ABSTRACT
Background:
Published data demonstrate promising results for rehabilitation in patients with multiple sclerosis (MS), including telerehabilitation technologies. Given the travel limitations during the coronavirus disease 2019 (COVID-19), telerehabilitation may provide a viable alternative to in-person physiotherapy.
Objective:
To determine the efficacy of telerehabilitation in MS patients during COVID-19.
Design/Methods:
A total of 42 patients participated in the study of which 24 were followed up till the end of 6 weeks. The investigated group consisted of 15 females and 09 males; the mean age was 42 ± 10 years. The telerehabilitation was provided for a duration of 6 weeks at a frequency of three classes per week. The patients used either laptops or mobile phones for attending these sessions. The inclusion criteria were a 6-minute walk test (with or without assistance). Motor function was evaluated using the Timed Up and Go (TUG) test and the 30-Second Sit-to-Stand (30STS) test. Patients were required to fill out two questionnaires also: 12-item MS Walking Scale (MSWS) and Modified Fatigue Impact Scale (MFIS). All the patient assessments were made by an independent physiotherapist before and after the intervention.
Results:
There was a statistically significant improvement in motor performance and MFIS and 12-item MSWS. The following results were observed: statistically improved parameters of TUG, 30STS, 12-item MSWS and MFIS.
Conclusions:
Based on the findings, it is reasonable to infer that the use of telemedicine in the rehabilitation of MS patients is very promising.
Keywords: COVID-19 pandemic, India, multiple sclerosis, telerehabilitation, virtual physiotherapy
Introduction
India reported the first coronavirus disease 2019 (COVID-19) case on 27 January 2020, in the southern state of Kerala.[1] India was one of the worst affected countries in Asia accounting for 182,143 cases, 86,984 recoveries (including one migration) and 5,164 fatalities nationwide till May 2020.[2] The rapidity of the spread coupled with strain on the limited healthcare infrastructure led to various unprecedented measures, such as complete nationwide shutdown which was extended multiple times.
Multiple sclerosis (MS) is a chronic neurological illness that causes a variety of physical and cognitive deficits owing to demyelination in the central nervous system (CNS). MacDougall et al.[3] speculated that there are two ways that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection could impact MS. First, as a direct result of a pro-inflammatory response, it may cause MS relapses in affected patients. Second, it can increase the long-term risk of developing MS in infected individuals by permanently changing the structural and cellular milieu of the CNS. Reyes et al.[4] published an international consensus statement on the management of MS during and after the COVID-19 pandemic. They suggested various strategies and updated recommendations to form a strong task force in managing the impact of this pandemic on MS patients. They recommended use of patient-reported outcome measurements to help with the remote evaluation and decrease non-essential hospital visits for persons with multiple sclerosis (pwMS).
Most of our Indian MS patients are from areas bereft of neurological and rehabilitation facilities. The pandemic further deprived them of access to health care, thereby potentially worsening the quality of life. Our physiotherapy department needed a plan to carefully manage their workforce and the patients with long-standing neurological problems who need routine physiotherapy to avoid a critical deterioration in health during this pandemic. The American Academy of Neurology (AAN) supports the use of telemedicine as a viable and appropriate method to assist in aspects of MS management.[5] The main challenges before us were a) to provide telerehabilitation using technology familiar to the pwMS and b) ensuring adherence to the rehabilitation regimen.
Early on in exercise involvement, adherence is frequently high, but it gradually declines.[6] Hence, strategies to increase exercise adherence especially during pandemics, when physiotherapist is remotely guiding the pwMS, are required. Low exercise adherence has an impact on treatment costs and efficacy. Although the findings were not conclusive, Keytsman et al.[7] did a comprehensive review and meta-analysis of randomised controlled trials (RCTs) on exercise adherence in MS. They indicated that supervised exercise sessions had higher compliance than unsupervised sessions.
Pilates is a useful treatment for MS patients that can enhance physical function and possibly help in lowering self-perceived fatigue. Sánchez-Lastra et al.[8] studied and critically analysed the usefulness of Pilates as a physical therapy for MS patients. Their results suggest that Pilates can be recommended for MS patients as a viable therapy which improves their physical function and may also help lessen the severity of self-perceived fatigue. Pilates can help pwMS recover. Low negative effects and high adherence were noted by few researchers in Pilates.[9,10]
Ghahfarrokhi et al.[11] in their systematic review on home-based exercises in MS suggested home-based exercise therapy (HBET) performed twice to seven times a week is advantageous, practical and secure. Despite this, there were significant flaws, such as (a) poor intervention adherence, which has to be addressed in future research, and (b) failure to take disability-related outcomes into account in HBET trials.
Physiotherapists can use technology-enhanced tools and programmes administered over the Internet or mobile devices with their patients as creative ways to administer home exercise and promote adherence. The usefulness of such therapies in patients with MS is, however, only partially studied. In the course of the COVID-19 pandemic, we aimed to determine whether pwMS adhered more closely to a home exercise regimen provided by a physical therapist that focused on improving their balance and mobility. We developed an easily accessible online physiotherapy package for patients, to guide them through their sessions, and at the same time strive to improve their balance and walking capabilities in a bid to avoid such pandemic-related crises.
Materials and Methods
Twenty-four subjects were enrolled for the study through convenient sampling. The trial was prospectively registered CTRI/2021/04/033267. All the patients were informed about this trial through online webinars held in association with the Multiple Sclerosis Society of India (Mumbai Chapter). Ethical approval was obtained from the Institutional Ethics Committee, BSL eye care, Patna, Bihar (Reg. No ECR/1328/Inst/BR/2019), protocol no BNDC/2021/003. Patients provided written informed consent. Recruitment occurred from May 2021 to September 2021.
Patients
For this single-arm trial, we recruited patients already diagnosed as definite/probable MS by a neurophysician (as per the latest diagnostic criteria) and of both genders a) who could complete 6-minute walk test (assisted/unassisted), b) who had a stable Internet connection and a device to undergo online training programme, c) a caregiver always available alongside during the exercise sessions, and d) who gave informed consent. We excluded the participants a) who could not complete 6-minute walk screening test, b) who had a recent relapse, less than 2 weeks, c) pregnant patients, d) patients with clinically diagnosed severe cognitive impairment and e) patients with a level of ataxia, clinically assessed, that would affect their abilities to perform training.
Physical therapists
A team of three physical therapists with an average of 13 years of clinical experience, working in a private physiotherapy clinic were recruited via word of mouth, contacts and social media. They were provided with a study manual. Before commencing the trial, the therapists were asked to try the therapy on at least five of their non-study participants under supervision.
Procedure
Patients who might be eligible for the study were informed about it through several online platforms run by our centre, Bihar Neuro, in Patna, India. They signed and sent a consent form, filled out online screening and baseline questionnaires in the form of a Google Form and indicated their willingness to participate [Figure 1]. Each participant received instructions on how to complete the various screening tests through telephonic discussions and tutorials on YouTube.
Figure 1.
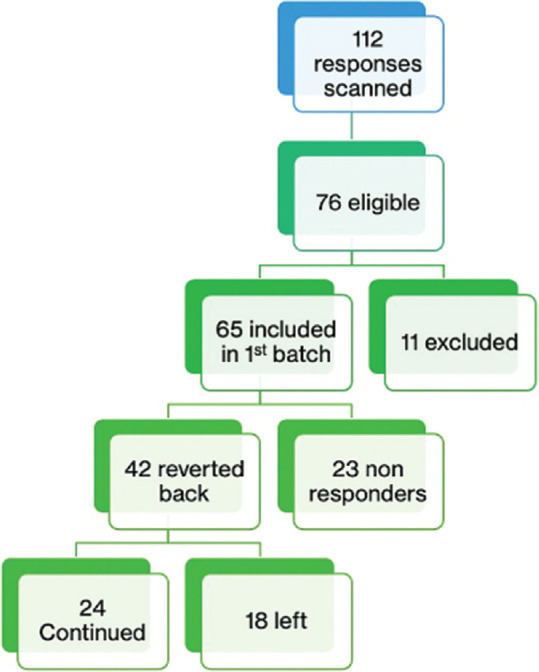
Flow chat of participants recruitment
For a period of 6 weeks, each registered participant received exercise session videos for 3 days per week. The participants were told to watch the video and do the activities at least 10 times during each of the two daily sessions. The participants were invited to upload their performance video over WhatsApp after four practice sessions [Figure 2]. The recordings were provided to two independent therapists at random for review, and they were asked to assess them. Another therapist informed the patient of the findings, and patients’ improvised videos were sought for. These were once more assigned at random to those two therapists for another evaluation, and so forth. This went on until the patient gave his or her best effort.
Figure 2.
(a) Sample patient performance feedback. (b) Sample patient performancecorrection
Outcome measures
The primary outcome was the Timed Up and Go (TUG) test and the 30-Second Sit-to-Stand (30STS) test. Patients were provided video tutorials on how to perform these tests and subsequently recorded their performance. The secondary outcome measure included the Multiple Sclerosis Fatigue Impact Scale (MFIS) and the Multiple Sclerosis Walking Scale-12 (MSWS-12). The consequences of weariness on physical, cognitive and psychosocial functioning are evaluated with this test. There are 21 items in the entire MFIS. The duration of the administration is between 5 and 10 minutes. The patient may typically complete this structured, self-report questionnaire with little to no assistance from the interviewer.
Statistical analysis
All data were analysed using the Statistical Package for the Social Sciences (SPSS for Windows, version 16.0. SPSS Inc., Chicago). A descriptive statistical analysis was conducted; percentages and frequencies were reported for categorical variables, while mean and standard deviation for continuous variables. The primary outcome measures did not follow Gaussian distribution and hence were analysed through the Wilcoxon signed-rank test. MFIS was analysed using paired-sample tests and the P-value ≤ 0.05 was set as a cut-off.
Observations
There were 112 responses overall. All of these were examined by an independent therapist, and after several screenings, only 24 agreed to take part in the study, as depicted in Figure 1.
Only nine participants reported using assistive devices in the form of walker (n = 3), walking stick (n = 5) and slight support of caregiver (n = 1). There were a total of 15 female and nine male participants. The mean age of the participants was 29.67 ± 8.37 years. Only one participant had a family history of MS. The participants had varied disease course with maximum participants (13 patients) having clinically diagnosed relapsing-remitting type [Tables 1 and 2].
Table 1.
Baseline descriptive characteristics of the patients with multiple sclerosis
| Age at diagnosis | Age at symptom/sign | |
|---|---|---|
| N | 24 | 23 |
| Mean | 29.67 | 28.83 |
| Median | 27.50 | 27.00 |
| Std. deviation | 8.365 | 8.211 |
| Minimum | 16 | 16 |
| Maximum | 49 | 48 |
| Percentiles | ||
| 25 | 24.00 | 24.00 |
| 50 | 27.50 | 27.00 |
| 75 | 35.25 | 33.00 |
Table 2.
Current multiple sclerosis disease course among the patients
| Frequency | Percent | |
|---|---|---|
| Primary progressive; | 3 | 12.5 |
| Progressive-relapsing (progressive with superimposed relapses) | 2 | 8.3 |
| Relapsing-remitting | 13 | 54.2 |
| Secondary progressive (relapsing-remitting evolving into progressive); | 6 | 25.0 |
| Total | 24 | 100.0 |
Only nine participants reported using assistive devices in the form of walker (n = 3), walking stick (n = 5) and slight support of caregiver (n = 1).
For primary outcome measures, both TUG test and 30STS showed significant improvements post-intervention [Tables 3 and 4, respectively].
Table 3.
Primary outcome measure performance in patients with MS as measured by pre- and post-TUG and post-STS tests
| PRE.TUG | PRE.30STS | Post.TUG | Post. 30STS | |
|---|---|---|---|---|
| N | 24 | 24 | 24 | 24 |
| Median | 70.00 | 9.00 | 30.00 | 11.00 |
| Percentiles | ||||
| 25 | 18.50 | 5.25 | 15.75 | 7.25 |
| 75 | 120.00 | 11.75 | 91.25 | 14.75 |
Table 4.
Wilcoxon signed-rank test for the Timed Up and Go test and the 30-Second Sit-to-Stand test
| Primary outcome measures | Test | Sig. | Decision | Other values | ||
|---|---|---|---|---|---|---|
| 1. | The median of differences between PRE.TUG and POST.TUG equals 0 | Related-samples Wilcoxon signed-rank test | 0.000 | Reject the null hypothesis | Test statistic | 10.500 |
| Std. error | 28.755 | |||||
| Std. test statistic | -3.651 | |||||
| Asymptotic sig. (2-sided test) | 0.000 | |||||
| 2. | The median of differences between PRE.30STS and POST.30STS equals 0 | Related-samples Wilcoxon signed-rank test | 0.001 | Reject the null hypothesis | Test statistic | 214.000 |
| Std. error | 28.599 | |||||
| Std. test statistic | 3.444 | |||||
| Asymptotic sig. (2-sided test) | 0.001 | |||||
Asymptotic significances are displayed. The significance level is. 05.
There was a significant improvement in the mean difference of pre- and post-values of MFIS, except over its cognitive domain. MSWS-12 also showed significant improvement in post-therapy session [Table 5].
Table 5.
Paired-sample test in secondary outcome measures
| Mean | Paired differences | t | df | Sig. (2-tailed) | |
|---|---|---|---|---|---|
| Pair 1 | MFIS.pre - MFIS.post | 7.7083 | 2.236 | 23 | 0.035 |
| Pair 2 | Physical.pre - Physical.post | 3.0833 | 3.159 | 23 | 0.004 |
| Pair 3 | Cognitive.pre - Cognitive.post | 1.8333 | 1.071 | 23 | 0.295 |
| Pair 4 | Psychosocial.pre - Psychosocial.post | 1.3333 | 2.352 | 23 | 0.028 |
| Pair 5 | MSWS12.pre - MSWS12.post | 7.1250 | 2.187 | 23 | 0.039 |
Overall, the results reflect significant percentage of improvement in post-therapy sessions [Tables 6 and 7].
Table 6.
Percentage of improvement in primary outcome measures
| Variables | Assessments | Percentage of improvement | Z | P | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| PRE | POST | ||||||
|
|
|
||||||
| Median (IQR) | Mean±SD | Median (IQR) | Mean±SD | ||||
| TUG | 70 (18.5 – 120) | 91.25±83.41 | 30 (15.75 – 91.25) | 57.13±57.22 | 37% | -3.65 | 0.001 |
| STS | 9 (5.25 – 11.75) | 9.75±6.87 | 11 (7.25 –14.75) | 11.71±6.79 | 20% | 3.44 | 0.001 |
Table 7.
Percentage of improvement in secondary outcome measures
| Variables | Assessments | Percentage of improvement | t | P | |
|---|---|---|---|---|---|
|
| |||||
| PRE | POST | ||||
|
| |||||
| Mean±SD | |||||
| MFIS | 45.33±16.88 | 37.63±21.27 | 17% | 2.24 | 0.035 |
| Physical | 15.67±4.73 | 12.58±6.07 | 20% | 3.16 | 0.004 |
| Cognitive | 16.58±9.18 | 14.75±10.96 | 11% | 1.07 | 0.295 |
| Psychosocial | 5.29±2.49 | 3.96±2.60 | 25% | 2.35 | 0.028 |
| MSWS-12 | 37.54±14.85 | 30.42±15.93 | 19% | 2.19 | 0.04 |
We tried to compare the performance over primary and secondary outcome measures among those using assistive devices and those who could independently complete 6-minute walk test Table 8 gives descriptive statistics of primary outcome measures in both the groups.
Table 8.
Performance on primary outcome measures in assistive device users and non-users
| Did you use any assistive device while walking? | PRE.TUG | PRE.30STS | Post.TUG | Post. 30STS | ||
|---|---|---|---|---|---|---|
| No | N | 15 | 15 | 15 | 15 | |
| Median | 80.00 | 10.00 | 23.00 | 11.00 | ||
| Percentiles | 25 | 14.00 | 7.00 | 18.00 | 8.00 | |
| 75 | 120.00 | 12.00 | 100.00 | 15.00 | ||
| Yes | N | 9 | 9 | 9 | 9 | |
| Median | 60.00 | 7.00 | 40.00 | 10.00 | ||
| Percentiles | 25 | 20.50 | 2.50 | 13.00 | 5.00 | |
| 75 | 180.00 | 10.50 | 92.50 | 13.50 | ||
Both the groups did not show any difference in their primary outcome measures [Table 9].
Table 9.
TUG and 30STS outcome measure difference among both the groups
| Assistive device used | Primary outcome measures | Test | Sig. | Decision | Z |
|---|---|---|---|---|---|
| No | The median of differences between PRE.TUG and POST.TUG equals 0 | Related-samples Wilcoxon signed-rank test | 0.008 | Reject the null hypothesis | -2.657 |
| Yes | The median of differences between PRE.TUG and POST.TUG equals 0 | Related-samples Wilcoxon signed-rank test | 0.011 | Reject the null hypothesis | -2.533 |
| No | The median of differences between PRE.30STS and POST.30STS equals 0 | Related-samples Wilcoxon signed-rank test | 0.018 | Reject the null hypothesis | 2.360 |
| Yes | The median of differences between PRE.30STS and POST.30STS equals 0 | Related-samples Wilcoxon signed-rank test | 0.011 | Reject the null hypothesis | 2.555 |
Discussion
Our online Pilates-based rehabilitation programme for mobile MS patients demonstrated improved adherence and significant results. This 6-week treatment was relevant and perhaps the first ever offered to MS sufferers in India. Despite the fact that this was urgently needed in light of the COVID-19 pandemic and the lengthening lockdowns, the programme gave patients more self-assurance to follow the recommended exercise regimen.
All 24 patients completed the exercise regimen as planned and continued to upload performance videos for evaluation on a regular basis. This may be attributable to the promotion of patient self-monitoring of exercise sessions, as documented in research by Snook et al.,[12] which may have led to potential patient behavioural changes.
Greater confidence to exercise may have been assisted by the availability of thorough exercise instructions and videos, clear exercise dose, preparatory motor imagery of the exercises and the ability to report any exercise difficulty to the physical therapist remotely. In contrast, higher levels of physical activity have been linked to higher levels of self-efficacy in pwMS.[13] In patients with MS, low self-efficacy has been recognised as a barrier to both physical therapy treatment adherence and home exercise adherence.[14] Therefore, increased self-efficacy might have influenced our findings. In fact, the research group showed a noticeable improvement on the MFIS.
It is important to note that even though nine patients needed assistive equipment during the TUG tests at both timelines, they all displayed significant gains in this parameter after 6 weeks of therapy. Thus, regardless of ambulation mode, therapeutic results are evident.
Future areas of research are indicated from our study’s findings. The physical capabilities of the patients can be evaluated in more ways, both objectively and subjectively, using online tutorials. This would enable a more thorough examination of the effects of online-based exercise programming systems and other technologies that can influence adherence, while the patient is comfortable in their own home, is energy-efficient for them physically and mentally and, most importantly, lessen the burden on the caretakers while also enhancing the quality of life for such patients. This is crucial for chronic illnesses where consistent exercise routine is expected. To ascertain which patient subgroups are most likely to respond and by what mechanism interventions promote adherence, future RCTs are required.
An online-based exercise programming system improved home exercise adherence and confidence to undertake a prescribed exercise programme for 6 weeks in patients with MS. Additionally, –COVID-19 has shown us that life always finds a way to thrive, function and enjoy itself. However, it needs to be considered that online mode of imparting requires a lot of motivation for the patient’s and caregiver’s end to ensure that the classes are undertaken in the prescribed format and for required duration. The outcome of telerehabilitation is largely dependent on patient’s support system and willingness.
Key points
Telerehabilitation has significant benefits by offering greater access to services and avoidance of needless frequent commuting to therapy centres.
Telerehabilitation aids in training the patients in their home environment rather than in clinical setting.
Such remote therapy sessions help to offload the caregivers’ burden by providing flexible therapy timings.
However, caution needs to be practised while using telerehabilitation as regular performance feedback to patients is necessary.
For an absolute clear picture on patient’s abilities, a few initial physical examination sessions are warranted.
Key message/Impact statement
Future patient management will be largely dependent on telerehabilitation. Alternate methods of providing therapy for treating chronic diseases that call for frequent therapy sessions should be pursued.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We would like to thank all our MS patients for participating in this study. We extend our gratitude to the Department of Biostatistics, National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, for providing assistance in statistical analysis of the study.
References
- 1.Andrews MA, Areekal B, Rajesh KR, Krishnan J, Suryakala R, Krishnan B, et al. First confirmed case of COVID-19 infection in India: A case report. Indian J Med Res. 2020;151:490–2. doi: 10.4103/ijmr.IJMR_2131_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hazra D, Chandy GM, Thanjavurkar A, Gunasekaran K, Nekkanti AC, Pal R, et al. A clinico-epidemiological profile, coinfections and outcome of patients with influenza like illnesses (ILI) presenting to the emergency department during the COVID-19 pandemic. J Family Med Prim Care. 2023;12:672–8. doi: 10.4103/jfmpc.jfmpc_1705_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MacDougall M, El-Hajj Sleiman J, Beauchemin P, Rangachari M. SARS-CoV-2 and multiple sclerosis: Potential for disease exacerbation. Front Immunol. 2022;13:871276. doi: 10.3389/fimmu.2022.871276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reyes S, Cunningham AL, Kalincik T, Havrdová EK, Isobe N, Pakpoor J, et al. Update on the management of multiple sclerosis during the COVID-19 pandemic and post pandemic: An international consensus statement. J Neuroimmunol. 2021;357:577627. doi: 10.1016/j.jneuroim.2021.577627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yeroushalmi S, Maloni H, Costello K, Wallin MT. Telemedicine and multiple sclerosis: A comprehensive literature review. J Telemed Telecare. 2020;26:400–13. doi: 10.1177/1357633X19840097. [DOI] [PubMed] [Google Scholar]
- 6.Dennett R, Madsen LT, Connolly L, Hosking J, Dalgas U, Freeman J. Adherence and drop-out in randomized controlled trials of exercise interventions in people with multiple sclerosis: A systematic review and meta-analyses. Mult Scler Relat Disord. 2020;43:102169. doi: 10.1016/j.msard.2020.102169. [DOI] [PubMed] [Google Scholar]
- 7.Keytsman C, Van Noten P, Verboven K, Van Asch P, Eijnde BO. Periodized versus classic exercise therapy in multiple sclerosis: A randomized controlled trial. Mult Scler Relat Disord. 2021;49:102782. doi: 10.1016/j.msard.2021.102782. [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Lastra MA, Martínez-Aldao D, Molina AJ, Ayán C. Pilates for people with multiple sclerosis: A systematic review and meta-analysis. Mult Scler Relat Disord. 2019;28:199–212. doi: 10.1016/j.msard.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Torres-Pareja M, Sánchez-Lastra MA, Iglesias L, Suárez-Iglesias D, Mendoza N, Ayán C. Exercise interventions for improving flexibility in people with multiple sclerosis: A systematic review and meta-analysis. Medicina (Kaunas) 2019;55:726. doi: 10.3390/medicina55110726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marques KAP, Trindade CBB, Almeida MCV, Bento-Torres NVO. Pilates for rehabilitation in patients with multiple sclerosis: A systematic review of effects on cognition, health-related physical fitness, general symptoms and quality of life. J Bodyw Mov Ther. 2020;24:26–36. doi: 10.1016/j.jbmt.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Ghahfarrokhi MM, Banitalebi E, Negaresh R, Motl RW. Home-based exercise training in multiple sclerosis: A systematic review with implications for future research. Mult Scler Relat Disord. 2021;55:103177. doi: 10.1016/j.msard.2021.103177. [DOI] [PubMed] [Google Scholar]
- 12.Snook EM, Motl RW. Physical activity behaviors in individuals with multiple sclerosis: Roles of overall and specific symptoms, and self-efficacy. J Pain Symptom Manage. 2008;36:46–53. doi: 10.1016/j.jpainsymman.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Motl RW, McAuley E, Snook EM, Gliottoni RC. Physical activity and quality of life in multiple sclerosis: intermediary roles of disability, fatigue, mood, pain, self-efficacy and social support. Psychol Health Med. 2009;14:111–24. doi: 10.1080/13548500802241902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikula P, Timkova V, Fedicova M, Szilasiova J, Nagyova I. Self-management, self-esteem and their associations with psychological well-being in people with multiple sclerosis. Multi Scler Relat Disord. 2021;53:103069. doi: 10.1016/j.msard.2021.103069. [DOI] [PubMed] [Google Scholar]