 . The characteristics of the included studies are summarized in Table 1. The excluded studies, with reasons for exclusion, are shown in Table S1. Quality assessment of the included studies is outlined in Table S2.
Figure 3.
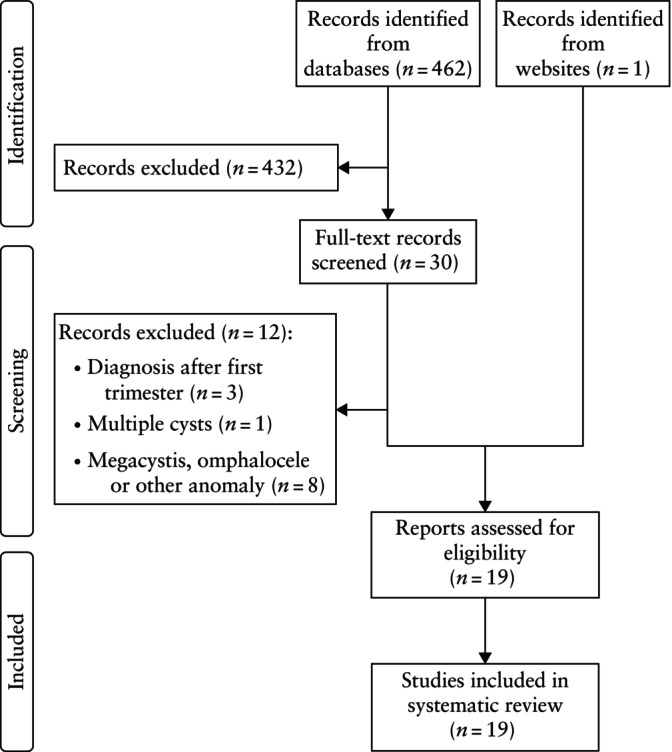
PRISMA flowchart summarizing inclusion of studies in systematic review.
Table 1.
Characteristics of 60 cases of fetal abdominal cyst in first trimester reported in 19 studies included in systematic review
| Study | GA (weeks) | Genetic results | NT (mm) | Size* (mm) | Cyst appearance/evolution | Location | Prenatal associated anomaly | Outcome |
|---|---|---|---|---|---|---|---|---|
| Zimmer (1991) 23 | ||||||||
| Case 1 | 11 + 4 | NA | NA | 13 | Anechoic | Midabdomen | Hydronephrosis | IUD |
| Case 2 | 12 | m45,X0 | NA | 13 | Anechoic | Entire fetal abdomen | Hydronephrosis, cystic hygroma, clubfoot | TOP |
| Case 3 | 13 | 46,XY | NA | 8 | Anechoic, resolution at 24 weeks | Right abdomen | Isolated | LB |
| Berg (2002) 13 | 13 | 46,XX | NA | 11 | Anechoic, persistence in 2nd trimester, aspiration of cyst at 22 weeks | Right upper quadrant | Isolated | LB, hepatic cyst |
| Lam (2002) 15 | 12 | 46,XY | 1.4 | 11 | Sausage‐shaped cyst, persistence in 2nd trimester | Right lower abdomen | Isolated | TOP, ARM |
| Taipale (2005) 16 | 12 | NA | 1.1 | 14 | Hypoechogenic, persistence | Lower abdomen | Isolated | LB, ARM |
| Gilbert (2006) 17 | 12 + 4 | 46,XY | NA | NA | Distal tapered cyst with echogenic focus, resolution at 17 weeks | Lower abdomen | Isolated | LB, ARM |
| Sepulveda (2008) 12 | ||||||||
| Case 1 | 13 + 2 | NA | 2.3 | 8 | Resolution | NA | Isolated | LB, IM |
| Case 2 | 13 + 1 | NA | 1.1 | 5 | Anechoic, persistence | Right abdomen | Isolated | LB, CC |
| Case 3 | 12 + 1 | NA | 0.7 | 10 | Anechoic, aspiration at 19 weeks | Upper abdomen | Isolated | LB |
| Case 4 | 11 + 5 | NA | 1.0 | 10 | Resolution | NA | Isolated | LB |
| Case 5 | 10 + 4 | NA | NA | 11 | Resolution | NA | Isolated | LB |
| Chen (2009) 4 | 12 | 46,XX | 1.9 | NA | Multiple dilated bowel loops, resolution at 17 weeks | Lower abdomen | Anorectal atresia, arthrogryposis multiplex | IUD at 18 weeks |
| Markov (2010) 14 | ||||||||
| Case 1 | 11–13 | NA | NA | NA | Persistence at 15 weeks | NA | Isolated | TOP |
| Case 2 | 11–13 | NA | NA | NA | Resolution | NA | Isolated | LB |
| Case 3 | 11–13 | NA | NA | NA | Resolution | NA | Isolated | LB |
| Novikova (2011) 18 | ||||||||
| Case 1 | 11 + 3 | T21 | 2.5 | 8 | Anechoic tubular cyst | Lower abdomen | T21 | TOP |
| Case 2 | 11–13 | 46,XX | 1.05 | 10 | Dilated bowel, persistence at 18 weeks | Lower abdomen | Renal agenesis | TOP, Fraser syndrome |
| Holschbach (2012) 24 | ||||||||
| Case 1 | 12 + 3 | Normal | 1.9 | 20 | Echogenic walls, resolution | Upper abdomen | SB | LB, SB |
| Case 2 | 13 | Normal | 1.1 | 15 | Echogenic walls, resolution | Upper abdomen | Isolated | LB |
| Case 3 | 13 | Normal | 1.7 | 21 | Echogenic walls, resolution | Upper abdomen | Isolated | LB |
| Santos (2013) 22 | 13 | 46,XY | NA | NA | Anechoic tubular cyst | Intra‐abdominal | Multiple anomalies (VACTERL) | TOP |
| Khalil (2014) 3 | ||||||||
| Case 1 | 12 + 4 | NA | NA | 6 | NA | NA | Pulmonary stenosis, anhydramnios | TOP |
| Case 2 | 12 + 4 | NA | NA | 6 | NA | NA | Cystic hygroma, SUA, UC cysts, echogenic bowel | IUD at 16 weeks |
| Case 3 | 12 + 5 | NA | NA | 7 | Resolution | NA | Hydronephrosis, esophageal atresia, SUA, UC cysts | LB, VACTERL |
| Case 4 | 14 | NA | NA | 20 | NA | NA | Microcephaly, VM, sacral SB, SUA, aortic stenosis | IUD, CMV positive |
| Case 5 | 12 + 3 | NA | NA | 6 | Persistence at 15 weeks | NA | Isolated | IUD |
| Case 6 | 13 + 4 | NA | NA | 6 | Persistence | Midabdomen | Isolated | LB, CC |
| Case 7 | 11 + 5 | NA | NA | 8 | Resolution | Left abdomen | Isolated | LB |
| Case 8 | 12 + 3 | NA | NA | 10 | Resolution | NA | Isolated | LB |
| Case 9 | 12 + 4 | NA | NA | 15 | Resolution | Right abdomen | Isolated | LB |
| Case 10 | 13 | NA | NA | 4 | Resolution | NA | Isolated | LB |
| Case 11 | 13 + 2 | NA | NA | 10 | Resolution | Left abdomen | Isolated | LB |
| Case 12 | 13 + 3 | NA | NA | 6 | Resolution | Right abdomen | Isolated | LB |
| Case 13 | 13 + 5 | NA | NA | 4 | Resolution | NA | Isolated | LB |
| Case 14 | 14 | NA | NA | 17 | Resolution | Bowel/urachus | Isolated | LB |
| Dhombres (2015) 10 | ||||||||
| Case 1 | 12 + 2 | 46,XY | 1.7 | 5 | Hyperechoic | NA | Diaphragmatic hernia | TOP |
| Case 2 | 12 + 6 | Normal | 1.9 | 16 | Mixed echogenicity | NA | Hepatorenal polycystosis | TOP |
| Case 3 | 13 + 6 | NA | 1.6 | 26 | Mixed echogenicity | NA | Cloacal dysgenesis | TOP |
| Case 4 | 14 | NA | NA | 18 | Mixed echogenicity | NA | VACTERL | TOP |
| Case 5 | 11 + 6 | NA | 1.6 | 5 | Anechoic, resolution | NA | Isolated | LB |
| Case 6 | 12 + 2 | 46,XY | 2.2 | 22 | Anechoic, resolution | NA | Isolated | LB |
| Case 7 | 12 + 3 | NA | 1.6 | 4 | Anechoic, resolution | NA | Isolated | LB |
| Case 8 | 12 + 6 | NA | 1.6 | 16 | Anechoic, resolution | NA | Isolated | LB |
| Case 9 | 12 + 2 | NA | 1.5 | 9 | Anechoic, resolution | NA | Isolated | LB, ARM |
| Case 10 | 12 + 3 | NA | 1.9 | 29 | Hyperechoic, resolution | NA | Isolated | LB |
| Karapetyan (2016) 6 | 13 | 46,XX | NA | 8 | Anechoic, resolution in 2nd trimester | Midabdomen | Arthrogryposis | TOP |
| Correia (2017) 21 | 12 | 46,XY | NA | 33 | Hypoechoic tubular shaped, persistence in 2nd trimester | Left abdomen | Isolated | TOP, DSD |
| Liberty (2018) 20 | 13 + 4 | 46,XY | 1.7 | 8 | Tubular cyst, persistence in 2nd trimester | Right abdomen | Isolated | TOP, ARM |
| Ples (2020) 19 | 11 + 3 | 46,XY | NA | NA | Anechoic, resolution | Left abdomen | Isolated | LB, ARM |
| Erculiani (2023) 11 | ||||||||
| Case 1 | 12 + 6 | 46,XY | NA | 8 | Anechoic, resolution | Lower abdomen | Altered sacrum, possible tethered cord | LB, Currarino syndrome |
| Case 2 | 13 | 46,XY | NA | 5 | Anechoic, resolution at 19 weeks | Lower abdomen | Isolated | LB, ARM |
| Case 3 | 12 + 4 | 46,XY | NA | 8 | Anechoic, resolution at 14 weeks | Lower abdomen | Isolated | LB, ARM |
| Garcia‐Aguilar (2023) 5 | ||||||||
| Case 1 | 12 | NA | NA | NA | NA | NA | Cystic kidneys, pulmonary hypoplasia, ARM, VSD | TOP |
| Case 2 | 13 | NA | NA | NA | NA | Liver | Polycystic kidneys | TOP |
| Case 3 | 13 | NA | NA | NA | NA | Lymphatic | Lymphatic cyst, hydrops | TOP |
| Case 4 | 12 | NA | NA | NA | Resolution | NA | Arthrogryposis, ToF | IUD at 33 weeks |
| Case 5 | 12 | NA | NA | NA | Resolution | NA | Isolated | IUD at 19 weeks, ARM |
| Case 6 | 11–13 | NA | NA | NA | Resolution | NA | Isolated | LB, ARM |
| Case 7 | 11–13 | NA | NA | NA | Resolution | NA | Isolated | LB |
Only first author is given for each study.
Maximum cyst diameter.
ARM, anorectal malformation; CC, choledocal cyst; CMV, cytomegalovirus; DSD, disorder of sexual development; GA, gestational age at diagnosis; IM, intestinal malrotation; IUD, intrauterine death; LB, live birth; m, mosaicism; NA, not available; NT, nuchal translucency; SB, spina bifida; SUA, single umbilical artery; T21, trisomy 21; ToF, tetralogy of Fallot; TOP, termination of pregnancy; UC, umbilical cord; VM, ventriculomegaly; VSD, ventricular septal defect.
Sixty cases of fetal abdominal cyst diagnosed in the first trimester were extracted from the identified studies (Figure 4). Among these, 39 (65%) cases were classified as isolated, of which 29 (74%) resolved spontaneously and 21 (54%) had a normal neonatal outcome. In seven (18%) cases of isolated cyst, the cyst resolved spontaneously during pregnancy but progressed to ARM (n = 6) or intestinal malrotation (n = 1), requiring neonatal surgery 5 , 10 , 11 , 12 , 17 , 19 . Persistence of the cyst was observed in 10 (26%) cases, of which four pregnancies were terminated, one resulted in intrauterine death and five resulted in live birth. Four of the liveborn infants subsequently underwent neonatal surgery for ARM (n = 1), choledochal cyst (n = 2) or hepatic cyst (n = 1) 3 , 12 , 13 , 16 .
Figure 4.
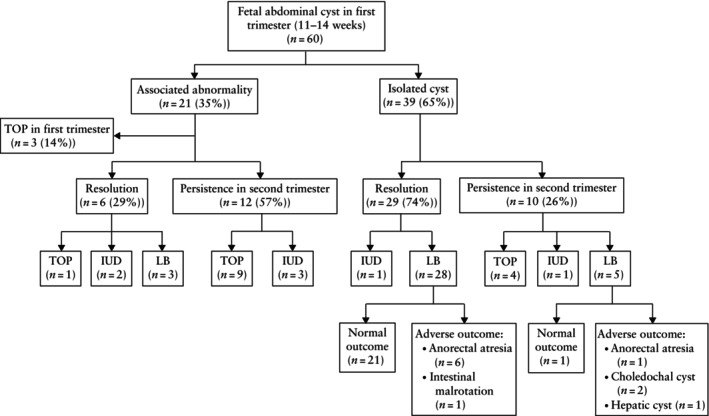
Flowchart summarizing findings and outcome in 60 fetuses diagnosed with abdominal cyst in first trimester (11–14 weeks' gestation) reported in literature. IUD, intrauterine death; LB, live birth; TOP, termination of pregnancy.
The cyst was non‐isolated in 21 (35%) cases, with associated anomalies (including cystic hygroma, echogenic bowel, hydronephrosis, esophageal atresia, microcephaly, cerebral ventriculomegaly, sacral spina bifida, cardiopathy, diaphragmatic hernia, hepatorenal polycystosis, cloacal dysgenesis, VACTERL syndrome and arthrogryposis multiplex) identified in the first or second trimester 3 , 4 , 5 , 6 , 10 , 11 , 18 , 22 , 23 , 24 . In most of these pregnancies, the cyst persisted; in only six cases did it resolve spontaneously. The majority of cases of non‐isolated cyst underwent termination of pregnancy or resulted in intrauterine death. In three cases, the pregnancy was carried to term, and liveborn infants were affected by spina bifida, VACTERL syndrome and Currarino syndrome, respectively 3 , 11 , 24 .
Thus, among the 60 cases of fetal abdominal cyst diagnosed in the first trimester, regardless of whether they were isolated or associated with another abnormality, only 37% (n = 22) demonstrated a completely normal outcome at birth. In 23% (n = 14) of cases, the infant was born alive but with subsequent complications, while 40% (n = 24) of pregnancies were terminated or resulted in intrauterine death.
DISCUSSION
Summary of the literature
The first‐trimester diagnosis of a fetal abdominal cyst is rare and the relevant literature is limited, comprising case reports and small retrospective studies.
The largest series to date is that of Khalil et al. 3 , which included 14 cases of fetal abdominal cyst detected at 11–14 weeks' gestation. They reported that 80% of isolated cysts resolved prenatally, with no apparent pregnancy or neonatal complications. However, four cases showed associated malformations: one had pulmonary stenosis and anhydramnios; another had cystic hygroma, single umbilical artery, echogenic bowel and umbilical cord cysts; one had cytomegalovirus infection; and one exhibited VACTERL syndrome.
The study of Sepulveda et al. 12 included five cases of fetal abdominal cyst diagnosed in the first trimester. At early second‐trimester follow‐up, the presence of the cystic mass was confirmed in all cases, but none exhibited associated abnormalities. The authors concluded that the finding of an abdominal cyst in the first trimester is associated with a good perinatal outcome in the majority of cases 12 .
In contrast, Garcia‐Aguilar et al. 5 reported that first‐trimester abdominal cysts are associated with other abnormalities in 71% (5/7) of cases and are more likely to result in adverse perinatal outcome. In one case (Case 4), they describe an abdominal cyst at 12 weeks, which resolved spontaneously, with subsequent appearance of associated abnormalities, including arthrogryposis, growth restriction and tetralogy of Fallot, resulting in stillbirth at 33 weeks 5 .
Chen et al. 4 published a case of ARM suspected at 12 weeks' gestation because of multiple dilated bowel loops. The 17‐week anomaly scan revealed an apparently normal bowel. Spontaneous miscarriage occurred at 18 weeks and postmortem examination showed ARM and AMC. The authors concluded that transient bowel dilatation may be a possible early marker for ARM 4 .
Another case report, by Karapetyan 6 , describes an isolated first‐trimester abdominal cyst that resolved in the second trimester. All major fetal joints were severely affected, and the fetal karyotype and array CGH were normal. Consequently, to date, our case report is the fourth to document an association between a first‐trimester fetal abdominal cyst and arthrogryposis.
Interpretation
AMC is a condition associated with multiple joint contractures in different parts of the body 7 , 8 . The detection rate of AMC on prenatal ultrasound has been estimated to be around 25%, thus current efforts to identify contractures prenatally and assess fetal movements result in approximately 75% of AMC cases not being detected until birth. The delay in diagnosis precludes further etiological and diagnostic investigations and prevents families from making informed pregnancy choices and scheduling delivery in a hospital with the appropriate level of care 25 , 26 .
Our results suggest that the finding of a fetal abdominal cyst in the first trimester is associated with other anomalies in 35% of cases, and that these cases typically have a poor outcome, including intrauterine death or termination of pregnancy. When the abdominal cyst was an isolated finding (65% of the cases described in the literature), a normal outcome was reported in only 54% of cases. Therefore, even if it is initially isolated and resolves spontaneously, a fetal abdominal cyst in the first trimester may be the first sign of a serious associated condition. The higher rate of unfavorable outcomes in our study compared to that reported previously may be because of the small number of cases reported in the literature and the high termination rate owing to the diagnosis of malformations in the first trimester.
Based on the findings of our systematic review, we propose an algorithm for the management of pregnancies with a first‐trimester diagnosis of fetal abdominal cyst (Figure 5). Prompt referral to a fetal medicine center is recommended for a comprehensive anatomical ultrasound evaluation, measurement of NT thickness and assessment of the cyst (size, location and appearance). We recommend offering invasive testing (CVS) for fetal karyotyping and array CGH analysis. Additionally, we propose a prognostic algorithm (Figure 6) to improve parental counseling and clinical management. Prognosis is strictly dependent on the association with other anomalies and genetic disorders, as well as on the evolution (resolution or persistence) of the cyst. For this reason, serial follow‐up scans should be scheduled, starting from an early anomaly scan at 16–17 weeks. In cases in which associated anomalies are identified, parental counseling should highlight the increased risk of adverse outcome, and should involve other professionals (neonatologists, geneticists, pediatricians) to formulate a targeted follow‐up plan, irrespective of negative genetic test results.
Figure 5.
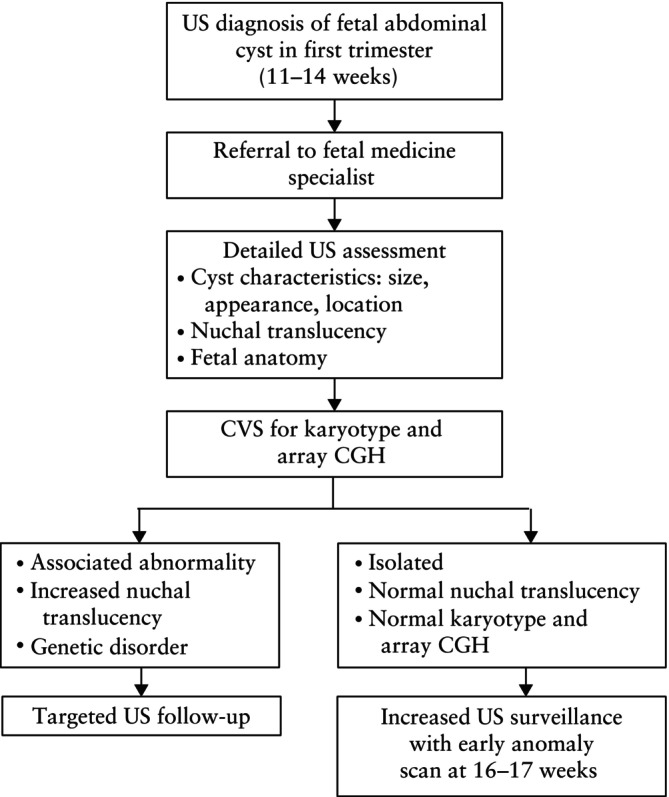
Proposed algorithm for prognostic evaluation of fetuses with diagnosis of abdominal cyst in first trimester (11–14 weeks' gestation). CGH, comparative genomic hybridization; CVS, chorionic villus sampling; GI, gastrointestinal; US, ultrasound.
Figure 6.
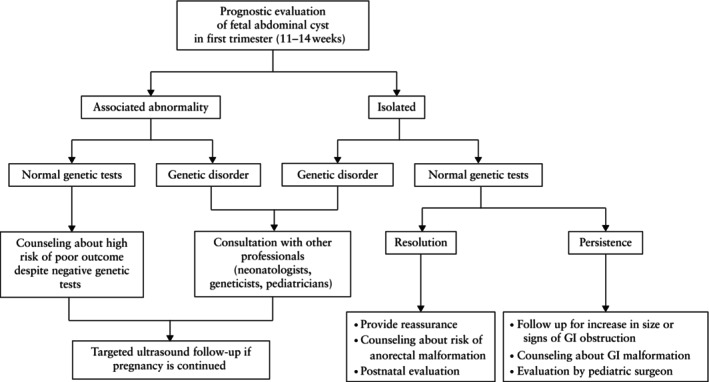
Proposed algorithm for prognostic evaluation of fetuses with diagnosis of abdominal cyst in first trimester (11–14 weeks' gestation). GI, gastrointestinal.
In the case of an isolated fetal abdominal cyst that resolves, patients should be reassured but counseled about the potential risk of later‐onset abnormalities during pregnancy and at birth, and postnatal evaluation should be scheduled. If the cyst persists, close surveillance will be needed to identify any increase in its size or any sign of gastrointestinal obstruction. Counseling regarding gastrointestinal anomalies is crucial, and evaluation by a pediatric surgeon is recommended.
Contrary to previous reports 3 , this review suggests that, even though the occurrence of AMC is rare, prenatal counseling for an isolated first‐trimester fetal abdominal cyst should consider the risk of developing complex anomalies and should prompt referral for additional genetic testing as well as an early detailed ultrasound anomaly scan at 16–17 weeks' gestation.
Strengths and limitations
The strength of this study is that, to date, it represents the largest systematic review including only cases of fetal abdominal cyst diagnosed at 11–14 weeks' gestation. Our results suggest that the likelihood of this finding representing an early marker of complex anomalies is higher than that reported previously, thus highlighting the need for revised management and counseling. A clear limitation is the retrospective design of the included studies.
Conclusions
The detection of a fetal abdominal cyst in the first trimester is a rare event, with different possible etiologies and outcomes, for which effective management is crucial. If the cyst is an isolated finding and it resolves spontaneously during pregnancy, the outcome is more likely to be good, but it can herald other abnormalities that may require surgery at birth. Appropriate counseling should be offered to parents because abdominal cysts in the first trimester can represent the first marker of subsequent severe anomalies. Caution should be exercised when defining the prognosis and outcome of these pregnancies.
Supporting information
Table S1 Excluded studies and reason for exclusion
Table S2 Quality assessment of included case reports and case series according to National Institutes of Health questions
ACKNOWLEDGMENT
Open access funding provided by BIBLIOSAN.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
REFERENCES
- 1. International Society of Ultrasound in Obstetrics and Gynecology , Bilardo CM, Chaoui R, et al. ISUOG Practice Guidelines (updated): performance of 11 – 14‐week ultrasound scan. Ultrasound Obstet Gynecol. 2023;61:127‐143. [DOI] [PubMed] [Google Scholar]
- 2. Karim JN, Roberts NW, Salomon LJ, Papageorghiou AT. Systematic review of first‐trimester ultrasound screening for detection of fetal structural anomalies and factors that affect screening performance. Ultrasound Obstet Gynecol. 2017;50:429‐441. [DOI] [PubMed] [Google Scholar]
- 3. Khalil A, Cooke PC, Mantovani E, Bhide A, Papageorghiou AT, Thilaganathan B. Outcome of first‐trimester fetal abdominal cysts: cohort study and review of the literature. Ultrasound Obstet Gynecol. 2014;43:413‐419. [DOI] [PubMed] [Google Scholar]
- 4. Chen M, Meagher S, Simpson I, Lau TK. Sonographic features of anorectal atresia at 12 weeks. J Matern Fetal Neonatal Med. 2009;22:931‐933. [DOI] [PubMed] [Google Scholar]
- 5. Garcia‐Aguilar P, Maiz N, Rodó C, et al. Fetal abdominal cysts: predicting adverse outcomes. Acta Obstet Gynecol Scand. 2023;102:883‐890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Karapetyan L. Arthrogryposis. 2016. https://thefetus.net/content/arthrogryposis‐26
- 7. Lowry RB, Sibbald B, Bedard T, Hall JG. Prevalence of multiple congenital contractures including arthrogryposis multiplex congenita in Alberta, Canada, and a strategy for classification and coding. Birth Defects Res A Clin Mol Teratol. 2010;88(12):1057‐1061. [DOI] [PubMed] [Google Scholar]
- 8. Society for Maternal‐Fetal Medicine , Rac MWF, McKinney J, Gandhi M. Arthrogryposis. Am J Obstet Gynecol. 2019;221(6):B7‐B9. [DOI] [PubMed] [Google Scholar]
- 9. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dhombres FS, Friszer O, Castaing R, Bessis J‐M. Jouannic images kystiques abdominales fœtales du premier trimestre. Gynécol Obstét Fertil. 2015;43:491‐495. [DOI] [PubMed] [Google Scholar]
- 11. Erculiani M, Trovalusci E, Zanatta C, et al. First trimester lower abdominal cysts as early predictor of anorectal malformations. J Ultrasound. 2023;26:543‐548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sepulveda W, Dickens K, Casasbuenas A, Gutierrez J, Dezerega V. Fetal abdominal cysts in the first trimester: prenatal detection and clinical significance. Ultrasound Obstet Gynecol. 2008;32:860‐864. [DOI] [PubMed] [Google Scholar]
- 13. Berg C, Baschat AA, Geipel A, et al. First‐trimester diagnosis of fetal hepatic cyst. Ultrasound Obstet Gynecol. 2002;19:287‐289. [DOI] [PubMed] [Google Scholar]
- 14. Markov D, Pavlova E, Atanasova D, Markov P, Ivanov S. First trimester cystic structures in the fetal abdomen: diagnosis and prognostic value. Akush Ginekol (Sofia). 2010;49:13‐19. [PubMed] [Google Scholar]
- 15. Lam YH, Shek T, Tang MHY. Sonographic features of anal atresia at 12 weeks. Ultrasound Obstet Gynecol. 2002;19:523‐524. [DOI] [PubMed] [Google Scholar]
- 16. Taipale P, Rovamo L, Hiilesmaa V. First‐trimester diagnosis of imperforate anus. Ultrasound Obstet Gynecol. 2005;25:187‐188. [DOI] [PubMed] [Google Scholar]
- 17. Gilbert CE, Hamill J, Metcalfe RF, Smith P, Teele RL. Changing antenatal sonographic appearance of anorectal atresia from first to third trimesters. J Ultrasound Med. 2006;25:781‐784. [DOI] [PubMed] [Google Scholar]
- 18. Novikova I, Solovyeva I, Lishtvan L, Venchikova N, Plevako T. First trimester sonographic features of anorectal atresia: report of two cases. Prenat Diagn. 2011;31(9):907‐909. [DOI] [PubMed] [Google Scholar]
- 19. Ples L, Chicea R, Poenaru MO, Neacsu A, Sima RM, Micu R. Can anorectal atresia be diagnosed in the first trimester of pregnancy? A systematic literature review. Medicina (Kaunas). 2020;56(11):583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liberty G, Bardin R, Gilboa Y, et al. First trimester expression of anorectal malformation: case report and review of the literature. J Clin Ultrasound. 2018;46(9):591‐597. [DOI] [PubMed] [Google Scholar]
- 21. Correia P, Moreira M, Rodrigues M, Inocencio G. Prenatal diagnosis of vesicorectal fistula. Ultrasound Q. 2017;33(1):112‐114. [DOI] [PubMed] [Google Scholar]
- 22. Santos J, Nogueira R, Pinto R, Cerveira I, Pereira S. First trimester diagnosis of VACTERL association. Clin Pract. 2013;3(1):e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zimmer EZ, Bronshtein M. Fetal intra‐abdominal cysts detected in the first and early second trimester by transvaginal sonography. J Clin Ultrasound. 1991;19:564‐567. [DOI] [PubMed] [Google Scholar]
- 24. Holschbach V, Lattrich CR, Ortmann O, Müller AM, Germer U. Upper abdominal cysts in first trimester fetuses. Ultraschall Med. 2012;33:E372‐E373. [DOI] [PubMed] [Google Scholar]
- 25. Busack B, Ott CE, Henrich W, Verlohren S. Prognostic significance of prenatal ultrasound in fetal arthrogryposis multiplex congenita. Arch Gynecol Obstet. 2021;303(4):943‐953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Filges I, Tercanli S, Hall JG. Fetal arthrogryposis: challenges and perspectives for prenatal detection and management. Am J Med Genet C Semin Med Genet. 2019;181:327‐336. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Excluded studies and reason for exclusion
Table S2 Quality assessment of included case reports and case series according to National Institutes of Health questions
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.


