Abstract
Background:
A labral injury contributes to glenohumeral instability. The Anterior Labral Circumferential Onlay Technique (ALCOT) reconstructs the labrum using the long head of the biceps tendon.
Hypothesis:
The ALCOT would restore glenohumeral joint stability in a cadaveric model without glenoid bone loss (1) comparable to the native state and (2) comparable to the Latarjet procedure.
Study Design:
Controlled laboratory study.
Methods:
A total of 10 fresh-frozen cadaveric shoulders were tested using a 6 degrees of freedom robotic arm in 5 consecutive states: (1) native, (2) capsular repair, (3) labral tear, (4) ALCOT, and (5) Latarjet procedure. Biomechanical testing consisted of 80 N of anteroinferior force and 50 N of compression in 90° of humerothoracic abduction. Lateral displacement of the humeral head and the force ratio during a dislocation were measured.
Results:
The mean lateral translation of the humeral head during a dislocation in the native state was 6.5 ± 2.2 mm and decreased to 5.4 ± 2.4 mm in the labral tear state (P < .001). The mean lateral translation of the humeral head was restored to 6.4 ± 2.2 mm (P > .99) with the ALCOT, showing no difference from the native state. The Latarjet procedure restored the mean force ratio during a dislocation to 1.3 ± 0.6 but failed to restore lateral translation, with a value of 5.6 ± 2.8 mm (P = .003 vs native; P = .94 vs labral tear). The mean force ratio was 1.8 ± 0.1 in the native state, decreased to 1.1 ± 0.4 in the labral tear state, and was 1.4 ± 0.4 (P < .27) with the ALCOT, showing no difference from the native state.
Conclusion:
The ALCOT is a novel technique for labral reconstruction that may have a role in the treatment of anterior glenohumeral instability in the setting of a deficient labrum without bone loss. In this study, the ALCOT restored the force ratio and lateral translation of the humeral head compared to the native state. The Latarjet procedure restored the force ratio but not lateral translation of the humeral head compared to the native state.
Clinical Relevance:
This study proposes and biomechanically validates the ALCOT as a surgical technique for labral reconstruction that may have a role in treating patients with chronic anterior shoulder instability in the setting of a deficient labrum.
Keywords: shoulder, AC joint, instability, glenoid labrum, biomechanics, chronic shoulder instability, recurrent dislocation
Anterior glenohumeral instability most commonly affects a young, physically active population. 6 After failed nonoperative treatment, the current standard of care is arthroscopic Bankart repair. The procedure consists of reattaching the displaced labrum in conjunction with capsuloligamentous plication. Recurrent instability remains a challenge, especially in young patients, with recurrence rates reported up to 22%.16,24,27 The surgeon may encounter poor tissue quality in patients with multiple dislocations or recurrence after arthroscopic repair. Some experts recommend primary bony procedures to treat anterior instability, even when there is no bone loss, to avoid recurrent instability.18,26,33 One frequently utilized surgical technique is the Latarjet procedure. 19 The Latarjet procedure transfers the coracoid to the anteroinferior glenoid to lengthen the glenoid arc, with the additional benefit of the sling effect, created from the conjoint tendons. 31 The Latarjet procedure has excellent midterm to long-term results in patients with relevant bone loss3,10,25 but does not lead to superior results over revision Bankart repair in patients with subcritical glenoid bone loss and recurrent anterior shoulder instability.5,30
In the setting of chronic glenohumeral instability, the labrum may be of poor quality because of repetitive trauma from recurrent instability events or prior surgery. 2 In these clinical settings, difficulty repairing the labrum may arise. As proposed solutions, some technical notes describe augmentation with allografts such as the semitendinosus or gracilis tendon. 21 In cases of an irreparable labrum, other authors have reconstructed the capsule and labrum entirely using an allograft with promising results.4,9 However, the availability, cost, and legal parameters regarding the use of allografts vary significantly between countries, which presents a major challenge. Alternatively, some authors have suggested the use of hamstring tendon autografts. 9 Potential downsides include the risk of harvest site morbidity, pain, and hamstring weakness compared to the other leg as well as an additional intervention on the leg. 11 Other nonanatomic options for anterior glenohumeral stabilization are dynamic anterior stabilization, the augmentation of primary Bankart repair with an additional long head of the biceps tendon (LHBT), and the use of the semitendinosus tendon as a subscapular sling.17,23 The LHBT as an attached intra-articular tendon, by shuttling the tendon through a drilled hole from the center of the humeral head to the bicipital groove, is another option that has been previously used to help stabilize the glenohumeral joint. 35
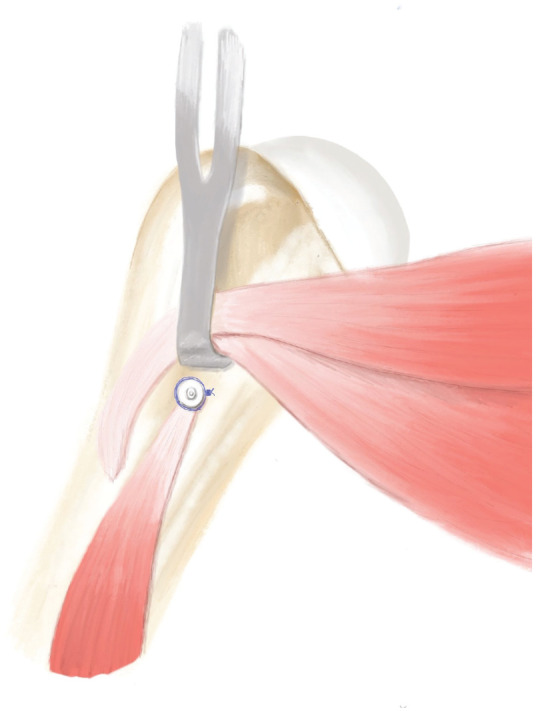
Although labral reconstruction is relatively uncommon in shoulders, it is frequently used in the hip with various graft options.8,29 By transferring the concept from the hip to the shoulder joint, a salvage procedure using the LHBT for recurrent shoulder instability has been described. This technique is called the Anterior Labral Circumferential Onlay Technique (ALCOT) and uses the onsite, proximally attached autologous LHBT to reconstruct the labrum (Figure 1).
Figure 1.
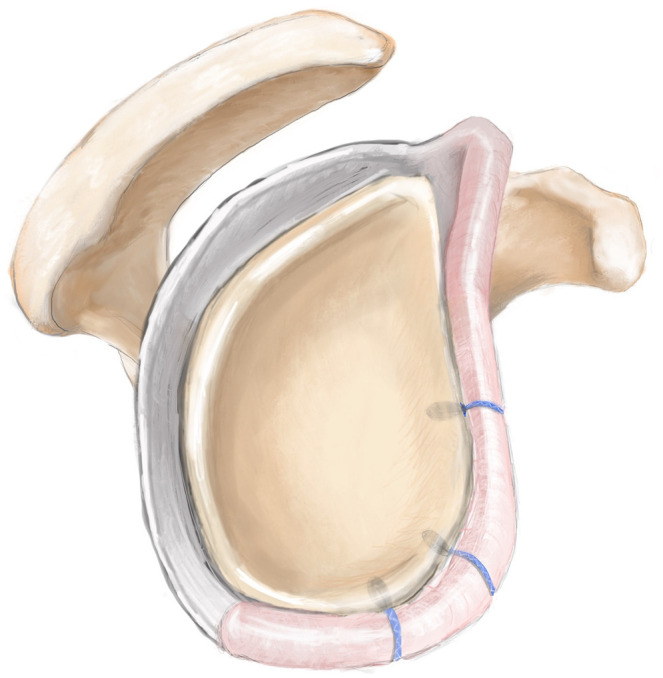
Representation of the Anterior Labral Circumferential Onlay Technique with the long head of the biceps tendon secured to the glenoid rim by 3 knotless all-suture anchors in the 3-o’clock, 4:30, and 6-o’clock positions.
The purpose of this study was to investigate the biomechanical properties of the ALCOT using a 6 degrees of freedom robotic arm. The secondary aim was to analyze the ability of the ALCOT to prevent anteroinferior dislocations and restore glenohumeral stability. Last, the presented novel technique was compared to various states including the native state, a labral tear, and the Latarjet procedure. We hypothesized that the ALCOT would restore glenohumeral joint stability in a cadaveric model (1) comparable to the native state and (2) comparable to the Latarjet procedure.
Methods
Specimen Preparation
A total of 10 fresh-frozen cadaveric shoulders (obtained with permission from Science Care; age range, 36-65 years) were tested in this study. 34 The specimens were donated to a tissue bank for medical research and then purchased by our institution. The use of cadaveric specimens did not require institutional review board approval at our institution. Specimens were excluded based on age >65 years, a history of shoulder injuries, shoulder surgery, osteoarthritis, joint stiffness, degenerative joint disease, osteoporosis, or other joint abnormalities. Specimens were examined by 2 orthopaedic surgeons (M.E.D.H. and R.O.D.H.) to ensure that no exclusion criteria existed. The shoulders were thawed at room temperature (72°F) overnight before testing.
All skin, subcutaneous tissue, and muscles distal to the deltoid were removed. The glenohumeral joint capsule, rotator cuff musculature, and both origins and insertions of the coracobrachialis and short head of the biceps tendon were left intact on the humerus. For the scapula, the clavicle and deltoid musculature were removed, and the origins of the rotator cuff muscles were left intact. The medial aspect of the scapula was potted in a rectangular prism-shaped mold with polymethyl methacrylate (PMMA; Fricke Dental), with the medial border of the scapula parallel to the horizontal plane. The lateral shaft of the humerus was potted 10 cm distal to the superior tip of the humerus in a cylindrical mold. The specimens were moistened with saline solution every 20 minutes throughout preparation and immediately before testing.
Each scapula was rigidly clamped to a custom fixture mounted to a 6-axis universal force torque sensor (ATI Industrial Automation) on a pedestal, and each humerus was rigidly clamped to a custom fixture mounted to the end effector of a 6 degrees of freedom robotic arm (KR60; KUKA), as shown in Figure 2. simVITRO software (Cleveland Clinic) was used to control the robotic arm. A joint coordinate system was established by digitizing landmarks using a coordinate measuring machine (ROMER Absolute Arm; Hexagon) according to the Internation Society of Biomechanics (ISB) standard. 36
Biomechanical Testing
During all tests, the shoulder joint was maintained in 90° of humerothoracic abduction. In vivo, placing the arm in this position requires both scapulothoracic and glenohumeral motion; however, the scapula was clamped in the present study. To overcome this limitation, a study by Ludewig et al 22 in which participants were asked to perform basic humerothoracic movements, including abduction, while measuring the relative positions of their scapula, humerus, thorax, and clavicle was referenced. That study provided the relative glenohumeral angles corresponding to 90° of humerothoracic abduction that were used in the present study: 53° of elevation, 58° of external rotation, and –18° of plane of elevation.
In the native state, each specimen was set to neutral by applying a 50-N compressive load and 0-N anterior and inferior loads and defining this position as 0 mm of anterior, lateral, and inferior translation. From there, each specimen underwent an initial test to determine the appropriate amount of anterior and inferior displacement that then served as a baseline for future tests. In the initial test, a 50-N compressive load was maintained, while an 80-N force was applied in the sagittal plane at a 45° angle between the anterior and inferior axes over a period of 10 seconds. The corresponding anterior and inferior displacement values were recorded. Then, in each state including the native state, a dislocation test was performed. In this test, a 50-N compressive load was maintained, while the joint was driven to the same position as the previously recorded positions on the anterior and inferior axes over a period of 10 seconds. The amount of force needed to displace the shoulder throughout this motion was recorded. The joint was inspected between tests to ensure that no bone loss occurred during testing.
Outcome Measures
There were 2 outcome measures analyzed. The first was the amount of lateral displacement of the humeral head that occurred during the dislocation. This represents the height of the glenoid rim that needed to be overcome by the humerus for the shoulder to dislocate; thus, higher lateral translation represents more stability. The second was the force ratio, which is the amount of anteroinferior force needed to dislocate the shoulder divided by the amount of compressive force. The reason for calculating this value is that the stability of the shoulder joint depends on the amount of compression applied. With more compression, the joint requires more force in the sagittal plane to dislocate. In the dislocation test, the target compressive force was set to 50 N, but based on the system dynamics and the control algorithm, the actual compressive force did not track 50 N perfectly. By looking only at the total amount of force in the sagittal plane, the dislocation force recorded would depend on the speed of the movement and the efficacy of the control algorithm in tracking 50 N of compressive loading. By normalizing the sagittal plane load to the compressive load, a force ratio was calculated, which was less dependent on the specific parameters of the control algorithm and the specific testing setup and which was more generalizable to any amount of compressive force.
Testing States
Each specimen underwent biomechanical testing in 5 consecutive states: (1) native, (2) capsular repair, (3) labral tear, (4) ALCOT, and (5) Latarjet procedure.
Native: Each prepared specimen was tested in its native state.
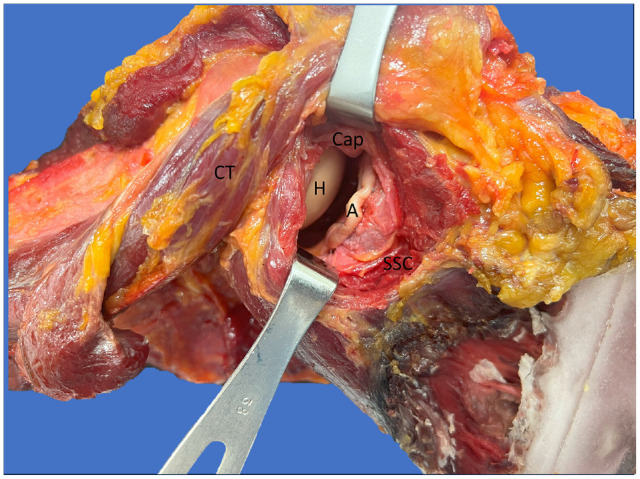
Capsular repair: The subscapularis (SSC) tendon was split horizontally from lateral to medial in the middle one-third of the tendon, the capsule and tendon were separated from each other, the capsule was then opened similarly from medial to lateral parallel to the tendon split (Figure 3), and the capsule and muscle were closed together through continuous suture repair. Then, the repaired capsule state was tested. This state was used to measure the influence of capsular repair on joint stability.
Labral tear: The stitches of the SSC tendon were reopened as well as the capsule's stitches. The labrum was then removed from the anteroinferior glenoid rim (2- to 7-o’clock position) and from the joint. The capsule and SSC tendon were closed as described before.
ALCOT: This technique can be performed either arthroscopically or open. For technical reasons in the testing setup, we used an open approach. The SSC tendon was reopened between the upper one-third and lower two-thirds along its fibers. Then, the joint was opened by opening the capsule's sutures as described before. At the anteroventral arm in the distal subpectoral position, the biceps tendon was cut with a scalpel (similar to the step of cutting the tendon for biceps tenodesis) (Figure 4). Inside the joint, a forceps was placed on top of the intra-articular portion of the LHBT, similar to the hook test, and the distal part of the tendon was pulled into the joint. The proximal attachment at the supraglenoid tubercle was left intact. Overall, 3 knotless all-suture anchors (1.8-mm Knotless FiberTak with No. 2 sutures; Arthrex) were placed in the 3-o’clock, 4:30, and 6-o’clock positions on the anterior glenoid rim using a cannula and a flexible drill (Spear; Arthrex), and the anchors were next inserted into their respective holes and, with gentle impaction, secured in the holes. Then, the sutures were pulled upward to secure the placement of the suture anchor. The biceps tendon was grasped and held under tension to pierce it with blue repair sutures by using a piercing device (Scorpion; Arthrex) that passed the sutures back and through the LHBT, placing 3 mattress sutures along the LHBT in the respective 3-o’clock, 4:30, and 6-o’clock positions (Figure 4). Then, each repair suture was passed through the loop of its corresponding shuttling suture, the shuttling suture was pulled firmly, and with tightening of the shuttling suture, the LHBT was secured to the glenoid rim, reconstructing the anterior labrum (Figure 5). The distal end of the LHBT was not sutured to the posterior labral stump. Finally, the capsule and SSC tendon were closed as described before.
Latarjet procedure: The capsule and SSC tendon were opened. The procedure was performed following the senior author's (P.J.M.) technique. 15 The coracoid was cut at its base (25 mm from the tip) using an oscillating saw with the conjoint tendons remaining intact. Next, 2 parallel holes were drilled into the coracoid using a coracoid drilling guide (Arthrex). Then, 2 corresponding K-wires were drilled into the glenoid using a guide with placement parallel to the glenoid rim. 15 The guide was removed, and 2 cannulated screws were placed, using the K-wires as guides, to secure the coracoid flush with the glenoid (cannulated screw, partially threaded, 3.75 mm × 30 mm; Arthrex). The capsule as well as the SSC tendon and muscle were closed (Figure 6).
Figure 2.

Experimental setup of a right shoulder with a 6 degrees of freedom robotic arm (posterior view).
Figure 3.
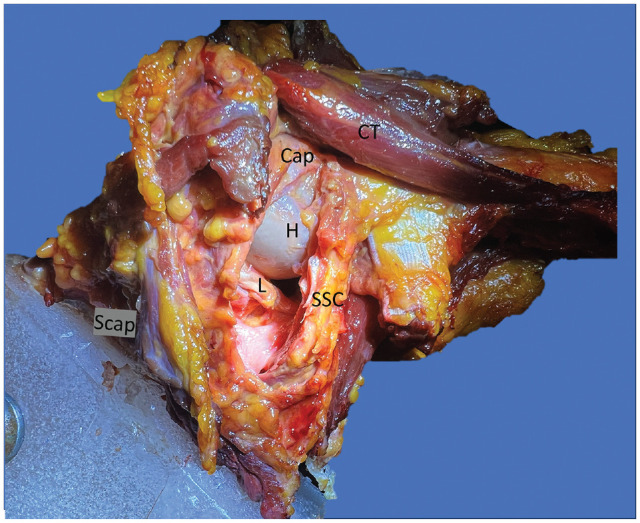
Left shoulder specimen with an opened capsule in the surgical setting. Major structures of importance are labeled. CT, conjoint tendon; H, humeral head; L, labrum; Scap, scapula; SSC, subscapularis tendon; Cap, capsule.
Figure 4.
Representation of subpectoral tenodesis. After performing the ALCO Technique the skin and underlying tissue is opened at the distal border of the subpectoral muscle. After identifying the distal part of the LHBT it is pulled out of the sulcu, shortened and then proximally attached to the subpectoral proximal humerus using a suture anchor.
Figure 5.
Right shoulder specimen with the Anterior Labral Circumferential Onlay Technique (ALCOT [A]) before capsular closure . CT, conjoint tendon; H, humeral head; SSC, subscapularis tendon. Cap, capsule.
Figure 6.

Right shoulder specimen with the Latarjet procedure (L). CT, conjoint tendon; G, glenoid; Scap, scapula; SSc, subscapularis tendon.
Statistical Analysis
To match the repeated-measures design of the study, 1-factor random-intercepts linear mixed-effects models were used to compare testing states. A separate model was created for each of the 2 primary outcome measures: lateral translation of the humeral head and force ratio. An unstructured covariance matrix was assumed for all linear mixed-effects models, and analysis of variance was run to determine if the effect of the shoulder state was a significant factor for each outcome measure. Estimated marginal means were reported, and the Tukey method was used to conduct all post hoc pairwise comparisons among the 5 shoulder states. Residual diagnostics were inspected to ensure a model fit, and those assumptions were met. Statistical software R (Version 4.0.0) 28 was used for all plots and analyses.
Results
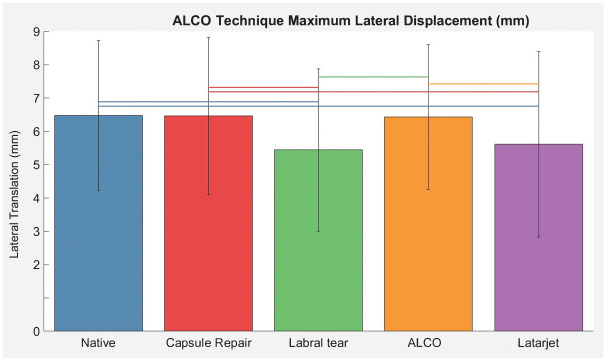
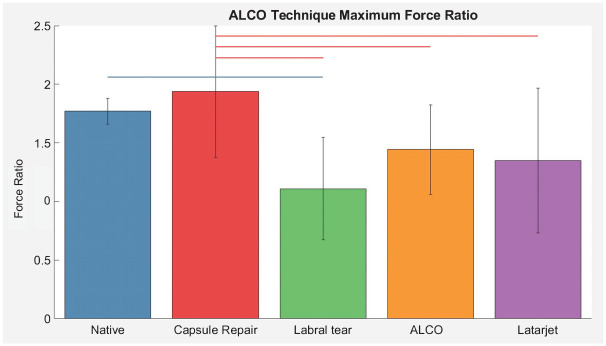
No significant differences were found between the native and capsular repair states for either outcome. Compared to the native state, a labral tear significantly decreased lateral translation of the humeral head during a dislocation from 6.5 ± 2.2 to 5.4 ± 2.4 mm (P < .001) and decreased the force ratio from 1.8 ± 0.1 to 1.1 ± 0.4 (P = .002), corresponding to a decrease from 90 to 55 N with 50 N of compressive loading (Figure 7). The ALCOT restored these values to 6.4 ± 2.2 mm and 1.4 ± 0.4, respectively, showing no statistically significant difference from the native state. The Latarjet procedure restored the force ratio to 1.3 ± 0.6 but failed to restore lateral translation, with a value of 5.6 ± 2.8 mm (P = .003 vs native; not significantly different vs labral tear) (Figure 8). The results for lateral displacement of the humeral head and force ratio are shown in Figures 7 and 8, respectively. P values for the differences are listed in Tables 1 and 2.
Figure 7.
Lateral translation by testing state. Error bars represent 1 standard deviation. A horizontal line represents a significant difference between 2 states. ALCO, Anterior Labral Circumferential Onlay.
Figure 8.
Force ratio by testing state. Error bars represent 1 standard deviation. A horizontal line represents a significant difference between 2 states. ALCO, Anterior Labral Circumferential Onlay.
Table 1.
Force Ratio a
| Difference | P | |
|---|---|---|
| ALCOT vs capsular repair | −0.49 | .03 |
| ALCOT vs labral tear | 0.34 | .25 |
| ALCOT vs Latarjet procedure | 0.10 | .98 |
| ALCOT vs native | −0.33 | .27 |
| Capsular repair vs labral tear | 0.83 | .00 |
| Capsular repair vs Latarjet Procedure | 0.59 | .01 |
| Capsular repair vs native | 0.17 | .83 |
| Labral tear vs Latarjet procedure | −0.24 | .57 |
| Labral tear vs native | −0.66 | .00 |
| Latarjet procedure vs native | −0.42 | .09 |
ALCOT, Anterior Labral Circumferential Onlay Technique. Bold P values indicate significant differences (P < 0.05).
Table 2.
Lateral Translation a
| Difference, mm | P Value | |
|---|---|---|
| ALCOT vs capsular repair | −0.03 | >.99 |
| ALCOT vs labral tear | 0.99 | .00 |
| ALCOT vs Latarjet procedure | 0.81 | .01 |
| ALCOT vs native | −0.05 | >.99 |
| Capsular repair vs labral tear | 1.02 | .00 |
| Capsular repair vs Latarjet procedure | 0.85 | .00 |
| Capsular repair vs native | −0.02 | >.99 |
| Labral tear vs Latarjet procedure | −0.17 | .94 |
| Labral tear vs native | −1.04 | .00 |
| Latarjet procedure vs native | −0.86 | .00 |
ALCOT, Anterior Labral Circumferential Onlay Technique. Bold P values indicate significant differences (P < 0.05).
Discussion
The most important finding of this study is that the presented ALCOT restored glenohumeral stability (ie, both the force ratio and lateral translation) compared to the native state. Further, in this cadaveric model without bone loss, the Latarjet procedure restored the force ratio but not lateral translation compared to the native state.
Recurrent glenohumeral instability remains a frequently observed problem in shoulder surgery. While patients with significant bone loss are successfully treated with bony procedures such as the Latarjet procedure or iliac crest grafting, there is no consensus on the best treatment approach for patients with subcritical bone loss. Therapeutic options comprise the abovementioned bony procedures and dynamic or static stabilization surgery.
The Latarjet procedure lengthens the articular arc, creating a sling effect through the conjoint tendons and capsular imbrication or reinforcement from the coracoacromial ligament. However, the nonanatomic nature and complication rates of 6% to 7% make it a suboptimal option for standardized use in patients without significant bone loss. 13
In our study, the Latarjet procedure restored the force ratio to the native state but failed to restore lateral translation. In contrast, the presented ALCOT restored both. It seems that lateral translation could be directly or indirectly dependent on the bumper-like function of the capsulolabral complex. While labral reconstruction is a well-established concept for the hip joint, there is a paucity of literature on static labral reconstruction. 29 Thus, we found no previous biomechanical evaluation in the literature to directly compare our results with. Acar et al 1 reported 2 case reports in which the biceps tendon was used for labral reconstruction with promising preliminary results. Lobao et al 20 reported the biomechanical results of biceps augmentation to Bankart repair for chronic anterior instability, with close to native restoration of the glenohumeral position. The Latarjet procedure remained superior in scenarios with >20% critical bone loss. 20 Although that investigation was different than the present study, the results seem to be comparable.
Evaluating labral reconstruction with other tendons than the LHBT for patients with recurrent instability, Dewing et al 9 reported the outcomes of anterior labral reconstruction using a semitendinosus or tibialis anterior allograft. Their study included patients with massive anterior instability in 20 shoulders, with 14 remaining stable after 3.8 years of follow-up and 6 shoulders failing, thus requiring revision surgery (3 underwent revision stabilization with tibialis anterior tendon allografts, 1 underwent glenohumeral fusion, and 2 underwent Latarjet procedures). The authors concluded that labral reconstruction may be used as a salvage procedure for young patients with end-stage shoulder instability or collagen disorders. 9 Even though Dewing et al 9 presented a high revision rate, their preliminary clinical results are strengthened by the biomechanical evaluation of our study. The ALCOT restored the force ratio and lateral translation to the native state. Benefits of the present study include the argument for the use of an autologous tendon without the need to detach the tendon from its origin, the risk of harvest morbidity, or additional surgery on the leg. The negative clinical effects of biceps tenodesis have been shown to be minimal from a biomechanical perspective.12,32
Applicable clinical scenarios for this technique range from failed arthroscopic Bankart repair to treating anterior labral periosteal sleeve avulsion lesions and poor labral tissue that is insufficient for Bankart repair. In addition to our investigation, it is important to also evaluate previously studied dynamic approaches. Willard 35 shuttled the LHBT through a transhumeral drilled tunnel to prevent anterior dislocations, they evaluated the technique in a case series of 10 shoulders, observing only 1 failure. Similarly, Collin and Lädermann 7 utilized a proximal tenotomized LHBT, shuttling it through the SSC tendon and attaching it to the anterior glenoid, thus creating a sling around the SSC tendon. Mehl et al 23 reported less relative anterior translation than isolated Bankart repair with this technique. The dynamic LHBT sling and dynamic conjoint tendon sling techniques could reduce anteroinferior translation and partially restore glenohumeral stability in patients with anterior shoulder instability with 20% anteroinferior glenoid defects compared with Bankart repair. 14 No comparison between static and dynamic stabilization techniques could be found in the literature.
Limitations
This study has several limitations that should be considered when interpreting the data. First, muscle and capsuloligamentous tension could not be evaluated because of our study's cadaveric design. However, by repairing the shoulder capsule and SSC tendon in each state of testing, the integrity of the static stabilizers and capsuloligamentous complex was restored. Second, the cadaveric setup did not include muscle forces, indicating that the conjoint tendons were not directly loaded in the comparative Latarjet procedure state. To mitigate this, the insertions of the coracobrachialis and short head of the biceps tendon were left intact and attached to the coracoid process while repairing the SSC tendon to maintain the static sling effect of these structures crucial to the Latarjet procedure. Third, the specimens did not have any bone loss, making it unclear whether the procedure will work in patients with subcritical bone loss. Fourth, there remains the possibility of a type 2 error because of the small number of specimens. Last, the present study reports the force ratio and degree of humeral displacement at time zero, as is typical for biomechanical studies. Additional in vivo studies are needed to interpret the healing response of the LHBT with the ALCOT and the subsequent changes that may or may not occur.
Conclusion
In our study, the ALCOT restored anteroinferior glenohumeral stability. Biomechanically, the ALCOT restored the force ratio and lateral translation to native values. Thus, the ALCOT may be an alternative salvage treatment option in chronic instability cases with degenerated or deficient labral tissue without glenoid bone loss. The Latarjet procedure restored the force ratio compared to the native state but not lateral translation of the humeral head.
Footnotes
Final revision submitted February 1, 2024; accepted February 12, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study received partial support from Arthrex for in-kind products supplied. P.J.M. has received a royalty or license from Arthrex, consulting fees from Arthrex, and nonconsulting fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
ORCID iDs: Rony-Orijit Dey Hazra  https://orcid.org/0000-0002-3530-6726
https://orcid.org/0000-0002-3530-6726
Peter J. Millett  https://orcid.org/0000-0002-8298-3746
https://orcid.org/0000-0002-8298-3746
References
- 1. Acar B, Kose O, Kircil C, Canbora K, Demirtas M. A novel technique for labral reconstruction using long head of biceps tendon: Duru technique. Cureus. 2021;13(2):2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alashkham A, Alraddadi A, Felts P, Soames R. Histology, vascularity and innervation of the glenoid labrum. J Orthop Surg (Hong Kong). 2018;26(2):230949901877090. [DOI] [PubMed] [Google Scholar]
- 3. Ali ZS, Hurley ET, Jamal MS, et al. Low rate of recurrent instability following the open Latarjet procedure as a revision procedure for failed prior stabilization surgery. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2110-2117. [DOI] [PubMed] [Google Scholar]
- 4. Braun S, Horan MP, Millett PJ. Open reconstruction of the anterior glenohumeral capsulolabral structures with tendon allograft in chronic shoulder instability. Oper Orthop Traumatol. 2011;23(1):29-36. [DOI] [PubMed] [Google Scholar]
- 5. Calvo E, Luengo G, Morcillo D, Foruria AM, Valencia M. Revision arthroscopic Bankart repair versus arthroscopic Latarjet for failed primary arthroscopic stabilization with subcritical bone loss. Orthop J Sports Med. 2021;9(5):23259671211001809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cameron KL, Mauntel TC, Owens BD. The epidemiology of glenohumeral joint instability: incidence, burden, and long-term consequences. Sports Med Arthrosc Rev. 2017;25(3):144-149. [DOI] [PubMed] [Google Scholar]
- 7. Collin P, Lädermann A. Dynamic anterior stabilization using the long head of the biceps for anteroinferior glenohumeral instability. Arthrosc Tech. 2018;7(1):e39-e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cooper JD, Dekker TJ, Ruzbarsky JJ, Pierpoint LA, Soares RW, Philippon MJ. Autograft versus allograft: the evidence in hip labral reconstruction and augmentation. Am J Sports Med. 2021;49(13):3575-3581. [DOI] [PubMed] [Google Scholar]
- 9. Dewing CB, Horan MP, Millett PJ. Two-year outcomes of open shoulder anterior capsular reconstruction for instability from severe capsular deficiency. Arthroscopy. 2012;28(1):43-51. [DOI] [PubMed] [Google Scholar]
- 10. Ernat JJ, Rakowski DR, Hanson JA, et al. High rate of return to sport and excellent patient-reported outcomes after an open Latarjet procedure. J Shoulder Elbow Surg. 2022;31(8):1704-1712. [DOI] [PubMed] [Google Scholar]
- 11. Essen C, McCallum S, Eriksson K, Barenius B. Minimal graft site morbidity using autogenous semitendinosus graft from the uninjured leg: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2022;30(5):1639-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Giphart JE, Elser F, Dewing CB, Torry MR, Millett PJ. The long head of the biceps tendon has minimal effect on in vivo glenohumeral kinematics. Am J Sports Med. 2012;40(1):202-212. [DOI] [PubMed] [Google Scholar]
- 13. Hurley ET, Schwartz LB, Mojica ES, et al. Short-term complications of the Latarjet procedure: a systematic review. J Shoulder Elbow Surg. 2021;30(7):1693-1699. [DOI] [PubMed] [Google Scholar]
- 14. Kang Y, Wang L, Wang M, et al. Bankart repair with transferred long head of the biceps provides better biomechanical effect than conjoined tendon transfer in anterior shoulder instability with 20% glenoid defect. Arthroscopy. 2022;38(9):2628-2635. [DOI] [PubMed] [Google Scholar]
- 15. Katthagen JC, Anavian J, Tahal DS, Millett PJ. Arthroscopic remplissage and open Latarjet procedure for the treatment of anterior glenohumeral instability with severe bipolar bone loss. Arthrosc Tech. 2016;5(5):e1135-e1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kennedy MI, Murphy C, Dornan GJ, et al. Variability of reporting recurrence after arthroscopic Bankart repair: a call for a standardized study design. Orthop J Sports Med. 2019;7(5):2325967119846915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Klungsøyr JA, Vagstad T, Klungsøyr PJ, Hellevik AI, Drogset JO. Dynamic and static stabilization of anterior shoulder instability with the subscapular sling procedure. Arthrosc Tech. 2021;10(7):e1773-e1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kramer J, Gajudo G, Pandya NK. Risk of recurrent instability after arthroscopic stabilization for shoulder instability in adolescent patients. Orthop J Sports Med. 2019;7(9):2325967119868995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49(8):994-997. [PubMed] [Google Scholar]
- 20. Lobao MH, Abbasi P, Murthi AM. Long head of biceps transfer to augment Bankart repair in chronic anterior shoulder instability with and without subcritical bone loss: a biomechanical study. J Shoulder Elbow Surg. 2022;31(5):1062-1072. [DOI] [PubMed] [Google Scholar]
- 21. Lobo FL, Conforto Gracitelli ME, Malavolta EA, et al. No clinical or radiographic difference seen in arthroscopic Bankart repair with knotted versus knotless suture anchors: a randomized controlled trial at short-term follow-up. Arthroscopy. 2022;38(6):1812-1823. [DOI] [PubMed] [Google Scholar]
- 22. Ludewig PM, Hassett DR, LaPrade RF, Camargo PR, Braman JP. Comparison of scapular local coordinate systems. Clin Biomech (Bristol, Avon). 2010;25(5):415-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mehl J, Otto A, Imhoff FB, et al. Dynamic anterior shoulder stabilization with the long head of the biceps tendon: a biomechanical study. Am J Sports Med. 2019;47(6):1441-1450. [DOI] [PubMed] [Google Scholar]
- 24. Miettinen SSA, Kiljunen T, Joukainen A. Anterior glenohumeral instability treated with arthroscopic Bankart operation: a retrospective 5-year follow-up study. Orthop Traumatol Surg Res. 2021;107(5):102943. [DOI] [PubMed] [Google Scholar]
- 25. Mook WR, Petri M, Greenspoon JA, Horan MP, Dornan GJ, Millett PJ. Clinical and anatomic predictors of outcomes after the Latarjet procedure for the treatment of anterior glenohumeral instability with combined glenoid and humeral bone defects. Am J Sports Med. 2016;44(6):1407-1416. [DOI] [PubMed] [Google Scholar]
- 26. Olds M, Ellis R, Donaldson K, Parmar P, Kersten P. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med. 2015;49(14):913-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Panzram B, Kentar Y, Maier M, Bruckner T, Hetto P, Zeifang F. Mid-term to long-term results of primary arthroscopic Bankart repair for traumatic anterior shoulder instability: a retrospective study. BMC Musculoskelet Disord. 2020;21(1):1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. R Core Team. R Foundation for Statistical Computing with additional packages lmer and emmeans. Published online 2020. Accessed May 20, 2020. https://cran.r-project.org/bin/windows/base/
- 29. Rahl MD, LaPorte C, Steinl GK, O’Connor M, Lynch TS, Menge TJ. Outcomes after arthroscopic hip labral reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2020;48(7):1748-1755. [DOI] [PubMed] [Google Scholar]
- 30. Rollick N, Ono Y, Kurji HM, et al. Long-term outcomes of the Bankart and Latarjet repairs: a systematic review. Open Access J Sports Med. 2017;8:97-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Schulze-Borges J, Agneskirchner JD, Bobrowitsch E, et al. Biomechanical comparison of open and arthroscopic Latarjet procedures. Arthroscopy. 2013;29(4):630-637. [DOI] [PubMed] [Google Scholar]
- 32. Shavana G, Cronjé JY, Mcduling C, et al. A biomechanical study on the effect of long head of biceps tenotomy on supraspinatus load and humeral head position during shoulder abduction. J Shoulder Elbow Surg. 2022;31(6):1294-1299. [DOI] [PubMed] [Google Scholar]
- 33. Waltenspül M, Ernstbrunner L, Ackermann J, Thiel K, Galvin JW, Wieser K. Long-term results and failure analysis of the open Latarjet procedure and arthroscopic Bankart repair in adolescents. J Bone Joint Surg Am. 2022;104(12):1046-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Waltz RA, Brown J, Brady AW, et al. Biomechanical evaluation of posterior shoulder instability with a clinically relevant posterior glenoid bone loss model. Am J Sports Med. 2023;51(9):2443-2453. [DOI] [PubMed] [Google Scholar]
- 35. Willard DP. The Nicola operation for recurrent dislocations of the shoulder. Ann Surg. 1936;103(3):438-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wu G, Siegler S, Allard P, et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion, part I: ankle, hip, and spine. J Biomech. 2002;35(4):543-548. [DOI] [PubMed] [Google Scholar]