Abstract
Background:
Mold exposures may contribute to the development of asthma, but previous studies have lacked a standardized approach to quantifying exposures.
Objective:
To determine whether mold exposures at the ages of 1 and/or 7 years were associated with asthma at the age of 7 years.
Methods:
This study followed up a high-risk birth cohort from infancy to 7 years of age. Mold was assessed by a DNA-based analysis for the 36 molds that make up the Environmental Relative Moldiness Index (ERMI) at the ages of 1 and 7 years. At the age of 7 years, children were evaluated for allergic sensitization and asthma based on symptom history, spirometry, exhaled nitric oxide, and airway reversibility. A questionnaire was administered to the parent regarding the child’s asthma symptoms and other potential cofactors.
Results:
At the age of 7 years, 31 of 176 children (18%) were found to be asthmatic. Children living in a high ERMI value (≥5.2) home at 1 year of age had more than twice the risk of developing asthma than those in low ERMI value homes (<5.2) (adjusted odds ratio [aOR], 2.6; 95% confidence interval [CI], 1.10–6.26). Of the other covariates, only parental asthma (aOR, 4.0; 95% CI, 1.69–9.62) and allergic sensitization to house dust mite (aOR, 4.1; 95% CI, 1.55–11.07) were risk factors for asthma development. In contrast, air-conditioning at home reduced the risk of asthma development (aOR, 0.3; 95% CI, 0.14–0.83). A high ERMI value at 7 years of age was not associated with asthma at 7 years of age.
Conclusions:
Early exposure to molds as measured by ERMI at 1 year of age, but not 7 years of age, significantly increased the risk for asthma at 7 years of age.
INTRODUCTION
Asthma is a multifactorial disease that may be modulated by social, environmental, and genetic factors.1,2 Asthma afflicts approximately 9% of school-age children, but the rates of asthma are often higher in children from poor, urban families.1 The direct medical costs of asthma are approximately $15 billion per year, with several thousand deaths and millions of lost work and school days.3 Asthma may have its origin in early life but once developed may persist for a lifetime.4,5 Environmental exposures during the first 3 years of life may be at least 1 of the critical risk factors.5
The present investigation is a part of the prospective Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS), which is investigating the role of aeroallergens and traffic exhaust in the development of atopic respiratory disorders.6,7 The major focus of this substudy of CCAAPS was exposure to molds during infancy and later childhood and the development of asthma. The Institutes of Medicine8 and World Health Organization (WHO)9 reviews of the scientific literature regarding dampness and/or mold and asthma concluded that there was an association between building dampness and/or mold and respiratory health effects, including asthma, which needs further clarification.
One of the problems with mold exposure estimates is the lack of quantitative standardized methods for describing the residential mold burden.10 A metric called the Environmental Relative Moldiness Index (ERMI) has recently been developed and validated in a national survey of homes.11 A DNA-based mold-specific quantitative polymerase chain reaction (MSQPCR) of 26 group 1 species associated with water-damaged homes and 10 group 2 species found in homes independent of water damage forms the basis of the ERMI.11 The unitless ERMI scale usually ranges from approximately −10 to 20 and is divided into quartiles, with the highest-quartile homes (ERMI value >5) having the highest mold burden.11
Previously, we reported that a higher ERMI value in the CCAAPS infants’ homes was predictive of the development of wheeze and rhinitis at 3 years of age.12 The children of this cohort have now reached an age (7 years) when spirometry with bronchodilator and methacholine challenge tests can be performed. This study reports on the assessment of residential mold exposures at the ages of 1 and 7 years and the association with asthma at 7 years of age.
METHODS
Study Population
Infants born in Cincinnati, Ohio, and Northern Kentucky between 2001 and 2003 were recruited using birth certificate data to obtain residential addresses. Eligibility for the study required that at least 1 parent was atopic, which was defined as having allergic symptoms and a positive reaction on a skin prick test to at least 1 of 15 common aeroallergens.6 The main focus of the overall CCAAPS was proximity to traffic; therefore, the primary selection criterion was based on birth addresses, with the test group being within 400 m and the control group being more than 1,500 m from a highway.6 Recruitment for the present substudy (n = 176) was performed from a pool of 577 CCAAPS dwellings that had a home assessment completed when the infant was 1 year of age and a recent clinical evaluation. For every home that contained some form of damage at this time point (visible mold, moldy odor, water damage, or history of water damage), a home with no reported mold or water damage was randomly selected.15 Of the 220 children invited for the in-home follow-up assessment, 21 (9.5%) were not reached, 6 (2.7%) had moved out of the area, 8 (3.6%) refused to participate, and 9 (4.1%) did not participate in the clinical evaluation. The study was approved by the institutional review board at the University of Cincinnati. Signed informed consent forms were obtained from parents.
Asthma Diagnosis
Children enrolled in CCAAPS were offered a clinical evaluation at the ages of 1, 2, 3, 4, and 7 years. Each clinical examination consisted of skin prick testing for 15 aeroallergens and milk and egg.6,13 In this study, we investigated the association between asthma and allergic sensitization to molds (Aspergillus, Alternaria, Cladosporium, and Penicillium), cat, dog, and house dust mite. In addition, a questionnaire on the infants’ exposure, health, and demographics was administered to the caregiver. At 7 years of age, the children also completed spirometry and tests for exhaled nitric oxide concentration (NIOX Flex; Aerocrine Inc, New Providence, New Jersey) and airway reversibility and/or airway hyperreactivity as described below.
Participating children underwent spirometry performed by trained technicians according to American Thoracic Society criteria. A subset of children received additional lung function testing. Those reporting asthma symptoms, an exhaled nitric oxide concentration greater than 10 ppb, or a predicted forced expiratory volume in 1 second (FEV1) less than 90% and/or an FEV1 ratio to forced vital capacity less than the lower limit of normal were administered 2.5 mg of levalbuterol by nebulizer followed in 15 minutes by repeat spirometry. Those with a 12% or lower increase in FEV1 after bronchodilation underwent methacholine challenge testing at a second visit. Children were defined as asthmatic if they fulfilled 2 criteria: (1) caregiver report of asthma symptoms and (2) demonstration of airway reversibility (defined as ≥12% increase in FEV1 after bronchodilation) or a positive methacholine challenge test result (defined as a ≥20% decrease in baseline FEV1 at a cumulative inhaled methacholine concentration of ≤4 mg/mL). Asthma symptoms included caregiver report of at least 1 of the following: (1) a tight or clogged chest or throat in the past 12 months, (2) difficulty breathing or wheezy after exercise, (3) wheezing or whistling in the chest in the previous 12 months, or (4) a previous physician diagnosis of asthma.
On-Site Home Visit and Exposure Assessment
On-site home visits were performed by trained 2-person teams when the infants were approximately 1 and 7 years of age. The purposes of the home evaluation were to investigate the presence of mold damage and to collect floor dust samples for mold exposure assessment.14,15 Dust samples were collected by vacuuming in the room where the child reportedly spend most of his/her time. Large dust particles were removed by sieving (355-μm sieve), and the fine dust was divided into subsamples and stored at −20°C before analyses.15
Mold Inspection and Classification
Simultaneously with dust sampling, a home inspection was performed and a questionnaire administered concerning home and family characteristics. Recorded home characteristics included age of the house and use of air-conditioning and dehumidifier. Among the family characteristics, household income, child’s race and sex, cigarette consumption, season of child’s birth, and parental asthma were documented.
At the time of inspection, an indoor visual and olfactory observation of the house conditions was conducted for the presence of carpets and evidence of mold. Class 0 homes had no history or signs of mold and/or water damage, including no moldy odor. Class 1 homes had either minor indications of mold and/or water damage or history of mold and/or water damage. Class 2 homes had at least 0.2 m2 of visible mold or mold and water damage combined.15
DNA Extraction and MSQPCR Analysis
Five milligrams of sieved dust was extracted and the DNA purified using the DNA-EZ kit (GeneRite, North Brunswick, New Jersey) and then the extract analyzed by MSQPCR, all as previously described.16,17
Statistical Analyses
The primary objective of this study was to evaluate the relationship between asthma at 7 years of age and levels of mold exposure in the child’s home at 1 and 7 years of age, adjusted for demographic, family, and home characteristics. The primary measure of mold exposure was the ERMI. A Bayesian change-point analysis was applied to the logit of predicted values from a nonlinear regression of asthma on the ERMI. The posterior probabilities of a change in the mean of the distribution of ERMI values at partitions of ordered values of the logit of ERMI were calculated. Lines were drawn connecting change points, which defined intervals where predicted values were relatively constant. The length of the interval shown in Figure 1 was, by far, the longest, indicating that a dichotomization of the ERMI at 5.2 was appropriate in regression models.
Figure 1.
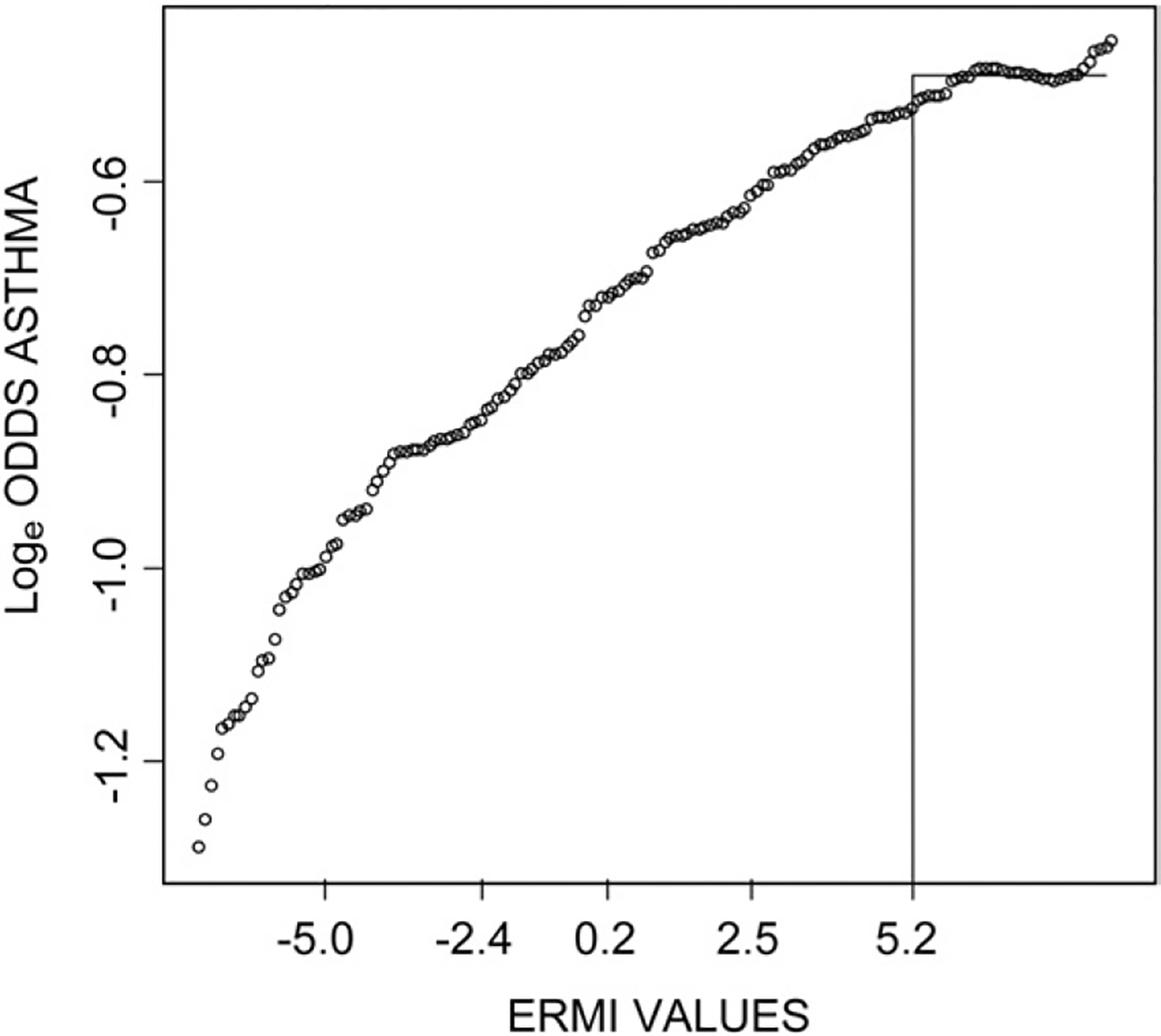
The change-point analysis plot. The line at the Environmental Relative Moldiness Index (ERMI) value of 5.2 represents the threshold above which the loge odds of asthma were relatively constant. The open circles represent the ERMI values in child’s home at age 1 and corresponding probabilities of the child developing asthma at age 7.
The associations between asthma and each independent variable (family and home characteristics) and ERMI were evaluated by univariate logistic regression. All independent variables that were significant at the 15% level were included in an initial multivariate model. These included ERMI, parental asthma, race, allergic sensitization to house dust mite, income, household cigarette smoking, and central air-conditioning at 1 year of age. The final multivariate model was obtained by sequential analyses using stepwise regression. A priori ERMI was maintained in each subsequent model, and other variables were assessed for removal beginning with the one having the highest P value. Previously removed variables were reentered at various stages to allow for the possibility that significance levels may have changed because of changes in the model. The final multivariate model included all independent variables with P < .05 and ERMI. Approximately 60% of the families moved between the home visits conducted at 1 and 7 years of age.15 Therefore, the multiple regression analysis was repeated using a logistic regression model stratified by moving status (moved or not moved). A sensitivity analysis of the final model was performed, in which 2 high ERMI values (29.7 and 31.2) were excluded from the analysis. Inferences were obtained by applying the generalized estimating equation method and using robust estimation of standard errors. The possibility of effect modification of the ERMI-asthma relationship was assessed for each independent variable that was initially evaluated for model inclusion. A logistic regression model was analyzed that included the independent variable, ERMI, and their interaction.
Analysis of variance and independent t tests were performed to compare mean values of ERMI at 1 year of age to categories of child demographic, family, and home characteristics at 1 year of age. SAS statistical software, version 9.2 (SAS Institute Inc, Cary, North Carolina), was used for the analyses. P ≤ .05 was considered to indicate statistical significance unless stated otherwise.
RESULTS
Of the 176 children in this substudy, 27% were black, 58% were male, 32% had a parent with asthma, and 18% were diagnosed as having asthma at 7 years of age (Table 1). A statistically significant increase in the risk of asthma was associated with parental asthma (odds ratio [OR], 3.9; 95% confidence interval [CI], 1.75–8.71), race (black vs other) (OR, 3.2; 95% CI, 1.42–7.11), and allergic sensitization to house dust mite (OR, 3.3; 95% CI, 1.34–8.14) (Table 1). Child sex and season of birth, however, were not significant. No significant difference was found in the mold sensitization between the high ERMI group (2.1%) and the low ERMI group (7.2%) (Fisher exact test P = .18) (data not shown).
Table 1.
Unadjusted ORs (95% CIs) for Asthma Diagnosis at 7 Years of Age According to the Demographic Characteristics of the 176 Study Children
| Characteristic | Asthma, No. (%) (n = 31) | Nonasthma, No. (%) (n = 145) | OR (95% CI) |
|---|---|---|---|
| Parental asthma (yes vs no) | 18 (58) | 38 (26) | 3.9 (1.75–8.71) |
| Race (black vs other) | 15 (48) | 33 (23) | 3.2 (1.42–7.11) |
| Sex (male vs female) | 19 (61) | 83 (57) | 1.2 (0.53–2.62) |
| Season of birth | |||
| Spring | 4 | 18 | 1.2 (0.33–4.57) |
| Summer | 8 | 25 | 1.8 (0.59–5.27) |
| Fall | 11 | 58 | 1.0 (0.39–2.81) |
| Winter | 8 | 44 | Referent |
| Allergic sensitization at 7 years of age | |||
| Mold (positive to any 4 mold types vs negative) | 3 (10) | 7 (5) | 2.1 (0.51–8.67) |
| Cat or dog (positive vs negative) | 8 (26) | 22 (15) | 1.9 (0.77–4.90) |
| Dust mite (positive vs negative) | 10 (32) | 18 (13) | 3.3 (1.34–8.14) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Univariate Analysis
Table 2 lists the unadjusted risk factors for 1 and 7 years of age and the risk of asthma at 7 years of age. At both ages, low family income (<$40,000 vs >$70,000 per year) was a significant independent risk factor for child asthma (OR, 3.7; 95% CI, 1.14–11.70; vs OR, 7.4; 95% CI, 2.31–23.74). Living in a home with air-conditioning at both 1 (OR, 0.3; 95% CI, 0.14–0.70) and 7 (OR, 0.3; 95% CI, 0.11–0.69) years of age was significantly associated with reduced asthma risk at 7 years of age.
Table 2.
Unadjusted ORs (95% CIs) for Having Asthma at 7 Years of Age by Characteristics of 6 Study Children at 1 and 7 Years of Age
| Characteristic | 1 Year of age | 7 Years of age | ||||
|---|---|---|---|---|---|---|
| Asthma at 7 years of age (n = 31) | Nonasthma at 7 years of age (n = 145) | OR (95% CI) | Asthma at 7 years of age (n = 31) | Nonasthma at 7 years of age (n = 145) | OR (95% CI) | |
| Family characteristics | ||||||
| Annual incomea | ||||||
| <$40,000 | 18 | 48 | 3.7 (1.14–11.70) | 18 | 34 | 7.4 (2.31–23.74) |
| $40,000–$70,0000 | 9 | 58 | 1.5 (0.44–5.26) | 9 | 55 | 2.3 (0.67–7.88) |
| >$70,000 | 4 | 39 | Referent | 4 | 56 | Referent |
| Cigarette smoking (yes vs no) | 12 (39) | 33 (23) | 2.1 (0.94–4.87) | 12 (40) | 26 (18) | 3.0 (1.31–7.03) |
| Home characteristics | ||||||
| Air-conditioning (yes vs no) | 16 (52) | 112 (77) | 0.3 (0.14–0.70) | 21 (68) | 128 (88) | 0.3 (0.11–0.69) |
| Dehumidifier (yes vs no) | 5 (16) | 23 (16) | 1.0 (0.35–2.93) | 6 (19) | 37 (26) | 0.7 (0.27–1.84) |
| Carpet (yes vs no) | 27 (87) | 119 (82) | 1.5 (0.48–4.58) | 26 (84) | 110 (76) | 1.7 (0.59–4.63) |
| Age of home (year built) | ||||||
| Before 1955 | 12 | 51 | 1.7 (0.55–5.23) | 13 | 45 | 2.6 (0.90–7.26) |
| 1955–1985 | 14 | 58 | 1.7 (0.58–5.23) | 12 | 47 | 2.3 (0.78–6.48) |
| After 1985 | 5 | 36 | Referent | 6 | 53 | Referent |
| Mold category based on visual and olfactory inspection | ||||||
| High (2) | 1 | 17 | 0.3 (0.03–2.04) | 4 | 15 | 1.1 (0.29–4.52) |
| Low (1) | 12 | 50 | 1.0 (0.46–2.34) | 20 | 100 | 0.8 (0.33–2.20) |
| No (0) | 18 | 78 | Referent | 7 | 30 | Referent |
| Exposure | ||||||
| ERMI | ||||||
| ≥5.2 | 15 | 33 | 3.1 (1.38–6.93) | 6 | 39 | 0.7 (0.25–1.71) |
| <5.2 | 16 | 109 | Referent | 25 | 106 | Referent |
Abbreviations: CI, confidence interval; ERMI, Environmental Relative Moldiness Index; OR, odds ratio.
The cut points for income group were approximately tertile. Values were adjusted down in year 7 for inflation.
Cigarette smoking in the home at 7 years of age, but not at 1 year of age, was a significant predictor of asthma at 7 years of age (OR, 3.0; 95% CI, 1.31–7.03) (Table 2). In contrast, a high ERMI value (≥5.2) at 1 year of age only was a significant predictor of asthma at 7 years of age (OR, 3.1; 95% CI, 1.38–6.93). In addition, it was found that the use of home dehumidifiers, presence of carpeting, age of home, and the categorization of home moldiness based on visual inspection at 1 and 7 years of age were not significant predictors of asthma development.
Multivariate Analysis
The final multivariate model for exposures at 1 year of age and asthma at 7 years of age examined all factors that were significantly related to asthma at the 15% significance level (Tables 1 and 2). Table 3 indicates that the odds of developing asthma if a child lived in a high ERMI value home at 1 year of age were 2.4 times greater than the odds for a child who lived in low ERMI value home (adjusted OR [aOR], 2.4; 95% CI, 1.04–5.73). Parental asthma, allergic sensitization to house dust mite, and air-conditioning remained statistically significant in the multivariate model, which initially also included race, income, and cigarette smoking. When the 2 separate sensitivity analyses were performed by stratifying by moving status or when the 2 highest ERMI values were excluded, the results were essentially unchanged. Effect modification was detected for dehumidifier use only (P < .15), and therefore dehumidifier use and its interaction with ERMI were added to the final multivariate model. The interaction effect and the main effect were not significant at the 5% level, and thus both were removed.
Table 3.
aORs (95% CIs) for Asthma Diagnosis at 7 Years of Age by Predictor Variables of the 176 Study Children
| Predictor variablea | aOR (95% CI) |
|---|---|
| ERMI at 1 year of age (high vs low)b | 2.6 (1.10–6.26) |
| Parental asthma (yes vs no) | 4.0 (1.69–9.62) |
| Dust mite sensitization at 7 years of age (positive vs negative) | 4.1 (1.55–11.07) |
| Air-conditioning at 1 year of age (yes vs no) | 0.3 (0.14–0.83) |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; ERMI, Environmental Relative Moldiness Index.
These variables remained statistically significant (P < .05) in a full multivariate model, which initially included ERMI, parental asthma, air-conditioning, race, income, and cigarette smoking.
High ERMI defined as 5.2 or greater.
Family and Home Characteristics
Because a high ERMI index at 1 year of age was significantly associated with asthma development at 7 years of age, we examined what characteristics of the child’s home or family might have been linked to this exposure. Hence, the relationship between ERMI category and characteristics at 1 year of age was investigated (Table 4). The odds of having a home with a high ERMI value were significantly and positively associated with race (black vs other) (OR, 3.0; 95% CI, 1.45–6.06) and negatively associated with home air-conditioning (OR, 0.4; 95% CI, 0.19–0.79). Carpeting, dehumidifier, age of the home, and the moldiness category were not significantly associated with the ERMI.
Table 4.
Mean (SD) ERMI Values at 1 Year of Age and Unadjusted OR Associations Between ERMI Categories and Demographic, Family, and Home Characteristics at 1 Year of Age for the 176 Study Children
| Characteristics | No. of patients | Mean (SD) ERMI at 1 year of age | OR (95% CI) |
|---|---|---|---|
| Child demographics | |||
| Parental asthma | |||
| Yes | 56 | 3.51 (7.44) | 1.6 (0.78–3.12) |
| No | 120 | 2.05 (7.61) | Referent |
| Race | |||
| Black | 48 | 4.59 (8.20) | 3.0 (1.45–6.06) |
| Other | 128 | 1.75 (7.20) | Referent |
| Sex | |||
| Male | 102 | 1.44 (6.96) | 0.6 (0.32–1.22) |
| Female | 74 | 4.04 (8.15) | Referent |
| Season of birth | |||
| Spring | 22 | 1.28 (7.27) | 1.3 (0.41–4.09) |
| Summer | 33 | 4.63 (8.67) | 2.4 (0.93–6.17) |
| Fall | 69 | 2.32 (7.77) | 1.0 (0.42–2.35) |
| Winter | 52 | 1.94 (6.55) | Referent |
| Family characteristics | |||
| Annual incomea | |||
| <$40,000 | 66 | 3.82 (8.18) | 1.6 (0.66–4.03) |
| $40,000–$70,000 | 67 | 2.82 (7.53) | 1.5 (0.60–3.68) |
| >$70,000 | 43 | 0.04 (6.06) | Referent |
| Cigarette smoking (yes vs no) | |||
| Yes | 45 | 5.06 (8.32) | 1.4 (0.69–3.00) |
| No | 131 | 1.63 (7.11) | Referent |
| Home characteristics | |||
| Air-conditioning | |||
| Yes | 128 | 1.27 (6.78) | 0.4 (0.19–0.79) |
| No | 48 | 5.88 (8.57) | Referent |
| Dehumidifier | |||
| Yes | 28 | 2.16 (6.93) | 1.4 (0.57–3.31) |
| No | 148 | 2.59 (7.70) | Referent |
| Carpet | |||
| Yes | 146 | 2.38 (7.28) | 0.9 (0.37–2.07) |
| No | 30 | 3.20 (8.94) | Referent |
| Age of home (year built)a | |||
| Before 1955 | 63 | 5.32 (7.88) | 1.9 (0.79–4.59) |
| 1955–1985 | 72 | 0.76 (6.80) | 0.7 (0.25–1.66) |
| After 1985 | 41 | 1.22 (7.22) | Referent |
| Mold category based on visual and olfactory inspection | |||
| 2 | 18 | 2.90 (9.77) | 1.2 (0.59–2.46) |
| 1 | 62 | 3.81 (7.64) | 1.1 (0.35–3.33) |
| 0 | 96 | 1.63 (7.00) | Referent |
Abbreviations: OR, adjusted odds ratio; CI, confidence interval; ERMI, Environmental Relative Moldiness Index.
The cut points for income group were approximately tertile.
DISCUSSION
This study has demonstrated that a high ERMI value in a home during infancy was associated with asthma diagnosis at 7 years of age. The odds of developing asthma were more than 2-fold if an infant lived in a high (≥5.2) vs low (<5.2) ERMI value home. The children examined in the present effort have previously been evaluated at 3 years of age for the development of wheeze and rhinitis, and a higher ERMI value measured at 1 year of age was also predictive of these conditions.12 However, not all children with wheeze and rhinitis develop asthma.18
Our results support previous studies showing that only a small percentage of mold-exposed people develop allergies to mold.19,20 The toxicologic mechanisms of health effects associated with mold exposures are complex and may include nonallergic mechanisms in addition to the classic allergic pathway.21 However, the 4 mold types included in the skin prick test panel represent only a small fraction of possible molds in homes. Additional research is needed to determine which mold species may be the most relevant for asthma pathogenesis. Our study also supports the well-established association between allergic sensitization to house dust mites and asthma.22 Sensitization to house dust mite in our study was significantly associated with asthma but was not a confounder of the ERMI-asthma relationship. Our study revealed that visual and olfactory observations of moldiness in the home of the child at 1 or 7 years of age were not predictive of asthma development at 7 years of age. This finding is consistent with the results demonstrating that homeowners and inspectors were unaware of or failed to detect significant mold problems in homes approximately 50% of the time.23
The WHO report entitled Indoor Air Guidelines: Dampness and Mold9 concluded that there is an association between dampness and/or mold and asthma. As a result, the WHO recommendation was to “minimize the exposure to molds.” To minimize exposure, however, the optimum approach would be to first quantify exposure in a standardized and objective manner and then implement an intervention with a follow-up exposure assessment.
US Environmental Protection Agency researchers, in conjunction with the US Department of Housing and Urban Development, standardized the sampling protocol for molds in homes and created a metric for describing the mold burden, the national ERMI.11 The application of the ERMI in this prospective study provided a predictive model, which showed that children residing in homes during early childhood with an ERMI value greater than 5.2 were significantly more likely to develop asthma at 7 years of age than children living in homes with an ERMI value below 5.2.
The ERMI analysis of dust samples has been applied in 3 other asthma studies. Homes in Cleveland, Ohio, with higher ERMI values, compared with control homes, were more likely to have a resident asthmatic child.24 Remediation of these homes resulted in significant reductions in hospital interventions for the children’s asthma.25 The ERMI was also used in studies in Detroit, Michigan,26 and Raleigh, North Carolina,27 which also showed significantly higher ERMI values in asthmatic children’s homes.
Only a few published longitudinal studies have assessed mold exposure before the asthma diagnosis,28–30 and the methods used for quantifying mold exposures were not standardized.10 The ERMI provides a simple metric for quantitatively describing the mold burdens in homes and for targeting mold remediation. The threshold ERMI value for this group of infants was 5.2. This value closely matches the highest mold burden quartile, which starts at approximately 5 on the national ERMI.
Overall, the total lifetime economic impact of a single case of asthma in 1999 (the year data were available) was $49,000 for an average asthma patient and $202,000 for a more severe case.31 Preventing some infants from being exposed to high ERMI value homes might prevent some cases of asthma, especially in homes of infants whose parents have a history as asthma. In addition, the homes of the children who developed asthma during this study typically lacked air-conditioning. The use of air-conditioning may help decrease the level of moisture in the home, which could reduce the mold growth, resulting in lower ERMI values. The study results suggest that exposure to mold during infancy is associated with the development of asthma, although further research using the ERMI approach is warranted. In addition, intervention studies for high-risk families, with the objective of reducing mold exposure by reducing the ERMI values in the home, are needed to further delineate the relationship between ERMI and the development of or exacerbation of asthma.
In summary, children at highest risk for developing asthma were those living in high ERMI value homes at 1 year of age, those without air-conditioning, and those who had a parent with asthma. This study does not prove that exposures to mold are a cause of asthma, but it does provide impetus to reduce the mold burden in infant homes based on the ERMI.
ACKNOWLEDGMENTS
We are grateful to all parents and children who participated in the study and to all home visit teams, subject recruitment teams, and clinic personnel of the CCAAPS.
Funding Sources:
This study was partially supported by the US Department of Housing and Urban Development grant OHLHH0162-07 and by the National Institute of Environmental Health Sciences grants RO1 ES11170 and ES10957 awarded to the University of Cincinnati. In addition, this research was supported by funding from the Environmental Protection Agency (EPA) Asthma Initiative.
Disclaimer:
The EPA through its Office of Research and Development funded and collaborated in the research described here. It has been subjected to the agency’s peer review and has been approved as an EPA publication. Mention of trade names or commercial products does not constitute endorsement or recommendation by the EPA for use.
Footnotes
Disclosures: Authors have nothing to disclose. The United States Environmental Protection Agency can derive royalties from the commerical use of MSQPCR.
REFERENCES
- 1.Eggleston PA. The environment and asthma in US inner cities. Chest. 2007;132(suppl):782S–788S. [DOI] [PubMed] [Google Scholar]
- 2.Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect. 2007;115:971–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss KB, Sullivan SD. The health economics of asthma and rhinitis, I: assessing the economic impact. J Allergy Clin Immunol. 2001;107:3–8. [DOI] [PubMed] [Google Scholar]
- 4.Arshad SH. Does exposure to indoor allergens contribute to the development of asthma and allergy? Curr Allergy Asthma Rep. 2010;10: 49–55. [DOI] [PubMed] [Google Scholar]
- 5.Saglani S, Bush A. The early-life origins of asthma. Curr Opin Allergy Clin Immunol. 2007;7:83–90. [DOI] [PubMed] [Google Scholar]
- 6.Ryan PH, LeMasters G, Biagini J, et al. Is it traffic type, volume, or distance? wheezing in infants living near truck and bus traffic. J Allergy Clin Immunol. 2005;16:279–284. [DOI] [PubMed] [Google Scholar]
- 7.Ryan PH, Lemasters GK, Biswas P, et al. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect. 2007;115:278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine, National Academies of Science. Damp Indoor Spaces and Health. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 9.World Health Organization (WHO) Europe. WHO Guidelines for Indoor Air Quality: Dampness and Mould. Copenhagen, Denmark: WHO; 2009. [PubMed]
- 10.Vesper S. Traditional mould analysis compared to a DNA-based method of mould analysis. Crit Rev Microbiol. 2010;37:15–24. [DOI] [PubMed] [Google Scholar]
- 11.Vesper SJ, McKinstry C, Haugland RA, et al. Development of an environmental relative moldiness index for homes in the U.S. J Occup Environ Med. 2007;49:829–833. [DOI] [PubMed] [Google Scholar]
- 12.Vesper SJ, McKinstry C, Haugland RA, et al. Relative moldiness index as predictor of childhood respiratory illness. J Exp Sci Environ Epidemiol. 2007;17:88–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LeMasters G, Wilson K, Levin L, et al. High prevalence of aeroallergen sensitization among infants of atopic parents. J Pediatr. 2006;149: 505–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cho SH, Reponen T, Bernstein DI, et al. The effect of home characteristics on dust antigen concentrations and loads in homes. Sci Total Environ. 2006;371:31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reponen T, Singh U, Schaffer C, et al. Visually observed mold and moldy odor versus quantitatively measured microbial exposure in homes. Sci Total Environ. 2010;408:5565–5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haugland RA, Brinkman NE, Vesper SJ. Evaluation of rapid DNA extraction methods for the quantitative detection of fungal cells using real time PCR analysis. J Microbiol Meth. 2002;50:319–323. [DOI] [PubMed] [Google Scholar]
- 17.Haugland RA, Varma M, Wymer LJ, Vesper SJ. Quantitative PCR of selected Aspergillus, Penicillium and Paecilomyces species. Syst Appl Microbiol. 2004;27:198–210. [DOI] [PubMed] [Google Scholar]
- 18.Van Cauwenberge P, Watelet JB, Van Zele T, et al. ; GA2LEN work packages 3.2 and 3.3. 2007: does rhinitis lead to asthma? Rhinology. 2007;45:112–121. [PubMed] [Google Scholar]
- 19.Taskinen T, Meklin T, Nousiainen M, Husman T, Nevalainen A, Korppi M. Moisture and mould problems in schools and respiratory manifestations in schoolchildren: clinical and skin test findings. Acta Paediatr. 1997;86:1181–1187. [DOI] [PubMed] [Google Scholar]
- 20.Immonen J, Meklin T, Taskinen T, Nevalainen A, Korppi M. Skin-prick test findings in students from moisture- and mould-damaged schools: a 3-year follow-up study. Pediatr Allergy Immunol. 2001;12:87–94. [DOI] [PubMed] [Google Scholar]
- 21.Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect. 2011. Jan 26 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heinrich J. Influence of indoor factors in dwellings on the development of childhood asthma. Int J Hyg Environ Health. 2011;214:1–25. [DOI] [PubMed] [Google Scholar]
- 23.Vesper S, McKinstry C, Cox D, Dewalt G. Correlation between ERMI values and other moisture and mold assessments of homes in the American Healthy Homes Survey. J Urban Health. 2009;86:850–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vesper SJ, McKinstry C, Yang C, et al. Specific molds associated with asthma. J Occup Environ Med. 2006;48:852–858. [DOI] [PubMed] [Google Scholar]
- 25.Kercsmar CM, Dearborn DG, Schluchter MD, et al. Urban mold and moisture project: asthma intervention. Environ Health Perspect. 2006; 114:1574–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vesper S, McKinstry C, Haugland R, et al. Higher Environmental Relative Moldiness Index (ERMIsm) values measured in Detroit homes of severely asthmatic children. Sci Total Environ. 2008;394:192–196. [DOI] [PubMed] [Google Scholar]
- 27.Vesper SJ, McKinstry C, Ashley P, et al. Quantitative PCR analysis of molds in the dust from homes of asthmatic children in North Carolina. J Environ Monit. 2007;9:826–830. [DOI] [PubMed] [Google Scholar]
- 28.Wickman M, Ahlstedt S, Lilja G, van Hage Hamsten M. Quantification of IgE antibodies simplifies the classification of allergic diseases in 4-year-old children: a report from the prospective birth cohort study–BAMSE. Pediatr Allergy Immunol. 2003;14:441–447. [DOI] [PubMed] [Google Scholar]
- 29.Belanger K, Beckett W, Triche E, et al. Symptoms of wheeze and persistent cough in the first year of life: associations with indoor allergens, air contaminants, and maternal history of asthma. Am J Epidemiol. 2003;158:195–202. [DOI] [PubMed] [Google Scholar]
- 30.Jaakkola JJ, Hwang BF, Jaakkola N. Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environ Health Perspect. 2005;113:357–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US EPA Cost of Illness Handbook. 2010. http://www.epa.gov/opptintr/coi/pubs/toc.html. Accessed March 26, 2011.


