ABSTRACT
Background:
The rural–urban healthcare disparity in India was exacerbated during the COVID-19 pandemic, with the second wave hitting rural areas particularly hard due to weak infrastructure. A study in Chhattisgarh aims to explore the experiences of severely ill COVID-19 survivors and caregivers to inform patient-centric care delivery in primary settings.
Methods:
In this qualitative study, we conducted in-depth interviews with seven patients and seven caregivers during home visits or telephonically to understand lived experiences of receiving care for COVID-19 in an ICU in the public health system. Socioecological model was used to guide the qualitative inquiry.
Results:
COVID-19 patients faced stigma due to their diagnosis. The survivors felt lonely due to isolation, uncertainty about their illness, and fear of death. Poor mental health during ICU stay affected their physical health. Patients with caregivers felt supported despite visitor restrictions. Transparent communication with health providers reduced distress.
Conclusion:
The study in Chhattisgarh, India, highlights ICU survivors’ and caregivers’ experiences, revealing fear and loneliness among patients. Effective communication and caregiver presence improve outcomes, emphasizing holistic support. There’s an urgent need for palliative care integration, caregiver inclusion, and comprehensive post-discharge follow-up by primary-level practitioners in rural settings. Lack of state-level palliative care policy emphasizes the need for comprehensive initiatives to enhance healthcare outcomes.
Keywords: Caregivers, COVID-19, India, palliative care, socioecological model, survivors
Introduction
About two-thirds of Indians live in rural areas of the country yet urban areas have a stronger healthcare system compared to rural areas, in terms of infrastructure, availability of human resources, and diagnostic and critical care equipment.[1] The second wave of COVID-19 hit the rural areas of India harder than the first wave, and the weak public health infrastructure was insufficient to handle it.[2] By May 2021, nearly 50% of cases were reported from rural districts.[3] Thus, by mid-May, the experience of getting sick with COVID-19 and a need for critical care support became a reality. Although the impact of the second wave on tertiary healthcare services in rural areas has been studied, there is a dearth of evidence on the lived experiences of people who were either hospitalized in tertiary care hospitals or had close relatives who were hospitalized. Hence, our study aimed to understand the perceptions and lived experiences of severely ill COVID-19 survivors and caregivers from one such rural district of Chhattisgarh state of India. Understanding the lived experiences and needs of these patients and caregivers is essential for delivering holistic, patient-centered care within primary care settings.
Methods
Study design
We employed qualitative methods to explore the experiences of COVID-19 ICU survivors and their caregivers. The socioecological systems model informed the inquiry to understand how an individual’s knowledge and behavior interact with various environments.[4] This approach allowed us to gain insights into the complex health issues within the cultural and linguistic context, facilitating the proposal of solutions. The interview guide was in Hindi, pretested, and reviewed by a senior researcher. Ethical approval was obtained; dated 30.07.2021.
Study settings
The study took place in Surguja district, Chhattisgarh, India, with more than half the population being tribal. Agriculture is the primary income source for 90% of residents, and 85% live in rural areas.[5] Healthcare is provided through a district hospital, 6 community health centers, and 28 primary health centers. Additionally, there is a government medical college in Ambikapur, serving 4.5 million people in six districts.[6] The study was conducted on survivors and caregivers of patients who received care at a teaching hospital in the Surguja division amid the second wave of COVID-19. Due to staff shortages, caregivers were permitted to visit patients in the hospital, although not all patients had caregivers present.
Sampling and inclusion criteria
We purposively selected participants for in-depth interviews from a list of 63 ICU patients admitted between May 17, 2021, and July 17, 2021. Criteria for inclusion were adult patients who received intensive care for COVID-19 and were discharged home or adult caregivers who had a family member who received intensive care for the same and had lost them at least two weeks before the interview. Out of 20 eligible participants, 14 consented and were included in the study.
Data collection
In-depth interviews were conducted between September 2021 and January 2022. Written informed consent was obtained from participants. Interviews were conducted in Hindi and lasted 24 to 50 minutes. Recordings were transcribed and translated into English. No follow-up interviews were conducted. Study findings adhere to Consolidated criteria for reporting qualitative guidelines for qualitative research.[7]
Data analysis
Data was analyzed using applied thematic analysis. Interview transcripts were independently reviewed by two authors. Themes were identified in advance, and coding was conducted accordingly. Triangulation of themes and codes was performed using field notes when necessary.
Results
A total of 14 individuals participated in the study. More than one-third of the patients and family members were from neighboring districts and the rest were from the Surguja district. Half of the participants were women. The age range of the participants was 18 to 55 years. The demographic and clinical information of the participants is shown in Table 1.
Table 1.
Demographic and clinical information of the participants
| Participant type | Age | Sex | Relationship with the patient | Age of the patient | Clinical condition | ICU LOS (in days) | Patient outcome | |
|---|---|---|---|---|---|---|---|---|
| P1 | Survivor | 25 | Male | Self | - | Severe COVID with pneumothorax, on oxygen support for 5 days | 13 | Discharged |
| P2 | Caregiver | 19 | Female | Daughter | 46 | Discharged on request for home care, needed hemodialysis, severe COVID, advanced carcinoma cervix with renal insufficiency | 11 | Discharged for home care, died 2 days later at home |
| P3 | Survivor | 54 | Female | Self | - | Severe COVID with rheumatoid arthritis | 6 | Discharged for home care |
| P4 | Caregiver | 17 | Male | Son | 48 | Discharged (On request/against medical advice), COVID with bloodstream infection and suspected chronic kidney disease (CKD) | 17 | Discharged, and needed hemodialysis |
| P5 | Caregiver | 42 | Female | Wife | 43 | Died, Severe COVID with pre-existing restrictive lung disease with hypoxia with acute respiratory distress syndrome (ARDS), needed noninvasive ventilation (NIV) for 4 days with oxygen support for 15 days | 15 | Died. |
| P6 | Survivor | 44 | Male | Self | - | Discharged, severe COVID with hypoxia, needed NIV support for 10 days, oxygen support for 20 days | 20 | Discharged |
| P7 | Caregiver | 18 | Female | Daughter | 21 | Died, of diabetic ketoacidosis with COVID with hypoxia and needed NIV for 1 day and oxygen support for 14 days | 14 | Died |
| P8 | Survivor | 40 | Male | Self | - | Severe COVID with pneumonia with ARDS, on NIV support for 28 days and oxygen support for 12 days | 40 | Discharged |
| P9 | Survivor | 28 | Male | Self | - | Severe COVID with hypoxia, needed NIV support for 5 days and oxygen support for 25 days | 21 | Discharged |
| P10 | Survivor | 55 | Female | Self | - | Severe COVID with hypoxia, needed NIV for 5 days and oxygen support for 14 days | 18 | Discharged |
| P11 | Caregiver | 36 | Male | Grandson | 77 | Severe COVID with hypoxia, needed NIV for 3 days and oxygen therapy for 7 days | 3 | Died |
| P12 | Survivor | 46 | Male | Self | - | Severe COVID with ARDS, on NIV for 7 days and oxygen therapy for 13 days | 20 | Discharged |
| P13 | Caregiver | 25 | Male | Son | 67 | Pre-existing CKD with COVID, on hemodialysis, developed ARDS, with orbital cellulitis with multiple cranial nerve palsies suspected to be due to mucormycosis, on NIV for 10 days and oxygen therapy for 5 days | 9 | Died |
| P14 | Caregiver | 20 | Male | Son | 2 | Severe COVID with hypoxia needed NIV for 10 days and oxygen therapy for 5 days | 15 | Died |
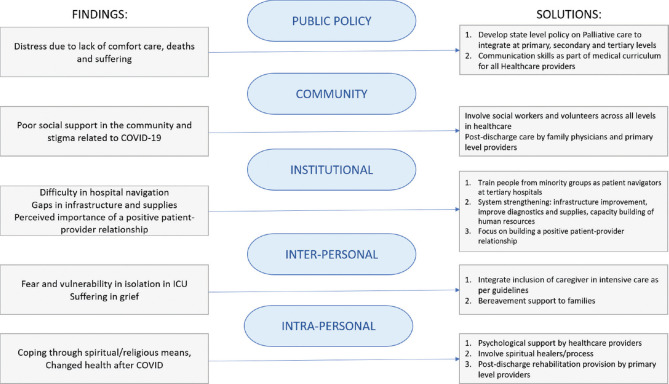
We interpreted the findings of the study using the socioecological model of health and illness. We identified themes under each level of this model, namely intrapersonal (or individual), interpersonal, institutional, and community. The subthemes under each level are described in detail below. The overarching conclusions of our study are visually represented in Figure 1.
Figure 1.
Applying the socio-ecological model of health and illness to the experiences and perceptions of COVID19 ICU survivors and caregiver experiences
Intrapersonal
The intrapersonal level includes awareness, perceptions, attitudes, beliefs, and knowledge of the patients and caregivers.
Fear of severe illness and being admitted to an intensive care
Most participants had no past ICU experience, either as patients or as caregivers. A majority of the participants said that they were fearful of the idea of being admitted to an ICU:
I was a bit scared when I was in the ICU. But then I had no other option, where could I go? (P8, survivor, 40 years old, male)
However, there was also a perception among some participants that in an ICU, one receives the highest quality of care. One of the COVID survivors recollected how the ICU helped him survive the severe disease:
And there were good doctors in the ICU, I received oxygen therapy and medicines there. I was confident that I will recover. I am now healthy due to everyone’s blessing, you and all other doctors. (P8, survivor, 40 years old, male)
Isolating experience of being in the hospital
Most participants shared that they felt that they were left to themselves in the ICU. They were worried if the providers could not attend to them, it might lead to unfavorable consequences as there are no family members with them:
I spoke to people who survived and relatives of people who died; I too shared my experiences with them. I feel the biggest reason for death among COVID patients is that they are left alone in the ICU, which should not happen. For example, if someone’s oxygen mask gets off, and they are unable to put it back, and doctors did not pay attention, and hence, due to lack of oxygen, that person passed away. (P8, survivor, 40 years old, male)
However, some participants did not feel the same way. They felt that they received emotional support from the ICU staff, and did not experience a sense of loneliness like others:
It felt like a family (in the ICU). There was more belongingness like that of a family. Doctors would suggest what to eat for breakfast. They would give advice, respond quickly, give timely medicines and injections. (P6, 44 years old, survivor, female)
The experience of witnessing the deaths and distress of other patients
Participants shared that they experienced distress when they had to witness the death or distress of other patients in the ICU. The sight of death in itself was scary and all of them said that they feared death too.
One participant shared the harrowing experience of lying between two dead bodies:
There was dead body on your one side, there’s another dead body on your other side.my experience is that… that we will never see this again, we had never witnessed such thing in our lives (before), that I saw in my life. (P10, 55 years old, survivor, female)
Such incidents often lead to increasing anxiety among the patients and their family members. One of the participants narrated how the healthcare providers intervened to address the anxiety related to bad outcomes in the ICU.
Coping with illness-induced stress
Many participants shared that they had to develop a coping mechanism to deal with fear and stress while in the ICU. Some of them shared that having an optimistic outlook helped them to cope:
..but I did not lose hope. I was always hopeful that I would not get ill and I would get better. (P8, 40 years old, survivor, male)
Changed health after COVID-19
For those who survived the COVID-19 infection after the ICU care, the physical impairments restricted them from going back to their routine life before this illness:
I had never thought I would get so sick in my life. Never! Never! I was so strong in my home. I was born in a poor household in a village and I am the elder most daughter in my family. helping in the work at home, helping my mother and father, in addition to going school.,,(used to) go into the forest…cook food on wood…did everything and did everything. And I was very strong too but now I don’t feel strong enough. (P10, 55 years old, survivor, female)
Interpersonal
Under the interpersonal level of the socioecological model, we evaluated the interactions of the participants with their immediate surroundings and family members.
Caring for a family member during the pandemic
One of the participants shared the importance of caring for her mother
She (patient, the mother) should not feel that she (patient) is unwell since so long, so there is nobody to bathe her, nobody to feed her, nobody to comb her hair, so, I (daughter) used to do all that…it made both of us feel good that I was there to take care of her, and she did not feel lonely (P2, 19 years old, caregiver, female)
One of the participants shared that they expected to shift focus to the comfort of the patients near the end of life:
We asked them (the healthcare provider) to at least give him some water to drink, he had not had water since last 2 days and he was having difficulty in breathing. Toward the end, even we got to know that he may not live. That is why we asked to allow him to drink some water. (P11, 36 years old, caregiver, male)
Deriving the meaning of loss, and experiencing grief
Participants who had lost their family members had to come to terms with the reality of death. They dealt with grief in different ways. They shared that their belief in a divine power helped them in making sense of the loss and grief they were experiencing:
I knew that mother, like earlier also, sir (ICU doctor) had told us after dialysis she is not improving…whatever we do, whatever we do, it was all in God’s hands. (P2, 19 years old, caregiver, female)
A caregiver (patient’s brother) shared that his parents were left deeply traumatized after they lost their elder son to COVID-19:
There is some problem (in sleep). Both my father and mother they get up in the middle of the night. Sometimes my mother gets scared suddenly. She suddenly starts crying while talking. (P14, 20 years old, caregiver, male)
Institutional
The rules, regulations, functioning and attitude toward patients of the healthcare institutions constitute the institutional level in the socioecological model.
Challenges of navigating a tertiary care government hospital during the pandemic
One of the caregivers said that they had difficulty in navigating their way around in the large government hospital:
We were having trouble finding it (isolation ward) there (in the medical college and hospital), we were told this room and that room, we were searching for two to three hours, everywhere, so it was evening by the time I got admitted. (P1, 25 years old, survivor, male)
Patient-provider relationship
A majority of the participants felt that the health providers were successful in maintaining transparency regarding the health condition of the patient, and communicated with both patients and caregivers in an empathetic manner:
They (doctors and nurses) all used to tell me whatever you feel like you can share, you are in the COVID ICU. ‘If you have anything to ask, please do,’(they) used to say like that. All were casual, used to joke, smile, greet like that, so I used to feel good, for all these things. (P1, 25 years old, survivor, male)
Some survivors said that it is important that health providers communicate with the patient. He felt that it had a bearing on the psychological status of the patient:
Talking is also part of the whole treatment. They used to come, talk, and joke with us. It was like a medicine…that makes us forget our family. (P12, 46 years old, survivor, male)
Perceived health system inadequacies
While describing their experiences, many participants shared their perceptions about the health system, both public and private. There were numerous reasons for this lack of preference for public hospitals:
I think infrastructure, testing facilities, cleanliness and hygiene and the staff too need to improve. (P13, caregiver, 25 years old, male)
Positive experiences improve trust in the institution
Participants shared that after a lived experience and also if one recovers from the illness, there is reduced fear and increased faith in the facility:
We thought that results were good here (district hospital) so let us not go anywhere else. we thought in our mind that treatment was good here…there was satisfaction (P14, caregiver, 20 years old, male)
Community
Finally, factors at the community level in the socioecological model shaped participants’ experiences. These included interaction of patients and caregivers within their locality or with their relatives.
COVID-19 stigma and discrimination
A majority of participants said that both patients and their caregivers experienced COVID-related stigma and discrimination:
When I was in ICU nobody used to go to my home. We were facing problems in getting ration and vegetables. My parents, children, everyone was at home. (P8, 40 years old, survivor, male)
Lack of social support
Participants shared that they did not receive adequate social support. This experience led to feelings of anger and resentment toward family members, friends, etc.:
When I took her to Raipur, nobody in our family supported us. It was only my brother and me. There was no one. It felt as if we did not have any family at that time. (P2, 19 years old, caregiver, female)
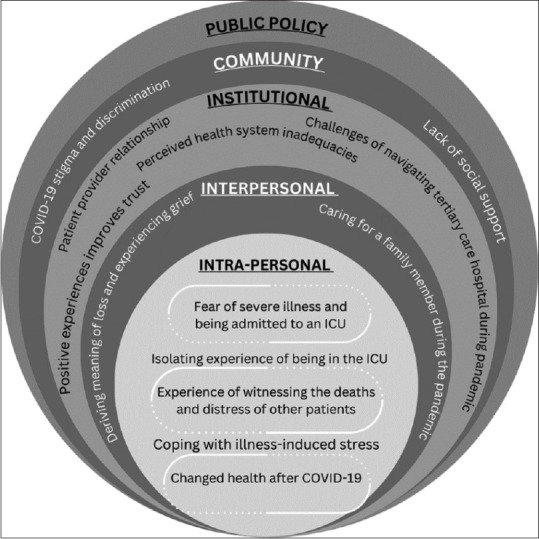
We adopted the socioecological model as a conceptual framework to interpret the findings of the study. We employed this model iteratively to devise novel solutions across different tiers [Figure 2].
Figure 2.
Use of the socioeconomic model to understand and improve patients’ and families’ experiences at a district hospital intensive care
Discussion
To summarize, participants associated hospital referral with illness severity and feared admission. Many survivors experienced ICU loneliness due to isolation, illness uncertainty, and fear of death, affecting their mental and physical health. Caregiver presence provided support and optimism and good communication with health providers reduced distress. Witnessing deaths was profound for survivors. Caregivers faced intense grief and mental trauma. Some felt their loved ones were denied compassionate end-of-life care, while others found solace in respectful treatment.
Survivors in our study reported stress and anxiety, aligning with previous research on COVID-19 ICU experiences.[8,9,10] They associated ICU admission with illness severity and anticipated a poor prognosis, consistent with findings from other studies.[10] Research suggests that patients admitted with family members cope better than those without, echoing our findings.[10] Clinical guidelines from 2005 recommend various measures to enhance patient and family experiences in the ICU, including shared decision-making, consistent communication, spiritual support, open visitation policies, and post-death family support.[11]
Survivors and caregivers in our study reported deep psychological implications after their experience in the hospital, consistent with a national-level study in India where 9.3% of ICU survivors experienced mental health issues within two months of discharge.[12] Some survivors faced impairments and reduced functionality post-discharge, which is especially impactful in rural areas where limited participation affects agricultural and household contributions.[13] Except for outpatient care, there were no comprehensive follow-ups for survivors or bereaved families, highlighting unmet mental health and rehabilitation needs in rural areas.[14]
In this study, severely ill patients and caregivers developed coping mechanisms for uncertainty and impending death. Optimism and spirituality provided mental and emotional strength. Previous literature demonstrates spiritual care in the ICU improves patient and family well-being, enhancing quality of life, reducing distress, and increasing satisfaction with medical care.[15] Social workers facilitated bereavement processes, aiding caregivers in expressing themselves.[8]
For severely ill patients with poor prognoses, caregivers found solace in the dignified treatment and care provided to their family members during their final days. However, some expressed distress over the perceived lack of compassion and basic care from healthcare providers. Studies in affluent nations underscored the significance of palliative care in COVID-19 ICU settings, emphasizing provider-patient relationships, communication, spiritual and psychosocial support, and bereavement care.[16,17,18] Validated tools like the Palliative Performance Scale were deemed beneficial for end-of-life care in COVID-19 patients, aiding in prognosis communication.[19,20,21] Many survivors stressed transparent, empathetic communication’s importance alongside medical care quality. Our findings advocate for enhanced palliative care training for doctors and nurses, focusing on communication and psychosocial support in end-of-life care and addressing barriers to good patient-provider communication.[22]
Patients in government hospitals face challenges navigating within the hospital without support, impacting patient outcomes. During the pandemic, fear of infection intensified this struggle. In Chhattisgarh, block and district-level hospitals have local community members as help-desk facilitators who usually aid navigation. There is compelling evidence to suggest that the inclusion of patient navigators and social workers across all levels of healthcare can improve outcomes for patients, families, and communities.[23,24]
Past experiences with hospital infrastructure and services lead to skepticism. Strengthening diagnostic and critical care services in rural areas like Surguja is urgent.[25] Positive experiences in the hospital with effective patient-provider relationships boost confidence in the public health system. The socioecological model suggests that these cumulative individual-level experiences will in turn influence experience and perceptions of the community.
Overall, the findings highlight the perceived necessity of integrating palliative care in intensive care, emphasizing empathetic communication, psychological and social support, alleviation of spiritual distress, comfort care provision, inclusion of families in patient care and bereavement support. The study underscores the imperative to bolster palliative care services in public health facilities, as exemplified in Kerala, India.[26]
Primary care and family medicine practitioners play a crucial role in supporting the patients and their families post-ICU discharge to ensure continuity of care at village and subdistrict levels.[27] Our findings might inform their practice and make it more people-centric.
The study has certain limitations. Firstly, logistical constraints prevented us from providing interview transcripts to participants for verification, and their feedback on the findings could not be sought. These findings may not be broadly applicable to other regions of Chhattisgarh or India. Nonetheless, this study pioneers examining ICU survivors’ and caregivers’ experiences and perceptions within a rural setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Anand S, Fav V. THE HEALTH WORKFORCE IN INDIA Human Resources for Health Observer Series. No. 16. Geneva: 2016. [[Last accessed on 2024 Jun 23]]. World Health Organization. Available from https://iris.who.int/bitstream/handle/10665/250369/9789241510523-eng.pdf?sequence=1 . [Google Scholar]
- 2.Panneer S, Bhat LD, Rice L, Kantamaneni K. The second wave of COVID-19 and beyond. [[Last acessed on 2023 Oct 31]];Economic and Political Weekly. 2022 57 Available from: https://www.epw.in/journal/2022/2/commentary/second-wave-covid-19-and-beyond.html . [Google Scholar]
- 3.Pandey B, Gu J, Ramaswami A. Characterizing COVID-19 waves in urban and rural districts of India. NPJ Urban Sustain. 2022;2:26. doi: 10.1038/s42949-022-00071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salihu HM, Wilson RE, King LM, Marty PJ, Whiteman VE. Socio-ecological model as a framework for overcoming barriers and challenges in randomized control trials in minority and underserved communities. Int J MCH AIDS. 2015;3:85–95. [PMC free article] [PubMed] [Google Scholar]
- 5.Registrar General and Census Commissioner of India. District Census Handbook, Surguja. 2011 Census of India. Series23, Part XIIA. 2016. [[Last accessed on 2023 Feb 14]]. Available from: https://censusindia.gov.in/nada/index.php/catalog/359 .
- 6.Ministry of Health and Family Welfare, Government of India. Rural Health Statistics 2020-21. 2021. [[Last accessed on 2023 Nov 04]]. Available from: https://main.mohfw.gov.in/sites/default/files/rhs20-21_1.pdf .
- 7.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 8.Connolly M, Bell M, Lawler F, Timmins F, Ryder M. Hospital-based palliative and end-of-life care in the covid-19 pandemic: A scoping review. Am J Hosp Palliat Med. 2022;39:1105–20. doi: 10.1177/10499091211057049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gunjiganvi M, Rai S, Awale RB, Mishra P, Gurjar M, Gupta D, et al. Depression and anxiety among COVID-19 Indian intensive care unit survivors: A prospective observational study. Indian J Crit Care Med. 2022;26:1267–74. doi: 10.5005/jp-journals-10071-24370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahoo S, Mehra A, Suri V, Malhotra P, Yaddanapudi LN, Puri GD, et al. Lived experiences of COVID-19 intensive care unit survivors. Indian J Psychol Med. 2020;42:387–90. doi: 10.1177/0253717620933414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007;35:605–22. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 12.Kumar G, Bhalla A, Mukherjee A, Turuk A, Talukdar A, Mukherjee S, et al. Post COVID sequelae among COVID-19 survivors: Insights from the Indian National Clinical Registry for COVID-19. BMJ Glob Health. 2023;8:e012245. doi: 10.1136/bmjgh-2023-012245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Towards a Common Language for Functioning, Disability and Health ICF Towards a Common Language for Functioning, Disability and Health: ICF The International Classification of Functioning, Disability and Health. Geneva: 2002. [[Last accessed 2024 Jun 23]]. Available from: https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf . [Google Scholar]
- 14.Uppal H, Rai S. Rehabilitation during COVID-19 pandemic: An Indian perspective. Disaster Med Public Health Prep. 2022;16:409–12. doi: 10.1017/dmp.2020.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willemse S, Smeets W, van Leeuwen E, Nielen-Rosier T, Janssen L, Foudraine N. Spiritual care in the intensive care unit: An integrative literature research. J Crit Care. 2020;57:55–78. doi: 10.1016/j.jcrc.2020.01.026. [DOI] [PubMed] [Google Scholar]
- 16.Schoenherr LA, Cook A, Peck S, Humphreys J, Goto Y, Saks NT, et al. Proactive identification of palliative care needs among patients with COVID-19 in the ICU. J Pain Symptom Manage. 2020;60:e17–21. doi: 10.1016/j.jpainsymman.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schockett E, Ishola M, Wahrenbrock T, Croskey A, Cain S, Benjenk I, et al. The impact of integrating palliative medicine into COVID-19 critical care. J Pain Symptom Manage. 2021;62:153–8.e1. doi: 10.1016/j.jpainsymman.2020.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fausto J, Hirano L, Lam D, Mehta A, Mills B, Owens D, et al. Creating a palliative care inpatient response plan for COVID-19—The UW medicine experience. J Pain Symptom Manage. 2020;60:e21–6. doi: 10.1016/j.jpainsymman.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Damani A, Ghoshal A, Rao K, Singhai P, Rayala S, Rao S, et al. Palliative care in coronavirus disease 2019 pandemic: Position statement of the Indian Association of Palliative Care. Indian J Palliat Care. 2020;26((Suppl 1)):S3–7. doi: 10.4103/IJPC.IJPC_207_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krishna LKR, Neo HY, Chia EWY, Tay KT, Chan N, Neo PSH, et al. The role of palliative medicine in ICU bed allocation in COVID-19: A joint position statement of the Singapore Hospice Council and the Chapter of Palliative Medicine Physicians. Asian Bioeth Rev. 2020;12:205–11. doi: 10.1007/s41649-020-00128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fiorentino M, Pentakota SR, Mosenthal AC, Glass NE. The Palliative Performance Scale predicts mortality in hospitalized patients with COVID-19. Palliat Med. 2020;34:1228–34. doi: 10.1177/0269216320940566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curtis JR, Patrick DL, Caldwell ES, Collier AC. Why don't patients and physicians talk about end-of-life care? Barriers to communication for patients with acquired immunodeficiency syndrome and their primary care clinicians. Arch Intern Med. 2000;160:1690–6. doi: 10.1001/archinte.160.11.1690. [DOI] [PubMed] [Google Scholar]
- 23.Saxe Zerden L de, Lombardi BM, Jones A. Social workers in integrated health care: Improving care throughout the life course. Soc Work Health Care. 2019;58:142–9. doi: 10.1080/00981389.2019.1553934. [DOI] [PubMed] [Google Scholar]
- 24.National Rural Health Mission Chhatisgarh, State Health Resource Centre Chhattisgarh. Mitanin support and career progression in Chhattisgarh. 2013. [[Last accessed on 2024 Jun 23]]. Available from: https://nhinp.org/wp-content/uploads/2021/09/2%20Mitanin_%20Career%20progression%20-%20Chhattisgarh.pptx .
- 25.Malik C, Lal R, Chandrakar K, Singh L, Jadhao S, Kalkonde Y, et al. Clinical features, management, and mortality because of COVID-19 in an intensive care unit in Surguja, a tribal district in Central India: A single-centre descriptive study. J Family Med Prim Care. 2022;11:6848. doi: 10.4103/jfmpc.jfmpc_185_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bag S, Mohanty S, Deep N, Salins N, Bag S. Palliative and end of life care in India-current scenario and the way forward. J Assoc Physicians India. 2020;68:61–5. [PubMed] [Google Scholar]
- 27.Puthucheary ZA. Primary care – The unrecognized member of the intensive care team. J Intensive Care Soc. 2015;16:361. doi: 10.1177/1751143715580584. [DOI] [PMC free article] [PubMed] [Google Scholar]