ABSTRACT
Background:
Breastfeeding is an important determinant of child survival. Breastfeeding practices vary throughout the nation.
Objectives:
To assess the breastfeeding practices and the knowledge of recently delivered mothers regarding breastfeeding practices.
Materials and Methods:
This community-based cross-sectional study was conducted among women who had delivered in the Moradabad region of Uttar Pradesh last year. A total of 423 households was divided between the six community health blocks according to probability sampling. A predesigned and pretested structured questionnaire was utilized to collect data. Knowledge scores were calculated.
Results:
The majority of respondents had the correct knowledge about breastfeeding immediately after birth (76.6%), prelacteal foods should not be provided (82.2%), colostrum feeding (89.0%), adequate frequency of breastfeeding (99.1%), and exclusively breastfeeding (78.7%). The knowledge scores about breastfeeding were good (64.9%) for mothers. A higher proportion of respondents practiced breastfeeding only, or cup fed with breast milk only their babies for the first 2 days of life (62.3%), and the majority fed their baby with adequate frequency. Only (55.7%) put their baby to breast within an hour after birth. Colostrum was not squeezed and thrown by nearly (59.7%) of mothers. The breastfeeding practices scores were good among one-third of mothers. Age of mother, type of family, mother’s education, socioeconomic status, and type of delivery were significant determinants of good breastfeeding practices (<0.05).
Conclusions:
The knowledge and practices of infant feeding can be strengthened by further engaging and counseling of mothers, family, and community members by health workers.
Keywords: Breastfeeding, knowledge, practices
Introduction
The first food for neonates, which is gifted by mother is breast milk. Breast milk is full of energy and nutrition, fulfilling the requirement of neonates for the first few months of age. Effective breastfeeding practices not only help in reducing newborn and child mortality rates but also reduce morbidity caused by diarrheal diseases, upper and lower respiratory tract infections, necrotizing enterocolitis, and sudden infant death syndrome.[1]
Breastfeeding is one of the most important determinants of child survival, birth spacing, and prevention of childhood infections.[2,3] World Health Organization (WHO) recommends early initiation of breastfeeding (EIBF) within the first hour and exclusive breastfeeding (EBF) for the first 6 months with continued breastfeeding up to 2 years or beyond, with the addition of nutritionally and age-appropriate complementary foods.[4,5] Globally, 42% of infants undergo EIBF, and 41% of infants have EBF for the first 6 months.[6] The National Family Health Survey 4 (NFHS 4) of India reported that about (42%) of the children who born in the last 5 years had EIBF, 54.9% of the children up to six months of age had EBF, and 42.7% of the children between 6 and 9 months of age received solid or semi-solid food along with breast milk.[7] Despite these recommendations, it is observed that breastfeeding practices are varied throughout the nation. However, according to WHO, exclusive breastfeeding practice rates till 6 months remain low in both low-income and high-income countries.[8] Therefore, it is essential to know the reasons to avoid optimal breastfeeding practices. Many mothers who are physically fit are willing to breastfeed their children; however, they face substantial problems and have certain barriers that prohibit them from doing so. Breastfeeding practices among the rural communities are mostly influenced by social, cultural, and economic factors.[2] Problems associated with low practice of EBF may also be related to religion, workplace, health system, family system, or even community norms.[9] Effective interventions in the health care systems needed to be addressed to explore the knowledge of mothers about breastfeeding and their practices including factors that influence exclusive breastfeeding and barriers to improve the practices and outcome with the help of policymakers for implementation of interventional programs.
Therefore, the present study was carried out to assess the practices of breastfeeding and to assess the knowledge of mothers who had delivered in the last year in the Moradabad region of Uttar Pradesh.
Materials and Methods
Ethical approval taken from Institutional Ethical Committee. Written informed consent taken from each study participant.
Study design
A community-based cross-sectional study was conducted among recently delivered women (whose baby aged 12 months or less) to accomplish the objectives of the study. Additionally, group discussions were also conducted with mothers/caregivers of infants.
Study setting
The project was implemented in all six community health blocks of Jyotiba Phule Nagar district in the Moradabad region of Uttar Pradesh. The district accounted for 0.90 percent of the state’s population during the 2011 census. A total of 6 blocks were chosen, and about 61 villages were covered by the project.
Study period
Twelve months duration.
Study tool
A structured questionnaire was used for data collection, which was predesigned and pretested. Questionnaire was designed to determine the knowledge and practices of postnatal mothers or caregivers assigned to newborn care. The tool was divided into two sections.
Section A: Sociodemographic information
Section B: Knowledge and Practice on breastfeeding.
The questionnaire consisted of 47 items regarding knowledge and practices of mothers/caregivers about newborn care. Each correct response was given one mark, so the maximum possible score for knowledge was 19 and 13 for practice. For each group of knowledge and practices, the total score was calculated separately and categorized into three grades: Good, Fair, and Poor.
Study population
The primary study population comprised women of reproductive age (15–49 years) who had delivered a live baby within the past 12 weeks before the conduct of this study (RDW). The 12-week limit is set with the purpose of mitigating recall bias by the mother.
Sample size estimation
The sample size for the study among the mothers of children aged 0-12 weeks was calculated based on the standard formula for one-point sample estimation:
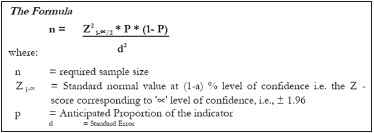
To ensure coverage of the minimum required sample size for estimating various outcome indicators of the project, the value of P (neonatal morbidity) is taken as 50.3%.[10] With the above assumption the required sample size at 95% level of confidence with 5% of permissible error in the estimates, is worked out as:
n = 1.962 * 0.503 * 0.497/0.052 = 384
With consideration of the 10% non-response rate, the sample size was 423.
The total sample of 423 households was divided between the six blocks according to probability proportional to size. Thus, in each block, the number of villages was selected for the survey with an assumption of 7 RDW per village to complete the required sample size.
Sampling procedures
Villages were selected by way of simple random sampling from each block, half among the nearby villages and the rest among the distant villages from the community health center, and high priority was given to villages where Accredited Social Health Activist and Auxiliary Nurse Midwife are appointed.
Procedure for selection of households
In each village, a systematic random sampling methodology was used to select the required number of respondents. The field supervisor moved to the center of the village and randomly selected the first household. In the contacted households, it was verified whether the household had a child who was aged 0-12 weeks of age. If the child and the mother are present there, then the household was selected, and the structured questionnaire was canvassed. If not, the investigator moved to the immediate next household for a similar inquiry.
Selection of respondents
In each selected household, the mother of the chosen child was contacted for the interview. If more than one child was present, the mother of the youngest child was contacted for the interview. The training was given for data collectors, and the overall data collection activities were supervised by the principal investigator.
Ethical consideration
Ethical approval was taken from the Institutional Ethical Committee. Written informed consent was taken from each study participant.
Statistical analysis
The data were entered in Excel, critically analyzed, and tabulated using SPSS-20 version software. Appropriate statistical tests of significance (logistic regression) were applied to test and validate the findings of the study. Adjusted and unadjusted odds ratios (OR) and their 95% confidence intervals (CIs) were used as indicators of the strength of the association. A P-value of 0.05 or less was used as a cut-off level for statistical significance.
Results
The majority of respondents had the correct knowledge about breastfeeding the baby immediately after birth (76.6%), no prelacteal foods to be provided (82.2%), colostrum to be fed to baby (89.0%), baby to be breastfed 8–12 times in 24 hours (99.1%) and baby to be exclusively breastfed for first 6 months (78.7%). The correct knowledge about early initiation of breastfeeding was highest in the Gajrola block (91.2%), and exclusive breastfeeding was highest in the Gangeshwari block (80.9%) [Table 1].
Table 1.
Distribution of respondents having correct knowledge about breastfeeding
| Variable | Block of Respondents | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Dhanaura | Amroha | Gajrola | Gangeshwari | Hasanpur | Joya | ||
| Breastfeeding the baby immediately after birth | 68.8% | 80.7% | 91.2% | 84.1% | 69.4% | 69.4% | 76.6% |
| No prelacteal foods to be provided | 85.9% | 81.9% | 87.7% | 71.4% | 80.6% | 84.7% | 82.2% |
| Colostrum to be fed to baby | 82.8% | 94.0% | 84.2% | 96.8% | 96.8% | 81.6% | 89.0% |
| Baby to be breastfed 8-12 times in 24 h | 100% | 100% | 100% | 93.7% | 100% | 100% | 99.1% |
| Baby to be exclusively breastfed for first 6 months | 76.6% | 78.3% | 80.7% | 80.9% | 80.6% | 76.5% | 78.7% |
The overall breastfeeding knowledge scores among the respondents residing in different blocks were found to be good (64.9%) in a higher proportion of respondents, followed by fair (23.2%) and poor (11.9%). The percentage of good scores was highest in Gajrola block (89.5) followed by Amroha (69.1%) block [Table 2].
Table 2.
Knowledge about Breastfeeding among respondents
| Breastfeeding Scores | Block of Respondents | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Dhanaura | Amroha | Gajrola | Gangeshwari | Hasanpur | Joya | ||
| Good (4-5) | 40 (63.5) | 58 (69.1) | 51 (89.5) | 30 (47.6) | 38 (61.3) | 60 (61.2) | 277 (64.9) |
| Fair (3) | 12 (19.1) | 16 (19.0) | 5 (8.8) | 24 (38.1) | 17 (27.4) | 26 (26.5) | 99 (23.2) |
| Poor (≤2) | 11 (17.5) | 10 (11.9) | 1 (1.8) | 9 (14.3) | 7 (11.3) | 12 (12.2) | 51 (11.9) |
| Total | 63 (100) | 84 (100) | 57 (100) | 63 (100) | 62 (100) | 98 (100) | 427 (100) |
A higher proportion of respondents practiced breastfeeding only or cup-fed with breast milk only for their babies for the first 2 days of life (62.3%). The majority (77.3%) fed their baby an adequate number of times during the day/night. Only 55.7% put their baby to breast within one hour after birth. First milk, which is called as colostrum, was not squeezed out and thrown away by nearly 59.7% of mothers. After delivery, no fluid/feeds were given to drink before breastfeeding for the first time by nearly half of the mothers. The highest percentage of correct practice of not discarding colostrum was observed in Hasanpur block (67.7%), and the highest percentage of correct practice of no prelacteal feeding was observed in Gajrola block (63.2%) [Table 3].
Table 3.
Correct Breastfeeding practices among respondents (immediately after recent delivery)
| Variable | Block of Respondents | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Amroha | Dhanaura | Gajrola | Gangeshwari | Hasanpur | Joya | ||
| The baby was breastfed only or, cup fed with breast milk only for the first 2 days of life | 63.9% | 59.4% | 64.9% | 63.5% | 62.9% | 60.2% | 62.3% |
| The baby was fed for an adequate number of times during day/night | 77.1% | 75.0% | 78.9% | 82.5% | 77.4% | 74.5% | 77.3% |
| The baby was put to the breast within an hour after birth | 59.0% | 48.4% | 63.2% | 65.1% | 53.2% | 48.9% | 55.7% |
| First milk (colostrum) was not squeezed out and thrown away | 65.1% | 60.9% | 49.1% | 65.1% | 67.7% | 52.1% | 59.7% |
| After delivery, no fluid/feeds were given to drink before breastfeeding for the first time | 50.6% | 51.6% | 63.2% | 31.7% | 45.2% | 58.2% | 50.6% |
The overall breastfeeding practices scores among a higher proportion of respondents were found to be poor (36.3%), followed by good (35.8%) and fair (27.9%). The percentage of good scores was highest in Gajrola block (49.1), followed by Gangeshwari (38.1%) and Hasanpur blocks (37.1%) [Table 4].
Table 4.
Distribution of Breastfeeding Practices scores
| Breastfeeding Practices Scores | Block of Respondents | Total | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Amroha | Dhanaura | Gajrola | Gangeshwari | Hasanpur | Joya | ||
| Good (4-5) | 27 (32.1) | 17 (26.9) | 28 (49.1) | 24 (38.1) | 23 (37.1) | 34 (34.7) | 153 (35.8) |
| Fair (3) | 25 (29.8) | 27 (42.9) | 9 (15.8) | 17 (27.0) | 14 (22.6) | 27 (27.6) | 119 (27.9) |
| Poor (≤2) | 32 (38.1) | 19 (30.2) | 20 (35.1) | 22 (34.9) | 25 (40.3) | 37 (37.8) | 155 (36.3) |
| Total | 83 (100) | 63 (100) | 57 (100) | 63 (100) | 62 (100) | 98 (100) | 427 (100) |
Age of the mothers and type of family were found to be the significant determinants of having Good Knowledge regarding breastfeeding among the study population (<0.05) [Table 5].
Table 5.
Determinants of Good Knowledge about breastfeeding among respondents
| Variable | Breastfeeding (Have Good Knowledge n=271) | |
|---|---|---|
|
| ||
| Unadjusted OR (95%CI) | Adjusted OR (95% CI) | |
| Age of mother | ||
| 18-25 years | 1 | 1 |
| 26-30 years | 0.7 (0.5-1.1) | 0.6 (0.3-0.9) |
| 31-35 years | 1.3 (0.5-3.3) | 1.1 (0.4-3.1) |
| >35 years | 0.5 (0.1-2.1) | 0.3 (0.07-1.4) |
| P | 0.033 | |
| Child’s mother’s religion | ||
| HinduRef | 1 | 1 |
| Muslim/Sikh/Other | 1.4 (0.9-2.1) | 1.5 (1.0-2.4) |
| P | 0.089 | |
| Child’s mother’s education | ||
| ≤10thRef | 1 | 1 |
| >10th | 0.7 (0.3-1.5) | 0.8 (0.3-1.8) |
| P | 0.057 | |
| Child’s mother’s occupation | ||
| HousewifeRef | 1 | 1 |
| Working | 3.5 (0.4-29.4) | 3.1 (0.3-27.2) |
| P | 0.054 | |
| Socioeconomic status | ||
| IRef | 1 | 1 |
| II | 2.0 (0.2-15.3) | 2.2 (0.2-17.8) |
| III | 2.0 (0.3-13.3) | 2.0 (0.3-13.7) |
| IV | 3.1 (0.5-19.2) | 3.9 (0.6-25.1) |
| V | 1.8 (0.2-11.9) | 2.3 (0.3-15.8) |
| P | 0.054 | |
| Type of family | ||
| NuclearRef | 1 | 1 |
| Joint | 1.6 (1.4-2.0) | 1.4 (1.2-1.9) |
| P | 0.039 | |
The mother’s educational and socioeconomic status, type of family, and type of delivery were found to be the significant determinants of having good breastfeeding practices among the study population (<0.05) [Table 6].
Table 6.
Determinants of Good Breastfeeding Practices among respondents
| Variable | Good Breastfeeding Practices (n=159) | |
|---|---|---|
|
| ||
| Unadjusted OR (95%CI) | Adjusted OR (95% CI) | |
| Age of mother | ||
| 18-25 yearsRef | 1 | 1 |
| 26-30 years | 1.0 (0.7-1.6) | 1.1 (0.7-1.7) |
| 31-35 years | 1.1 (0.5-2.7) | 1.2 (0.5-3.1) |
| >35 years | 1.0 (0.2-4.5) | 1.2 (0.2-5.6) |
| P | 0.053 | |
| Child’s mother’s religion | ||
| HinduRef | 1 | 1 |
| Muslim/Sikh/Others | 0.7 (0.5-1.1) | 0.7 (0.4-1.0) |
| P | 0.096 | |
| Child’s mother’s education | ||
| ≤10thRef | 1 | 1 |
| >10th | 0.7 (0.3-1.5) | 0.6 (0.2-1.3) |
| P | 0.021 | |
| Child’s mother’s occupation | ||
| HousewifeRef | 1 | 1 |
| Working | 2.2 (0.5-10.3) | 2.1 (0.4-10.1) |
| P | 0.053 | |
| Socioeconomic status | ||
| IRef | 1 | 1 |
| II | 2.9 (0.2-31.2) | 3.2 (0.2-36.8) |
| III | 2.5 (0.2-23.9) | 3.4 (0.3-34.7) |
| IV | 2.4 (0.2-22.1) | 3.0 (0.3-29.5) |
| V | 2 (0.2-18.8) | 2.7 (0.2-27.0) |
| P | 0.041 | |
| Type of family | ||
| NuclearRef | 1 | 1 |
| Joint | 1.2 (0.8-1.5) | 1.1 (0.6-1.4) |
| P | 0.036 | |
| Type of delivery | ||
| HomeRef | 1 | 1 |
| Institutional | 2.2 (1.3-3.5) | 2.1 (1.4-3.3) |
| P | 0.042 | |
Discussion
The majority of respondents had the correct knowledge about breastfeeding the baby immediately after birth (76.6%), no prelacteal foods to be provided (82.2%), colostrum to be fed to baby (89.0%), baby to be breastfed 8–12 times in 24 hours (99.1%) and exclusively breastfed for first 6 months were (78.7%). Our findings are similar to the cross-sectional study conducted in South India, where 75% of them had adequate knowledge of EBF and the benefits of EBF.[10] The NFHS-4 data reports an increase in exclusive breastfeeding (46.4% (NFHS-3) to 54.9% (NFHS-4)).[7] In a recent study conducted at Banaras Medical College Hospital regarding knowledge about breastfeeding, the majority of females (71.4%) considered breast milk as the best food for a newborn.[11]
Our findings are also similar to a study in Northwest India, where 87.74% of the subjects knew that colostrum should be given to newborns.[12] On the contrary, Gupta et al.,[13] in their study in the urban slums of Lucknow reported that only about half of the respondents thought that colostrum might prevent babies from illness. In another study by Das et al. 64% of mothers had a good opinion about colostrum.[14]
The knowledge scores about breastfeeding among most of the respondents were good (64.9%), followed by fair (23.2%) and poor (11.9%). Lactation guidance by health care workers and counselors during the pre- and postnatal period is recommended so that the mother can obtain early information about breastfeeding.[15]
A higher proportion of respondents practiced breastfeeding only or were cup-fed with breast milk only for their babies for the first 2 days of life (62.3%). The majority (77.3%) fed their baby an adequate number of times during the day/night. Only 55.7% put their baby to breast within an hour after birth. First, milk (colostrum) was not squeezed out and thrown away by nearly 59.7% of mothers.
The infant and young child feeding guidelines (IYCF 2016) recommend breastfeeding initiation, preferably within one hour after birth.[16] Similarly, a study from Gujarat showed that 57.5% of the children received EIBF.[17] In another study, less than one-third of infants were breastfed within the first hour of birth, and one-third were receiving a prelacteal feed.[18] A study by Senanayake et al.[19] used information from a total sample of 94,401 mothers and indicated that 41.5% of Indian mothers had EIBF, with similar but significantly different proportions estimated for those who resided in rural (41.0%) and urban (42.9%) areas. In this study, after delivery, nearly half of the mothers were given no fluid/feeds to drink before breastfeeding for the first time. Ghutti (water mixed with honey and herbs) was a commonly used prelacteal feed in a previous study at Bareilly.[20,21] Prelacteal feeding is a common custom prevalent in India and other developing countries.[22,23,24] It is believed that prelacteal fluids clear the meconium. Unfortunately, the mothers are ignorant that the prelacteal feeds could be a source of contamination.[25]
The breastfeeding practices scores among a higher proportion of respondents were poor (36.3%), followed by good (35.8%) and fair (27.9%). EIBF and EBF of children below six months are considered the most decisive indicators for assessing breastfeeding practices.[26] Any opportunity should not be missed to counsel the mothers and equip them with correct knowledge and skills related to breastfeeding.[27] Breastfeeding promotes the cognitive development of the newborn. EIBF prevents 22% of neonatal deaths.[28]
Age of mother and type of family were found to be significant determinants of Good Knowledge about breastfeeding among respondents (<0.05). The child’s mother’s education, socioeconomic status, type of family, and type of delivery were found to be significant determinants of good breastfeeding practices among respondents (<0.05). The findings are compatible with those reported by Ogbo et al.[29] where key modifiable determinants for EBF were higher maternal education in Central India and frequent antenatal care (≥4) visits in northern India. Similarly, in a North Indian study, EIBF was positively associated with maternal knowledge, counseling during pregnancy/delivery, and vaginal delivery while EBF was positively associated with maternal knowledge, beliefs, self-efficacy, parity, and socioeconomic status.[18]
Although prior research[30,31,32,33,34] has implemented interventions for EIBF, promote colostrum intake and EBF through counseling during antenatal visits or at tertiary-care settings by trained female health workers, however. Further engaging and counseling of mothers, family (husbands and mother-in-laws) and community members by health workers is critical to improving breastfeeding practices. Although a validated questionnaire was used by trained data collectors, which could be mentioned as the strength of the study; however, the recall method may cause overestimation of the percentage of some infant feeding practices, which could be a limitation of this study.
Recommendations
Health care workers/providers should be trained in breastfeeding counseling for women, families, and community members.
Proper breastfeeding behavior should be encouraged during the antenatal and postnatal periods.
The importance of colostrum feeding EBF for the first 6 months, EIBF, and continued breastfeeding along with appropriate complementary foods up to and beyond 2 years of age should be discussed.
Prelacteal feeding should be strongly discouraged.
Common nursing issues should be discussed, and in case of severe problems, referral for expert advice should be performed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rajak P, Jana JK, Gayen S. Knowledge of breastfeeding practices among mothers attending a tertiary care setting in East India. Cureus. 2023;15:e37146. doi: 10.7759/cureus.37146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haroon S, Das JK, Salam RA, Imdad A, Bhutta ZA. Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health. 2013;13((Suppl 3)):S20. doi: 10.1186/1471-2458-13-S3-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–90. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 4.WHO (World Health Organization) Global strategy for infant and young child feeding. Geneva: World Health Organization; 2003. [[Last accessed on 2024 Mar 28]]. Available from: https://iris.who.int/bitstream/handle/10665/42590/9241562218.pdf?sequence=1WHO%20(World%20Hea l th%20Organization).%20Global%20strategy%20for%20infant%20and%20young%20child%20feeding.%20Geneva:%20World%20Health%20Organization;%202003 . [Google Scholar]
- 5.Khatib MN, Gaidhane A, Upadhyay S, Telrandhe S, Saxena D, Simkhada PP, et al. Interventions for promoting and optimizing breastfeeding practices: An overview of systematic review. Front Public Health. 2023;11:984876. doi: 10.3389/fpubh.2023.984876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNICEF. (2018) UNICEF Global Databases. Nutrition: Infant and Young Child Feeding. [[Last accessed on 2023 Dec 15]]. Available from: https://data.unicef.org/topic/nutrition/infant-andyoung-child-feeding/
- 7.International Institute of Population Sciences (IIPS). National Family Health Survey, India: Key Findings from NFHS-4. [[Last accessed on 2024 Jan 14]]. Available from: http://rchiips.org/NFHS/factsheet_NFHS-4.shtml .
- 8.Appiah PK, Amu H, Osei E, Konlan KD, Mumuni IH, Verner ON, et al. Breastfeeding and weaning practices among mothers in Ghana: A population-based cross-sectional study. PLoS One. 2021;16:e0259442. doi: 10.1371/journal.pone.0259442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tomori C. Overcoming barriers to breastfeeding. Best Pract Res Clin Obstet Gynaecol. 2022;83:60–71. doi: 10.1016/j.bpobgyn.2022.01.010. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Maternal Health and Safe Motherhood Programme and Meeting of Technical Working Group on Thermal Control of the Newborn [Internet]. 1993. [[Last accessed on 2021 Jan 10]]. Available from: https://apps.who.int/iris/handle/10665/60042 .
- 11.Sultania P, Agrawal NR, Rani A, Dharel D, Charles R, Dudani R. Breastfeeding knowledge and behavior among women visiting a tertiary care center in India: A cross-sectional survey. Ann Glob Health. 2019;85:64. doi: 10.5334/aogh.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verma AK, Kumari R, Hussain S, Langer B, Gupta RK, Singh P. Knowledge and practices regarding breastfeeding: A community-based cross-sectional study in a rural area of Northwest India. Int J Med Sci Public Health. 2017;6:1056–60. [Google Scholar]
- 13.Gupta P, Srivastava V, Kumar V, Jain S, Masood J, Ahmad N, et al. Newborn care practices in urban slums of Lucknow city, UP. Indian J Community Med. 2010;35:82–5. doi: 10.4103/0970-0218.62570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Das R, Mukherjee A. Knowledge, attitude and practices of infant feeding practices among rural women in Eastern India. J Evol Med Dent Sci. 2014;3:506–12. [Google Scholar]
- 15.Awaliyah SN, Rachmawati IN, Rahmah H. Breastfeeding self-efficacy as a dominant factor affecting maternal breastfeeding satisfaction. BMC Nurs. 2019;18((Suppl 1)):30. doi: 10.1186/s12912-019-0359-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tiwari S, Bharadva K, Yadav B, Malik S, Gangal P, Banapurmath CR, et al. Infant and Young Child Feeding Guidelines, 2016. Indian Pediatr. 2016;53:703–13. doi: 10.1007/s13312-016-0914-0. [DOI] [PubMed] [Google Scholar]
- 17.Patel DV, Bansal SC, Nimbalkar AS, Phatak AG, Nimbalkar SM, Desai RG. Breastfeeding practices, demographic variables, and their association with morbidities in children. Adv Prev Med. 2015;2015:892825. doi: 10.1155/2015/892825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young MF, Nguyen P, Kachwaha S, Tran Mai L, Ghosh S, Agrawal R, et al. It takes a village: An empirical analysis of how husbands, mothers-in-law, health workers, and mothers influence breastfeeding practices in Uttar Pradesh, India. Matern Child Nutr. 2020;16:e12892. doi: 10.1111/mcn.12892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senanayake P, O'Connor E, Ogbo FA. National and rural-urban prevalence and determinants of early initiation of breastfeeding in India. BMC Public Health. 2019;19:896. doi: 10.1186/s12889-019-7246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahmood SE, Srivastava A, Shrotriya VP, Mishra P. Infant feeding practices in the rural population of north India. J Family Community Med. 2012;19:130–5. doi: 10.4103/2230-8229.98305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kavle JA, Picolo M, Buccini G, Barros I, Dillaway CH, Pérez-Escamilla R. Strengthening counseling on barriers to exclusive breastfeeding through use of job aids in Nampula, Mozambique. PLoS One. 2019;14:e0224939. doi: 10.1371/journal.pone.0224939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roy MP, Mohan U, Singh SK, Singh VK, Srivastava AK. Determinants of prelacteal feeding in rural northern India. Int J Prev Med. 2014;5:658–63. [PMC free article] [PubMed] [Google Scholar]
- 23.Amele EA, Demissie BW, Desta KW, Woldemariam EB. Prelacteal feeding practice and its associated factors among mothers of children age less than 24 months old in Southern Ethiopia. Ital J Pediatr. 2019;45:15. doi: 10.1186/s13052-019-0604-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chea N, Asefa A. Prelacteal feeding and associated factors among newborns in rural Sidama, south Ethiopia: A community based cross-sectional survey. Int Breastfeed J. 2018;13:7. doi: 10.1186/s13006-018-0149-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manikam L, Prasad A, Dharmaratnam A, Moen C, Robinson A, Light A, et al. Systematic review of infant and young child complementary feeding practices in South Asian families: The India perspective. Public Health Nutr. 2018;21:637–54. doi: 10.1017/S136898001700297X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1 Definitions. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 27.Bhanderi DJ, Pandya YP, Sharma DB. Barriers to exclusive breastfeeding in rural community of central Gujarat, India. J Family Med Prim Care. 2019;8:54–61. doi: 10.4103/jfmpc.jfmpc_329_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith ER, Hurt L, Chowdhury R, Sinha B, Fawzi W, Edmond KM Neovita Study Group. Delayed breastfeeding initiation and infant survival: A systematic review and meta-analysis. PLoS One. 2017;12:e0180722. doi: 10.1371/journal.pone.0180722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ogbo FA, Dhami MV, Awosemo AO, Olusanya BO, Olusanya J, Osuagwu UL, et al. Regional prevalence and determinants of exclusive breastfeeding in India [published correction appears in Int Breastfeed J 2019 Jun 4;14:22] Int Breastfeed J. 2019;14:20. doi: 10.1186/s13006-019-0214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khan MH, Khalique N, Siddiqui AR, Amir A. Impact of behavior change communication among pregnant women regarding neonatal care. Indian J Public Health. 2013;80:804–8. doi: 10.1007/s12098-013-1076-x. [DOI] [PubMed] [Google Scholar]
- 31.Gami N, Mishra A, Kocher S. To study the effect of counselling on early initiation of breast feeding in the first hour of life. Glob J Med Res. 2014;13:17–24. [Google Scholar]
- 32.Avula R, Oddo VM, Kadiyala S, Menon P. Scaling-up interventions to improve infant and young child feeding in India: What will it take? Matern Child Nutr. 2017;13((Suppl 2)):e12414. doi: 10.1111/mcn.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Das A, Chatterjee R, Karthick M, Mahapatra T, Chaudhuri I. The influence of seasonality and community-based health worker provided counselling on exclusive breastfeeding-Findings from a cross-sectional survey in India. PLoS One. 2016;11:e0161186. doi: 10.1371/journal.pone.0161186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain S, Thapar RK, Gupta RK. Complete coverage and covering completely: Breast feeding and complementary feeding: Knowledge, attitude, and practices of mothers. Med J Armed Forces India. 2018;74:28–32. doi: 10.1016/j.mjafi.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]


