ABSTRACT
Background:
Modified Bishop score (MBS) and cervical length determination by transvaginal sonography (TVS) are the two methods for predicting successful vaginal delivery based on pre-induction favourability of the cervix.
Aims and Objectives:
This study compared both methods for predicting successful vaginal delivery. The primary objective was to compare the predictive value of MBS and TVS in predicting successful induction of labor. The secondary objective was to obtain the cut-off score of MBS and TVS for successful induction of labor.
Methods:
A prospective study was done involving 100 pregnant women admitted for induction of labor. TVS was done to measure the cervical length before induction of labor. MBS was also calculated for all the patients. Labor was induced with prostaglandins. Labor induction was considered successful if there was an onset of uterine contractions and cervical dilatation within 24 h of induction.
Results:
For successful induction of labor, the cutoff of cervical length by TVS and MBS was 2.5 cm and 6, respectively. Cervical length assessment by TVS performed better than the MBS (sensitivity 61.8% vs. 28.9%, Specificity 95.8% vs. 100%).
Conclusion:
MBS and cervical length measurement by sonography both are good predictors of successful induction of labor. Cervical length measurement by TVS provides a better prediction of the likelihood of vaginal delivery.
Keywords: Induction of labor, modified bishop score, negative predictive value, positive predictive value, prediction of labor, sensitivity, specificity, transcervical length
Introduction
Labor needs to be induced in a variety of clinical settings. Post-dated pregnancy, pre-eclampsia, fetal growth restriction, intrauterine death, and intrahepatic cholestasis of pregnancy are a few common indications needing labor induction.[1] Bishop score was the traditional method for predicting successful vaginal delivery till its modification by Calder.[2,3] Modified Bishop score (MBS) is used nowadays. It is based on pre-induction favorability of the cervix and is assessed manually. Its components are cervical dilation (in centimeters), length of the cervix (in centimeters), cervical consistency (soft or firm or medium), cervical position (posterior or mid or anterior), and fetal station. The score is between 0–13. An MBS of 9 or more favors successful induction. A score of 4 or less means an unripe cervix and the need for cervical ripening.[3] However, this method is subjective and irreproducible. Many researchers have shown a poor correlation between MBS and labor outcomes. In 1986, O’Leary and Ferrell proposed an ultrasound scoring system and evaluated this system against the MBS.[4] This scoring system evaluated the thickness and contour of the lower uterine segment, and the length and dilation of the cervix using transabdominal ultrasound. A full bladder required to assess the cervix adequately may falsely lengthen the cervix by opposing the anterior and posterior lower uterine segments. It may also conceal a shortened or funneled cervix. High BMI, shadowing from fetal parts and the need for lower frequency transducers also make interpretation of transabdominal ultrasound difficult for assessing the cervix. In contrast, a transvaginal ultrasound is performed with an empty bladder. Cervical length determination by transvaginal sonography (TVS) is more objective and reproducible. Thus, it can be a better method for the prediction of successful induction of labor as the supra-vaginal portion of the cervix comprises about 50% of the cervical length[5,6] and it is very difficult to assess digitally in a closed cervix. However, some anatomic or technical difficulties may be encountered while doing TVS too. Focal myometrial contraction can obscure the internal os and make the cervix appear longer on vaginal sonography. Similarly, endocervical mucus or polyps may appear to separate the anterior and posterior borders of the endocervical canal and make the cervix measure shorter. Technically minimal pressure on the cervix falsely elongates the cervical length measurement.[7] Transvaginal sonographic assessment of the cervix should be done taking care of these technical difficulties and by following standard protocol. The availability of ultrasound in all district hospitals makes it easier for all primary-level health givers to utilize it in predicting induction of labor in their setup.
Aims and Objectives
The aim of the study was to determine whether transvaginal ultrasound could predict the outcome of induction of labor better than the MBS.
The objectives included comparing the predictive value of MBS and TVS in successful induction of labor and obtaining the cut-off score of MBS and mean cervical length by TVS for prediction of successful induction of labor.
Materials and Methods
A prospective observational study was conducted after obtaining ethical clearance from the Institutional Ethics Committee and in accordance with the Helsinki Declaration.
A sample size of 100 was calculated based on a previous study by Agrawal et al.[8] (Sensitivity 93.24 vs. 67.57%, Specificity 73.08 vs. 65.38%) and according to the formula:
* Se = Sensitivity, Sp = Specificity, Prev = Prevalence/Incidence of outcome Type I error (α) = 5% Z1-α/2 = 1.96, d = Precision.
Inclusion criteria
Pregnant women with a singleton pregnancy with a live fetus in need of induction of labor with no contraindications for vaginal delivery.
Exclusion criteria
Patients with known allergies to prostaglandins, having a contraindication to vaginal delivery like placenta previa or a history of uterine surgeries like previous lower segment cesarean section and myomectomy were excluded. Pregnant patients with cardiac diseases were also excluded.
A total of 100 pregnant women who fulfilled the inclusion criteria were enrolled after written informed consent over a period of one year. Baseline characters such as age, gestational age, and indication for induction were noted. Cervical length was measured by TVS. An ultrasound machine of the Samsung H60 model with a TVS probe frequency of 5–7.5 MHz was used. Women were examined in a dorsal lithotomy position with an empty urinary bladder. A clean TVS probe covered by a condom was inserted into the vagina. Once the cervical canal was identified the probe was withdrawn slightly so there was no pressure of the tip of the probe on the cervix. A sagittal plane through the cervix was identified where the external cervical os, the cervical canal, and the internal os were visible. The image was enlarged so that the cervix occupied at least 2/3rd of the image. The length of the cervix was measured from the internal to the external os as a straight line. Three measurements were obtained in the absence of uterine contraction and mean measurement was noted. Then digital examination was performed by the attending obstetrician for cervical consistency, length, dilatation, position, and station of the presenting part as described in the MBS. Cervical length noted by TVS and MBS was noted in proforma. Induction of labor was carried out according to standard protocol. Prostaglandins were used as per indication of induction, which was done within 1 h of cervical assessment. The labor induction was considered successful if there was an onset of uterine contractions and cervical dilatation within 24 h of induction.
Statistical analysis
The statistical analysis was done using Microsoft Excel 2013 and SPSS statistical and multivariate analysis software, version 2021. Descriptive statistics were used to measure central tendency. Receiver operating characteristic curves (ROC) were used to calculate and compare the cut-off points for cervical length and MBS. The diagnostic accuracy of both measurements was done by comparing the area under the ROC curves. Two-sided P values were reported throughout, P < 0.05 was considered statistically significant.
Results
Mean Maternal age (Years) was 25.33 ± 3.58 [Table 1].
Table 1.
Showing distribution of participants according to maternal age
| Age Group (Years) | n=100 |
|---|---|
| 18–25 | 53 (53%) |
| 26–30 | 45 (45%) |
| 31–35 | 2 (2%) |
Mean Gestational age (weeks) was 38.41 ± 2.23 [Table 2].
Table 2.
Showing distribution of participants according to gestational age
| Gestational Age (Weeks) | n=100 |
|---|---|
| <28 | 1 (1%) |
| 28–33+6 | 5 (5%) |
| 34–36+6 | 11 (11%) |
| >37 | 83 (83%) |
Most common indication for Induction of Labour was Intrahepatic Cholestasis of Pregnancy [Table 3].
Table 3.
Indications for induction of labor
| Indication(s) | n=100 | 95%CI |
|---|---|---|
| IHCP† | 32 (32%) | 24.0–43.4% |
| Post-dated Pregnancy | 27 (27%) | 19.4–38% |
| PROM | 14 (14%) | 8.4–23.4% |
| Oligohydramnios | 23 (23%) | 15.9–33.6% |
| GDM | 3 (3%) | 0.8–9.4% |
| Others | 7 (7%) | 3.2–14.8% |
†IHCP- Intrahepatic cholestasis of pregnancy
A total of 92 (92.0%) of the participants had no obstetric complications. Eight (8.0%) of the participants had post-partum hemorrhage as an obstetric complication. Seventy-eight (78.0%) of the participants had no medical complications. Two (2.0%) of the participants had chronic hypertension. Thirteen (13.0%) of the participants had hypothyroidism. Three (3.0%) of the participants had anemia. Two (2.0%) of the participants had beta-thalassemia trait. Two (2.0%) of the participants had thrombocytopenia.
The mean Cervical Length on TVS (cm) was 2.59 ± 0.47 [Table 4].
Table 4.
Distribution of Participants in terms of Cervical length on TVS (cm) (n=100)
| Cervical Length on TVS (cms) | |
|---|---|
| Mean (SD) | 2.59 (0.47) |
| Median (IQR) | 2.6 (2.32–2.81) |
| Range | 1.8–4.44 |
The mean MBS was 4.54 ± 1.14 [Table 5].
Table 5.
Distribution of Participants in terms of MBS (n=100)
| Modified Bishop Score | |
|---|---|
| Mean (SD) | 4.54 (1.14) |
| Median (IQR) | 5 (4-5) |
| Range | 2-7 |
A total of 87% of the participants had successful induction of labor. Sixty-two (62.0%) of the participants had vaginal delivery. Thirty-eight (38.0%) of the participants had undergone LSCS. Thirteen (34.2%) of the participants had failed induction as an indication for LSCS. Sixteen (42.1%) had fetal distress. Nine (23.7%) of the participants had non-progress of labor. The mean Induction-Active phase Interval was 17.61 ± 11.63 h [Table 6].
Table 6.
Distribution of Participants in terms of Induction -Active Phase Interval (Hours) (n=64)
| I-A lnterval (hours) | |
|---|---|
| Mean (SD) | 17.61 (11.63) |
| Median (IQR) | 15 (10-21.25) |
| Range | 4-63 |
The mean Induction-Delivery Interval was 19.65 ± 10.90 h [Table 7]. The skewness of the data was 1.43, and it suggested that the data was positively skewed, thus suggesting it was not normally distributed. The kurtosis of the data was 3.8, and it suggested that the data was not normally distributed. Shapiro–Wilk test for the data was significant (P = <0.001), suggesting that the data was not normally distributed. There appeared to be more than one mode/peak in the data, thus making it multimodal. Since the data was multimodal (had more than one peak), it appeared that the data was not normally distributed (did not follow a bell-shaped curve). The mean (SD) of cervical length on TVS (cm) for vaginal delivery and LSCS was 2.50 (0.46) and 2.75 (0.45), respectively. There was a significant difference between the two groups in terms of cervical length on TVS (cm) (W = 647.500, P = <0.001), with the median cervical length on TVS (cm) being highest in the LSCS group.
Table 7.
Distribution of Participants in terms of Induction -Delivery Interval (Hours) (n=64)
| I-D lnterval (hours) | |
|---|---|
| Mean (SD) | 19.65 (10.90) |
| Median (IQR) | 18 (11–26) |
| Range | 3–67 |
The variable cervical length on TVS (cm) was not normally distributed in the two subgroups of the variable Successful Induction [Table 8]. Thus, non-parametric tests (Wilcoxon–Mann–Whitney U Test) were used to make group comparisons. There was a significant difference between the two groups in terms of cervical length on TVS (cm) (W = 358.500, P = <0.001), with the median cervical length on TVS (cm) being the highest in the failed induction group. The mean (SD) of MBS in the vaginal delivery and LSCS group was 4.71 (1.11) and 4.26 (1.16), respectively. There was no significant difference between the groups in terms of MBS (W = 1401.500, P = 0.101).
Table 8.
Success of induction based on cervical length by TVS
| Cervical length on TVS | Successful induction | Wilcoxon–Mann–Whitney U test | ||
|---|---|---|---|---|
|
|
|
|||
| Yes | No | W | P | |
| Mean (SD) | 2.51 (0.48) | 2.85 (0.29) | 358.500 | <0.001 |
| Median (IQR) | 2.4 (2.25–2.65) | 2.88 (2.66–3) | ||
| Range | 1.8-4.44 | 2.02–3.32 | ||
The diagnostic efficacy of cervical length measurement by TVS was more than MBS (70% vs. 46%) [Table 9].
Table 9.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) of modified bishop score and cervical length measured by TVS
| Variable | Sensitivity | Specificity | PPV | NPV | Diagnostic Accuracy |
|---|---|---|---|---|---|
| Cervical Length on TVS (cms) | 61.8% (50–73) | 95.8% (79–100) | 97.9% (89–100) | 44.2% (30–59) | 70% (60–79) |
| Modified Bishop Score | 28.9% (19–40) | 100% (86–100 | 100% (85–100) | 30.8% (21–42) | 46% (36–56) |
The area under the Receiver operating characteristic curve (AUROC) for cervical length on TVS (cm) predicting Successful Induction vs failed Induction was 0.803 (95% CI: 0.71–0.897), thus demonstrating good diagnostic performance. It was statistically significant (P = <0.001). At a cutoff of cervical length on TVS (cm) ≤2.58, it predicted successful induction with a sensitivity of 62% and a specificity of 96% [Figure 1].
Figure 1.
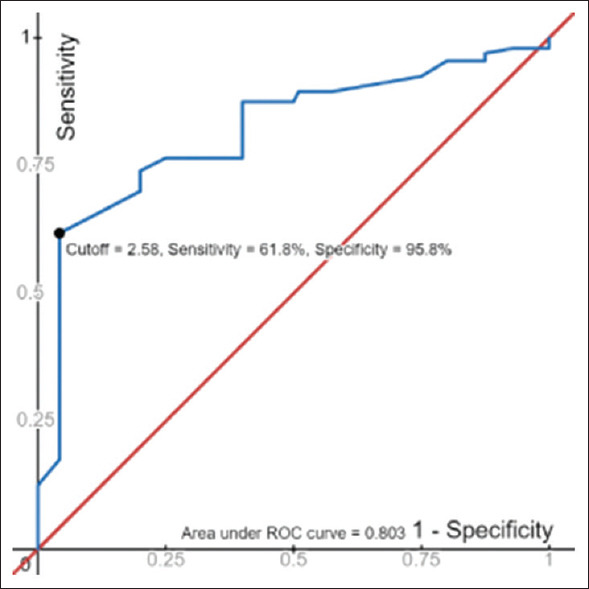
Receiver operating Characteristics curve 1 for TVS
The area under the receiver operating curve (AUROC) for MBS predicting successful induction vs failed induction was 0.6 (95% CI: 0.49–0.711), thus demonstrating poor diagnostic performance. It was not statistically significant (P = 0.127) [Figure 2].
Figure 2.
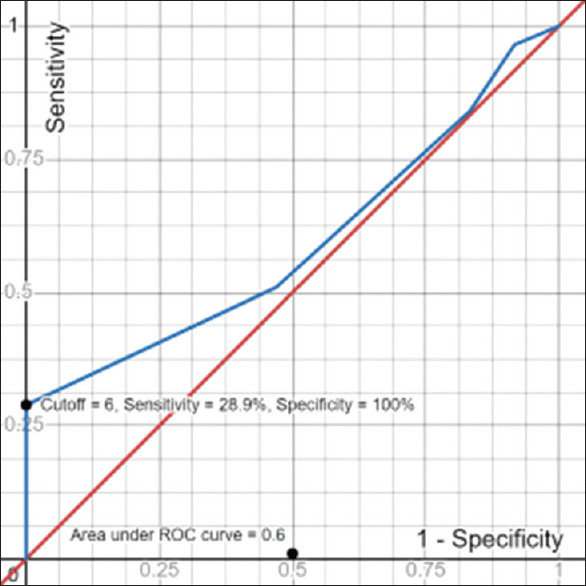
Receiver operating characteristics curve 2 for MBS
At a cutoff of MBS ≥6, it predicts successful induction with a sensitivity of 29% and a specificity of 100%. The mean birth weight was 2.85 ± 0.53 kg. The mean (SD) of APGAR (1 Minute) was 7.93 (1.34). The median (IQR) of APGAR (1 min) was 8.00 (8–9). The APGAR (1 min) ranged from 3 to 10.
Discussion
Pre-induction counseling and explaining the chances of successful inductions are very important for primary care physicians. Ultrasound assessment of the cervix can help primary care physicians in predicting the likely outcome of induced labor as an alternative to clinical digital examination. Studies have explored possible relationships between cervical length, internal cervical os shape, and assessment of the angle between the cervical axis and the wall of the inferior segment of the uterus.[9] The assessment of the cervix should always be done immediately before applying prostaglandins to prevent the effect of these chemicals on the cervical tissue.[10] In our study, both cervical length by TVS and cervical assessment by MBS were proved to be complementary tools for the prediction of successful induction of labor. Cervical length by TVS had better sensitivity at a cutoff of 2.58 cm. MBS had better specificity (cutoff-6). The best parameter in terms of positive predictive value was MBS. The best parameter in terms of negative predictive value and diagnostic accuracy was cervical length on TVS.
A study to find out the effectiveness of assessment of cervical length by transvaginal ultrasonography in predicting preterm delivery between 22 weeks and 24 weeks of gestation, concluded that TVS was an efficient tool in assessing the risk of preterm delivery in patients with short cervix.[11] In another study comparing cervical length by TVS and MBS it was found that cervical length and Modified Bishop’s score were complementary tools for predicting successful induction of labor, but TVS had better specificity and positive predictive value at cutoff of 2.8 cm.[12] One study showed that cervical length measurement by TVS at the cutoff of 2.8 cm was a better predictor of successful induction of labor.[13] However, another showed that cervical length measurement by TVS at the cutoff of 2.7 cm was a better predictor of successful induction of labor.[14] A study compared TVS with Modified Bishop scoring in 100 women. At cut-off scores of ≥4, the TVS cervical Score performed better than the MBS (sensitivity 93.24 vs. 67.57%, Specificity 73.08 vs. 65.38%). Two components of MBS, namely cervical length and station demonstrated significant and independent prediction of the likelihood of failure of induction and risk of operative delivery.[15] Though cervical length was superior in predicting the success of labor induction compared to the Bishop score, the sensitivity for cervical length was not significantly in the higher range.[16] This may be because only the latent phase of labor can be correlated with cervical length, not the active phase. Hence latent phase of the labor will be longer in women with longer cervical length.[17] Women with a shorter cervical length of less than 2.7 cm can be counseled that delivery will possibly occur earlier after induction, compared to those with longer cervix.[18] Parity, estimated fetal weight, maternal BMI, and strength of uterine contractions are other factors influencing the duration of the latent phase, active phase, and induction delivery interval. Other predictors for favorable induction of labor have been investigated in recent times like the Tetrapolar pencil probe, cervical elastography, biomarkers like fetal fibronectin, and insulin-like growth factor binding protein-1.[19,20,21]
Conclusion
Many pregnant women require induction of labor. Many factors influence the choice of opting for vaginal delivery. Both MBS and transvaginal cervical length measurement are good predictors of successful induction of labor. Cervical length assessment by TVS could be used as a better alternative to the MBS in settings where the appropriate equipment and expertise are available. However, MBS retains its place in assessing pregnant patients for favorability for induction of labor.
Abbreviations used
MBS- Modified Bishop Score
TVS- Transvaginal Sonography
LSCS-Lower Segment of Caesarean Section
BMI- Body Mass Index
IHCP- Intrahepatic Cholestasis of Pregnancy
SD- Standard deviation
IQR- Intra-Quartile Range
ROC- Receiver Operating Characteristic Curve.
Limitations of study
It was a hospital-based study with a small sample size, so the results could not be generalized.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would like to thank all participants, nursing staff, and residents of the Department of OBG, IGIMS, Patna who actively participated in this study.
References
- 1.Induction and augmentation of labor. Cunningham F, Leveno K. J, Bloom S. L, Dashe J. S, Hoffman B. L, Casey B. M, Spong C. Y, editors. Williams Obstetrics, 25e. McGraw Hill Education(503-512) ISBN 978-1-259-64432-0 MHID 1-259-64432-4 [Google Scholar]
- 2.Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol. 1964;24:266–8. [PubMed] [Google Scholar]
- 3.Khan S, Rao S. Cervical effacement, as an independent parameter versus modified bishop score, for predicting the favorability of vaginal delivery in a primigravida at 40 weeks gestation and beyond. Int J Reprod Contracept Obstet Gynecol. 2020;9 doi: 10.18203/2320-1770.ijrcog20201486. [Google Scholar]
- 4.O'Leary JA, Ferrell RE. Comparison of ultrasonographic and digital cervical evaluation. Obstet Gynecol. 1986;68:718–9. [PubMed] [Google Scholar]
- 5.Anderson HF. Transvaginal and transabdominal ultrasonography of the uterine cervix during pregnancy. Am J Clin Ultrasound. 1991;19:77–83. doi: 10.1002/jcu.1870190204. [DOI] [PubMed] [Google Scholar]
- 6.To MS, Skentou C, Chan C, Zagaliki A, Nicolaides KH. Cervical assessment at the routine 23-week scan: Standardizing techniques. Ultrasound Obstet Gynecol. 2001;17:217–9. doi: 10.1046/j.1469-0705.2001.00369.x. [DOI] [PubMed] [Google Scholar]
- 7.Rane SM, Guirgis RR, Higgins B, Nicolaides KH. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2004;24:538–49. doi: 10.1002/uog.1100. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal A, Tripathi PS, Bhandari G, Kheti P, Madhpuriya G, Rathore R. Comparative study of TVS cervical score and Bishop score in prediction of successful labour induction. Egypt J Radiol Nucl Med. 2022;53:138. [Google Scholar]
- 9.Chandra S, Crane JM, Hutchens D, Young DC. Transvaginal ultrasound and digital examination in predicting successful labor induction. Obstet Gynecol. 2001;98:2–6. doi: 10.1016/s0029-7844(01)01386-2. [DOI] [PubMed] [Google Scholar]
- 10.Al-Adwy AM, Sobh SM, Belal DS, Omran EF, Hassan A, Saad AH, et al. Diagnostic accuracy of posterior cervical angle and cervical length in the prediction of successful induction of labor. Int J Gynaecol Obstet. 2018;141:102–7. doi: 10.1002/ijgo.12425. [DOI] [PubMed] [Google Scholar]
- 11.Tanvir, Ghose S, Samal S, Armugam S, Parida P. Measurement of cervical biometry using transvaginal ultrasonography in predicting preterm labor. J Nat Sc Biol Med. 2014;5:369–72. doi: 10.4103/0976-9668.136189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El Mekkawi SF, Hanafi S, Khalaf-Allah AE, Abdelazim IA, Mohammed EK. Comparison of transvaginal cervical length and modified Bishop's score as predictors for labor induction in nulliparous women. Asian Pac J Reprod. 2019;8:34–8. [Google Scholar]
- 13.Alanwar A, Hussein SH, Allam HA, Hussein AM, Abdelazim IA, Abbas AM, et al. Transvaginal sonographic measurement of cervical length versus Bishop score in labor induction at term for prediction of caesarean delivery. J Matern Fetal Neonatal Med. 2021;34:2146–53. doi: 10.1080/14767058.2019.1659770. [DOI] [PubMed] [Google Scholar]
- 14.Atal R, Mokharia J, Chauhan M. Study on comparison of transvaginal cervical length and bishop score in predicting successful labour induction. Int J Recent Trends Sci Technol. 2016;18:181–4. [Google Scholar]
- 15.Bajpai N, Bhakta R, Kumar P, Rai L, Hebbar S. Manipal cervical scoring system by transvaginal ultrasound in predicting successful labour induction. J Clin Diagn Res. 2015;9:QC04–9. doi: 10.7860/JCDR/2015/12315.5970. doi: 10.7860/JCDR/2015/12315.5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sreenivas A, Geetha K, Subhashini M. Transvaginal sonographic cervical length assessment in predicting the outcome of induction of labour. Int J Reprod Contracept Obstet Gynecol. 2022;11:853–8. [Google Scholar]
- 17.Park KH. Transvaginal ultrasonographic cervical measurement in predicting failed labor induction and cesarean delivery for failure to progress in nulliparous women. J Korean Med Sci. 2007;22:722–7. doi: 10.3346/jkms.2007.22.4.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monika, Jakhar B, Choudhary N, Khoiwal S. Study of comparison of transvaginal cervical length and Bishop score in predicting successful labour induction-A prospective study from a tertiary care hospital of Rajasthan. Int J Reprod Contracept Obstet Gynecol. 2023;12:2475–80. [Google Scholar]
- 19.O'Connell MP, Avis NJ, Brown BH, Killick SR, Lindow SW. Electrical impedance measurements: An objective measure of prelabor cervical change. J Matern Fetal Neonatal Med. 2003;14:389–91. doi: 10.1080/14767050412331312230. [DOI] [PubMed] [Google Scholar]
- 20.Wang B, Zhang Y, Chen S, Xiang X, Wen J, Yi M, He B, Hu B. Diagnostic accuracy of cervical elastography in predicting preterm delivery: A systematic review and meta-analysis. Medicine. 2019;98:e16449. doi: 10.1097/MD.0000000000016449. doi: 10.1097/MD.0000000000016449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grab D, Doroftei B, Grigore M, Nicolaiciuc OS, Anton SC, Simionescu G, et al. Fetal fibronectin and cervical length as predictors of spontaneous onset of labour and delivery in term pregnancies. Healthcare. 2022;10:1349. doi: 10.3390/healthcare10071349. doi: 10.3390/healthcare10071349. [DOI] [PMC free article] [PubMed] [Google Scholar]


