Abstract
Introduction
Maternal‐neonatal healthcare services were severely disrupted during the COVID‐19 pandemic in even high‐income countries within the World Health Organization (WHO) European Region. The objective of this study was to compare trends in the quality of maternal and neonatal care (QMNC) in Sweden and Norway to 12 other countries from the WHO European Region during the COVID‐19 pandemic, and to identify domains for improvement.
Material and Methods
This cross‐sectional study included women giving birth in Europe from March 1, 2020 to December 31, 2022. Women answered an online, anonymous questionnaire which included 40 WHO Standard‐based Quality Measures collectively scored as the total QMNC index (0–400) and separately in four subdomains (0–100): provision of care, experience of care, availability of human and physical resources, and reorganizational changes due to COVID‐19. To assess reported QMNC changes over time, we used adjusted quantile regression models. ClinicalTrials.gov Identifier: NCT04847336.
Results
Of the 45151 women included in the study, 13 117 (29.1%) were from Sweden and Norway and 32034 (70.9%) from the 12 WHO European countries. The total QMNC index for Sweden and Norway (median: 325, IQR: 285–355) was higher than the 12 WHO European countries (median: 315, IQR: 265–350, p < 0.001) as were trends in QMNC index over time (Sweden and Norway median: 310–345; 12 WHO European countries median: 305–340). Sweden and Norway also had higher scores in three‐of‐four QMNC subdomains, with the 12 WHO European countries scoring higher only for reorganizational changes due to COVID‐19. In adjusted quantile models of the total QMNC index, Sweden and Norway had higher scores, with largest differences in the lower quantiles (p < 0.001 in all percentiles).
Conclusions
Across Europe, there are significant gaps in the quality of maternal‐neonatal healthcare services. Although women giving birth in Sweden and Norway reported higher QMNC scores in all subdomains except for “reorganizational changes due to COVID‐19,” there is room for improvement and shared learning across Europe. Policymakers should prioritize long‐term investments in maternal and neonatal healthcare, ensuring that facilities are adequately equipped during public health crises and that all women have access to high‐quality, evidence‐based, equitable, and respectful care.
Keywords: childbirth, COVID‐19, European region, maternal, maternity care, newborn, Norway, quality of care, questionnaire, Scandinavia, survey, Sweden, time trend analysis, WHO standards
Reporting on the quality of maternal and neonatal care as experienced by 45151 women giving birth across Europe during the COVID‐19 pandemic, women in Sweden and Norway reported a better quality of care as compared to women in 12 other WHO European countries.
Abbreviations
- COVID‐19
Coronavirus Disease of 2019
- IMAgiNE EURO
Improving maternal newborn care in the European Region study group
- IQR
interquartile range
- PPE
personal protective equipment
- QMNC
quality of maternal and neonatal care
- WHO
World Health Organization
Key message.
Reporting on the quality of maternal and neonatal care as experienced by 45151 women giving birth across Europe during the COVID‐19 pandemic, women in Sweden and Norway reported a better quality of care as compared to women in 12 other WHO European countries.
1. INTRODUCTION
Sweden and Norway have consistently exhibited favorable trends in maternal and neonatal health that distinguish them from other countries in the WHO European Region. 1 With some of the lowest rates of maternal and neonatal mortality and morbidity in the world, Sweden and Norway share common geo‐political history and are stable social democracies in Europe. 1 , 2 Citizens in Sweden and Norway are offered universal health care coverage and share cultural and social norms which are distinctive from other countries in the WHO European Region. 2
With approximately 115000 and 55000 births/year in Sweden and Norway respectively, antenatal care is universally available and free of charge. 3 , 4 , 5 , 6 Home births are uncommon with the overwhelming majority of births (>98.5%) occurring at specialized maternity hospitals. 7 Midwives are the main providers of maternal health care unless the pregnancy is deemed high risk. In such cases, obstetricians are involved to help monitor and plan specific strategies aimed at preventing complications. Maternal healthcare staff follow national and local guidelines that aim to provide the highest standard of evidence‐based care. While there is typically good continuity of care during pregnancy, the midwife who attends childbirth and takes care of the mother and the newborn in the immediate postpartum period is often not the same as the midwife who cared for the woman during pregnancy. 3 , 4 , 5 , 6 , 7 , 8
The COVID‐19 pandemic imposed immense challenges on health care systems throughout the world. Most European countries reported disruptions in essential maternal‐newborn health services resulting in reduced medical counseling and support, increased medicalization of care, and limitations on evidence‐based practices such as companions of choice, breastfeeding, and rooming‐in. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 Considering the increasing importance of maternal‐reported outcomes, 14 and the unique characteristics of maternity services in Sweden and Norway, 3 , 4 , 13 this analysis explores women's reported experiences of the quality of maternal and neonatal care (QMNC) over time and compares them with other European countries. Using survey data from a large cross‐sectional study of QMNC in WHO European countries called IMAgiNE EURO, 14 the objective of our study was to compare QMNC trends in Sweden and Norway to QMNC trends in 12 other countries from the WHO European Region during the COVID‐19 pandemic, and to identify domains for future improvement.
2. MATERIAL AND METHODS
This was a cross‐sectional study, and the Strengthening the Reporting of Observational Studies (STROBE) in Epidemiology guidelines for reporting on cross‐sectional studies were followed. 21 The STROBE Checklist for this study is reported as Table S1.
Women ≥18 years of age, who gave birth in a country of the WHO European Region from March 1, 2020 to December 31, 2022 voluntarily participated in an anonymous online survey. Women who did not match the above criteria, declined participation, or gave birth outside the hospital setting were excluded from the study.
The questionnaire was made available in 26 languages and disseminated by project partners from September 2, 2020 onwards. Women were invited to join the study and respond to the questionnaire in their preferred language regardless of the country they gave birth in. Each national team predefined a written survey dissemination plan, which included dissemination through social media, institutional websites and local networks including mothers' groups and non‐governmental organizations. We did not exclude respondents who gave birth in WHO European Region countries not represented by a project partner. The online survey is still ongoing, and the study network is growing. For the analysis, the Scandinavian countries of Sweden and Norway were compared to the following 12 countries in the WHO European Region: Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Slovenia, and Switzerland.
Data were collected using a validated structured online questionnaire, 14 based on the WHO quality standards, 22 and recorded using REDCap 8.5.21—© 2021 Vanderbilt University, via a centralized platform. The questionnaire included two different major paths, women who underwent labor and those who did not (i.e. had a planned/elective cesarean), each with 40 key quality measures equally distributed in four subdomains: the three subdomains of the WHO Standards (i.e. provision of care, experience of care, and availability of human and physical resources) and the additional domain regarding reorganizational changes related to COVID‐19. The QMNC index was calculated based on a predefined score of 0, 5, or 10 points attributed to each possible answer for the 40 key quality measures. 14 , 23 The sum of these measures generated the total QMNC index (range 0–400 points, with higher values indicating higher adherence to WHO Standards). 22 The QMNC index was also calculated by each domain (range 0–100 points). Brief socio‐demographic data were also collected from the participants.
To follow the highest standards of good scientific practice, the questionnaire was initially developed in English and translated into other languages and then back‐translated to English following guidance of the Professional Society for Health Economics and Outcomes Research (ISPOR) Task Force for Translation and Cultural Adaptation Principles of Good Practice. 24
Data were cleaned according to predefined standardized operating procedures. 14 Responses with 20% or more missing data were deleted. Internal consistency among data was checked and duplicates were identified using date and place of birth, other socio‐demographic and obstetric data and excluded according to predefined standard operating procedures. 14 Of Scandinavian countries, Denmark and Finland were not included in the analysis due to their low sample size. Non‐Scandinavian WHO European countries were included when there were more than 300 women answering the survey and these answers were distributed over three‐fourths of the time periods, with at least 70 participants for three periods and 30 participants in another three periods. This approach ensures a more robust comparison and even data distribution throughout the time periods, allowing trend analysis.
2.1. Statistical analyses
Sociodemographic indicators were presented as absolute frequencies and percentages while the QMNC index was presented as median and interquartile range (IQR) since it was not normally distributed. Differences between Sweden and Norway to the other 12 countries of the WHO European region (Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Switzerland, and Slovenia) were tested using the Chi‐square test, Fisher exact test or Mann–Whitney test for categorical or continuous data respectively. To assess differences between Sweden and Norway, the characteristics of the respondents were separately compared using the Chi‐square test (Table S2).
To observe trends in reported QMNC over time, both for the total index and by subdomains, median QMNC index and their IQR were explored graphically over time periods. The initial time period was for 3 months, and the remaining time periods were divided equally into 4 month intervals. The period from October 2022 to December 2022 was not included due to too few participants. To assess if the QMNC index trend in Sweden and Norway or the 12 WHO countries had a significant increasing or decreasing trend, a two‐sided Mann‐Kendall test was performed in the overall time period of the study. In addition, quantile regression models were performed to test the time trend adjusting for geographical area, maternal age, educational level, mode of birth, mother giving birth in the same country where she was born (to represent migrant status), parity, type of hospital, and type of healthcare provider who directly assisted the birth. Five quantile models were performed, one with the total QMNC index as dependent variable and other four with the index subdomains. In the models, for categorical and ordinal variables the most frequent category was selected as the reference category, allowing for comparisons against the most typical group.
A two tailed p‐value <0.05 was considered statistically significant. Statistical analyses were performed using Stata/SE version 14.0 (Stata Corporation, College Station, TX, USA) and R software 4.2.2.
3. RESULTS
The selection of participants for the final study population is illustrated in Figure 1. Of a total of 70721 women that accessed the online questionnaire, 63953 gave consent (90.4%). Of these, 59704 met the inclusion criteria and, after screening for questionnaires with ≥20% missing information and suspected duplicates, 50632 remained. After removal of all countries where the total participating women were less than 300 or recruited after the 31st of December 2022, our final study population consisted of 45151 women with validated data. Of these, 13 117 (29.1%) were from Sweden and Norway and 32034 (70.9%) were from the other 12 WHO European countries. In the 12 WHO European countries, the sample collected in each country was compared to the estimated total births during the study period. This accounted for at least 1% of the total expected births in seven countries (Croatia, Greece, Italy, Latvia, Lithuania, Portugal and Slovenia).
FIGURE 1.
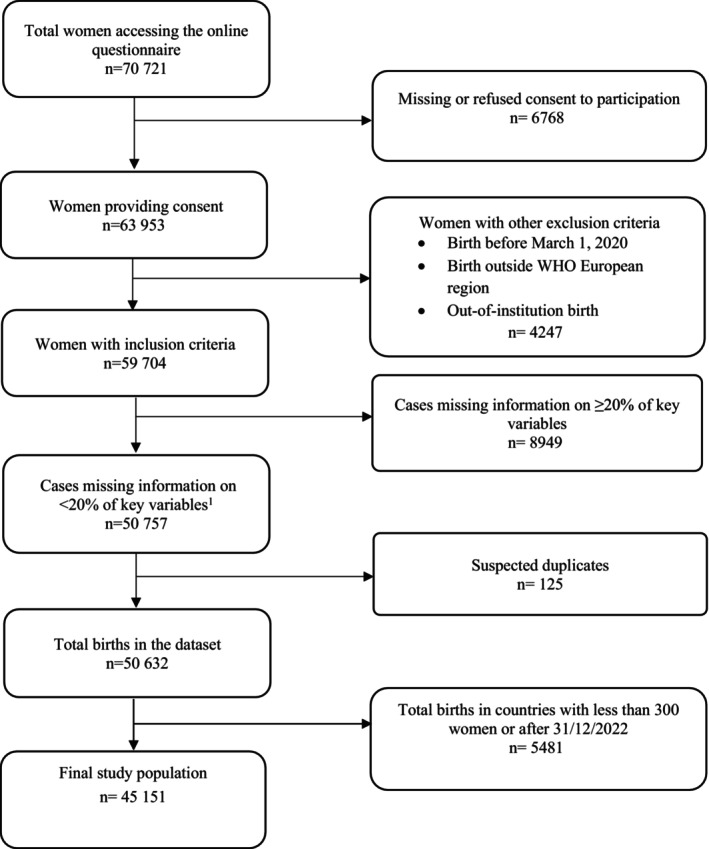
Flowchart of study population.
Socio‐demographic and obstetric data comparing participants from Sweden and Norway to the other 12 WHO European countries are outlined in Table 1. Significant differences were observed for year of birth (in 2020: Sweden and Norway 65.7%, 12 WHO European countries 55.4%, p < 0.001), woman gave birth in the same country where she was born (Sweden and Norway 92.8%, 12 WHO European countries 93.8%, p < 0.001), maternal age ranges (ages 25–34: Sweden and Norway 81.9%, 12 WHO European countries 71.9%, p < 0.001), parity (primiparous: Sweden and Norway 60.9%, 12 WHO European countries 62%, p = 0.027), educational level (university: Sweden and Norway 55.5%, 12 WHO European countries 34.7%, p < 0.001), birth mode (spontaneous vaginal birth: Sweden and Norway 73.4%, 12 WHO European countries 62.1%, p < 0.001), type of hospital (public: Sweden and Norway 98.9%, 12 WHO European countries 85.6%, p < 0.001 and type of healthcare provider who assisted birth (midwife: Sweden and Norway 98.7%, 12 WHO European countries 83.2%, p < 0.001).
TABLE 1.
Characteristics of study participants (N = 45151).
| Scandinavia a n (%) | 12 WHO European Countries b n (%) | p‐value | |
|---|---|---|---|
| N = 13 117 | N = 32034 | ||
| Year of giving birth | |||
| 2020 | 8618 (65.7%) | 17757 (55.4%) | <0.001 |
| 2021 | 3790 (28.9%) | 11731 (36.6%) | <0.001 |
| 2022 | 709 (5.4%) | 2546 (7.9%) | <0.001 |
| Woman gave birth in the same country where she was born | |||
| Yes | 12177 (92.8%) | 30035 (93.8%) | <0.001 |
| No | 936 (7.1%) | 1995 (6.2%) | <0.001 |
| Missing | 4 (0.0%) | 4 (0.0%) | 0.241 |
| Age range | |||
| 18–24 | 677 (5.2%) | 1479 (4.6%) | 0.015 |
| 25–34 | 10744 (81.9%) | 23048 (71.9%) | <0.001 |
| 35–39 | 1386 (10.6%) | 5689 (17.8%) | <0.001 |
| ≥40 | 310 (2.4%) | 1818 (5.7%) | <0.001 |
| Parity | |||
| Primiparous | 7989 (60.9%) | 19869 (62%) | 0.027 |
| Multiparous | 5127 (39.1%) | 12161 (38%) | 0.027 |
| Missing | 1 (0.0%) | 4 (0.0%) | >0.99 |
| Educational level c | |||
| None | 4 (0.0%) | 13 (0.0%) | 0.792 |
| Elementary school | 6 (0.0%) | 130 (0.4%) | <0.001 |
| Junior High school | 172 (1.3%) | 2063 (6.4%) | <0.001 |
| High School | 2997 (22.8%) | 7639 (23.8%) | 0.023 |
| University degree | 7278 (55.5%) | 11110 (34.7%) | <0.001 |
| Postgraduate degree/Master/Doctorate or higher | 2659 (20.3%) | 11076 (34.6%) | <0.001 |
| Missing | 1 (0.0%) | 3 (0.0%) | >0.99 |
| Birth mode | |||
| Spontaneous vaginal birth | 9625 (73.4%) | 19884 (62.1%) | <0.001 |
| Instrumental vaginal birth | 1284 (9.8%) | 2531 (7.9%) | <0.001 |
| Emergency cesarean section during labor | 1190 (9.1%) | 3423 (10.7%) | <0.001 |
| Emergency cesarean section before labor | 371 (2.8%) | 1954 (6.1%) | <0.001 |
| Elective cesarean section | 647 (4.9%) | 4242 (13.2%) | <0.001 |
| Type of hospital | |||
| Public | 12976 (98.9%) | 27412 (85.6%) | <0.001 |
| Private | 140 (1.1%) | 4615 (14.4%) | <0.001 |
| Missing | 1 (0.0%) | 7 (0.0%) | 0.452 |
| Type of healthcare providers who directly assisted birth | |||
| Midwife | 12946 (98.7%) | 26650 (83.2%) | <0.001 |
| Nurse | 5456 (41.6%) | 11828 (36.9%) | <0.001 |
| A student (i.e. before graduation) | 3863 (29.5%) | 2696 (8.4%) | <0.001 |
| Obstetrics registrar / medical resident (under post‐graduation training) | 2697 (20.6%) | 5767 (18%) | <0.001 |
| Obstetrics and gynecology doctor | 4311 (32.9%) | 20590 (64.3%) | <0.001 |
| I don't know (healthcare providers did not introduce themselves) | 1076 (8.2%) | 3661 (11.4%) | <0.001 |
| Other | 3571 (27.2%) | 2179 (6.8%) | <0.001 |
Scandinavia pertains to Sweden and Norway.
Following 12 WHO European countries were included: Italy (n = 10057), Croatia (n = 3211), Latvia (n = 3194), Portugal (n = 2430), Greece (n = 2200), Switzerland (n = 1415), Slovenia (n = 2534), Lithuania (n = 1192), Germany (n = 1294), Poland (n = 1842), France (n = 1409) and Romania (n = 1256).
Wording on education levels agreed among partners during the Delphi; questionnaire translated and back translated according to Professional Society for Health Economics and Outcomes Research (ISPOR) Task Force for Translation and Cultural Adaptation Principles of Good Practice guidelines (24).
The distribution of the included study population across the WHO European Region is displayed in Figure 2. Swedish participants (N = 7696/13117; 58.7%) were more in number as compared to Norwegian participants (N = 5421/13117; 41.3%) (Table S2), with differences observed for year of giving birth (p < 0.001), woman gave birth in same country where she was born (p = 0.004), age ranges 18–24 (p < 0.001), and 25–34 (p = 0.019), educational level from junior high school grade level upwards (p < 0.001), spontaneous and instrumental vaginal birth (p < 0.001), elective cesarean section (p = 0.03), type of hospital (p < 0.001), and type of healthcare provider who directly assisted birth if it was a nurse (p < 0.001), student (p < 0.001), obstetrics resident (p < 0.001) or obstetrics and gynecology physician (p < 0.001).
FIGURE 2.
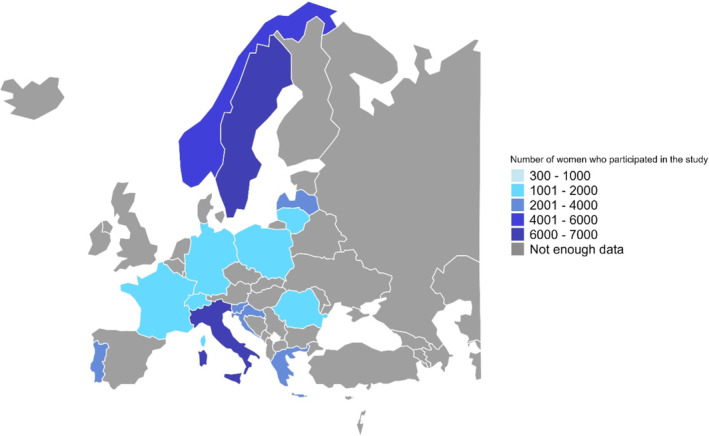
Total distribution of women according to the country where women gave birth. Note: Grey colour represents countries with no participants or fewer than 300 participants
3.1. Overall QMNC indexes
During the entire study period, the total QMNC index (Table 2) was significantly higher in Sweden and Norway (median: 325, IQR: 285–355) as compared to the other 12 WHO European countries (median: 315, IQR: 265–350, p < 0.001). When data were analyzed by QMNC subdomains, a higher median score was reported in Sweden and Norway than the 12 WHO European countries on three of the four subdomains: “provision of care” [median: 90 (IQR: 80–95) vs. median: 85 (IQR: 70–90), respectively, p < 0.001], “experience of care” [median: 90 (IQR: 75–95) vs. median: 80 (IQR: 65–90), respectively, p < 0.001] and “availability of physical and human resources” [median: 65 (IQR: 50–80) vs. median: 65 (IQR: 50–85), respectively, p < 0.001]. In the latter subdomain, even though the medians were similar, differences were exhibited in the IQR across the two populations, which was extracted from the density distribution of the populations. Regarding “reorganizational changes due to COVID‐19”, a lower median score was reported in Sweden and Norway as compared to 12 WHO European countries [median: 80 (IQR: 65–90) vs. median: 85 (IQR: 70–95) respectively, p < 0.001].
TABLE 2.
Total quality of maternal and newborn care (QMNC) index and by subdomain in Scandinavia vs. 12 WHO European Countries.
| Norway and Sweden | 12 WHO European countries | |||||
|---|---|---|---|---|---|---|
| QMNC domain | Median | 25th percentile | 75th percentile | Median | 25th percentile | 75th percentile |
| Provision of care | 90 | 80 | 95 | 85 | 70 | 90 |
| Experience of care | 90 | 75 | 95 | 80 | 65 | 90 |
| Availability of physical and human resources | 65 | 50 | 80 | 65 | 50 | 85 |
| Reorganizational changes due to the COVID‐19 pandemic | 80 | 65 | 90 | 85 | 70 | 95 |
| Total QMNC index | 325 | 285 | 355 | 315 | 265 | 350 |
Note: the 12 WHO European countries included: Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Switzerland, and Slovenia. Total sample size for women participating in QMNC Index for provision of care domain were N = 34983; for experience of care domain were N = 38415; for Availability of human and physical resources were N = 45151; for Reorganizational changes due to COVID‐19 were 45151; for the total QMNC index were N = 33171.
Abbreviations: IQR, interquartile range; QMNC, Quality of Maternal and Neonatal Care.
3.2. QMNC indexes over time
Changes in the QMNC index over time intervals during the COVID‐19 pandemic are outlined in Table S3 and visually displayed in Figure 3. For Sweden and Norway, the median scores (median: 310–345, IQR: 265–370, Mann‐Kendall test p < 0.726), displayed higher values than the 12 WHO European countries (median: 305–340, IQR: 255–360, Mann‐Kendall test p < 0.001). When investigating changes in QMNC index for the subdomain “reorganizational changes due to COVID‐19” over time (Figure 3e), Sweden and Norway started with an overall higher score in the beginning of the pandemic (March–May 2020), the 12 WHO European countries displayed higher scores soon thereafter, peaking in June–October 2022 (median 90, IQR: 75–95), whereas Sweden and Norway improved during the time interval October 2021–February 2022 (median 90, IQR: 75–95), declining to end with a lower median score of 87.5 (IQR: 80–99).
FIGURE 3.
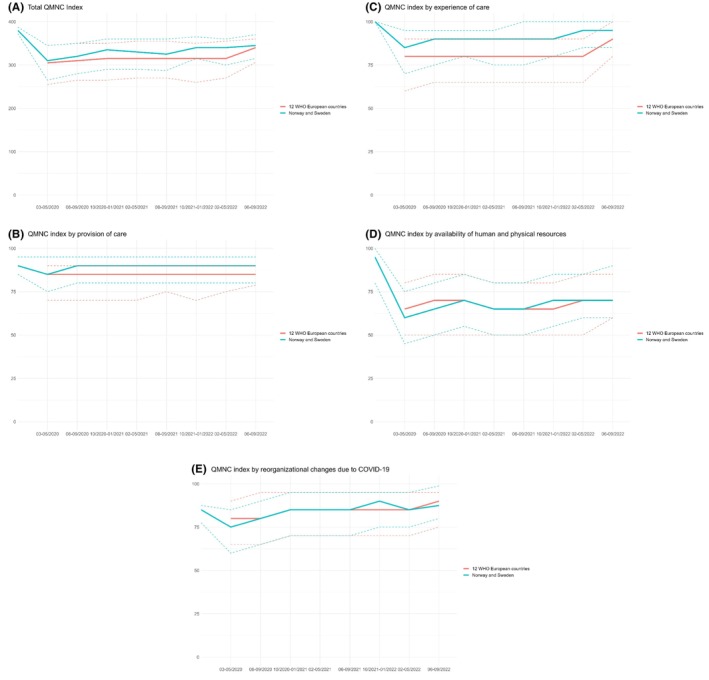
Quality of maternal and newborn care (QMNC) indexes by time in Norway and Sweden vs 12 WHO European Countries from 2020 to 2022 (N = 33 171). Note: Figures show the median QMNC index (undashed line) and interquartile range (dotted line). Scandinavia pertaining to Sweden and Norway; the 12 WHO European countries included: Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Switzerland, and Slovenia. Women participating A) QMNC index were N= 33,171; QMNC index for B) provision of care domain were N=34,983; C) experience of care domain were N=38,415; D) availability of human and physical resources were N=45,151; E) reorganizational changes due to COVID‐19 were 45,151. Abbreviation: QMNC, Quality of Maternal and Neonatal Care.
3.3. Quantile regression models
Results from the quantile models with the total QMNC index as dependent variable in all countries (Table 3), showed that when adjusting for relevant variables (geographical area, maternal age, educational level, mode of birth, migrant status, parity, type of hospital, and type of healthcare provider who directly assisted birth), women Sweden and Norway reported higher total QMNC indexes as compared to the other 12 WHO European countries. This was especially the case for the lower scores of the index (+3.20, +1.70, +0.90, p < 0.001 across all percentiles). When adjusted for the above mentioned variables, subsequent time periods (analyzed in 4 months periods) were significantly associated with higher total QMNC indexes in all the analyzed percentiles with slightly greater effect for the lower percentiles (change every 4 months of +0.71 in the 25th percentile, +0.61 in the 50th percentile, +0.49 in the 75th percentile, p < 0.001 for all percentiles). Younger women (ages: 18–24 years) reported significantly lower QMNC index scores (−2.2, −2.3, −1.3, p < 0.001 in all percentiles) as compared to women ages 25–34 years. Birth modes other than spontaneous vaginal birth had a significantly negative impact on all percentiles (p < 0.001) with emergency cesareans with greater effect (emergency cesarean section during labor: −7.5, −6, −4.6; emergency cesarean section before labor: −7.5, −5.9; −4.3). The presence of healthcare providers had a greater impact on women's reported experience, with midwives and nurses having a significant positive impact across all percentiles (midwife: +5.50, +5.00, +3.20; nurse: +2.20, +1.60, +0.70, p < 0.001 in all percentiles). Healthcare providers who did not present themselves by name had the greatest significant negative impact along all percentiles (−13.9, −13.4, −11.3, p < 0.001 in all percentiles).
TABLE 3.
Quantile models with total QMNC index in 14 countries as dependent variable, N = 33171.
| 25th percentile | 50th percentile | 75th percentile | ||||
|---|---|---|---|---|---|---|
| Coefficient (95%CI) | p‐value | Coefficient (95%CI) | p‐value | Coefficient (95%CI) | p‐value | |
| Subsequent time periods (4 months) | 0.71 (0.6; 0.8) | <0.001 | 0.61 (0.6; 0.7) | <0.001 | 0.49 (0.5; 0.5) | <0.001 |
| Norway and Sweden | 3.2 (2.9; 3.6) | <0.001 | 1.7 (1.4; 2) | <0.001 | 0.9 (0.7; 1.1) | <0.001 |
| 12 WHO European countries a | Ref | Ref | Ref | |||
| Age range | ||||||
| 18–24 | −2.2 (−2.9; −1.6) | <0.001 | −2.3 (−2.9; −1.8) | <0.001 | −1.3 (−1.7; −1) | <0.001 |
| 25–34 | Ref | Ref | Ref | |||
| 35–39 | 0 (−0.4; 0.4) | 0.984 | 0 (−0.3; 0.2) | 0.9 | 0.2 (0; 0.4) | 0.287 |
| ≥40 | 0.5 (−0.1; 1.1) | 0.362 | 0.6 (0.1; 1.1) | 0.196 | 0.7 (0.3; 1) | 0.043 |
| Educational level | ||||||
| None | −1.9 (−15.3; 11.6) | 0.889 | 2.2 (−4.1; 8.5) | 0.728 | 3.1 (−0.6; 6.8) | 0.399 |
| Elementary school | 2.4 (0.3; 4.6) | 0.262 | 1.2 (−0.5; 2.9) | 0.492 | 1.6 (0.1; 3.1) | 0.271 |
| Junior High school | 2.4 (1.7; 3.1) | 0.001 | 2.1 (1.6; 2.6) | <0.001 | 0.9 (0.6; 1.3) | 0.003 |
| High school | Ref | Ref | Ref | |||
| University degree | 0.1 (−0.2; 0.5) | 0.705 | −0.4 (−0.7; −0.2) | 0.099 | −0.5 (−0.6; −0.3) | 0.011 |
| Postgraduate/Master/Doctorate or higher | 1.4 (1; 1.8) | <0.001 | 0.2 (−0.1; 0.4) | 0.534 | −0.3 (−0.5; −0.1) | 0.158 |
| Mode of birth | ||||||
| Spontaneous vaginal birth | Ref | Ref | Ref | |||
| Instrumental vaginal birth | −2.7 (−3.2; −2.2) | <0.001 | −2.6 (−3; −2.2) | <0.001 | −1.6 (−1.9; −1.4) | <0.001 |
| Emergency cesarean section during labor | −7.5 (−8; −7) | <0.001 | −6 (−6.5; −5.5) | <0.001 | −4.6 (−4.9; −4.3) | <0.001 |
| Emergency cesarean section before labor | −7.5 (−8.3; −6.7) | <0.001 | −5.9 (−6.5; −5.3) | <0.001 | −4.3 (−4.9; −3.8) | <0.001 |
| Elective cesarean section | −6.1 (−6.7; −5.5) | <0.001 | −4.5 (−4.9; −4.1) | <0.001 | −3.3 (−3.6; −2.9) | <0.001 |
| Mother giving birth in the same country where she was born | ||||||
| No | 0.4 (−0.2; 1) | 0.494 | 1.1 (0.7; 1.6) | 0.008 | 1.6 (1.3; 1.8) | <0.001 |
| Yes | Ref | Ref | Ref | |||
| Parity | ||||||
| Primiparous | Ref | Ref | Ref | |||
| Multiparous | 4.6 (4.3; 4.8) | <0.001 | 3.4 (3.2; 3.6) | <0.001 | 2.2 (2; 2.4) | <0.001 |
| Type of hospital | ||||||
| Private | 6.9 (6.4; 7.3) | <0.001 | 5.8 (5.5; 6.1) | <0.001 | 4.8 (4.5; 5) | <0.001 |
| Public | Ref | Ref | Ref | |||
| Type of healthcare providers who directly assisted birth b | ||||||
| Midwife | 5.5 (5; 6) | <0.001 | 5 (4.6; 5.4) | <0.001 | 3.2 (2.8; 3.5) | <0.001 |
| Nurse | 2.2 (1.9; 2.5) | <0.001 | 1.6 (1.4; 1.8) | <0.001 | 0.7 (0.6; 0.9) | <0.001 |
| A student (eg before graduation) | 1 (0.6; 1.4) | 0.007 | 0.6 (0.3; 0.8) | 0.02 | 0.3 (0.1; 0.5) | 0.161 |
| Obstetrics registrar / medical resident (under post‐graduation training) | −1.9 (−2.2; −1.5) | <0.001 | −1.6 (−1.9; −1.3) | <0.001 | −1.1 (−1.3; −0.9) | <0.001 |
| Obstetrics and gynecology doctor | 0.2 (−0.1; 0.5) | 0.529 | 0 (−0.2; 0.3) | 0.88 | −0.1 (−0.3; 0.1) | 0.669 |
| I don't know (healthcare providers did not introduce themselves) | −13.9 (−14.4; −13.5) | <0.001 | −13.4 (−13.8; −12.9) | <0.001 | −11.3 (−11.7; −10.8) | <0.001 |
| Other | 1.2 (0.8; 1.6) | 0.005 | 1.2 (0.9; 1.5) | <0.001 | 1 (0.8; 1.2) | <0.001 |
12 WHO European countries included: Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Switzerland, and Slovenia.
The reference category for all types of healthcare providers is defined as the absence of them.
Quantile regression analyses for the total QMNC index and subdomains individually are shown in Table S5. When compared to the 12 WHO European countries, women in Sweden and Norway reported higher indexes for the subdomains “provision of care” (+5.00, +5.00, +5.00, p < 0.001 for all percentiles) and “experience of care” (+9.50, +6.70, +4.60, p < 0.001 for all percentiles), lower index for “reorganizational changes due to the COVID‐19” (−2.10, −3.10, −3.20, p < 0.001 for all percentiles), and no significant difference for “availability of physical and human resources.” Subsequent time periods (analyzed in 4 months periods) were not associated with higher QMNC indexes in the domain “provision of care” while it had a positive significant association in all the other domains (except for 50th percentile of the domain “availability of physical and human resources”) with higher effect for “experience of care” (+1.04, p < 0.001 in the 25th percentile; +0.83, p < 0.001 in the 50th percentile; +0.48, p = 0.037 in the 75th percentile) and “reorganizational changes due to COVID‐19” subdomains (+1.31 + 1.11, +0.81, p < 0.001 for all percentiles).
3.4. Supplementary information
A list of confounders with their description as used in quantile models is given in Table S9. The proportion of participants in the study as compared to expected number of births per country within the study period is given in Table S10. The original survey in English, as administered to the women participating in the study can be found as Table S11.
4. DISCUSSION
This large, cross‐sectional study, reporting the experiences of women giving birth across Europe during the COVID‐19 pandemic, found that the QMNC was higher in Sweden and Norway as compared to 12 WHO European countries (Croatia, France, Germany, Greece, Italy, Latvia, Lithuania, Poland, Portugal, Romania, Switzerland, and Slovenia). In the subdomain “reorganizational changes due to COVID‐19” however, Sweden and Norway were surpassed by the 12 WHO European countries. These findings suggest room for improvement and shared learning across the countries included in the study.
The COVID‐19 pandemic posed significant challenges to healthcare systems worldwide. 25 Maternal mortality, stillbirth, maternal stress, and depression increased during the pandemic. 25 , 26 , 27 , 28 , 29 , 30 , 31 One proposed explanation for this increase in adverse pregnancy outcomes was reduced access to healthcare services and the emergency restrictive policies put in place to limit the spread of the disease. 25
Using a multicounty sample, we observed that for Sweden and Norway the total QMNC index was higher as compared to 12 WHO European countries. Women giving birth in Sweden and Norway perceived higher standards regarding the “provision of care,” “experience of care” and “availability of physical and human resources,” Regarding “reorganizational changes due to COVID‐19,” this was the only subdomain where women reported lower scores for Sweden and Norway in the beginning of the COVID‐19 pandemic as compared to 12 other European countries. Eventually, here too Sweden and Norway QMNC scores became equivalent to the 12 WHO European countries. However, these findings may underline a slower, initial response time in Sweden and Norway. For Sweden, the healthcare system's response to the spread of COVID‐19 early on in the pandemic was deemed inadequate to uphold quality protection measures. 32 For example, a general lack of personal protective equipment (PPE) was evident in the Sweden in the beginning of the pandemic, and this may have influenced the subdomain scores for “reorganizational changes due to COVID‐19” negatively. 13 , 14 , 33 It is also important to point out that the initial increase of the Swedish and Norwegian scores align with the recommendations to vaccinate pregnant women. 34 During the later stages of the pandemic, the availability of PPE was better and probably affected the score in a positive direction. 33 This is an important area of learning for the development of preparedness programs in the face of future pandemics.
Scandinavian countries, like Sweden and Norway, have developed very different systems of maternal and neonatal care with respect to the training and regulation of midwives, nurses, and the development of obstetrics both as a branch of general practice and as a specialty as compared with most other European countries. 3 , 4 These standards were exemplified in examining maternal‐neonatal adverse outcomes during the COVID‐19 pandemic, where Sweden and Norway reported lower rates of maternal mortality, decreased instances of preterm births, and the maintenance of quality prenatal care services. 35 , 36 In contrast, several WHO European countries faced difficulties in sustaining optimal maternal and neonatal care, especially early on during the pandemic. 25 , 37
Sweden and Norway took vastly different approaches in how to handle the pandemic. Despite having nearly identical governmental systems and initially facing similar infection threats, Sweden implemented far less stringent countermeasures compared to Norway. 38 While Norway's government responded similarly to many other European nations, Sweden attracted international attention for its voluntary approach, which largely consisted of recommendations and guidelines rather than strict regulations. 38 Scholars have described that Sweden viewed the pandemic more as a public health‐crisis while Norway viewed the pandemic as a healthcare‐crisis, and the countermeasures taken by the government reflected this. 38 Sweden did not close schools or children's activities for example. Despite the completely different approaches taken in the two countries, public trust in the government's measures to protect the public remained high in both Sweden and Norway. 38 Confidence in healthcare and politicians was high among pregnant women before the pandemic and rose even further during it, despite significant concerns about their own health, their unborn babies, and their partners. 39 However, during the first phase of the pandemic, health‐related worries surged dramatically for pregnant women, their partners, and families. 39 , 40 In Sweden, pregnant women's worries were comparable to those of the elderly. 39
Although the total QMNC remained relatively high in Sweden and Norway, one could argue that the lower total QMNC index seen at the beginning of the pandemic in the Sweden and Norway group might reflect some of this worry. The expectations for maternal and neonatal care were very high, and deviations in the care provided could have directly impacted the total QMNC index score, particularly in postnatal care. However, the IMAgiNE EURO questionnaire was not designed to explore postnatal care indicators, and other authors have described such indicators as lacking in both Sweden and Norway during the pandemic. 41
A study evaluating postnatal care conducted two months after childbirth found that COVID‐19 restrictions, which excluded partners from postnatal wards, significantly decreased partners' satisfaction with care. 41 Partners felt staff shortages led to deficiencies in care, which likely also affected the women. 41 These findings suggest that while Swedish women perceived health care during childbirth as good before the pandemic, they noticed a decline in its quality during the pandemic.
On the other hand, it is plausible that efficient healthcare infrastructure, established prenatal and perinatal care programs, and effective public health interventions contributed to the improved QMNC scores observed in Sweden and Norway, as reported by the women participating in this study. The total QMNC index improved over time in both Sweden and Norway, as well as in the other 12 WHO European countries, indicating that healthcare organizations adapted to the pandemic and became less affected by pandemic‐related concerns over time.
One of the main strengths of the current study was the use of a standardized validated questionnaire that comprehensively covered key quality measures based on the WHO Quality Standards for maternal and neonatal care. 22 The survey was disseminated widely using social media and local champions, leading to a sizable population sample across countries in Europe. Rigorous translation of the survey to local languages using standard operating procedures further added to the success of the dissemination of the survey during the pandemic. 23 However, the generalizability of the results needs to be interpreted with caution, as the cross‐sectional design of the study provided only a snapshot of the participant experiences at a given time, and it was not possible to follow up participants at a later time point. Additionally, despite the large number of women who answered the survey, they represent a small proportion of the total number of individuals who underwent pregnancy and childbirth during the COVID‐19 pandemic in Europe. The potential for recall bias must also be considered, as the questionnaires were completed by women during the pandemic, which was the sole time frame required for participation in the study. However, it is well established that maternal childbirth experiences remain vividly etched in the memories of birthing women for many years. Consequently, we do not anticipate that the responses provided were significantly affected by recall bias. 42 , 43 , 44
There was also a relative over‐representation of highly educated women in our study. It is well known that women with higher education are more empowered to express their views freely and have better access to internet resources. 45 This may lead to selection bias in the study population and a relative under‐estimation of the actual quality of care as highly educated mothers may be overly critical in their viewpoints 45 but may also receive prejudicially better care than less educated and poorer women. Additionally, the cohort may have had selection bias regarding other characteristics which we have been unable to account for in the current study.
Although European countries share many political, economic, and demographic commonalities, our study highlights that there are differences within and between countries, and significant gaps regarding healthcare services in maternal and neonatal care. Policymakers should prioritize long‐term investments in maternal and neonatal healthcare infrastructure, ensuring that facilities are adequately equipped to handle surges in demand during public health crises, such as during the COVID‐19 pandemic. 46 , 47 Ensuring that health facilities have a sufficient number of qualified maternal health providers, have access to essential medical supplies and equipment, with alternate supply chains planned and secured, especially during crises, are lessons to be learned for future pandemics and emergencies. Further, countries should commit to uphold quality standards, including those related to positive experiences of care. By encouraging collaborative initiatives and sharing best practices, strategies, and lessons learned, national health systems can collectively enhance their preparedness and response capabilities for future pandemics. 46 , 47 International collaboration can be fostered through regional health organizations and collaborative research projects such as the IMAgiNE EURO network.
5. CONCLUSION
Although Sweden and Norway upheld a better quality of maternal and neonatal healthcare during the COVID‐19 pandemic, there is an opportunity for enhancement and mutual learning both within Europe and globally. The divergent trends in the quality of maternal and neonatal healthcare during the COVID‐19 pandemic across Europe emphasize the need for specific policies and strategic investments in healthcare systems to ensure resiliency and person‐centered care even during population emergencies. Policymakers should prioritize strengthening reproductive, maternal, and newborn health infrastructure and human resource capacity and promote international collaboration to guarantee the sustained delivery of high‐quality maternal and neonatal care in the presence of future challenges.
AUTHOR CONTRIBUTIONS
Marzia Lazzerini conceived the IMAgiNE EURO Project, with inputs from all partners. Mehreen Zaigham conceived the study, with major inputs from Karolina Linden, Helen Elden, Marzia Lazzerini and additional inputs from all other authors. All authors promoted the surveys and supported the process of data collection. Stefano delle Vedove analyzed data, with major inputs from Mehreen Zaigham, Ilaria Mariani and the other authors. Mehreen Zaigham wrote the first draft, with major inputs from all authors. All authors have approved the final version of the manuscript for submission.
FUNDING INFORMATION
This study was supported by the Ministry of Health, Rome, Italy, in collaboration with the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste, Italy; the Swedish Research Council Grant 2022–00208 (MZ); and the Swedish governmental funding of clinical research ALF YF00054 (MZ). EPIUnit (UIDB/04750/2020), ITR (LA/P/0064/2020), and HEI–Lab R&D Unit (UIDB/05380/2020, https://doi.org/10.54499/UIDB/05380/2020) are financed by the FCT (Portuguese Ministry of Science, Technology and Higher Education).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The study was approved by the Institutional Review Board of the coordinating center: the IRCCS Burlo Garofolo Trieste (IRB‐BURLO 05/2020) on July 15, 2020. The study protocol was also reviewed and approved by the ethical committees of four countries where local regulations implied this further step: Portugal (protocol approved by Instituto de Saude Pública da Universidade do Porto, CE20159), Germany (Bielefeld University ethics committee, 2020–176), Latvia (Riga Stradins University Research Ethics Committee 22–2/140/2021 on March 16, 2021) and Norway (approved by Norwegian Regional Committee for Medical Research Ethics, considered to be outside the remit of the Norwegian Act on Medical and Health Research 2020/213047). Since no sensitive personal data was collected, and the survey was completely anonymous, permission from the Swedish Ethical Review Authority was not required. The study was conducted according to General Data Protection (GDPR) regulations. Participation in the online survey was voluntary and anonymous. Anonymity in data collection during the survey phase was ensured by not collecting any information that could disclose participants' identity. Data transmission and storage were secured by encryption. Women were informed prior to the survey about the objectives and methods of the study, including their rights in declining participation, and were provided a written consent before responding to the questionnaires (Table S12).
Supporting information
Table S1.
Table S2.
Table S3.
Table S4.
Table S5.
Table S6.
Table S7.
Table S8.
Table S9.
Table S10.
Table S11.
Table S12.
Table S13.
ACKNOWLEDGMENTS
The authors would like to thank all project partners and IMAgiNE EURO study group (Table S13), partner's institutions and volunteers who helped in the development and dissemination of the questionnaire. We thank all respondents who took time to respond to this survey.
Zaigham M, Linden K, Elden H, et al. Trends in the quality of maternal and neonatal care in Sweden and Norway as compared to 12 WHO European countries: A cross‐sectional survey investigating maternal perspectives during the COVID‐19 pandemic. Acta Obstet Gynecol Scand. 2024;103:2485‐2498. doi: 10.1111/aogs.14994
Karolina Linden and Helen Elden contributed equally.
REFERENCES
- 1. Maternal and newborn—Mortality/causes of death. [Internet]. Accessed 2024‐02‐04. Available from: https://www.who.int/data/gho/data/themes/topics/topic‐details/mca/maternal‐and‐newborn‐‐‐mortality‐causes‐of‐death
- 2. The Age of Social Democracy. Norway and Sweden in the Twentieth Century. [Internet]. Accessed 2024‐02‐04. Available from: https://reviews.history.ac.uk/review/1184
- 3. Pregnancy and childbirth in Norway. [Internet]. Accessed 19 January, 2024. Available at: https://www.norden.org/en/info‐norden/pregnancy‐and‐childbirth‐norway
- 4. Pregnancy (Sweden). [Internet]. Accessed 19 January, 2024. Available at: https://www.informationsverige.se/en/jag‐har‐fatt‐uppehallstillstand/vard‐och‐halsa/graviditet.html#:~:text=Pregnancy%20and%20maternal%20care&text=You%20go%20to%20the%20maternity,%2C%20childbirth%20and%20breast%2Dfeeding
- 5. Births and deaths 1970–2022 and projection 2023–2070. [Internet]. Accessed 19 January, 2024. Available at: https://www.scb.se/en/finding‐statistics/statistics‐by‐subject‐area/population/population‐projections/population‐projections/pong/tables‐and‐graphs/births‐and‐deaths‐by‐sex‐and‐country‐of‐birth‐and‐projection/
- 6. Births (Norway). [Internet]. Accessed 19 January, 2024. Available at: https://www.ssb.no/en/befolkning/fodte‐og‐dode/statistikk/fodte
- 7. Galková G, Böhm P, Hon Z, Heřman T, Doubrava R, Navrátil L. Comparison of frequency of home births in the member states of the EU between 2015 and 2019. Glob Pediatr. Health. 2022;9:2333794X211070916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gamst N. Municipal midwifery services in Norway‐ The realization of policy guidelines within municipal midwifery services in the light of the coordination reform. 2020. Available at: https://www.duo.uio.no/bitstream/handle/10852/34514/Master‐Nora‐Gamst.pdf?sequence=2&isAllowed=y
- 9. Miani C, Wandschneider L, Batram‐Zantvoort S, et al. Individual and country‐level variables associated with the medicalization of birth: multilevel analyses of IMAgiNE EURO data from 15 countries in the WHO European region. Int J Gynaecol Obstet. 2022;159(1):9‐21. [DOI] [PubMed] [Google Scholar]
- 10. Lazzerini M, Valente EP, Covi B, et al. Rates of instrumental vaginal birth and cesarean and quality of maternal and newborn health care in private versus public facilities: results of the IMAgiNE EURO study in 16 countries. Int J Gynaecol Obstet. 2022;159(1):22‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Costa R, Rodrigues C, Dias H, et al. Quality of maternal and newborn care around the time of childbirth for migrant versus nonmigrant women during the COVID‐19 pandemic: results of the IMAgiNE EURO study in 11 countries of the WHO European region. Int J Gynaecol Obstet. 2022;159(1):39‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chertok I, Medvedik R, Arendt M, et al. Factors associated with exclusive breastfeeding at discharge during the COVID‐19 pandemic in 17 WHO European region countries. Int Breastfeed J. 2022;17:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zaigham M, Linden K, Sengpiel V, et al. Large gaps in the quality of healthcare experienced by Swedish mothers during the COVID‐19 pandemic: a cross‐sectional study based on WHO standards. Women Birth. 2022;S1871‐5192:10‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lazzerini M, Covi B, Mariani I, et al. Quality of facility‐based maternal and newborn care around the time of childbirth during the COVID‐19 pandemic: online survey investigating maternal perspectives in 12 countries of the WHO European region. Lancet reg Health Eur. 2022;13:100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Labrusse C, Abderhalden‐Zellweger A, Mariani I, et al. Quality of maternal and newborn care in Switzerland during the COVID‐19 pandemic: a cross‐sectional study based on WHO quality standards. Int J Gynaecol Obstet. 2022;159(Suppl 1):70‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nedberg IH, Vik ES, Kongslien S, et al. Quality of health care around the time of childbirth during the COVID‐19 pandemic: results from the IMAgiNE EURO study in Norway and trends over time. Int J Gynaecol Obstet. 2022;159(1):85‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Drandić D, Drglin Z, Mihevc Ponikvar B, et al. Women's perspectives on the quality of hospital maternal and newborn care around the time of childbirth during the COVID‐19 pandemic: results from the IMAgiNE EURO study in Slovenia, Croatia, Serbia, and Bosnia‐Herzegovina. Int J Gynaecol Obstet. 2022;159(1):54‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pumpure E, Jakovicka D, Mariani I, et al. Women's perspectives on the quality of maternal and newborn care in childbirth during the COVID‐19 pandemic in Latvia: results from the IMAgiNE EURO study on 40 WHO standards‐based quality measures. Int J Gynaecol Obstet. 2022;159(1):97‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Costa R, Barata C, Dias H, et al. Regional differences in the quality of maternal and neonatal care during the COVID‐19 pandemic in Portugal: results from the IMAgiNE EURO study. Int J Gynaecol Obstet. 2022;159(1):137‐153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Otelea MR, Simionescu AA, Mariani I, et al. Women's assessment of the quality of hospital‐based perinatal care by mode of birth in Romania during the COVID‐19 pandemic: results from the IMAgiNE EURO study. Int J Gynaecol Obstet. 2022;159(1):126‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453‐1457. [DOI] [PubMed] [Google Scholar]
- 22. World Health Organization . Standards for improving quality of maternal and newborn care in health facilities. 2016. Accessed 19 January, 2024. Available at: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/improving‐mnh‐health‐facilities/en/
- 23. Lazzerini M, Argentini G, Mariani I, et al. WHO standards‐based tool to measure women's views on the quality of care around the time of childbirth at facility level in the WHO European region: development and validation in Italy. BMJ Open. 2022;12:e048195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient‐reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94‐104. [DOI] [PubMed] [Google Scholar]
- 25. Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID‐19 pandemic on maternal and perinatal outcomes: a systematic review and meta‐analysis. Lancet Glob Health. 2021;9:e759‐e772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shukla VV, Rahman AF, Shen X, et al. Trends in maternal outcomes during the COVID‐19 pandemic in Alabama from 2016 to 2021. JAMA Netw Open. 2022;5:e222681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McClymont E, Albert AY, Alton GD, et al. Association of SARS‐CoV‐2 infection during pregnancy with maternal and perinatal outcomes. JAMA. 2022;327:1983‐1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Llotey J, Chatterjee S, Kew T, et al. SARS‐CoV‐2 positivity in offspring and timing of mother‐to‐child transmission: living systematic review and meta‐analysis. BMJ. 2022;376:e067696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID‐19 pan‐ demic on maternal and child mortality in low‐income and middle‐income countries: a modelling study. Lancet Glob Health. 2020;8:e901‐e908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alabi QK, Oyedeji AS, Kayode OO, Kajewole‐Alabi DI. Impact of COVID‐19 pandemic on mother and child health in sub‐Saharan Africa—A review. Pediatr Res. 2023;94:1278‐1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sun S, Savitz DA, Wellenius GA. Changes in adverse pregnancy outcomes associated with the COVID‐19 pandemic in the United States. JAMA Netw Open. 2021;4:e2129560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ludvigsson JF. How Sweden approached the COVID‐19 pandemic: summary and commentary on the National Commission Inquiry. Acta Paediatr. 2023;112:19‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Akerstrom M, Carlsson Y, Sengpiel V, et al. Working conditions for hospital‐based maternity and neonatal health care workers during extraordinary situations—A pre−/post COVID‐19 pandemic analysis and lessons learned. Sex Reprod Healthc. 2022;33:100755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Norman M, Magnus MC, Söderling J, et al. Neonatal outcomes after COVID‐19 vaccination in pregnancy. JAMA. 2024;331:396‐407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Engjom H, Aabakke AJM, Klungsøyr K, et al. COVID‐19 in pregnancy‐characteristics and outcomes of pregnant women admitted to hospital because of SARS‐CoV‐2 infection in the Nordic countries. Acta Obstet Gynecol Scand. 2021;100:1611‐1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Magnus MC, Oakley LL, Hansen AV, et al. Fetal death after the introduction of COVID‐19 mitigation measures in Sweden, Denmark and Norway: a registry‐based study. Sci Rep. 2022;12:20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Coxon K, Turienzo CF, Kweekel L, et al. The impact of the coronavirus (COVID‐19) pandemic on maternity care in Europe. Midwifery. 2020;88:102779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Askim J, Bergström T. Between lockdown and calm down. Comparing the COVID‐19 responses of Norway and Sweden. Local Gov Stud. 2022;48:291‐311. [Google Scholar]
- 39. Naurin E, Markstedt E, Stolle D, et al. Pregnant under the pressure of a pandemic: a large‐scale longitudinal survey before and during the COVID‐19 outbreak. Eur J Pub Health. 2021;31:7‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Linden K, Domgren N, Zaigham M, Sengpiel V, Andersson ME, Wessberg A. Being in the shadow of the unknown—Swedish women's lived experiences of pregnancy during the COVID‐19 pandemic, a phenomenological study. Women Birth. 2022;35:440‐446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Olander P, Berglin L, Naurin E, et al. The impact of exclusion due to COVID‐19 restrictions on partners' satisfaction with Swedish hospital postnatal ward care: a multi‐methods approach. Birth. 2024;51:612‐619. [DOI] [PubMed] [Google Scholar]
- 42. Bossano CM, Townsend KM, Walton AC, Blomquist JL, Handa VL. The maternal childbirth experience is more than a decade after delivery. Am J Obstet Gynecol. 2017;217:342. [DOI] [PubMed] [Google Scholar]
- 43. Simkin P. Just another day in a woman's life? Women's long‐term perceptions of their first birth experience. Birth. 1991;18:203‐210. [DOI] [PubMed] [Google Scholar]
- 44. Simkin P. Just another day in a woman's life? Part II: nature and consistency of women's long‐term memories of their first birth experiences. Birth. 1992;19:64‐81. [DOI] [PubMed] [Google Scholar]
- 45. Rishard M, Fahmy FF, Senanayake H, et al. Correlation among experience of person‐centered maternity care, provision of care and women's satisfaction: cross sectional study in Colombo. Sri Lanka PLoS One. 2021;16:e0249265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Maintaining the provision and use of services for maternal, newborn, child and adolescent health and older people during the COVID‐19 pandemic: lessons learned from 19 countries. World Health Organization. 2021:12‐21. Accessed 19 January, 2024. Available at: https://www.who.int/publications/i/item/9789240040595 [Google Scholar]
- 47. Health and Care Workforce in Europe: Time to Act. WHO Regional Office for Europe; 2022. [Internet]. Accessed 19 January, 2024. Available at: https://www.who.int/europe/publications/i/item/9789289058339 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Table S2.
Table S3.
Table S4.
Table S5.
Table S6.
Table S7.
Table S8.
Table S9.
Table S10.
Table S11.
Table S12.
Table S13.


