Abstract
Aim:
Exploring the healthcare costs and resource use among privately insured US patients with post-traumatic stress disorder (PTSD).
Methods:
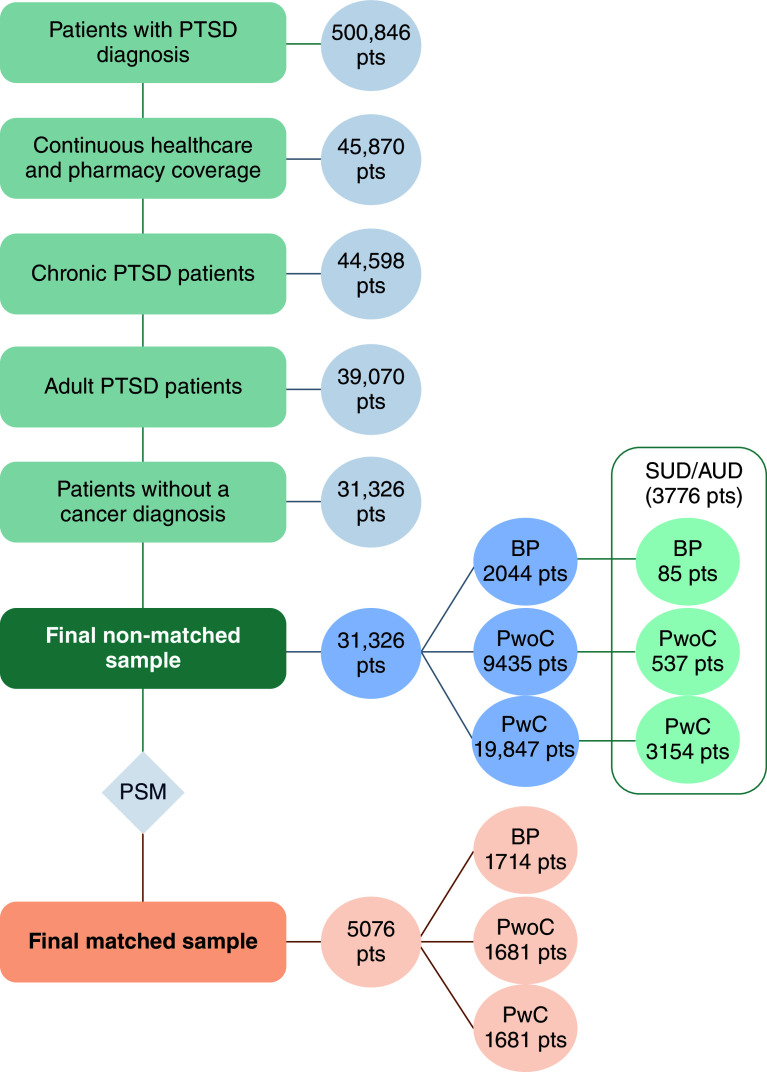
This study used Merative MarketScan data. The index date was defined as the first PTSD claim. Study period included a 1-year pre-index and 2-year post-index follow-up. Cases with only acute PTSD, cancer, or insurance gap during the study period were excluded. The PTSD with (PwC) and PTSD without comorbidities (PwoC) cohorts were defined by the presence/absence of comorbid mental health conditions (schizophrenia, bipolar and major depressive disorder). Baseline PTSD (BP) cohort included PwoC cases with only index PTSD event and without FDA-approved PTSD medications or psychotherapy. Sub-analysis is conducted among patients with PTSD and substance/alcohol use disorder. Study cohorts were matched in a 1:1:1 ratio.
Results:
The matched sample included 5076 patients (1681 PwC, 1681 PwoC, 1714 BP). PwC patients had higher 2-year PTSD-related costs than PwoC and BP patients ($3762 vs $1750 and $841; all p < 0.001). The same trend was noted among all-cause and anxiety-related costs. PwC patients had higher 2-year PTSD-related inpatient and emergency department (ED) rates than PwoC (10.2% vs 1.7% and 6.8% vs 2.6%, all p < 0.001) and inpatient and outpatient rates than BP (10.2% vs 2.1% and 98.0% vs 93.1%; all p ≤ 0.004). The sub-analysis had 3776 patients (3154 PwC, 537 PwoC, 85 BP). PwC had higher 2-year PTSD-related costs than PwoC and BP ($7668 vs $2919 and $1,483; all p < 0.001). The same trend was noted in all-cause and anxiety-related costs. PwC also had higher 2-year PTSD-related inpatient and ED rates than PwoC (25.6% vs 10.4% and 12.7% vs 5.2%; all p < 0.001) and inpatient and outpatient rates than BP (25.6% vs 8.2% and 95.5% vs 84.7%; all p < 0.001).
Conclusion:
PTSD is associated with high healthcare costs and resource use. The highest economic burden was observed in patients with PTSD and mental health comorbidities.
Keywords: alcohol use disorder, disease severity, economic burden, healthcare costs, hospitalization, mental health, post-traumatic stress disorder, real-world evidence, resource use, substance use disorder
Plain language summary
Healthcare Costs & resource use of patients with post-traumatic stress disorder (PTSD)
What is this article about?
The research evaluated the economic burden of patients with PTSD classified by disease severity. Healthcare costs and resource use were assessed during the 2-year period after the diagnosis of PTSD. In addition, study outcomes were also explored among patients diagnosed with PTSD and substance/alcohol use disorder (SUD/AUD).
What were the results?
All-cause and PTSD-related healthcare costs and resource use were explored among Baseline PTSD, PTSD without comorbidities and patients with PTSD and mental health comorbidities. The most relevant results were:
Patients with PTSD and comorbidities had higher total all-cause and PTSD-related costs than PTSD without comorbidities and Baseline PTSD
The majority of healthcare costs occurred during the first year after PTSD diagnosis in all study cohorts
Patients diagnosed with PTSD and SUD/AUD had higher healthcare costs, with the highest expenses noted among patients with PTSD and comorbidities
Patients with PTSD and SUD/AUD and mental comorbidities had higher usage rates of hospitalizations and emergency department visits than Baseline PTSD and PTSD without comorbidities
What do the results mean?
PTSD is associated with large healthcare costs and resource use, with the highest economic burden observed in patients with PTSD and comorbidities.
Tweetable abstract
#post-traumaticStressDisorder (#PTSD) is associated with high #HealthcareCosts and #ResourceUse per patient, especially in #PTSDwithComorbidities. Co-occurrence of #SubstanceUseDisorder or #AlcoholUseDisorder among patients with PTSD yielded higher #EconomicBurden for #USHealthcare.
Post-traumatic stress disorder (PTSD) is a psychiatric syndrome characterized by intrusive symptoms of re-experiencing memories of a traumatic event, avoidance, negative alterations in cognition and mood and marked alterations in arousal and reactivity following exposure to trauma [1]. Although the results may vary by population and trauma types, roughly 10% of adults exposed to severe trauma develop some form of PTSD despite the resilience of biological systems [2]. Trauma exposure disbalances the release of hormones, neurotransmitters and other mediators by the persistent alteration of hypothalamic-pituitary-adrenal axis activity, leading to PTSD [3]. PTSD symptoms can persist beyond three months and lead to the chronic stage of disease with a risk of lasting over an individual's lifetime [1,4,5].
PTSD is frequently associated with comorbid psychiatric disorders, especially major depressive disorder (MDD), due to similarities in pathophysiological mechanisms [3]. As such, disease management may overlap with the management of other psychiatric conditions. American Psychological Association (APA) clinical practice guideline provides strong recommendations for several psychotherapy approaches and conditional recommendations for certain pharmacological treatments [5]. The US FDA has approved only sertraline and paroxetine for PTSD treatment, while guidelines also propose the use of off-label medications, including other antidepressants, antipsychotics and anticonvulsants [6–8].
Studies of the US population report a 1-year PTSD prevalence of 2.3% to 9.1% among civilians and 6.7% to 50.2% among military personnel. Although a precise contemporary estimate of the PTSD burden in the US is still lacking, available data suggest that female gender, Native American/Alaskan heritage, younger age and lower income are risk factors [9]. Additionally, patients with PTSD are associated with an increased risk of premature death, with approximately 1.2 and 1.8-times the mortality rate reported in non-PTSD civilians and veterans, respectively [10]. Trauma also has significant negative long-term effects on the emotional, functional and physical well-being of patients [11].
In 2018, the estimated total economic burden of PTSD in the US was $232.2 billion higher than in the population without PTSD ($19.6 thousand per patient). Excess expenditures were higher in the military population compared with civilian ($25.7 and $18.6 thousand per patient, respectively), mostly driven by direct healthcare costs. Unemployment among civilians and disability in the military population were also large drivers for the high economic burden [10]. In the real-world setting, psychotherapy and medication utilization rates among patients with PTSD were seen to reduce over longer time periods. These decreasing trends were followed by a decline in healthcare costs, outpatient services, inpatient visits and length of hospital stay. During a 2-year observation period following PTSD diagnosis, payer expenditures decreased by 20.1% per patient with PTSD [12].
To the authors knowledge, currently available publications depicting the economic PTSD burden in the US are either outdated, briefly explored healthcare expenditures as a side topic, conducted in a small samples or combined real-world evidence with assumptions from literature.
Objectives
This study aimed to comprehensively assess the healthcare costs and resource utilization among patients with chronic PTSD across healthcare settings in the US. Findings are compared between patients with chronic PTSD stratified by estimated patients' severity. Additionally, a sub-group analysis evaluated study outcomes within the patients diagnosed with chronic PTSD and substance/alcohol use disorder (SUD/AUD).
Methodology
Data source
This study was conducted using US insurance claims data from the Merative MarketScan® Commercial and Medicare Part B claims database. This database consists of medical and prescription data for over 273 million individuals, encompassing employees, their spouses and dependents covered by employer-sponsored private health insurance in the US [13]. The study evaluated insurance data claims captured between 1 November 2017 and 31 October 2022.
Study population
The study population was identified based on the pre-defined inclusion/exclusion criteria to ensure a homogenous pool of patients with chronic PTSD.
Inclusion criteria:
Patients diagnosed with chronic PTSD based on the International Classification of Diseases – Clinical Modification (ICD-10-CM) codes (Supplementary Appendix, Table A1)
Adults ≥18 years of age
Exclusion criteria:
A gap (at least 1 day) in health plan or pharmaceutical coverage during the observational period (1-year pre-index and 2-year follow-up period)
Patients with only acute PTSD diagnosis during the observational period (Supplementary Appendix, Table A2)
Patients with a cancer diagnosis during the observational period (Supplementary Appendix, Table A3). Majority of cancer patients are claimed with the high healthcare costs and they are excluded as potential outliers which may significantly impact study results
Study design & cohort selection
Patients diagnosed with chronic PTSD were captured in the database between 1 November 2017 and 31 October 2022. The index date was defined as the first PTSD diagnosis and the study observational period consisted of 1-year pre-index and 2-year post-index follow-up (Figure 1), during which patients were required to have continuous healthcare and pharmaceutical coverage. Based on the chronic PTSD diagnosis and severity, patients were assigned to one of three study cohorts: baseline PTSD (BP), PTSD without comorbidities (PwoC) and PTSD with comorbidities (PwC). Patients with only one PTSD claim (index date admission) and without a diagnosis of MDD, bipolar disorder, or schizophrenia during the 2-year follow-up period were assigned to the BP cohort. In addition, patients in the BP cohort did not receive FDA-approved medications or psychotherapy during the study observational period. Patients with more than one PTSD claim (other than index date admission) were stratified into the PwC and PwoC cohorts. Based on previously published analyses, the PwoC cohort included patients without MDD, bipolar disorder, or schizophrenia claims during the 2-year follow-up period, while patients with these complex mental health comorbidities during the follow-up were categorized in PwC cohort [14,15]. MDD, bipolar disorder and schizophrenia were captured based on the relevant ICD-10-CM codes (Supplementary Appendix, Table A4). FDA-approved medications were identified via relevant National Drug Code (NDC) codes (Supplementary Appendix, Table A5), while psychotherapies were captured using current procedural terminology (CPT) codes (Supplementary Appendix, Table A6).
Figure 1. . Study design.
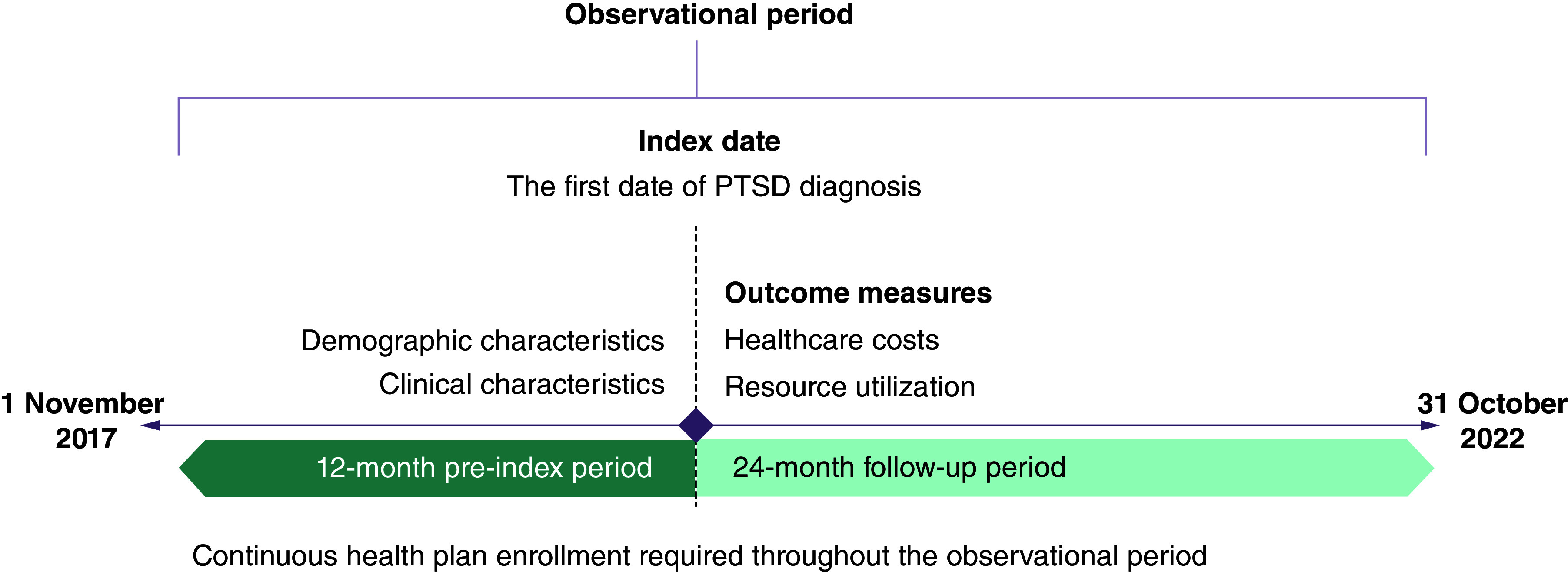
PTSD: Post-traumatic stress disorder.
Demographic characteristics of the study population were assessed on the index date, while clinical characteristics (assessed via the Charlson Comorbidity Index [CCI]) were evaluated during the 1-year pre-index period. Outcome measures (healthcare costs and resource utilization) were assessed during the 2-year follow-up period.
Outcome measures
Healthcare costs & resource use
All-cause, PTSD-related, mental health and anxiety-related (captured via relevant ICD-10-CM codes, Supplementary Appendix Table A7) healthcare costs were assessed during the 2-year follow-up period. Healthcare costs from the payer's perspective, patients' out-of-pocket and total healthcare costs are evaluated. Patients' out-of-pocket costs consisted of healthcare costs associated with deductibles, copayments, coinsurance and coordination of benefits/savings. Total healthcare costs accounted for healthcare costs from payer's perspective and patients' out-of-pocket costs. The utilization rates of all-cause and PTSD-related services were also assessed. The number of outpatient, emergency department (ED) and hospitalization visits, as well as total duration of hospital stay were the main outcomes that reflected resource utilization. Additionally, healthcare costs and resource use measures were assessed in the first year of the follow-up period to explore the economic burden more granularly.
All study outcomes were assessed and compared between the cohorts among the total population of chronic PTSD (main analysis), as well as among the sub-group of patients with chronic PTSD and SUD/AUD (sub-analysis).
Statistical analysis
Continuous variables were summarized as means with standard deviations, while categorical variables were summarized as numbers and proportions of the sample.
One-way ANOVA with Tamhane's T2 post-hoc test was employed to test the differences between three study cohorts for continuous variables. Additionally, an independent t-test (continuous variables) was performed to test the difference between the two comparable cohorts. The chi-square test of independence was performed to test the differences related to each category of categorical variables. P-values (2-sided) lower than 0.05 implied statistical significance between the cohorts.
Propensity-score matching (PSM) with the nearest-neighbor matching algorithm was performed to minimize selection bias. The demographic characteristics of patients observed on the index date and the relevant clinical characteristics observed throughout the pre-index period were used for the matching process. PSM in a 1:1:1 ratio was employed to match the BP, PwoC and PwC cohorts based on the cohort size (the smallest cohort was matched with the middle-sized cohort in a 1:1 ratio, followed by matching of the matched middle-sized cohort with the largest cohort in a 1:1 ratio).
Results
Main analysis
Out of 500,846 patients with a PTSD diagnosis, 31,326 were identified in the final sample of the non-matched population after applying inclusion/exclusion criteria (2044 BP, 9435 PwoC and 19,847 PwC; Figure 2). The PSM analysis yielded 5076 patients in the final sample (1714 patients in BP and 1681 patients in PwoC and PwC cohorts).
Figure 2. . Patient selection flow diagram.
BP: Baseline PTSD; PTSD: Post-traumatic stress disorder; Pts: Patients; PwoC: PTSD without comorbidities; PwC: PTSD with comorbidities; PSM: Propensity score matching; SUD/AUD: Substance or alcohol use disorder.
Non-matched population
The mean age of the non-matched study population was 38.4 years (Table 1). On average, BP patients were older than the other cohorts (42.0 years, all p < 0.001), while patients with PTSD and comorbidities were on average the youngest (37.6 years, all p < 0.001). Patients were predominantly women (70.0%), with the highest prevalence in the PwC cohort (74.6%, all p < 0.001). The highest proportion of men was observed in the BP cohort (49.5%, all p < 0.001). Most patients had health insurance coverage with a Preferred Provider Organization health plan (49.1%). Statistical differences were observed across geographical regions.
Table 1. . Demographic characteristics of the non-matched population.
| Total sample (n = 31,326) | Baseline PTSD (n = 2044) | PTSD without comorbidities (n = 9435) | PTSD with comorbidities (n = 19,847) | p-value† | |
|---|---|---|---|---|---|
| Age, mean (SD) | 38.4 (12.8) | 42.0 (12.2) | 39.4 (12.3) | 37.6 (13.0) | <0.001‡,§,¶ |
| Gender, n (%) | |||||
| Male | 9408 (30.0) | 1012 (49.5) | 3359 (35.6) | 5037 (25.4) | <0.001‡,§,¶ |
| Female | 21,918 (70.0) | 1032 (50.5) | 6076 (64.4) | 14,810 (74.6) | <0.001‡,§,¶ |
| Health plan, n (%) | |||||
| Comprehensive | 920 (2.9) | 61 (3.0) | 240 (2.5) | 619 (3.1) | 0.006¶ |
| Exclusive provider organization | 134 (0.4) | 9 (0.4) | 44 (0.5) | 81 (0.4) | 0.772 |
| Health maintenance organization | 5648 (18.0) | 398 (19.5) | 1693 (17.9) | 3557 (17.9) | 0.215 |
| Non-capitated point-of-service | 1567 (5.0) | 91 (4.5) | 521 (5.5) | 955 (4.8) | 0.009¶ |
| Point-of-service with capitation | 76 (0.2) | 5 (0.2) | 21 (0.2) | 50 (0.3) | 0.892 |
| Preferred provider organization | 15,376 (49.1) | 1003 (49.1) | 4612 (48.9) | 9761 (49.2) | 0.892 |
| Consumer-driven health plan | 3958 (12.6) | 246 (12.0) | 1136 (12.0) | 2576 (13.0) | 0.024¶ |
| High deductible health plan | 3357 (10.7) | 217 (10.6) | 1084 (11.5) | 2056 (10.4) | 0.003¶ |
| Unknown | 290 (0.9) | 14 (0.7) | 84 (0.9) | 192 (1.0) | 0.407 |
| Region, n (%) | |||||
| Northeast | 4072 (13.0) | 226 (11.1) | 1354 (14.4) | 2492 (12.6) | <0.001‡,¶ |
| North Central | 7409 (23.7) | 387 (18.9) | 2162 (22.9) | 4860 (24.5) | ≤0.003‡,§,¶ |
| South | 13,040 (41.6) | 984 (48.1) | 3743 (39.7) | 8313 (41.9) | <0.001‡,§,¶ |
| West | 6759 (21.6) | 445 (21.8) | 2156 (22.9) | 4158 (21.0) | <0.001¶ |
| Unknown | 46 (0.1) | 2 (0.1) | 20 (0.2) | 24 (0.1) | 0.137 |
Chi-square test was performed for categorical variables and ANOVA (Tamhane's T2 test) for continuous variables.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
PTSD: Post-traumatic stress disorder.
Significant differences between the study cohorts were observed in almost all CCI components except for moderate/severe liver disease (Table 2).
Table 2. . Clinical characteristics of the non-matched population.
| Total sample (n = 31,326) | Baseline PTSD (n = 2044) | PTSD without comorbidities (n = 9435) | PTSD with comorbidities (n = 19,847) | p-value† | |
|---|---|---|---|---|---|
| Charlson Comorbidity Index, n (%) | |||||
| 0 | 23,151 (73.9) | 1521 (74.4) | 7362 (78.0) | 14,268 (71.9) | ≤0.015‡,§,¶ |
| 1 | 4729 (15.1) | 295 (14.4) | 1252 (13.3) | 3182 (16.0) | ≤0.007¶ |
| 2 | 1477 (4.7) | 91 (4.5) | 352 (3.7) | 1034 (5.2) | <0.001¶ |
| 3 | 1136 (3.6) | 62 (3.0) | 307 (3.3) | 767 (3.9) | 0.009¶ |
| 4+ | 833 (2.7) | 75 (3.7) | 162 (1.7) | 596 (3.0) | <0.001‡,¶ |
| Charlson Comorbidity Index, mean (SD) | 0.5 (1.1) | 0.5 (1.2) | 0.4 (0.9) | 0.5 (1.1) | <0.001‡,¶ |
| Charlson Comorbidity Index components, n (%) | |||||
| Myocardial infarction | 165 (0.5) | 19 (0.9) | 42 (0.4) | 104 (0.5) | ≤0.020‡,§ |
| Congestive heart failure | 253 (0.8) | 25 (1.2) | 64 (0.7) | 164 (0.8) | 0.011‡ |
| Peripheral vascular disease | 270 (0.9) | 26 (1.3) | 65 (0.7) | 179 (0.9) | 0.007‡ |
| Cerebrovascular disease | 588 (1.9) | 38 (1.9) | 151 (1.6) | 399 (2.0) | 0.016¶ |
| Dementia | 79 (0.3) | 4 (0.2) | 16 (0.2) | 59 (0.3) | 0.043¶ |
| Chronic pulmonary disease | 3449 (11.0) | 187 (9.1) | 851 (9.0) | 2411 (12.1) | <0.001§,¶ |
| Rheumatic disease | 556 (1.8) | 25 (1.2) | 123 (1.3) | 408 (2.1) | ≤0.010§,¶ |
| Peptic ulcer disease | 197 (0.6) | 17 (0.8) | 33 (0.3) | 147 (0.7) | ≤0.003‡,¶ |
| Mild liver disease | 1160 (3.7) | 82 (4.0) | 288 (3.1) | 790 (4.0) | ≤0.026‡,¶ |
| Moderate or severe liver disease | 50 (0.2) | 1 (0.0) | 14 (0.1) | 35 (0.2) | 0.369 |
| Diabetes without chronic complication | 2273 (7.3) | 173 (8.5) | 572 (6.1) | 1528 (7.7) | <0.001‡,¶ |
| Diabetes with chronic complication | 1353 (4.3) | 104 (5.1) | 327 (3.5) | 922 (4.6) | <0.001‡,¶ |
| Hemiplegia or paraplegia | 142 (0.5) | 4 (0.2) | 29 (0.3) | 109 (0.5) | ≤0.033§,¶ |
| Renal disease | 1233 (3.9) | 92 (4.5) | 286 (3.0) | 855 (4.3) | ≤0.001‡,¶ |
| Malignancy | 0 | 0 | 0 | 0 | - |
| Metastatic solid tumor | 0 | 0 | 0 | 0 | - |
| AIDS/HIV | 127 (0.4) | 8 (0.4) | 26 (0.3) | 93 (0.5) | 0.015¶ |
Chi-square test was performed for categorical variables and ANOVA (Tamhane's T2 test) for continuous variables.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
PTSD: Post-traumatic stress disorder; SD: Standard deviation.
Matched population
No statistically significant between-group differences in the demographic and clinical characteristics were observed in the matched population (Supplementary Tables A8 and A9). Matched patients were approximately 41 years of age, primarily women (53.7%), covered by Preferred Provider Organization insurance type (53.7%) and located in the South region (49.5%). The mean CCI score was 0.3 and most patients had a score of 0 (81.0%). The most common comorbidity was chronic pulmonary disease (7.7%).
Healthcare costs
For the total sample and all cohorts, the majority of the full 2-year follow-up costs were observed during the first year of follow-up (Table 3) across all measured costs (i.e., prescription, outpatient, inpatient, ED and total) and all cost subgroups (i.e., all-cause, PTSD-, mental health- and anxiety-related). Mean costs for the PwC cohort were significantly higher than other cohorts across all but one category in the 1-year follow-up period. The exception was a lack of statistical difference between the BP and PwC cohorts in the PTSD-related ED costs during the first year of follow-up ($96 vs $146, respectively; p ≥ 0.050). PwoC had significantly higher costs than the BP cohort in most outpatient categories (all-cause, PTSD-related and anxiety-related costs during 1-year and 2-year follow-up periods; all p < 0.001) and some total cost categories (PTSD- and anxiety-related during 1-year and 2-year follow-up periods; all p ≤ 0.038). The PwC cohort had significantly higher mean all-cause total healthcare costs during the 1-year ($16,567) and 2-year ($32,302) follow-up periods than other cohorts (all p < 0.001). However, there were no statistically significant differences in these costs between the BP and PwoC cohorts (all p ≥ 0.050). Mental health-related mean total costs in the PwC cohort were $3911 during the first year of follow-up and $6586 during the 2-year follow-up (all p < 0.001 vs other cohorts). Mean PTSD- and anxiety-related total costs during the 2-year follow-up increased from the BP cohort to the PwoC cohort and from the PwoC cohort to the PwC cohort; all differences were statistically significant between study cohorts (all p < 0.001). The same trend was observed in the first year of follow-up (all p ≤ 0.038). In the total sample, the largest contributors to the total mean costs were those associated with outpatient settings ($9650) and prescriptions ($4349).
Table 3. . Healthcare costs of PTSD patients from the payer's perspective during the 2-year follow-up period within the matched population.
| Payer Perspective | Total sample (n = 5076) | Baseline PTSD (n = 1714) | PTSD without comorbidities (n = 1681) | PTSD with comorbidities (n = 1681) | p-value† |
|---|---|---|---|---|---|
| Healthcare costs (per patient), stratified by service setting, mean (SD) | |||||
| Prescription cost | $4349 (25,456) | $3032 (23,706) | $3558 (17,865) | $6483 (32,533) | ≤0.004§,¶ |
| First-year prescription cost | $2119 (13,213) | $1549 (11,916) | $1679 (8388) | $3138 (17,627) | ≤0.007§,¶ |
| All-cause outpatient cost | $9650 (24,420) | $5886 (13,487) | $7605 (11,970) | $15,532 (37,674) | <0.001‡,§,¶ |
| First-year all-cause outpatient cost | $5241 (13,962) | $3062 (6472) | $4140 (7268) | $8565 (21,822) | <0.001‡,§,¶ |
| PTSD outpatient cost | $1259 (4676) | $267 (1250) | $1329 (3112) | $2199 (7272) | <0.001‡,§,¶ |
| First-year PTSD outpatient cost | $939 (3,792) | $267 (1250) | $977 (2692) | $1586 (5807) | <0.001‡,§,¶ |
| Mental health outpatient cost | $1129 (6,356) | $0 (0) | $0 (0) | $3405 (10,690) | <0.001§,¶ |
| First-year mental health outpatient cost | $705 (4,564) | $0 (0) | $0 (0) | $2130 (7738) | <0.001§,¶ |
| Anxiety outpatient cost | $1017 (4798) | $183 (1083) | $517 (1875) | $2367 (7877) | <0.001‡,§,¶ |
| First-year anxiety outpatient cost | $594 (3,488) | $111 (801) | $297 (1164) | $1385 (5813) | <0.001‡,§,¶ |
| All-cause inpatient cost | $3997 (23,407) | $2236 (12,073) | $2,074 (11,694) | $7715 (36,729) | <0.001§,¶ |
| First-year all-cause inpatient cost | $2118 (11,273) | $1480 (9646) | $1360 (10,039) | $3528 (13,610) | <0.001§,¶ |
| PTSD inpatient cost | $733 (6081) | $478 (6124) | $356 (4587) | $1371 (7197) | <0.001§,¶ |
| First-year PTSD inpatient cost | $588 (5425) | $478 (6124) | $313 (4455) | $974 (5529) | ≤0.039§,¶ |
| Mental health inpatient cost | $904 (8077) | $0 (0) | $0 (0) | $2731 (13,859) | <0.001§,¶ |
| First-year mental health inpatient cost | $498 (4513) | $0 (0) | $0 (0) | $1504 (7746) | <0.001§,¶ |
| Anxiety inpatient cost | $627 (5620) | $91 (1269) | $227 (3065) | $1574 (9111) | <0.001§,¶ |
| First-year anxiety inpatient cost | $365 (3656) | $66 (1067) | $124 (2119) | $911 (5856) | <0.001§,¶ |
| All-cause ED cost | $1606 (5085) | $1200 (3537) | $1055 (3020) | $2572 (7404) | <0.001§,¶ |
| First-year all-cause ED cost | $842 (3008) | $658 (2341) | $536 (1882) | $1335 (4223) | <0.001§,¶ |
| PTSD ED cost | $118 (1051) | $96 (892) | $65 (817) | $192 (1360) | ≤0.043§,¶ |
| First-year PTSD ED cost | $97 (890) | $96 (892) | $49 (570) | $146 (1120) | 0.005¶ |
| Mental health ED cost | $148 (1488) | $0 (0) | $0 (0) | $448 (2559) | <0.001§,¶ |
| First-year mental health ED cost | $92 (1242) | $0 (0) | $0 (0) | $277 (2146) | <0.001§,¶ |
| Anxiety ED cost | $174 (1517) | $64 (728) | $86 (869) | $375 (2365) | <0.001§,¶ |
| First-year anxiety ED cost | $93 (991) | $52 (686) | $43 (507) | $185 (1488) | ≤0.003§,¶ |
| All-cause total cost | $19,602 (52,584) | $12,355 (32,795) | $14,292 (27,942) | $32,302 (78,945) | <0.001§,¶ |
| First-year all-cause total cost | $10,320 (27,699) | $6749 (18,617) | $7714 (16,858) | $16,567 (40,264) | <0.001§,¶ |
| PTSD total cost | $2109 (8164) | $841 (6298) | $1750 (5754) | $3762 (11,104) | <0.001‡,§,¶ |
| First-year PTSD total cost | $1623 (6889) | $841 (6298) | $1339 (5335) | $2706 (8519) | ≤0.038‡,§,¶ |
| Mental health total cost | $2181 (12,217) | $0 (0) | $0 (0) | $6586 (20,539) | <0.001§,¶ |
| First-year mental health total cost | $1295 (7609) | $0 (0) | $0 (0) | $3911 (12,832) | <0.001§,¶ |
| Anxiety total cost | $1818 (8869) | $338 (1885) | $831 (4216) | $4315 (14,379) | <0.001‡,§,¶ |
| First-year anxiety total cost | $1052 (5772) | $229 (1531) | $463 (2469) | $2481 (9437) | ≤0.003‡,§,¶ |
One-way ANOVA test (Tamhane's T2 test) was used for continuous variables to assess differences between study cohorts.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
PTSD: Post-traumatic stress disorder; SD: Standard deviation.
The highest amount of total out-of-pocket costs was claimed within the first year of the follow-up period (Supplementary Table A10). Total all-cause out-of-pocket costs were statistically different between the study cohorts, with the PwC cohort having the highest costs (Figure 3, all p ≤ 0.001). The same trends were observed during the first year of follow-up. The significantly higher costs of the PwC cohort were noted during the 2-year follow-up in all categories, except for PTSD-related outpatient costs ($498 vs $443 in PwoC, p ≥ 0.05). Across healthcare settings, the highest mean costs were observed for outpatient services ($1983 all-cause and $347 PTSD-related costs), while ED and inpatient costs were similar ($251 and $293 all-cause and $40 and $21 PTSD-related, respectively). There were no statistically significant differences between the cohorts in PTSD-related ED (1-year and 2-year follow-ups) and anxiety-related ED out-of-pocket costs (1-year follow-up).
Figure 3. . Out-of-pocket costs during the 2-year follow-up period among matched population with post-traumatic stress disorder.
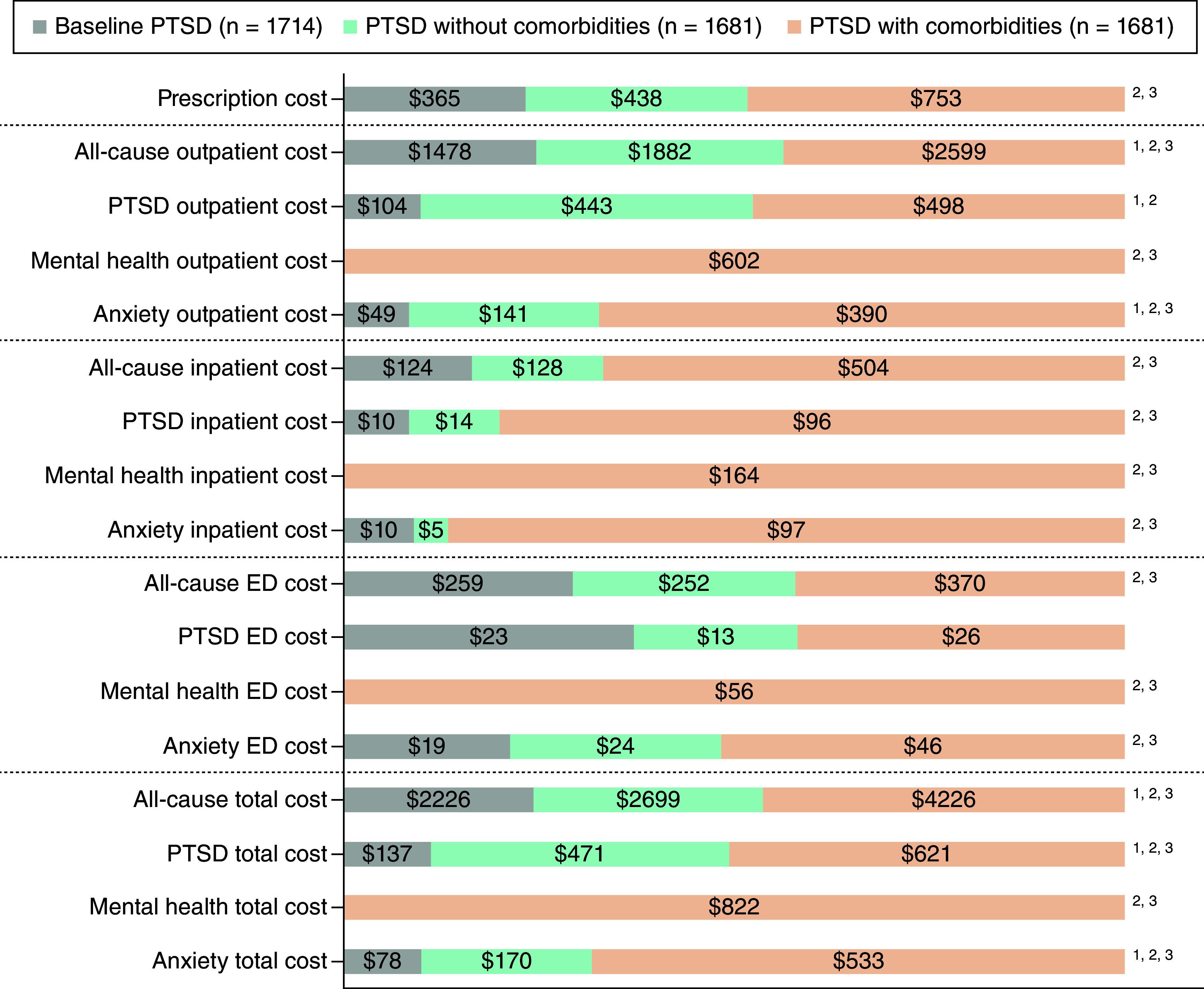
1 Baseline PTSD versus PTSD without comorbidities, p < 0.05.
2 Baseline PTSD versus PTSD with comorbidities, p < 0.05.
3 PTSD without comorbidities versus PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder.
Overall PTSD-, mental health- and anxiety-related healthcare services yielded the highest healthcare costs in the first year of the follow-up compared with the second year (Supplementary Table A11 and Figure 4). The PwC cohort had significantly higher total mean costs across all categories differences versus other cohorts ($36,527, $4383, $7408 and $4849 for all-cause, PTSD-related, mental health and anxiety-related costs, respectively; all p < 0.001). The PwoC cohort had significantly higher mean total PTSD- and anxiety-related costs than the BP cohort ($2221 vs $978 and $1000 vs $416, respectively; both p < 0.001). The same trends were observed for total costs during the first year of follow-up (all p ≤ 0.001). Total costs were mainly driven by outpatient services ($11,633) and prescriptions ($4867), followed by inpatient ($4248) and ED admissions ($1900). PTSD-related overall costs were also higher in outpatient than inpatient and ED settings ($1605, $773 and $139, respectively). The PwC cohort had a significantly greater burden than other cohorts across all categories, apart from PTSD-related overall ED costs ($219 vs $119 in BP, p ≥ 0.050). In addition, the PwoC cohort showed significantly higher overall costs than BP cases in the outpatient setting ($9487 vs $7365, respectively; p < 0.001), as well for outpatient services associated with PTSD ($1772 vs $371, respectively; p < 0.001) and anxiety ($658 vs $232, respectively; p < 0.001).
Figure 4. . Overall costs during the 2-year follow-up period among matched population with post-traumatic stress disorder.
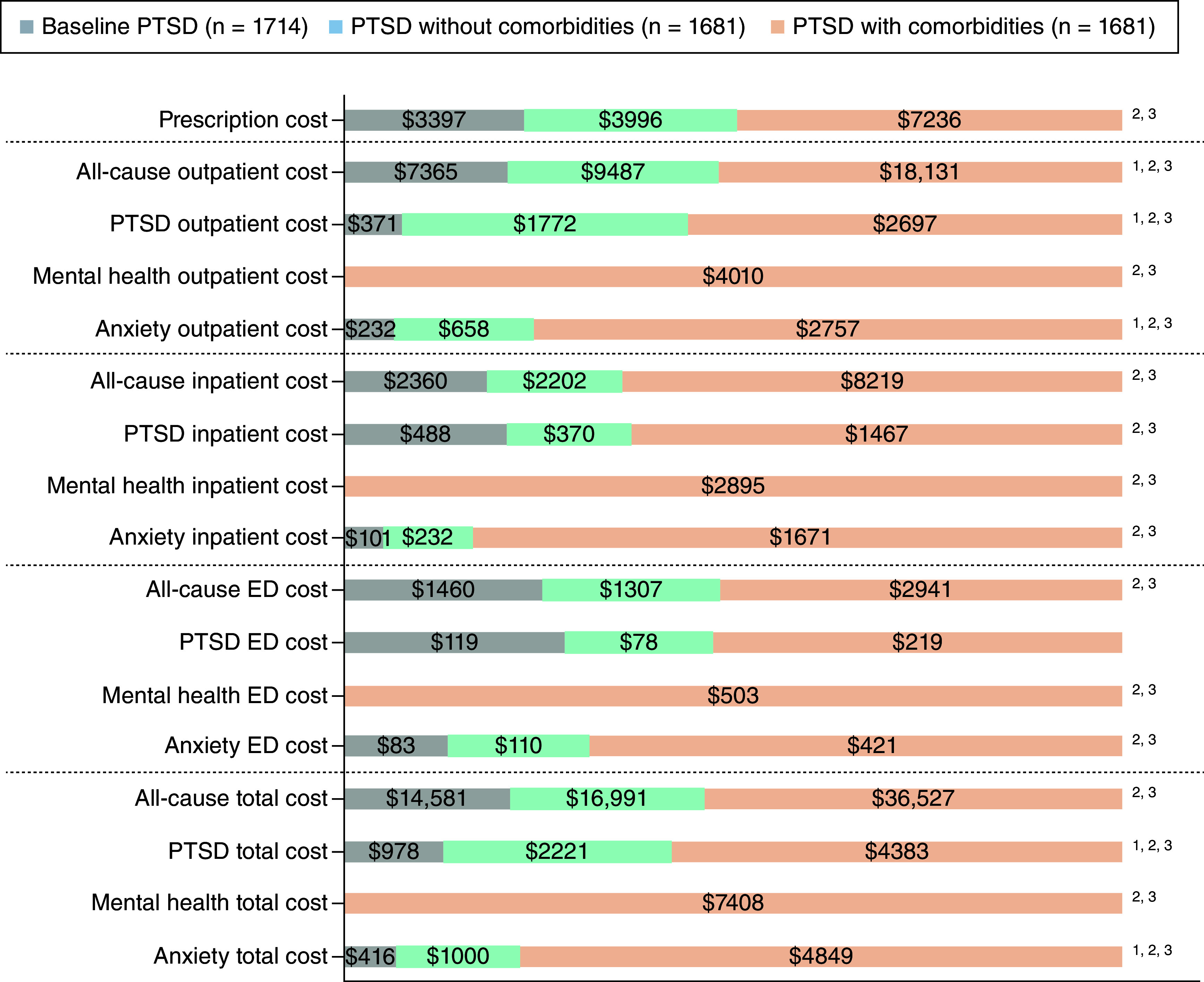
1 Baseline PTSD versus PTSD without comorbidities, p < 0.05.
2 Baseline PTSD versus PTSD with comorbidities, p < 0.05.
3 PTSD without comorbidities versus PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder.
Resource utilization
Cohort of patients with PTSD and comorbidities had greater utilization of healthcare resources than those in the BP and PwoC cohorts during the 2-year follow-up period (Table 4), with significantly higher mean all-cause outpatient visits (56.1 vs 21.2 and 38.3, respectively; both p < 0.001), ED visits (1.4 vs 0.7 and 0.7, respectively; both p < 0.001), hospitalizations (0.4 vs 0.1 and 0.1, respectively; both p < 0.001) and length of hospitalization (3.3 vs 0.4 and 0.4 days, respectively; p < 0.001). The same trends were observed for PTSD-related visits.
Table 4. . Resource use of PTSD patients during the 2-year follow-up period within the matched population.
| 2-Year Follow-Up Period | Total sample (n = 5076) | Baseline PTSD (n = 1714) | PTSD without comorbidities (n = 1681) | PTSD with comorbidities (n = 1681) | p-value† |
|---|---|---|---|---|---|
| Resource utilization, stratified by healthcare setting | |||||
| Outpatient visits | |||||
| All-cause outpatient visits§, n, mean (SD) | 38.4 (37.2) | 21.2 (21.6) | 38.3 (32.4) | 56.1 (45.1) | <0.001¶,#,†† |
| At least one all-cause outpatient visit, n (%) | 5074 (100.0) | 1712 (99.9) | 1681 (100.0) | 1681 (100.0) | 0.141 |
| All-cause outpatient visits‡, n, mean (SD) | 38.4 (37.2) | 21.2 (21.6) | 38.3 (32.4) | 56.1 (45.1) | <0.001¶,#,†† |
| PTSD outpatient visits§, n, mean (SD) | 9.7 (16.6) | 0.9 (0.3) | 13.1 (18.4) | 15.2 (19.3) | ≤0.003¶,#,†† |
| At least one outpatient PTSD visit, n (%) | 4909 (96.7) | 1595 (93.1) | 1667 (99.2) | 1647 (98.0) | ≤0.004¶,#,†† |
| PTSD outpatient visits‡, n, mean (SD) | 10.0 (16.8) | 1.0 (-) | 13.2 (18.4) | 15.5 (19.4) | ≤0.001¶,#,†† |
| Emergency department (ED) visits | |||||
| All-cause ED visits§, n, mean (SD) | 0.9 (2.2) | 0.7 (1.5) | 0.7 (1.5) | 1.4 (3.2) | <0.001#,†† |
| At least one all-cause ED visit, n (%) | 1922 (37.9) | 572 (33.4) | 554 (33.0) | 796 (47.4) | <0.001#,†† |
| All-cause ED visits‡, n, mean (SD) | 2.4 (3.1) | 2.1 (1.9) | 2.0 (2.1) | 3.0 (4.1) | <0.001#,†† |
| PTSD ED visits§, n, mean (SD) | 0.1 (0.4) | 0.1 (0.2) | 0.0 (0.3) | 0.1 (0.5) | <0.001#,†† |
| At least one PTSD ED visit, n (%) | 253 (5.0) | 95 (5.5) | 43 (2.6) | 115 (6.8) | <0.001¶,†† |
| PTSD ED visits‡, n, mean (SD) | 1.4 (0.9) | 1.0 (-) | 1.5 (0.7) | 1.7 (1.2) | <0.001¶,# |
| Hospitalizations | |||||
| All-cause hospitalizations§, n, mean (SD) | 0.2 (0.9) | 0.1 (0.4) | 0.1 (0.4) | 0.4 (1.4) | <0.001#,†† |
| Length of all-cause hospitalizations (days)§, mean (SD) | 1.3 (8.4) | 0.4 (2.2) | 0.4 (2.5) | 3.3 (14.0) | <0.001#,†† |
| At least one all-cause hospitalization, n (%) | 634 (12.5) | 141 (8.2) | 128 (7.6) | 365 (21.7) | <0.001#,†† |
| All-cause hospitalizations‡, n, mean (SD) | 1.7 (2.0) | 1.2 (0.8) | 1.3 (0.7) | 2.0 (2.6) | <0.001#,†† |
| Length of all-cause hospitalizations (days)‡, mean (SD) | 10.8 (21.5) | 4.3 (6.4) | 5.3 (7.6) | 15.2 (26.8) | <0.001#,†† |
| PTSD hospitalizations§, n, mean (SD) | 0.1 (0.3) | 0.0 (0.1) | 0.0 (0.2) | 0.1 (0.5) | <0.001#,†† |
| Length of PTSD hospitalizations (days)§, mean (SD) | 0.5 (3.8) | 0.1 (0.6) | 0.1 (1.5) | 1.2 (6.4) | <0.001#,†† |
| At least one PTSD hospitalization, n (%) | 236 (4.6) | 36 (2.1) | 29 (1.7) | 171 (10.2) | <0.001#,†† |
| PTSD hospitalizations‡, n mean (SD) | 1.3 (0.9) | 1.0 (-) | 1.3 (0.7) | 1.4 (1.0) | ≤0.046¶,# |
| Length of PTSD hospitalizations (days)‡, mean (SD) | 9.9 (15.0) | 3.5 (2.7) | 7.9 (8.3) | 11.6 (16.9) | ≤0.030¶,# |
Chi-square test was performed for categorical variables. ANOVA with Tamhane's T2 post hoc test (three cohorts comparison) and independent sample t-test (two cohorts comparison) were performed for continuous variables.
Considering only patients who experienced at least one event of interest.
Across the total sample.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder; SD: Standard deviation.
The first year of the follow-up period also demonstrated greater resource utilization among the PwC cohort compared with the BP and PwoC cohorts (Supplementary Table A12). There were significantly higher mean all-cause outpatient visits (31.2 vs 11.0 and 22.0, respectively; both p < 0.001), ED visits (0.7 vs 0.4 and 0.4, respectively; both p < 0.001), hospitalizations (0.2 vs 0.1 and 0.1, respectively; both p < 0.001) and length of hospitalization (2.0 vs 0.2 and 0.3 days, respectively; p < 0.001) in the PwC cohort. The same trends were observed for PTSD-related visits.
Sub-analysis population
Out of 31,326 patients in the final sample of non-matched patients, 3776 patients were identified with an SUD/AUD diagnosis during the observational period (85, 537 and 3154 patients in the BP, PwoC and PwC cohorts, respectively).
The total sample of SUD/AUD patients had a mean age of 35.2 years, were predominantly women (59.5%), were most commonly covered by a Preferred Provider Organization plan (49.0%) and generally resided in the South (40.4%; Supplementary Table A13). The PwC cohort had the youngest patients compared with BP and PwoC cohorts (34.6 vs 38.7 and 38.3 years, respectively; p ≤ 0.024) and had a comparatively lower proportion of men (36.7% vs 67.1% and 58.5%, respectively; both p < 0.001). No significant differences were seen for region of residence or type of healthcare coverage between study cohorts, except for a higher rate of PwC than PwoC patients being located in the North Central region (15.2% vs 11.7%, respectively; p = 0.038).
The mean CCI score of the total SUD/AUD sample was 0.6, with most patients not having relevant comorbidities (71.1%; Supplementary Table A14). In addition, there were no differences in mean CCI scores between the study cohorts, except for a significantly higher proportion of patients in the BP cohort with a CCI score ≥4 (8.2% vs 3.4% and 3.8%, respectively; p ≤ 0.038). The most common comorbid condition was chronic pulmonary disease (12.2%), with a significantly higher rate among PwC than PwoC patients (12.7% vs 9.3%, respectively; p = 0.027).
Healthcare costs
The highest amount of healthcare costs among the total sample of patients with SUD/AUD were claimed during the first year of the follow-up, except for outpatient prescription costs (Table 5). The PwC cohort had the highest all-cause, PTSD-related and anxiety-related total costs from the payer's perspective during the 2-year follow-up ($55,560, $7668 and $8234, respectively; all p < 0.001). Mental health-related total costs were only observed within the PwC cohort ($14,897). The same trends were observed during the first year of follow-up (all p < 0.001). There were no differences in total healthcare costs between the BP and PwoC cohorts (all p ≥ 0.05). Across all healthcare settings over the 2-year follow-up period, the PwC cohort had significantly higher costs than other cohorts except for all-cause inpatient and PTSD-related ED costs compared with the BP ($18,146 vs $11,962 and $288 vs $232, respectively; all p ≥ 0.05). The only significant differences between PwoC and BP cohorts during the 2-year follow-up were reported for outpatient PTSD- ($1746 vs $193, respectively; p < 0.001) and anxiety-related services ($1078 vs $166, respectively; p ≤ 0.007).
Table 5. . Healthcare costs from the payer's perspective during the 2-year follow-up period within the sub-sample of patients diagnosed with substance/alcohol use disorder.
| Payer perspective | Total sample (n = 3776) | Baseline PTSD (n = 85) | PTSD without comorbidities (n = 537) | PTSD with comorbidities (n = 3154) | P-value† |
|---|---|---|---|---|---|
| Healthcare costs (per patient), stratified by service setting, mean (SD) | |||||
| Prescription cost | $7075 (21,190) | $3229 (9983) | $3804 (11,725) | $7736 (22,559) | <0.001§,¶ |
| First-year prescription cost | $3343 (10,221) | $1531 (4919) | $1894 (6176) | $3638 (10,836) | ≤0.001§,¶ |
| All-cause outpatient cost | $21,511 (43,377) | $7011 (14,135) | $11,459 (38,139) | $23,614 (44,417) | <0.001§,¶ |
| First-year all-cause outpatient cost | $12,107 (27,207) | $3190 (5773) | $7103 (32,277) | $13,199 (26,470) | ≤0.032‡,§,¶ |
| PTSD outpatient cost | $3726 (14,200) | $193 (491) | $1746 (4823) | $4158 (15,371) | <0.001‡,§,¶ |
| First-year PTSD outpatient cost | $2470 (9798) | $193 (491) | $1307 (4079) | $2730 (10,568) | <0.001‡,§,¶ |
| Mental health outpatient cost | $5286 (16,969) | $0 (0) | $0 (0) | $6328 (18,388) | <0.001§,¶ |
| First-year mental health outpatient cost | $3276 (11,850) | $0 (0) | $0 (0) | $3922 (12,868) | <0.001§,¶ |
| Anxiety outpatient cost | $3491 (11,578) | $166 (624) | $1078 (6779) | $3991 (12,293) | ≤0.007‡,§,¶ |
| First-year anxiety outpatient cost | $2079 (8161) | $159 (615) | $743 (6531) | $2358 (8485) | <0.001§,¶ |
| All-cause inpatient cost | $16,317 (43,726) | $11,962 (39,892) | $6266 (27,053) | $18,146 (45,839) | <0.001¶ |
| First-year all-cause inpatient cost | $9302 (27,808) | $5,823 (18,797) | $3410 (18,671) | $10,399 (29,150) | <0.001¶ |
| PTSD inpatient cost | $2864 (10,992) | $1058 (7277) | $1042 (6100) | $3223 (11,667) | ≤0.028§,¶ |
| First-year PTSD inpatient cost | $2084 (8917) | $1058 (7277) | $752 (5432) | $2338 (9401) | <0.001§ |
| Mental health inpatient cost | $6188 (20,545) | $0 (0) | $0 (0) | $7408 (22,278) | <0.001§,¶ |
| First-year mental health inpatient cost | $3946 (14,814) | $0 (0) | $0 (0) | $4724 (16,096) | <0.001§,¶ |
| Anxiety inpatient cost | $2980 (12,842) | $738 (3500) | $412 (2889) | $3477 (13,935) | <0.001§,¶ |
| First-year anxiety inpatient cost | $1815 (9580) | $267 (1747) | $236 (2135) | $2125 (10,414) | <0.001§,¶ |
| All-cause ED cost | $5502 (11,771) | $3490 (6580) | $2519 (6124) | $6064 (12,507) | ≤0.003§,¶ |
| First-year all-cause ED cost | $2973 (7175) | $1598 (3156) | $1495 (4710) | $3262 (7556) | <0.001§,¶ |
| PTSD ED cost | $264 (1333) | $232 (1034) | $131 (983) | $288 (1390) | 0.005¶ |
| First-year PTSD ED cost | $175 (872) | $232 (1034) | $89 (757) | $188 (885) | 0.019¶ |
| Mental health ED cost | $970 (3,164) | $0 (0) | $0 (0) | $1161 (3430) | <0.001§,¶ |
| First-year mental health ED cost | $591 (2305) | $0 (0) | $0 (0) | $708 (2506) | <0.001§,¶ |
| Anxiety ED cost | $669 (2471) | $168 (936) | $185 (1435) | $765 (2623) | <0.001§,¶ |
| First-year anxiety ED cost | $379 (1659) | $31 (204) | $130 (1356) | $431 (1721) | <0.001§,¶ |
| All-cause total cost | $50,406 (82,432) | $25,691 (54,484) | $24,048 (52,500) | $55,560 (86,178) | <0.001§,¶ |
| First-year all-cause total cost | $27,725 (49,510) | $12,143 (24,113) | $13,903 (40,898) | $30,498 (50,874) | <0.001§,¶ |
| PTSD total cost | $6854 (20,677) | $1483 (7298) | $2919 (8235) | $7668 (22,245) | <0.001§,¶ |
| First-year PTSD total cost | $4729 (15,131) | $1483 (7298) | $2148 (7057) | $5256 (16,203) | <0.001§,¶ |
| Mental health total cost | $12,443 (32,461) | $0 (0) | $0 (0) | $14,897 (35,000) | <0.001§,¶ |
| First-year mental health total cost | $7813 (22,432) | $0 (0) | $0 (0) | $9354 (24,249) | <0.001§,¶ |
| Anxiety total cost | $7140 (20,529) | $1072 (4085) | $1675 (7692) | $8234 (22,064) | <0.001§,¶ |
| First-year anxiety total cost | $4273 (14,559) | $457 (1854) | $1110 (7107) | $4914 (15,575) | <0.001§,¶ |
One-way ANOVA test (Tamhane's T2 test) was used for continuous variables to assess differences between study cohorts.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder; SD: Standard deviation.
The same trend of out-of-pocket healthcare costs was noted, as seen with payer-related costs, mainly captured within the first year of follow-up (Supplementary Table A15). Patients with PTSD and comorbidities had significantly higher costs across all service categories ($5722, $926, $1522 and $826 for all-cause, PTSD-related, mental-health and anxiety-related total out-of-pocket costs, respectively; all p ≤ 0.009; Figure 5). The PwoC cohort had significantly higher costs than BP cases during the 2-year follow-up only for services associated with PTSD ($647 vs $97, respectively; p ≤ 0.009) and anxiety ($297 vs $83, respectively; p ≤ 0.003). The highest out-of-pocket costs were seen in the outpatient setting with $2869 all-cause and $603 PTSD costs, while inpatient and ED settings reported only $1034 and $697 all-cause and $228 and $36 PTSD costs, respectively. The PwC cohort mostly had significantly greater costs across most healthcare setting categories during the 2-year follow-up. Exceptions were outpatient prescription ($774 vs $483 in BP, p ≥ 0.050), PTSD-related outpatient ($635 vs $506 in PwoC, p ≥ 0.050), all-cause ED ($725 vs $625 in BP, p ≥ 0.050) and PTSD-related ED costs ($36 vs $37 in PwoC and $51 in BP).
Figure 5. . Out-of-pocket costs during the 2-year follow-up period within the sub-sample of patients diagnosed with substance/alcohol use disorder.
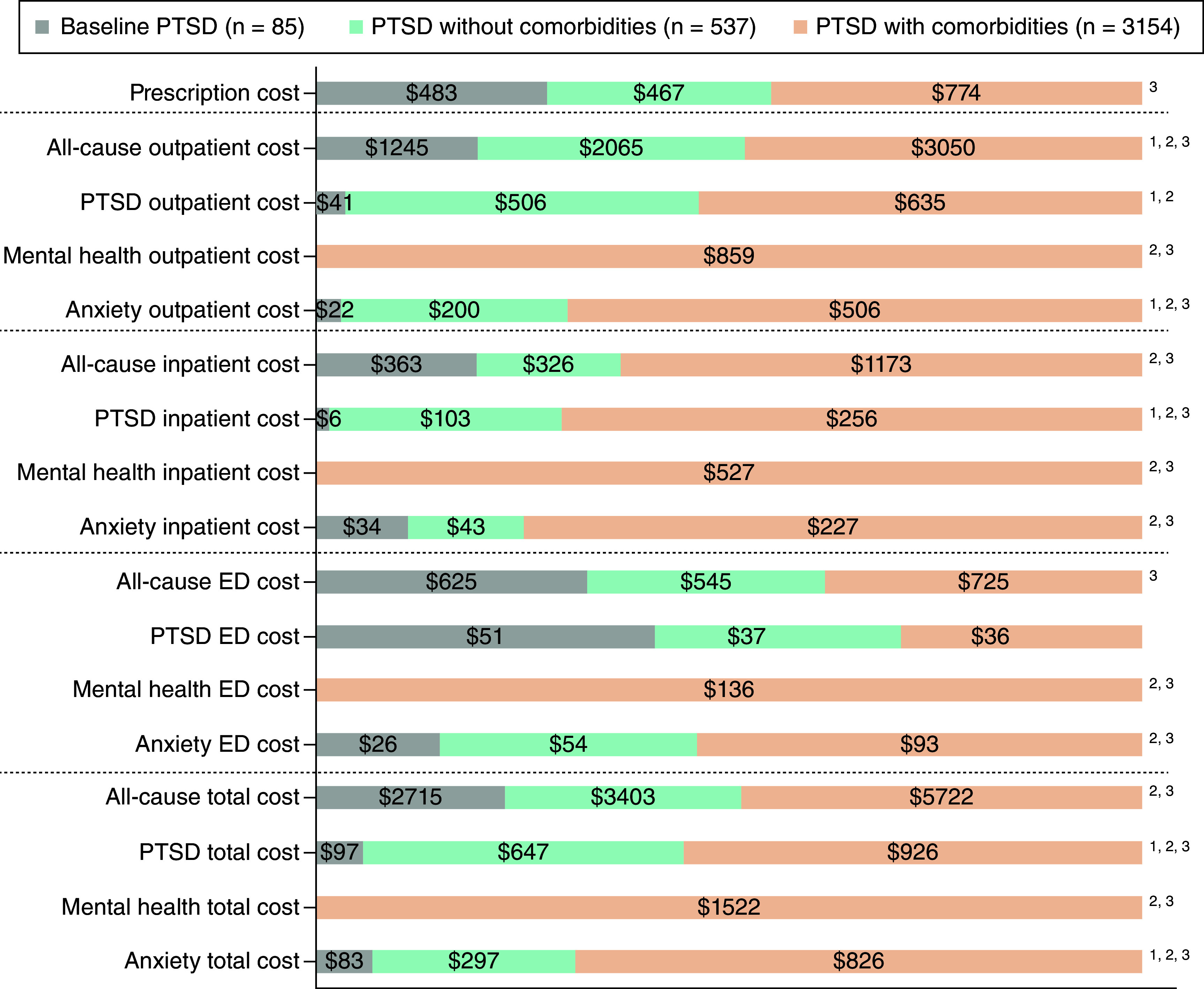
1 Baseline PTSD versus PTSD without comorbidities, p < 0.05.
2 Baseline PTSD versus PTSD with comorbidities, p < 0.05.
3 PTSD without comorbidities versus PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder.
The PwC cohort had significantly higher overall total costs (Supplementary Table A16 and Figure 6) across all service type groups than other cohorts ($61,282, $8594, $16,419 and $9060 for all-cause, PTSD-related, mental health and anxiety-related costs, respectively; all p < 0.001). There were no statistically significant differences between PwoC and BP cohorts in any category of overall total costs. The high economic burden was mostly driven by outpatient and inpatient costs. All-cause and PTSD-related costs were $24,380 and $4329 in the outpatient setting and $17,351 and $3092 in the inpatient setting, respectively. The PwC cohort also had significantly higher costs among all healthcare and service type categories than other individuals, except for all-cause inpatient ($19,319 vs $12,325 in BP) and PTSD-related ED costs ($323 vs $283 in BP). The same trends for total costs and expenditures per healthcare setting were observed during the first year of the follow-up period.
Figure 6. . Overall costs during the 2-year follow-up period within the sub-sample of patients diagnosed with substance/alcohol use disorder.
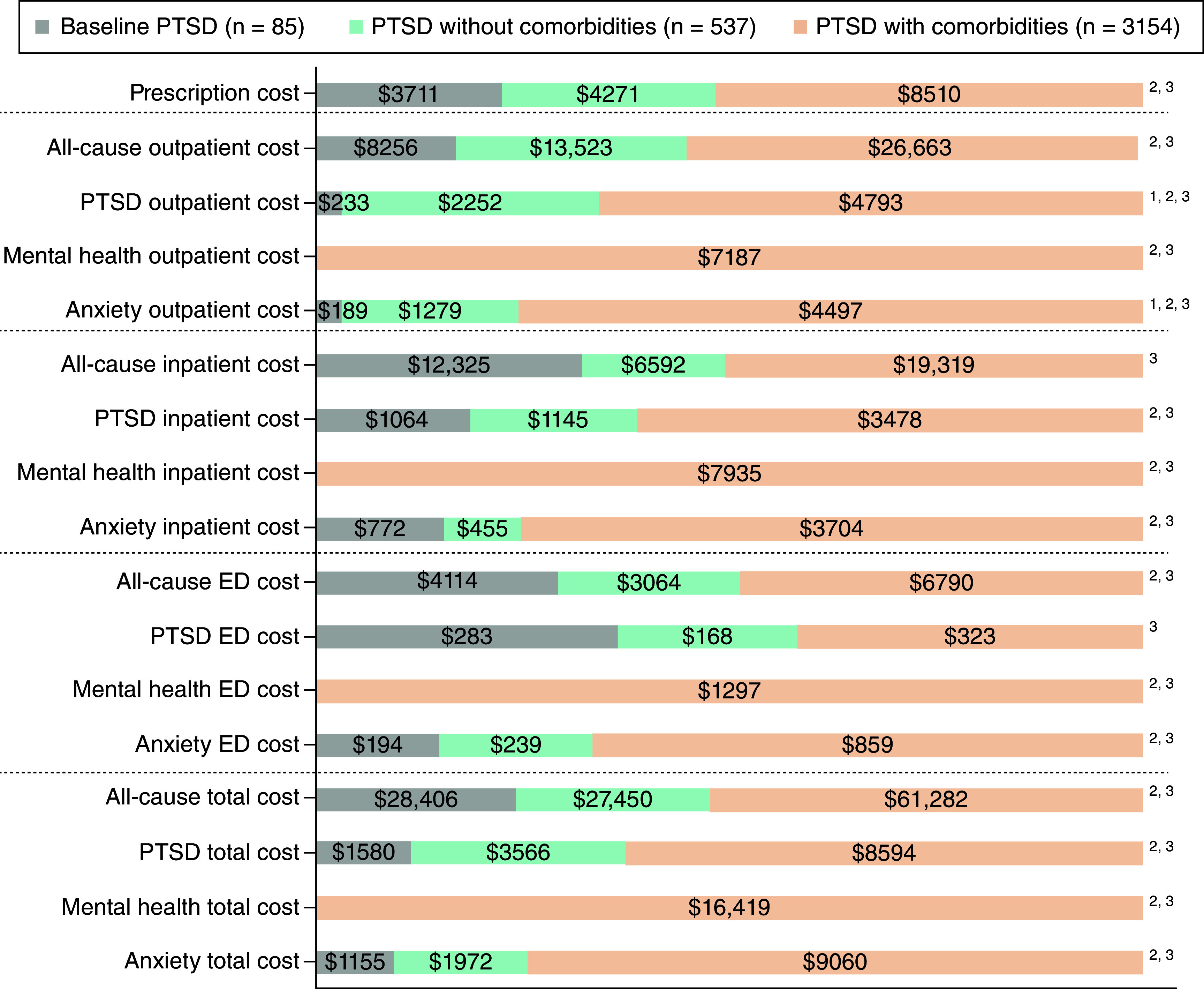
1 Baseline PTSD versus PTSD without comorbidities, p < 0.05.
2 Baseline PTSD versus PTSD with comorbidities, p < 0.05.
3 PTSD without comorbidities versus PTSD with comorbidities, p < 0.05.
ED: Emergency department; PTSD: Post-traumatic stress disorder.
Resource utilization
During the 2-year follow-up, the PwC cohort had significantly higher utilization of healthcare resources than other cohorts (Table 6), except when comparing rates of BP patients with at least one all-cause ED visit (70.5% vs 61.2%, p ≥ 0.050) or PTSD-related ED visit (12.7% vs 9.4%, p ≥ 0.050). Additionally, there were no differences between the proportions of patients with at least one all-cause outpatient visit (p = 0.347).
Table 6. . Resource use during the 2-year follow-up period within the sub-sample of chronic PTSD patients diagnosed with SUD/AUD.
| 2-year follow-up | Total sample (n = 3776) | Baseline PTSD (n = 85) | PTSD without comorbidities (n = 537) | PTSD with comorbidities (n = 3154) | p-value† |
|---|---|---|---|---|---|
| Resource Utilization, stratified by healthcare setting | |||||
| Outpatient visits | |||||
| All-cause outpatient visits§, n, mean (SD) | 63.9 (55.3) | 22.9 (22.8) | 38.5 (33.0) | 69.3 (57.2) | <0.001¶,#,†† |
| At least one all-cause outpatient visit, n (%) | 3774 (99.9) | 85 (100.0) | 536 (99.8) | 3153 (100.0) | 0.347 |
| All-cause outpatient visits‡, n, mean (SD) | 63.9 (55.2) | 22.9 (22.8) | 38.6 (33.0) | 69.3 (57.2) | <0.001¶,#,†† |
| PTSD outpatient visits§, n, mean (SD) | 16.5 (22.7) | 0.8 (0.4) | 12.1 (17.3) | 17.7 (23.6) | <0.001¶,#,†† |
| At least one outpatient PTSD visit, n (%) | 3,613 (95.7) | 72 (84.7) | 529 (98.5) | 3012 (95.5) | <0.001¶,#,†† |
| PTSD outpatient visits‡, n, mean (SD) | 17.2 (22.9) | 1.0 (0.0) | 12.3 (17.4) | 18.5 (23.8) | <0.001¶,#,†† |
| Emergency department (ED) visits | |||||
| All-cause ED visits§, n, mean (SD) | 3.0 (5.0) | 2.0 (3.0) | 1.5 (2.7) | 3.3 (5.3) | ≤0.001#,†† |
| At least one all-cause ED visit, n (%) | 2544 (67.4) | 52 (61.2) | 269 (50.1) | 2223 (70.5) | <0.001†† |
| All-cause ED visits‡, n, mean (SD) | 4.4 (5.6) | 3.2 (3.2) | 2.9 (3.2) | 4.6 (5.8) | ≤0.010#,†† |
| PTSD ED visits§, n, mean (SD) | 0.2 (0.7) | 0.1 (0.3) | 0.1 (0.4) | 0.2 (0.8) | ≤0.001#,†† |
| At least one PTSD ED visit, n (%) | 435 (11.5) | 8 (9.4) | 28 (5.2) | 399 (12.7) | <0.001†† |
| PTSD ED visits‡, n, mean (SD) | 1.7 (1.3) | 1.0 (0.0) | 1.6 (1.0) | 1.8 (1.4) | ≤0.010¶,# |
| Hospitalizations | |||||
| All-cause hospitalizations§, n, mean (SD) | 1.1 (2.3) | 0.5 (1.3) | 0.4 (0.9) | 1.3 (2.5) | ≤0.001#,†† |
| Length of all-cause hospitalizations (days)§, mean (SD) | 9.7 (23.3) | 2.5 (8.2) | 2.4 (9.3) | 11.1 (25.0) | ≤0.001#,†† |
| At least one all-cause hospitalization, n (%) | 1670 (44.2) | 23 (27.1) | 119 (22.2) | 1528 (48.4) | <0.001#,†† |
| All-cause hospitalizations‡, n, mean (SD) | 2.6 (2.9) | 1.8 (2.0) | 1.6 (1.3) | 2.7 (3.0) | <0.001†† |
| Length of all-cause hospitalizations (days)‡, mean (SD) | 21.9 (31.1) | 9.1 (14.0) | 10.8 (17.3) | 22.9 (31.9) | <0.001#,†† |
| PTSD hospitalizations§, n, mean (SD) | 0.3 (0.8) | 0.1 (0.3) | 0.1 (0.4) | 0.4 (0.9) | ≤0.001#,†† |
| Length of PTSD hospitalizations (days)§, mean (SD) | 3.2 (10.0) | 0.2 (0.9) | 0.8 (3.7) | 3.7 (10.8) | ≤0.004¶,#,†† |
| At least one PTSD hospitalization, n (%) | 871 (23.1) | 7 (8.2) | 56 (10.4) | 808 (25.6) | <0.001#,†† |
| PTSD hospitalizations‡, n, mean (SD) | 1.5 (1.1) | 1.0 (0.0) | 1.2 (0.4) | 1.5 (1.1) | ≤0.009¶,#,†† |
| Length of PTSD hospitalizations (days)‡, mean (SD) | 13.8 (17.0) | 3.0 (1.2) | 8.1 (8.6) | 14.3 (17.4) | <0.001¶,#,†† |
Chi-square test was performed for categorical variables. ANOVA with Tamhane's T2 post hoc test (three cohorts comparison) and independent sample t-test (two cohorts comparison) were performed for continuous variables.
Considering only patients who experienced at least one event of interest.
Across the total sample.
Baseline PTSD vs PTSD without comorbidities, p < 0.05.
Baseline PTSD vs PTSD with comorbidities, p < 0.05.
PTSD without comorbidities vs PTSD with comorbidities, p < 0.05.
The PwC cohort had significantly greater utilization of healthcare resources than other cohorts (Supplementary Table A17), except when comparing to the mean number of PTSD-related ED visits and rate of patients with at least one ED visit in the BP cohort (0.2 versus 0.1 and 10.3% versus 9.4%, respectively. Difference between the PwoC and BP cohorts was observed only in the number of all-cause outpatient services, with a mean of 22.5 versus 12.2 visits per patient (p < 0.001).
Discussion
This real-world claims data analysis provided a comprehensive, contemporary summary assessing the economic burden of adult PTSD in the US. This study reported a high economic burden related to PTSD diagnosis, especially among patients within the PwC cohort, who had significantly higher costs and resource utilization than those in the PwoC and BP cohorts. It was demonstrated that the highest healthcare costs and resource utilization were claimed in the first year after PTSD diagnosis, with a decreasing trend in the second year. Healthcare costs from payer's perspective and patients' out-of-pocket healthcare costs were both significantly higher among PwC patients than in other study cohorts. Healthcare services were most commonly provided in the outpatient setting, with the highest impact on total healthcare costs. Patients with PTSD and a co-occurring SUD/AUD diagnosis cost more than the general sample of patients with PTSD, with higher costs related to inpatient services.
Economic evaluations of PTSD burden in the US clinical setting were performed by Davis et al. [10,12]. An initial study assessed excess direct and indirect healthcare costs compared with individuals without PTSD, using evidence from published literature (US PTSD prevalence, non-healthcare direct cost and indirect cost estimates) and MarketScan® insurance claims data (Commercial, Medicare Supplemental and Multi-State Medicaid). After weighting results by patient distribution across health plans, a real-world data analysis reported the overall healthcare cost (payer and out-of-pocket) of $13,016 for civilians, including pharmacy and medical expenses. The findings suggested that the population with PTSD had a $6495 direct healthcare cost increment per patient compared with those without PTSD diagnosis [10]. However, applying health plan weights, using a prevalence-based approach and other evidence substantially affects the real-world expenditure estimates. Additionally, the authors did not thoroughly explain the population selection process and did not depict if they used PTSD-related service costs or all-cause service costs of patients with PTSD; therefore, the results may be overestimated. In contrast, our analysis was based only on real-world data and provided an in-depth patient selection process and thorough stratification of healthcare costs (per healthcare setting, PTSD severity, type of service, first year of follow-up and cost perspective).
A second retrospective MarketScan® analysis by Davis et al. [12] explored the patient journey 6 months before and 2 years after index PTSD diagnosis. The study included privately insured PTSD adults treated with selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, or atypical antipsychotics, assessing changes in healthcare costs and resource utilization over time. The results demonstrated decreasing trends in economic burden measures after the index event, with 6-month total healthcare cost increments per patient ranging between $9410 and $11,845. The proportions of patients with at least one inpatient visit also decreased after index PTSD diagnosis, decreasing from 14.4% in the first 6 months to 8.0% in the last 6 months of follow-up. The mean hospitalization duration was approximately 11 days [12]. In addition, many patients with PTSD do not receive pharmacological treatments (especially with less severe disease stages) or may be treated with a wide range of off-label medications recommended by guidelines (i.e., propranolol). Therefore, the results may be misinterpreted and the generalizability of findings is substantially limited [12]. Conversely, our real-world analysis reported the economic burden of the general population with diagnosed PTSD and presented both all-cause and PTSD-related service costs and utilization measures. The costs of mental health conditions closely related to PTSD were also demonstrated. Based on our findings, the pool of evidence regarding PTSD economic burden appears to be greater than previously reported.
Previous research denoted a mutual causality between PTSD and SUD/AUD and demonstrated a significantly greater disease burden among patients with both diagnoses. In a study by Bowe et al. [16], an SUD/AUD comorbidity was associated with higher burden compared with other comorbid conditions among patients with PTSD such as seizures (odds ratio [OR]: 1.92, 95% confidence intervals [CIs]: 1.31–2.82), liver diseases (OR: 1.71, 95% CI: 1.68–1.73), bipolar disorder (OR: 1.27, 95% CI: 1.25–1.29), HIV (OR: 1.16, 95% CI: 1.11–1.22), MDD (OR: 1.12, 95% CI: 1.11–1.13) and anxiety (OR: 1.11, 95% CI: 1.10–1.13). Higher utilization of healthcare resources was also reported to have the greatest impact on mental health-related inpatient services (OR: 1.9, 95% CI: 1.93–1.99) [16]. Our analysis extended the available evidence regarding the disease burden of patients with PTSD and an SUD/AUD comorbidity by assessing economic outcomes. Numerically higher costs (payer perspective, out-of-pocket and overall costs) and resource utilization were demonstrated across all healthcare settings in the total sample and among patients with comorbid SUD/AUD.
Strengths & limitations
The results of this retrospective claims analysis should be interpreted with caution. The first and main limitation of this study is related to the real-world database characteristics and restrictions in coding systems. Since insurance data are primarily collected for billing purposes, there may be miscoding cases, duplicate claims, negative inputs, or other data entry errors. Such impact was reduced or removed by performing thorough data cleaning, precise patient selection and using the PSM analysis to minimize the selection bias and balance study cohort differences. A second limitation is the lack of PTSD severity data and the consequential introduction of assumptions that would stratify patients by disease severity. This way of defining cohorts may interfere with the between-group results but is still considered the most appropriate approach based on peer-reviewed literature for this type of analysis [14,15]. The third and final limitation is associated with the generalizability of study findings, as we used data from commercially insured individuals without including Veterans Affairs (VA), Medicare, or Medicaid databases. Unlike clinical or VA data, civilian insurance claims do not provide direct information on PTSD severity. There are various methodological approaches used to stratify patients based on comorbidities present with PTSD that are published. The most suitable approach by Seng et al. [14,15] was applied in this research. Other methods [17–19] were considered inappropriate as they focused on patient profiling versus our research goal to explore and compare the economic burden of patients with different PTSD categorization. Findings in this study fill the gaps in published literature by providing estimates regarding healthcare costs and resource utilization among PTSD with and without mental health comorbidities.
Conclusion
PTSD was associated with a substantial economic burden and resource use in a real-world setting. Outpatient services were the single biggest driver of the study results. The highest costs and resource use across all healthcare settings were reported in individuals with PTSD and co-occurring mental health comorbidities. This study also demonstrated a high occurrence of SUD/AUD among the PwC cohort with high economic burden.
Besides the large economic burden reported in this study, PTSD is associated with a high disease prevalence, which indicates the need for alternative treatment solutions. More research and regulatory approval of innovative approaches appear to be needed in the treatment and management of PTSD.
Summary points
This was a retrospective commercial claims analysis (2017–2022) including adult patients diagnosed with chronic post-traumatic stress disorder (PTSD) stratified by patients' severity and assigned to baseline PTSD (BP), PTSD without comorbidities (PwoC) and PTSD with comorbidities (PwC) cohorts.
The main study outcomes were healthcare costs and resource utilization during the first year after PTSD diagnosis and the entirety of the 2-year follow-up period.
For the total sample and all cohorts, the majority of healthcare costs were observed during the first year of follow-up across all measured costs (i.e., prescription, outpatient, inpatient, emergency department [ED] and total) and all cost subgroups (i.e., all-cause, PTSD-, mental health- and anxiety-related).
Mean healthcare costs (from the payer's perspective, out-of-pocket costs and overall costs) captured during the 2-year follow-up period for the PwC cohort were significantly higher than other cohorts across all but one category (costs associated with emergency department services).
Patients with PTSD and comorbidities had greater use of healthcare resources than BP and PwoC cohorts during the 2-year follow-up period, with significantly (all p < 0.001) higher mean all-cause outpatient visits, ED visits, hospitalizations and length of hospitalization.
The PwC patients diagnosed with a substance or alcohol use disorder (SUD/AUD) had the highest all-cause, PTSD-related and anxiety-related total costs from the payer's perspective during the 2-year follow-up period.
The same trends were observed regarding out-of-pocket costs and overall healthcare costs, with significantly higher expenditures reported for patients with PTSD, mental health comorbidities and co-occurring SUD/AUD than BP and PwoC and co-occurring SUD/AUD.
Resource utilization rates (especially emergency department visits and hospitalizations) were numerically higher among patients with PTSD and SUD/AUD compared with the general population with diagnosed PTSD.
PTSD is associated with a large economic burden in the real-world setting, with the highest healthcare costs and resource use observed among patients with PTSD and comorbidities.
Supplementary Material
Acknowledgments
All steps in conducting this research were supervised and critically reviewed by experts from Lykos Therapeutics.
Footnotes
Supplementary data
To view the supplementary data that accompany this paper please visit the journal website at: https://bpl-prod.literatumonline.com/doi/10.57264/cer-2024-0058
Author contributions
F Stanicic, V Zah and D Grbic equally contributed to this research. All three authors were included in performing RWE data analyses, including study conceptualization, patient selection process, evidence synthesis and data validation and also manuscript preparation (defining study objectives and unmet needs, explaining the methodological approach, results interpretation and discussion as well as the technical processes like formatting, designing figures and reference annotations). D de Angelo and W Bibeau also participated in this research by contributing to study conceptualization, data validation and manuscript preparation. All authors gained final approval of the current manuscript version to be published and agreed to be accountable for all research aspects in ensuring that questions related to the accuracy or integrity of the work are appropriately investigated and resolved.
Financial disclosure
This work was funded with support from Lykos Therapeutics. F Stanicic, V Zah and D Grbic are employees of ZRx Outcomes Research Inc., which received funding from Lykos Therapeutics for this work. DD Angelo is an employee of and owns stocks/stock options in Lykos Therapeutics. W Bibeau was an employee of Lykos Therapeutics at the time of study conduction. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Competing interests disclosure
The authors have no competing interests or relevant affiliations with any organization or entity with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Writing disclosure
No writing assistance was funded for manuscript preparation.
Open access
This work is licensed under the Attribution-NonCommercial-NoDerivatives 4.0 Unported License. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc-nd/4.0/
References
- 1.American Psychological Association. Diagnostic and statistical manual of mental disorders: DSM-5™ (5th Edition). American Psychiatric Publishing, Inc, VA, USA: (2013) [Google Scholar]
- 2.De Vries GJ, Olff M. The lifetime prevalence of traumatic events and post-traumatic stress disorder in the Netherlands. J. Trauma. Stress 22(4), 259–267 (2009). [DOI] [PubMed] [Google Scholar]
- 3.Dunlop BW, Wong A. The hypothalamic-pituitary-adrenal axis in PTSD: pathophysiology and treatment interventions. Prog. Neuropsychopharmacol. Biol. Psychiatry 89, 361–379 (2019). [DOI] [PubMed] [Google Scholar]
- 4.Doron-Lamarca S, Niles BL, King DW, King LA, Pless Kaiser A, Lyons MJ. Temporal associations among chronic PTSD symptoms in U.S. combat veterans. J. Trauma. Stress 28(5), 410–417 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical practice guideline for the treatment of post-traumatic stress disorder (PTSD) in adults. (2023). https://www.apa.org/ptsd-guideline/ptsd.pdf
- 6.Clinical practice guideline for the treatment of post-traumatic stress disorder (PTSD) in adults. (2023). https://www.apa.org/ptsd-guideline/ptsd.pdf
- 7.post-traumatic stress disorder prevention and treatment guidelines – Methodology and recommendations (2023).
- 8.Clinical practice guideline for management of post-traumatic stress disorder and acute stress disorder (version 4.0). (2023). https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPG-PTSD-Full-CPGAug242023.pdf
- 9.Schein J, Houle C, Urganus A et al. Prevalence of post-traumatic stress disorder in the United States: a systematic literature review. Curr. Med. Res. Opin. 37(12), 2151–2161 (2021). [DOI] [PubMed] [Google Scholar]
- 10.Davis LL, Schein J, Cloutier M et al. The economic burden of post-traumatic stress disorder in the United States from a societal perspective. J. Clin. Psychiatry 83(3), 21m14116 (2022). [DOI] [PubMed] [Google Scholar]
- 11.Herrera-Escobar JP, Deroon-Cassini T, Brasel K et al. Development and validation of a revised trauma-specific quality of life instrument. J. Trauma Acute Care Surg. 88(4), 501–507 (2020). [DOI] [PubMed] [Google Scholar]
- 12.Davis LL, Urganus A, Gagnon-Sanschagrin P et al. Patient journey before and after a formal post-traumatic stress disorder diagnosis in adults in the United States – a retrospective claims study. Curr. Med. Res. Opin. (2023). [DOI] [PubMed] [Google Scholar]
- 13.IBM MarketScan Research Databases is now Merative™ MarketScan® Research Databases. (2023). https://www.merative.com/real-world-evidence
- 14.Seng JS, Clark MK, Mccarthy AM, Ronis DL. PTSD and physical comorbidity among women receiving Medicaid: results from service-use data. J. Trauma. Stress 19(1), 45–56 (2006). [DOI] [PubMed] [Google Scholar]
- 15.Seng JS, Graham-Bermann SA, Clark MK, Mccarthy AM, Ronis DL. post-traumatic stress disorder and physical comorbidity among female children and adolescents: results from service-use data. Pediatrics 116(6), e767–776 (2005). [DOI] [PubMed] [Google Scholar]
- 16.Bowe A, Rosenheck R. PTSD and substance use disorder among veterans: characteristics, service utilization and pharmacotherapy. J. Dual Diagn. 11(1), 22–32 (2015). [DOI] [PubMed] [Google Scholar]
- 17.Soria-Saucedo R, Chung JH, Walter H, Soley-Bori M, Kazis LE. Factors that predict the use of psychotropics among children and adolescents with PTSD: evidence from private insurance claims. Psychiatr. Serv. 69(9), 1007–1014 (2018). [DOI] [PubMed] [Google Scholar]
- 18.Hsu TW, Bai YM, Tsai SJ, Chen TJ, Chen MH, Liang CS. Risk of autoimmune diseases after post-traumatic stress disorder: a nationwide cohort study. Eur. Arch. Psychiatry Clin. Neurosci. (2023). [DOI] [PubMed] [Google Scholar]
- 19.Wang TY, Wei HT, Liou YJ et al. Risk for developing dementia among patients with post-traumatic stress disorder: a nationwide longitudinal study. J. Affect. Disord. 205, 306–310 (2016). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.