Abstract
Background
Liver disease causes over two million deaths annually worldwide, comprising approximately 4% of all global fatalities. We aimed to analyze liver disease-related mortality trends from 1990 to 2021 using the World Health Organization (WHO) Mortality Database and forecast global liver disease-related mortality rates up to 2050.
Methods
This study examined age-standardized liver disease-related death rates from 1990 to 2021, employing data from the WHO Mortality Database across 112 countries across five continents. The rates over time were calculated using a locally weighted scatter plot smoother curve, with weights assigned based on the population of each country. Furthermore, this study projected liver disease-related mortality rates up to 2050 using a Bayesian age-period-cohort (BAPC) model. Additionally, a decomposition analysis was conducted to discern influencing factors such as population growth, aging, and epidemiological changes.
Results
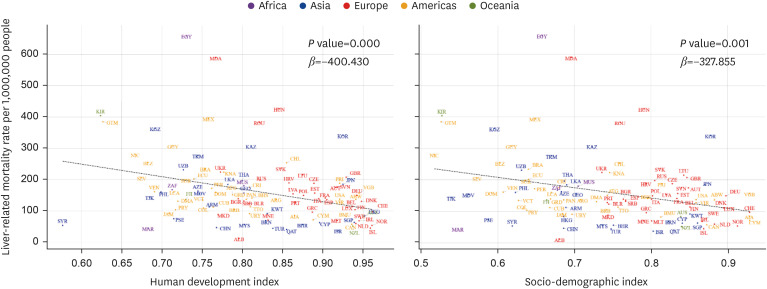
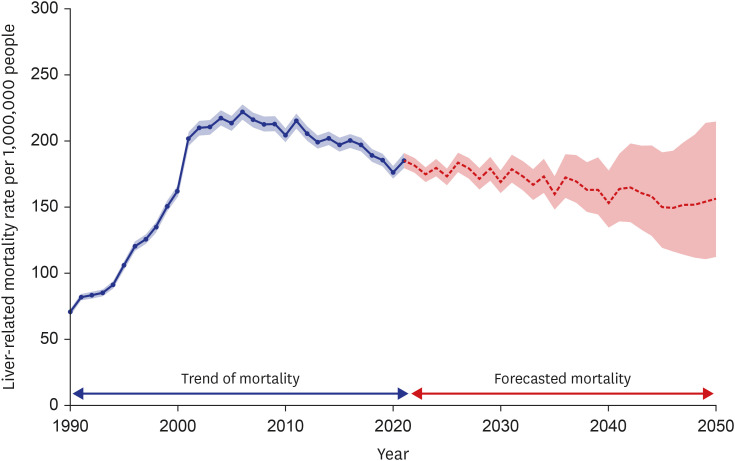
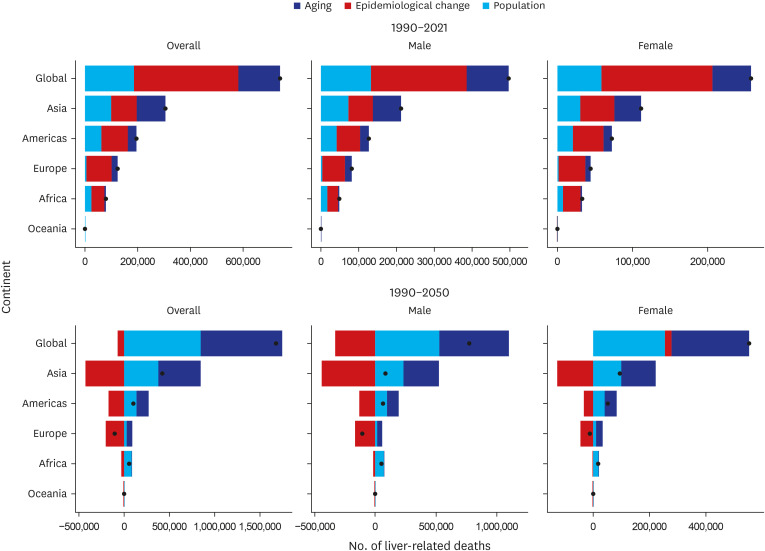
The estimated global age-standardized liver disease-related mortality rates surged significantly from 1990 to 2021 across 112 countries, rising from 103.4 deaths per 1,000,000 people (95% confidence interval [CI], 88.16, 118.74) in 1990 to 173.0 deaths per 1,000,000 people (95% CI, 155.15, 190.95) in 2021. This upward trend was particularly pronounced in low- and middle-income countries, in Africa, and in populations aged 65 years and older. Moreover, age-standardized liver disease-related mortality rates were correlated with a lower Human Development Index (P < 0.001) and sociodemographic index (P = 0.001). According to the BAPC model, the projected trend indicated a sustained and substantial decline in liver disease-related mortality rates, with an estimated decrease from 185.08 deaths per 1,000,000 people (95% CI, 179.79, 190.63) in 2021 to 156.29 (112.32, 214.77) in 2050. From 1990 to 2021, age-standardized liver disease-related deaths surged primarily due to epidemiological changes, whereas from 1990 to 2050, the impact of population aging and growth became the primary contributing factors to the overall increase.
Conclusion
Global age-standardized liver disease-related mortality has increased significantly and continues to emerge as a crucial global public health issue. Further investigation into liver disease-related mortality rates in Africa is needed, and updating policies is necessary to effectively manage the global burden of liver disease.
Keywords: Liver Disease, Mortality, WHO Mortality Database, Global Trend, Prediction Model
Graphical Abstract
INTRODUCTION
Liver disease, encompassing conditions such as cirrhosis, viral hepatitis, and liver cancer, contributes to over two million deaths each year globally, representing approximately 4% of all deaths worldwide, equating to one in every 25 deaths.1 Chronic liver disease and its associated cirrhosis contribute to approximately one million deaths annually, while liver cancer accounts for 600,000 to 900,000 deaths.2 Liver disease ranks as the 11th leading cause of death and the 15th leading cause of disability-associated life-years globally.1 In addition, adults with liver disease experience greater financial distress compared to those without liver disease, with liver disease-related expenditure reaching $32.5 billion in the US in 2016.3
The 2016 World Health Organization (WHO) Global Health Sector Strategy (GHSS) outlined a path for eradicating viral hepatitis as a public health issue by 2030.4 As a result, mortality rates stemming from hepatitis B virus (HBV)-related conditions decreased across all age brackets, with age-standardized mortality rates also witnessing a decline during this timeframe.5 Similarly, the mortality rate associated with hepatitis C virus (HCV)-related conditions also decreased.6 Nevertheless, the African continent continues to grapple with a substantial burden of chronic liver diseases, which stem from various factors including persistent viral hepatitis infections, elevated levels of alcohol consumption, and metabolic dysfunction-associated steatotic liver disease (MASLD).7 Additionally, the prevalence of alcoholic liver disease (ALD) is on the rise in the US, Europe, and the Asia-Pacific region, especially among younger individuals.8,9,10,11,12 Moreover, the worldwide prevalence of non-alcoholic fatty liver disease (NAFLD) is escalating rapidly.13 Consequently, there has been a significant increase in the global burden of cirrhosis associated with NAFLD.
Previous studies on the global burden of chronic liver disease and cirrhosis utilized data from the Global Burden of Disease Study (GBD) 2017.14 The GBD data is widely used in research due to its advantages, such as providing estimates for missing data.15 However, it often relies on meta-analyses and primarily uses statistical modelling in regions with limited data. This approach increases dependence on estimates rather than actual data, thereby raising the potential for errors.16,17 In contrast, WHO data, derived from the direct collection of information from national reports, enhances data reliability and can be utilized to improve the precision of research studies.
Our study aimed to utilize the WHO Mortality Database to report on liver disease-related mortality from 1990 to 2021 across five continents, covering 112 countries, by age, sex, and national-level indicators (income level classified by World Bank Group country, Human Development Index [HDI], and Socio-demographic Index [SDI]). Additionally, it aimed to predict the global age-standardized liver disease-related mortality up to 2050 and investigate the relative contributions of population growth, aging, and epidemiological factors to liver disease-related mortality.
METHODS
Following the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) guidelines (Supplementary Data 1), our study explored international trends in liver disease-related mortality rates from 1990 to 2021 using the WHO Mortality Database from 112 countries across five continents. To forecast liver disease-related mortality rates up to 2050, we fitted Bayesian age-period-cohort (BAPC) models to past trends.18
Data sources of liver disease-related mortality and population demographics
The primary data source for our study was the WHO Mortality Database. This database contains comprehensive annual mortality rates, as reported by the civil registration systems of WHO member nations, categorized by age, sex, and cause of death. We extracted both the crude number of liver disease-related deaths and the corresponding population estimates from all available countries across all sex and age groups.19
To be included in our study, the data required a minimum of 10 years of complete data from 1990 to 2021. The causes of death were categorized using the International Statistical Classification of Diseases and Related Health Problems (ICD) codes. Liver disease-related deaths were identified using the following metrics: ICD-8 (70, 571, 155, or 1977–1978) and ICD-9 (70, 155, 571, 1,552, S347, or 230.8), and B15-B19, C22, or K70-76 in ICD-10 (Supplementary Table 1). United Nations dataset was used to derive the population data for the countries included in this study. Data collection were independently performed and verified by two authors (Hyeri Lee and Soeun Kim), using Python software (version 3.11.4; Python Software Foundation, Wilmington, DE, USA).
Statistical analysis
To account for differences in population structure across countries and over time, age-standardized liver disease-related mortality rates were calculated. These rates were evaluated for specific age groups: under 25 years, 25–64 years (in 10-year increments), and 65 years and above, using the WHO World Standard Population for standardization.19,20 To ensure accuracy in the mortality calculation, the execution of this process was cross-verified by two independent researchers, Hyeri Lee and Soeun Kim. It is important to note that all instances of zero mortality were true zeros, authentically representing the absence of liver disease-related deaths in specific years and age groups.
For trend analysis, we utilized a locally weighted scatter plot smoother (LOESS) curve to illustrate a smoothed curve of global trends in liver disease-related mortality for 112 countries, with adjustments for each population (Supplementary Table 2); the smoothing parameter was set using the default method of the software. SAS software (version 9.4, SAS Inc., Cary, NC, USA) was used to produce the LOESS curves and their 95% confidence intervals (CIs).19 Additionally, descriptive statistics were processed, with continuous variables as means and categorical variables as counts and percentages. Additional explanations of the methodology can be found in the Supplementary Data 2.
Our study employed an income-based classification to analyze the global age-standardized liver disease-related mortality rates over different time intervals. Countries were categorized according to World Bank income thresholds. Those with a Gross National Income (GNI) per capita above $13,846 were categorized as high-income countries (HICs), whereas those below this threshold were categorized as low-and middle-income countries (LMICs), as detailed in Supplementary Table 3. The stratification in our study aimed to identify distinct characteristics among countries by analyzing their economic profiles. This involves comparing countries with identical GNI levels to understand disparities in their HDI outcomes.21 The HDI, formulated by the United Nations, assesses human development based on factors such as health, knowledge, and living standards.22 Countries were categorized based on their HDI values: an HDI of 0.9 or higher indicates a very high development level, 0.8 to 0.89 signifies a high level of development, and 0.7 and 0.79 indicates a middle-level development (Supplementary Table 4).16 This categorization highlights that some nations with comparable GNI levels may show varying human development levels, as illustrated by the HDI distinctions.
Correlation analysis
To explore the correlation between the country-specific average liver disease-related mortality rate and various socioeconomic indicators, we utilized two indices: HDI and SDI. Using Python software, our study utilized the generation of scatter plots and the application of linear analyses for visualization and correlation, respectively.16 The HDI measures human development through health, knowledge, and living standards, while the SDI, from the GBD, focuses on developmental status with components such as income, education, and birth rates.16,17 These indices are normalized from 0 to 1, with higher values indicating greater development or equality.22,23,24 The correlation analysis results are presented with β coefficients and P values.
BAPC statistical modeling
To forecast liver disease-related mortality rates from 2022 to 2050 across various sex and age groups in 112 countries, we utilized BAPC models, developed through the "bamp" package in R. These models are based on the principle that the logit risk of death in a specific age group and period is a linear function accounting for the combined effects of age, period, and cohort factors. BAPC models, known for their flexibility, accommodate various constants or linear time trends, including random walks of the first or second order. Such flexibility allows for the incorporation of heterogeneity and the consideration of various model structures. For each disease and sex across all 112 countries, the most optimal model structure was selected based on the root mean square errors, with lower root mean square error values indicating higher model precision and appropriateness.25 The outcomes of the BAPC models are presented as median values with 95% CIs, based on the posterior distributions of the model. We assumed that the uncertainty in these model outputs, particularly when aggregating data from subnational to national levels, was uncorrelated; this assumption with regards to the uncertainty is important to accurately interpret the results. BAPC statistical modeling was performed using R statistical software (version 4.1.2; R Foundation, Vienna, Austria). Further statistical analyses of this study are presented in Supplementary Data 2.
Decomposition method for differences in liver disease-related deaths in the period
To discern the varying impacts of population growth, aging, and epidemiological change (age-specific mortality rate) on liver disease-related deaths, our study employed a decomposition analysis; it utilizes data on population size, age-specific mortality rates, and the proportion of the population within specific age groups in comparing the reference year (i.e., 1990 [scenario one], 2021 [scenario two], and 2050 [scenario three] in the present study).18,26 We then estimated the change due to population growth by subtracting 1990 actual deaths from scenario one, the change due to population ageing by calculating the differences between scenario two and scenario one, and the change due to age-specific mortality rate, by subtracting scenario two from 2021 actual deaths. We conducted the same calculation for the scenario one and scenario three.27
Additionally, our decomposition method, unlike other decomposition methods which might have possibility of being sensitive to the choice of decomposition order and the reference group, overcomes this limitation and avoids inconsistent results from identical data sets.18,26 After segmenting the data by sex and World Bank income level, the decomposition method was applied to calculate the absolute contribution of three factors—population growth, aging, and epidemiological change—to liver disease-related mortality trends. This process distinguishes between positive and negative contributions, presented as increases and decreases in total deaths, respectively. Decomposition analyses were performed using R statistical software. The detailed information is provided in Supplementary Data 2.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Kyung Hee University (KHSIRB-23-085). The requirement for written consent was waived by the ethics committee owing to the population-level dataset.
RESULTS
Age-standardized liver disease-related mortality rates from the WHO Mortality Database were available for 112 countries across five continents, from 1990 to 2021 (Table 1, Supplementary Table 5). Among the 112 countries analyzed, 59 (52.6%) were classified as HICs and 53 (47.3%) were categorized as LMICs (Supplementary Table 3). Additionally, 67 (59.8%) were classified as very high HDI countries, 34 (30.3%) were classified as high HDI countries, and 11 (9.8%) were categorized as medium HDI countries (Supplementary Table 4). Africa comprises four countries, Europe 38 countries, Asia 27 countries, the Americas 39 countries, and Oceania 4 countries.
Table 1. LOESS smoothed liver-related mortality rates (per 1,000,000 people) across variables in 112 countries, 1990–2021.
| Variables | Year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | ||
| Global | 103.45 (88.16, 118.74) | 133.45 (125.41, 141.48) | 169.26 (160.90, 177.62) | 178.18 (169.94, 186.42) | 178.86 (170.55, 187.17) | 179.98 (172.09, 187.87) | 179.09 (170.63, 187.55) | 178.04 (168.43, 187.64) | 176.98 (165.76, 188.21) | 175.67 (162.44, 188.91) | 174.36 (158.87, 189.85) | 173.05 (155.15, 190.95) | |
| Sex | |||||||||||||
| Male | 148.28 (129.79, 166.77) | 194.61 (184.34, 204.87) | 238.47 (228.25, 248.69) | 254.32 (244.29, 264.35) | 255.56 (245.39, 265.73) | 255.52 (244.95, 266.08) | 255.12 (243.39, 266.86) | 254.75 (241.49, 268.02) | 254.38 (239.33, 269.43) | 253.89 (236.81, 270.98) | 253.40 (234.12, 272.68) | 252.91 (231.32, 274.49) | |
| Female | 62.43 (50.50, 74.35) | 77.41 (71.11, 83.70) | 104.73 (98.12, 111.34) | 110.64 (104.10, 117.17) | 112.12 (105.56, 118.69) | 114.97 (108.62, 121.31) | 114.54 (107.91, 121.18) | 112.49 (105.45, 119.52) | 110.43 (112.13, 118.73) | 108.04 (97.84, 118.25) | 105.66 (93.14, 118.17) | 103.27 (88.23, 118.32) | |
| Income | |||||||||||||
| HICs | 100.22 (87.11, 113.33) | 124.03 (116.57, 131.48) | 145.91 (138.90, 152.91) | 154.34 (147.33, 161.36) | 149.01 (141.95, 156.06) | 143.05 (135.33, 150.78) | 141.93 (133.35, 150.51) | 140.81 (131.20, 150.41) | 139.68 (128.92, 150.44) | 138.60 (126.54, 150.66) | 137.51 (124.07, 150.95) | 136.43 (121.55, 151.31) | |
| LMICs | 109.24 (87.37, 131.11) | 147.55 (134.60, 160.49) | 183.30 (172.46, 194.15) | 205.43 (194.25, 216.61) | 215.96 (205.56, 226.35) | 222.65 (209.49, 235.80) | 223.57 (209.05, 238.08) | 224.37 (208.25, 240.49) | 225.17 (207.26, 243.08) | 225.97 (206.15, 245.80) | 226.78 (204.94, 248.61) | 227.58 (203.66, 251.50) | |
| Human Development Index | |||||||||||||
| Very high human development | 95.47 (83.36, 107.58) | 118.58 (111.55, 125.61) | 140.83 (134.17, 147.50) | 150.45 (143.91, 156.98) | 149.60 (143.04, 156.17) | 150.02 (142.97, 157.07) | 150.26 (142.46, 158.07) | 150.53 (141.80, 159.26) | 150.80 (141.02, 160.57) | 151.11 (140.16, 162.06) | 151.43 (139.23, 163.63) | 151.75 (138.23, 165.26) | |
| High human development | 121.14 (93.96, 148.32) | 156.71 (139.85, 173.57) | 190.51 (176.72, 204.31) | 212.21 (198.02, 226.40) | 215.73 (202.58, 228.88) | 211.79 (194.23, 229.35) | 210.64 (191.37, 229.90) | 209.29 (188.06, 230.52) | 207.94 (184.57, 231.31) | 206.60 (180.96, 232.23) | 205.25 (177.25, 233.25) | 203.90 (173.46, 234.35) | |
| Medium human development | 122.57 (77.26, 167.88) | 173.00 (145.95, 200.04) | 220.14 (197.39, 242.90) | 249.80 (228.03, 271.58) | 276.79 (254.34, 299.23) | 312.15 (280.08, 344.21) | 319.84 (284.42, 355.26) | 327.53 (288.45, 366.62) | 335.23 (292.23, 378.22) | 342.92 (295.85, 390.00) | 350.62 (299.32, 401.92) | - | |
| Geographical areas | |||||||||||||
| Africa | 116.98 (−21.65, 255.62) | 165.07 (66.59, 263.55) | 211.62 (142.70, 280.54) | 257.41 (198.97, 315.85) | 297.87 (239.26, 356.47) | 332.68 (251.90, 413.47) | 339.56 (252.14, 426.98) | 346.50 (251.79, 441.21) | 353.45 (251.03, 455.86) | 360.39 (249.94, 470.85) | 367.34 (248.58, 486.10) | 374.28 (247.00, 501.56) | |
| Asia | 136.58 (113.41, 159.74) | 141.73 (125.39, 158.08) | 146.31 (134.44, 158.18) | 150.65 (139.21, 162.09) | 152.79 (141.12, 164.45) | 154.98 (139.02, 170.93) | 155.43 (138.26, 172.60) | 155.98 (137.47, 174.49) | 156.52 (136.60, 176.45) | 157.07 (135.67, 178.47) | 157.62 (134.70, 180.54) | 158.16 (133.68, 182.65) | |
| Europe | 106.36 (87.59, 125.12) | 128.96 (117.82, 140.10) | 151.94 (142.32, 161.56) | 172.88 (162.72, 183.04) | 179.44 (170.09, 188.79) | 175.92 (164.45, 187.39) | 174.81 (162.19, 187.43) | 173.43 (159.44, 187.41) | 172.04 (156.52, 187.56) | 170.65 (153.48, 187.83) | 169.27 (150.35, 188.19) | 167.88 (147.15, 188.61) | |
| Americas | 104.84 (82.53, 127.14) | 121.25 (107.36, 135.14) | 201.35 (187.92, 214.79) | 194.40 (181.40, 207.40) | 185.55 (172.50, 198.59) | 189.07 (176.41, 201.73) | 188.03 (174.96, 201.10) | 185.53 (172.19, 198.88) | 182.27 (166.56, 197.98) | 178.79 (159.16, 198.42) | 175.29 (150.63, 199.94) | 171.78 (141.53, 202.04) | |
| Oceania | 107.20 (22.28, 192.12) | 134.75 (86.42, 183.09) | 150.84 (104.89, 196.80) | 124.60 (81.23, 167.96) | 100.55 (54.30, 146.79) | 99.25 (37.13, 161.37) | 99.26 (30.47, 168.05) | 99.27 (23.11, 175.43) | 99.28 (15.22, 183.34) | 99.29 (6.95, 191.63) | 99.30 (−1.61, 200.21) | 99.31 (−10.40, 209.01) | |
| Age group, yr | |||||||||||||
| < 25 | 5.31 (3.82, 6.80) | 5.88 (5.05, 6.71) | 7.82 (6.93, 8.70) | 5.86 (4.98, 6.74) | 5.36 (4.48, 6.23) | 4.58 (3.75, 5.41) | 4.42 (3.56, 5.27) | 4.20 (3.33, 5.06) | 3.97 (2.97, 4.97) | 3.75 (2.50, 4.99) | 3.50 (1.94, 5.06) | 3.25 (1.33, 5.16) | |
| 25–34 | 34.78 (29.93, 39.63) | 37.78 (34.84, 40.72) | 40.31 (37.89, 42.73) | 40.41 (37.82, 43.01) | 36.96 (34.61, 39.32) | 31.96 (28.93, 34.99) | 30.89 (27.55, 34.23) | 29.78 (26.07, 33.49) | 28.67 (24.55, 32.80) | 27.56 (22.99, 32.13) | 26.45 (21.42, 31.49) | 25.35 (19.83, 30.86) | |
| 35–44 | 141.05 (128.60, 153.50) | 142.96 (134.96, 150.96) | 144.22 (138.02, 150.43) | 141.01 (134.50, 147.52) | 131.62 (125.52, 137.73) | 121.45 (113.27, 129.64) | 119.40 (110.48, 128.32) | 117.29 (107.53, 127.05) | 115.18 (104.52, 125.84) | 113.07 (101.46, 124.68) | 110.96 (98.36, 123.56) | 108.85 (95.24, 122.47) | |
| 45–54 | 336.84 (310.50, 363.17) | 346.40 (329.48, 363.32) | 354.93 (341.81, 368.06) | 356.33 (342.56, 370.09) | 338.91 (325.78, 352.03) | 313.39 (296.03, 330.76) | 308.20 (289.21, 327.18) | 302.78 (281.94, 323.62) | 297.37 (274.52, 320.22) | 291.96 (266.98, 316.93) | 286.54 (259.35, 313.74) | 281.13 (251.65, 310.61) | |
| 55–64 | 564.48 (517.03, 611.93) | 599.76 (570.38, 629.14) | 631.48 (607.47, 655.49) | 643.95 (619.14, 668.76) | 632.87 (610.03, 655.70) | 613.71 (583.59, 643.83) | 609.59 (576.55, 642.63) | 605.42 (569.02, 641.82) | 601.25 (561.17, 641.32) | 597.08 (553.10, 641.05) | 592.90 (544.85, 640.96) | 588.73 (536.47, 640.99) | |
| ≥ 65 | −16.02 (−113.33, 81.30) | 149.71 (91.85, 207.58) | 587.95 (532.76, 643.13) | 653.36 (598.53, 708.20) | 741.94 (687.13, 796.75) | 867.73 (809.99, 925.47) | 879.36 (825.98, 932.75) | 876.46 (822.51, 930.41) | 869.48 (807.01, 931.95) | 861.53 (783.89, 939.16) | 851.10 (753.67, 948.53) | 840.67 (720.97, 960.38) | |
Values are presented as LOESS smoothed rate (95% confidence interval).
LOESS = locally weighted scatter plot, HIC = high-income country, LMIC = low- and middle-income country.
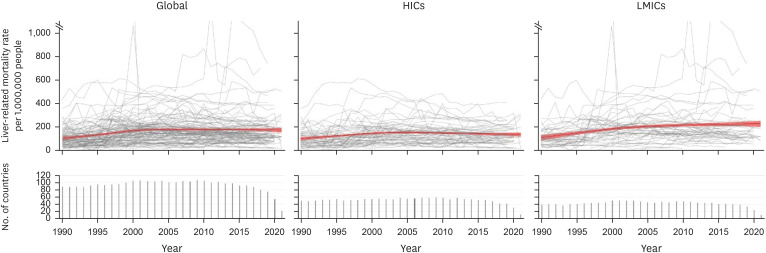
The LOESS smoothed rate for liver disease-related mortality was 103.4 deaths per 1,000,000 people (95% CI, 88.16, 118.74) in 1990 and 173.0 deaths per 1,000,000 people (95% CI, 155.15, 190.95) in 2021 (Fig. 1). The liver disease-related mortality rate in LMICs notably increased, rising from 109.2 deaths per 1,000,000 people (95% CI, 87.37, 131.11) in 1990 to 227.5 deaths per 1,000,000 people (95% CI, 203.66, 251.50) in 2021 (Fig. 1). An increase in liver disease-related mortality in LMICs was observed, irrespective of sex. In men, the rate rose from 155.11 deaths per 1,000,000 people (95% CI, 126.20, 1,184.03) in 1990 to 325.4 deaths per 1,000,000 people (95% CI, 293.83, 357.09) in 2021. Similarly, in women, the rate increased from 65.78 deaths per 1,000,000 people (95% CI, 48.36, 83.19) in 1990 to 143.18 deaths per 1,000,000 people (95% CI, 123.42, 162.93) in 2021 (Supplementary Figs. 1 and 2, Supplementary Tables 6 and 7).
Fig. 1. Age-standardized liver-related mortality rates for the global, HICs, and LMICs population among 112 countries for the years 1990–2021. The LOESS mortality rates with 95% confidence levels, weighted by country population, are shown in red. HICs included 59 countries, including Anguilla, Antigua and Barbuda, Aruba, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Chile, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Guyana, Hong Kong SAR, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Netherlands, New Zealand, Norway, Panama, Poland, Portugal, Puerto Rico, Qatar, Republic of Korea, Romania, Saint Kitts and Nevis, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America, Uruguay, and Virgin Islands (USA). LMICs included 53 countries, including Albania, Argentina, Armenia, Azerbaijan, Belarus, Belize, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Egypt, El Salvador, Fiji, Georgia, Grenada, Guatemala, Jamaica, Kazakhstan, Kiribati, Kyrgyzstan, Malaysia, Maldives, Mauritius, Mexico, Montenegro, Morocco, Nicaragua, North Macedonia, Occupied Palestinian Territory, Paraguay, Peru, Philippines, Republic of Moldova, Russian Federation, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Sri Lanka, Suriname, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, Ukraine, Uzbekistan, and Venezuela.
HIC = high-income country, LMIC = low- and middle-income country, LOESS = locally weighted scatterplot smoother.
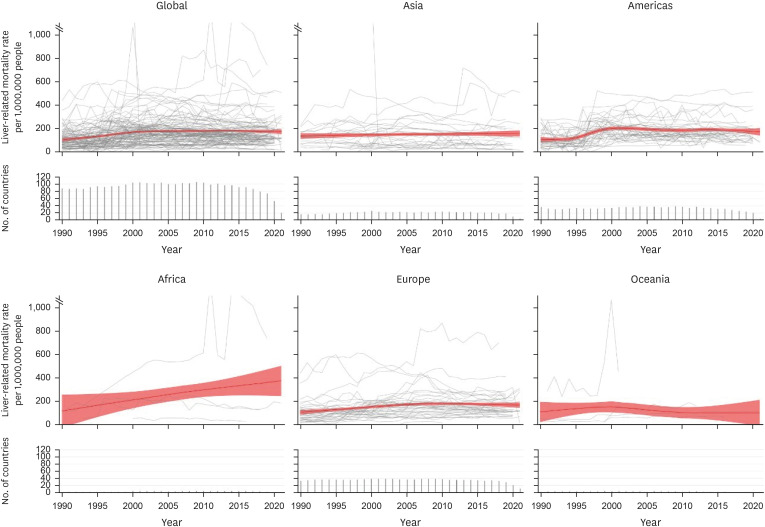
Fig. 2 shows the age-standardized liver disease-related mortality rates for 112 countries across five continents, from 1990 to 2021. The LOESS smoothed curves of liver disease-related mortality rates were overwhelmingly highest in Africa (116.98 deaths per 1,000,000 people [95% CI, −21.65, 255.62] in 1990 to 374.28 deaths per 1,000,000 people [247.00, 501.56] in 2021), while there was an increasing trend in Asia, America, and Europe (Asia: 136.58 [95% CI, 113.41, 159.74] in 1990 to 158.16 deaths per 1,000,000 people [95% CI, 133.68, 182.65] in 2021; America: 104.84 [82.53, 127.14] in 1990 and 171.78 [141.53, 202.04] in 2021; Europe: 106.36 [87.59, 125.12] in 1990 and 167.88 [147.15, 188.61] in 2021). However, Oceania exhibited a decreasing trend (Oceania: 107.20 deaths per 1,000,000 people) (Table 1).
Fig. 2. Age-standardized liver-related mortality rates across the globe and five continents among 112 countries. The LOESS mortality rates with 95% confidence levels, weighted by country population, are shown in red. Africa includes 4 countries: Egypt, Mauritius, Morocco, and South Africa. Asia includes 27 countries: Armenia, Azerbaijan, Bahrain, Brunei, Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan. Americas includes the 39 countries, including Anguilla, Antigua and Barbuda, Argentina, Aruba, Bahamas, Barbados, Belize, Bermuda, Brazil, British Virgin Islands, Canada, Cayman Islands, Chile, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Guyana, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and Grenadines, Suriname, Trinidad and Tobago, United States of America, Virgin Islands (USA), Uruguay, and Venezuela. Europe includes 38 countries: Albania, Austria, Belgium, Bulgaria, Croatia, the Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, the Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and the United Kingdom. Oceania includes 4 countries: including Australia, Fiji, Kiribati, and New Zealand.
LOESS = locally weighted scatterplot smoother.
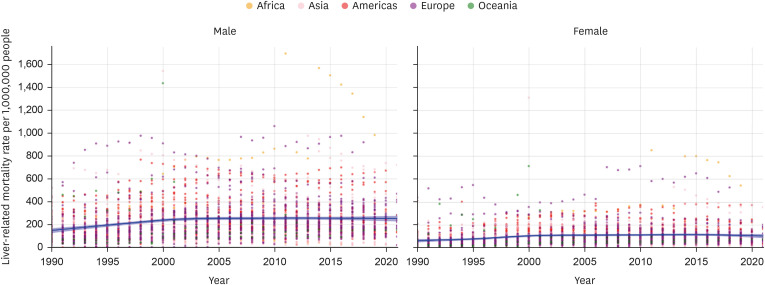
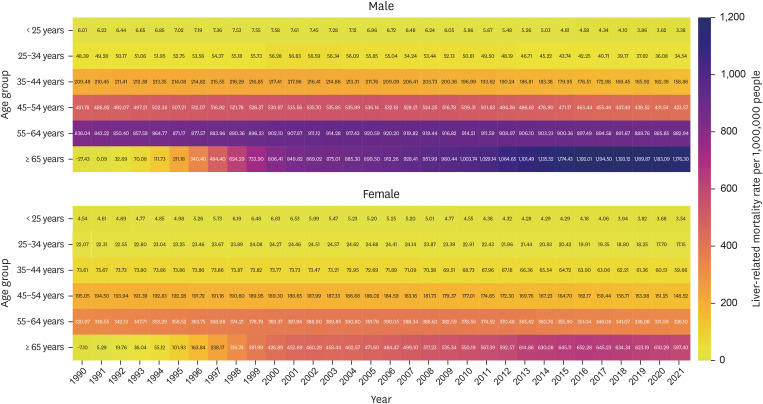
In the global population, the age-standardized liver disease-related mortality rates were higher in men than in women (Fig. 3 and Table 1). This pattern was consistently observed across Africa, Asia, America, Europe, and Oceania (Supplementary Figs. 3, 4, 5, 6, 7). In older populations, particularly those aged 65 and older, LOESS smoothed liver disease-related mortality rates increased sharply (above 65 years: −16.02 [95% CI, −113.33, 81.30] deaths per 1,000,000 people in 1990 and 840.67 [720.97, 960.38] in 2021; Table 1). An increasing trend associated with age was observed irrespective of sex and occurred in both HICs and LMICs across all HDI groups and on all continents (Fig. 4, Supplementary Figs. 8, 9, 10, 11, 12, Supplementary Tables 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25). The age group of 55–64 exhibited a slight increasing trend, while those below the age of 55 showed a decrease. Additional analyses for specific age and sex subgroups showed similar patterns (Supplementary Tables 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25).
Fig. 3. Age-standardized liver-related mortality rates for the global population by sex among 112 countries, 1990–2021. The LOESS mortality rates with 95% confidence levels, weighted by country population, are shown in blue. Africa includes 4 countries: Egypt, Mauritius, Morocco, and South Africa. Asia includes 27 countries: Armenia, Azerbaijan, Bahrain, Brunei, Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan. Americas includes the 39 countries, including Anguilla, Antigua and Barbuda, Argentina, Aruba, Bahamas, Barbados, Belize, Bermuda, Brazil, British Virgin Islands, Canada, Cayman Islands, Chile, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Guyana, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and Grenadines, Suriname, Trinidad and Tobago, United States of America, Virgin Islands (USA), Uruguay, and Venezuela. Europe includes 38 countries: Albania, Austria, Belgium, Bulgaria, Croatia, the Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, the Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and the United Kingdom. Oceania includes 4 countries: including Australia, Fiji, Kiribati, and New Zealand.
LOESS = locally weighted scatterplot smoother.
Fig. 4. LOESS smoothed liver-related mortality rates by sex and age group among 112 countries, 1990–2021.
LOESS = locally weighted scatter plot smoother.
The age-standardized liver disease-related mortality rates show a negative correlation with the HDI (β, −400.430, P < 0.001) and the SDI (β, −327.855, P = 0.001; Fig. 5). According to the BAPC models, age-standardized liver disease-related mortality rates are predicted to gradually decrease, with 185.08 deaths per 1,000,000 people (95% credible interval, 179.79, 190.63) in 2021, 168.95 (160.70, 177.74) in 2030, 152.67 (134.44, 177.69) in 2040, and 156.29 (112.32, 214.77) in 2050. Additional analyses based on sex, geographical area, HDI and income yielded similar results. In the specific age group, individuals aged 25 years and older demonstrated a similar trend, while those under 25 years showed a gradual increase from 3.94 deaths per 1,000,000 people (95% credible intervals, 3.56, 4.38) in 2021 to 4.86 (2.68, 8.34) in 2050 (Fig. 6 and Supplementary Table 26).
Fig. 5. Correlation between age-standardized liver-related mortality rates and Human Development Index, Socio-demographic Index, and Gender Gap Index.
Fig. 6. Projections in age-standardized liver-related mortality rates from 1990 to 2050 by Bayesian age-period-cohort models. The dashed line represents the Bayesian age-period-cohort value for forecasted mortality, whereas the shaded area represents the 95% credible intervals.
The number of liver disease-related deaths from 1990 to 2021 and from 1990 to 2050 was associated with three components: population aging, population growth, and epidemiological changes (Fig. 7). From 1990 to 2021, the increase in the number of liver disease-related deaths was mainly attributed to the impact of epidemiological changes, accounting for 393,967 deaths compared to other factors. Population aging contributed to an additional 159,355 deaths, and population growth led to a further increase of 187,754 deaths (Supplementary Table 27). However, from 1990 to 2050, the impact of population aging and population growth accounted for the majority of the increase, with population aging contributing 900,299 deaths per 1,000,000 people, population growth contributing 846,268 deaths per 1,000,000 people, and epidemiological change contributing −70,259 deaths per 1,000,000 people (Supplementary Table 27).
Fig. 7. Changes in the number of liver-related deaths associated with aging, epidemiological change, and population from 1990 to 2021 and 1990 to 2050 by sex and income level. The dots represent the integrated outcomes of the three factors: aging, epidemiological change, and population.
DISCUSSION
In this study, there was a notable rise in the estimated global age-standardized liver disease-related mortality rates in 112 countries across five continents, increasing from 103.4 (95% CI, 88.16, 118.74) to 173.0 (95% CI, 155.15, 190.95) deaths per 1,000,000 people between 1990 and 2021. This surge was particularly evident in LMICs, which exhibited a substantial 2.1-fold increase in liver disease-related mortality. Across different regions, there were clear disparities, with Africa experiencing substantial increases; Asia, America, and Europe showing upward trends; and Oceania exhibiting downward trends. Age-standardized liver disease-related mortality rates were higher in men than in women across all continents from 1990 to 2021, with a notable increase in liver disease-related mortality rates in the population aged 65 years and older within the same time frame. Additionally, our analysis found an inverse correlation between liver disease-related mortality rates and indices such as HDI and SDI. From 1990 to 2021, the increase in liver disease-related deaths is predominantly linked to the effects of epidemiological changes. However, from 1990 to 2050, the influence of population aging and growth became the primary contributors to the overall increase. According to the BAPC models, projected future trends suggest a consistent and substantial decline in liver disease-related mortality rates, anticipating a decrease by 2050.
A previous study systematically analyzed the burden of liver cirrhosis, not liver disease-related mortality, using the GBD data.14,28 That study analyzed data from 1990 to 2017 and reported that the number of deaths caused by cirrhosis gradually increased compared to 1990, while the age-standardized death rate decreased.14 Additionally, subgroup analysis by region, income level, country, and cause of cirrhosis was reported. Similarly, a study analyzing data up to 2019 reported an increase in the number of deaths caused by cirrhosis and a decrease in the age-standardized death rate.28 Additionally, subgroup analysis by sex and cause of cirrhosis was reported. However, the analysis was conducted using databases up to 2019, and correlation data for the HDI and SDI were not provided. Furthermore, the analysis did not include future predictions of age-standardized death rates, nor did it incorporate changes in the number of liver-related deaths associated with aging, epidemiological changes, or the population. This underscores the importance of conducting research that reflects current and future trends, as demonstrated in the present study. Moreover, GBD-based studies often rely on meta-analyses and frequently depend on statistical modeling for areas with insufficient data, leading to a higher reliance on estimations over actual data and increasing the potential for errors.16,17 In contrast, we rely on mortality data directly reported by WHO member countries. This approach enhanced data reliability.
The age-standardized liver disease-related mortality rates in our study showed a 1.67-fold increase compared to rates prior to the 1990s. However, since 2014, there has been a stable or slightly decreasing pattern, rather than an increasing trend. This can be explained by the evolving epidemiology of liver disease-related mortality, which primarily includes cirrhosis and liver cancer.1 While the number of liver deaths due to cirrhosis and liver cancer is increasing, the age-standardized death rate is decreasing.14,29 Examining these causes, it was determined that cirrhosis is still mainly attributed to viral hepatitis; however, with the introduction of direct-acting antivirals and hepatitis B and C vaccinations, along with the implementation of the WHO’s GHSS on viral hepatitis, mortality related to HBV and HCV has significantly decreased.4,6,30,31 This trend is also evident in our study, showing stable or decreasing patterns since 2014.
Interestingly, mortality rates related to NAFLD and alcohol-related liver disease are increasing.2,32,33 This explains the sharp increase in mortality rates among those aged 65 and older observed in our study. Liver disease-related mortality increases with age in patients with cirrhosis, and the risk of hepatocellular carcinoma (HCC) is highest in those aged 60 years and above.34 Thus, the burden of NAFLD increases with age, and mortality from liver diseases among patients with NAFLD also increases with age.35,36 Moreover, as alcohol consumption increases, so does the prevalence of alcohol-associated liver disease. 1,37,38 Taking these factors, this suggests a transition in the primary causes of cirrhosis and chronic liver disease from viral hepatitis to NAFLD and alcohol-related liver disease.39,40 Based on these trends, it is expected that the increase in liver disease-related mortality due to population growth and aging will become more pronounced in the future. This aligns with our study’s projections up to 2050, in which the main factors driving the increase in liver disease-related mortality were population growth and aging.
Liver disease-related mortality burden, including liver cirrhosis,14,28 liver cancer,29 and alcohol-associated liver deaths,41 has been reported to be higher in men than in women, and similar findings were observed in this study.1 The observed high liver disease-related mortality in LMICs, particularly in Africa, aligns with previous studies.2 Firstly, Africa is known to have a high prevalence of the main causes of cirrhosis burden, including hepatitis B, C, and HCC.1,14 Additionally, alcohol per-capita consumption and alcohol-associated cirrhosis, which contribute to increasing liver disease-related mortality, are also prevalent in Africa.37 Lastly, the disparities in access to essential diagnostic and treatment services contribute to the high liver disease-related mortality in LMICs.42
In this study, age-standardized liver disease-related mortality rates were negatively correlated with the HDI and SDI. Previous research has also indicated that in regions with a higher SDI, cirrhosis-related mortality rates are lower, while mortality rates related to alcohol-related liver diseases and acute liver failure are higher in LMICs.14,43 Additionally, when comparing rural and urban areas, rural areas tend to exhibit higher age-adjusted mortality rates for cirrhosis.44 Analyzing the causes of these disparities, differences in accessibility to healthcare and the strength of healthcare infrastructure can be attributed as primary factors. Chronic liver diseases are often diagnosed in an advanced state, leading to high mortality rates.45 Moreover, chronic liver diseases are associated with significant economic burden due to increased healthcare expenditures.46 Socioeconomic disadvantages can influence the risk and progression of NAFLD; indeed, these financial difficulties can elevate overall mortality rates among adults with liver diseases.3,47 These factors contribute to the higher liver disease-related mortality observed in countries with lower HDI and SDI.
Global age-standardized liver disease-related mortality rates and projections of future liver disease-related deaths have significant implications for policy development. First, in Africa, where liver disease-related mortality rates are overwhelmingly high, interventions for early diagnosis and treatment of chronic liver diseases as well as screening programs are necessary. Chronic viral hepatitis, excessive alcohol consumption, and MASLD are major contributors to chronic liver diseases in Africa.7 Additionally, liver cancer ranks second among men and fourth among women in Africa in terms of mortality rates, with delayed diagnoses being common.48 The WHO's GHSS on viral hepatitis has provided a roadmap for eliminating viral hepatitis as a public health problem by 2030, resulting in notable global progress towards hepatitis elimination.4,49 Direct-acting antivirals for the treatment of HCV have significantly reduced extrahepatic manifestation-related mortality, and both all-age and age-standardized death rates due to HBV-related diseases are decreasing.5,50 Second, policy changes are needed because of epidemiological shifts in liver disease-related mortality rates. The risk factors for liver disease-related mortality are transitioning from virus-related to non-viral liver diseases.51 Moreover, ALD- and MASLD-related cirrhosis and chronic liver diseases are increasing, necessitating public health policies to address these issues. ALD-related cirrhosis accounts for 27.3% of the annual 1.32 million cirrhosis-related deaths, and the burden of ALD continues to rise, especially among the younger generation.9,14 Alcohol control policies have a significant and immediate impact on cirrhosis mortality and are cost-effective as well.52 However, MASLD increases mortality risk independent of excessive alcohol consumption, requiring management strategies.53 In Europe, where alcohol consumption is high and there is an increased prevalence of ultra-processed food consumption and obesity, the rates of both incidence and mortality associated with ALD are elevated.8
This analysis presents global trends in liver disease-related mortality rates from 1990 to 2021 and forecasts the projected burden of liver disease deaths up to 2050. However, this study has several limitations. First, our analysis, which relies on data reported by member countries in the WHO Mortality Database, faces the challenges of potential data incompleteness and variability in data quality across different nations. To address this issue, we restrict our analysis to datasets with comprehensive records spanning a minimum of 10 years. Second, existing data on liver disease-related mortality lack adequate representation of African patients, with only four countries (Egypt, Mauritius, Morocco, and South Africa) included in the dataset. This limited representation poses a challenge in establishing a comprehensive understanding of regional variations in liver disease-related mortality. To overcome this limitation, we conducted additional country-specific analyses to better capture regional differences. Third, we analyzed liver disease-related mortality by broadly categorizing it into viral hepatitis, cirrhosis, and liver cancer using ICD codes. This approach differs from other studies that focused on single-disease pathologies, such as cirrhosis, viral hepatitis, or liver cancer, potentially resulting in heterogeneous outcomes.6,14,29 Additionally, we aimed to provide new insights by analyzing the overall liver disease-related mortality from a global perspective and examined the trajectory of liver disease burden through future projections up to 2050. This study contributes to the understanding of the overall burden of liver disease from a global public health perspective and aids in policy formulation. Fourth, our predictions were based on future population estimates calculated using the BAPC model, assuming that the influences of age, period, and cohort factors on liver disease-related mortality will remain constant from 2021 to 2050. Therefore, as a significant phenomenon that affects liver disease-related mortality, re-analysis of these aforementioned factors is necessary. Fifth, well-designed prospective studies controlling for confounding factors are needed to estimate the risk of liver disease-related mortality more accurately. Lastly, while our research was primarily focused on liver disease-related mortality, further studies are required to explore the burden of disease attributable to morbidity to provide a more comprehensive assessment.
Despite these limitations, this study has several strengths. This study utilized the WHO mortality database to illustrate global trends in liver disease-related mortality from 1990 to 2021. Moreover, it employs an innovative method to predict liver disease-related fatalities by the year 2050. This research delves into the relationship between liver disease-related mortality rates and national-level indicators, such as the level of development. By employing LOESS techniques, this study effectively analyzed patterns in liver disease-related mortality rates, and adaptively modeled complex nonlinear data relationships without the need to assume a specific functional form.
In conclusion, our study offers insights into age-standardized liver disease-related mortality on a global scale, considering various factors such as income, sex, age, and geographical region. These findings highlighted the persistent significance of LD-related mortality as a global public health concern. Further investigations, particularly focusing on Africa, are imperative to gain a deeper understanding of liver disease-related mortality in this region. Additionally, interventions aimed at the early diagnosis and treatment of chronic liver diseases, along with the implementation of screening programs, are crucial. Lastly, the epidemiological shift in liver disease-related mortality rates emphasizes the need for policy changes to effectively manage the global burden of liver disease.
ACKNOWLEDGMENTS
The authors acknowledge the World Health Organization for permission to access and use the data analysed in this study. The information provided should not be interpreted as representing the official statement of the World Health Organization.
Footnotes
Funding: This research was supported by grants from the National Research Foundation of Korea (NRF), funded by the Korean government (MSIT; RS-2023-00248157), the Ministry of Food and Drug Safety (21153MFDS601) in 2024, and the MSIT (Ministry of Science and ICT), Korea, under the ITRC (Information Technology Research Center) support program (IITP-2024-RS-2024-00438239) supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation). The funders had no role in the study design, data collection, data analysis, data interpretation, or manuscript writing.
Disclosure: The authors have no potential conflicts of interest to disclose.
Data Availability Statement: The WHO Mortality Database represents a worldwide cooperative collection of death rates as reported by member countries of the WHO. Dong Keon Yon (yonkkang@gmail.com) was contacted for the study protocols and statistical codes. Access to the dataset was provided by the WHO under a data-use agreement.
- Conceptualization: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Data curation: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Formal analysis: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Funding acquisition: Yon DK.
- Investigation: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Methodology: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Project administration: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Resources: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Software: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Supervision: Yon DK.
- Validation: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Visualization: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Writing - original draft: Hahn JW, Woo S, Park J, Kim S, Yon DK.
- Writing - review & editing: Hahn JW, Woo S, Park J, Lee H1, Kim HJ, Ko JS, Moon JS, Rahmati M, Smith L, Kang J, Pizzol D, Tully MA, Dragioti E, Sánchez GFL, Lee K, Ha Y, Lee J, Lee H2, Rhee SY, Son Y, Kim S, Yon DK.
Lee H1, Lee Hyeri; Lee H2, Lee Hayeon.
SUPPLEMENTARY MATERIALS
Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER)
Age-standardized mortality rate calculation, socio-economic indicators, and advanced statistical methods
Liver-related code list for ICD-8, ICD-9, and ICD-10
List of 112 countries and their corresponding 3 letter codes
Classification of countries into HICs and LMICs group
Classification of countries into Human Development Index group
LOESS smoothed liver-related mortality rates (per 1,000,000 people) in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for male in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for female in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for individuals ≥ 65 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for males ≥ 65 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for females ≥ 65 years in 112 countries, 1990–2021
The age-standardized liver-related mortality rate (95% CI) at the national level is estimated for 2021, 2030, 2040, and 2050 using Bayesian age-period-cohort models, based on variable categories
Changes in the number of liver-related deaths associated with aging, epidemiological change, and population from 1990 to 2021 and 1990 to 2050 by sex and continent
Age-standardized liver-related mortality rates for the global, HICs, and LMICs population among 112 countries by male for the years 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in red. HICs included 59 countries, including Anguilla, Antigua and Barbuda, Aruba, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Chile, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Guyana, Hong Kong SAR, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Netherlands, New Zealand, Norway, Panama, Poland, Portugal, Puerto Rico, Qatar, Republic of Korea, Romania, Saint Kitts and Nevis, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America, Uruguay, and Virgin Islands (USA). LMICs included 53 countries, including Albania, Argentina, Armenia, Azerbaijan, Belarus, Belize, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Egypt, El Salvador, Fiji, Georgia, Grenada, Guatemala, Jamaica, Kazakhstan, Kiribati, Kyrgyzstan, Malaysia, Maldives, Mauritius, Mexico, Montenegro, Morocco, Nicaragua, North Macedonia, Occupied Palestinian Territory, Paraguay, Peru, Philippines, Republic of Moldova, Russian Federation, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Sri Lanka, Suriname, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, Ukraine, Uzbekistan, and Venezuela.
Age-standardized liver-related mortality rates for the global, HICs, and LMICs population among 112 countries by female for the years 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in red. HICs included 59 countries, including Anguilla, Antigua and Barbuda, Aruba, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Chile, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Guyana, Hong Kong SAR, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Netherlands, New Zealand, Norway, Panama, Poland, Portugal, Puerto Rico, Qatar, Republic of Korea, Romania, Saint Kitts and Nevis, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America, Uruguay, and Virgin Islands (USA). LMICs included 53 countries, including Albania, Argentina, Armenia, Azerbaijan, Belarus, Belize, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Egypt, El Salvador, Fiji, Georgia, Grenada, Guatemala, Jamaica, Kazakhstan, Kiribati, Kyrgyzstan, Malaysia, Maldives, Mauritius, Mexico, Montenegro, Morocco, Nicaragua, North Macedonia, Occupied Palestinian Territory, Paraguay, Peru, Philippines, Republic of Moldova, Russian Federation, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Sri Lanka, Suriname, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, Ukraine, Uzbekistan, and Venezuela.
Age-standardized liver-related mortality rates in the Africa population by sex among 4 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Africa includes the 4 countries, including Egypt, Mauritius, Morocco, and South Africa.
Age-standardized liver-related mortality rates in the Asia population by sex among 27 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Asia includes the 27 countries, including Armenia, Azerbaijan, Bahrain, Brunei Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan.
Age-standardized liver-related mortality rates in the Europe population by sex among 38 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Europe includes the 38 countries, including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
Age-standardized liver-related mortality rates in the Americas population by sex among 39 countries, 1990–2021. The LOESS mortality rates with 95% confidence levels, weighted by country population, are shown in blue. Americas include the 39 countries, including Anguilla, Antigua and Barbuda, Argentina, Aruba, Bahamas, Barbados, Belize, Bermuda, Brazil, British Virgin Islands, Canada, Cayman Islands, Chile, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Guyana, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago, United States of America, Uruguay, Venezuela, and Virgin Islands (USA).
Age-standardized liver-related mortality rates in the Oceania population by sex among 4 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue Oceania includes the 4 countries, including Canada, Panama, Puerto Rico, and United States of America.
LOESS smoothed liver-related mortality rates by sex and age group among 4 countries in Africa, 1990–2021. Africa includes the 4 countries, including Egypt, Mauritius, Morocco, and South Africa.
LOESS smoothed liver-related mortality rates by sex and age group among 27 countries in Asia, 1990–2021. Asia includes the 27 countries, including Armenia, Azerbaijan, Bahrain, Brunei Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan.
LOESS smoothed liver-related mortality rates by sex and age group among 38 countries in Europe, 1990–2021. Europe includes the 38 countries, including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
LOESS smoothed liver-related mortality rates by sex and age group among 39 countries in Americas, 1990–2021. Americas include the 39 countries, , including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
LOESS smoothed liver-related mortality rates by sex and age group among 4 countries in Oceania, 1990–2021. Oceania includes the 4 countries, including Australia, Fiji, Kiribati, and New Zealand.
References
- 1.Devarbhavi H, Asrani SK, Arab JP, Nartey YA, Pose E, Kamath PS. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, Wong G, Anstee QM, Henry L. The global burden of liver disease. Clin Gastroenterol Hepatol. 2023;21(8):1978–1991. doi: 10.1016/j.cgh.2023.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Ayyala-Somayajula D, Dodge JL, Farias A, Terrault N, Lee BP. Healthcare affordability and effects on mortality among adults with liver disease from 2004 to 2018 in the United States. J Hepatol. 2023;79(2):329–339. doi: 10.1016/j.jhep.2023.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Easterbrook P, Luhmann N, Newman M, Walsh N, Lesi O, Doherty M. New WHO guidance for country validation of viral hepatitis B and C elimination. Lancet Gastroenterol Hepatol. 2021;6(10):778–780. doi: 10.1016/S2468-1253(21)00267-3. [DOI] [PubMed] [Google Scholar]
- 5.GBD 2019 Hepatitis B Collaborators. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7(9):796–829. doi: 10.1016/S2468-1253(22)00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GBD 2019 Europe Hepatitis B & C Collaborators. Hepatitis B and C in Europe: an update from the Global Burden of Disease Study 2019. Lancet Public Health. 2023;8(9):e701–e716. doi: 10.1016/S2468-2667(23)00149-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sonderup MW, Kamath PS, Awuku YA, Desalegn H, Gogela N, Katsidzira L, et al. Managing cirrhosis with limited resources: perspectives from sub-Saharan Africa. Lancet Gastroenterol Hepatol. 2024;9(2):170–184. doi: 10.1016/S2468-1253(23)00279-0. [DOI] [PubMed] [Google Scholar]
- 8.Karlsen TH, Sheron N, Zelber-Sagi S, Carrieri P, Dusheiko G, Bugianesi E, et al. The EASL-Lancet Liver Commission: protecting the next generation of Europeans against liver disease complications and premature mortality. Lancet. 2022;399(10319):61–116. doi: 10.1016/S0140-6736(21)01701-3. [DOI] [PubMed] [Google Scholar]
- 9.Singal AK, Kwo P, Kwong A, Liangpunsakul S, Louvet A, Mandrekar P, et al. Research methodologies to address clinical unmet needs and challenges in alcohol-associated liver disease. Hepatology. 2022;75(4):1026–1037. doi: 10.1002/hep.32143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deutsch-Link S, Jiang Y, Peery AF, Barritt AS, Bataller R, Moon AM. Alcohol-associated liver disease mortality increased from 2017 to 2020 and accelerated during the COVID-19 pandemic. Clin Gastroenterol Hepatol. 2022;20(9):2142–2144.e2. doi: 10.1016/j.cgh.2022.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danpanichkul P, Ng CH, Muthiah M, Suparan K, Tan DJH, Duangsonk K, et al. From shadows to spotlight: exploring the escalating burden of alcohol-associated liver disease and alcohol use disorder in young women. Am J Gastroenterol. 2024;119(5):893–909. doi: 10.14309/ajg.0000000000002642. [DOI] [PubMed] [Google Scholar]
- 12.Hahn JW, Yang HR, Moon JS, Chang JY, Lee K, Kim GA, et al. Global incidence and prevalence of autoimmune hepatitis, 1970–2022: a systematic review and meta-analysis. EClinicalMedicine. 2023;65:102280. doi: 10.1016/j.eclinm.2023.102280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2022;7(9):851–861. doi: 10.1016/S2468-1253(22)00165-0. [DOI] [PubMed] [Google Scholar]
- 14.GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi: 10.1016/S2468-1253(19)30349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray CJL. The Global Burden of Disease Study at 30 years. Nat Med. 2022;28(10):2019–2026. doi: 10.1038/s41591-022-01990-1. [DOI] [PubMed] [Google Scholar]
- 16.Shin YH, Hwang J, Kwon R, Lee SW, Kim MS, et al. GBD 2019 Allergic Disorders Collaborators. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Allergy. 2023;78(8):2232–2254. doi: 10.1111/all.15807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chong B, Jayabaskaran J, Kong G, Chan YH, Chin YH, Goh R, et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. EClinicalMedicine. 2023;57:101850. doi: 10.1016/j.eclinm.2023.101850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiyoshige E, Ogata S, O’Flaherty M, Capewell S, Takegami M, Iihara K, et al. Projections of future coronary heart disease and stroke mortality in Japan until 2040: a Bayesian age-period-cohort analysis. Lancet Reg Health West Pac. 2022;31:100637. doi: 10.1016/j.lanwpc.2022.100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ebmeier S, Thayabaran D, Braithwaite I, Bénamara C, Weatherall M, Beasley R. Trends in international asthma mortality: analysis of data from the WHO Mortality Database from 46 countries (1993–2012) Lancet. 2017;390(10098):935–945. doi: 10.1016/S0140-6736(17)31448-4. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: a New WHO Standard. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 21.Hahn JW, Lee K, Shin JI, Cho SH, Turner S, Shin JU, et al. Global incidence and prevalence of eosinophilic esophagitis, 1976–2022: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2023;21(13):3270–3284.e77. doi: 10.1016/j.cgh.2023.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol. 2012;13(8):790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 23.The Lancet. 2020: a critical year for women, gender equity, and health. Lancet. 2020;395(10217):1. doi: 10.1016/S0140-6736(19)33170-8. [DOI] [PubMed] [Google Scholar]
- 24.India State-Level Disease Burden Initiative Mental Disorders Collaborators. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. Lancet Psychiatry. 2020;7(2):148–161. doi: 10.1016/S2215-0366(19)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmid VJ, Held L. Bayesian age-period-cohort modeling and prediction-BAMP. J Stat Softw. 2007;21(8):1–15. [Google Scholar]
- 26.Cheng X, Yang Y, Schwebel DC, Liu Z, Li L, Cheng P, et al. Population ageing and mortality during 1990–2017: a global decomposition analysis. PLoS Med. 2020;17(6):e1003138. doi: 10.1371/journal.pmed.1003138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qi J, Li M, Wang L, Hu Y, Liu W, Long Z, et al. National and subnational trends in cancer burden in China, 2005–20: an analysis of national mortality surveillance data. Lancet Public Health. 2023;8(12):e943–e955. doi: 10.1016/S2468-2667(23)00211-6. [DOI] [PubMed] [Google Scholar]
- 28.Lan Y, Wang H, Weng H, Xu X, Yu X, Tu H, et al. The burden of liver cirrhosis and underlying etiologies: results from the Global Burden of Disease Study 2019. Hepatol Commun. 2023;7(2):e0026. doi: 10.1097/HC9.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rumgay H, Arnold M, Ferlay J, Lesi O, Cabasag CJ, Vignat J, et al. Global burden of primary liver cancer in 2020 and predictions to 2040. J Hepatol. 2022;77(6):1598–1606. doi: 10.1016/j.jhep.2022.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Politi J, Guerras JM, Donat M, Belza MJ, Ronda E, Barrio G, et al. Favorable impact in hepatitis C-related mortality following free access to direct-acting antivirals in Spain. Hepatology. 2022;75(5):1247–1256. doi: 10.1002/hep.32237. [DOI] [PubMed] [Google Scholar]
- 31.Ly KN, Yin S, Spradling PR. Regional differences in mortality rates and characteristics of decedents with hepatitis B listed as a cause of death, united states, 2000–2019. JAMA Netw Open. 2022;5(6):e2219170. doi: 10.1001/jamanetworkopen.2022.19170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jung JY, Park SK, Oh CM, Chung PW, Ryoo JH. Non-alcoholic fatty liver disease and its association with depression in Korean general population. J Korean Med Sci. 2019;34(30):e199. doi: 10.3346/jkms.2019.34.e199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoo HW, Jin HY, Yon DK, Effenberger M, Shin YH, Kim SY, et al. Non-alcoholic fatty liver disease and COVID-19 susceptibility and outcomes: a Korean nationwide cohort. J Korean Med Sci. 2021;36(41):e291. doi: 10.3346/jkms.2021.36.e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han J, Wang B, Liu W, Wang S, Chen R, Chen M, et al. Declining disease burden of HCC in the United States, 1992–2017: a population-based analysis. Hepatology. 2022;76(3):576–588. doi: 10.1002/hep.32355. [DOI] [PubMed] [Google Scholar]
- 35.Danpanichkul P, Ng CH, Muthiah MD, Duangsonk K, Yong JN, Tan DJH, et al. The silent burden of non-alcoholic fatty liver disease in the elderly: a global burden of disease analysis. Aliment Pharmacol Ther. 2023;58(10):1062–1074. doi: 10.1111/apt.17714. [DOI] [PubMed] [Google Scholar]
- 36.Lin H, Yip TC, Zhang X, Li G, Tse YK, Hui VW, et al. Age and the relative importance of liver-related deaths in nonalcoholic fatty liver disease. Hepatology. 2023;77(2):573–584. doi: 10.1002/hep.32633. [DOI] [PubMed] [Google Scholar]
- 37.Huang DQ, Mathurin P, Cortez-Pinto H, Loomba R. Global epidemiology of alcohol-associated cirrhosis and HCC: trends, projections and risk factors. Nat Rev Gastroenterol Hepatol. 2023;20(1):37–49. doi: 10.1038/s41575-022-00688-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yoon JH, Jun CH, Kim JH, Yoon EL, Kim BS, Song JE, et al. Changing trends in liver cirrhosis etiology and severity in Korea: the increasing impact of alcohol. J Korean Med Sci. 2021;36(21):e145. doi: 10.3346/jkms.2021.36.e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang DQ, Terrault NA, Tacke F, Gluud LL, Arrese M, Bugianesi E, et al. Global epidemiology of cirrhosis - aetiology, trends and predictions. Nat Rev Gastroenterol Hepatol. 2023;20(6):388–398. doi: 10.1038/s41575-023-00759-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jang WY, Chung WJ, Jang BK, Hwang JS, Lee HJ, Hwang MJ, et al. Changes in characteristics of patients with liver cirrhosis visiting a tertiary hospital over 15 years: a retrospective multi-center study in Korea. J Korean Med Sci. 2020;35(29):e233. doi: 10.3346/jkms.2020.35.e233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karaye IM, Maleki N, Hassan N, Yunusa I. Trends in alcohol-related deaths by sex in the US, 1999–2020. JAMA Netw Open. 2023;6(7):e2326346. doi: 10.1001/jamanetworkopen.2023.26346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bajaj JS, Choudhury AK, Xie Q, Kamath PS, Topazian M, Hayes PC, et al. Global disparities in mortality and liver transplantation in hospitalised patients with cirrhosis: a prospective cohort study for the CLEARED Consortium. Lancet Gastroenterol Hepatol. 2023;8(7):611–622. doi: 10.1016/S2468-1253(23)00098-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vento S, Cainelli F. Acute liver failure in low-income and middle-income countries. Lancet Gastroenterol Hepatol. 2023;8(11):1035–1045. doi: 10.1016/S2468-1253(23)00142-5. [DOI] [PubMed] [Google Scholar]
- 44.Ufere NN, Patzer RE, Kavalieratos D, Louissaint J, Kaplan A, Cross SH. Rural-urban disparities in mortality from cirrhosis in the United States from 1999 to 2019. Am J Gastroenterol. 2022;117(7):1162–1165. doi: 10.14309/ajg.0000000000001712. [DOI] [PubMed] [Google Scholar]
- 45.Abeysekera KW, Macpherson I, Glyn-Owen K, McPherson S, Parker R, Harris R, et al. Community pathways for the early detection and risk stratification of chronic liver disease: a narrative systematic review. Lancet Gastroenterol Hepatol. 2022;7(8):770–780. doi: 10.1016/S2468-1253(22)00020-6. [DOI] [PubMed] [Google Scholar]
- 46.Kim LY, Yoo JJ, Chang Y, Jo H, Cho YY, Lee S, et al. The epidemiology of hepatitis B virus infection in Korea: 15-year analysis. J Korean Med Sci. 2024;39(4):e22. doi: 10.3346/jkms.2024.39.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allen AM, Lazarus JV, Younossi ZM. Healthcare and socioeconomic costs of NAFLD: a global framework to navigate the uncertainties. J Hepatol. 2023;79(1):209–217. doi: 10.1016/j.jhep.2023.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nhlane R, Kreuels B, Mallewa J, Chetcuti K, Gordon MA, Stockdale AJ. Late presentation of hepatocellular carcinoma highlights the need for a public health programme to eliminate hepatitis B. Lancet. 2021;398(10318):2288. doi: 10.1016/S0140-6736(21)02138-3. [DOI] [PubMed] [Google Scholar]
- 49.Cui F, Blach S, Manzengo Mingiedi C, Gonzalez MA, Sabry Alaama A, Mozalevskis A, et al. Global reporting of progress towards elimination of hepatitis B and hepatitis C. Lancet Gastroenterol Hepatol. 2023;8(4):332–342. doi: 10.1016/S2468-1253(22)00386-7. [DOI] [PubMed] [Google Scholar]
- 50.Jeong D, Wong S, Karim ME, Manges AR, Makuza JD, Bartlett SR, et al. Treatment of HCV with direct-acting antivirals on reducing mortality related to extrahepatic manifestations: a large population-based study in British Columbia, Canada. Lancet Reg Health Am. 2023;29:100658. doi: 10.1016/j.lana.2023.100658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singal AG, Kanwal F, Llovet JM. Global trends in hepatocellular carcinoma epidemiology: implications for screening, prevention and therapy. Nat Rev Clin Oncol. 2023;20(12):864–884. doi: 10.1038/s41571-023-00825-3. [DOI] [PubMed] [Google Scholar]
- 52.Thursz M, Lingford-Hughes A. Advances in the understanding and management of alcohol-related liver disease. BMJ. 2023;383:e077090. doi: 10.1136/bmj-2023-077090. [DOI] [PubMed] [Google Scholar]
- 53.van Kleef LA, de Knegt RJ, Brouwer WP. Metabolic dysfunction-associated fatty liver disease and excessive alcohol consumption are both independent risk factors for mortality. Hepatology. 2023;77(3):942–948. doi: 10.1002/hep.32642. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER)
Age-standardized mortality rate calculation, socio-economic indicators, and advanced statistical methods
Liver-related code list for ICD-8, ICD-9, and ICD-10
List of 112 countries and their corresponding 3 letter codes
Classification of countries into HICs and LMICs group
Classification of countries into Human Development Index group
LOESS smoothed liver-related mortality rates (per 1,000,000 people) in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for male in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for female in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among individuals aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for individuals ≥ 65 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among males aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for males ≥ 65 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females < 25 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 25–34 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 35–44 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 45–54 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) among females aged 55–64 years in 112 countries, 1990–2021
LOESS smoothed liver-related mortality rates (per 1,000,000 people) for females ≥ 65 years in 112 countries, 1990–2021
The age-standardized liver-related mortality rate (95% CI) at the national level is estimated for 2021, 2030, 2040, and 2050 using Bayesian age-period-cohort models, based on variable categories
Changes in the number of liver-related deaths associated with aging, epidemiological change, and population from 1990 to 2021 and 1990 to 2050 by sex and continent
Age-standardized liver-related mortality rates for the global, HICs, and LMICs population among 112 countries by male for the years 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in red. HICs included 59 countries, including Anguilla, Antigua and Barbuda, Aruba, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Chile, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Guyana, Hong Kong SAR, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Netherlands, New Zealand, Norway, Panama, Poland, Portugal, Puerto Rico, Qatar, Republic of Korea, Romania, Saint Kitts and Nevis, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America, Uruguay, and Virgin Islands (USA). LMICs included 53 countries, including Albania, Argentina, Armenia, Azerbaijan, Belarus, Belize, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Egypt, El Salvador, Fiji, Georgia, Grenada, Guatemala, Jamaica, Kazakhstan, Kiribati, Kyrgyzstan, Malaysia, Maldives, Mauritius, Mexico, Montenegro, Morocco, Nicaragua, North Macedonia, Occupied Palestinian Territory, Paraguay, Peru, Philippines, Republic of Moldova, Russian Federation, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Sri Lanka, Suriname, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, Ukraine, Uzbekistan, and Venezuela.
Age-standardized liver-related mortality rates for the global, HICs, and LMICs population among 112 countries by female for the years 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in red. HICs included 59 countries, including Anguilla, Antigua and Barbuda, Aruba, Australia, Austria, Bahamas, Bahrain, Barbados, Belgium, Bermuda, British Virgin Islands, Brunei Darussalam, Canada, Cayman Islands, Chile, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Guyana, Hong Kong SAR, Hungary, Iceland, Ireland, Israel, Italy, Japan, Kuwait, Latvia, Lithuania, Luxembourg, Malta, Netherlands, New Zealand, Norway, Panama, Poland, Portugal, Puerto Rico, Qatar, Republic of Korea, Romania, Saint Kitts and Nevis, Singapore, Slovakia, Slovenia, Spain, Sweden, Switzerland, Trinidad and Tobago, United Kingdom, United States of America, Uruguay, and Virgin Islands (USA). LMICs included 53 countries, including Albania, Argentina, Armenia, Azerbaijan, Belarus, Belize, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, Egypt, El Salvador, Fiji, Georgia, Grenada, Guatemala, Jamaica, Kazakhstan, Kiribati, Kyrgyzstan, Malaysia, Maldives, Mauritius, Mexico, Montenegro, Morocco, Nicaragua, North Macedonia, Occupied Palestinian Territory, Paraguay, Peru, Philippines, Republic of Moldova, Russian Federation, Saint Lucia, Saint Vincent and the Grenadines, Serbia, South Africa, Sri Lanka, Suriname, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, Ukraine, Uzbekistan, and Venezuela.
Age-standardized liver-related mortality rates in the Africa population by sex among 4 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Africa includes the 4 countries, including Egypt, Mauritius, Morocco, and South Africa.
Age-standardized liver-related mortality rates in the Asia population by sex among 27 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Asia includes the 27 countries, including Armenia, Azerbaijan, Bahrain, Brunei Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan.
Age-standardized liver-related mortality rates in the Europe population by sex among 38 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue. Europe includes the 38 countries, including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
Age-standardized liver-related mortality rates in the Americas population by sex among 39 countries, 1990–2021. The LOESS mortality rates with 95% confidence levels, weighted by country population, are shown in blue. Americas include the 39 countries, including Anguilla, Antigua and Barbuda, Argentina, Aruba, Bahamas, Barbados, Belize, Bermuda, Brazil, British Virgin Islands, Canada, Cayman Islands, Chile, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Guyana, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Puerto Rico, Saint Kitts and Nevis, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago, United States of America, Uruguay, Venezuela, and Virgin Islands (USA).
Age-standardized liver-related mortality rates in the Oceania population by sex among 4 countries, 1990–2021. The LOESS mortality rates with 95 % confidence levels, weighted by country population, are shown in blue Oceania includes the 4 countries, including Canada, Panama, Puerto Rico, and United States of America.
LOESS smoothed liver-related mortality rates by sex and age group among 4 countries in Africa, 1990–2021. Africa includes the 4 countries, including Egypt, Mauritius, Morocco, and South Africa.
LOESS smoothed liver-related mortality rates by sex and age group among 27 countries in Asia, 1990–2021. Asia includes the 27 countries, including Armenia, Azerbaijan, Bahrain, Brunei Darussalam, China, Cyprus, Georgia, Hong Kong SAR, Israel, Japan, Kazakhstan, Kuwait, Kyrgyzstan, Malaysia, Maldives, Occupied Palestinian Territory, Philippines, Qatar, Republic of Korea, Singapore, Sri Lanka, Syrian Arab Republic, Tajikistan, Thailand, Turkey, Turkmenistan, and Uzbekistan.
LOESS smoothed liver-related mortality rates by sex and age group among 38 countries in Europe, 1990–2021. Europe includes the 38 countries, including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
LOESS smoothed liver-related mortality rates by sex and age group among 39 countries in Americas, 1990–2021. Americas include the 39 countries, , including Albania, Austria, Belarus, Belgium, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Ukraine, and United Kingdom.
LOESS smoothed liver-related mortality rates by sex and age group among 4 countries in Oceania, 1990–2021. Oceania includes the 4 countries, including Australia, Fiji, Kiribati, and New Zealand.