Abstract
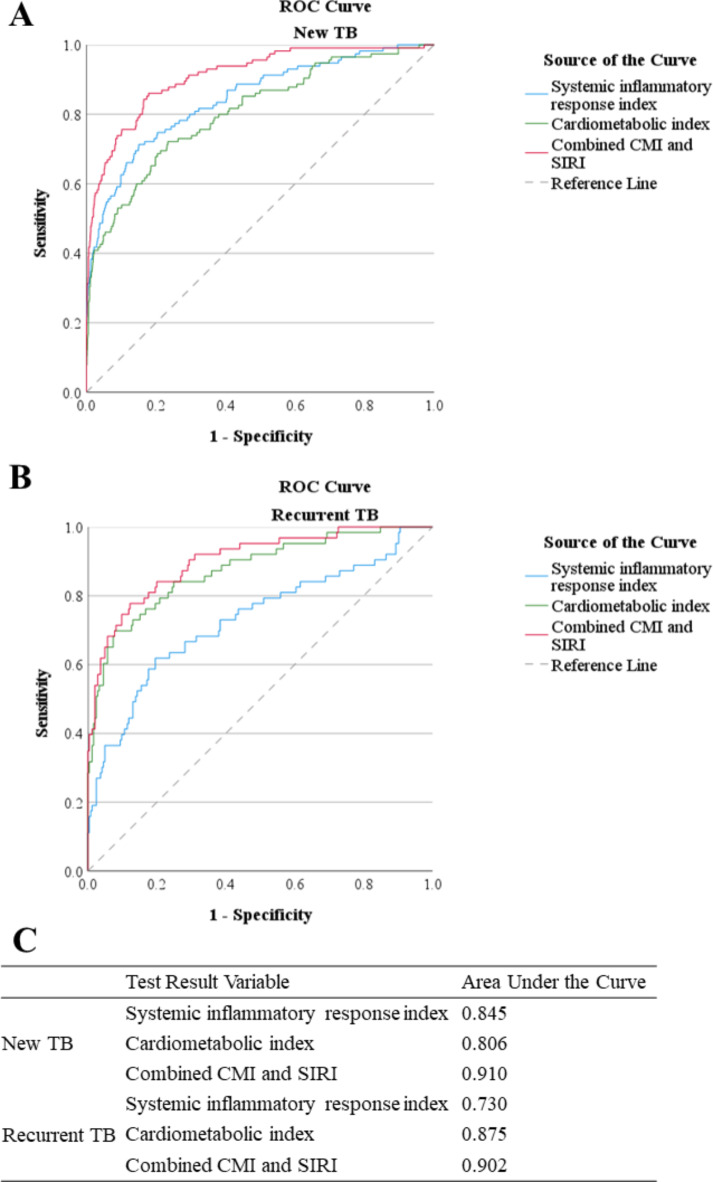
Multidrug-resistant tuberculosis (MDR-TB) remains a global public health challenge. We aimed to investigate the utility of combining the cardiometabolic index (CMI) and systemic inflammation response index (SIRI) as biomarkers for rapid MDR-TB screening. Data were collected from 2,620 TB patients in Zibo city from 2018 to 2021. Logistic regression and receiver operating characteristic (ROC) curve analyses were used to evaluate the associations and diagnostic performance of CMI and SIRI with MDR-TB. The prevalence of MDR-TB was 5.0% in new TB patients and 20.5% in recurrent TB patients. Both CMI and SIRI were significantly associated with MDR-TB in all models (P < 0.05). In new TB patients, the area under the curve (AUC) values of the ROC curves for SIRI, CMI, and their combination were 0.845, 0.806, and 0.910, respectively. In recurrent TB patients, the AUC values were 0.730, 0.875, and 0.902, respectively. The optimal cut-off points for SIRI and CMI were 0.72 and 1.81 in new TB patients, and 1.05 and 1.48 in recurrent TB patients, respectively. In conclusion, combining CMI and SIRI shows promise as a low-invasive, cost-effective tool for early MDR-TB screening, warranting further validation in diverse populations and TB subtypes.
Keywords: Cardiometabolic risk factors, Drug Resistance, Dyslipidaemias, Obesity, Inflammation
Subject terms: Biomarkers, Infectious diseases, Diagnosis
Introduction
Tuberculosis (TB) remains a significant global public health challenge, particularly with the rise of multidrug-resistant TB (MDR-TB). According to the World Health Organization, TB is one of the top ten causes of death worldwide and is the leading cause of death from a single infectious agent, surpassing even HIV/AIDS1. The emergence of MDR-TB, defined as TB resistant to at least isonicotinic acid hydrazide (INH) and rifampicin (RIF), complicates treatment regimens and significantly increases morbidity and mortality2. Rapid and accurate identification of MDR-TB is crucial for effective treatment and containment of the disease. Traditional diagnostic methods for TB drug resistance, including Mycobacterium tuberculosis culture and drug susceptibility testing, are time-consuming and resource-intensive. While innovative molecular technologies such as Xpert MTB/RIF have improved the diagnostic speed, they are not easily accessible because of their high cost and equipment requirements3. Therefore, there is an urgent need for simplified, cost-effective screening tools that can rapidly identify individuals at high risk of developing MDR-TB, enabling timely intervention and appropriate treatment.
The cardiometabolic index (CMI), a composite measure incorporating anthropometric and metabolic parameters, has been extensively studied in the context of cardiovascular diseases and metabolic disorders4. Mounting evidence indicates that disturbances in glucose and lipid metabolism may influence TB progression and treatment response5,6. However, the potential association between CMI and drug-resistant TB remains unclear. The systemic inflammation response index (SIRI) is a novel complex biomarker adopted to demonstrate the body’s overall inflammatory and immune response7. Elevated SIRI levels have been linked to poor outcomes in various chronic inflammatory conditions, including cancer and cardiovascular diseases7–9. In the context of TB, despite the close relationship between systemic inflammation and TB pathogenesis and progression, few studies have assessed whether the SIRI is a valuable clinical indicator for predicting or assisting in the diagnosis of drug-resistant TB.
In this study, we aimed to evaluate the utility and reliability of combining the CMI and SIRI as a rapid and simplified screening tool for TB drug resistance.
Results
Characteristics of the study participants
The sociodemographic and clinical characteristics of the patients categorized by new or recurrent TB are summarized in Table 1. The median age of all patients was 41.7 years, with no significant differences observed between new and recurrent TB patients in terms of median age or age distribution. A significant difference in sex distribution was observed, with males accounting for 64.4% of new patients and 70.8% of recurrent patients (P = 0.027). With respect to educational attainment, a greater proportion of the recurrent patients had a lower level of education than did the new patients (P = 0.001). Specifically, 55.2% of the recurrent patients had only a primary education level, whereas 44.1% of the new patients did. In terms of health-related behaviours, recurrent TB patients were more likely to be smokers and reported higher alcohol consumption than new patients (41.6% versus 34.1%, P = 0.009 for smoking; 47.7% versus 39.2%, P = 0.004 for alcohol consumption). Significant differences in certain inflammatory and metabolic variables, including the neutrophil count, lymphocyte count, and triglyceride level, were also detected between new and recurrent patients (all P < 0.05).
Table 1.
Sociodemographic and clinical characteristics of new and recurrent tuberculosis patients in Zibo City, China, 2018–2021.
| New TB patients | Recurrent TB patients | P value | |
|---|---|---|---|
| Number | 2312 | 308 | |
| Age | 41.5 (30.5–55.4) | 44.3 (30.6–59.5) | 0.127 |
| Young (≤ 35 years) | 876 (37.9) | 110 (35.7) | 0.149 |
| Middle (36–55 years) | 864 (37.4) | 106 (34.4) | |
| Elder (≥ 56 years) | 572 (24.7) | 92 (29.9) | |
| Gender | |||
| Male | 1489 (64.4) | 218 (70.8) | 0.027 |
| Female | 823 (35.6) | 90 (29.2) | |
| Educational attainment level | |||
| High (≥ 13 years) | 589 (25.5) | 61(19.8) | 0.001 |
| Middle (10–12 years) | 704 (30.4) | 77 (25.0) | |
| Primary (≤ 9 years) | 1019 (44.1) | 170 (55.2) | |
| Diabetes | |||
| No | 2119 (91.7) | 279 (90.6) | 0.527 |
| Yes | 193 (8.3) | 29 (9.4) | |
| Smoking | |||
| No | 840 (36.3) | 87 (28.2) | 0.009 |
| Previous | 683 (29.5) | 93 (30.2) | |
| Yes | 789 (34.1) | 128 (41.6) | |
| Alcohol drinking | |||
| No | 1406 (60.8) | 161 (52.3) | 0.004 |
| Yes | 906 (39.2) | 147 (47.7) | |
| Drug-resistant tuberculosis | |||
| No | 1832 (79.2) | 143 (46.4) | < 0.001 |
| Yes | 480 (20.8) | 165 (53.6) | |
| MDR-TB | |||
| No | 2197 (95.0) | 245 (79.5) | < 0.001 |
| Yes | 115 (5.0) | 63 (20.5) | |
| Neutrophil count, 109/L | 3.5 (2.7–4.6) | 4.0 (2.8–5.3) | < 0.001 |
| Monocyte count, 109/L | 0.2 (0.1–0.4) | 0.2 (0.1–0.4) | 0.792 |
| Lymphocyte count, 109/L | 2.2 (1.7–2.8) | 2.1 (1.6–2.7) | 0.001 |
| Systemic Inflammation Response Index | 0.4 (0.2–0.7) | 0.4 (0.2–0.8) | 0.003 |
| Triglyceride, mmol/L | 1.0 (0.7–1.6) | 1.2 (0.8–2.0) | < 0.001 |
| HDL-c, mmol/L | 0.6 (0.5–1.0) | 0.6 (0.5–0.8) | 0.059 |
| Waist-Height Ratio | 0.5 (0.4–0.5) | 0.5 (0.4–0.6) | 0.006 |
| Cardiometabolic Index | 0.8 (0.4–1.6) | 0.9 (0.5–2.0) | < 0.001 |
Data are presented as median (interquartile range) or number (percentage). P values are derived from the results of Mann-Whitney U test or Chi-square test. MDR-TB, multidrug-resistant tuberculosis. HDL-c, high-density lipoprotein cholesterol.
Associations of inflammatory and metabolic biomarkers with TB drug resistance
The results of the logistic regression analysis presented in Table 2 indicate that the CMI and SIRI were positively associated with drug-resistant TB and MDR-TB, regardless of whether patients were newly diagnosed or had received prior treatment.
Table 2.
Logistic regression analyses of CMI and SIRI associations with drug-resistant TB among patients in Zibo City, China, 2018–2021.
| Factor | New TB patients | Recurrent TB patients | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug–resistant TB | MDR–TB | Drug–resistant TB | MDR–TB | ||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | ||
| CMI | Crude | 1.27 (1.20–1.35) | < 0.001 | 1.74 (1.59–1.90) | < 0.001 | 1.61 (1.32–1.96) | < 0.001 | 2.08 (1.69–2.55) | < 0.001 |
| Model 1 | 1.26 (1.19–1.34) | < 0.001 | 1.73 (1.58–1.89) | < 0.001 | 1.64 (1.34–2.01) | < 0.001 | 2.10 (1.70–2.59) | < 0.001 | |
| Model 2 | 1.21 (1.13–1.28) | < 0.001 | 1.70 (1.56–1.86) | < 0.001 | 1.67 (1.35–2.06) | < 0.001 | 2.09 (1.70–2.58) | < 0.001 | |
| SIRI | Crude | 2.23 (1.89–2.63) | < 0.001 | 6.17 (4.68–8.13) | < 0.001 | 1.90 (1.25–2.89) | 0.003 | 4.22 (2.55–7.00) | < 0.001 |
| Model 1 | 2.19 (1.86–2.59) | < 0.001 | 6.05 (4.56–8.02) | < 0.001 | 1.92 (1.26–2.93) | 0.002 | 4.31 (2.57–7.21) | < 0.001 | |
| Model 2 | 2.02 (1.71–2.39) | < 0.001 | 5.67 (4.25–7.56) | < 0.001 | 2.15 (1.32–3.49) | 0.002 | 5.03 (2.90–8.73) | < 0.001 | |
P values are derived from logistic regression analysis. CI, confidence interval; CMI, Cardiometabolic Index; MDR-TB, multidrug-resistant tuberculosis; OR, odds ratio; SIRI, systemic inflammation response index; TB, tuberculosis. Model 1: Adjusted for gender and age; Model 2: Adjusted for gender, age, education level, smoking status, and drinking status.
In terms of CMI, among new TB patients, the crude odds ratio (OR) of the CMI was 1.27 (95% CI: 1.20–1.35) for drug-resistant TB and 1.74 (95% CI: 1.59–1.90) for MDR-TB. These associations remained significant after adjusting for sex and age in the Model 1 and further adjusted for education level, smoking status, and alcohol consumption in the Model 2 (all P < 0.05). In recurrent TB patients, the OR of the CMI in relation to MDR-TB showed a similar trend, with a crude OR of 2.08 (95% CI: 1.69–2.55), which remained significant after adjustment in the Model 1 (OR = 2.10, 95% CI: 1.70–2.59) and Model 2 (OR = 2.09, 95% CI: 1.70–2.58).
In new TB patients, the crude OR of the SIRI was 2.23 (95% CI: 1.89–2.63) for drug-resistant TB and 6.17 (95% CI: 4.68–8.13) for MDR-TB. In recurrent TB patients, the crude OR of the SIRI was 1.90 (95% CI: 1.25–2.89) for drug-resistant TB and 4.22 (95% CI: 2.55–7.00) for MDR-TB. Similar to CMI, further adjustments for confounding factors in Model 1 and Model 2 mildly changed but did not substantially affect the above associations (all P < 0.05).
Diagnostic usefulness of combined CMI and SIRI
The diagnostic performance of the combined CMI and SIRI for detecting MDR-TB is presented in Fig. 1. In new TB patients, the area under the curve (AUC) values for the SIRI, CMI, and their combination were 0.845, 0.806, and 0.910, respectively. For recurrent TB patients, the AUC values for the SIRI, CMI, and their combination were 0.730, 0.875, and 0.902, respectively. The optimal cut-off points were determined via the Youden index method. Among new TB patients, a combined SIRI value of 0.72 and a CMI value of 1.81 yielded the highest Youden’s index of 0.682, corresponding to a sensitivity of 0.861 and a specificity of 0.821. In recurrent TB patients, a combined SIRI value of 1.05 and a CMI value of 1.48 maximized the Youden index at 0.655, with a sensitivity of 0.778 and a specificity of 0.878.
Fig. 1.
ROC curves of CMI and SIRI for the detection of multidrug-resistant tuberculosis. (A) New tuberculosis patients; (B) recurrent tuberculosis patients; (C) Summary table of AUC values for incident and recurrent TB patients. CMI, cardiometabolic index; ROC, receiver operating characteristic; SIRI, systemic inflammation response index.
Discussion
In this study, we explored the diagnostic usefulness of combining CMI and SIRI for detecting MDR-TB in both new and recurrent TB patients. Our findings suggest that this combined approach has significant potential for rapid and cost-effective screening of MDR-TB, offering a practical and scalable solution for TB management, especially in resource-limited settings.
The associations among metabolic disturbances, chronic systemic inflammation, and drug-resistant TB are increasingly recognized in the literature5,10,11. An increased inflammatory response, which is usually characterized by elevated inflammatory cytokines and altered immune cell proportions, may cause an imbalance in the systemic microenvironment, and promote the development and progression of drug-resistant TB12,13. The close link between aberrant glucose‒lipid metabolic profiles and the inflammatory response has been extensively studied in recent decades14,15. Diabetes, obesity, and dyslipidaemia are strongly associated with elevated levels of numerous inflammatory cytokines, including IL-7, TNF-α, and TGF-β14. During the progression of TB infection, low HDL-c levels can exacerbate systemic inflammation16. A recent study demonstrated that obesity-induced chronic dysbiosis aggravated pulmonary inflammation via increased production of IFN-γ in TB-infected mice17. Taken together, it is reasonable to conjecture that CMI, which integrates central obesity and lipid metabolism, and SIRI, which are used to assess systemic integrated inflammation, could be applied in the initial clinical screening and prediction of drug-resistant TB. We found that CMI and SIRI individually have good diagnostic value, while their combination provides a better model, which improves the diagnostic efficacy from “good” (0.7 ≤ AUC < 0.9) to “excellent” (AUC ≥ 0.9)18. These results provide preliminary support for our previous hypothesis to some extent.
To date, conventional culture-based drug susceptibility testing remains the gold standard for diagnosing drug-resistant TB. However, its limitations are evident, including time consumption and susceptibility to contamination. Recent advancements in molecular-based tests, such as the Xpert MTB/RIF Assay, offer a rapid and accurate method for identifying drug-resistant TB. Nonetheless, the special equipment requirements and high testing costs present substantial challenges for widespread implementation of these ideal technologies, particularly in most low- and some middle-income countries and areas19. Unlike molecular-based tests, CMI and SIRI are derived from routine clinical examinations and laboratory tests, making them widely accessible and affordable. It is worth noting that while CMI and SIRI cannot diagnose drug-resistant TB on their own, they can be used in combination with other methods to improve diagnostic efficiency without additional economic burden and extra invasive examination. More importantly, they may serve as a low-cost early screening tool to identify patients at high risk of developing drug-resistant TB before it occurs. Early identification of TB patients susceptible to drug resistance can enable timely initiation of appropriate preventive intervention, potentially reducing the development and transmission of drug-resistant strains and improving overall TB control, which is relevant in resource-limited areas.
This study has several strengths, including a large sample size, the inclusion of both new and recurrent TB patients, and the use of real-world clinical data. To the best of our knowledge, this is the first study to evaluate the combined diagnostic utility of CMI and SIRI for MDR-TB, providing a feasible and practical diagnostic strategy that can be easily integrated into various healthcare settings. However, the limitations of this study should also be cautiously considered. First, the study was conducted in a single centre in a city in China, which may restrict the applicability of our results to other populations with various demographic and environmental characteristics. Further external validation in diverse settings is essential to confirm the model’s utility. Additionally, smear-negative TB patients were not included, meaning the associations of CMI and SIRI with drug-resistant TB and the predictive performance of this composite index for drug resistance in smear-negative patients remain unclear. Finally, the cross-sectional design limits our ability to establish causality between the observed associations. Prospective studies are needed to assess the predictive value of CMI and SIRI for the risk of developing drug-resistant TB.
In conclusion, our study highlights the potential of combining CMI and SIRI as a rapid, cost-effective, and low-invasive screening tool for MDR-TB. This approach leverages the metabolic and inflammatory pathways involved in TB pathogenesis, offering a more comprehensive assessment of risk.
Methods
Study population and study design
All Ziehl–Neelsen smear-positive pulmonary TB patients treated at Zibo Specialized Tuberculosis Hospital from 1 January 2018 to 31 December 2021 were included in this study initially (number = 3033), and the details of this study have been described previously20. Patients were excluded if they met the following exclusion criteria: non-provision of valid informed consent (number = 247); incomplete medical records or missing some clinical data (number = 131); history of self-reported or diagnosed severe drug, tobacco, or alcohol dependence (number = 23); diagnosed cancer or malignant tumour (number = 12). Finally, A total of 2,620 TB patients were enrolled in this study. All TB diagnoses followed the Chinese clinical guidelines for TB diagnosis and treatment. Drug susceptibility tests were performed according to the World Health Organization technical manual21. This study was approved by the Ethics Committee of Zibo First Hospital. The design and all procedures of this study were in accordance with the Declaration of Helsinki.
Data collection
Demographic and clinical information, including age, gender, educational level, medical records, and disease history, was collected by well-trained clinicians. Diabetes was diagnosed based on fasting blood glucose ≥ 7.0 mmol/L or self-reported previously diagnosed diabetes. Smoking status was classified as smoker, former smoker, or non-smoker22. Smokers refer to individuals who are currently smoking and have smoked within the past 30 days. The former refers to individuals who used to smoke but had not smoked within the past 30 days. Drinking was defined as average alcohol consumption of at least 40 g per week during the past 12 months23.
The physical examinations were conducted by trained staff. Height and weight were measured with a calibrated instrument, and waist were measured with a tape. Blood glucose, triglyceride (TG), and high-density lipoprotein cholesterol (HDL-c) levels derived from clinical chemistry test were assessed via standard enzymatic methods with a Beckman AU680 analyser (Beckman Coulter, USA). Neutrophil, monocyte, and lymphocyte counts derived from complete blood count were performed with an Automated Haematology Analyser XS1000i/800i (Sysmex, Japan). The CMI was calculated as the product of the TG/HDL-c ratio and waist-to-height ratio4. The SIRI was calculated as the product of the neutrophil and monocyte counts divided by the lymphocyte count7.
Statistical analysis
Data are presented as medians (interquartile ranges) or numbers (percentages). The Mann-Whitney U test was used to compare nonnormally distributed continuous variables, whereas the Chi-square test was used to compare categorical variables across groups. Univariable and multivariable binary logistic regression analyses were conducted to assess the associations of the CMI and SIRI with drug-resistant TB and MDR-TB. A receiver operating characteristic (ROC) curve was used to evaluate the screening performance of the CMI, SIRI, or both for detecting drug-resistant TB. All the statistical tests were two-tailed, and P < 0.05 was considered statistically significant. Statistical analysis was conducted with SPSS 18.0 software (IBM Corp., USA).
Acknowledgements
We would like to thank all study subjects for their participation and cooperation.
Abbreviations
- AUC
Area under the curve
- CI
Confidence interval
- CMI
Cardiometabolic index
- HDL-c
High-density lipoprotein cholesterol
- INH
Isonicotinic acid hydrazide
- MDR-TB
Multidrug-resistant tuberculosis
- OR
Odds ratio
- RIF
Rifampicin
- ROC
Receiver operating characteristic
- SIRI
Systemic inflammation response index
- TB
Tuberculosis
Author contributions
SY, MC and YH contributed to conception and design of the study. SY, HS, YC, and YL performed the experiments and organized the original data. SY, MC, and YH performed the statistical analysis. MC and YH prepared the tables and figures. SY and MC wrote the first draft of the manuscript. SY, MC, and YH wrote the final version of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was funded by the Zibo Medical and Health Research Project (20231800129), the Affiliated Hospital of Weifang Medical University Science and Technology Development Project (2023FYM060), the Suzhou Science and Education Strengthening Health Youth Project (KJXW2021011), and the Suzhou Medical Innovation and Application Research Project (SKY2023119).
Data availability
The data are available from the corresponding author upon reasonable request and with permission from Zibo First Hospital.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Zibo First Hospital, and signed informed consent forms were obtained from all participants.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Meizhi Cai, Email: caimeizhi1987@hotmail.com.
Yifan Huang, Email: yyzhyf@hotmail.com.
References
- 1.Chakaya, J. et al. The WHO Global Tuberculosis 2021 report–not so good news and turning the tide back to end TB. Int. J. Infect. Dis.124, S26–S29. 10.1016/j.ijid.2022.03.011 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dheda, K. et al. Multidrug-resistant tuberculosis. Nat. Rev. Dis. Primers. 10, 22. 10.1038/s41572-024-00504-2 (2024). [DOI] [PubMed] [Google Scholar]
- 3.Pantoja, A., Fitzpatrick, C., Vassall, A., Weyer, K. & Floyd, K. Xpert MTB/RIF for diagnosis of tuberculosis and drug-resistant tuberculosis: A cost and affordability analysis. Eur. Respir J.42, 708–720. 10.1183/09031936.00147912 (2013). [DOI] [PubMed] [Google Scholar]
- 4.Wakabayashi, I. & Daimon, T. The cardiometabolic index as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin. Chim. Acta. 438, 274–278. 10.1016/j.cca.2014.08.042 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Baluku, J. B. et al. Association between biomarkers of inflammation and dyslipidemia in drug resistant tuberculosis in Uganda. Lipids Health Dis.23, 65. 10.1186/s12944-024-02063-7 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quinonez, C. G. et al. The role of fatty acid metabolism in drug tolerance of Mycobacterium tuberculosis. MBio 13, e03559-03521 (2022). 10.1128/mbio.03559-21 [DOI] [PMC free article] [PubMed]
- 7.Qi, Q. et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 122, 2158–2167. 10.1002/cncr.30057 (2016). [DOI] [PubMed] [Google Scholar]
- 8.Kong, F. et al. System inflammation response index: a novel inflammatory indicator to predict all-cause and cardiovascular disease mortality in the obese population. Diabetol. Metab. Syndr.15, 195. 10.1186/s13098-023-01178-8 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu, L. T. et al. Systemic inflammation response index (SIRI) predicts prognosis in hepatocellular carcinoma patients. Oncotarget. 8, 34954–34960. 10.18632/oncotarget.16865 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shetty, S., Pappachan, J. M. & Fernandez, C. J. Diabetes and tuberculosis: an emerging dual threat to healthcare. World J. Diabetes. 15, 1409–1416. 10.4239/wjd.v15.i7.1409 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ngo, M. D., Bartlett, S. & Ronacher, K. Diabetes-associated susceptibility to tuberculosis: contribution of hyperglycemia vs. dyslipidemia. Microorganisms. 9, 2282. 10.3390/microorganisms9112282 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basingnaa, A., Antwi-Baffour, S., Nkansah, D. O., Afutu, E. & Owusu, E. Plasma levels of cytokines (IL-10, IFN-γ, and TNF-α) in multidrug resistant tuberculosis and drug responsive tuberculosis patients in Ghana. Diseases. 7, 2. 10.3390/diseases7010002 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sampath, P. et al. Cytokine upsurge among drug-resistant tuberculosis endorse the signatures of hyper inflammation and disease severity. Sci. Rep.13, 785. 10.1038/s41598-023-27895-8 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu, H. Z. & Ballantyne, C. M. Metabolic inflammation and insulin resistance in obesity. Circ. Res.126, 1549–1564. 10.1161/Circresaha.119.315896 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rohm, T. V., Meier, D. T., Olefsky, J. M. & Donath, M. Y. Inflammation in obesity, diabetes, and related disorders. Immunity. 55, 31–55. 10.1016/j.immuni.2021.12.013 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inoue, M. et al. High-density lipoprotein suppresses tumor necrosis factor alpha production by mycobacteria-infected human macrophages. Sci. Rep.8, 6736. 10.1038/s41598-018-24233-1 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palma Albornoz, S. P. et al. Obesity-induced dysbiosis exacerbates IFN-γ production and pulmonary inflammation in Mycobacterium tuberculosis infection. Cells. 10, 1732. 10.3390/cells10071732 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carter, J. V., Pan, J. M., Rai, S. N. & Galandiuk, S. ROC-ing along: evaluation and interpretation of receiver operating characteristic curves. Surgery. 159, 1638–1645. 10.1016/j.surg.2015.12.029 (2016). [DOI] [PubMed] [Google Scholar]
- 19.Chopra, K. K., Singh, S. & Tuberculosis Newer diagnostic tests: applications and limitations. Indian J. Tuberc. 67, S86–S90. 10.1016/j.ijtb.2020.09.025 (2020). [DOI] [PubMed] [Google Scholar]
- 20.Yuan, S. Z. et al. Prevalence, temporal trends and risk factors of drug-resistant TB in Zibo, China, 2018–2021. Int. J. Tuberc Lung Dis.28, 57–58. 10.5588/ijtld.23.0296 (2024). [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Technical manual for drug susceptibility testing of medicines used in the treatment of tuberculosis. (2018).
- 22.Ryan, H., Trosclair, A. & Gfroerer, J. Adult current smoking: differences in definitions and prevalence Estimates—NHIS and NSDUH, 2008. J. Environ. Public. Health. 2012 (1–11). 10.1155/2012/918368 (2012). [DOI] [PMC free article] [PubMed]
- 23.Fan, J. G. & Farrell, G. C. Epidemiology of non-alcoholic fatty liver disease in China. J. Hepatol.50, 204–210. 10.1016/j.jhep.2008.10.010 (2009). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available from the corresponding author upon reasonable request and with permission from Zibo First Hospital.