ABSTRACT
Context:
Over-medicalization of normal pregnancy is associated with unnecessary inductions of labor leading to operative deliveries. In a busy outpatient department (OPD) or low-resource setup where ultrasound availability, experience, and cost will be a concern, routine ultrasound at term can be avoided if the clinical estimation of fetal weight is more or less equal to the actual birth weight.
Aims:
To assess the reliability and validity of fetal weight estimation at term by ultrasound and clinical estimation.
Settings and Design:
A prospective study of diagnostic accuracy was done over a period of 1.5 years in a tertiary hospital, which included 100 women with term singleton pregnancies admitted in obstetric wards or labor room.
Methods and Material:
To find out the agreement between actual birthweight and ultrasound fetal weight interclass correlation coefficient (ICC) was used. Mean difference plots (Bland–Altman plots) were done. The mean percentage error was compared with the consultant estimate and registrar estimate across groups. The sensitivity, specificity, and predictive values by clinical and ultrasound estimate were calculated for actual birth weight ≤ 2.5 kg.
Results:
Both methods of fetal weight estimation have moderate reliability in predicting the actual birth weight. The sensitivity of identifying birthweight < 2.5 kg babies by ultrasound was slightly higher. For birth weight less than 2.5 kg, there was an overestimation of fetal weight by clinical estimation done by postgraduate with mean percentage error being statistically significant as compared with ultrasound estimation.
Conclusions:
In a developing country like ours where ultrasound is not readily available in all healthcare setups, the clinical method is an easy, cost-effective, simple one that can be used by all medical professionals after adequate training.
Keywords: Clinical estimation of fetal weight, estimation of fetal weight, fetal weight, Hadlock’s formula, Leopold’s maneuvers, ultrasound fetal weight estimation
Introduction
Estimation of fetal weight with reasonable accuracy is essential for successful management of labor and care of the newborn in the neonatal period. It also helps predict fetal macrosomia or low-birthweight babies, thereby avoiding complications due to the same. Thus, decreasing perinatal morbidity and mortality.[1,2,3,4,5] Correct estimation of fetal weight, along with gestational age and the adequacy of the mother’s pelvis, is important information for managing labor and delivery.
It is undeniable that knowing the estimated fetal weight (EFW) will prove beneficial for the mother and baby by helping in determining the timing and mode of delivery. Hence ultrasound (USG) in obstetrics is an important tool that has revolutionized obstetric care and reduced maternal and perinatal mortality and morbidity significantly.
However, over-medicalization of a normal pregnancy is associated with unnecessary inductions of labor, which results in unnecessary operative deliveries. In a busy outpatient department (OPD) or low-resource setup where USG availability, experience, the cost will be a concern, routine USG at term for fetal weight estimation can be avoided if the clinical estimation of fetal weight is more or less equal to the actual birth weight. Hence in this study, clinical and USG estimation of fetal weight was done on all recruited participants, and it was compared with actual birth weight.
Aim and Objectives
The study aims to assess the reliability and validity of fetal weight estimation at term by USG and clinical estimation. The objectives include the following:
To measure the interclass correlation of clinical estimate and USG estimate of fetal weight versus the actual birth weight.
To assess the sensitivity, specificity, and predictive values of clinical and USG estimation of fetal weight less than 2.5 kg.
To calculate the mean percentage error of the clinical method and USG method of fetal weight estimation among the various weight groups.
Materials and Methods
This was a prospective study of diagnostic accuracy that was done over a period of 1.5 years in a large tertiary center after institutional review board clearance was obtained. The procedures followed were in accordance with the ethical standards of the Institutional Review Board committee and with the Helsinki Declaration of 1975, as revised in 2000. The study included women with term singleton pregnancies admitted in obstetric wards or labor room for induction of labor or elective lower segment cesarean section (LSCS) who fulfill the eligibility criteria.
Inclusion criteria
Women at term (>37 weeks till 40 + 6 weeks)
Singleton pregnancy
Cephalic presentation
Intact membranes
Not in labor
Admitted in labor room or obstetric wards electively for induction of labor or elective LSCS
Planned for delivery within the next 48 Hours
Exclusion criteria
Multiple gestations
Poly and oligohydramnios
Previous abdominal or pelvic surgeries other than previous cesarean section
Malpresentation
Antepartum hemorrhage
Pregnancies with intrauterine fetal demise
Pelvic or abdominal masses and
Fetus with congenital anomalies
Clinical fetal weight estimation was done by Leopold’s Maneuvers by one final-year obstetric resident and by one obstetrics consultant with a minimum of 3 years but less than 5 years’ experience in the field. USG fetal weight estimation by Hadlock’s formula was performed by the primary investigator using a TOSHIBA FAMIO 30 USG machine or a GE LOGIQ-e USG machine with a 3.5 Hz transducer and curvilinear probe. Repeat USG was not done if the woman already had a scan with the EFW measured within 7 days of recruitment. The reference standard which is the actual birth weight was measured by a standard weighing scale in the labor room, which was calibrated monthly [Refer Figure 1].
Figure 1.
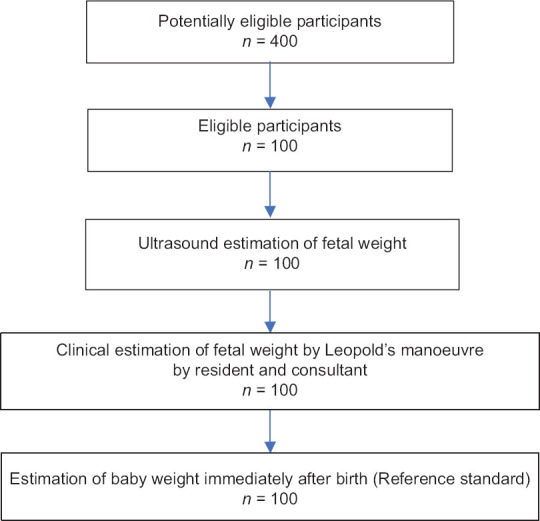
Flowchart of sampling method
Statistical analysis
The incidence of low birth weight was expected to be about 15%. To get 80% agreement (kappa statistic) that should be greater than the chance agreement of 50% with α and β errors at 5% and 10%, respectively, we had to study about 80 subjects who will go through USG and clinical estimation of birth weight. However, we studied about 100 subjects.
Descriptive statistics were used such as mean and standard deviation for age, body mass index (BMI), and gestational age, and frequency and percentage were presented for categorical variables. To find out the agreement between actual birthweight and USG fetal weight interclass correlation coefficient (ICC) was used. Mean difference plots (Bland–Altman) plots were done. The actual birth weight was categorized into four categories (groups) <2.5 kg, 2.5–3.0 kg, 3.0–3.5 kg, and > 3.5 kg. The mean percentage error was compared with the consultant estimate and registrar estimate across groups.
The mean percentage error represented the sum of the positive (overestimation) and negative (underestimation) estimation from actual birth weight. Wilcoxon signed ranks tests were used to look for significance.
To find the association between categorized birth weight and study variable, Chi-square test was used. The sensitivity, specificity, and predictive values by clinical and USG estimate were calculated for actual birth weight ≤ 2.5 kg. A P value less than 0.05 was considered statistically significant. All the analyses were carried out using Statistical Package for the Social Sciences (SPSS) v21.0.
Results
A total of 100 women were recruited for this study. There was no discontinuation or missing data in this study. Hence data was analyzed for 100 study samples. Their demographic profile is as follows [Refer Table 1].
Table 1.
Distribution of socio-demographic characteristics of the study group
| Parameters | Frequency (n) | Percentage | Mean |
|---|---|---|---|
| Age (Years) | |||
| 18–24 | 31 | 31.0 | 26.27 (3.91) |
| 25–30 | 54 | 54.0 | |
| >30 | 15 | 15.0 | |
| Gestational age | |||
| 37-37 + 6 weeks | 12 | 12.0 | 38.6 (4.03) |
| 38-38 + 6 weeks | 32 | 32.0 | |
| 39-39 + 6 weeks | 29 | 29.0 | |
| ≥40+ weeks | 27 | 27.0 | |
| BMI | |||
| <18.5 | 6 | 6.0 | 26.12 (5.35) |
| 18.5-<25 | 39 | 39.0 | |
| 25.0-<30 | 33 | 33.0 | |
| 30.0-<35 | 16 | 16.0 | |
| ≥35 | 6 | 6.0 | |
| Parity | |||
| Nulli | 71 | 71.0 | |
| 1 | 25 | 25.0 | |
| >1 | 4 | 4.0 | |
| Socioeconomic class | |||
| Upper | 9 | 9.0 | |
| Upper middle | 46 | 46.0 | |
| Middle | 26 | 26.0 | |
| Lower middle | 18 | 18.0 | |
| Lower | 1 | 1.0 |
The actual birth weight of the 100 subjects was grouped into four groups as follows [Refer Table 2]. A total of 47% study population had babies with birth weights between 2.6 kg and 3.0 kg. The minimum birth weight was 1.61 kg and the maximum birth weight was 3.77 kg. The mean birth weight was 2.852 kg. As seen in Table 2, in birthweight < 2.5 kg, clinical estimation is lower indicating overestimation. Similarly for birthweight > 3.5 kg, clinical estimation is lower indicating underestimation of weight.
Table 2.
Distribution of patients across various birth weight groups
| Actual birth weight | Ultrasound estimate | Clinical estimate | ||
|---|---|---|---|---|
|
| ||||
| Postgraduate | Consultant | |||
| ≤2.5 kg | 21 | 21 | 16 | 18 |
| 2.6–3.0 kg | 47 | 48 | 58 | 60 |
| 3.1–3.5 kg | 26 | 26 | 23 | 21 |
| >3.5 kg | 6 | 5 | 3 | 1 |
It was seen that the sensitivity of identifying birthweight < 2.5 kg babies by clinical method is the same among postgraduates and consultant (57.14%) [Refer Table 3]. The specificity and positive predictive values are higher in clinical estimates by postgraduates at 94.94% and 75.00%, respectively. The negative predictive value is almost the same among clinical estimate groups (89%). However, the sensitivity was higher by the USG estimate (66%) compared with the clinical estimate (57%).
Table 3.
Distribution of the power of sonographic and clinical methods of fetal weight estimation in predicting actual birth weight
| Method of estimation/birth weight ≤2.5 kg | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| Clinical | ||||
| By postgraduate | 57.14 | 94.94 | 75.00% | 89.29% |
| By consultant | 57.14 | 92.41 | 66.67% | 89.02% |
| Ultrasound | 66.67 | 91.14 | 66.67% | 91.14% |
As seen in Tables 4 and 5, the overall mean percentage error among clinical estimates by postgraduate is 1.55 while by consultant is − 0.01.
Table 4.
Accuracy between methods of fetal weight estimation
| Mean percentage error | Clinical estimate by Consultant | Ultrasound estimate | P |
|---|---|---|---|
| <2.5 kg | 8.53 (13.84) | 6.07 (10.96) | 0.313 |
| 2.5–3.0 kg | −0.30 (9.23) | 2.16 (9.48) | 0.063 |
| 3.1–3.5 kg | −3.73 (8.75) | −1.99 (9.71) | 0.316 |
| >3.5 kg | −11.54 (6.42) | −14.50 (9.50) | 0.753 |
| Overall | −0.01 (11.27) | 0.90 (10.83) | 0.43 |
Table 5.
Accuracy between methods of fetal weight estimation
| Mean percentage error | Clinical estimate by postgraduate | Ultrasound estimate | P |
|---|---|---|---|
| <2.5 kg | 11.96 (11.70) | 6.07 (10.96) | 0.001 |
| 2.5–3.0 kg | 1.75 (7.94) | 2.16 (9.48) | 0.922 |
| 3.1–3.5 kg | −4.19 (9.21) | −1.99 (9.71) | 0.123 |
| >3.5 kg | −11.52 (5.11) | −14.50 (9.50) | 0.249 |
| Overall | 1.55 (11.03) | 0.90 (10.83) | 0.429 |
Estimating fetal weight by USG has an overall mean percentage error of 0.90. However, the P value is not < 0.05, hence not statistically significant. However, the clinical estimate by the consultant has a lesser mean percentage error of 8.53, which is not statistically significant.
In birth weight groups 3.1 kg–3.5 kg and > 3.5 kg, we see there is an underestimation by clinical and USG methods. However, they are not statistically significant.
The interclass coefficient is shown in below Table 6.
Table 6.
Interclass coefficient between methods of fetal weight estimation
| Method of estimation Actual birth weight vs | ICC (95% Confidence Interval) (CI) | Percentage error | Precision |
|---|---|---|---|
| Ultrasound fetal weight | 0.739 (0.636, 0.817) | 0.22 | 0.617 |
| Clinical estimate by postgraduate | 0.722 (0.613, 0.804) | 0.212 | 0.595 |
| Clinical estimate by consultant | 0.74 (0.637, 0.817) | 0.212 | 0.589 |
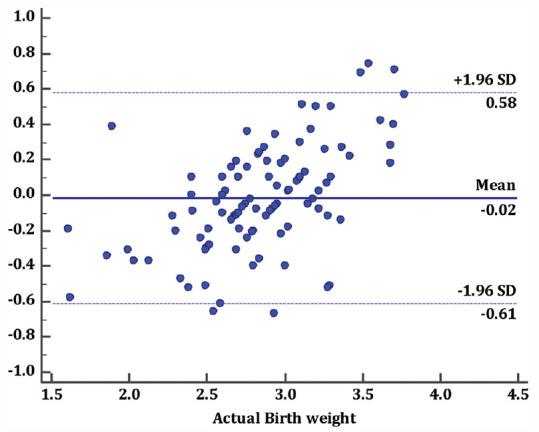
In the Bland–Altman plot [Refer Figures 2-4], the points are scattered all over the place, above and below zero. It suggests that there is no consistent bias of clinical/USG estimates versus actual birth weight.
Figure 2.
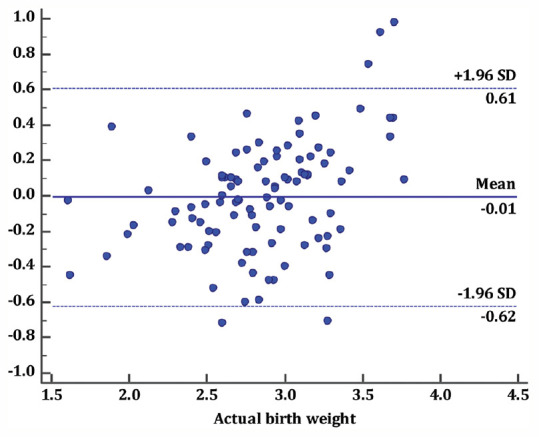
Plot 1: Actual birth weight vs. ultrasound fetal weight
Figure 4.
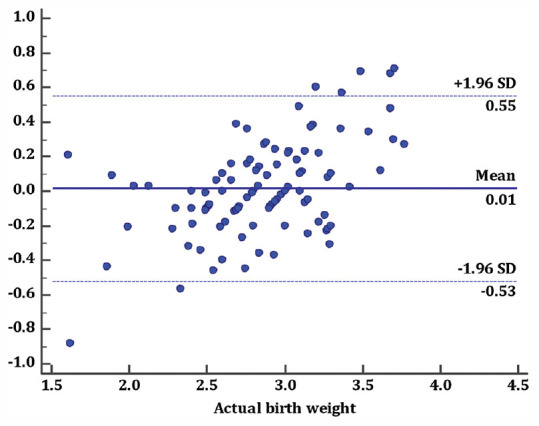
Plot 3: Actual birth weight vs. clinical estimate of fetal weight by consultant
Figure 3.
Plot 2: Actual birth weight vs. clinical estimate of fetal weight by postgraduate
Discussion
In our study, it is seen that the sensitivity of identifying birthweight < 2.5 kg babies by clinical method is the same among postgraduates and consultants (57.14%). The specificity and positive predictive value are higher in clinical estimates by postgraduate at 94.94% and 75.00%, respectively. The negative predictive value is almost the same among clinical estimate groups (89%). However, the sensitivity was higher by the USG estimate (66%) compared with the clinical estimate (57%).
A study by Ugwa et al.[6] in 2015, reported that in the 2.5 kg group, sensitivity, specificity, positive predictive value, and negative predictive value were better for sonographic than clinical estimates.
Noumi et al.[7] in 2004, showed that for both clinical and USG methods, the sensitivity was only 50% in predicting the birthweight of 4 kg or more.
In our study, it was seen that the ICC between the actual birth weight and USG fetal weight was found to be 0.739 (95% CI interval of 0.636, 0.817). This shows moderate reliability between the two groups. Similarly, the ICC between the actual birth weight and clinical estimate by postgraduate was found to be 0.72 (95% confidence interval of 0.613, 0.804). This shows moderate reliability between the two groups. Furthermore, 0.74 was the ICC between the actual birth weight and clinical estimate by the consultant (95% intraclass confidence interval of 0.637 and 0.817). This again shows moderate reliability between the two groups.
In previous studies, Predanic et al.[8] reported that a significant improvement in estimation of fetal weight occurred with advancing training among residents.
The precision of USG estimation of fetal weight was a little higher (0.617) compared with clinical estimate by postgraduate (0.59) or consultant (0.58).
In the Bland–Altman plot, the points are scattered all over the place, above and below zero. It suggests that there is no consistent bias of clinical/USG estimates versus actual birth weight. As seen in the plot, for birth weight above 3.5 kg, there was an underestimation by a clinical estimate by both postgraduate and consultant. For birth weight less than 2.5 kg, there was overestimation by both clinical estimates by postgraduate and consultant.
As seen in Tables 4 and 5, in the birth weight less than 2.5 kg group, there is an overestimation by postgraduate (11.96), which is statistically significant (P = 0.001). However, the clinical estimate by the consultant has a lesser mean percentage error of 8.53, which is not statistically significant.
In birth weight groups 3.1 kg–3.5 kg and > 3.5 kg, we see there is an underestimation by clinical and USG methods. However, they are not statistically significant.
In a study by Shittu et al.[9] in 2007, where clinical and USG fetal weight were studied, it was seen that both methods were accurate in predicting birthweight in the normal birth weight range. However, for low birthweight (<2.5 kg), there was overestimation, but USG was statistically more accurate.
Similar results of USG estimation being more accurate for birth weight less than 2.5 kg were seen in other studies by Sherman et al.[10] and Titapant et al.[11]
Our observation implies that clinical estimation of fetal weight by Leopold’s maneuverer is as accurate as USG estimation by Hadlock’s formula, except in birth weight less than 2.5 kg. Therefore, when there is a clinical estimation of around 2.5 kg, it may be prudent to do an USG estimation of fetal weight to monitor fetal being.
Conclusion
Clinical estimation of fetal weight is definitely an important tool in estimating fetal weight. Though USG is useful in the low birth weight group, 73% of the participants had babies with normal birth weight (2.6–3.5 kg). Hence routine USG estimation of fetal weight for all term pregnancies is not warranted. Particularly clinical estimation by postgraduates showed overestimation in the low birth weight group compared with clinical estimation by the consultant. This implies the need for regular training and workshops targeted at improving clinical skills among postgraduates, especially in estimating fetal weights.
However, since there is a reasonable correlation between clinical estimates by postgraduate and junior consultants to the actual birth weight, we can conclude that training in an appropriate setting may be sufficient to optimize training in clinical estimation of fetal weight. This will be of much help to primary care providers and family physicians in estimating fetal weight. Although routine USG in the third trimester is discouraged, we should consider third-trimester USG when low birth weight is suspected.
Prudent use of USG will therefore avoid unnecessary interventions like induction of labor, instrumental delivery, and cesarean delivery. Good clinical estimation of fetal weight will reduce the cost of care, and minimize hospital visits without compromising the quality of antenatal care.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chauhan SP, Hendrix NW, Magann EF, Morrison JC, Jenney SP, Devoe LD. Limitations of clinical and sonographic estimates of birth weight: Experience with 1034 parturients. Obstet Gynecol. 1998;91:72–7. doi: 10.1016/s0029-7844(97)00590-5. [DOI] [PubMed] [Google Scholar]
- 2.Nzeh DA, Oyawoye O, Adetoro OO. Ultrasound estimation of birth weight in late pregnancy among African women. West Afr J Ultrasound. 2000;1:9–14. [Google Scholar]
- 3.Hanretty KP, Neilson JP, Fleming EE. Re-evaluation of clinical estimation of fetal weight: A comparison with ultrasound. J Obstet Gynaecol. 1990;10:199–201. [Google Scholar]
- 4.Wilcox AJ, Skjaerven R. Birth weight and perinatal mortality: The effect of gestational age. Am J Public Health. 1992;82:378–82. doi: 10.2105/ajph.82.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cecatti JG, Machado MR, Dos Santos FF, Marussi EF. [Curve of normal fetal weight values estimated by ultrasound according to gestational age. Cad Saude Publica Brazil. 2000;16:1083–90. doi: 10.1590/s0102-311x2000000400026. [DOI] [PubMed] [Google Scholar]
- 6.Ugwa EA, Gaya S, Ashimi A. Estimation of fetal weight before delivery in low-resource setting of North-west Nigeria: Can we rely on our clinical skills? J Matern Fetal Neonatal Med. 2015;28:949–53. doi: 10.3109/14767058.2014.938627. [DOI] [PubMed] [Google Scholar]
- 7.Noumi G, Collado-Khoury F, Bombard A, Julliard K, Weiner Z. Clinical and sonographic estimation of fetal weight performed during labor by residents. Am J Obstet Gynecol. 2005;192:1407–9. doi: 10.1016/j.ajog.2004.12.043. [DOI] [PubMed] [Google Scholar]
- 8.Predanic M, Cho A, Ingrid F, Pellettieri J. Ultrasonographic estimation of fetal weight: Acquiring accuracy in residency. J Ultrasound Med. 2002;21:495–500. doi: 10.7863/jum.2002.21.5.495. [DOI] [PubMed] [Google Scholar]
- 9.Shittu AS, Kuti O, Orji EO, Makinde NO, Ogunniy SO, Ayoola OO, et al. Clinical versus sonographic estimation of fetal weight in Southwest Nigeria. J Health Popul Nutr. 2007;25:14–23. [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman DJ, Arieli S, Tovbin J, Siegel G, Caspi E, Bukovsky I. A comparison of clinical and ultrasonic estimation of fetal weight. Obstet Gynecol. 1998;91:212–7. doi: 10.1016/s0029-7844(97)00654-6. [DOI] [PubMed] [Google Scholar]
- 11.Titapant V, Chawanpaiboon S, Mingmitpatanakul K. A comparison of clinical and ultrasound estimation of fetal weight. J Med Assoc Thai. 2001;84:1251–7. [PubMed] [Google Scholar]


