Abstract
Dyskalemia are associated with an increased risk of mortality in patients undergoing maintenance hemodialysis (MHD). However, studies evaluating the impact of serum potassium variability on mortality in MHD patients are scarce. To investigate serum potassium variability and its association with prognosis in MHD patients, we conducted a retrospective study on maintenance hemodialysis patients from three campus of Renji Hospital between June 2018 and December 2022. The exposure of interest was serum potassium variability defined as the coefficient of variation of serum potassium levels (CVSP). Cox regression models and Kaplan-Meier survival analysis were used to assess the prognostic significance of serum potassium variability. In a subgroup analysis, the association between serum potassium variability and prognosis was investigated in patients within normal serum potassium concentration range. Total of 588 maintenance hemodialysis patients were included. During a median follow-up of 45 months (24, 54), 121 patients (20.6%) died. The survival analysis suggested significantly higher survival rates for both all-cause (p < 0.01) and cardiovascular (p < 0.01) death in patients in the highest group of CVSP (H-CVSP) compared with those in the the lowest group (L-CVSP). After adjustment, the all-cause mortality hazard ratio compared to L-CVSP was 2.17 [95% confidence interval (CI) 1.18, 3.97] for H-CVSP (p < 0.05) and was 2.53 [95%CI 1.03, 6.22] for cardiovascular mortality (p < 0.05). In the subgroup analysis, 493 patients (83.8%) presented normokalemia (the mean of serum potassium levels ≥ 3.5mmol/L and ≤ 5.0mmol/L) were included. Similar association was found between serum potassium variability and accumulated survival rates, and higher serum potassium variablity was remained an independent risk factor for cardiovascular mortality (2.69, 95% CI 1.07–6.78, p < 0.05) in patients within normal serum potassium concentration range. In conclusion, a higher serum potassium variability was associated with all-cause and cardiovascular mortality in maintenance haemodialysis patients, even in the normal range.
Keywords: Potassium variability, Hemodialysis, Prognosis, Chronic kidney disease
Subject terms: Haemodialysis, End-stage renal disease, Risk factors
Introduction
Serum potassium levels play an important role in maintaining the electrophysiological properties of the resting membrane potential in the body and fluctuate within a narrow range due to the balance between intake and excretion1,2. The kidneys are responsible for excreting approximately 80–90% of the potassium that intaked by a healthy individual on a daily basis1. However, the renal excretory function is reduced in MHD patients, and the regulation of potassium homeostasis in these patients depends primarily on hemodialysis sessions.
Dyskalemia is common in MHD patients3–8. Both hyperkalemia and hypokalemia can modify the electrical stability of cell membrane and increase the risk of cardiac arrhythmias and arrest9. It has been well documented that serum potassium levels are associated with an increasing risk of all-cause and cardiovascular mortality in MHD patients, showing a “U”-shaped association10–14.
Moreover, the fluctuations of serum potassium levels may also lead to instability of the resting membrane potential with cardiac arrhythmia and other adverse effects15–17. Although several studies have analyzed the relationship between serum potassium variability and clinical outcomes and suggested that higher serum potassium variability was associated with higher mortality risk in intensive care unit (ICU) patients, in-hospital patients or patients with acute myocardial infarction18–21, there are few studies investigating on the effect of serum potassium variability on prognosis in MHD patients. A recent study reported an independent association between higher serum potassium variability and all-cause mortality in MHD patients22, and study focused on facility-level potassium variability also showed poorer prognosis in MHD patients in dialysis centre with higher facility-level potassium variability23.
The aim of this study was to investigate the association between serum potassium variability and mortality in MHD patients, especially in patients within the normal serum potassium concentration range.
Methods
Patients
This retrospective observational study was performed on patients undergoing regular in-centre maintenance hemodialysis in the three campus of Renji Hospital Shanghai Jiaotong University School of Medicine between June 2018 and December 2022. Patients aged 18 years or older and received thrice-weekly hemodialysis for more than three months were included. And patients were excluded due to a lack of available baseline data. To assess serum potassium variability, patients who had less than three measurements of serum potassium levels were also excluded. A total of 588 patients were enrolled in the final analysis.
This research protocol was approved by Shanghai Jiaotong University School of Medicine, Renji Hospital Ethics Commitee (KY2022-021-B) and written informed consent was waived. The methods in this study were in accordance with the guidelines of Ethics Commitee of the institution.
Data collection
Data were obtained from the hospital medical records and patient files. Demographic details, primary kidney disease, medications, comorbidities and dialysis prescription were collected at baseline. Demographic details included age, sex, dialysis vintage, and body mass index (BMI). Patients were divided into four categories of primary kidney disease, including chronic glomerulonephritis, diabetic nephropathy, hypertensive nephropathy and others. History of use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEI/ARB), beta-blockers, diuretics and potassium binders was collected, considered to affect serum potassium levels1. A history of cardiovascular disease, hypertension and diabetes mellitus were recorded as comorbidities. And cardiovascular diseases was defined as any history of congestive heart failure, coronary artery disease, arrhythmias or stroke. All patients were treated with three times weekly dialysis with a duration of 4 h per session. Dialysate composition was uniform, with a dialysate potassium concentration of 2 mmol/L.
Serum potassium levels and other laboratory values such as haemoglobin, platelet count, urea nitrogen before and after dialysis, albumin, prealbumin, alkaline phosphatas (ALP), triglycerides, total cholesterol, low-density lipoprotein, high density lipoprotein, intact parathyroid hormone, serum calcium, serum phosphorus, bicarbonate and ferritin were obtained every three months during the follow-up. Urea reduction radio (URR) and serum corrected calcium were calculated. All of these values were included in the form of a mean of all examinations during the follow-up.
Exposure of interest and grouping
The exposure of interest was serum potassium variability. CVSP was calculated by the ratio between the standard deviation (SD) and the mean of serum potassium levels over the follow-up, used as the measurement for serum potassium variability18. Serum potassium levels was collected every three months immediately before dialysis. We used restricted cubic spline regressions to model and visualize the relation of CVSP with all-cause mortality and cardiovascular mortality (Fig. 1). And according to the restricted cubic splines, patients were divided into low CVSP (L-CVSP, CVSP ≤ 15%), moderate CVSP (M-CVSP, CVSP > 15% and ≤ 20%) and high CVSP (H-CVSP, CVSP > 20%) three groups. Patients were also grouped by serum potassium level to three groups, T1 (serum potassium level ≤ 4.0mmol/L), T2 (serum potassium level > 4.0mmol/L and ≤ 5.0mmol/L) and T3 (serum potassium level > 5.0mmol/L), according to the splines for serum potassium level and clinical significance.
Fig. 1.
The restricted cubic spline for the relationship between CVSP and mortality risk. The unadjusted hazard ratio of CVSP for all-cause (a) and cardiovascular (b) mortality was expressed by the solid black lines with grey areas showing 95% confidence intervals. Reference lines for a hazard ratio of 1.0 are indicated by the dashed lines. And the associations between serum potassium levels and all-cause mortality were shown in c while the associations between serum potassium levels and cardiovascular mortality were in d.
In the subgroup analysis, normal serum potassium concentration range was defined as the mean of serum potassium levels ≥ 3.5mmol/L and ≤ 5.0mmol/L24. After excluding patients with hyperkalemia and hypokalemia, patients within normal serum potassium concentration range were also divided into three groups by CVSP as mentioned above.
Outcomes
The primary outcomes were all-cause mortality and cardiovascular mortality. Cardiovascular mortality was defined as death due to heart failure, acute coronary syndrome, lethal arrhythmia, cardiac arrest or stroke. Survival was defined as the time from enrollment to death or censoring such as renal transplantation, transfer to other dialysis centers, loss to follow-up, or end of the study period25.
Statistical analyses
Patients characteristics were presented as mean ± standard deviation for continuous normally distributed variables, median [interquartile range] for continuous skewed distribution variables and counts (percentage) for categorical variables. Restricted cubic splines with three knots at 10th, 50th and 90th was preliminarily used to visualize the relation of CVSP with all-cause and cardiovascular mortality in a unadjusted model. And according to the unadjusted restricted cubic spline regressions, patients were divided into three groups by CVSP as mentioned above. Values were compared among groups of CVSP by one-way analysis of variance, Kruskal–Wallis test or chi-square test. To identify factors effecting serum potassium variability, bivariate correlation analysis was performed using Spearman’s correlation coefficient and Pearson correlation, and variables with statistical significance (p-value < 0.05) were included in multivariate linear regression analysis23. As CVSP was not normally distributed, statistical analysis was performed after log transformation22.Survival analysis was conducted using the Kaplan-Meier curve and tested by the log-rank test. Unadjusted and adjusted cox proportional hazards regression analyses were also used to assess the association between groups and the risk of all-cause and and cardiovascular mortality taking the L-CVSP as reference. The adjusted covariates included age, sex, dialysis vintage, BMI, use of ACEI/ARB, beta-blockers, diuretics and potassium binders, history of cardiovascular disease and diabetes mellitus, serum potassium levels, haemoglobin, albumin and URR18,22,23. A subgroup analysis was performed in patients within normal serum potassium concentration. Serum potassium levels were also grouped by unadjusted restricted cubic regression and the relationship between serum potassium levels and all-cause and cardiovascular mortality was evaluated with Kaplan-Meier curve and similar Cox regression with the same covariates excluding serum potassium levels and including serum potassium variability. 2-sided p-value < 0.05 was considered as statistical significance for all statistical analyses. Statistical analysis and visualisation were performed using SPSS version 27.0, GraphPad Prism version 10.1.2 and R 4.3.2.
Result
Patient characteristics
A total of 588 hemodialysis patients were included. The mean age of patients was 60.3 ± 13.3 years with a median vintage of 37 (5, 102) months, and 59.7% of the cohort was male. Patients had a median number of serum potassium measurements of 15 (9, 18), with an average serum potassium levels of 4.4 ± 0.5mmol/L.
In Fig. 1, We used restricted cubic splines to model and visualize the association of CVSP and serum potassium levels with all-cause and cardiovascular mortality, respectively. Non-linear association between CVSP and all-cause mortality (Fig. 1a) was observed (p for non-linearity < 0.05), while linear association with cardiovascular mortality (Fig. 1b) was showed (p for non-linearity = 0.06). The plots suggested an increased risk with higher CVSP. Similar association was observed in serum potassium levels with non-linear association for all-cause mortality (Fig. 1c) (p < 0.01) and linear association for cardiovascular mortality (Fig. 1d) (p = 0.91). 439 patients were placed in the L-CVSP group, 105 patients were in the M-CVSP group and 44 patients were in the H-CVSP. Patient characteristics grouped by CVSP are shown in Table 1.
Table 1.
Characteristics overall and by groups of serum potassium variability in study population.
| Variables | All patients (n = 588) |
L-CVSP (n = 439) |
M-CVSP (n = 105) |
H-CVSP (n = 44) |
P-value |
|---|---|---|---|---|---|
| Age, years | 60.3 ± 13.3 | 59.6 ± 13.4 | 62.6 ± 12.7 | 61.1 ± 13.5 | 0.11 |
| Males, n(%) | 351 (59.7%) | 271 (61.7%) | 56 (53.3%) | 24 (54.5%) | 0.22 |
| Dialysis vintage, months | 37 (5, 102) | 39 (5, 105) | 29 (4, 101) | 12 (4, 70) | 0.05 |
| Follow-up, months | 45 (24, 54) | 50 (27, 54) | 41 (19, 53) | 28 (12, 41) | < 0.01 |
| BMI, kg/m2 | 22.1 ± 3.5 | 22.1 ± 3.4 | 22.3 ± 4.0 | 22.2 ± 3.7 | 0.89 |
| Primary kidney disease | 0.47 | ||||
| Chronic glomerulonephritis, n(%) | 209 (35.5%) | 161 (36.7%) | 36 (34.4%) | 12 (27.3%) | |
| Diabetic nephropathy, n(%) | 104 (17.7%) | 80 (18.2%) | 15 (14.3%) | 9 (20.5%) | |
| Hypertensive nephropathy, n(%) | 41 (7.0%) | 33 (7.5%) | 7 (6.7%) | 1 (2.3%) | |
| Others, n(%) | 234 (39.8%) | 165 (37.6%) | 47 (44.8%) | 22 (9.4%) | |
| History of cardiovascular diseases, n(%) | 181 (30.8%) | 125 (28.5%) | 40 (38.1%) | 16 (36.4%) | 0.11 |
| History of diabetes mellitus, n(%) | 172 (29.3%) | 127 (73.8%) | 30 (28.6%) | 15 (34.1%) | 0.76 |
| Medications | |||||
| ACEI/ARB, n(%) | 352 (59.9%) | 265 (60.4%) | 59 (56.2%) | 28 (63.6%) | 0.64 |
| Beta-blockers, n(%) | 276 (46.9%) | 212 (48.3%) | 46 (43.8%) | 18 (40.9%) | 0.50 |
| Diuretics, n(%) | 57 (9.7%) | 43 (9.8%) | 9 (8.6%) | 5 (11.4%) | 0.86 |
| Potassium binders, n(%) | 14 (2.4%) | 13 (3%) | 0 (0%) | 1 (2.3%) | 0.17 |
| URR, % | 72.1 (68.2, 77.3) | 72.0 (68.3, 77.0) | 72.7 (68.4, 77.4) | 71.4 (66.6, 78.0) | 0.55 |
| Hemoglobin, g/L | 110.0 ± 9.9 | 110.8 ± 9.6 | 107.7 ± 9.2 | 107.8 ± 11.4 | < 0.01 |
| Platelet count, *10^3/µl | 188.3 ± 57.3 | 185.7 ± 58.5 | 195.4 ± 52.0 | 196.7 ± 56.5 | 0.18 |
| Albumin, g/L | 38.0 ± 2.8 | 38.2 ± 2.6 | 37.3 ± 3.5 | 38.2 ± 2.7 | < 0.01 |
| Pre-albumin, mg/L | 305.5 ± 63.7 | 309.6 ± 62.0 | 287.7 ± 67.9 | 306.9 ± 64.4 | < 0.01 |
| Alkaline phoshatase, U/L | 85.3 (68.6, 105.0) | 84.1 (68.3, 104.0) | 98.0 (75.1, 113.9) | 78.1 (61.3, 94.9) | < 0.01 |
| Total cholesterol, mmol/L | 4.0 (3.5, 4.6) | 4.0 (3.5, 4.6) | 4.1 (3.4, 4.8) | 4.3 (3.8, 4.8) | 0.10 |
| Triglycerides, mmol/L | 1.8 (1.3, 2.7) | 1.8 (1.3, 2.7) | 1.8 (1.2, 2.4) | 2.0 (1.3, 2.7) | 0.22 |
| Low-density cholesterol, mmol/L | 2.4 (1.9, 2.8) | 2.3 (1.9, 2.8) | 2.4 (1.8, 2.9) | 2.5 (2.1, 3.0) | 0.20 |
| High-density cholesterol, mmol/L | 1.0 (0.8, 1.2) | 1.0 (0.8, 1.2) | 1.0 (0.8, 1.2) | 1.0 (0.8, 1.3) | 0.73 |
| Phosphorus, mmol/L | 1.8 ± 0.4 | 1.8 ± 0.4 | 1.7 ± 0.5 | 1.9 ± 0.6 | 0.10 |
| intact parathyroid hormone, pg/ml | 256.4 (141.2, 457.4) | 258.8 (141.1, 448.3) | 246.1 (131.1, 470.7) | 262.3 (146.5, 398.5) | 0.94 |
| Ferritin, ng/ml | 226.4 (92.8, 439.8) | 207.3 (87.4, 439.9) | 266.4 (114.1, 453.6) | 226.9 (95.3, 422.9) | 0.34 |
| Bicarbonate, mmol/L | 21.7 ± 1.7 | 21.7 ± 1.7 | 22.0 ± 2.0 | 21.7 ± 1.7 | 0.19 |
| Corrected calcium, mmol/L | 2.3 ± 0.2 | 2.3 ± 0.2 | 2.3 ± 0.2 | 2.3 ± 0.2 | 0.17 |
| Mean of serum potassium, mmol/L | 4.4 ± 0.5 | 4.4 ± 0.5 | 4.3 ± 0.5 | 4.4 ± 0.5 | 0.22 |
| CVSP, % | 12.3 (10.2, 15.2) | 11.3 (9.5, 12.8) | 16.8 (15.7, 18.1) | 22.8 (21.1, 24.6) | < 0.01 |
Values expressed as mean ± SD, number (percentage), or median (interquartile range).
Factors associated with serum potassium variability
Bivariate correlation analysis suggested a negative correlation of CVSP with vintage (r -0.11, 95% CI -0.19- -0.02, p = 0.01), serum hemoglobin (r -0.11, 95% CI -0.19- -0.03, p < 0.01) and prealbumin levels(r −0.10, 95% CI −0.18– -0.02, p < 0.05) and a positive correlation with ALP (r 0.11, 95% CI 0.03–0.19, p < 0.01). The use of beta-blockers (r −0.09, 95% CI −0.17– -0.00, p < 0.05) was associated with lower CVSP, while patients with a history of diabetes mellitus (r 0.08, 95% CI −0.00–0.16, p < 0.05) were significantly associated with higher CVSP. (Table 2)
Table 2.
Variables correlation with serum potassium variability.
| Variables | r (95% CI) | p-value |
|---|---|---|
| Age | 0.05 (−0.03, 0.13) | 0.25 |
| Male a | −0.06 (−0.14, 0.03) | 0.17 |
| Dialysis vintage | −0.11 (−0.19, −0.02) | 0.01 |
| BMI | 0.05 (−0.03, 0.13) | 0.25 |
| History of cardiovascular diseases b | 0.07 (−0.01, 0.15) | 0.08 |
| History of diabetes mellitus b | 0.08 (−0.00, 0.16) | < 0.05 |
| URR | 0.01 (−0.08, 0.09) | 0.90 |
| Use of ACEI/ARB c | 0.03 (−0.06,0.11) | 0.55 |
| Use of beta-blockers c | −0.09 (−0.17, −0.00) | 0.04 |
| Use of diuretics c | −0.02 (−0.10, 0.07) | 0.68 |
| Use of potassium binders c | −0.05 (−0.14, 0.03) | 0.20 |
| Hemoglobin | −0.11 (−0.19, −0.03) | < 0.01 |
| Albumin | −0.06 (−0.14,0.02) | 0.16 |
| Prealbumin | −0.10 (−0.18, −0.02) | < 0.05 |
| Alkaline phoshatase | 0.11 (0.03, 0.19) | < 0.01 |
| Total cholesterol | 0.03 (−0.06,0.11) | 0.55 |
| Triglycerides | −0.03 (−0.11, 0.05) | 0.48 |
| Low-density cholesterol | 0.03 (−0.05, 0.11) | 0.47 |
| High-density cholesterol | 0.01 (−0.07, 0.09) | 0.82 |
| Phosphorus | 0.01 (−0.07, 0.09) | 0.76 |
| Intact parathyroid hormone | 0.01 (−0.08, 0.09) | 0.89 |
| Ferritin | 0.06 (−0.03, 0.14) | 0.19 |
| Bicarbonate | 0.02 (−0.06, 0.10) | 0.68 |
| Corrected calcium | −0.03 (−0.11, 0.05) | 0.43 |
| Mean of serum potassium | 0.05 (−0.03, 0.14) | 0.19 |
a Compared to female.
b Compared to patients without history of cardiovascular diseases or diabetes mellitus.
c Compared to patients without use of ACEI/ARB, beta-blockers, diuretics or potassium binders.
In multivariate linear regression analysis, CVSP remained significantly negatively correlated with vintages (β=-0.09, p < 0.05), pre-albumin levels (β=-0.09, p < 0.05) and serum hemoglobin levels (β=-0.09, p < 0.05) in MHD patients. (Table 3)
Table 3.
Multivariate linear regression of serum potassium variability.
| Variables | Standard error | Standardized β | t | P-value |
|---|---|---|---|---|
| Dialysis vintage | 0 | −0.09 | −2.12 | < 0.05 |
| History of diabetes mellitus a | 0.02 | 0.02 | 0.52 | 0.61 |
| Use of beta-blockers b | 0.01 | −0.06 | −1.45 | 0.15 |
| Hemoglobin | 0 | −0.09 | −2.17 | < 0.05 |
| Prealbumin | 0 | −0.09 | −2.01 | < 0.05 |
| Alkaline phoshatase | 0 | 0.04 | 1.03 | 0.30 |
a Compared to patients without history of diabetes mellitus.
b Compared to patients without use of beta-blockers.
CVSP and prognosis in the whole cohort
During a median follow-up of 45 months (25, 45), 121 patients (20.6%) died and the all-cause death rate was 6.4 per 100 person-years. 49 patients (8.3%) died attributed to cardiovascular causes and the cardiovascular death rate was 2.6 per 100 person-years.
The Kaplan-Meier survival curves for all-cause and cardiovascular mortality in different groups of CVSP are displayed in Fig. 2. Although there was no significant difference compared to M-CVSP, patients in L-CVSP were associated with a significantly higher probability of survival for both all-cause (p < 0.01) and cardiovascular (p < 0.01) death compared to those in H-CVSP.
Fig. 2.
Kaplan-Meier survival curves for mortality according to serum potassium variability. (a) all-cause mortality; (b) cardiovascular mortality.
In an unadjusted cox regression model with L-CVSP as the reference group, a significantly higher risk of all-cause mortality (2.79, 95% CI 1.55–5.03, p < 0.01) was observed in H-CVSP, and the association was remained even after adjusting for confounders. In other words, higher CVSP was an independent factor associated with a higher risk of all-cause mortality (2.17, 95% CI 1.18–3.97, p < 0.05). The risk of cardiovascular mortality (3.025, 95% CI 1.27–7.24, p < 0.05) was also increased in H-CVSP compared with L-CVSP, and it was remained statistically significant (2.53, 95% CI 1.03–6.22, p < 0.05) in the adjusted model. (Table 4)
Table 4.
Association between serum potassium variability and risk of mortality in all study population.
| CVSP | N patients (%) | HR (95%, CI), All-cause mortality | HR (95%, CI), Cardiovascular mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | p-value | Adjusted | p-value | Unadjusted | p-value | Adjusted | p-value | ||
| L-CVSP | 439 (75.7%) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| M-CVSP | 105 (17.9%) | 1.50 (0.96, 2.35) | 0.08 | 1.10 (0.69, 1.75) | 0.70 | 1.13 (0.52, 2.43) | 0.76 | 1.01 (0.46, 2.26) | 0.97 |
| H-CVSP | 44 (7.5%) | 2.79 (1.55, 5.03) | < 0.01 | 2.17 (1.18, 3.97) | < 0.05 | 3.03 (1.27, 7.24) | < 0.05 | 2.53 (1.03, 6.22) | < 0.05 |
HR hazard ratio.
.
CVSP and prognosis in normal serum potassium concentration range
We further investigated the association between CVSP and prognosis in patients with normal serum potassium concentration range. A total of 493 patients were included in the subgroup analysis with a mean age of 60.4 ± 13.3 years and a median vintage of 38 (5,103) months. There were 100 (20.3%) all-cause deaths during a median follow-up of 45 (24–45) months corresponding to a rate of 6.3 per 100 person-years, and 42 patients (15.4%) were died of cardiovascular causes with a rate of 2.6 per 100 person-years.
The Kaplan-Meier survival curves in the subgroup are shown in Fig. 3 and indicated a similar result in patients with normokalemia for all-cause mortality, that patients with higher serum potassium variability (H-CVSP) had a poorer probability of survival compared to those in L-CVSP (p = 0.01) (Fig. 3a). And for cardiovascular mortality, there was a significantly higher survival rate in both L-CVSP (p < 0.01) and M-CVSP (p < 0.05) compared to H-CVSP (Fig. 3b).
Fig. 3.
Kaplan-Meier survival curves for mortality in the subgroup. (a) all-cause mortality; (b) cardiovascular mortality.
The results of unadjusted and adjusted Cox regression models for all-cause and cardiovascular mortality in the subgroup are shown in Table 5. H-CVSP was associated with a higher risk of both all-cause (2.36, 95% CI 1.21–4.60, p < 0.05) and cardiovascular (3.35, 95% CI 1.39–8.12, p < 0.01) mortality compared to L-CVSP. Even after adjustment, the association between H-CVSP and cardiovascular mortality remained statistically significant (2.69, 95% CI 1.07–6.78, p < 0.05).
Table 5.
Association between serum potassium variability and risk of mortality in the subgroup.
| CVSP | N patients (%) | HR (95%, CI), All-cause mortality | HR (95%, CI), Cardiovascular mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | p-value | Adjusted | p-value | Unadjusted | p-value | Adjusted | p-value | ||
| L-CVSP | 366 (74.2%) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| M-CVSP | 88 (17.8%) | 1.33 (0.81, 2.19) | 0.26 | 1.03 (0.62, 1.73) | 0.90 | 0.93 (0.39, 2.24) | 0.88 | 0.76 (0.30, 1.92) | 0.56 |
| H-CVSP | 39 (8.9%) | 2.36 (1.21, 4.60) | < 0.05 | 1.81 (0.91, 3.59) | 0.92 | 3.35 (1.39, 8.12) | < 0.01 | 2.69 (1.07, 6.78) | < 0.05 |
CVSP the coefficient of variation of serum potassium levels, HR hazard ratio.
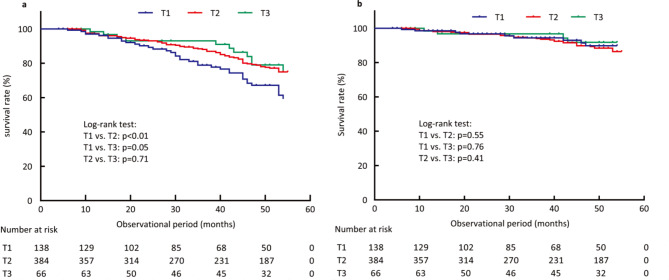
Serum potassium levels and prognosis
The Kaplan-Meier survival curves for serum potassium levels were shown in Fig. 4. Compared with T2, T1 was associated with poorer probability of survival form all-cause death. There was no significant difference in survival from cardiovascular death among the three groups.
Fig. 4.
Kaplan-Meier survival curves for the relationship between serum potassium levels and mortality . (a) all-cause mortality; (b) cardiovascular mortality.
Patients in T1 were associated with an increased risk of all-cause mortality (1.70, 95% CI 1.15–2.52, p < 0.01) compared with T2 (Table 6). However, the association disappeared after adjustment. There was no statistical significance in the association with cardiovascular mortality for T1 and T3 compared with T2.
Table 6.
Association between serum potassium levels and risk of mortality.
| Groups | N patients (%) | HR (95%, CI), All-cause mortality | HR (95%, CI), Cardiovascular mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | p-value | Adjusted | p-value | Unadjusted | p-value | Adjusted | p-value | ||
| T1 | 138 (23.5%) | 1.70 (1.15, 2.52) | < 0.01 | 1.10 (0.73, 1.67) | 0.65 | 0.80 (0.38, 1.66) | 0.54 | 0.68 (0.32, 1.46) | 0.32 |
| T2 | 384 (65.3%) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| T3 | 66 (11.2%) | 0.89 (0.47, 1.68) | 0.72 | 1.09 (0.57, 2.08) | 0.79 | 0.65 (0.23, 1.81) | 0.65 | 0.66 (0.23, 1.91) | 0.45 |
Discussion
We conducted a retrospective observational study in three campus of our dialysis center to investigate the association between serum potassium variability and prognosis in maintenance hemodialysis patients. Serum potassium variability was associated with poorer patient prognosis, and after adjustment, higher serum potassium variability showed an independent association with higher risk of all-cause and cardiovascular mortality in MHD patients. We also found that the association between serum potassium variability and prognosis was remained even in normal serum potassium concentration range.
MHD patients with longer vintages had a more stable serum potassium fluctuation which may be due to more stable dialysis prescriptions and medication used than those with shorter vintages, and we speculated that better compliance and stricter dietary management may also contribute to the negative correlation of vintage with serum potassium variability. In addition, our results showed that hemoglobin was negatively correlated with serum potassium variability, which are consistent with a recent study that reported a protective effect of hemoglobin on facility-level serum potassium variability23. Unlike Zhao et al.23, who found no statistical significance in multivariate analysis, we found an independent correlation of hemoglobin with serum potassium variability. This could be due to the differences in sample size and study population, Zhao et al. focused on the variability of serum potassium at the facility level, whereas we focus on intra-patient. It is possible that low hemoglobin levels reflect a poor nutritional status of MHD patients. Previous studies have demonstrated that anemia is an independent risk factor for cardiac disease and mortality26, and lower hemoglobin concentration or hematocrit level was associated with higher mortality27–29. Several studies also revealed the relationship between hemoglobin variability. Although the results are arguable, some studies have found that hemoglobin variability is associated with increased mortality30–32. The relationship between hemoglobin and serum potassium levels is also controversial23,33,34, and there is a lack of evidence to explain the association between hemoglobin and serum potassium variability. Moreover, serum prealbumin levels also showed a negative correlation with blood potassium variability in MHD patients in the bivariate correlation analysis. Prealbumin is a useful marker for nutritional risk assessment and is related to protein intake in MHD patients35. Previous studies have demonstrated that prealbumin was the best nutritional predictor of survival in dialysis patients36. Poor nutritional status suggested by low prealbumin could hypothetically be attributed to unstable serum potassium fluctuations. And this negative correlation remained statistically significant in multivariate analysis.
The relationship between serum potassium levels and clinical outcome in MHD patients have been widely explored. Although the optimal range of serum potassium levels remains controversial, it has been well documented that both hyperkalemia and hypokalemia are associated with an increased risk of all-cause and cardiovascular mortality10–14. Our study was consistent with previous reports that hypokalemia was associated with an increasing risk of mortality in MHD patients, with the prognostic relevance decreasing or even disappearing after adjustment for confounders factors such as general condition, nutritional status, and dialysis adequacy. However, we did not find an association between hyperkalemia and the risk of all-cause and cardiovascular mortality. The lower rate of comorbid hyperkalaemia and the lower severity of hyperkalaemia in the patients included in our study may explain the non-significant association between hyperkalaemia and the risk of all-cause and cardiovascular mortality.
Previous studies have also found that the rapid decline in serum potassium levels during and after a dialysis session is associated with an increased in frequency of ventricular premature depolarizations and other electrocardiographic alterations15–17. These studies suggest that in addition to serum potassium levels assessed by baseline, average or peak values, fluctuations of serum potassium levels are also associated with clinical outcomes in MHD patients.
To date, an increasing number of studies have reported that serum potassium variability is an important predictor of mortality. Retrospective studies with large cohorts in ICU patients conducted by Hessels et al.20 and Engelhardt et al.19 reported an association of higher serum potassium variability with an increase risk of mortality. A consistent result was also found for the association between in-hospital mortality and serum potassium fluctions in patients with acute myocardial infarction21. Similar findings were observed by Xu et al.25 and Li et al.37 in peritoneal dialysis (PD) patients, where serum potassium variability was independently associated with both all-cause and cardiovascular mortality. Compared to PD patients, MHD patients suffer from more frequent fluctuations in serum potassium levels. However, only a few studies have investigated in the association between serum potassium variability and mortality in MHD patients. A recent study included 45 dialysis centre in China showed a significant association between higher facility-level potassium variability and poorer prognosis in MHD patients23. Yamaguchi et al.22 reported that serum potassium variability was an independent risk factor for all-cause mortality in MHD patients, but there was no association with cardiovascular death in their study.
The restricted cubic regression was consistent with these results, showing an increased risk with higher serum potassium variability in unadjusted model. And in further investigation, our results were consistent with previous findings that higher serum potassium variability was a predictor of prognosis in MHD patients, associated with higher survival from both all-cause and cardiovascular death and it was an independent risk factor associated with both all-cause and cardiovascular mortality in MHD patients. These results could be directly explained by instability of membrane resting potential caused by potassium fluctuations. And it is also possible that higher potassium variability indicates the poorer nutritional and health status in MHD patients and indirectly leads to adverse outcomes in MHD patients.
Furthermore, Lombardi et al.18 first demonstrated that higher serum potassium variability was associated with increased in-hospital mortality independent of the presence of hyperkalemia or hypokalemia in a large cohort of inpatients within normal serum potassium concentration range. Thus, we performed a subgroup analysis in MHD patients within normokalemia and our results are aligned with certain aspects of Lombardi et al.18. We confirmed that the association between serum potassium variability and the survival rate of all-cause and cardiovascular mortality in MHD patients was statistical significance even in the normal range. We also confirmed that serum potassium fluctuations were an independent risk factor for cardiovascular mortality in MHD patients within normokalemia. However, unlike Lombardi et al.18, our study showed no statistical significance of this association of all-cause mortality in hemodialysis patients after adjusting for confounders such as age, medication use, comorbidities, nutritional status and serum potassium levels. The differences could be explained by different study population and sample size. These results suggest that increased potassium variability may be associated with cardiovascular events and indicate an unstable condition in MHD patients. Early identification of factors that may cause potassium fluctuations, such as nutritional status and health condition, may be beneficial in improving the prognosis in MHD patients. One of the strengths of our study is that we grouped potassium variability according to the restricted cubic regression model which showed a non-linear relationship between serum potassium variability and all-cause mortality. Additional studies are needed to further investigate the association between potassium variability and mortality in MHD patients, especially normal serum potassium concentration range.
Limitations
Our study has several limitations. First, due to the nature of observational and retrospective study, a direct causal relationship cannot be inferred from our results. In addition, the three campus of our center may have differences in patient characteristics, dialysis prescriptions and potassium management, which was expected to reduce the selection bias. However, the sample size of this study is relatively small. Therefore, prospective studies with a large cohort are needed to confirm our findings in the future. Second, because of incomplete data collection due to the limitations of retrospective studies or different laboratory values used to assess the same status in different campus, factors that affect serum potassium levels, such as inflammation, residual renal function, dry weight, adequacy of dialysis and dietary intake were not included in this analysis. Other confounders such as blood pressure especially after weekend dialysis and left ventricular mass index, which were considered associated with increased CV events38, were also needed to pay attention to in further study. Finally, our study only collected serum potassium levels measured immediately before dialysis, which may resulted in missing abnormal potassium levels between visits and affected the evaluation of potassium variability. And MHD patients experience cyclical serum potassium fluctuations with a rapid decline during a dialysis session, changes in serum potassium levels after dialysis may also play an important role in prognosis which were not collected in this study and further studies are needed. Neverthless, to the best of our knowledge, this is the first study to analysis the association between serum potassium variability and prognosis in MHD patients within normal serum potassium concentration range, providing a new insight for clinical practice and further studies in optimizing the management of serum potassium in MHD patients.
Conclusions
Serum potassium variability was a predictor of prognosis associated with all-cause and cardiovascular mortality even in normal range in MHD patients. More attention should be paid to the role of reducing potassium fluctuations in MHD patients in clinical practice and further studies are desired to confirming the causal association between potassium variability and prognosis in MHD patients.
Acknowledgements
The authors thank the investigators and study nurses of dialysis center, Renji Hospital, Shanghai Jiao Tong University School of Medicine.
Abbreviations
- MHD
Maintenance hemodialysis
- CVSP
Coefficient of variation of serum potassium levels
- CI
Confidence interval
- ICU
Intensive care unit
- BMI
Body mass index
- ACEI/ARB
Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers
- ALP
Alkaline phosphatas
- URR
Urea reduction radio
- SD
Standard deviation
- HR
Hazard ratio
Author contributions
RM, MZ and WZ contributed to the conception and design of the study. RM, MZ and JW performed the statistical analysis and interpreted the data. PL, SL, YZ, RL and HP participated in acquiring the data. WZ and LG supervised data interpretation. RM and MZ wrote and revised the manuscript. WZ critically reviewed and improved the drafts of manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by an investigator initiated trial granted by Renji Hospital, Shanghai Jiaotong University School of Medicine (KY2022-021-B) and Hospital-pharma Integration Project on Innovation-boosting Expertise Training (SHDC2022CRS030) by Shanghai Hospital Development Center.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Ru Men and Minxia Zhu.
References
- 1.Bansal, S. & Pergola, P. E. Current management of hyperkalemia in patients on dialysis. Kidney Int. Rep.5, 779–789 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shibata, S. & Uchida, S. Hyperkalemia in patients undergoing hemodialysis: its pathophysiology and management. Ther. Aphere. Dial.26, 3–14 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwagami, M. et al. Association of hyperkalemia and hypokalemia with patient characteristics and clinical outcomes in Japanese hemodialysis (HD) patients. J. Clin. Med.12, (2023). [DOI] [PMC free article] [PubMed]
- 4.Huang, N. et al. Mediation of serum albumin in the association of serum potassium with mortality in Chinese dialysis patients: a prospective cohort study. Chin. Med. J.136, 213–220 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bem, D. et al. The effect of hyperkalemia and long inter-dialytic interval on morbidity and mortality in patients receiving hemodialysis: a systematic review. Ren. Fail.43, 241–254 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karaboyas, A. et al. Hyperkalemia excursions are associated with an increased risk of mortality and hospitalizations in hemodialysis patients. Clin. Kidney J.14, 1760–1769 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossignol, P. et al. Hyperkalaemia prevalence, recurrence and management in chronic haemodialysis: a prospective multicentre French regional registry 2-year survey. Nephrol. Dial. Transpl.32, 2112–2118 (2017). [DOI] [PubMed] [Google Scholar]
- 8.Agiro, A. et al. The prevalence of predialysis hyperkalemia and associated characteristics among hemodialysis patients: the RE-UTILIZE study. Hemodial. Int.26, 397–407 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss, J. N., Qu, Z. & Shivkumar, K. Electrophysiology of hypokalemia and hyperkalemia. Circulation Arrhythmia Electrophysiol.10, (2017). [DOI] [PMC free article] [PubMed]
- 10.de Rooij, E. N. M. et al. Serum potassium and mortality risk in hemodialysis patients: a cohort study. Kidney Med.4, (2022). [DOI] [PMC free article] [PubMed]
- 11.Kovesdy, C. P. et al. Serum and dialysate potassium concentrations and survival in hemodialysis patients. Clin. J. Am. Soc. Nephrol.2, 999–1007 (2007). [DOI] [PubMed] [Google Scholar]
- 12.Tafesse, E. et al. Serum potassium as a predictor of adverse clinical outcomes in patients with increasing comorbidity burden. Eur. Heart J. Qual. Care Clin. Outcomes8, 61–69 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoppe, L. K. et al. Association of abnormal serum potassium levels with arrhythmias and cardiovascular mortality: a systematic review and meta-analysis of observational studies. Cardiovasc. Drugs Ther.32, 197–212 (2018). [DOI] [PubMed] [Google Scholar]
- 14.Pun, P. H., Lehrich, R. W., Honeycutt, E. F., Herzog, C. A. & Middleton, J. P. Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics. Kidney Int.79, 218–227 (2011). [DOI] [PubMed] [Google Scholar]
- 15.Santoro, A. et al. Patients with complex arrhythmias during and after haemodialysis suffer from different regimens of potassium removal. Nephrol. Dial. Transpl.23, 1415–1421 (2008). [DOI] [PubMed] [Google Scholar]
- 16.Morrison, G., Michelson, E. L., Brown, S. & Morganroth, J. Mechanism and prevention of cardiac arrhythmias in chronic hemodialysis patients. Kidney Int.17, 811–819 (1980). [DOI] [PubMed] [Google Scholar]
- 17.Buemi, M. et al. The effect of two different protocols of potassium haemodiafiltration on QT dispersion. Nephrol. Dial. Transpl.20, 1148–1154 (2005). [DOI] [PubMed] [Google Scholar]
- 18.Lombardi, G., Gambaro, G. & Ferraro, P. M. Serum potassium variability is associated with increased mortality in a large cohort of hospitalized patients. Nephrol. Dial Transpl.37, 1482–1487 (2022). [DOI] [PubMed] [Google Scholar]
- 19.Engelhardt, L. J. et al. Association between potassium concentrations, variability and supplementation, and in-hospital mortality in ICU patients: a retrospective analysis. Ann. Intensive Care9, 100 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hessels, L. et al. The relationship between serum potassium, potassium variability and in-hospital mortality in critically ill patients and a before-after analysis on the impact of computer-assisted potassium control. Crit. Care19, 4 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiyovich, A., Gilutz, H. & Plakht, Y. Potassium fluctuations are associated with inhospital mortality from acute myocardial infarction. Soroka acute myocardial infarction II (SAMI-II) project. Angiology69, 709–717 (2017). [DOI] [PubMed] [Google Scholar]
- 22.Yamaguchi, K. et al. Association between annual variability of potassium levels and prognosis in patients undergoing hemodialysis. Clin. Exp. Nephrol.27, 873–881 (2023). [DOI] [PubMed] [Google Scholar]
- 23.Zhao, X. et al. High facility-level serum potassium variability associated with mortality in hemodialysis patients: results from Chinese dialysis outcomes and practice patterns study (DOPPS). Ren. Fail.45, (2023). [DOI] [PMC free article] [PubMed]
- 24.Clase, C. M. et al. Potassium homeostasis and management of dyskalemia in kidney diseases: conclusions from a kidney disease: Improving global outcomes (KDIGO) controversies conference. Kidney Int.97, 42–61 (2020). [DOI] [PubMed]
- 25.Xu, Q. et al. Serum potassium levels and its variability in incident peritoneal dialysis patients: associations with mortality. PLoS ONE9, e86750 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foley, R. N. et al. The impact of anemia on cardiomyopathy, morbidity, and and mortality in end-stage renal disease. Am. J. Kidney Dis.28, 53–61 (1996). [DOI] [PubMed] [Google Scholar]
- 27.Locatelli, F. et al. Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the dialysis outcomes and practice patterns study (DOPPS). Nephrol. Dial. Transpl.19, 121–132 (2004). [DOI] [PubMed] [Google Scholar]
- 28.Ma, J. Z., Ebben, J., Xia, H. & Collins, A. J. Hematocrit level and associated mortality in hemodialysis patients. J. Am. Soc. Nephrol.10, 610–619 (1999). [DOI] [PubMed] [Google Scholar]
- 29.Ma, L. & Zhao, S. Risk factors for mortality in patients undergoing hemodialysis: a systematic review and meta-analysis. Int. J. Cardiol.238, 151–158 (2017). [DOI] [PubMed] [Google Scholar]
- 30.Brunelli, S. M. et al. History-adjusted marginal structural analysis of the association between hemoglobin variability and mortality among chronic hemodialysis patients. Clin. J. Am. Soc. Nephrol.3, 777–782 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eckardt, K. U. et al. Hemoglobin variability does not predict mortality in European hemodialysis patients. J. Am. Soc. Nephrol.21, 1765–1775 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang, W. et al. Hemoglobin variability and mortality in ESRD. J. Am. Soc. Nephrol.18, 3164–3170 (2007). [DOI] [PubMed] [Google Scholar]
- 33.Wang, H. H. et al. Hypokalemia, its contributing factors and renal outcomes in patients with chronic kidney disease. PLoS ONE8, e67140 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yin, S. et al. Multifactorial analysis of renal anemia-associated substandard hemoglobin levels and prevalence of anemia in patients on maintenance hemodialysis in Liaoning province: a cross-sectional study. Ann. Palliat. Med.11, 3743–3754 (2022). [DOI] [PubMed] [Google Scholar]
- 35.Mittman, N., Avram, M. M., Oo, K. K. & Chattopadhyay, J. Serum prealbumin predicts survival in hemodialysis and peritoneal dialysis: 10 years of prospective observation. Am. J. Kidney Dis.38, 1358–1364 (2001). [DOI] [PubMed] [Google Scholar]
- 36.Sreedhara, R. et al. Prealbumin is the best nutritional predictor of survival in hemodialysis and peritoneal dialysis. Am. J. Kidney Dis.28, 937–942 (1996). [DOI] [PubMed] [Google Scholar]
- 37.Li, S. H. et al. Time-averaged serum potassium levels and its fluctuation associate with 5-year survival of peritoneal dialysis patients: two-center based study. Sci. Rep.5, 15743 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Io, H. et al. Relationship among left ventricular hypertrophy, cardiovascular events, and preferred blood pressure measurement timing in hemodialysis patients. J. Clin. Med.9, (2020). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.